Abstract
Introduction
We aimed to quantify and identify associated factors of linkage to HIV care following home-based HIV counselling and testing (HBHCT) in the ongoing ANRS 12249 treatment-as-prevention (TasP) cluster-randomized trial in rural KwaZulu-Natal, South Africa.
Methods
Individuals ≥16 years were offered HBHCT; those who were identified HIV positive were referred to cluster-based TasP clinics and offered antiretroviral treatment (ART) immediately (five clusters) or according to national guidelines (five clusters). HIV care was also available in the local Department of Health (DoH) clinics. Linkage to HIV care was defined as TasP or DoH clinic attendance within three months of referral among adults not in HIV care at referral. Associated factors were identified using multivariable logistic regression adjusted for trial arm.
Results
Overall, 1323 HIV-positive adults (72.9% women) not in HIV care at referral were included, of whom 36.9% (n=488) linked to care <3 months of referral (similar by sex). In adjusted analyses (n=1222), individuals who had never been in HIV care before referral were significantly less likely to link to care than those who had previously been in care (<33% vs. >42%, p<0.001). Linkage to care was lower in students (adjusted odds-ratio [aOR]=0.47; 95% confidence interval [CI] 0.24–0.92) than in employed adults, in adults who completed secondary school (aOR=0.68; CI 0.49–0.96) or at least some secondary school (aOR=0.59; CI 0.41–0.84) versus ≤ primary school, in those who lived at 1 to 2 km (aOR=0.58; CI 0.44–0.78) or 2–5 km from the nearest TasP clinic (aOR=0.57; CI 0.41–0.77) versus <1 km, and in those who were referred to clinic after ≥2 contacts (aOR=0.75; CI 0.58–0.97) versus those referred at the first contact. Linkage to care was higher in adults who reported knowing an HIV-positive family member (aOR=1.45; CI 1.12–1.86) versus not, and in those who said that they would take ART as soon as possible if they were diagnosed HIV positive (aOR=2.16; CI 1.13–4.10) versus not.
Conclusions
Fewer than 40% of HIV-positive adults not in care at referral were linked to HIV care within three months of HBHCT in the TasP trial. Achieving universal test and treat coverage will require innovative interventions to support linkage to HIV care.
Keywords: HIV/AIDS, home-based HIV counselling and testing, linkage to care, universal test and treat, South Africa
Introduction
Initiating antiretroviral treatment (ART) as early as possible after acquiring HIV infection results in better health outcomes, reducing HIV-related morbidity or mortality [1,2]. Further, decreasing viral load with ART significantly reduces HIV transmission from the treated infected to the uninfected sexual partner in HIV-discordant couples [3–5]. Results from mathematical models suggest that universal and repeat HIV testing followed by immediate ART initiation could substantially decrease HIV incidence at population level [6]; this has been supported by subsequent results from an observational cohort study in rural KwaZulu-Natal, South Africa [7]. The World Health Organization (WHO) recently updated its HIV treatment and prevention guidelines, recommending universal test and treat with ART to be initiated in anyone living with HIV, regardless of clinical or immunological stage [8]. This was translated into the programmatic UNAIDS HIV “90–90–90” treatment targets, aiming for “90% of people living with HIV knowing their HIV status, 90% of those with diagnosed HIV infection receiving ART and 90% of those receiving ART having durable viral suppression” by 2020 [9].
South Africa carries one of the highest HIV burdens worldwide, with an estimated 6.3 million people living with HIV in 2013, and an HIV prevalence of 19.1% among 15- to 49-year-olds [10]. To achieve universal HIV testing in such a high HIV prevalence setting, community-based HIV testing services should be offered in addition to those offered in health facilities [11]. Among them, Home-Based HIV Counseling and Testing (HBHCT) has been shown to be acceptable and effective in increasing the number of people who know their HIV status, especially in South Africa [12–18], but there are limited data on linkage to care following HBHCT [19]. Further, while it is crucial that all HIV-identified individuals access HIV care and initiate ART as soon as possible, results from studies in sub-Saharan Africa have previously shown that many newly diagnosed HIV-positive people do not enter HIV care immediately following HIV diagnosis consequently delaying time to ART initiation [20,21].
The objectives of our analysis were to quantify the proportion of adults never or not currently in care who linked to HIV care within three months following an HIV diagnosis through HBHCT and to investigate factors associated with linkage to HIV care. The analysis was performed within the context of a cluster-randomized trial of treatment as prevention (TasP) conducted in rural and high HIV prevalence area in KwaZulu-Natal province, South Africa.
Methods
Study setting
We used data from the ANRS 12249 TasP trial, an ongoing cluster-randomized trial evaluating the effectiveness of immediate ART on HIV incidence. The trial is implemented since March 2012 in Hlabisa sub-district, northern KwaZulu-Natal, South Africa, a largely rural area, with scattered homesteads, an estimated HIV prevalence of 29% [22] and a decentralized local HIV programme [23].
Trial procedures
The TasP trial protocol has been described previously [24,25]. HBHCT is offered every six months to eligible members of the trial communities contacted during home visits. Household members are informed about the trial objectives and procedures, and about ART eligibility criteria according to their cluster of residence. All participants identified as HIV positive receive a TasP referral card and are encouraged to access the TasP trial clinic in their cluster, situated <45 minutes walking distance from where they live.
In TasP trial clinics of the intervention clusters, ART initiation is offered immediately to all HIV-positive adults regardless of their CD4 count or clinical staging. In control clusters, ART initiation is offered according to South African guidelines (March 2012–April 2013: CD4≤350 cells/µL or WHO stage IV; April 2013–January 2015: CD4≤350 cells/µL or WHO stage III/IV or pregnant women or tuberculosis co-infected). TasP trial participants can also access HIV and ART care in the Department of Health (DoH clinics).
The TasP trial started in 10 (2×5) clusters from March 2012 to July 2014, with a further 12 (2×6) clusters from July 2014, bringing the total number of clusters to 22 (2×11) at full implementation. Each cluster is composed of an average of about 1000 residents ≥16 years. Data from the first 10 clusters were used for this analysis.
Study population
We included all residents aged ≥16 years from both arms of the trial who were (i) contacted by a fieldworker, (ii) ascertained HIV positive (positive rapid HIV test result or self-reported to be HIV positive), (iii) referred to a TasP clinic between March 2012 and June 2014, and (iv) never been or not in HIV care at the time of referral (i.e. no CD4 count or viral load measurements in the DoH or TasP clinics in the 13 months before referral).
