Abstract
Despite a large body of literature on the food environment, little is known about the role of supercenters in human nutrition and health. The objectives of this review are to examine what is currently known about the association between supercenters, nutrition, and obesity, to identify how supercenters may affect disparities in food access and nutritional quality of food purchases, and to document the rapid rise of supercenters as a source of food purchases in the United States. A case study of Wal-Mart, the largest food retailer in the United States, is presented that demonstrates the major and increasing role of supercenters as a source of packaged food purchases in the United States, particularly among low-income households, as well as the role of supercenters in supplying key nutrients. Taken together, this review and case study highlight the dominant role of supercenters in the US diet and the need to better understand how supercenters can be leveraged to improve the nutritional quality of what consumers buy and eat.
Keywords: diet, disparities, food environment, food purchases, food stores, Wal-Mart.
INTRODUCTION
There is a large body of literature establishing that the local food environment, and in particular, access to supermarkets, is associated with achieving a healthy diet 1–3 and lower prevalence of overweight and obesity, 4 , 5 although these results are not conclusive. 6 In addition, food retailers have been increasingly recognized by public health experts as potential agents for improving nutrition and preventing obesity, 7 , 8 not only because of their major role as a source of daily energy 9 , 10 but also because of their pivotal position between food companies and the public. Much less is known, however, about the nutritional and health impact of supercenters, which, in the last decade, have grown more than all other store formats. 11 Owing to a concurrent trend toward consolidation and proliferation of chain food retailers, some of these supercenters have become predominant sources of food purchases and, thus, food intake. 11–13 Current perceptions of supercenters in the field seem to be that the food available and purchased there is less healthful than that available at more traditional food stores or farmers’ markets, but the literature on this topic is nascent. Given the rapid growth of supercenters in the United States and globally, 14 , 15 it is important to understand how supercenters differ from more traditional food retail formats, how these differences relate to the healthfulness of food purchases made there, and the extent to which supercenters increasingly serve as a source of food purchases and key nutrients.
The objectives of this narrative review are to review the literature on several topics: (1) the known impact of supercenters on diet quality and human health, along with the potential for supercenters to contribute to (or alleviate) diet-related disparities; (2) the spread of supercenters both in the United States and globally, including probable drivers; and (3) the research gaps that are critical to understanding the impact of this spread on how food is produced and purchased around the globe. To showcase the growing contribution of supercenters as a source of food and key nutrients, a case study analysis of packaged food purchases (PFPs) from Wal-Mart, the largest supercenter chain (and overall largest food retailer) in the United States, was conducted from 2000 to 2012.
DIFFERENCE BETWEEN SUPERCENTERS AND OTHER FOOD RETAILERS IN KEY DIMENSIONS OF HEALTHY FOOD RETAIL ENVIRONMENTS
A great deal has been written about the relationship between the food environment, including food stores (convenience stores, grocery stores, and supermarkets), diet, and health, and this literature has been reviewed elsewhere. 16–19 In general, the relationship between food stores, diet, and health, is predicated on key dimensions – where food is sold (i.e., accessibility of stores within a community), what food is sold (i.e., availability and quality of healthy foods within a store), and how food is sold (i.e., pricing, promotion, or education strategies to inform consumer choices) – which then purportedly influence what people buy and subsequently eat. 20 , 21 Currently, the evidence is mixed with regard to whether introducing a new grocery store or supermarket or changing within-store options improves the healthfulness of food purchases. 18 , 22 Recent studies suggest that placing grocery stores in areas of low access is not sufficient to improve the nutritional profile of purchases 23–25 and that educational differences, not introduction of new stores or changes in store offerings, are the major determinants of disparities in purchasing. 24 On the other hand, there is evidence to suggest that the type of retailer matters: for example, a number of studies have focused on convenience stores as contributors to poorer diet quality and increased obesity. 17 , 26 , 27
Supercenters differ from grocery stores or supermarkets in all 3 dimensions of food store healthfulness (what, where, and how). Supercenters tend to be large stores, averaging over 180 000 square feet, and combine discount department stores with grocery retail, selling a wide assortment of food and nonfood products, including clothing, drugs, and home office supplies, in contrast to supermarkets or grocery stores, which specialize in selling food (although they may sell some nonfood products as well). 28 , 29 Supercenters are also more likely to open in suburbs, due to lower rent, increased space requirements, and fewer landholders with whom to negotiate, 30 making them potentially less accessible to those in inner cities, rural areas, or without transportation. Relative to grocery stores and supermarkets, supercenters set lower, less variable prices (i.e., “everyday low pricing”) across a wide assortment of products, and, while offering more categories, offer less variety within categories compared to traditional grocers. 31–33
These differences have potential implications for the nutritional quality of foods purchased at supercenters, the subsequent diet and health outcomes, and the diet-related disparities. Yet, relative to the literature on corner stores and grocery stores, much less is known about how the supercenter store format influences the healthfulness of food purchases. The remainder of this review will highlight existing knowledge of the link between supercenters, nutrition, health, and disparities, as well as the rapid rise of supercenters in the United States and globally.
LINK BETWEEN SUPERCENTERS AND POORER NUTRITIONAL QUALITY
While the literature directly comparing supercenters with grocery stores and supermarkets is virtually nonexistent, limited evidence from the United States is suggestive but inconclusive that supercenters are linked to poorer nutritional quality.
A study conducted by Bustillos et al. 34 in 2006 found that in 2 rural counties in Texas, the food available in mass merchandisers may be less healthful than that available in grocery stores or supermarkets. The study also found that mass merchandisers offered healthful food items, including canned fruits and vegetables, canned meat and fish, milk, and grains, and offered a greater variety of healthful packaged options, including canned tuna and poultry, reduced-fat and skimmed milk, and low-fat tortillas than did traditional food stores like supermarkets. However, considering that the mass merchandisers surveyed offered no fresh fruits or vegetables, these retailers likely do not represent most supercenters, which carry a full line of groceries, including fresh produce, and have evolved in recent years to carry even more fresh produce.
A number of works have examined the link between food store density and some measure of food “healthfulness,” but these have been ecological in nature and limited in their ability to establish the nutrient quality of purchases at one type of retailer compared with another. For example, using an instrumental variables approach, Bonnano et al. 35 found that state-level increases in the density of Wal-Mart stores was associated with a decreased percentage of adults consuming at least 5 servings of fruits or vegetables per day, and an increased percentage of obese adults. Similarly, Volpe, 36 using household purchase data from 1998–2006, found that a 1% increased supermarket share was associated with decreased “basket healthfulness,” of 0.10% to 0.46%, although basket healthfulness was measured by grouping foods on the basis of the 2010 Dietary Guidelines for Americans rather than actual nutrient content. When comparing supercenter baskets with supermarket baskets, authors found slight but significant differences, with fruits and vegetables accounting for 6.6% and 7.3% of food expenditures at supermarkets compared with 4.8% and 5% at supercenters, and commercially prepared foods (i.e., snacks, sweets, prepared meals) accounting for 45.1% of expenditures at supercenters compared with 37.3% at supermarkets. Volpe 36 also found some evidence of regional variation, with the difference between supercenter and supermarket basket healthfulness scores being substantially less in the South than in the West, Midwest, and Northeast. Perhaps most importantly, Volpe 36 found that the negative effect of increased supercenter share diminished over time, with little impact by 2006, suggesting that, by the mid-2000s, supercenters were becoming comparable to more traditional store formats.
One potential contributor to the link between supercenters and diet is the shift to “one-stop shopping” that big-box retailers offer. Although these retailers have shifted from mainly processed foods and staples to offering of produce, 37 one major question is whether shoppers are more likely to purchase more nonperishable food items at the expense of fresh produce if they make less frequent trips. Bhargava 38 found that, among food stamp recipients, decreasing shopping trip frequency was associated with decreased calcium, fiber, and β-carotene densities, suggestive of less produce purchased. As far as can be determined, no work has examined how one-stop shopping affects the types of food consumers buy and thus consume. However, despite the lack of evidence about how supercenters affect what people buy at these stores, supercenters have generated improvements in food quality through their focus on food safety and solving cold chain distribution issues. 39
Supercenters can also affect diet quality indirectly by lowering the cost of the food supply. In addition to gains achieved by advances in technology and economies of scale, supercenters procure lower costs through strong purchasing power, vendor relations, and more efficient transportation and logistics. 40 On average, prices of foods at supercenters are 27% lower than the same product at a supermarket or other conventional store format. 28 In fact, one study found that store type is the most significant determinant of food costs, 41 and that supercenters were associated with decreased cost of low-fat dairy, whole grains, and dark green vegetables. Another study found the biggest cost differentials for meat (about 12% lower), produce and dairy (11% lower), and grain (6% lower), with the differential being greater for private-label vs nationally branded products. 42 Notably, little work has looked explicitly at cost differences in less healthful, higher-energy food groups, including sugary beverages, sweets, and savory snacks. Prices at supercenters also result in lower prices at competing supermarkets, including prices of fresh produce, red meat, dairy, and consumer packaged goods, 28 , 43 for both private-label and nationally branded products, 44 although this price reduction tends to be bigger at smaller grocery outlets than at bigger supermarket chains (e.g., Kroger’s, Safeway). 45
Finally, the link between supercenters and nutrition is likely changing – at least in the United States. Increasingly, food retailers, including supercenters, claim to be implementing healthier foods initiatives to help consumers make more nutritious choices. Notably, Wal-Mart rolled out an initiative in 2011, aimed improving the nutritional quality and affordability of their products. Wal-Mart’s initiative entailed 3 major components: (1) development of a front-of-package labeling system for Wal-Mart-brand products that meet specified health criteria; (2) strategic price reductions on healthier items; and (3) product reformulation of Wal-Mart-brand products, with goals to achieve elimination of trans fats, a 25% reduction in sodium, and 10% reduction in added sugar in key PFP categories by 2015. 46 , 47 The company has also reported increasing sales of locally sourced and organic foods. 48 , 49 However, to date, no independent research has empirically tested whether these initiatives have actually improved the nutritional quality of foods purchased, and retailers may simultaneously engage in marketing efforts that would counteract these initiatives. For example, Wal-Mart recently faced criticism for promoting high-sugar, high-fat, and high-sodium foods and beverages in its advertisements targeted at low-income customers. 50 It is also important to note that Wal-Mart made this commitment for the United States but did not carry this over to its global markets, and it is unclear whether other major supercenters are considering similar initiatives in other countries.
