Abstract
We report a case of a stress fracture of the scapular spine which developed as a late complication of a reverse shoulder arthroplasty. After initially doing well after surgery, our patient developed pain and decreased shoulder function. A nondisplaced scapular spine fracture was noted on radiographs. Because reverse shoulder arthroplasty is a relatively new procedure in this country, radiologists may be unfamiliar with its potential complications. Stress or insufficiency fractures of the scapular spine and acromion are a potential complication of reverse shoulder arthroplasty, due to increased functional demands of the deltoid muscle, which is often combined with deficiency of acromial bone due to rotator cuff arthropathy and osteopenia.
Abbreviations: CT, computed tomography
Introduction
The reverse shoulder arthroplasty is a relatively new procedure which has been performed in the United States since 2004. The device is indicated for use in patients who have irreparable rotator cuff damage, arthropathy and pain and severe limitation in shoulder function [1, 2]. Revision arthroplasty is the second most common indication. This prosthesis can also be utilized for reconstruction after surgery for infection and tumor [3]. In patients with large rotator cuff tears, traditional total shoulder arthroplasties are not used because of tendency for rapid loosening of the glenoid component, which occurs in the absence of the stabilizing effect of the rotator cuff. The main advantage of the reverse shoulder prosthesis over conventional total shoulder prosthesis is the transfer of the center of rotation of the shoulder joint distally and medially, allowing the deltoid muscle to assume greater control over humeral motion [4]. This alteration in the center of rotation is accomplished by reversing the standard ball and socket configuration of the shoulder. The reverse shoulder prosthesis consists of a cup shaped proximal humeral component that articulates with a ball shaped glenoid component (“glenosphere”) attached to a base plate (“metaglene”) which is fixed to the native glenoid with screws [5, 6].
Case Report
A 73-year-old male presented with shoulder pain and limited range of motion. He had a history of rotator cuff repair approximately 25 years prior. After that surgery he continued to have pain and weakness, and felt that he never completely regained strength in his shoulder. More recently, he noted increasing pain and progressively decreasing range of motion of the shoulder. This was treated with physical therapy without improvement. Radiographs and a CT (Figure 1) were obtained revealing a lytic lesion in the right humeral head with an associated soft tissue mass. Biopsy revealed a giant cell tumor. In addition to the tumor, a preoperative MRI (Figure 2) also showed a recurrent full thickness tear of the supraspinatus and infraspinatus tendons with significant medial retraction of the torn tendons and severe muscle atrophy. Physical exam revealed a man with a well healed anterior right shoulder incision, who was otherwise fairly healthy. The right shoulder had limited range of motion with approximately 30 degrees of elevation, 40 degrees of abduction, and 50 degrees of external rotation. There was marked weakness in abduction and external rotation. He had significant subacromial crepitus.
Figure 1.
Coronal reconstructed CT of the right shoulder demonstrating a lytic lesion with a sclerotic border (arrow) involving the humeral head. [Powerpoint Slide]
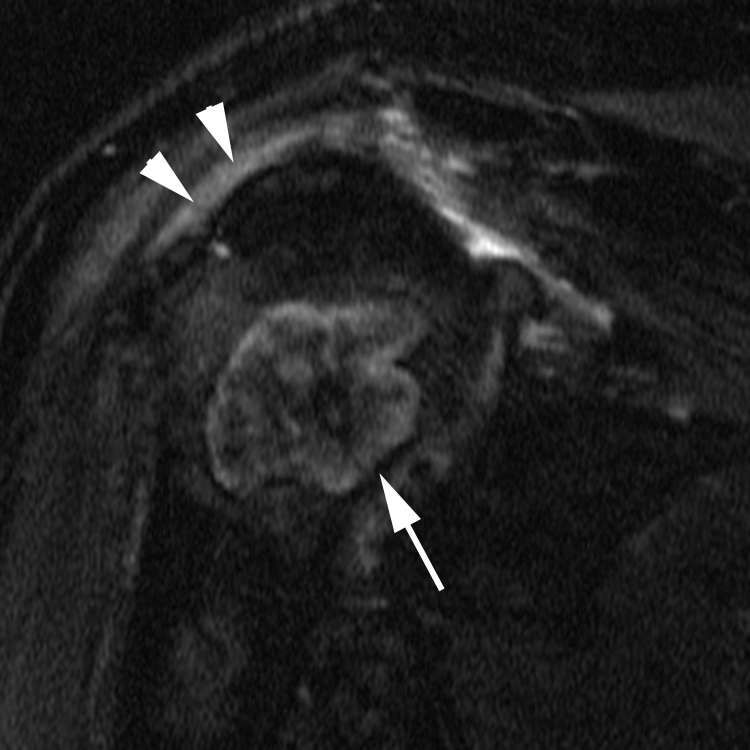
Figure 2.