We excluded individuals with inconsistent dates (date of first clinic visit, death or out-migration before the date of first referral), as well as those with a period of observation shorter than three months. We focused statistical analyses on individuals without missing data for explanatory variables.
Outcome and explanatory variables
The outcome was linkage to HIV care following HIV diagnosis within three months of first referral in individuals who had never or not recently been in HIV care. Linkage to care was defined as attending a TasP clinic (the variable used was date of visit) or a DoH clinic (the variable used was date of last CD4 count or viral load measurement), after matching between the TasP trial database and the ARTemis database. We obtained ethics approval to match the TasP trial database with the DoH HIV care and treatment database (ARTemis), both developed and hosted at the Africa Centre [23]. Matching was based on South African ID number, first names, last names, dates of birth and cell phone numbers. The period of three months (i.e. 91 days) between first referral and linkage to care was chosen in accordance with Fox et al. [26].
Matching between TasP and ARTemis databases was also used to define the variable “HIV care status at referral” with four categories: (i) newly diagnosed (positive rapid HIV test through HBHCT, no self-report of HIV diagnosis and not in the ARTemis database before referral); (ii) already diagnosed but never accessed HIV care in the local HIV programme (self-reported HIV positive through HBHCT, not in the ARTemis database before referral); (iii) already accessed HIV care in the local HIV programme but considered lost-to-follow-up (LTFU) for 13 to 24 months (in ARTemis database before first referral but no CD4 count or viral load measurements in the DoH or TasP clinics in the 13–24 months before referral); or (iv) LTFU for more than 24 months.
Further explanatory socio-demographic and HIV-related variables were based on questionnaires administered face to face by trained interviewers during the repeat home-based visits; we considered information from the home visit before and closest to the date of first referral. We also included trial calendar round (CR) of HBHCT at referral (CR1: identification of HIV infection at the first home visit by HIV fieldworkers; CR2/CR3: identification of HIV infection at the second or the third home visit [individuals identified HIV positive in CR2/CR3 could be those not tested for HIV during the first round (CR1) because they were not at home, they refused to be tested, they seroconverted between rounds or they had just become eligible because they turned 16 years old]).
Statistical analysis
Linkage to HIV care following HIV diagnosis was described with Kaplan–Meier curves stratified by sex. The association between sex and linkage to HIV care was estimated using a log-rank test. Univariable and multivariable logistic regression models were conducted to explore factors associated with linkage to HIV care within three months of referral. For ordinal variables, a test for trend was also conducted. Multivariable analysis was adjusted for sex and trial arm, and included variables associated with linkage to HIV care with a p-value <0.20 in univariable analysis. The interactions with sex and HIV care status at referral were tested, but no interactions were found (Supplementary Table 1). Analyses were carried out using STATA version 13.0 (StataCorp, College Station, Texas).
Ethical approval
The trial was approved by the Biomedical Research Ethics Committee (BREC) of the University of KwaZulu-Natal (BFC 104/11) and the Medicines Control Council of South Africa.
Our consent procedures include at home level, for each survey round, verbal consent of the homestead's owner and of the head of household, as well as written individual consent. For participants aged 16 or 17, we collect both the consent of the participant and the consent of a parent or a guardian.
Results
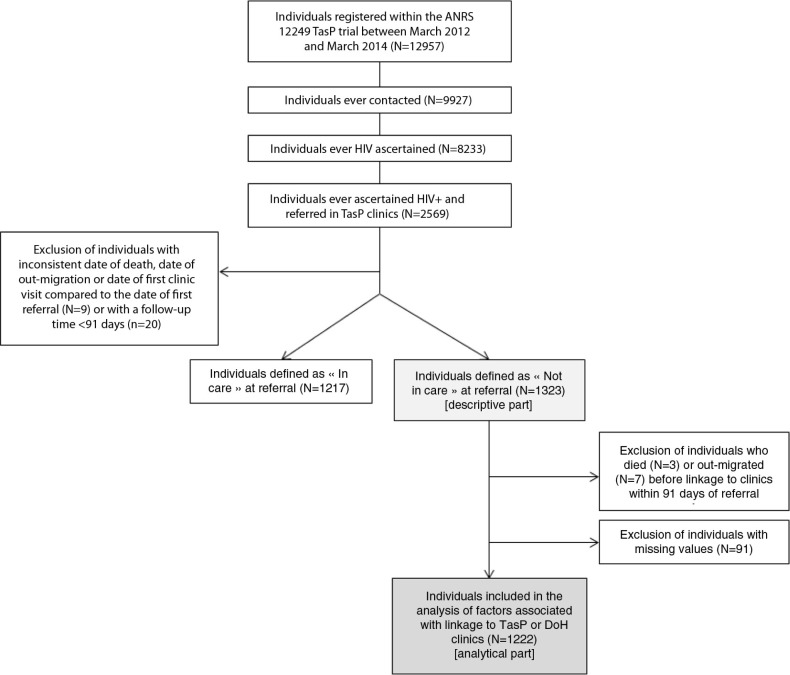
Of the 12,957 adults registered in the TasP trial, 9927 were ever contacted, of whom 8233 had their HIV status ascertained. Of these, 2569 (31.2%) were identified HIV positive and referred to a TasP clinic (Figure 1); and among them, 29 adults were excluded because they had inconsistent dates (n=9) or their period of observation was <3 months (n=20). Of the remaining 2540 adults, 1323 were considered “never or not currently in care,” of whom 72.9% (n=965) were women.
Figure 1.
Flowchart of the cohort, ANRS TasP trial, rural South Africa, 2012–2014.
At the time of referral, about 43% of included adults were newly diagnosed and 26% had previously been diagnosed but had never accessed care (Table 1); about 31% of adults had already accessed HIV care in the local HIV programme but were considered LTFU, half of them for >24 months. About 60% of HIV-positive adults were identified as HIV positive in the first round of fieldwork (Table 1, trial characteristics).
Table 1.
