Abstract
Introduction:
Ischemia leads to loss of neurons by apoptosis in specific brain regions, especially in the hippocampus. The purpose of this study was investigating the effects of exercise preconditioning on expression of Bax, Bcl-2, and caspase-3 proteins in hippocampal CA1 neurons after induction of cerebral ischemia.
Methods:
Male rats weighing 260–300 g were randomly allocated into three groups (sham, exercise, and ischemia). The rats in exercise group were trained to run on a treadmill 5 days a week for 4 weeks. Ischemia was induced by the occlusion of both common carotid arteries (CCAs) for 20 min. Levels of expression of Bax, Bcl-2, and caspase-3 proteins in CA1 area of hippocampus were determined by immunohistochemical staining .
Results:
The number of active caspase-3-positive neurons in CA1 area were significantly increased in ischemia group, compared to sham-operated group (P<0.001), and exercise preconditioning significantly reduced the ischemia/reperfusion-induced caspase-3 activation, compared to the ischemia group (P<0.05). Also, results indicated a significant increase in Bax/Bcl-2 ratio in ischemia group, compared to sham-operated group (P<0.001).
Discussion:
This study indicated that exercise has a neuroprotective effects against cerebral ischemia when used as preconditioning stimuli.
Keywords: Ischemia, Exercise, Hippocampus, Apoptosis, Bax, Bcl-2, Caspase-3
1. Introduction
Cerebral ischemia causes tissue damage through the interaction of complex patho-physiological processes, including excitotoxicity, inflammation, and apoptosis. Furthermore, reperfusion generates an overproduction of Reactive Oxygen Species (ROS), or better known as free radicals, leading to reperfusion injury (Dirnagl, Iadecola, & Moskowitz, 1999).
Apoptosis resulted from cerebral Ischemia/Reperfusion (I/R) is one of the main causes of cell death (Mattson, Duan, Pedersen, & Culmsee, 2001). As a matter of fact, mitochondria plays an essential role in most cases of apoptosis (Zamzami et al., 1996). In other words, the permeability of the outer mitochondrial membrane increases when it receives an apoptotic signal, resulting in a reduction of the mitochondrial membrane potential followed by the trans-location of the proapoptotic factor (i.e. cytochrome c) from the mitochondrial inter-membrane space to the cytosol. Release of cytochrome c into the cytosol leads to the formation of the apoptosome complex (Li et al., 1997). The apoptosome permits the autoactivation of caspase-9, which is followed by the activation of caspase-3. The activation of caspase-3 induces DNA fragmentation and apoptotic neuronal cell death (Chen et al., 1998). Therefore, inhibition of caspase-3 can significantly reduce ischemia-related cell death.
The Bcl-2 (an antiapoptotic protein) is associated with the mitochondrial outer membrane and can inhibit the release of cytochrome c (Kluck, Bossy-Wetzel, Green, & Newmeyer, 1997). Also, the Bax (a proapoptotic protein) may damage the outer mitochondrial membrane, which can result in the release of cytochrome c. Furthermore, Bax can bind to Bcl-2 and inhibit its antiapoptotic functions (Wattenberg & Lithgow, 2001). It has been reported that dramatic downregulation of Bcl-2 and upregulation of Bax proteins in vulnerable tissues following ischemia occur. The ratio of proapoptotic/antiapoptotic proteins (i.e. Bax/Bcl-2) determines the susceptibility of cells to a death signal (Adams & Cory, 1998).
The hippocampus, which plays an important role in both learning and memory (Erfani, Khaksari, Oryan, Shamsaei, Aboutaleb, Nikbakht, et al., 2015), is more sensitive to ischemic insults than other areas of brain. Damage to the hippocampus causes amnesia and memory loss in long-term period (Albasser, Amin, Lin, Iordanova, & Aggleton, 2012). Based on the results of previous studies, the CA1 pyramidal neurons in hippocampus are particularly vulnerable to ischemic insult; in fact, these neurons die 3–7 days after transient forebrain ischemia (Ouyang, Voloboueva, Xu, & Giffard, 2007). Also, transient global ischemia for 15 min damages the vulnerable cells, particularly in the CA1 area of the hippocampus (Olsson, Wieloch, & Smith, 2003).
