Abstract
Objective. To evaluate the impact of an interprofessional blended learning course on medical and pharmacy students’ patient-centered interpersonal communication skills and to compare precourse and postcourse communication skills across first-year medical and second-year pharmacy student cohorts.
Methods. Students completed ten 1-hour online modules and participated in five 3-hour group sessions over one semester. Objective structured clinical examinations (OSCEs) were administered before and after the course and were evaluated using the validated Common Ground Instrument. Nonparametric statistical tests were used to examine pre/postcourse domain scores within and across professions.
Results. Performance in all communication skill domains increased significantly for all students. No additional significant pre/postcourse differences were noted across disciplines.
Conclusion. Students’ patient-centered interpersonal communication skills improved across multiple domains using a blended learning educational platform. Interview abilities were embodied similarly between medical and pharmacy students postcourse, suggesting both groups respond well to this form of instruction.
Keywords: blended learning, communication skills, objective structured clinical examinations
INTRODUCTION
Effective communication is paramount to practicing patient-centered care, and cultivating this skill is a vital component in the training of all health care students. Medical and pharmacy school accreditation bodies recognize the importance of this competency in the training of future clinicians as programmatic curricula incorporating the formalized instruction of interpersonal communication skills are mandatory.1,2 From a physician’s perspective, patient-centered care “seeks to focus medical attention on the individual patient’s needs and concerns, rather than the doctor’s.”3
This general definition could easily apply to pharmacists and other health professionals as well. The concept of delivering patient-centered care is at the heart of health care reform, and cultivating a clinician-patient relationship is a foundation for its successful deployment. Exemplary communication skills are the ultimate in patient-centeredness, and the emphasis of the course is to truly help students of all disciplines begin to focus on the issues of the patient primarily. Yet, learning to balance clinician-centered aspects (ie, diagnosis, medications) of communication with patient-centered aspects (ie, fears, concerns, expectations) and performing them at a competent level requires instruction and regular practice for the student learner.
Suggested pedagogical methods to teach communication skills are varied and can involve observation (real time or recorded), self-assessment, role-playing, and role modeling.4 Experiential-based instruction with feedback improves student communication competencies over traditional or instructional-based formats.5 Yet, few studies have been conducted comparing two or more experiential methods in communication training. One study evaluating standardized patients (SP) and peer role-playing concluded both methods improved self-efficacy and objective structured clinical examination (OSCE) scores, however the role-play technique led to higher empathic responses.6
Many training institutions have employed SP interactions for experiential learning.7-10 This type of interaction is preferred over actual patients because a SP can be a helpful ally in teaching and assessment.11 However, early learners also need exposure to traditional instructional methods to introduce desirable and effective core communication concepts. One approach to delivery is using a blended learning format whereby students first learn and observe basic communication skills on their own time and follow that with an experiential component. With this approach, students come prepared to practice learned patient-centered communication techniques and receive feedback, which uses the training time more efficiently.
Blended learning, a form of e-learning using electronic media, is defined as “the thoughtful integration of classroom face-to-face learning experiences with online learning experiences.”12 The online component may be classified as either synchronous (eg, videoconferencing, instant messaging, chat) or asynchronous (eg, web-based presentations, lectures or modules, e-mail, blogs). Advantages of blended learning formats compared to traditional learning formats are that they are valued by self-directed adult learners, help overcome the limitations of meeting time and space, reach a larger number of students, support instructional methods hard to achieve using textbooks, save training costs, produce high student ratings, increase student perceptions of achieving course objectives, and achieve academic results equivalent to strict face-to-face teaching.13-16
Blended learning is used in health education to teach a broad scope of subject matter such as acute care, pediatrics, otolaryngology, cardiovascular pharmacotherapy, oral radiology, orthodontics, respiratory care, research ethics, and interprofessional team development.14,16-23 There is also “rudimentary” evidence that blended learning strategies can help students improve their clinical competencies.24 Health professions students express acceptance using e-learning methods and view its role as complementary to, but not entirely substitutionary for, traditional face-to-face faculty-led instruction.25-27
Communication Skills for Health Professionals is a 2-credit hour course at East Tennessee State University’s (ETSU) Academic Health Science Center (AHSC) and has been previously described in the Journal.28 Briefly, course enrollment is interdisciplinary and consists of medical, nursing, pharmacy, and psychology students divided into small groups (6-7 students per group) containing representation from at least three colleges. The small groups are led by a diverse group of faculty members with appointments at one or more of the participating colleges.