Coronal T2-weighted, fat suppressed MR image of the right shoulder also demonstrating the humeral head lesion (arrow). Abnormal signal involving the rotator cuff (arrowheads) was confirmed to represent full thickness tearing on additional images. Study was degraded by patient motion. [Powerpoint Slide]
Because of his irreparable rotator cuff tear, a reverse shoulder arthroplasty was performed (Figure 3) rather than a conventional total shoulder arthroplasty at the time of the giant cell tumor resection. The patient did well postoperatively, and at three months was essentially pain free, with markedly improved shoulder mobility. Physical exam revealed 150 degrees of elevation, 140 degrees of abduction, and 30 degrees external rotation. The patient returned at four months post surgery with recurrent pain, which began after a day of heavy yard work and digging. He reported swelling, which had subsequently resolved, with persistent pain and decreased range of motion. Physical exam at that time revealed only 20 degrees of active elevation and abduction. Radiographs demonstrated a mildly displaced scapular spine fracture (Figure 4). He was treated with rest, analgesics and physical therapy. Repeat radiographs at six months post op showed mild progressive inferior displacement of the fracture (Figure 5). The patient was treated nonoperatively and regained function with physical therapy, but reported persistent pain with use of the shoulder at 3 year follow up.
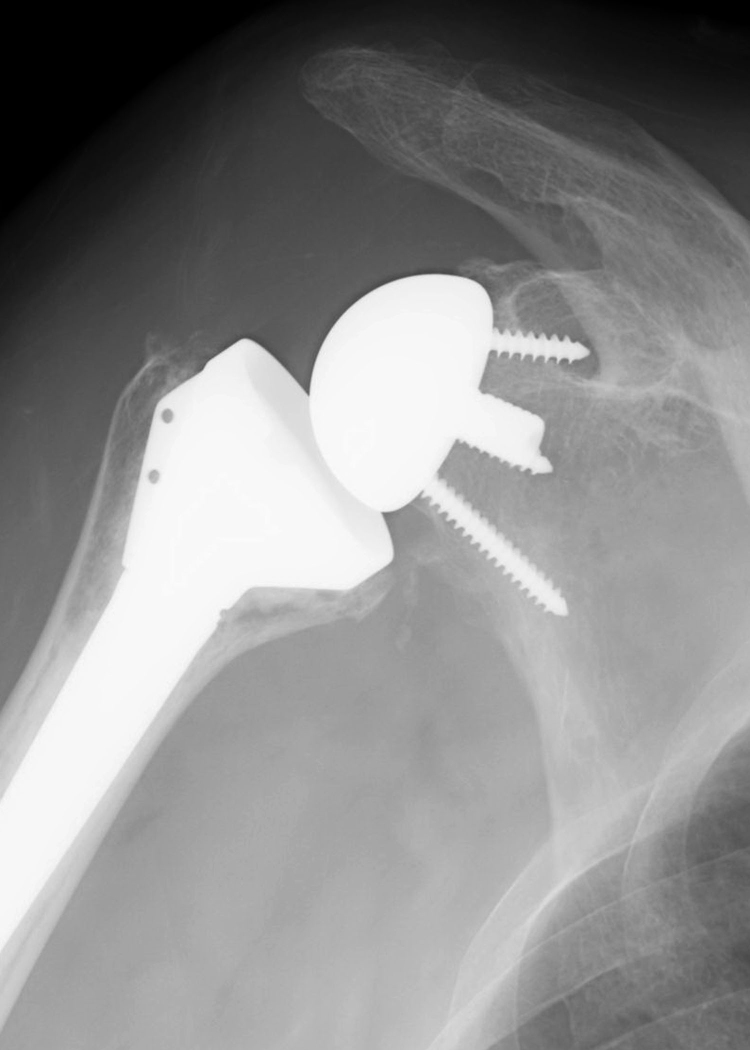
Figure 3.