Description of the study population at referral, ANRS TasP trial, rural South Africa, 2012–2014 (N=1323)
| Total (N=1323) |
Women (N=965) |
Men (N=358) |
||||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| HIV care status at referral | ||||||
| Never in care, newly diagnosed | 567 | (42.9) | 381 | (39.5) | 186 | (52.0) |
| Never in care, already diagnosed | 346 | (26.1) | 247 | (27.6) | 79 | (22.1) |
| LTFU >24 months | 202 | (15.3) | 161 | (16.7) | 41 | (11.4) |
| LTFU 13–24 months | 208 | (15.7) | 156 | (16.2) | 52 | (14.5) |
| Socio-demographic characteristics | ||||||
| Age at referral (years) | ||||||
| 16–19 | 78 | (5.9) | 69 | (7.1) | 9 | (2.5) |
| 20–29 | 464 | (35.1) | 356 | (36.9) | 108 | (30.2) |
| 30–39 | 355 | (26.8) | 242 | (25.1) | 113 | (31.6) |
| 40–49 | 189 | (14.3) | 127 | (13.2) | 62 | (17.3) |
| 50–84 | 193 | (14.6) | 139 | (14.4) | 54 | (15.1) |
| Missing | 44 | (3.3) | 32 | (3.3) | 12 | (3.3) |
| Education level | ||||||
| Primary or less | 491 | (37.1) | 342 | (35.4) | 149 | (41.6) |
| Some secondary | 440 | (33.3) | 320 | (33.2) | 120 | (33.5) |
| At least completed secondary | 383 | (28.9) | 297 | (30.8) | 86 | (24.0) |
| Missing | 9 | (0.7) | 6 | (0.6) | 3 | (0.9) |
| Occupational status | ||||||
| Employed | 210 | (15.9) | 120 | (12.4) | 90 | (25.1) |
| Student | 109 | (8.2) | 89 | (9.2) | 20 | (5.6) |
| Not student, not employed | 985 | (74.5) | 741 | (76.8) | 244 | (68.2) |
| Missing | 19 | (1.4) | 15 | (1.6) | 4 | (1.1) |
| Household wealth assetsa | ||||||
| Low | 471 | (35.6) | 350 | (36.3) | 121 | (33.8) |
| Middle | 554 | (41.9) | 408 | (42.3) | 146 | (40.8) |
| High | 287 | (21.7) | 198 | (20.5) | 89 | (24.9) |
| Missing | 11 | (0.8) | 9 | (0.9) | 2 | (0.5) |
| Characteristics relating to HIV knowledge and perception | ||||||
| Knowing HIV-positive family member | ||||||
| No | 821 | (62.5) | 565 | (59.2) | 256 | (71.5) |
| Yes | 491 | (37.1) | 391 | (40.5) | 100 | (27.9) |
| Missing | 5 | (0.4) | 3 | (0.3) | 2 | (0.6) |
| Would take ARV if diagnosed HIV positive | ||||||
| Agree | 1216 | (91.9) | 876 | (90.8) | 340 | (95.0) |
| Disagree | 63 | (4.8) | 56 | (5.8) | 7 | (2.0) |
| Don't know | 25 | (1.9) | 18 | (1.9) | 7 | (2.0) |
| Missing | 19 | (1.4) | 15 | (1.5) | 4 | (1.0) |
| Think that people avoid HIV-positive individuals | ||||||
| Agree | 470 | (35.5) | 356 | (36.9) | 114 | (31.8) |
| Disagree | 697 | (52.7) | 496 | (51.4) | 201 | (56.2) |
| Don't know | 137 | (10.4) | 100 | (10.4) | 37 | (10.3) |
| Missing | 19 | (1.4) | 13 | (1.3) | 6 | (1.7) |
| Think that people don't blame HIV-positive individuals | ||||||
| Agree | 707 | (53.4) | 515 | (53.4) | 192 | (53.6) |
| Disagree | 448 | (33.9) | 330 | (34.2) | 118 | (33.0) |
| Don't know | 153 | (11.6) | 110 | (11.4) | 43 | (12.0) |
| Missing | 15 | (1.1) | 10 | (1.0) | 5 | (1.4) |
| Trial characteristics | ||||||
| Distance from home to the closest TasP clinic | ||||||
| <1 km | 486 | (36.7) | 355 | (36.8) | 131 | (36.6) |
| 1–2 km | 468 | (35.4) | 343 | (35.5) | 125 | (34.9) |
| 2–5 km | 369 | (27.9) | 267 | (27.7) | 102 | (28.5) |
| Calendar round at referral | ||||||
| CR1 | 793 | (59.9) | 590 | (61.1) | 203 | (56.7) |
| CR2/CR3 | 530 | (40.1) | 375 | (38.9) | 155 | (43.3) |
| Trial arm | ||||||
| Control | 717 | (54.2) | 535 | (55.4) | 182 | (50.8) |
| Intervention | 606 | (45.8) | 430 | (44.6) | 176 | (49.2) |
LTFU, lost-to-follow-up; ARV, antiretroviral; CR, calendar round at referral.
Household wealth assets had been defined in three categories (low, middle and high) in agreement with a principal component analysis considering sources of energy, amenities and access to drinking water and toilet facilities in this populations [27].
The included population was relatively young (44% of women and 32% of men were <30 years) and with a low education level (35% of women and 41% of men did not go to secondary school). A large proportion of the population was neither employed nor studying (>76% of women and >68% of men). Almost 41% of women and 28% of men declared that they knew at least one other family member who was HIV positive. About one-third of the included population perceived stigma against HIV-positive individuals (>35% agreed that people of the community avoid HIV-positive individuals and almost 34% disagreed that people of the community don't blame HIV-positive individuals). More than 90% of men and women reported they would take ARVs “as soon as possible” if diagnosed HIV positive (Table 1).
Linkage to care proportion
Overall, 36.9% of included adults never or not currently in HIV care at the time of referral were linked to care (in either TasP or DoH clinic) within three months of HBHCT (Table 2).
Table 2.
Linkage to HIV care within three months of referral, ANRS TasP trial, rural South Africa, 2012–2014 (N=1323)
| Total (N=1323) |
Women (N=965) |
Men (N=358) |
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Linkage to clinics | 488 | 36.9 | 349 | 36.2 | 139 | 38.8 |
| Linkage to TasP clinic only | 381 | 28.8 | 267 | 27.7 | 114 | 31.8 |
| Linkage to DoH then to TasP clinics | 39 | 3.0 | 28 | 2.9 | 11 | 3.1 |
| Linkage to TasP then to DoH clinics | 7 | 0.5 | 4 | 0.4 | 3 | 0.8 |
| Linkage to DoH clinic only | 61 | 4.6 | 50 | 5.2 | 11 | 3.1 |
| Death | 3 | 0.2 | 3 | 0.3 | 0 | 0.0 |
| Out-migration | 7 | 0.5 | 7 | 0.7 | 0 | 0.0 |
| No linkage to clinics | 825 | 62.4 | 606 | 62.8 | 219 | 61.2 |
DoH, Department of Health; TasP, treatment as prevention.
Linkage to HIV care occurred mostly during the first month after referral then increased slowly over time, with no significant differences by sex (Figure 2).
Figure 2.