The evidence indicates that exercise has a neuroprotective role against ischemic injury (Zhang et al., 2011). However, the protective mechanisms against ischemia (particularly neuronal death in the hippocampus) induced by physical exercise, have still poorly understood. The present work aimed to investigate the effects of exercise preconditioning on apoptosis-related proteins (Bax, Bcl-2, and caspase-3) in rat hippocampal CA1 neurons following transient cerebral ischemia.
2. Methods
2.1. Animals
Twenty-one adult male Wistar rats (weighting 260–300g) were obtained from Tehran Pasteur Institute and housed in standard cages and controlled environment (22–24°C, 45–50% humidity, and 12:12 h light/dark cycle), with free access to food and water. All experiments were performed in accordance with the Helsinki Declaration.
2.2. Experimental groups
Rats were randomly divided into three groups: sham operation group, exercise plus ischemia group (ischemia with 4 weeks of pre-ischemic exercise), and ischemia group (7 rats in each group). In the ischemia group, the animals underwent occlusion of both common carotid arteries. In exercise plus ischemia group, the animals spent 4 weeks of exercise before induction of ischemia. Sham operated animals (served as controls) were subjected to the same surgical procedures except that the common carotid arteries were not occluded.
2.3. Exercise training protocol
The rats in the training intervention group were trained to run on a treadmill (4-lane animal treadmill; IITC Life Science Inc., USA) 5 days a week for 4 weeks. Initially, the rats were acclimatized to run for 10–15 min at 5–7 m/min, 0% slope for 2 days before the formal treadmill training sessions. Initially, electrical shocks (1.0 mA) were needed to force animals to run forward. Subsequently, they ran without electrical stimulation. After adaptive running session, the rats started formal training. The rats in the training groups were scheduled to run on the treadmill during all 4 weeks. The formal treadmill training was started with a speed of 18 m/min for 35 min and 0° slope for 5 days per week in the first week. The duration and intensity of the exercise and treadmill slope were increased progressively, so that the animals were running for 40 min at 18 m/min with 5° slope, 45 min at 18 m/min with 10° slope, and 50 min at 18 m/min with 15° slope, respectively in the second, third, and fourth week of the training. Sedentary animals were placed daily on a stationary treadmill and were given electrical stimulation in a manner identical to that used for the exercise group. In order to monitor any possible stress induced by treadmill running, body weight was monitored every 3 days.
2.4. Induction of transient global cerebral ischemia
To induce transient cerebral ischemia (Erfani, Khaksari, Oryan, Shamsaei, Aboutaleb, & Nikbakht, 2015), rats were anesthetized with ketamine/xylazine (40 mg/kg, IP). Then, their common carotid arteries were exposed and freed from its carotid sheet; their vagus nerves were carefully separated. Both common carotid arteries were occluded for 20 min using Yashargil Aneurism clips. Next, the carotid arteries were released and inspected for immediate reperfusion. Recirculation of blood flow was established by releasing the clips and restoration of blood flow in the carotid arteries was confirmed by observation. Their rectal temperature was maintained at 36.5±0.5°C throughout the surgery using a feedback-regulated heating system. Animals were returned to their home cage after the surgery with free access to food and water and kept separately for 4 days (96 h).
2.5. Tissue preparation
Four days (96 h) after ischemia, the rats were anesthetized and transcardiac perfusion was performed with 0.9% saline, followed by 4% paraformaldehyde in 0.1 M phosphate buffer (pH 7.4) (Aboutaleb et al., 2014). Then, their brains were extracted and postfixed in the same fixative overnight. Next, the brains were embedded in paraffin. Afterward, paraffin-embedded coronal sections were cut (with a cryostat) at 7μm thicknesses for immunohistochemical stains, between 3.3 and 4.2 mm posterior to bregma fortune according to the paxinos atlas (Paxinos & Watson, 2006).