POSSIBLE LINK BETWEEN SUPERCENTERS AND INCREASES IN OBESITY
One major economic theory on the increase in obesity in the United States and globally is that technological advances have led to decreased costs in both food production and distribution, which, coupled with declines in physical activity, have led to excess energy intake and subsequent weight gain. 51–55 Supercenters are associated with decreased prices of foods within the retailer and at surrounding retailers, 28 leading to an overall cheaper food supply. In fact, according to Lakdawalla and Philipson, 54 40% of growth in body mass index in the United States from 1976 to 1994 was due to reductions in the price of food. On the other hand, cheaper prices of fruits and vegetables could have a beneficial effect, decreasing the overall energy density of household food purchases.
To date, the empirical evidence has been equivocal, complicated by a number of studies that grouped supercenters together with supermarkets 56 and the fact that most studies have been conducted at the aggregate level. For example, using county-level data on urban food environment and the rate of obesity, Salois 57 found that an additional standard deviation in supercenter density is associated with a lower rate of childhood obesity, but only in metropolitan counties. A 2011 study by Jilcott et al. 58 found that a 1–standard deviation increase in the number of grocery stores or supercenters per 1000 residents was associated with a 0.59% increase in county-level obesity prevalence, while a small (n = 197) 2012 study by the same author found that, in eastern North Carolina, among female Supplemental Nutrition Assistance Program (SNAP) participants, body mass index was not associated with distance to or use of any particular food venue, including supercenters. 59
On the other hand, a recent study of county-level data found that an additional supercenter was associated with an increase in obesity of 26–30 people per 10 000 in metropolitan regions and 24–26 people per 10 000 in nonmetropolitan regions, while an additional grocery store decreases obesity by 7–8 people per 10 000 (metropolitan regions only) and additional specialized food store decreases obesity by 25–30 people per 10 000 (metropolitan regions) or 35–38 people per 10 000 (nonmetropolitan). 60 Using an instrumental variables approach, Courtemanche and Carden 55 found that an additional Wal-Mart Supercenter per 100 000 residents increases the likelihood of obesity by 2.4%, with a stronger effect among women, low-income married individuals, and those living in rural areas. Similarly, using state-level data on Wal-Mart store density, with instrumental variables to control for potential endogeneity of Wal-Mart store location, Bonanno and Goetz 61 found that an additional one Wal-Mart Supercenter was associated with a 0.26% increase in the rate of adult obesity. Moreover, the impact of additional Wal-Mart stores depended upon how many Wal-Mart stores were already in an area: states with fewer Wal-Mart stores showed weaker links between Wal-Mart and obesity, whereas states with many Wal-Mart stores showed an increase in obesity ranging from 1.0 to 1.56 percentage points for each additional Wal-Mart per 100 000 people.
Finally, a recent study examining multiple retailer types (supermarkets, supercenters, convenience stores, and specialty stores), found that, while counties with an overall greater number of retailers had a lower obesity prevalence, a 10% increase in the number of supercenters was associated with a 2.56% increase in obesity prevalence. 62 However, since the location of supercenters is not chosen randomly, one possibility is that supercenters are opening in locations that are already more prone to becoming obese. In addition, most households shop at more than one retailer, 63 complicating any analysis of the link between a single retailer or retailer type and diet or obesity. More work is needed to understand both the temporality of this relationship and the pathway linking food purchases to food intake and obesity.
SUPERCENTERS, SOCIOECONOMIC STATUS, AND DISPARITIES IN ACCESS AND PURCHASING
While research on associations between socioeconomic status and the food environment is well established and indicates that individuals of low socioeconomic status tend to have less access to supermarkets, 64 , 65 most studies do not include supercenters, indicate whether supercenters are included, or distinguish supercenters from supermarkets. 4 , 27 , 66
As noted above, supercenters tend to open in suburbs 30 and can actually exacerbate disparities in food access, since it is more challenging for low-income, rural, and inner-city residents to access them. In particular, residents in rural areas may be most affected by the rapid growth of supercenters, 67 as food sales have shifted from counties without supercenters to those with supercenters, 68 while smaller retailers disappear. 69 Other work has shown that the effect of supercenter entry on other grocery store sales is substantially bigger in nonmetropolitan areas. 70 The overall effect is to create pockets with minimal proximal food access, where residents must either pay higher prices at gas stations, convenience stores, or small grocers or have access to a vehicle and the time required to reach a major grocery outlet, 71 which is a major barrier for low-income households. 72 , 73
In addition, work from Sharkey et al. 74 shows that Texas residents in more deprived neighborhoods and rural areas must travel farther to reach a supercenter, 75 although in Louisiana, income level is not associated with supercenter locations. 41 Kaufman 76 showed that, across the United States, low-income and urban populations have lower access to both supermarkets and supercenters. Data on access to supercenters by race/ethnicity are more limited: although it is well established that black neighborhoods have fewer supermarkets than white neighborhoods, 66 , 77 the literature on supercenter density in these neighborhoods is minimal, although minorities are more likely to live inside cities, 78 where supercenters are less likely to locate.
Despite these indications that lower-income and racial or ethnic minorities may face more barriers in traveling to supercenters, the evidence suggests that African American individuals are more likely to shop at lower-priced outlets and supercenters. 28 , 63 Additionally, low-income households spend a greater share of their food expenditures at supercenters. 79 Supercenters could also have an impact on food purchases in the SNAP: 2008 data shows that 86% of SNAP benefits are redeemed at supermarkets and large grocery stores (although it is not clear whether this includes supercenters), 80 and Wal-Mart is among the largest recipient of SNAP spending. 81 Other work has suggested the possibility of reverse causality: using spatial econometric methods, Goetz and Swaminathan 82 found that additional Wal-Mart stores were associated with increases (or smaller decreases) in family poverty rates during the 1990s. As far as can be determined, aside from issues of access, no studies have examined whether the actual nutritional quality of what people buy at supercenters differs by race/ethnicity or income status.
More work is needed to parse out the effect of supercenters on disparities in both access to food and the nutritional quality of purchases. The answer is likely complicated, as it is possible for supercenters to increase disparities in access to food while potentially improving the nutritional quality of purchases for those who do shop there by offering a wider assortment of foods and lower-priced produce. On the other hand, for those who must travel to reach a supercenter, other questions are whether supercenters shift consumers away from produce, which is perishable, and toward packaged foods, which are more shelf stable, and whether these substitutions are nutritionally similar (i.e., canned fruit instead of fresh fruit) or potentially harmful (i.e., fruit snacks instead of fresh fruit). In addition, factors that predict whether someone can or wants to shop at a supercenter must be taken into account when evaluating disparities in food purchases across retailer types, as those who can or are willing to shop at a supercenter might have other underlying characteristics also associated with the differential nutritional profile of purchases, which introduces selectivity. For example, if someone who is willing to drive to a supercenter has a stronger preference for less-healthy foods, or if supercenters tend to locate in areas where people are more strongly inclined to buy less-healthy foods, this could create a spurious association of supercenters with a worse nutritional profile of purchases. In other words, it will be important to consider whether the nutritional profile of purchases truly varies between groups or is simply a reflection of who the store attracts or who is able to shop there.
GROWING DOMINANCE OF SUPERCENTERS AND CHAIN RETAILERS
These links between supercenters, diet quality, and health become especially important when considering the rapid growth of supercenters in the United States and around the globe.
Growth of supercenters in the United States
Since the mid-1900s, the places where US households shop for food has shifted from independent grocery stores and supermarkets to large chain supermarkets, 83–87 and especially to supercenters. 83 , 88 The advent of this trend toward chain retailers occurred in the late 1800s, with the introduction of the A&P “economy” store format, which shifted food retailing from a vast number of specialty and general stores operating on credit and home deliveries to a standardized, cash-based store format, selling A&P branded products. 86 This model gave rise to a number of chain retailers that integrated vertically from manufacturing and distribution, harnessing powers of economy and also leading to the growth of store-branded products. After World War II, increased urbanization, suburbanization, and income, coupled with increased use of automobiles and refrigerators, meant customers could visit stores less frequently but buy more when they went, spawning an influx of the first supercenters on the outskirts of town, where rents were lower. These new stores focused on low prices and carrying an assortment of both food and nonfood products, while also shifting from the prior model of offering store-branded products to a model based on the increased popularity of nationally branded products. 86 By the 1980s, the chain supermarket format was well established, with food retailers expressing little or no interest in developing supercenters.