The biweekly format employs asynchronous, online, self-directed learning modules to teach core communication skills alternating with a live, 3-hour small group session. This schedule makes available most of the class time for student learners to interview SPs. An objective assessment of each student’s communication skills is measured by trained faculty members during mid-point and end-of-course OSCEs. Our research objective was to determine the effectiveness of this blended course design in teaching medical and pharmacy student patient-centered interpersonal communication skills and compare the results across disciplines. To our knowledge, this is the first study to measure the effectiveness of a blended learning format to teach patient-centered communication.
METHODS
An e-mail was sent to all enrolled incoming first-year medical and second-year pharmacy students about three weeks before the start of the course inviting them to participate in the study. The e-mail contained a description of the study objectives along with a disclaimer that the interviews would be timed and recorded in a format identical to the final OSCE examination, but not viewed until course completion to avoid potential biasing of faculty members toward any participant based on precourse OSCE performance. In addition, students were instructed that their precourse OSCE scores would not affect their grade. No rewards or incentives were given to participants. Nursing and psychology students were not included because their academic calendars began later and did not allow sufficient time for precourse research activities.
Two discipline-specific, precourse recording schedules were held in August 2012. On the day of their scheduled interview, students were given eight minutes to interview an SP without interruptions. A “door chart” provided the reason for the patient visit (to talk about quitting smoking) and was the only information shared with the student prior to the start of the interview. No instructional feedback was given when finished.