2.6. Immunohistochemical staining
Immunohistochemical staining was performed on 7μm tissue sections (Gheibi et al., 2014; Khaksari, Aboutaleb, Nasirinezhad, Vakili, & Madjd, 2012). Briefly, tissue sections were incubated for 30 min at 60°C, rehydrated through a descending alcohol series, and treated with 10% hydrogen peroxide in methanol for 10 min to reduce endogenous peroxidase activity. After being washed in Tris buffer (H2NC (CH2OH)3, pH7×4), antigens were retrieved by autoclaving for 11 min in citrate buffer (C6H5Na3O7×2H2O, pH6). Sections were then incubated with primary antibodies (Biorbyt, UK) at 4°C temperature overnight. Optimal dilution was found to be 1/100.
Tissues were then incubated in the goat polyclonal secondary antibody (HRP) (Biorbyt, UK) for 30 min at room temperature with the addition of 3, 3′-diaminobenzidine (DAB, Sigma, USA) to achieve visualization of the antigen. In the final step, tissue sections were lightly counterstained with Hematoxylin (Sigma), dehydrated in alcohol, cleared in xylene (Sigma), and mounted for visualization. The primary antibody was not included in the processing of the negative control slide. Human cervical carcinoma tissue was used as a positive control. Photomicrographs of sections were prepared using light microscopy at ×400 magnifications by a blinded investigator. The number of immune positive cells was counted along the transect of 400μm length (0.160 mm2) of CA1 area of the right hippocampus.
2.7. Statistical analysis
All results are reported as a mean±SD. The Kolmogorov-Smirnov test was used to verify the normality of the distribution. One-way analysis of variance (ANOVA) test was used to compare the differences between the groups. When a significant difference was revealed, the Dunnett’s T3 or Scheffe’s post hoc test was used to specify where the difference occurred. When the homogeneity of variance was established, the Scheffe’s post hoc test was used; otherwise, we applied the Dunnett’s T3 post hoc test. The level of significance was set at P≤0.05. All data were analyzed by the SPSS (SPSS for Windows; SPSS Inc., Chicago, IL, USA; Version 16.0).