Around the same time period, however, Wal-Mart and Meijer pioneered the supercenter model, with Meijer in the Midwest and Wal-Mart initially in the South but expanding rapidly and reaching over 4000 stores across all 50 US states by 2014. 89 , 90 Other discount stores, like Kmart and Target, also began opening their versions of supercenters in the early 1990s. 91 , 92 From 2000 to 2011, supercenters and warehouse club stores doubled their share of food sales from 7.1% to 16%, and in 2013, Wal-Mart was largest food retailer in the United States, with $117.4 billion in grocery sales, nearly $40 billion more than the Kroger, the second-largest retailer. 11
Global growth of the supercenter model
In Europe, the concept of a supercenter has been around since 1963 in the form of hypermarkets (i.e., the combination of discount department store and supermarket, namely Carrefour), which grew rapidly from 1970 to 1999, especially in France and Germany. 90 , 93 Wal-Mart also entered Europe in the late 1990s, primarily by acquiring existing hypermarkets (ASDA in the United Kingdom, and Wertkauf and Interspar in Germany), 40 , 94 although it exited Germany in 2006, primarily due to poor integration culturally and competition from other discount retailers. 95 In developing regions, per capita income growth and the rapid expansion of the middle class increased demand for processed foods, providing supermarkets and supercenters with an additional advantage owing to economies of scale. 15 , 96 Modernization of the supply chain, coupled with the growth of large-scale food manufacturers and an increase in direct foreign investment, further bolstered this shift. 37 , 96
This diffusion of large chain retailers, including supercenters, began in Latin America, Central Europe, and South Africa in the early 1990s, with particularly rapid expansion in Latin America, as supermarkets moved from 10%–20% of the retail sector in 1990 to 50%–60% in 2000. 96 This expansion was followed in the mid-1990s by the spread of supermarkets in Southeast Asia, Central America, and Mexico, and finally in China, Vietnam, India, and Russia in the late 1990s and 2000s, 97 with especially rapid expansion in India and China. 37 Currently, Wal-Mart is the largest international retailer, with operations in Argentina, Brazil, Canada, China, Costa Rica, El Salvador, Guatemala, Honduras, Japan, Mexico, Nicaragua, Puerto Rico, and the United Kingdom. 98 Perceptions of Wal-Mart’s growth spawned further consolidation of supercenters across the globe, as Carrefour’s merger with Promodes made it the second largest retailer, with a strong presence in Europe and Latin America. 13 The growth of supercenters also affects global farming, as these major chains create direct linkages with farmers in Asia and other regions and directly control farm decision-making for increasing numbers of farmers. 99
DRIVERS OF THE SHIFT TOWARD SUPERCENTERS
Advances in information technology, transportation, and logistics
Rapid expansion of supercenters was both driven by and a driver of increased efficiencies: as retailers grew in both the size and the number of stores, they were better able to take advantage of economies of scale, lowering the relative cost, which further promoted expansion. 98 These increases in scale were achievable largely through major evolutions in information technology, including the adoption of the barcode and store scanner technology by the late 1980s, which reduced the cost of processing shipments by half 100 and vastly increased the number of products stores could carry. 86 These developments benefitted chain stores more than independent retail stores, as economies of scale lowered the relative cost of implementing technologies. 101 Moreover, the technologies themselves reduced labor costs more at bigger retailers, resulting in more rapid adoption of technology 98 and enabling bigger chains to grow even more rapidly. Wal-Mart in particular was an early adopter of technologies, including the use of computers and software to link stores and distribution centers beginning in the 1970s. 98 By 2005, the implementation of radio-frequency identification tags, which allowed retailers to monitor and respond in real time to data on shipments, inventory, and sales, 102 further drove down supply-chain costs, promoting further expansion.
Social and economic drivers of growth
The growth of the supercenter model has also been driven by a number of social and economic shifts as consumers have begun to prioritize cost and time savings over other factors like quality, convenience, or service. Skyrocketing global food prices in 2007 and the “Great Recession” in the United States 103–105 further increased discount-seeking behavior and cost-consciousness and reduced overall food expenditures. 88 , 106 These increases in discount-seeking have made supercenters, with their “everyday low pricing” strategy, more appealing than traditional grocery formats, which offer periodic deep discounts on fewer foods. 63 , 90 In addition, previous findings have shown that that shoppers who purchase more private-label (store-branded) items are more likely to shop at Wal-Mart. 29 Thus, growth of market share in the private-label sector over the last decade 106 , 107 could also drive consumers toward increased supercenter purchases, although, as far as can be determined, this has not been tested empirically and could simply reflect increased discount-seeking. Finally, increased perceptions of time scarcity in the United States, 108 as well as urbanization and the entry of women into the formal labor market in developing countries, 109 have increased the convenience advantage of the supercenter’s “one-stop shopping” format, which allows shoppers to buy a wide range of products at one time. 33 , 87 , 90 , 110
Despite the documentation of overall increases in the prevalence of supercenters, the sales from these stores, and the potential drivers of these changes, relatively little is known about the extent to which supercenters serve as a source of food and nutrients in the United States. As consolidation and proliferation creates an environment in which fewer food retailers account for a larger share of groceries, it is important to understand who shops at supercenters, how much they buy there, and the contributions of these retailers to total food purchases and key nutrients in order to identify whether and to what degree supercenters (or a single supercenter chain) can be leveraged to improve diet quality, especially among low-income and racial or ethnic minority households. Yet, as pointed out previously, little work has explicitly examined the associations between income, race/ethnicity, and supercenters, and as far as can be determined, no work has documented shifts in the nutritional contribution of superstores to total food store purchases. Differential patterns of supercenter shopping by socioeconomic status are particularly important to identify, in order to better understand issues of selectivity in future efforts to model the supercenter-diet relationship. The following section presents a “case study” of the United States’ largest supercenter, to document this shift in how many and the characteristics of households who shop there, as well as the contributions to key nutrients purchased.
WAL-MART IN THE UNITED STATES: A CASE STUDY
Perhaps the most important supercenter to understand is Wal-Mart, which opened its first supercenter with a full line of groceries in 1988 111 and is now is the largest grocery retailer in the United States. 112 Despite a large body of work examining the impact of Wal-Mart’s expansion on wages, jobs, and other food retailers, 70 , 98 , 113–116 as far as can be determined, no independent research has examined shifts in food purchases at Wal-Mart stores over time or the role of Wal-Mart stores as a source of energy and other key nutrients. Existing work has predominantly looked only at how the share of Wal-Mart supercenters in a geographical region relates to food purchases, rather than examining the purchases themselves or the actual nutrients purchased. Key questions relate to not only what percentage of households shop for food at Wal-Mart, but how much households are buying there. Do a small fraction of households purchase a large share of food purchases at Wal-Mart, or do the majority of households shopping at Wal-Mart buy only a small fraction of their total food purchases there? To what degree do Wal-Mart purchases contribute to total energy purchased? Are low-income households more likely to buy more there, and is this relationship consistent across racial or ethnic groups? Understanding the size and scope of Wal-Mart purchases is important for understanding how this dominant supercenter – and supercenters in general – affect the nutritional quality of what households buy and eat.
The objective of this case study is to examine trends in the percentage of US households shopping at Wal-Mart as well as changes in the distribution of the proportion of food purchases these households purchase there. In addition, the per capita contribution of Wal-Mart purchases to total energy, sugar, sodium, and saturated fat purchased is described. Finally, several trends are examined: whether low-income households are more likely to purchase a higher proportion of food purchases at Wal-Mart than higher-income households, whether this has changed over time, and whether the association of low income with Wal-Mart purchasing is constant across racial or ethnic groups.
Methods
To conduct this case study, Nielsen Homescan, 117 a commercial dataset containing information on PFPs in the United States at the household-quarter level, was used. Packaged food purchases include all food and beverages with a barcode, including all consumer packaged goods as well as packaged fresh fruit and vegetables (e.g., bag of lettuce, bag of potatoes) but excluding unpackaged meats and produce (e.g., an apple). Participating households use a handheld scanner to record all purchases during each shopping trip. Households are sampled from 76 markets and are weighted to be nationally representative. Households report detailed information on each PFP purchased from outlet channels, including grocery (e.g., Kroger’s, Safeway, etc.), drug, supercenters (e.g., Super Target, Wal-Mart), club stores (e.g., Sam’s Club), dollar stores, and convenience stores. Because the types of products available may differ at nontraditional food outlets, for this study, total food store purchases included all PFPs from grocery stores, supermarkets, and supercenters, and excluded warehouse, drug, club, dollar, and convenience stores. Purchases were aggregated at the year-household level, for a total of 663 073 household-year observations from 158 382 unique households.
Statistical analysis
All statistical analyses were performed using STATA, version 13 (StataCorp; College Station, TX, USA).
Survey commands (for logistic regression) and probability weights (for quantile regression) were used to adjust estimates to be nationally representative using Nielsen’s projection factors. Data were treated as pooled cross-sectional data and did not account for the nonindependence of repeated measurements of households in the sample over time, because robust covariance estimators are not permitted in STATA in conjunction with these methods. However, all models were re-run without adjustment to be nationally representative but with robust covariance estimators; the results were found to be virtually identical.
Logistic regression was used to describe changes in the likelihood of shopping at Wal-Mart (i.e., spent >0$ on any PFP at Wal-Mart) for each year from 2000 to 2012. Secondly, the mean per capita contribution of Wal-Mart PFPs to total food store purchases of key nutrients, including energy, total sugar, saturated fat, and sodium, was examined. Next, among Wal-Mart-shopping households, quantile regression was used to examine changes in the distribution of percent volume of PFPs purchased at Wal-Mart relative to total food store purchases at the 50th, 75th, and 95th percentiles. In each model, the predicted percentage of households, percent contribution to total nutrients, or percent volume of PFPs purchased was compared with findings from 2000, using the Bonferroni correction for multiple comparisons.
To examine the association between income, race/ethnicity, and proportion of PFPs purchased at Wal-Mart, households were divided into quartiles of Wal-Mart shoppers on the basis of the proportion of PFPs purchased at Wal-Mart in 2012. On average, nonshopper households purchased 0% of PFPs from Wal-Mart (range 0.0%–0.3%), low-shopper households purchased 3% (range 3.0%–7.2%, medium-shopper households purchased 18% (range 7.2%–33.9%), and top shoppers purchased 68% (range 33.9%–100%) of PFPs from Wal-Mart. Multinomial logistic models included household race (non-Hispanic white, Hispanic, non-Hispanic black, and non-Hispanic other) and household income [low <185% of the Federal Poverty Level (FPL), medium 185%–400% of the FPL, high >400% of the FPL]. These models controlled for head of household education (≤high school degree, some college, ≥college degree), household type (single adult, multiple adults with no kids, adult(s) with kid(s), and household composition (numbers of men or women aged 19–29, 30–39, 40–49, 50–59, and ≥60 years, and numbers of boys and girls aged 0–1, 2–5, 6–12, and 13–18 years). In addition, models controlled for whether there was a Wal-Mart present in a given market in a given year, as defined by >$10 000 annual sales from PFPs per market per year. Additional cutoff points for determining the presence of a market were also tested (>$0 and $5000) and generally yielded similar results; however, to be sure that purchases in a market were actually from that market and not a neighboring market where households may have traveled to purchase items, the higher cutoff point (>$10 000) was used.