Cumulative incidence of linkage to TasP or DoH clinics within three months of referral, stratified by sex, ANRS TasP trial, rural South Africa, 2012–2014 (N=1323). DoH: Department of Health; TasP: treatment as prevention.
Factors associated with linkage to HIV care within three months of referral
For this analysis, we excluded individuals who died (n=3) or had out-migrated (n=7) within three months of referral, as well as those with missing values (n=91). In total, 1222 individuals were thus included (Figure 1); included individuals were more likely to have had previous contact with the local HIV programme than those excluded before HIV identification within the TasP trial (20.8% vs. 31.9%, p=0.002, Supplementary Table 2).
HIV care status at referral was significantly associated with linkage to HIV care (Table 3): 32.1% of individuals newly diagnosed were linked to HIV care within three months of referral, compared with 42.8% among those who had already accessed HIV care previously but were LTFU for >24 months at the time of referral linked to HIV care (adjusted odd ratio [aOR]=1.44, 95% confidence interval [CI] =1.00–2.06), and 56.9% among those LTFU for more than 13 to 24 months (aOR=0.2.52, CI=1.77–3.61). No significant difference in linkage to care percentages was observed between individuals who were newly diagnosed and those already diagnosed but having never been in care.
Table 3.
Factors associated with linkage to TasP or DoH clinics within three months of referral, ANRS TasP trial, rural South Africa, 2012–2014 (N=1222 – complete data)
| Univariable analysis | Multivariable analysisa | |||||||
|---|---|---|---|---|---|---|---|---|
| n | % linkage | OR | 95%CI | p* | aOR | 95%CI | p* | |
| HIV care status at referral | ||||||||
| Never in care, newly diagnosed | 529 | 32.1 | 1.00 | – | <0.001 | 1.00 | – | <0.001 |
| Never in care, already diagnosed | 304 | 31.6 | 0.97 | 0.72–1.32 | 0.97 | 0.71–1.34 | ||
| LTFU >24 months | 194 | 42.8 | 1.58 | 1.13–2.21 | 1.44 | 1.00–2.06 | ||
| LTFU 13–24 months | 195 | 56.9 | 2.79 | 1.99–3.90 | 2.52 | 1.77–3.61 | ||
| Socio-demographic characteristics | ||||||||
| Sex | ||||||||
| Men | 336 | 39.6 | 1.00 | – | 0.39 | 1.00 | – | 0.47 |
| Women | 886 | 36.9 | 0.89 | 0.69–1.16 | 0.90 | 0.68–1.20 | ||
| Age at referral (years) | ||||||||
| 16–19 | 75 | 20.0 | 0.54 | 0.30–0.99 | <0.001 | 0.77 | 0.40–1.48 | 0.40 |
| 20–29 | 437 | 31.6 | 1.00 | – | 1.00 | – | ||
| 30–39 | 340 | 38.2 | 1.34 | 1.00–1.81 | 1.09 | 0.79–1.50 | ||
| 40–49 | 185 | 44.3 | 1.72 | 1.21–2.46 | 1.16 | 0.77–1.74 | ||
| 50–84 | 185 | 51.4 | 2.29 | 1.61–3.25 | 1.47 | 0.94–2.28 | ||
| Education level | ||||||||
| Primary or less | 455 | 47.7 | 1.00 | – | <0.001 | 1.00 | – | 0.01 |
| Some secondary | 407 | 33.7 | 0.56 | 0.42–0.73 | 0.68 | 0.49–0.96 | ||
| At least completed secondary | 360 | 29.4 | 0.46 | 0.34–0.61 | 0.59 | 0.41–0.84 | ||
| Occupational status | ||||||||
| Employed | 200 | 42.5 | 1.00 | – | <0.001 | 1.00 | – | 0.07 |
| Student | 102 | 16.7 | 0.27 | 0.15–0.49 | 0.47 | 0.24–0.92 | ||
| Not student, not employed | 920 | 38.9 | 0.86 | 0.63–1.18 | 0.94 | 0.67–1.31 | ||
| Household wealth assets | ||||||||
| Low | 439 | 37.1 | 1.00 | – | 0.62 | |||
| Middle | 514 | 39.1 | 1.09 | 0.84–1.41 | ||||
| High | 269 | 35.7 | 0.94 | 0.69–1.29 | ||||
| Characteristics relating to HIV knowledge and perception | ||||||||
| Knowing HIV-positive family member | ||||||||
| No | 764 | 35.0 | 1.00 | – | 0.01 | 1.00 | – | 0.004 |
| Yes | 458 | 42.1 | 1.36 | 1.07–1.72 | 1.45 | 1.12–1.86 | ||
| Would take ARV is diagnosed HIV positive | ||||||||
| Agree | 1141 | 38.5 | 1.83 | 1.01–3.34 | 0.06 | 2.16 | 1.13–4.10 | 0.03 |
| Disagree | 59 | 25.4 | 1.00 | – | 1.00 | – | ||
| Don't know | 22 | 27.3 | 1.10 | 0.36–3.33 | 1.18 | 0.37–3.76 | ||
| Think that people avoid HIV-positive individuals | ||||||||
| Agree | 446 | 36.8 | 0.91 | 0.71–1.16 | 0.39 | |||
| Disagree | 652 | 39.1 | 1.00 | – | ||||
| Don't know | 124 | 33.1 | 0.77 | 0.51–1.15 | ||||
| Think that people don't blame HIV-positive individuals | ||||||||
| Agree | 661 | 38.1 | 1.03 | 0.80–1.32 | 0.87 | |||
| Disagree | 424 | 37.5 | 1.00 | – | ||||
| Don't know | 137 | 35.8 | 0.93 | 0.62–1.39 | ||||
| Trial characteristics | ||||||||
| Distance to the closest TasP clinic | ||||||||
| 0–1 km | 447 | 45.0 | 1.00 | – | <0.001 | 1.00 | – | <0.001 |
| 1–2 km | 433 | 33.7 | 0.62 | 0.47–0.82 | 0.58 | 0.44–0.78 | ||
| 2–5 km | 342 | 33.0 | 0.60 | 0.45–0.81 | 0.57 | 0.41–0.77 | ||
| Calendar round at referral | ||||||||
| CR1 | 734 | 41.3 | 1.00 | – | 0.001 | 1.00 | – | 0.03 |
| CR2/CR3 | 488 | 32.2 | 0.67 | 0.53–0.86 | 0.75 | 0.58–0.97 | ||
OR, odd ratio; 95%CI, 95% confidence interval; aOR, adjusted odd ratio; LTFU, lost-to-follow-up; ARV, antiretroviral; CR, calendar round at referral; DoH, Department of Health; TasP, treatment as prevention.
p, likelihood ratio test p-values.