3. Results
3.1. Exercise preconditioning and reduction of the ischemia/reperfusion-induced caspase-3 activation
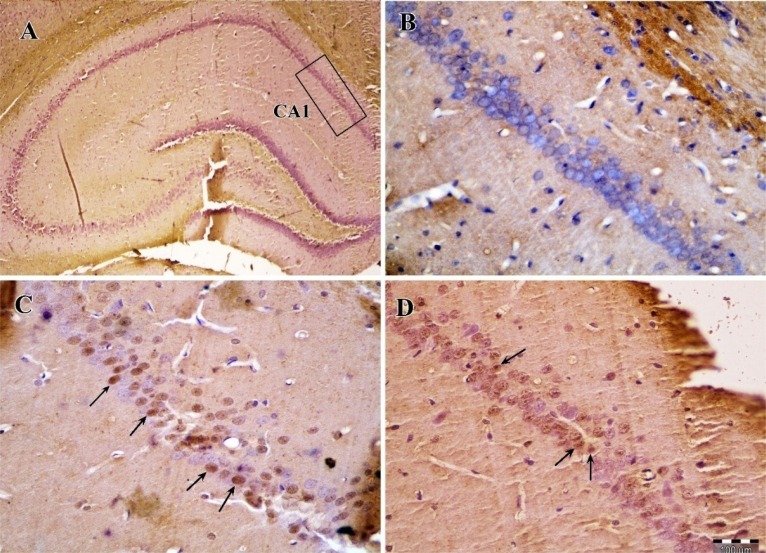
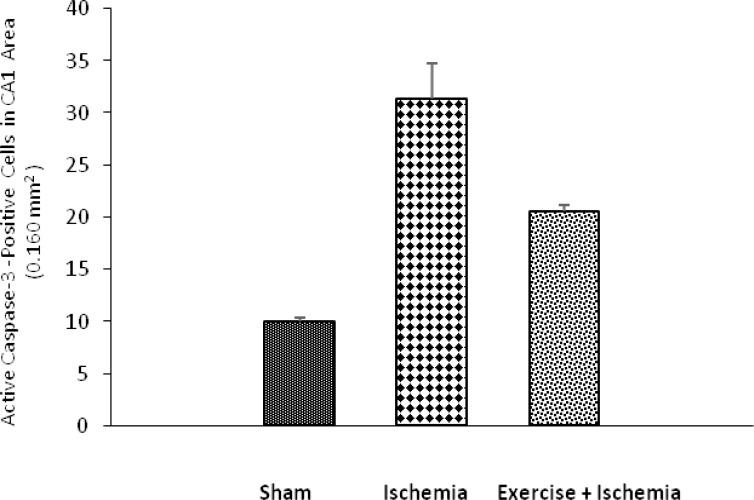
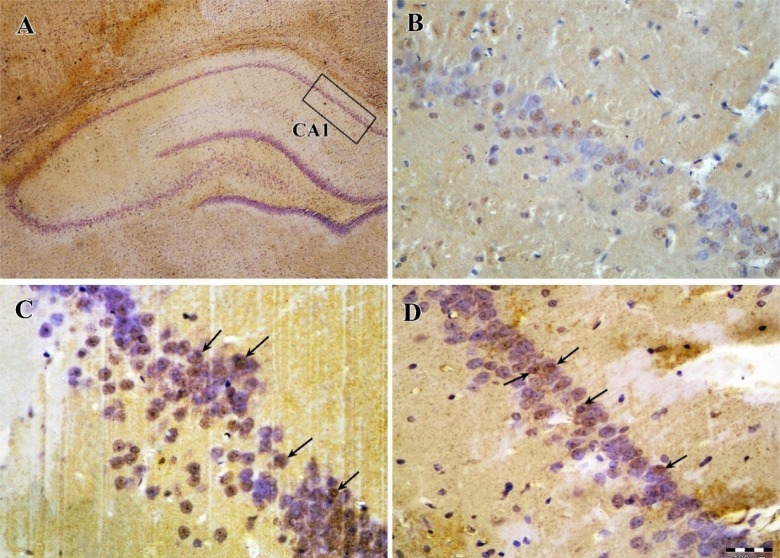
The results of caspase-3 immunohistochemical staining showed that, there is a significant difference among groups with respect to the number of active caspase-3-immunopositive cells in the CA1 area of the rats’ right hippocampus. The number of active caspase-3-positive cells was significantly increased in ischemia group (31.33±8.477, in 0.160mm2) compared to sham-operated group (10±0.816, P<0.001, in 0.160mm2). In ischemic rats preconditioned with exercise, the number of active caspase-3-positive cells in CA1 (20.6±1.342, in 0.160 mm2) was significantly lower than that seen in ischemic rats (P<0.05, in 0.160 mm2), (Figures 1, 2).
Figure 1.
Photomicrographs of caspase-3 immunohistochemical staining in the CA1 area of the right hippocampus after transient global cerebral ischemia. (A) The CA1 area of hippocampus, (B) sham-operated group, (C) ischemia group, (D) exercise plus ischemia group (Arrows indicate the active caspase-3 positive cells, Magnification ×400).
Figure 2.
Effects of exercise preconditioning on the number of active caspase-3 positive cells in the rats’ hippocampal CA1 area after the transient global cerebral ischemia. Exercise preconditioning significantly attenuated the ischemia/reperfusion-induced caspase-3 activation.
*Significantly different compared to sham group (P<0.001).
#Significantly different compared to sham (P<0.05) and ischemia (P<0.05) groups.