The SPs were recruited from the ETSU Standardized Patient Program and were given a smoking cessation case scenario that included instructions on how to portray the scene emotionally and how to divulge scripted “clues” reflecting the patient’s perspective of the situation. The case was written by course faculty members and has been used as part of the course’s final OSCE for several years. The subject of smoking cessation was chosen because it is a common health topic relevant to all health professions. The course is designed to ensure the patient-centered emotions, perspectives, and concerns are the focus rather than the student’s clinical knowledge base.
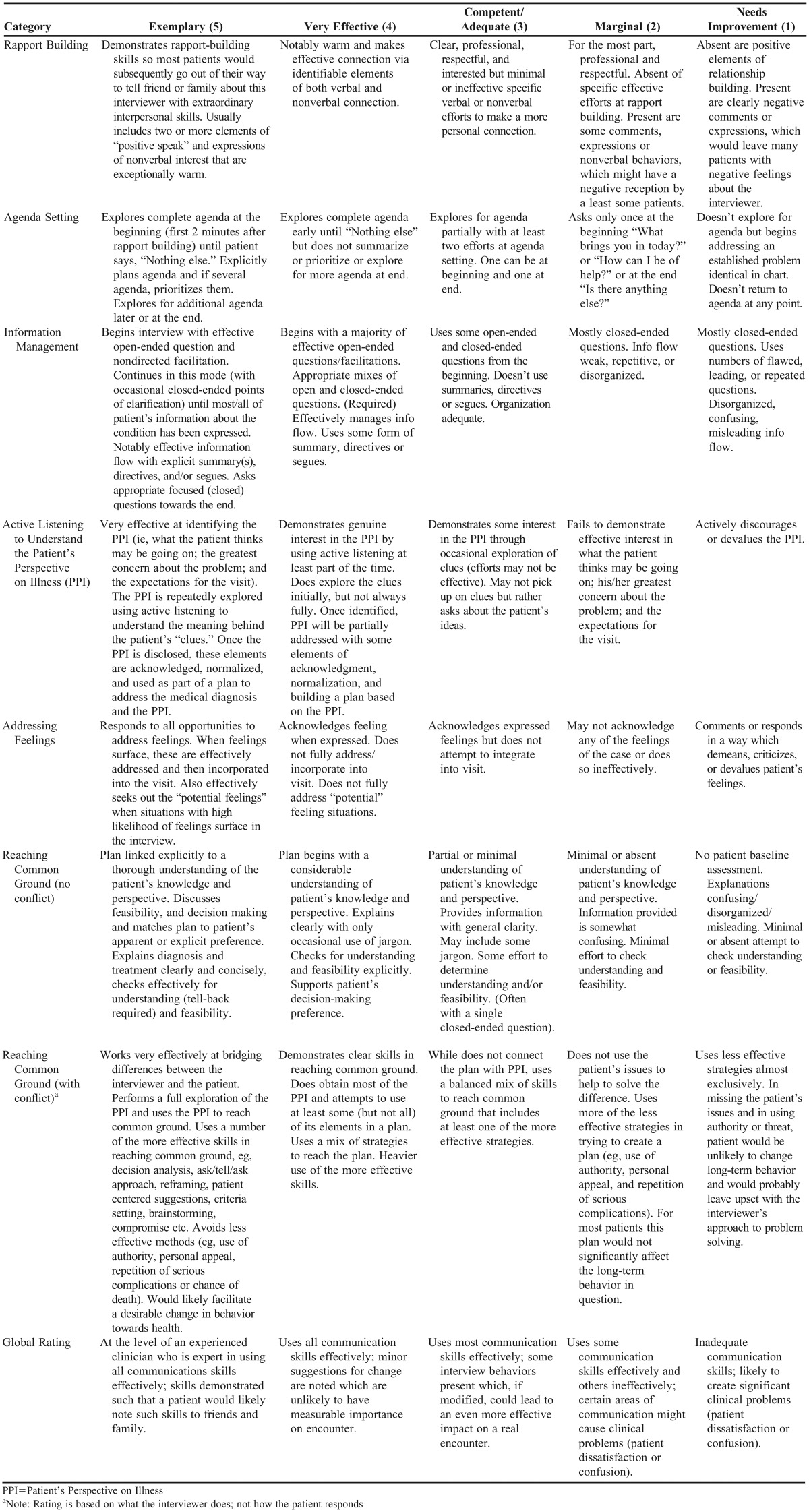
Prior to evaluating students, all evaluators completed a training session conducted by course coordinators that provided opportunities to use the validated Common Ground Rating Scale OSCE assessment tool.29 Evaluators watched a recorded interview and assessed six communication skill constructs (rapport building, agenda setting, information management, active listening, addressing feelings, and establishing common ground) as well as global interview performance using the Common Ground Rating Scale rubric (Table 1). Scores from the practice assessment training were compared to scores from communication experts to ensure inter-rater reliability. Course coordinators randomly selected and scored 10% of all pre/postcourse OSCEs to assess inter-rater reliability. Ratings were considered reliable if scores were within 20% for each communication skill construct. One evaluation was completed for each participant.
Table 1.
Communication Skills Domain Rating Categories and Observable Descriptions
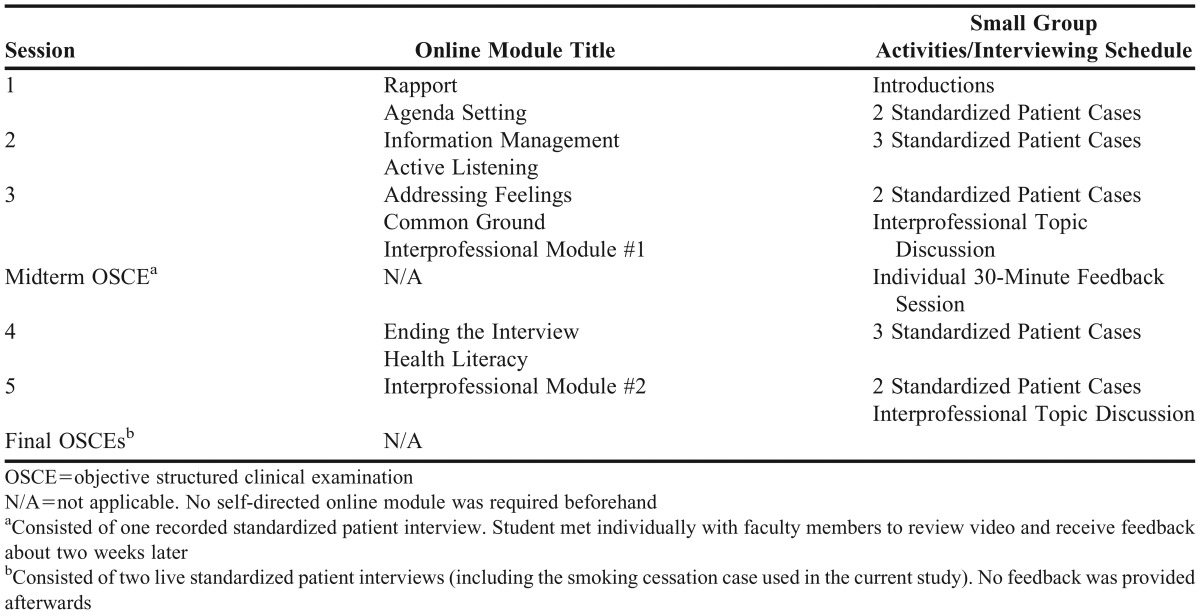
One week after completion of the precourse OSCE, 192 first-year medical, nursing, clinical psychology, and second-year pharmacy students began Communication Skills Health Professionals in the fall 2012 semester. Over the semester, students completed 10 online modules and attended five small group sessions (Table 2). Following the third small group session, all students completed a midterm OSCE. Faculty member provided feedback 1-2 weeks later to students during 30-minute individual appointments. The final