Additional models tested interactions of income and year, as well as income and race/ethnicity, using Wald “chunk” tests for joint significance of interaction. 118 Robust cluster variance estimators were used to adjust the standard errors to reflect the nonindependence of households who remained in the sample across time. 119 , 120 For each model, STATA’s margins command was used to estimate the predicted percentage of households in a shopper category for each income, race/ethnicity, or year combination. All analyses were Bonferonni corrected for multiple comparisons, and statistical significance was set at P < 0.01 for main effects and P < 0.05 for interactions.
Results
Wal-Mart-shopping households were more likely to have children, be less educated, be non-Hispanic white, and have a low or middle level of income (Table 1).
Table 1.
Household characteristics of the Nielsen Homescan sample (n = 663073) according to whether a household shopped at Wal-Mart from 2000 to 2012 a
| Household characteristic | Wal-Mart nonshopper (%) b | Wal-Mart shopper (%) b | P value c |
|---|---|---|---|
| Household composition | |||
| Single adult | 37 | 23 | <0.001 |
| Multiple adults, no children <18 y | 38 | 39 | 0.015 |
| Single adult, with children <18 y | 19 | 29 | <0.001 |
| Adults, with children <18 y | 6 | 8 | <0.001 |
| Race/ethnicity | |||
| Non-Hispanic white | 72 | 75 | <0.0001 |
| Hispanic | 11 | 10 | 0.049 |
| Non-Hispanic black | 11 | 11 | 0.012 |
| Non-Hispanic other | 6 | 4 | <0.001 |
| Education level, male head of household | |||
| ≤High school degree | 21 | 32 | <0.001 |
| Some college | 20 | 21 | 0.45 |
| ≥College degree | 30 | 18 | <0.001 |
| No male head of household | 29 | 29 | 0.273 |
| Education level, female head of household | |||
| ≤High school degree | 23 | 36 | <0.001 |
| Some college | 21 | 27 | <0.001 |
| ≥College degree | 24 | 21 | <0.001 |
| No female head of household | 32 | 16 | <0.001 |
| Income level d | |||
| Low | 20 | 26 | <0.001 |
| Middle | 32 | 40 | <0.001 |
| High | 47 | 34 | <0.001 |
aCalculations based in part on data reported by Nielsen through its Homescan Services for the food and beverage categories for the US market; copyright © 2015, Nielsen Company. Data used with permission.
bPercentages weighted to be nationally representative. A household was defined as "Wal-Mart shopper" if it spent >$0 on any packaged food or beverage in a 1-year period.
cFrom proportions testing between Wal-Mart-shopping households and non-Wal-Mart–shopping households. Bonferonni correction used for multiple comparisons.
dIncome level defined as low, <185% of Federal Poverty Level (FPL); middle, 185%–400% of FPL, and high, >400% of FPL.
The percentage of US households who shopped for PFPs at Wal-Mart increased from 71% in 2000 to 82% in 2012 (P < 0.01). Over the same time period, percent energy from Wal-Mart PFPs increased from 9% in 2000 to 23% in 2012 (P < 0.01), with similar increases observed for sodium, total sugar, and saturated fat (Table 2).
Table 2.
Percent contribution of nutrients from Wal-Mart purchases to total packaged food purchases (PFPs), 2000–2012 a , b
| Year | Energy |
Sodium |
Total sugar |
Saturated fat |
||||
|---|---|---|---|---|---|---|---|---|
| Percent | SE | Percent | SE | Percent | SE | Percent | SE | |
| 2000 | 8.6 | 0.17 | 8.0 | 0.17 | 8.9 | 0.17 | 8.6 | 0.17 |
| 2001 | 11.1 | 0.17 | 10.5 | 0.17 | 11.4 | 0.17 | 11.0 | 0.17 |
| 2002 | 13.2 | 0.15 | 12.9 | 0.16 | 13.4 | 0.15 | 13.0 | 0.15 |
| 2003 | 15.0 | 0.17 | 14.7 | 0.18 | 15.4 | 0.17 | 14.8 | 0.17 |
| 2004 | 16.9 | 0.18 | 16.8 | 0.19 | 17.1 | 0.19 | 16.7 | 0.19 |
| 2005 | 19.1 | 0.17 | 19.1 | 0.18 | 19.3 | 0.17 | 18.8 | 0.18 |
| 2006 | 20.8 | 0.16 | 20.7 | 0.16 | 21.2 | 0.16 | 20.7 | 0.16 |
| 2007 | 22.3 | 0.17 | 22.2 | 0.17 | 22.9 | 0.17 | 22.1 | 0.17 |
| 2008 | 23.0 | 0.18 | 23.1 | 0.18 | 23.5 | 0.18 | 22.7 | 0.18 |
| 2009 | 23.6 | 0.19 | 23.9 | 0.19 | 24.1 | 0.19 | 23.2 | 0.19 |
| 2010 | 23.0 | 0.19 | 23.4 | 0.2 | 23.8 | 0.2 | 22.6 | 0.19 |
| 2011 | 22.6 | 0.19 | 22.8 | 0.19 | 23.2 | 0.19 | 22.2 | 0.19 |
| 2012 | 22.7 | 0.18 | 22.9 | 0.18 | 23.3 | 0.18 | 22.4 | 0.18 |
Abbreviation: SE, standard error.
aCalculations based in part on data reported by Nielsen through its Homescan Services for the food and beverage categories for the US market; copyright © 2015, Nielsen Company. Data used with permission.
bBold print indicates that the percent contribution of PFPs from Wal-Mart to nutrients from total PFPs was different than that in 2000, P < 0.01.
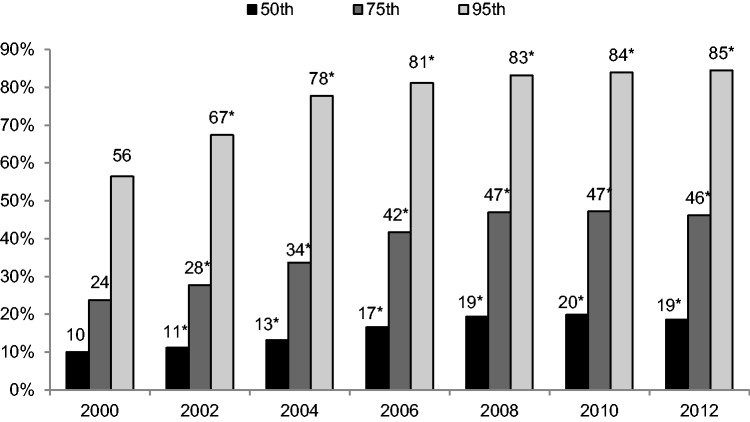
Among households who shopped at Wal-Mart, the median household nearly doubled the proportion of PFPs purchased from Wal-Mart, from 10% in 2000 to 19% in 2012 (P < 0.01) (Figure 1). Increases in the proportion of PFPs purchased from Wal-Mart were even greater at the upper end of the distribution. In particular, households in the 95th percentile of Wal-Mart shoppers increased the proportion of PFPs purchased at Wal-Mart from 56% in 2000 to 85% in 2012 (P < 0.01).
Figure 1.
Percentage of food and beverage packaged food purchases (PFPs) from Wal-Mart (g) by percentile among Wal-Mart customers, 2000–2012. Asterisks indicate that the proportion of PFPs (g) purchased from Wal-Mart in a given year, within that percentile, is different from that in 2000, P < 0.01. Calculations based in part on data reported by Nielsen through its Homescan Services for the food and beverage categories for the US market; copyright © 2015, Nielsen Company. Data used with permission.
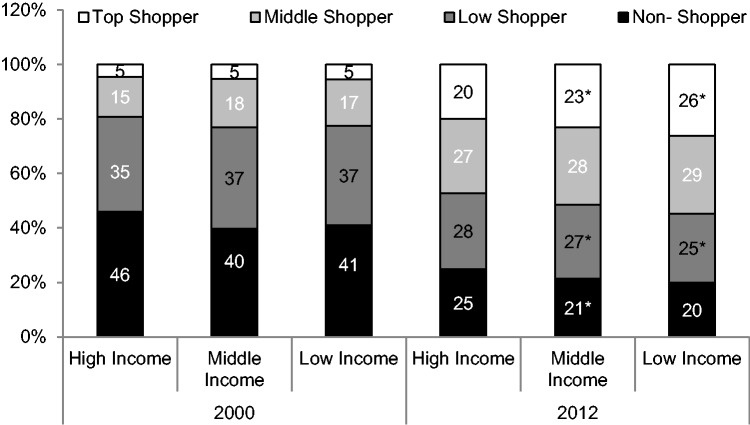
Across all time periods, low- and middle-income households were less likely to be Wal-Mart nonshoppers than high-income households, and were more likely to be top shoppers than high-income households. All income levels showed a decrease in the percentage of Wal-Mart nonshoppers and low shoppers between 2000 and 2012 (Figure 2). However, low-income and middle-income households showed a bigger decline than high-income shoppers: the proportion of low shoppers declined by 12%, 10%, and 7% for low-, middle-, and high-income households, respectively (P < 0.05 for interaction). Similarly, while all income levels showed an increase in the proportion of households who were top shoppers, low- and middle-income households showed larger increases than high-income households, with increases of 21%, 18%, and 15% of households in the top shopper category from 2000 to 2012 for low-, middle-, and high-income households, respectively (P < 0.05 for interaction).
Figure 2.