3.2. Exercise preconditioning and reduction of the Bax protein levels after ischemia
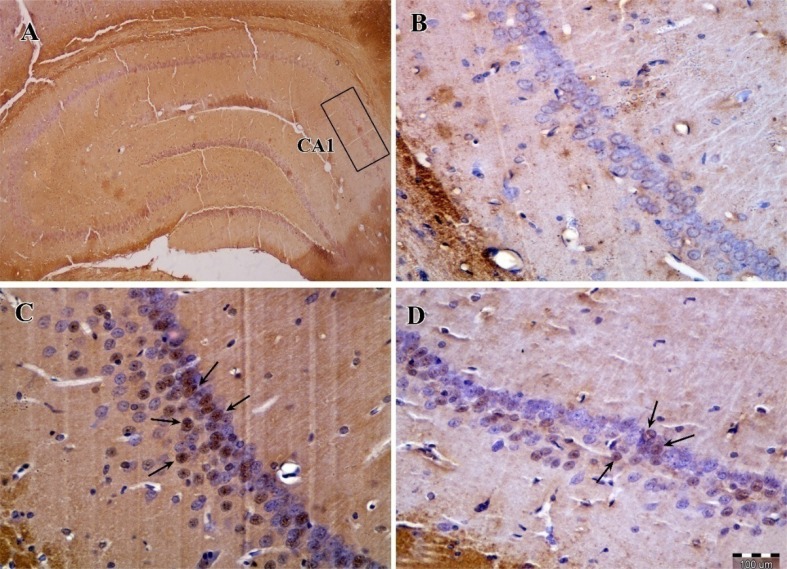
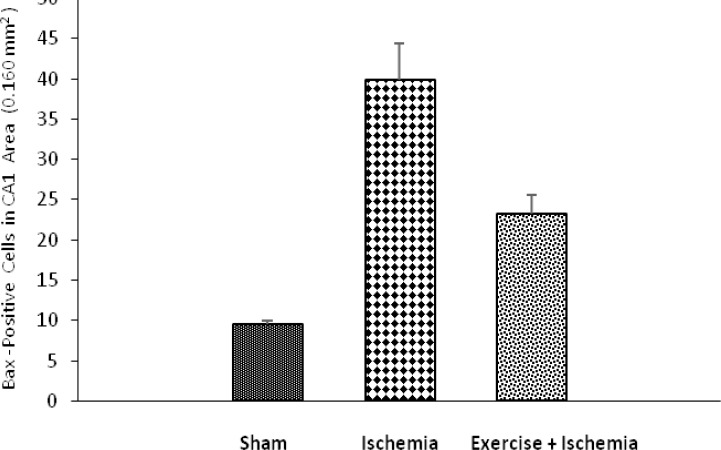
The results of Bax immunohistochemical staining showed that, in the CA1 area of the rats’ right hippocampus, there were statistically significant differences among groups with respect to the number of Bax-positive cells. Bax were weakly expressed in sham-operated group (9.5±0.707, in 0.160 mm2), also, the number of Bax-positive cells increased in ischemia group (39.86±11.852, in 0.160 mm2), (P<0.01). In ischemic rats preconditioned with exercise, the number of Bax-positive cells decreased (23.17±5.707, in 0.160 mm2) compared to the ischemia group (P<0.05), (Figures 3, 4).
Figure 3.
Photomicrographs of Bax immunohistochemical staining in the CA1 area of the right hippocampus after transient global cerebral ischemia. (A) The CA1 area of hippocampus, (B) sham-operated group, (C) ischemia group, (D)exercise plus ischemia group (Arrows indicate the Bax-positive cells, Magnification ×400).
Figure 4.
Effects of exercise preconditioning on the Bax levels in the rats’ hippocampal CA1 area after the transient global cerebral ischemia. Exercise preconditioning significantly attenuated the ischemia/reperfusion-induced increase in Bax levels.
*Significantly different compared to the sham group (P<0.01).
#Significantly different compared to the ischemia group (P<0.05).