OSCE consisted of two consecutive SP interviews with the last case identical to the precourse OSCE. Faculty members graded the interview performance live, but no postinterview feedback was provided. Again, one evaluation was completed for each participant and none of the pre/postcourse evaluators or SPs were identical.
Table 2.
Course Content and Schedule
Scores on pre/postcourse communication skill constructs and the global rating score were analyzed using SPSS, v22 (IBM, Armonk, NY). Descriptive statistics were calculated for all construct scores. All communication skill constructs were scored using the Common Ground Rating Scale rubric on a 1-5 scale (1=needs improvement; 2=marginal; 3=competent/adequate; 4=effective; 5=exemplary), with half-point increments allowed. Data were treated as interval-level variables. Means (standard deviations) and medians (interquartile ranges) were calculated for each communication skill construct. Nonparametric Mann-Whitney and Wilcoxon rank sum tests were used to compare paired pre/postcourse scores and pre/postcourse scores across colleges, respectively. An alpha level of 0.05 was set a priori. The East Tennessee State University Institutional Review Board approved the study.
RESULTS
One hundred twenty-four students (n=67 medicine, 66% male and 34% female; n=57 pharmacy, 39% male and 61% female) completed the OSCEs before and after the course, representing 79.4% of all medical and pharmacy students who were enrolled in the course.
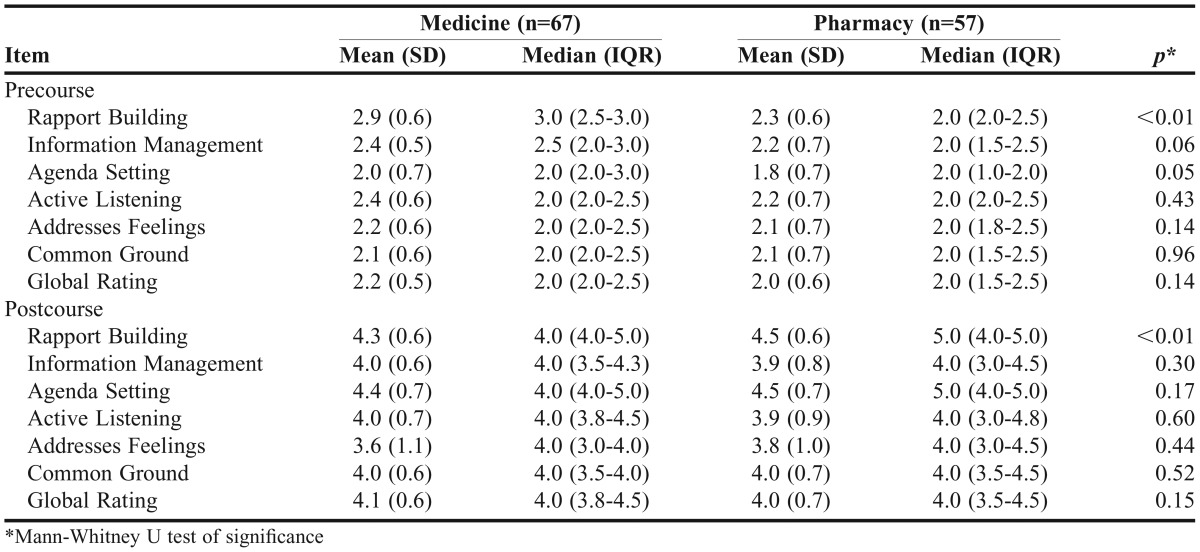
Precourse agenda setting, information management, active listening, addressing feelings, and establishing common ground construct scores were not significantly different when comparing medical to pharmacy students (Table 3). Precourse scores for the rapport building construct were significantly higher for medical students (median=3) compared to pharmacy students (median=2) (p<0.01). Median medical student scores ranged from 2 to 3 across all communication constructs, whereas all median values for pharmacy students were 2. Median global rating precource scores were 2 for both medical and pharmacy students.