Percentage of households who were non-, low, middle, and top shoppers of packaged food purchases (PFPs) from Wal-Mart by income status and year, 2000–2012. Shopper categories were based on the average percentage of PFPs from Wal-Mart of total PFPs purchased: nonshoppers purchased on average 0%; low shoppers purchased on average 3%; middle shoppers purchased on average 18%; and top shoppers purchased on average 65%. Income status is defined as low, <131% of Federal Poverty Level (FPL); middle, 131%–185% of FPL; and high, >185% of FPL. Asterisks indicate change in the probability of being in a given Wal-Mart shopper category between 2000 and 2012 is different for medium- or low-income households than for high-income households, P < 0.01. Calculations based in part on data reported by Nielsen through its Homescan Services for the food and beverage categories for the US market; copyright © 2015, Nielsen Company. Data used with permission.
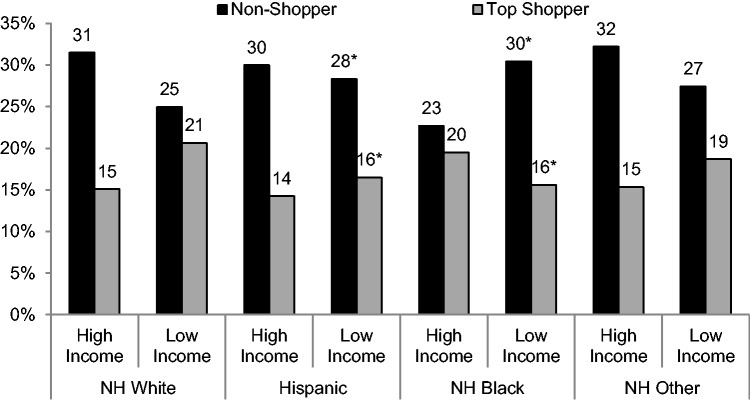
Across all time periods, there were minimal differences in the likelihood of being a non-, low, middle, or top Wal-Mart shopper by race/ethnicity. The only clear difference was that non-Hispanic blacks were less likely to be nonshoppers than non-Hispanic whites (24% vs 28%, respectively [P < 0.01]) (data not shown). However, as shown in Figure 3, there was a significant interaction between race/ethnicity and income level. For non-Hispanic whites, Hispanics, and non-Hispanic others, high-income households were more likely to be nonshoppers than low-income households, and low-income households were more likely to be top shoppers than high-income households. However, among black households, this trend was reversed: low-income households were 7% more likely to be nonshoppers than high-income households, and high-income households were 4% more likely to be top shoppers than low-income households (P < 0.05 for interaction).
Figure 3.
Percentage of households who were nonshoppers or top shoppers of packaged food purchases (PFPs) from Wal-Mart by race/ethnicity and income, 2000–2012. Shopper categories were based on the average percentage of PFPs (g) from Wal-Mart: nonshoppers purchased on average 0%; top shoppers purchased on average 68%. Income status is defined as low, <131% of Federal Poverty Level (FPL); middle, 131%–185% of FPL; and high, >185% of FPL. Asterisks indicate that the difference in the probability of being in a given Wal-Mart shopper category between high-income and low-income households in a given race/ethnic group was different than non-Hispanic whites. Calculations based in part on data reported by Nielsen through its Homescan Services for the food and beverage categories for the US market; copyright © 2015, Nielsen Company. Data used with permission.
Case study summary
Using a dataset of household PFPs, the findings show that the majority (81%) of US households shop for food and beverages at Wal-Mart, and households are buying a larger proportion of PFPs there. Over time, low-income households were increasingly likely to buy more PFPs at Wal-Mart, with the exception of low-income black households, who were less likely to shop there than high-income black households.
Implications and future directions
In the last decade, Wal-Mart has become an increasingly dominant source of PFPs: not only did more US households shop at Wal-Mart, households – and especially low-income households – bought larger shares of volume and energy there over time. This growing dominance underscores the need for more research to fully understand the nutritional impact of the shifts toward supercenters and Wal-Mart in the United States, as well as the impact of other major supercenters that dominate in other countries. 37 , 99 , 121 , 122 In particular, there is currently no work that longitudinally examines whether purchases at supercenters are nutritionally different than those at supermarkets or grocery stores, or whether any observed differences are due to underlying dietary preferences that drive households to shop at a certain store type to begin with. For example, recent studies have shown that introducing a grocery store in a food desert did not change the healthfulness of residents’ purchases (i.e., they did not purchase more produce), 6 , 25 suggesting that the store type (or access to a particular store type) may be less important than underlying preferences.
In addition, this case study clearly demonstrates that some households (low-income white, Hispanic, and non-Hispanic others, in particular), are more likely to buy more at Wal-Mart. If these characteristics – or other underlying household characteristics, like discount-seeking behavior – are also associated with households’ choices of what foods to buy, the associations between supercenter purchases and nutrition could be an artifact of selection bias rather than a true reflection of nutritional discrepancies in supercenter food vs food from other types of food stores. Methods to deal with issues of time-varying selectivity, such as inverse probability weighting, are needed in order to understand differences in the nutritional profile of foods by store type as well as how these differences have changed over time.
In addition, cross-country comparisons are needed to understand both the contribution of supercenters to food purchases and the link between supercenters and obesity in countries undergoing the nutrition transition. It is possible that, by increasing food access and food safety, supercenters could improve nutrition in countries still struggling with malnutrition. On the other hand, countries in later phases of the nutrition transition, like China, could be harmed as shoppers shift from a model dominated by preparing fresh foods purchased almost daily to a supercenter model in which foods are purchased less frequently and are more likely to be packaged or processed.
The rapid growth of supercenters as a source of food also offers a potential public health opportunity to leverage Wal-Mart and other major supercenters as key players to improve diet and reduce obesity. The size and scope of these major national retailers also imbues them with negotiating power over manufacturers, further increasing their potential to drive improvements in nutritional quality.
To assess this potential, more work is needed to understand the current impact of healthier foods initiatives by these retailers. 46 , 123 Research on grocery- and supermarket-based healthier foods initiatives have been equivocal: while some field studies have found that these initiatives demonstrate moderate to high reach 124–126 and improve healthy food availability, sales of targeted foods, and self-reported knowledge, purchasing, and intake of healthier foods, 124 , 127–131 others have found that common components of healthier foods initiatives, such as nutrition labels or targeted discounts, are ineffective at changing long-term purchasing behaviors. 88 , 132–142 These studies, however, have been conducted predominantly in a single store or set of stores, do not include supercenters, are short-term in duration (≈6–18 months of follow-up), and are limited to a few target foods. However, healthier foods initiatives at major national supercenter chains, including Wal-Mart, are not short-term or geographically isolated interventions but rather represent a long-term shift in how foods are produced, marketed, and sold across the United States, creating the need to understand how this shift affects the nutritional quality of purchases over the long term. It is also currently unclear if and how these initiatives work, whether by changing the nutritional content of what people buy (i.e., product reformulation or introducing or removing products) or by changing the choices people make (through front-of-package labeling, price cuts, or other promotions). In addition, it is unclear whether these initiatives actually translate into healthier purchases and improved health, or whether they simply attract more health-conscious consumers.
This review also shows that lower-income households are increasingly buying a larger share of food purchases at Wal-Mart, suggesting that, if effective, supercenter-based initiatives could be useful in reducing diet disparities in this key group. However, it is currently unclear whether healthier foods initiatives affect key subpopulations differentially. While some studies show that lower-income customers tend to be more cost conscious 143 and more likely to take advantage of price promotions, 144 others suggest that low-income customers may not be more responsive to price cuts than higher-income consumers. 145–148 Similarly, better educated customers report higher usage of food labels. 149 , 150 More work is needed to understand whether subpopulations who ostensibly should benefit most from increased availability and affordability of healthier foods, such as low-income and racial or ethnic minorities, actually benefit from supercenter-based healthier foods initiatives.
Finally, no work has considered that people tend to shop at multiple retailers. 31 One major question is that, if people do purchase less-healthy foods at supercenters, do they purchase more healthy foods at other retailers where they shop, so that total-purchase healthfulness remains stable? Or is the effect of supercenters such that it deteriorates the overall nutritional quality of food purchases? Addressing these questions is essential to fully understand both the impact of the food environment on diet and the types of shopping behaviors that should be encouraged or discouraged to maximize nutrition across store formats.
CONCLUSION
This article shows that supercenters, and notably Wal-Mart, are a major and growing source of the US diet, especially among low-income households. As fewer retailers account for a greater share of food purchases, Wal-Mart and other supercenter chains will have an important and growing impact on the nutritional quality of what people buy and eat. Supercenters are a unique type of food retailer with regard to where they locate, what they sell, and how they sell, and these differences can have implications for nutrition and health. While the current evidence suggests that supercenters are associated with a lower nutritional profile of food purchases and increased obesity, longitudinal research is needed to understand whether this remains the case after the selectivity of shopping at supercenters is taken into account. In fact, the growing dominance of supercenters in the United States and globally presents a major research and policy opportunity: understanding how these retailers affect the nutrient profile of purchases could provide valuable insight into strategies and potential avenues for improving the healthfulness of food purchases, especially in countries undergoing the nutrition transition. In the United States in particular, more work is needed to understand the effects of the rapid expansion of Wal-Mart and other supercenters on disparities in food access and food purchasing.
In addition, Wal-Mart’s demonstrated willingness to engage in nutrition promotion through its healthier foods initiative could represent a major opportunity to improve the healthfulness of food and beverage purchases in the United States, especially if other supercenters and food retailers follow suit. Future research is needed to examine whether healthier foods initiatives improve the nutrient profile of foods purchased at supercenters, especially for low-income households, who shop at these stores the most.
Acknowledgments
The authors would like to thank Dr Donna Miles for her excellent work managing the data used for this study, as well as Dr David Guilkey, Dr Anna Maria Siega-Riz, and Dr Mary Story for their insights and review of the manuscript.
Funding. Funding for this study comes from the Robert Wood Johnson Foundation (grant nos. 67506, 68793, 70017, and 71837), the National Institutes of Health (grant no. R01DK098072), and the Carolina Population Center (grant nos. R24 HD050924 and T32 HD007168). No funding source had a role in the design, analysis, or interpretation of the data or in the writing of this report.