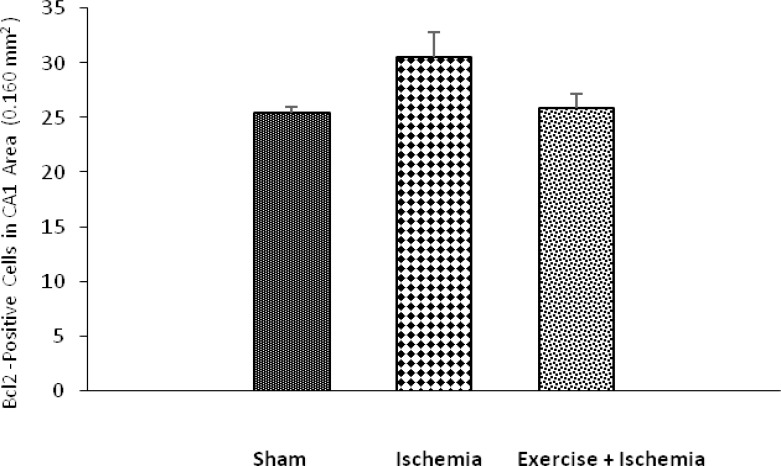
3.3. Effect of exercise preconditioning on Bcl-2 protein levels after ischemia
The results of Bcl-2 immunohistochemical staining showed that, in the CA1 area of the rats’ right hippocampus, there were no significant difference among groups with respect to the number of Bcl-2-positive cells. The levels of Bcl-2 in ischemia group (30.6±4.98, in 0.160 mm2) showed no statistically significant difference compared to sham-operated group (25.5±0.707, in 0.160 mm2), (P>0.05). Also levels of Bcl-2 in exercise group (25.86±3.532, in 0.160 mm2) showed no statistically significant difference compared to ischemia group (P>0.05), (Figures 5, 6).
Figure 5.
Photomicrographs of Bcl-2 immunohistochemical staining in the CA1 area of right hippocampus after transient global cerebral ischemia. (A) The CA1 area of hippocampus, (B) sham-operated group, (C) ischemia group, (D) exercise plus ischemia group (Arrows indicate the Bcl-2-positive cells, Magnification ×400).
Figure 6.
Effects of exercise preconditioning on the Bcl-2 levels in the rats’ hippocampal CA1 area after the transient global cerebral ischemia.
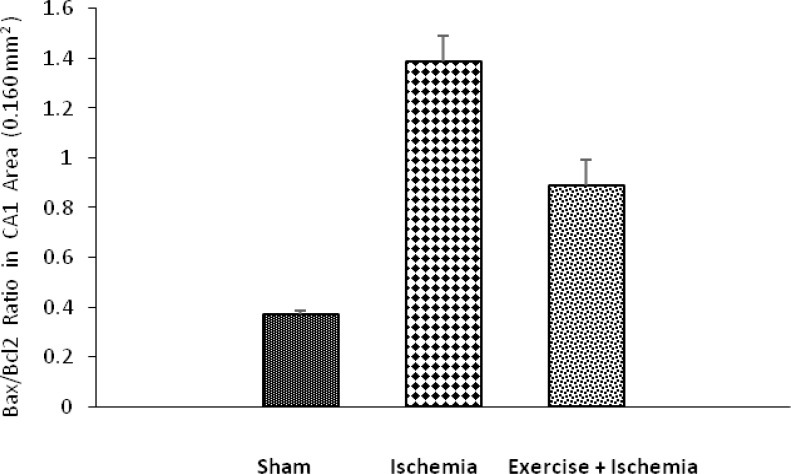
3.4. Exercise preconditioning and modulation of Bax/Bcl-2 Ratio after ischemia
The results of Bax/Bcl-2 ratio showed that, in the CA1 area of the rats’ right hippocampus, there were statistically significant differences among groups. The Bax/Bcl-2 ratio is increased in ischemia group (1.387±0.239, in 0.160 mm2) compared to sham-operated group (0.372±0.016, in 0.160 mm2), (P<0.001). In ischemic rats preconditioned with exercise, the Bax/Bcl-2 ratio decreased (0.889±0.251, in 0.160 mm2) compared to the ischemia group (P<0.05), (Figure 7).
Figure 7.