Variables included in the multivariable model: HIV care status, sex, age, education level, occupational status, knowing HIV-positive family member, ARV if diagnosed HIV positive, distance to clinic, trial calendar round.
Linkage to care significantly decreased with education level (p for trend<0.001) and was associated with occupational status: 16.7% of students linked to HIV care compared to 42.5% of employed (aOR=0.47, CI=0.24–0.92). However, linkage to care did not differ significantly between employed individuals and those who were neither student nor employed.
Further, percentages of linkage to care were higher in individuals who declared knowing at least another HIV-positive family member (42.1% vs. 35.0% among those who did not know another HIV-positive family member, aOR=1.45, CI=1.12–1.86), as well as in those who stated they would agree taking ARVs “as soon as possible” if diagnosed HIV positive (38.5% vs. 25.4% among those who didn't agree, aOR=2.16, CI=1.13–4.10).
Living closer to a TasP clinic was significantly associated with increased linkage to care (p for trend <0.001). Finally, adults who were ascertained HIV positive and referred to a TasP clinic in the second or the third round of trial fieldwork were less likely to be linked to HIV care (32.2% vs. 41.3%, aOR=0.75, CI=0.58–0.97) (Table 3).
The percentages of linkage to care also increased significantly with age (p trend <0.001), but this association lost significance in the multivariable model. Household wealth and stigma-related variables were not significantly associated with linkage to care.
Discussion
In this rural area, fewer than 40% of individuals identified HIV positive through HBHCT in the TasP trial, and who had never or were not currently in HIV care, accessed an HIV clinic within three months of referral. These results are in line with a previous study in Kenya (42% linkage to care following HBHCT) [28] but lower than seen in other studies in rural South Africa (62%) [19], Uganda and South Africa (86%) [29]. However, it is difficult to compare these studies as definitions of linkage to care varied (especially regarding the time between HIV diagnosis and linkage to care used in these studies) [19]. We also observed that linkage to care, if it happened, was most likely in the first month after referral; we hypothesize that this pattern, also seen elsewhere [19], is suggestive of an element of being ready to engage with HIV care and treatment, and where this fits in terms of personal priorities.
Linkage to HIV care did not significantly differ according to sex, a finding consistent with the Kenya study [28]. We identified several other factors associated with linkage to HIV care. The first was HIV care status at referral, which allows for previous HIV diagnosis and care. Adults who had never been in HIV care when identified as HIV positive during the TasP trial were significantly less likely to link to HIV care than those who had previously been in HIV care but had been LTFU. This may suggest that the latter may have already come to terms with their HIV diagnosis and may possibly already have disclosed their HIV status to relatives and friends; it has indeed previously been reported that HIV disclosure is associated with access to HIV care following HBHCT in Kenya [28]. Further, individuals who were previously in care may have a better understanding of what is involved in HIV care than those who never accessed HIV care and may thus be more inclined to re-engage with HIV care when provided with a convenient alternative which is closer to them as in the TasP trial. Among people who had never been in care, there were no differences in linkage to care whether people were newly diagnosed in the trial or not, which was also found in Kenya [28]; these findings suggest that, beyond the need for time required to process an HIV-positive status following diagnosis [30,31], there are additional challenges for linkage to care which should be explored further.
While stigma variables, as collected within the trial, were not significantly associated with linkage to HIV care, people who knew another family member to be HIV positive were more likely to access HIV care than those who did not. This could suggest that people with HIV history in the family may have a better knowledge of HIV care and treatment and may thus be more disposed to access HIV care themselves when they are referred. They may also be more confident in disclosing their HIV status, and trust they will receive family support. This is especially important in a context where HIV care is offered in dedicated services or clinics, separated from general care, where patients are easily identified as HIV positive, as it is the case in this TasP trial as well as in the local HIV programme.
Linkage to care was also especially low in students (16.7%); these individuals may be less economically and logistically independent and may not consider HIV care a priority.
We also showed that people who were identified HIV positive at the first home-based contact were significantly more likely to link to HIV care than those identified HIV positive only at second or third contact. People referred to care for the first time only after several contacts may either be recent HIV seroconverters, needing time to accept their HIV status, or who refused HIV testing initially, and who, we hypothesize, may be less inclined to access care once diagnosed than those readily accepting an HIV test at the first contact.
Linkage to HIV care was lower in people with higher education levels. A possible suggestion for this may include being able to afford HIV care outside of the trial if closer to their place of employment (private sector, clinics outside of the areas). Higher education level may also be associated with being at work or engaged in other productive activity, which could have hindered clinic attendance.
Linkage to HIV care also decreased significantly with distance to clinic. Although everyone lived within a 45-minute walking distance to the trial clinic in their cluster, those who were even closer to the clinic, and required less travel time to access it, were more likely to link to care than those who lived further away. We hypothesize that the role of distance to clinic in linkage to care would be even more important in settings where HIV clinics are not as accessible as in the TasP trial area. Economic and logistic barriers associated with distance to clinic would need further investigation.
Finally, while it has not been considered in this study, an association between perception of health status and linkage to HIV care following HBHCT has been observed in other settings in Kenya [28] and South Africa [19]. For a long time in these countries, the public health message has been to wait for the CD4 count to drop below a certain threshold before being able to initiate ART. With the 2015 WHO recommendation of ART initiation to all HIV-positive individuals regardless of clinical or immunological status, public health messaging will need to change with specific education and counselling at community and individual levels.
Given the number of individual-level factors associated with a link to HIV care in our study, strategies of patient-centred HIV care with specific social support should be considered [32]. The engagement of health system navigators who can call, visit people at home or in neutral places and, if needed, escort them to clinic could also be proposed [33,34] although this was not found to be successful in urban South Africa [35,36]. For people who face difficulties in accessing a clinic, home-based ART initiation with home-based care could be implemented [37] although it remains important to evaluate the impact of such an intervention on long-term follow-up.
Our study has some methodological limitations. First, it was nested in a large randomized trial with specific trial clinics providing higher coverage of HIV care than would ordinarily be available within a standard HIV programme. Another limitation is that we do not know whether people linked to care outside of both the TasP trial and the local HIV programme, which could have led to an underestimation of the proportion of linkage to HIV care. However, such an underestimation is unlikely to be substantial as our definition of linkage to care considers a short time period (three months) following referral during which people from this relatively poor area would have found difficult to access HIV care outside the area. Finally, we excluded about 10% of the sample (who had missing data) in the analysis of factors associated with linkage to HIV care; included individuals may not be representative of the overall population as they were more likely to have previously sought HIV care in the local HIV programme before TasP trial implementation, than excluded people. However, we did not observe other statistically significant differences between included and excluded participants, and the population size was sufficient to statistically test factors associated with linkage to HIV care in the trial.