Declaration of interest. The authors have no relevant interests to declare.
References
- 1. Morland K, Wing S, Roux AD. The contextual effect of the local food environment on residents' diets: the Atherosclerosis Risk in Communities study. Am J Public Health. 2002;92:1761–1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Larson N, Story M. A review of environmental influences on food choices. Ann Behav Med. 2009;38(suppl 1):S56–S73. [DOI] [PubMed] [Google Scholar]
- 3. Popkin BM, Duffey K, Gordon-Larsen P. Environmental influences on food choice, physical activity and energy balance. Physiol Behav. 2005;86:603–613. [DOI] [PubMed] [Google Scholar]
- 4. Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place. 2009;15:491–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the US [published online November 1, 2008]. Am J Prev Med. 2009;36:74–81. [DOI] [PubMed] [Google Scholar]
- 6. Boone-Heinonen J, Gordon-Larsen P, Kiefe CI, et al. Fast food restaurants and food stores: longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Arch Intern Med. 2011;171:1162–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hawkes C. Dietary implications of supermarket development: a global perspective. Dev Policy Rev. 2008;26:657–692. [Google Scholar]
- 8. Glanz K, Bader MD, Iyer S. Retail grocery store marketing strategies and obesity: an integrative review. Am J Prev Med. 2012;42:503–512. [DOI] [PubMed] [Google Scholar]
- 9. Poti JM, Popkin BM. Trends in energy intake among US children by eating location and food source, 1977–2006. J Am Diet Assoc. 2011;111:1156–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Smith LP, Ng SW, Popkin BM. Trends in US home food preparation and consumption: analysis of national nutrition surveys and time use studies from 1965–1966 to 2007–2008. Nutr J. 2013;12:45 doi:10.1186/1475-2891-12-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. United States Department of Agriculture, Economic Research Service. Retail trends. USDA/ERS website. http://www.ers.usda.gov/topics/food-markets-prices/retailing-wholesaling/retail-trends.aspx#.U0uybPldWSq. Updated 2014. Accessed January 10, 2015.
- 12. Wood S. Revisiting the US food retail consolidation wave: regulation, market power and spatial outcomes. J Econ Geog. 2013;13:299–326. [Google Scholar]
- 13. Te Morenga LA, Howatson AJ, Jones RM, et al. Dietary sugars and cardiometabolic risk: systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids. Am J Clin Nutr. 2014;100:65–79. [DOI] [PubMed] [Google Scholar]
- 14. Popkin BM. Nutrition, agriculture and the global food system in low and middle income countries. Food Policy. 2014;47:91–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reardon T, Timmer CP, Barrett CB, et al. The rise of supermarkets in Africa, Asia, and Latin America. Am J Agric Econ. 2003;85:1140–1146. [Google Scholar]
- 16. Caspi CE, Sorensen G, Subramanian SV, et al. The local food environment and diet: a systematic review. Health Place. 2012;18:1172–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Langellier BA, Garza JR, Prelip ML, et al. Corner store inventories, purchases, and strategies for intervention: a review of the literature. Calif J Health Promot. 2013;11:1–13. [PMC free article] [PubMed] [Google Scholar]
- 18. Escaron AL, Meinen AM, Nitzke SA, et al. Supermarket and grocery store-based interventions to promote healthful food choices and eating practices: a systematic review. Prev Chronic Dis. 2013;10:E50 doi:10.5888/pcd10.120156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gamba RJ, Schuchter J, Rutt C, et al. Measuring the food environment and its effects on obesity in the United States: a systematic review of methods and results. J Community Health. 2015;40:464–475. [DOI] [PubMed] [Google Scholar]
- 20. Glanz K, Sallis JF, Saelens BE, et al. Nutrition Environment Measures Survey in stores (NEMS-S): development and evaluation. Am J Prev Med. 2007;32:282–289. [DOI] [PubMed] [Google Scholar]
- 21. Penney TL, Brown HE, Maguire ER, et al. Local food environment interventions to improve healthy food choice in adults: a systematic review and realist synthesis protocol. BMJ Open. 2015;5:e007161 doi: 10.1136/bmjopen-2014-007161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Seymour JD, Yaroch AL, Serdula M, et al. Impact of nutrition environmental interventions on point-of-purchase behavior in adults: a review. Prev Med. 2004;39:108–136. [DOI] [PubMed] [Google Scholar]
- 23. Elbel B, Moran A, Dixon LB, et al. Assessment of a government-subsidized supermarket in a high-need area on household food availability and children's dietary intakes. Public Health Nutr. 2015;18:2881–2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Handbury J, Rahkovsky I, Schnell M. What drives nutritional disparities? Retail Access and Food Purchases Across the Socioeconomic Spectrum. National Bureau of Economic Research; 2015. [Google Scholar]
- 25. Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff (Millwood). 2014;33:283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rummo PE, Meyer KA, Boone-Heinonen J, et al. Neighborhood availability of convenience stores and diet quality: findings from 20 years of follow-up in the Coronary Artery Risk Development in Young Adults study. Am J Public Health. 2015;105:e65–e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the Atherosclerosis Risk in Communities study. Am J Prev Med. 2006;30:333–339. [DOI] [PubMed] [Google Scholar]
- 28. Hausman J, Leibtag E. Consumer benefits from increased competition in shopping outlets: measuring the effect of Wal-Mart. J Appl Econom. 2007;22:1157–1177. [Google Scholar]
- 29. Singh VP, Hansen KT, Blattberg RC. Market entry and consumer behavior: an investigation of a Wal-Mart supercenter. Marketing Sci. 2006;25:457–476. [Google Scholar]
- 30. Thomas B. Food deserts and the sociology of space: distance to food retailers and food insecurity in an urban American neighborhood. Int J Human Soc Sci. 2010;5:400–409. [Google Scholar]
- 31. Fox EJ, Montgomery AL, Lodish LM. Consumer shopping and spending across retail formats. J Bus. 2004;77:S25–S60. [Google Scholar]
- 32. Bell DR, Lattin JM. Shopping behavior and consumer preference for store price format: why “large basket” shoppers prefer EDLP. Marketing Sci. 1998;17:66–88. [Google Scholar]
- 33. Tang CS, Bell DR, Ho T-H. Store choice and shopping behavior: how price format works. Calif Manag Rev. 2001;43:56–74. [Google Scholar]
- 34. Bustillos B, Sharkey JR, Anding J, et al. Availability of more healthful food alternatives in traditional, convenience, and nontraditional types of food stores in two rural Texas counties. J Am Diet Assoc. 2009;109:883–889. [DOI] [PubMed] [Google Scholar]
- 35. Bonanno A, Goetz SJ. Food store density, nutrition education, eating habits and obesity. Int Food Agribus Manag Rev. 2012;15:1–26. [Google Scholar]
- 36. Volpe R, Okrent A, Leibtag E. The effect of supercenter-format stores on the healthfulness of consumers’ grocery purchases. Am J Agric Econ. 2013;95:568–589. [Google Scholar]
- 37. Reardon T, Timmer CP, Minten B. Supermarket revolution in Asia and emerging development strategies to include small farmers. Proc Natl Acad Sci U S A. 2012;109:12332–12337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bhargava A. Socio-economic and behavioural factors are predictors of food use in the National Food Stamp Program Survey. Brit J Nutr. 2004;92:497–506. [DOI] [PubMed] [Google Scholar]
- 39. Minten B, Reardon T. Food prices, quality, and quality’s pricing in supermarkets versus traditional markets in developing countries. Appl Econ Perspect Policy. 2008;30:480–490. [Google Scholar]
- 40. Fernie J, Arnold SJ. Wal-Mart in Europe: prospects for Germany, the UK and France. Int J Retail Distrib Manag. 2002;30:92–102. [Google Scholar]
- 41. Hatzenbuehler PL, Gillespie JM, O'Neil CE. Does healthy food cost more in poor neighborhoods? An analysis of retail food cost and spatial competition. Agric Resource Econ Rev. 2012;41:43–56. [Google Scholar]
- 42. Leibtag ES, Barker C, Dutko P. How Much Lower are Prices at Discount Stores? An Examination of Retail Food Prices. Washington, DC: United States Department of Agriculture, Economic Research Service; 2010. [Google Scholar]
- 43. Woo B-J, Huang CL, Epperson JE, et al. Effect of a new Wal-Mart supercenter on local retail food prices. J Food Distrib Res. 2001;32:173–181. [Google Scholar]
- 44. Volpe RJ, Lavoie N. The effect of Wal-Mart supercenters on grocery prices in New England. Appl Econ Perspect Pol. 2008;30:4–26. [Google Scholar]
- 45. Basker E, Noel M. The evolving food chain: competitive effects of Wal-Mart's entry into the supermarket industry. J Econ Manag Strategy. 2009;18:977–1009. [Google Scholar]
- 46. Wal-Mart Stores, Inc. Making healthier food a reality for all. Corporate Wal-Mart website. http://corporate.walmart.com/global-responsibility/hunger-nutrition/our-commitments. Updated 2013. Accessed October 15, 2013.
- 47. Wal-Mart Stores, Inc. Walmart report: “Great for You” food labeling initiative. Corporate Wal-Mart website. http://corporate.walmart.com/global-responsibility/hunger-nutrition/great-for-you. Updated 2013. Accessed October 15, 2013.
- 48. Martinez S, Hand MS, Da Pra M, et al. Local Food Systems: Concepts, Impacts, and Issues. Washington, DC: US Department of Agriculture, Economic Research Service; 2010. [Google Scholar]
- 49. Wal-Mart, Inc. Sustainable agriculture. http://corporate.walmart.com/global-responsibility/environment-sustainability/sustainable-agriculture. Corporate Wal-Mart website. Updated 2014. Accessed April 15, 2014.