Initial radiographs of the reverse shoulder prosthesis were normal. [Powerpoint Slide]
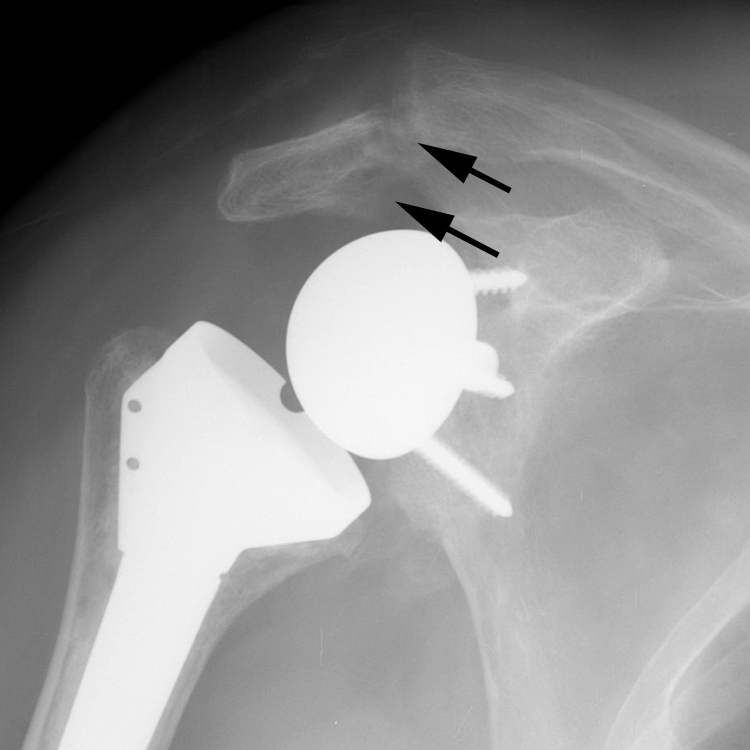
Figure 4.
Mildly displaced scapular spine fracture (arrows) at four months post op, becoming clinically evident after heavy yard work. [Powerpoint Slide]
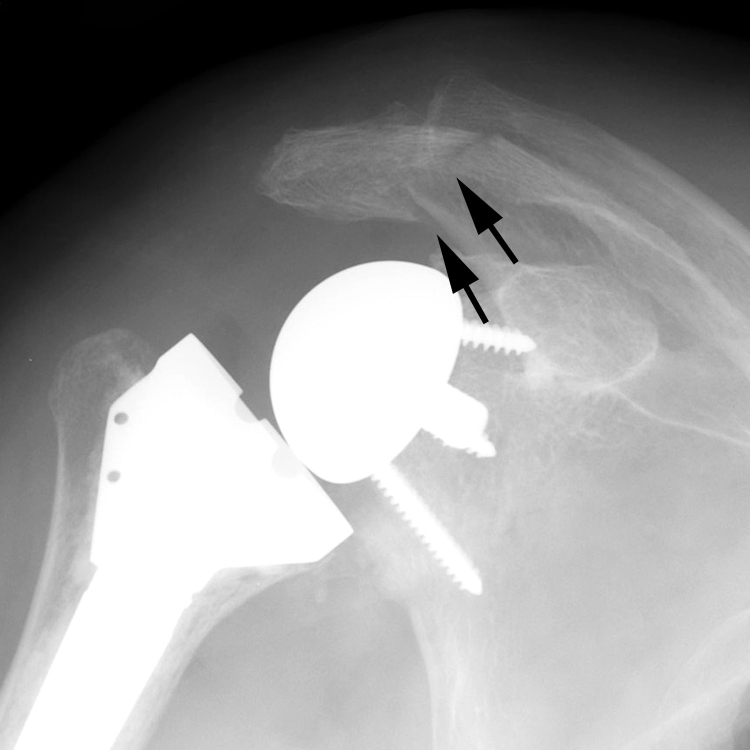
Figure 5.
Progressively displaced scapular spine fracture (arrows) at six months post op. [Powerpoint Slide]
Discussion
Experience with reverse shoulder arthroplasty and its complications since the US release in 2004 are limited but evolving. More extensive European experience with earlier versions of the reverse shoulder prosthesis is documented in the literature. Some of the more frequently reported radiographically evident complications include dislocation, infection, loosening, malpositioning, and impingement of the inferior glenoid by the humeral component leading to scapular erosion or notching [7, 8, 9, 10]. Stress fracture of the scapular spine has also been infrequently reported as a late complication after reverse shoulder arthroplasty [11]. Boileau et al observed two acromial fractures that appeared as incidental findings on the three-month postoperative radiographs [11]. In their study, neither patient could recall any trauma, both were completely asymptomatic, and there did not appear to be any detrimental effect on function. Werner et al reported four cases of acromial or scapular spine fracture in a series of 58 consecutive patients with reverse shoulder arthroplasty [8]. All four of their patients were treated successfully, two with open reduction and internal fixation with tension banding and the other two treated conservatively [8]. This is in contradistinction to our patient, who had progressive pain and disfunction which worsened as his degree of inferior acromial displacement progressed.
Pathogenesis
The etiology of scapular spine/acromial fractures in the setting of reverse shoulder arthroplasty has been postulated to be related to added stress on the scapular spine at the attachment of the deltoid muscle. The deltoid muscle confers a greater load to the acromion as it assumes a greater role for shoulder abduction and flexion in patients with the reverse shoulder arthroplasty. Patients with rotator cuff arthropathy also often have osteoporosis and eroded acromial bone, additionally predisposing them to a scapular spine fracture, which would be more accurately termed an insufficiency fracture. Over tensioning of the deltoid muscle at surgery may also predispose to acromial fracture, and may result in a slight and permanent abduction of the arm with inability for the patient to adduct the arm at the side.