Conclusions
A major strength is that the study has been conducted prospectively within a large population. The results are particularly relevant in the context of rapidly evolving HIV care. Indeed, in the light of the recent findings from the TEMPRANO and START trials [1,2] demonstrating the strong clinical benefits of early ART at an individual level, international HIV guidelines have been expanded towards a universal test and treat strategy [8]. The critical remaining questions relate to how best to ensure operational implementation of such a strategy at a population level in order to achieve the UNAIDS 90–90–90 target [9]. Our results show that an HBHCT intervention is useful not only to diagnose HIV-positive individuals who do not know their HIV status, but also to re-engage people previously in care but LTFU. We also highlighted the challenges inherent in achieving the second “90%” of the UNAIDS target: the number of people linked to HIV care and initiating ART must be substantially increased with combined interventions at the patient-level. Such strategies will need to be fully evaluated in different settings, including ours, at population level.
Supplementary Material
Acknowledgements
We thank all the participants of the ANRS 12249 TasP trial as well as all the fieldworkers and the data centre team of the Africa Centre.
Appendix
Composition of the TasP Study Group
| Name | Role | Affiliation |
|---|---|---|
| Investigators | ||
| François Dabis | Co-PI (France) | Univ. Bordeaux, ISPED, Centre Inserm U897 – Epidemiologie-Biostatistique, Bordeaux, France |
| INSERM, ISPED, Centre Inserm U897 – Epidemiologie-Biostatistique, Bordeaux, France | ||
| Marie-Louise Newell | Co-PI (United Kingdom) | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa Faculty of Medicine, University of Southampton, UK |
| Deenan Pillay | Co-PI (South Africa) | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa Faculty of Medical Sciences, University College London, UK |
| Coordinators | ||
| Collins Iwuji | Trial Coordinator and HIV Physician (South Africa) | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa Research Department of Infection and Population Health, University College London, UK |
| Joanna Orne-Gliemann | Trial Coordinator (France) | Univ. Bordeaux, ISPED, Centre Inserm U897 – Epidemiologie-Biostatistique, Bordeaux, France INSERM, ISPED, Centre Inserm U897 – Epidemiologie-Biostatistique, Bordeaux, France |
| Study team | ||
| Till Bärnighausen | Health economics | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa |
| Dept of Global Health & Population, Harvard School of Public Health, Harvard Univ. Boston | ||
| Eric Balestre | Epidemiology and Biostatistics | Univ. Bordeaux, ISPED, Centre Inserm U897 – Epidemiologie-Biostatistique, Bordeaux, France INSERM, ISPED, Centre Inserm U897 – Epidemiologie-Biostatistique, Bordeaux, France |
| Sylvie Boyer | Health economics | INSERM, UMR912 (SESSTIM), Marseille, France |
| Aix Marseille Université, UMR_S912, IRD, Marseille, France | ||
| ORS PACA, Observatoire Régional de la Santé Provence-Alpes-Côte d'Azur, Marseille, France | ||
| Alexandra Calmy | Adult Medicine | Service des maladies infectieuses, Hôpital Universitaire de Geneve, Genève. |
| Vincent Calvez | Virology | Department of virology, Hôpital Pitié-Salpétrière, Paris, France |
| Marie-Laure Chaix | Virology | EA 3620, Université Paris-Descartes, Laboratoire de Virologie, Hôpital Necker-Enfants Malades, AP-HP, Paris |
| Rosemary Dray-Spira | Social sciences | INSERM U1018, CESP, Epidemiology of Occupational and Social Determinants of Health, Villejuif, France |
| University of Versailles Saint-Quentin, UMRS 1018, Villejuif, France | ||
| Kamal ElFarouki | Social sciences | INSERM U1018, CESP, Epidemiology of Occupational and Social Determinants of Health, Villejuif, France |
| University of Versailles Saint-Quentin, UMRS 1018, Villejuif, France | ||
| Kenneth Freedberg | Modelling | Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA. |
| Kobus Herbst | Data management | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa |
| John Imrie | Social sciences | Futures Group, Johannesburg, South Africa |
| Centre for Sexual Health and HIV Research, Research Department of Infection and Population, Faculty of Population Health Sciences, University College London, London, UK | ||
| Sophie Karcher | Data management | Univ. Bordeaux, ISPED, Centre Inserm U897 – Epidemiologie-Biostatistique, Bordeaux, France |
| INSERM, ISPED, Centre Inserm U897 – Epidemiologie-Biostatistique, Bordeaux, France | ||
| Joseph Larmarange | Social sciences | CEPED (Centre Population & Développement-UMR 196-Paris Descartes/INED/IRD), IRD (Institut de Recherche pour le Développement), Paris, France. |
| Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa | ||
| France Lert | Social Sciences | INSERM U1018, CESP, Epidemiology of Occupational and Social Determinants of Health, Villejuif, France |
| University of Versailles Saint-Quentin, UMRS 1018, Villejuif, France | ||
| Richard Lessells | Adult medicine | London School of Hygiene and Tropical Medicine, UK |
| Thembisa Makowa | Field operations | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa |
| Anne-Geneviève Marcelin | Virology | Department of virology, Hôpital Pitié-Salpétrière, Paris, France |
| Laura March | Health economics | INSERM, UMR912 (SESSTIM), Marseille, France |
| Aix Marseille Université, UMR_S912, IRD, Marseille, France | ||
| ORS PACA, Observatoire Régional de la Santé Provence-Alpes-Côte d'Azur, Marseille, France | ||
| Nuala McGrath | Epidemiology/Social sciences | Academic Unit of Primary Care and Population Sciences, and Department of Social statistics and Demography, University of Southampton, United Kingdom |
| Kevi Naidu | Adult medicine | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa |
| Colin Newell | Data management | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa |
| Nonhlanhla Okesola | Nurse manager | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa |
| Tulio de Oliveira | Bioinformatics | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa |
| Melanie Plazy | Epidemiology/social sciences | Univ. Bordeaux, ISPED, Centre Inserm U897- Epidemiologie-Biostatistique, Bordeaux, France |
| INSERM, ISPED, Centre Inserm U897- Epidemiologie-Biostatistique, Bordeaux, France | ||
| Tamsen Rochat | Anthropology/psychology | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa |
| Bruno Spire | Health economics | INSERM, UMR912 (SESSTIM), 13006, Marseille, France |
| Aix Marseille Université, UMR_S912, IRD, Marseille, France | ||
| ORS PACA, Observatoire Régional de la Santé Provence-Alpes-Côte d'Azur, Marseille, France | ||
| Frank Tanser | Epidemiology and Biostatistics | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa |
| Rodolphe Thiébaut | Epidemiology and Biostatistics | Univ. Bordeaux, ISPED, Centre Inserm U897 – Epidemiologie-Biostatistique, Bordeaux, France INSERM, ISPED, Centre Inserm U897 – Epidemiologie-Biostatistique, Bordeaux, France |
| Johannes Viljoen | Virology | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa |
| Thembelile Zuma | Psychology/Social sciences | Africa Centre for Health and Population Studies, University of KwaZulu-Natal, South Africa |
Scientific advisory board
Chair: Bernard Hirschel (Switzerland)
International experts: Xavier Anglaret (Ivory Coast), Hoosen Cooavdia (South Africa), Alpha Diallo (France), Bruno Giraudeau (France), Jean-Michel Molina (France), Lynn Morris (South Africa), François Venter (South Africa), Sibongile Zungu (South Africa)
Community representatives: Eric Fleutelot (France), Eric Goemaere (South Africa), Calice Talom (Cameroon)
Sponsor representatives (ANRS): Brigitte Bazin, Claire Rekacewicz
Pharmaceutical company representatives: Golriz Pahlavan-Grumel (MSD), Alice Jacob (Gilead)
Data safety and monitoring board
Chair: Patrick Yeni (France)
Members: Sinead Delany-Moretlwe (South Africa), Nathan Ford (South Africa), Catherine Hankins (Netherlands), Helen Weiss (UK)
Competing interests
CI has received honoraria for services rendered to Gilead Sciences. All other authors declare no competing interest.