Table 3.
Results for Medical and Pharmacy Students Before and After Communication Skills Course
Five of six postcourse communication skill construct scores were similar across medicine and pharmacy as was the global rating (Table 3). Rapport building scores were significantly higher for pharmacy students (median=5) compared to medical students (median=4, p<0.01). Median medical student postcourse scores were 4 across all communication constructs and the global rating. Median values for pharmacy students ranged from 4 to 5 across all communication constructs and the global rating.
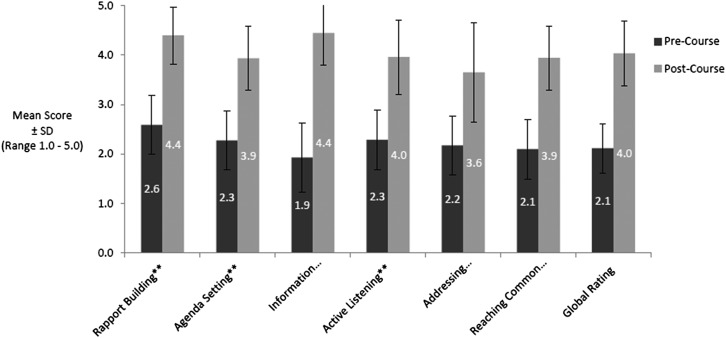
Communication skill construct scores and the global rating scores significantly increased for both medicine and pharmacy students postcourse compared to precourse (p values<0.01). Figure 1 presents pre/postcourse median scores across disciplines.
Figure 1.
Precourse vs Postcourse Mean Score for Combined Medicine and Pharmacy Students (n=124) ** p<0.01.
DISCUSSION
The blended learning course significantly improved medical and pharmacy students’ patient-centered communication skills. Similarities in communication domain scores indicate that this course increased both medical and pharmacy students’ patient-centered communication skill competency. In general, both medical and pharmacy students scored poorly in all communication skill domains at baseline. Medical students’ higher interpersonal skills coming into the course may be related to significantly better scores than pharmacy students in precourse rapport building. Pharmacy students, being less equipped for the patient-centered setting, may have benefited more from the practice and, therefore, showed significantly more improvement in that domain.
After the course, a large majority of students in both professions demonstrated patient-centered communication skills with SPs that were considered effective. Meaningful clinician-patient relationships, which are vital to fostering patient-centered care, were cultivated by the effective communication strategies emphasized in this course. The current project specifically evaluated patient interviewing skills in a smoking cessation case, a clinical scenario students will likely encounter at some point as learners and certainly as future clinicians. Yet, the patient-centered communication skills taught can be applied to diverse clinical situations.
Within the course itself, students interview SPs portraying clinical case examples such as addressing a depressed patient with or without suicide ideation, breaking bad news by informing a patient they have cancer, negotiating with a patient visit requesting narcotics refill during a first-time visit, and resolving an unintentional drug error that resulted in patient harm. While the course serves as a primer for early learners to practice patient-centered communication skills, regular exercise of the talents must be maintained or it will decline.5 Evaluation and assessment of the students’ skills beyond the course with other OSCE assessments and within direct patient care settings is needed.