Imaging
Scapular spine and acromial fractures may be difficult to detect on standard shoulder radiographs unless they are displaced or there is periosteal reaction/callus formation. Significant inferior displacement of the fractured scapular spine may occur due to the inferior pull of the deltoid muscle. An interpretation checklist for radiologic evaluation of reverse shoulder arthroplasty can be helpful for those not familiar with these prostheses (Table 1) [2]. Of note, the search for fractures was included on this checklist when it was initially published, but scapular spine and acromial complications were not specifically mentioned.
Table 1.
Interpretation checklist for evaluation of a reverse shoulder arthroplasty
|
(Table 1 reproduced with permission from Roberts CC, Ekelund AL, Renfree KJ, Liu PT, Chew FS. Radiologic assessment of reverse shoulder arthroplasty. Radiographics. 2007 Jan-Feb;27(1): 223-35.)
Treatment
Treatment of scapular spine/acromial fractures in patients with reverse shoulder arthroplasty has not yet been established due to the relative lack of experience with this procedure and its complications. Treatment options include conservative treatment with shoulder immobilization to allow fracture healing. In patients with distal acromial fractures, thus conservative management is typically employed. Open reduction and internal fixation may be indicated in some patients with scapular spine fractures [12]. Untreated inferior displacement of the acromion may decrease the resting length of the deltoid and further decrease shoulder elevation and abduction. Asymptomatic patients may not require any treatment
Conclusion
Reverse shoulder arthroplasty is a relatively new treatment option for patients with irreparable rotator cuff pathology. Although many patients experience significant improvement in pain and function, complications are frequent and the radiologist should be aware of normal and abnormal imaging appearances of the reverse shoulder prosthesis to facilitate prompt diagnosis. Fractures of the scapular spine and acromion, which are otherwise uncommon, can be seen more frequently in patients with reverse shoulder arthroplasty likely due to a combination of exaggerated acromial stress from increased deltoid muscle load and inherently weakened acromial bone from longstanding rotator cuff arthropathy.
Footnotes
Published: June 27, 2007
References
- 1.Rockwood CA., Jr. The reverse total shoulder prosthesis. The new kid on the block. J Bone Joint Surg Am. 2007 Feb;89(2):233–235. doi: 10.2106/JBJS.F.01394. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Roberts CC, Ekelund AL, Renfree KJ, Liu PT, Chew FS. Radiologic assessment of reverse shoulder arthroplasty. Radiographics. 2007 Jan-Feb;27(1):223–235. doi: 10.1148/rg.271065076. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.De Wilde L, Sys G, Julien Y, Van Ovost E, Poffyn B, Trouilloud P. The reversed Delta shoulder prosthesis in reconstruction of the proximal humerus after tumour resection. Acta Orthop Belg. 2003 Dec;69(6):495–500. [PubMed] [PubMed] [Google Scholar]
- 4.De Wilde LF, Audenaert EA, Berghs BM. Shoulder prostheses treating cuff tear arthropathy: a comparative biomechanical study. J Orthop Res. 2004 Nov;22(6):1222–1230. doi: 10.1016/j.orthres.2004.03.010. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993 Jan;16(1):65–68. doi: 10.3928/0147-7447-19930101-11. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005 Jan-Feb;14(1 Suppl S):147S–161S. doi: 10.1016/j.jse.2004.10.006. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004 Apr;86(3):388–395. doi: 10.1302/0301-620x.86b3.14024. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005 Jul;87(7):1476–1486. doi: 10.2106/JBJS.D.02342. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Simovitch RW, Zumstein MA, Lohri E, Helmy N, Gerber C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg Am. 2007 Mar;89(3):588–600. doi: 10.2106/JBJS.F.00226. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.McFarland EG, Sanguanjit P, Tasaki A, Keyurapan E, Fishman EK, Fayad LM. The reverse shoulder prosthesis: A review of imaging features and complications. Skeletal Radiol. 2006 Jul;35(7):488–496. doi: 10.1007/s00256-006-0109-1. [PubMed] [DOI] [PubMed] [Google Scholar]
- 11.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006 Sep-Oct;15(5):527–540. doi: 10.1016/j.jse.2006.01.003. [PubMed] [DOI] [PubMed] [Google Scholar]
- 12.Matsen FA, 3rd, Boileau P, Walch G, Gerber C, Bicknell RT. The reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2007 Mar;89(3):660–667. doi: 10.2106/00004623-200703000-00027. [PubMed] [DOI] [PubMed] [Google Scholar]