- 50. Harkinson J. Walmart ads target “low income” consumers with junk food. http://www.motherjones.com/mojo/2013/11/walmart-targets-low-income-consumers-junk-food. Mother Jones website. Published November 18, 2013. Accessed May 15, 2014.
- 51. Philipson TJ, Posner RA. The Long-run Growth in Obesity as a Function of Technological Change. NBER Working Paper no. 7423. Cambridge, MA: National Bureau of Economic Research; 1999. [Google Scholar]
- 52. Philipson T, Posner R. Is the Obesity Epidemic a Public Health Problem? A Decade of Research on the Economics of Obesity. NBER Working Paper no. 14010. Cambridge, MA: National Bureau of Economic Research; 2008. [Google Scholar]
- 53. Chou S-Y, Grossman M, Saffer H. An economic analysis of adult obesity: results from the Behavioral Risk Factor Surveillance System. J Health Econ. 2004;23:565–587. [DOI] [PubMed] [Google Scholar]
- 54. Lakdawalla D, Philipson T. The Growth of Obesity and Technological Change: a Theoretical and Empirical Examination. NBER Working Paper no. 8946. Cambridge, MA: National Bureau of Economic Research; 2002. [Google Scholar]
- 55. Courtemanche C, Carden A. Supersizing supercenters? The impact of Walmart Supercenters on body mass index and obesity. J Urban Econ. 2011;69:165–181. [Google Scholar]
- 56. Bodor JN, Rice JC, Farley TA, et al. The association between obesity and urban food environments. J Urban Health. 2010;87:771–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Salois MJ. The built environment and obesity among low-income preschool children. Health Place. 2012;18:520–527. [DOI] [PubMed] [Google Scholar]
- 58. Jilcott SB, Keyserling T, Crawford T, et al. Examining associations among obesity and per capita farmers' markets, grocery stores/supermarkets, and supercenters in US counties. J Am Diet Assoc. 2011;111:567–572. [DOI] [PubMed] [Google Scholar]
- 59. Jilcott Pitts SB, McGuirt JT, Carr LJ, et al. Associations between body mass index, shopping behaviors, amenity density, and characteristics of the neighborhood food environment among female adult Supplemental Nutrition Assistance Program (SNAP) participants in eastern North Carolina. Ecol Food Nutr. 2012;51:526–541. [DOI] [PubMed] [Google Scholar]
- 60. Yan R, Bastian ND, Griffin PM. Association of food environment and food retailers with obesity in US adults. Health Place. 2015;33:19–24. [DOI] [PubMed] [Google Scholar]
- 61. Bonanno A, Goetz SJ. Adult Obesity and Food Stores’ Density – Evidence from State-Level Panel Data. Denver, CO: Agricultural and Applied Economics Association; 2010. [Google Scholar]
- 62. Marlow ML. Big box stores and obesity. Appl Econ Lett. 2014;22:938–944. [Google Scholar]
- 63. Carpenter JM, Moore M. Consumer demographics, store attributes, and retail format choice in the US grocery market. Int J Retail Distrib Manag. 2006;34:434–452. [Google Scholar]
- 64. Powell LM, Slater S, Mirtcheva D, et al. Food store availability and neighborhood characteristics in the United States. Prev Med. 2007;44:189–195. [DOI] [PubMed] [Google Scholar]
- 65. Kaufman PR, MacDonald J, Lutz SM, et al. Do the Poor Pay More for Food? Item Selection and Price Differences Affect Low-Income Household Food Costs. Agricultural Economic Report no. 759. Washington, DC: Food and Rural Economics Division, Economic Research Service, US Department of Agriculture; 1997. [Google Scholar]
- 66. Morland K, Wing S, Diez Roux Z, et al. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22:23–29. [DOI] [PubMed] [Google Scholar]
- 67. Sharkey JR. Measuring potential access to food stores and food-service places in rural areas in the US. Am J Prev Med. 2009;36(suppl 4):S151–S155. [DOI] [PubMed] [Google Scholar]
- 68. Martens B, Florax R, Dooley F. The effect of entry by supercenter and warehouse club retailers on grocery sales and small supermarkets: a spatial analysis. Paper presented at: American Agricultural Economics Association Annual Meeting; July 24–27, 2005; Providence, RI.
- 69. Blanchard T, Irwin M, Tolbert C, et al. Suburban sprawl, regional diffusion, and the fate of small retailers in a large retail environment, 1977–1996. Sociol Focus. 2003;36:313–331. [Google Scholar]
- 70. Artz GM, Stone KE. Analyzing the impact of Wal-Mart supercenters on local food store sales. Am J Agr Econ. 2006;88:1296–1303. [Google Scholar]
- 71. Blanchard TC, Matthews TL. Retail concentration, food deserts, and food-disadvantaged communities in rural America. In: Hinrichs CC, Lyson TA, eds. Remaking the North American Food System: Strategies for Sustainability. Lincoln, NE: University of Nebraska Press; 2007. [Google Scholar]
- 72. Wiig K, Smith C. The art of grocery shopping on a food stamp budget: factors influencing the food choices of low-income women as they try to make ends meet. Public Health Nutr. 2009;12:1726–1734. [DOI] [PubMed] [Google Scholar]
- 73. Talukdar D. Cost of being poor: retail price and consumer price search differences across inner-city and suburban neighborhoods. J Consumer Res. 2008;35:457–471. [Google Scholar]
- 74. Sharkey JR, Horel S, Han D, et al. Association between neighborhood need and spatial access to food stores and fast food restaurants in neighborhoods of colonias. Int J Health Geogr. 2009;8:8–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Dean WR, Sharkey JR. Rural and urban differences in the associations between characteristics of the community food environment and fruit and vegetable intake. J Nutr Educ Behav. 2011;43:426–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Kaufman PR. Measuring access to nutritious, affordable food: a national assessment. J Food Distrib Res. 2010;41:70–74. [Google Scholar]
- 77. Moore LV, Diez Roux AV. Associations of neighborhood characteristics with the location and type of food stores. Am J Public Health. 2006;96: 325–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. United States Census Bureau. The black population: 2010. https://www.census.gov/prod/cen2010/briefs/c2010br-06.pdf. Published September 2011. Accessed January 1, 2015.
- 79. Broda C, Leibtag E, Weinstein DE. The role of prices in measuring the poor's living standards. J Econ Perspect. 2009;23:77–97.20052301 [Google Scholar]
- 80. United States Department of Agriculture, Economic Research Service. Access to affordable and nutritious food: measuring and understanding food deserts and their consequences. http://www.ers.usda.gov/media/242675/ap036_1_.pdf. Published June 2009. Accessed October 15, 2013.
- 81. Banjo S, Gasparro A. Retailers brace for reduction in food stamps. Wall Street Journal. http://www.wsj.com/article. November 4, 2013. Accessed May 15, 2015. [Google Scholar]
- 82. Goetz SJ, Swaminathan H. Wal-Mart and county-wide poverty. Soc Sci Quart. 2006;87:211–226. [Google Scholar]
- 83. Stiegert KW, Sharkey T. Food pricing, competition, and the emerging supercenter format. Agribusiness. 2007;23:295–312. [Google Scholar]
- 84. Balto DA. Supermarket merger enforcement. J Public Policy Mark. 2001;20:38–50. [Google Scholar]
- 85. Davis DE. Prices, promotions, and supermarket mergers. J Agr Food Ind Organ. 2010;8:1–27. [Google Scholar]
- 86. Ellickson P. The evolution of the supermarket industry: from A&P to Wal-Mart. Bradley Policy Research Center, Working Paper no. FR-11-17. Rochester, NY: University of Rochester, William E. Simon Graduate School of Business Administration; April 1, 2011.
- 87. Basker E, Klimek S, Hoang Van P. Supersize It: The Growth of Retail Chains and the Rise of the “Big-Box” Store. J Econ Manag Strategy. 2012;21:541–582. [Google Scholar]
- 88. Food Marketing Institute. US Grocery Shopper Trends 2012: Executive Summary. Arlington, VA: Food Marketing Institute; 2012. [Google Scholar]
- 89. Wal-Mart, Inc. Our Locations. Corporate Wal-Mart website. http://corporate.walmart.com/our-story/our-business/locations/. Updated 2014. Accessed April 6, 2015.
- 90. Seiders K, Simonides C, Tigert DJ. The impact of supercenters on traditional food retailers in four markets. Int J Retail Distrib Manag. 2000;28:181–193. [Google Scholar]
- 91. The New York Times. A timeline of the Kmart Corporation. http://www.nytimes.com/2002/01/22/business/22KMART-HISTORY.html. New York Times. January 22, 2002. Accessed April 15, 2015.
- 92. Target Corporation. Target through the years. https://corporate.target.com/about/history/Target-through-the-years. Updated January 2015. Accessed January 10, 2015.
- 93. The Carrefour Group. Hypermarkets. http://www.carrefour.com/content/hypermarkets. Updated 2014. Accessed January 10, 2015.