Effects of exercise preconditioning on the Bax/Bcl-2 ratio in the rat’s hippocampal CA1 neurons after the transient global cerebra l ischemia. Exercise preconditioning significantly modulated the ischemia/reperfusion-induced increase in Bax/Bcl-2 ratio.
*Significantly different compared to sham group (P<0.001).
#Significantly different compared to ischemia group (P<0.05).
4. Discussion
In this study, we studied the effects of exercise preconditioning on apoptosis-related proteins (Bax, Bcl-2, and caspase-3) in hippocampal CA1 neurons after induction of cerebral ischemia. The results of caspase-3 immunohistochemical staining demonstrate that the number of active caspase-3 positive cells in the CA1 area of hippocampus significantly increased following transient global cerebral ischemia. This indicates that ischemia induces apoptotic neuronal cell death in CA1 area. Moreover, the present study showed that exercise preconditioning significantly reduced the ischemia/reperfusion-induced caspase-3 activation. The results of Bax/Bcl-2 ratio demonstrate that ischemic insult enhances Bax/Bcl-2 ratio in the hippocampal CA1 area and exercise preconditioning markedly attenuated the ischemia/reperfusion-induced increase in Bax/Bcl-2 ratio in CA1 (by reducing the levels of Bax, no change in levels of Bcl-2).
Our findings approve the hypothesis that modulation alterations in Bax/Bcl-2 ratio with exercise regulate downstream caspase-driven apoptosis after transient global cerebral ischemia in the hippocampal CA1 area cells. The underlying mechanism by which this action takes place is still poorly known. However, caspase signaling, inflammatory factors, oxidative stress, calcium dysregulation, and excitotoxicity are the main causes of neuronal apoptosis (Moskowitz, Lo, & Iadecola, 2010) . So, any factor that inhibits this process can be used in the treatment of brain ischemia.
Exercise, through the amelioration of risk factors, protects against ischemia/reperfusion-induced brain injury. One of the possible mechanisms for neuroprotective ability of exercise in the CA1 area following transient global ischemia/reperfusion is the capacity to block the NMDA-induced cytotoxicity (Gao et al., 2007). Elevations of NMDA receptor-mediated intracellular calcium ([Ca2+]i), and subsequently high levels of Ca2+ within mitochondria has an essential role in mitochondrial membrane depolarization and modulating its permeability (Gao et al., 2007). This is an important step in the process of caspase activation and apoptosis. Previous studies have shown that cerebral ischemia can lead to the uncontrolled release of glutamate. Jia et al. (2009) in their study showed that treadmill training can protect striatal neurons from ischemic injury. They suggested that this protective effect takes place via preventing NMDA-induced cytotoxicity (Jia et al., 2009).
The other possible mechanism for neuroprotective ability of exercise could be its capacity in blocking free radical formation (Hoffman-Goetz & Spagnuolo, 2007). Reperfusion injury plays an important role in the brain ischemia cascade (White et al., 2000). Returned blood flow can reintroduce oxygen to the cells, causing damages to their proteins, DNA, and plasma membranes. The level of free radicals may increase, if plasma membrane gets damaged. These processes may play an important role in redox signaling and ultimately causing cell apoptosis (Chen et al., 1997). Reactive Oxygen Species (ROS) are produced in the mitochondrial electron transport chain as a normal product, but when their level exceeds cellular antioxidant capacity, they can lead to cell death. ROS-induced oxidative stress plays a crucial role in the ischemic cascade (Chan et al., 2001). It has been shown that Bcl2 protein can enhance antioxidant activity by increasing GSH level and Cu/Zn superoxide dismutase (SOD1) activity (Lee et al., 2001).
Therefore, another possible mechanism for neuroprotective ability of exercise in the CA1 area of the hippocampus following cerebral ischemia can be related to decreasing the Bax/Bcl-2 ratio and its ability to blocking free radical formation. According to previous studies, physical exercise enhances antioxidant activity and increases Cu/Zn superoxide dismutase (SOD1) protein expression in mouse (Hoffman-Goetz & Spagnuolo, 2007).