Our results suggest the blended learning methods are effective regardless of student discipline. There are several aspects of the blended learning course that foster communication skill development, both in the online modules and during in-person class sessions. First, students are provided examples of effective and ineffective communication via videos embedded in online content prior to practicing with SPs. They also observe their classmates as they practice communication skills. Thus, students are given multiple opportunities to develop communication self-efficacy beliefs individually and through observation of classmates in groups. Having 6-7 students in each class session provides students and their facilitator with an intimate supportive environment. Students have multiple opportunities to receive peer, SP, and facilitator feedback in a formative, low stakes environment.
Bandura’s self-efficacy theory is defined as a belief that one possesses the capability to successfully perform a particular behavior or execute a specific task.30 Cultivating self-efficacy through education and training is a vital component to improving communication skills and has been demonstrated with medical students and residents.6,31,32 Pharmacy students have also demonstrated improved self-efficacy and reduced communication apprehension over time through using a variety of teaching methods on patient counseling.33 Our previous research with medical, nursing, and pharmacy students indicated self-efficacy beliefs specific to patient-centered communication skills improved significantly through successful completion of this course.28
Improved communication skills observed in this study is likely secondary to the blended learning format as it repeatedly incorporates all three learning styles for adult learners – visual, auditory, and kinesthetic. Visual learners are able to observe short communication vignettes embedded within the online modules and watch their peers interview. Auditory learners listen to the recorded dialogue examples from the online videos and hear themselves provide feedback during small group activities as well as from faculty members and peers. Finally, kinesthetic learners benefit from repeated interview practice using SPs and providing regular feedback in small group settings. Future research examining whether students’ self-efficacy scores correlate positively with OSCE assessments across disciplines would confirm if perception is reality.
Common objectives found in current Liaison Committee on Medical Education (LCME) and Accreditation Council for Pharmacy Education (ACPE) standards are proficiency in communication with patients, their members of support, and with other health care professionals.1,2 Considering communication accreditation standards for both disciplines, it is apparent that the core communication competencies across both professions are increasingly similar. Recent revisions to ACPE Standards included expectations that upon graduation, pharmacy students should be able to proficiently communicate both verbally and nonverbally, provide thorough patient counseling, and possess excellent listening skills.34
Few educational research studies use e-learning methods to teach any type of oral communication for health professional students. One randomized trial concluded that an e-learning module followed by coached practice time improved second-year medical students’ oral presentation skills.35 The blended learning format used in the course allowed students to come to the small groups already prepared, permitting more practice time for interviewing. It is not known if the blended learning format increases communication skills performance more than SP interaction alone or by computer-based learning alone. In addition, it is not known if interprofessional communication skills, which were introduced but not formally assessed, can be developed via this method equally across disciplines. That question can be answered with future research and deserves attention.
There are a few limitations to the study. First, the study is limited to one institution and therefore may not be generalizable to other medical and pharmacy students. The pharmacy student participants were entering their second professional year while the medical students were entering their first year, which is not ideal. However, no communication courses were taught during the first year of the pharmacy curriculum and baseline scores across both cohorts were similar. Another limitation to the study was the possibility that another intervention occurring during the 16-week study period could have positively impacted changes in communication skills in the cohorts. However, this course is the only course that targets communication skill development during the semester in which it is offered. Therefore, the authors feel confident that changes in communication skills were a direct result of the course.
Second, the interval descriptions found in the survey instrument may not have clearly conferred meaningful intervals between measurements as half-point increments were allowed when a blend of interviewing behaviors was observed. However, the use of a validated survey instrument strengthens the findings. Third, the current project evaluated patient-centered communication skills using a smoking cessation case in a test/retest design. Further research is warranted to evaluate the sustainability of the competencies across a myriad of clinical scenarios postcourse and at multiple academic health science centers. Fourth, the focus of instruction was on oral patient-centered interpersonal skills only and not on written communication. Finally, demographic information (eg, gender) and additional trait-level student characteristics (eg, personality type) that could potentially influence communication skills were not assessed in this study.
CONCLUSION
Medical and pharmacy student patient-centered interpersonal communication skills improved significantly through completion of an interprofessional, blended learning course focusing on skill development. Interview abilities were embodied similarly between medical and pharmacy students postcourse, suggesting both groups respond well to this form of instruction. The design employed in the course could be replicated in both interprofessional and discipline-specific environments.