- 94. Arnold SJ. Research note: Wal-Mart in Europe. Int J Retail Distrib Manag. 1999;27:48–51. [Google Scholar]
- 95. Landler M, Barbaro M. Wal-Mart finds that its formula doesn't fit every culture. New York Times. August 2, 2006. [Google Scholar]
- 96. Reardon T, Berdegue JA. The rapid rise of supermarkets in Latin America: challenges and opportunities for development. Dev Policy Rev. 2002;20:371–388. [Google Scholar]
- 97. Reardon T, Timmer CP, Barrett CB, et al. The rise of supermarkets in Africa, Asia, and Latin America. Am J Agric Econ. 2003;85:1140–1146. [Google Scholar]
- 98. Basker E. The causes and consequences of Wal-Mart's growth. J Econ Perspect. 2007;21:177–198. [Google Scholar]
- 99. Reardon T, Chen KZ, Minten B, et al. The quiet revolution in Asia's rice value chains. Ann N Y Acad Sci. 2014;1331:106–118. [DOI] [PubMed] [Google Scholar]
- 100. Vance SS, Scott RV. Wal-Mart: A History of Sam Walton's Retail Phenomenon. New York, NY: Twayne Publishers; 1994. [Google Scholar]
- 101. Moody GR. Information technology and the economic performance of the grocery store industry. Washington, DC: US Department of Commerce, Economics and Statistics Administration, Office of Policy Development; 1997. [Google Scholar]
- 102. Prater E, Frazier GV, Reyes PM. Future impacts of RFID on e-supply chains in grocery retailing. Supply Chain Manag. 2005;10:134–142. [Google Scholar]
- 103. Brinkman de Pee S, Sanogo I, H-J, et al. High food prices and the global financial crisis have reduced access to nutritious food and worsened nutritional status and health. J Nutr. 2010;140:153S–161S. [DOI] [PubMed] [Google Scholar]
- 104. Bernstein AM, Bloom DE, Rosner BA, et al. Relation of food cost to healthfulness of diet among US women. Am J Clin Nutr. 2010;92:1197–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Monsivais P, Drewnowski A. The rising cost of low-energy-density foods. J Am Diet Assoc. 2007;107:2071–2076. [DOI] [PubMed] [Google Scholar]
- 106. Beatty TK, Senauer B. The new normal? U.S. food expenditure patterns and the changing structure of food retailing. Am J Agric Econ. 2013;95:318–324. [Google Scholar]
- 107. Ng SW, Slining MM, Popkin BM. Turning point for US diets? Recessionary effects or behavioral shifts in foods purchased and consumed. Am J Clin Nutr. 2014;99:609–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Jabs J, Devine CM. Time scarcity and food choices: an overview. Appetite. 2006;47:196–204. [DOI] [PubMed] [Google Scholar]
- 109. Roberts ML, Wortzel LHl. New life-style determinants of women's food shopping behavior. J Marketing. 1979;43:28–39. [Google Scholar]
- 110. Bell DR, Ho T-H, Tang CS. Determining where to shop: fixed and variable costs of shopping. J Marketing Res. 1998;35:352–369. [Google Scholar]
- 111. Wal-mart Stores, Inc. History. http://corporate.walmart.com/our-story/history/. Corporate Wal-Mart website. Accessed April 15, 2014.
- 112. Euromonitor International. Grocery Retailers in the US. London: Euromonitor International; 2013. [Google Scholar]
- 113. Basker E. Job creation or destruction? Labor market effects of Wal-Mart expansion. Rev Econ Stat. 2005;87:174–183. [Google Scholar]
- 114. Goetz SJ, Rupasingha A. Wal-Mart and social capital. Am J Agric Econ. 2006;88:1304–1310. [Google Scholar]
- 115. Neumark D, Zhang J, Ciccarella S. The effects of Wal-Mart on local labor markets. J Urban Econ. 2008;63:405–430. [Google Scholar]
- 116. Drewianka S, Johnson D. Wal-Mart and local labor markets, 1990–2004. Working paper. Milwaukee, WI: University of Wisconsin-Milwaukee; 2006.
- 117. The Nielsen Company. Consumer panel & retail measurement. http://www.nielsen.com/us/en/nielsen-solutions/nielsen-measurement/nielsen-retail-measurement.html. Update 2014. Accessed April 15, 2014.
- 118. Kleinbaum DG, Klein M. Modeling strategy for assessing interaction and confounding. In: Logistic Regression. New York, NY: Springer Science+Business; 2010:203–239. [Google Scholar]
- 119. Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56:645–646. [DOI] [PubMed] [Google Scholar]
- 120. Rogers WH. Regression standard errors in clustered samples. Stata Technical Bulletin. 1993;13:19–23. [Google Scholar]
- 121. Srivastava RK. Changing retail scene in India. Int J Retail Distrib Manag. 2008;36:714–721. [Google Scholar]
- 122. Zhang QF, Pan Z. The transformation of urban vegetable retail in China: wet markets, supermarkets and informal markets in Shanghai. J Contemp Asia. 2013;43:497–518. [Google Scholar]
- 123. The Kroger Co. Health matters. https://www.kroger.com/topic/health-matters-3. Kroger website. Updated 2014. Accessed April 15, 2014.
- 124. Gittelsohn J, Song H-J, Suratkar S, et al. An urban food store intervention positively affects food-related psychosocial variables and food behaviors. Health Educ Behav. 2010;37:390–402. [DOI] [PubMed] [Google Scholar]
- 125. Gittelsohn J, Suratkar S, Song H-J, et al. Process evaluation of Baltimore Healthy Stores: a pilot health intervention program with supermarkets and corner stores in Baltimore City. Health Promot Pract. 2010;11:723–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Curran S, Gittelsohn J, Anliker J, et al. Process evaluation of a store-based environmental obesity intervention on two American Indian Reservations. Health Educ Res. 2005;20:719–729. [DOI] [PubMed] [Google Scholar]
- 127. Song H-J, Gittelsohn J, Kim M, et al. A corner store intervention in a low-income urban community is associated with increased availability and sales of some healthy foods. Public Health Nutr. 2009;12:2060–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Gittelsohn J, Dyckman W, Tan ML, et al. Development and implementation of a food store–based intervention to improve diet in the Republic of the Marshall Islands. Health Promot Pract. 2006;7:396–405. [DOI] [PubMed] [Google Scholar]
- 129. Gittelsohn J, Dyckman W, Frick KD, et al. A pilot food store intervention in the Republic of the Marshall Islands. Pac Health Dialog. 2007;14:43–53. [PubMed] [Google Scholar]
- 130. Gittelsohn J, Vijayadeva V, Davison N, et al. A food store intervention trial improves caregiver psychosocial factors and children's dietary intake in Hawaii. Obesity (Silver Spring). 2010;18(suppl 1):S84–S90. [DOI] [PubMed] [Google Scholar]
- 131. Levy AS, Matthews O, Stephenson M, et al. The impact of a nutrition information program on food purchases. J Public Policy Mark. 1985;1–13. [Google Scholar]
- 132. Mhurchu CN, Gorton D. Nutrition labels and claims in New Zealand and Australia: a review of use and understanding. Aust N Z J Public Health. 2007;31:105–112. [DOI] [PubMed] [Google Scholar]
- 133. Rayner M, Boaz A, Higginson C. Consumer use of health-related endorsements on food labels in the United Kingdom and Australia. J Nutr Educ. 2001;33:24–30. [DOI] [PubMed] [Google Scholar]
- 134. Jeffery RW, Pirie PL, Rosenthal BS, et al. Nutrition education in supermarkets: an unsuccessful attempt to influence knowledge and product sales. J Behav Med. 1982;5:189–200. [DOI] [PubMed] [Google Scholar]
- 135. Ernst ND, et al. Nutrition education at the point of purchase: the foods for health project evaluated. Prev Med. 1986;15:60–73. [DOI] [PubMed] [Google Scholar]
- 136. Mayer JA, Dubbert PM, Elder JP. Promoting nutrition at the point of choice: a review. Health Educ Behav. 1989;16:31–43. [DOI] [PubMed] [Google Scholar]
- 137. Steenhuis I, van Assema P, van Breukelen G, et al. The effectiveness of nutrition education and labeling in Dutch supermarkets. Am J Health Promot. 2004;18:221–224. [DOI] [PubMed] [Google Scholar]
- 138. Olson CM, Bisogni CA, Thonney PF. Evaluation of a supermarket nutrition education program. J Nutr Educ. 1982;14:141–145. [Google Scholar]
- 139. Kristal AR, Goldenhar L, Muldoon J, et al. Evaluation of a supermarket intervention to increase consumption of fruits and vegetables. Am J Health Promot. 1997;11:422–425. [DOI] [PubMed] [Google Scholar]
- 140. Hawkes C. Sales promotions and food consumption. Nutr Rev. 2009;67:333–342. [DOI] [PubMed] [Google Scholar]
- 141. Gittelsohn J, Rowan M, Gadhoke P. Interventions in small food stores to change the food environment, improve diet, and reduce risk of chronic disease [published online February 16, 2012]. Prev Chronic Dis. 2012;9:e59. [PMC free article] [PubMed] [Google Scholar]
- 142. Geliebter A, Ang IY, Bernales-Korins M, et al. Supermarket discounts of low-energy density foods: effects on purchasing, food intake, and body weight [published online July 5, 2013]. Obesity (Silver Spring). 2013;17:E42–E48. doi:10.1002/oby.20484. [DOI] [PubMed] [Google Scholar]
- 143. Steenhuis IH, Waterlander WE, de Mul A. Consumer food choices: the role of price and pricing strategies. Public Health Nutr. 2011;14:2220–2226. [DOI] [PubMed] [Google Scholar]
- 144. Walters R, Jamil M. Measuring cross-category specials purchasing: theory, empirical results, and implications. J Mark Focus Manag. 2002;5:25–42. [Google Scholar]
- 145. Bartlett RW. Fluid milk sales as related to demand elasticities. J Dairy Sci. 1964;47:1314–1321. [Google Scholar]
- 146. Huang KS, Lin B-H. Estimation of Food Demand and Nutrient Elasticities from Household Survey Data. Technical Bulletin no. TB-1887. Washington, DC: US Department of Agriculture, Economic Research Service; 2000. [Google Scholar]
- 147. Park JL, Holcomb RB, Raper KC, et al. A demand systems analysis of food commodities by US households segmented by income. Am J Agric Econ. 1996;78:290–300. [Google Scholar]
- 148. Gould BW, Cox TL, Perali F. The demand for fluid milk products in the US: a demand systems approach. Western J Agr Econ. 1990;15:1–12. [Google Scholar]
- 149. Vyth EL, Steenhuis IH, Vlot JA, et al. Actual use of a front-of-pack nutrition logo in the supermarket: consumers’ motives in food choice. Public Health Nutr. 2010;13:1882–1889. [DOI] [PubMed] [Google Scholar]
- 150. Williams P. Consumer understanding and use of health claims for foods. Nutr Rev. 2005;63:256–264. [DOI] [PubMed] [Google Scholar]