Authors' contributions
MP, KEF, CI and RDS developed the concept and discussed the analysis plan. MP and KEF conducted the statistical analysis. MP drafted the manuscript. All authors contributed to interpretation of the analysis results and commented on drafts of the manuscript. All authors have read and approved the final manuscript.
Funding
The French National Agency for AIDS and Viral Hepatitis Research (ANRS) is the sponsor and co-funder of the trial. Research discussed in this publication has been co-funded by the International Initiative for Impact Evaluation, Inc. (3ie) with support from the Bill & Melinda Gates Foundation. The content is solely the responsibility of the authors and does not necessarily represent the official views of 3ie or the Bill & Melinda Gates Foundation. The Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ) co-funded the trial.
The trial is conducted with the support of Merck & Co. Inc. and Gilead Sciences that provided the Atripla® drug supply. The Africa Centre for Population Health receives core funding from the Wellcome Trust, which provides the platform for the population- and clinic-based research at the Centre.
Mélanie Plazy was supported by the French National Agency for AIDS Research (ANRS) and is now supported by the French Charity Sidaction.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Danel C, Moh R, Gabillard D, Badje A, Le Carrou J, Ouassa T, et al. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med. 2015;373(9):808–22. doi: 10.1056/NEJMoa1507198. [DOI] [PubMed] [Google Scholar]
- 2.Lundgren JD, Babiker AG, Gordin F, Emery S, Grund B, Sharma S, et al. Initiation of antiretroviral therapy in early asymptomatic HIV Infection. N Engl J Med. 2015;373(9):795–807. doi: 10.1056/NEJMoa1506816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Attia S, Egger M, Muller M, Zwahlen M, Low N. Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS. 2009;23(11):1397–404. doi: 10.1097/QAD.0b013e32832b7dca. [DOI] [PubMed] [Google Scholar]
- 4.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donnell D, Baeten JM, Kiarie J, Thomas KK, Stevens W, Cohen CR, et al. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet. 2010;375(9731):2092–8. doi: 10.1016/S0140-6736(10)60705-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373(9657):48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 7.Tanser F, Barnighausen T, Grapsa E, Zaidi J, Newell ML. High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science. 2013;339(6122):966–71. doi: 10.1126/science.1228160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. 2015 [cited 2015 Oct 19] Available from: http://apps.who.int/iris/bitstream/10665/186275/1/9789241509565_eng.pdf?ua=1. [PubMed]
- 9.UNAIDS. 90-90-90. An ambitious treatment target to help end the AIDS epidemic. 2014 [cited 2015 Sept 9] Available from: http://www.unaids.org/sites/default/files/media_asset/90-90-90_en_0.pdf.
- 10.UNAIDS. The gap report. 2014 [cited 2015 Sept 9] Available from: http://www.unaids.org/sites/default/files/media_asset/UNAIDS_Gap_report_en.pdf.
- 11.WHO. Consolidated guidelines on HIV testing services. 2015 [cited 2015 Sept 9] Available from: http://apps.who.int/iris/bitstream/10665/179870/1/9789241508926_eng.pdf?ua=1.