REFERENCES
- 1.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. https://www.acpe-accredit.org/pdf/CPE_Standards_Final.pdf. Accessed March 10, 2015.
- 2.Liaison Committee on Medical Education. Functions and structure of a medical school: standards for accreditation of medical education programs leading to the MD degree. Revised March 2014. http://lcme.org/publications/. Accessed April 28, 2016.
- 3.Bardes CL. Defining “patient-centered medicine.”. N Engl J Med. 2012;366(9):782–783. doi: 10.1056/NEJMp1200070. [DOI] [PubMed] [Google Scholar]
- 4.Rider EA, Keefer CH. Communication skills competencies: definitions and a teaching toolbox. Med Educ. 2006;40(7):624–629. doi: 10.1111/j.1365-2929.2006.02500.x. [DOI] [PubMed] [Google Scholar]
- 5.Aspegren K. BEME. Guide No. 2: teaching and learning communication skills in medicine – a review with quality grading of articles. Med Teach. 1999;21(6):563–570. doi: 10.1080/01421599978979. [DOI] [PubMed] [Google Scholar]
- 6.Bosse HM, Schultz JH, Nickel M, et al. The effect of using standardized patients or peer role play on ratings of undergraduate communication training: a randomized controlled trial. Patient Educ Couns. 2012;87(3):300–306. doi: 10.1016/j.pec.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 7.Wallman A, Vaudan C, Sporrong SK. Communications training in pharmacy education, 1995-2010. Am J Pharm Educ. 2013;77(2):Article 36. doi: 10.5688/ajpe77236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yedidia MJ, Gillespie CC, Kachur E, et al. Effect of communications training on medical student performance. JAMA. 2003;290(9):1157–1165. doi: 10.1001/jama.290.9.1157. [DOI] [PubMed] [Google Scholar]
- 9.Lane C, Rollnick S. The use of simulated patients and role-play in communication skills training: a review of the literature to August 2005. Patient Educ Couns. 2007;67(1-2):13–20. doi: 10.1016/j.pec.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 10.Boyle D, Dwinnell B, Platt F. Invite, listen, and summarize: a patient-centered communication technique. Acad Med. 2005;80(1):29–32. doi: 10.1097/00001888-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Barrows HS. An overview of the uses of standardized patients for teaching and evaluating clinical skills. AAMC. Acad Med. 1993;68(6):443–453. doi: 10.1097/00001888-199306000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Garrison DR, Kanuka H. Blended learning: uncovering its transformative potential in higher education. The Internet and Higher Education. 2004;7(2):95–105. [Google Scholar]
- 13.Gray K, Tobin J. Introducing an online community into a clinical education setting: a pilot study of student and staff engagement and outcomes using blended learning. BMC Med Educ. 2010;10:6. doi: 10.1186/1472-6920-10-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dankbaar ME, Storm DJ, Teeuwen IC, Schuit SC. A blended design in acute care training: similar learning results, less training costs compared with a traditional format. Perspect Med Educ. 2014;3(4):289–299. doi: 10.1007/s40037-014-0109-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ausburn LJ. Course design elements most valued by adult learners in blended online education environments: an American perspective. Educ. Media Int. 2004;41(4):327–337. [Google Scholar]
- 16.Carbonaro M, King S, Taylor E, Satzinger F, Snart F, Drummond J. Integration of e-learning technologies in an interprofessional health science course. Med Teach. 2008;30(1):25–33. doi: 10.1080/01421590701753450. [DOI] [PubMed] [Google Scholar]
- 17.Spedding R, Jenner R, Potier K, Mackway-Jones K, Carley S. Blended learning in paediatric emergency medicine: preliminary analysis of a virtual learning environment. Eur J Emerg Med. 2013;20(2):98–102. doi: 10.1097/MEJ.0b013e3283514cdf. [DOI] [PubMed] [Google Scholar]
- 18.Grasl MC, Pokieser P, Gleiss A, et al. A new blended learning concept for medical students in otolaryngology. Arch Otolaryngol Head Neck Surg. 2012;138(4):358–366. doi: 10.1001/archoto.2012.145. [DOI] [PubMed] [Google Scholar]