- 12.Tabana H, Nkonki L, Hongoro C, Doherty T, Ekstrom AM, Naik R, et al. A cost-effectiveness analysis of a home-based HIV counselling and testing intervention versus the standard (Facility Based) HIV testing strategy in rural South Africa. PLoS One. 2015;10(8):e0135048. doi: 10.1371/journal.pone.0135048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muloongo K, Tshuma N, Chimoyi L, Setswe G, Sarfo B, Nyasulu P. Factors contributing to home-based acceptability of rapid testing for HIV infection among the inner city commuter population in Johannesburg, South Africa. Trans R Soc Trop Med Hyg. 2014;108(10):632–8. doi: 10.1093/trstmh/tru122. [DOI] [PubMed] [Google Scholar]
- 14.van Rooyen H, Barnabas RV, Baeten JM, Phakathi Z, Joseph P, Krows M, et al. High HIV testing uptake and linkage to care in a novel program of home-based HIV counseling and testing with facilitated referral in KwaZulu-Natal, South Africa. J Acquir Immune Defic Syndr. 2013;64(1):1–8. doi: 10.1097/QAI.0b013e31829b567d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doherty T, Tabana H, Jackson D, Naik R, Zembe W, Lombard C, et al. Effect of home based HIV counselling and testing intervention in rural South Africa: cluster randomised trial. BMJ. 2013;346:f3481. doi: 10.1136/bmj.f3481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Naik R, Tabana H, Doherty T, Zembe W, Jackson D. Client characteristics and acceptability of a home-based HIV counselling and testing intervention in rural South Africa. BMC Public Health. 2012;12:824. doi: 10.1186/1471-2458-12-824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maheswaran H, Thulare H, Stanistreet D, Tanser F, Newell ML. Starting a home and mobile HIV testing service in a rural area of South Africa. J Acquir Immune Defic Syndr. 2012;59(3):43–6. doi: 10.1097/QAI.0b013e3182414ed7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larmarange J, Balestre E, Orne-Gliemann J, Iwuji C, Okesola N, Newell M-L, et al. HIV ascertainment through repeat home-based testing in the context of a treatment as prevention trial (ANRS 12249 TasP) in rural South Africa. HIV Research for Prevention; 2014 October 28–31; Cape Town, South Africa. abstract P52.05. [Google Scholar]
- 19.Naik R, Doherty T, Jackson D, Tabana H, Swanevelder S, Thea DM, et al. Linkage to care following a home-based HIV counselling and testing intervention in rural South Africa. J Int AIDS Soc. 2015;18:19843. doi: 10.7448/IAS.18.1.19843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mugglin C, Estill J, Wandeler G, Bender N, Egger M, Gsponer T, et al. Loss to programme between HIV diagnosis and initiation of antiretroviral therapy in sub-Saharan Africa: systematic review and meta-analysis. Trop Med Int Health. 2012;17(12):1509–20. doi: 10.1111/j.1365-3156.2012.03089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosen S, Fox MP. Retention in HIV care between testing and treatment in sub-Saharan Africa: a systematic review. PLoS Med. 2011;8(7):e1001056. doi: 10.1371/journal.pmed.1001056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zaidi J, Grapsa E, Tanser F, Newell ML, Barnighausen T. Dramatic increase in HIV prevalence after scale-up of antiretroviral treatment. AIDS. 2013;27(14):2301–5. doi: 10.1097/QAD.0b013e328362e832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Houlihan CF, Bland RM, Mutevedzi PC, Lessells RJ, Ndirangu J, Thulare H, et al. Cohort profile: Hlabisa HIV treatment and care programme. Int J Epidemiol. 2011;40(2):318–26. doi: 10.1093/ije/dyp402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iwuji CC, Orne-Gliemann J, Tanser F, Boyer S, Lessells RJ, Lert F, et al. Evaluation of the impact of immediate versus WHO recommendations-guided antiretroviral therapy initiation on HIV incidence: the ANRS 12249 TasP (Treatment as Prevention) trial in Hlabisa sub-district, KwaZulu-Natal, South Africa: study protocol for a cluster randomised controlled trial. Trials. 2013;14:230. doi: 10.1186/1745-6215-14-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orne-Gliemann J, Larmarange J, Boyer S, Iwuji C, McGrath N, Barnighausen T, et al. Addressing social issues in a universal HIV test and treat intervention trial (ANRS 12249 TasP) in South Africa: methods for appraisal. BMC Public Health. 2015;15:209. doi: 10.1186/s12889-015-1344-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fox MP, Larson B, Rosen S. Defining retention and attrition in pre-antiretroviral HIV care: proposals based on experience in Africa. Trop Med Int Health. 2012;17(10):1235–44. doi: 10.1111/j.1365-3156.2012.03055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Morris SS, Carletto C, Hoddinott J, Christiaensen LJ. Validity of rapid estimates of household wealth and income for health surveys in rural Africa. J Epidemiol Community Health. 2000;54(5):381–7. doi: 10.1136/jech.54.5.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Medley A, Ackers M, Amolloh M, Owuor P, Muttai H, Audi B, et al. Early uptake of HIV clinical care after testing HIV-positive during home-based testing and counseling in western Kenya. AIDS Behav. 2013;17(1):224–34. doi: 10.1007/s10461-012-0344-5. [DOI] [PubMed] [Google Scholar]
- 29.Barnabas RV, van Rooyen H, Tumwesigye E, Murnane PM, Baeten JM, Humphries H, et al. Initiation of antiretroviral therapy and viral suppression after home HIV testing and counselling in KwaZulu-Natal, South Africa, and Mbarara district, Uganda: a prospective, observational intervention study. Lancet HIV. 2014;1(2):68–76. doi: 10.1016/S2352-3018(14)70024-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wringe A, Roura M, Urassa M, Busza J, Athanas V, Zaba B. Doubts, denial and divine intervention: understanding delayed attendance and poor retention rates at a HIV treatment programme in rural Tanzania. AIDS Care. 2009;21(5):632–7. doi: 10.1080/09540120802385629. [DOI] [PubMed] [Google Scholar]
- 31.Nakigozi G, Atuyambe L, Kamya M, Makumbi FE, Chang LW, Nakyanjo N, et al. A qualitative study of barriers to enrollment into free HIV care: perspectives of never-in-care HIV-positive patients and providers in Rakai, Uganda. Biomed Res Int. 2013;2013:470245. doi: 10.1155/2013/470245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barnabas RV, Van Rooyen H, Tumwesigye E, Brantley J, Krows M, van Heerden A, et al. Community-based HIV testing and linkage effectively delivers combination HIV prevention: results from a multisite randomized trial. 8th International AIDS Society Conference on HIV Pathogenesis, Treatment and Prevention; 19–22 Jul; Vancouver, Canada. abstract MOAC0105LB. [Google Scholar]
- 33.Hatcher AM, Turan JM, Leslie HH, Kanya LW, Kwena Z, Johnson MO, et al. Predictors of linkage to care following community-based HIV counseling and testing in rural Kenya. AIDS Behav. 2012;16(5):1295–307. doi: 10.1007/s10461-011-0065-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nsigaye R, Wringe A, Roura M, Kalluvya S, Urassa M, Busza J, et al. From HIV diagnosis to treatment: evaluation of a referral system to promote and monitor access to antiretroviral therapy in rural Tanzania. J Int AIDS Soc. 2009;12:31. doi: 10.1186/1758-2652-12-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bassett IV, Giddy J, Chaisson CE, Ross D, Bogart LM, Coleman SM, et al. A randomized trial to optimize HIV/TB care in South Africa: design of the Sizanani trial. BMC Infect Dis. 2013;13:390. doi: 10.1186/1471-2334-13-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bassett IV, Coleman SM, Giddy J, Bogart LM, Chaisson CE, Ross D, et al. Linkage to HIV/TB care in South Africa: a randomized trial of health navigators. Conference on Retroviruses and Opportunistic Infections (CROI); 2015 Feb 23–26; Seattle, USA. 2015. abstract 93. [Google Scholar]
- 37.MacPherson P, Lalloo DG, Webb EL, Maheswaran H, Choko AT, Makombe SD, et al. Effect of optional home initiation of HIV care following HIV self-testing on antiretroviral therapy initiation among adults in Malawi: a randomized clinical trial. JAMA. 2014;312(4):372–9. doi: 10.1001/jama.2014.6493. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.