- 19.Crouch MA. An advanced cardiovascular pharmacotherapy course blending online and face-to-face instruction. Am J Pharm Educ. 2009;73(3):Article 51. doi: 10.5688/aj730351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kavadella A, Tsiklakis K, Vougiouklakis G, Lionarakis A. Evaluation of a blended learning course for teaching oral radiology to undergraduate dental students. Eur J Dent Educ. 2012;16(1):e88–e95. doi: 10.1111/j.1600-0579.2011.00680.x. [DOI] [PubMed] [Google Scholar]
- 21.Bains M, Reynolds PA, McDonald F, Sherriff M. Effectiveness and acceptability of face-to-face, blended and e-learning: a randomised trial of orthodontic undergraduates. Eur J Dent Educ. 2011;15(2):110–117. doi: 10.1111/j.1600-0579.2010.00651.x. [DOI] [PubMed] [Google Scholar]
- 22.Strickland S. The effectiveness of blended learning environments for the delivery of respiratory care education. J Allied Health. 2009;38(1):e11–e16. [PubMed] [Google Scholar]
- 23.Cho KC, Shin G. Operational effectiveness of blended e-learning program for nursing research ethics. Nurs Ethics. 2013;21(4):484–495. doi: 10.1177/0969733013505310. [DOI] [PubMed] [Google Scholar]
- 24.Rowe M, Frantz J, Bozalek V. The role of blended learning in the clinical education of healthcare students: a systematic review. Med Teach. 2012;34(4):e216–e221. doi: 10.3109/0142159X.2012.642831. [DOI] [PubMed] [Google Scholar]
- 25.de Leng BA, Dolmans DH, Muijtjens AM, van der Vleuten CP. Student perceptions of a virtual learning environment for a problem-based learning undergraduate medical curriculum. Med Educ. 2006;40(6):568–575. doi: 10.1111/j.1365-2929.2006.02484.x. [DOI] [PubMed] [Google Scholar]
- 26.Ruiz JG, Mintzer MJ, Leipzig RM. The impact of E-learning in medical education. Acad Med. 2006;81(3):207–212. doi: 10.1097/00001888-200603000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Salter SM, Karia A, Sanfilippo FM, Clifford RM. Effectiveness of E-learning in pharmacy education. Am J Pharm Educ. 2014;78(4):Article 83. doi: 10.5688/ajpe78483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hagemeier NE, Hess R, Hagen KS, Sorah EL. Impact of an interprofessional communication course on nursing, medical and pharmacy students’ communication skill self-efficacy beliefs. Am J Pharm Educ. 2014;78(10):Article 186. doi: 10.5688/ajpe7810186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lang F, McCord R, Harvill L, Anderson DS. Communication assessment using the common ground instrument: psychometric properties. Fam Med. 2004;36(3):189–198. [PubMed] [Google Scholar]
- 30.Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: Macmillan; 1997. [Google Scholar]
- 31.Bragard I, Etienne AM, Merckaert I, Libert Y, Razavi D. Efficacy of a communication and stress management training on medical residents’ self-efficacy, stress to communicate and burnout: a randomized controlled study. J Health Psychol. 2010;15(7):1075–1081. doi: 10.1177/1359105310361992. [DOI] [PubMed] [Google Scholar]
- 32.Woods JL, Pasold TL, Boateng BA, Hense DJ. Medical student self-efficacy, knowledge and communication in adolescent medicine. Int J Med Educ. 2014;5:165–172. doi: 10.5116/ijme.53d3.7b30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rogers ER, King SR. The influence of a patient-counseling course on the communication apprehension, outcome expectations, and self-efficacy of first-year pharmacy students. Am J Pharm Educ. 2012;76(8):Article 152. doi: 10.5688/ajpe768152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Accreditation Council for Pharmacy Education. Standards 2016. https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf. Accessed March 10, 2015.
- 35.Heiman HL, Uchida T, Adams C, et al. E-learning and deliberate practice for oral case presentation skills: a randomized trial. Med Teach. 2012;34(12):e820–e826. doi: 10.3109/0142159X.2012.714879. [DOI] [PubMed] [Google Scholar]