Extracellular signal-regulated kinases (ERK1/2) are involved in mitogen-activated protein kinase pathways and are constitutively expressed in the adult brain (Sharony et al., 2006). These ERK1/2-regulated pathways are very important in signal transduction and neuroprotection in the setting of ischemia/reperfusion injury. Based on the results of previous studies, activation of this regulatory kinase enables tissue repair in the setting of ischemia/reperfusion injury, which results in the decrease of cell death (Cavanaugh, 2004). Furthermore, exercise preconditioning appears to upregulate ERK1/2, leading to an ischemic neuronal tolerance under hypoxic condition (Jones & Bergeron, 2004).
Heat Shock Protein (HSP)-70 facilitates optimum folding of proteins during normal and stressful conditions, including ischemia, oxidative stress, glucose deprivation, and exposure to toxins (Liebelt et al., 2010). Overexpression of HSP-70 has been previously shown to be neuroprotective in the setting of ischemia/reperfusion (Giffard & Yenari, 2004). Also, HSP-70 and ERK1/2 can decrease the Bax/Bcl-2 ratio (Ohtsuka & Suzuki, 2000). A recent study demonstrated that preischemic treadmill training by upregulation of HSP-70 can reduce brain infarction volume (Liebelt et al., 2010).
Tumor Necrosis Factor (TNF)-α is a major deleterious proinflammatory cytokine found throughout the systemic circulation, which is upregulated following stroke and traumatic brain injury. Despite its inflammatory and injurious effects, evidence shows that TNF-α is a beneficial factor in tissue repair and neuroprotection. Furthermore, this cytokine may serve to induce endogenous neuroprotection following chronic exercise preconditioning (Guo et al., 2008). Dinh et al. (2008) showed that TNF-α toxicity may be mediated through upregulation of Bax and TNFR1 expression as well as an increase in the Bax/Bcl-2 ratio (Dinh et al., 2008). It is believed that exercise training produces a chronic low rating increase in TNF-α concentration, ultimately generating neuronal tolerance and protection in the setting of ischemia/reperfusion injury. Mechanisms underlying this complex picture of TNF-α have not been completely discovered, but it might involve the expression of TNF-α receptors. Previous studies have shown that the chronic exercise-induced levels of TNF-α serve to reduce the expression of TNF-α receptor after ischemia/reperfusion (Reyes Jr et al., 2006).
In conclusion, our study demonstrated that pre-ischemic exercise reduces neuronal injuries of hippocampal CA1 neurons after cerebral ischemia through reduction of Bax/Bcl-2 ratio and caspase-3 activation. Exercise exerts those protective effects in ischemic brain models via some possible mechanisms, which include preventing NMDA receptor cytotoxicity, reducing ROS production, and upregulation of ERK1/2 and HSP-70. These neuroprotective mechanisms of exercise can provide a therapy that will both promote cell survival and decrease neuronal death, therefore ameliorating much of the functional and memory loss caused by brain ischemic injury.
Acknowledgments
This research was supported by a grant sponsored by the Iran National Science Foundation (INSF). The authors are very grateful to INSF for their financial support.
Footnotes
Conflict of Interest
Nahid Aboutaleb, Nabi Shamsaei, Hamid Rajabi, Sohaila Erfani, Mehdi Khaksari, Farnaz Nikbakht, Pezhman Motamedi, and Ali Shahbazi declare that they have no conflict of interest.
References
- Aboutaleb N., Kalalian-Moghaddam H., Eftekhari S., Shahbazi A., Abbaspour H., Khaksari M. (2014). Apelin-13 inhibits apoptosis of cortical neurons following brain ischemic reperfusion injury in a transient model of focal cerebral ischemia. International Journal of Peptide Research and Therapeutics, 20(2), 127–132. [Google Scholar]
- Adams J. M., Cory S. (1998). The Bcl-2 protein family: arbiters of cell survival. Science, 281(5381), 1322–1326. [DOI] [PubMed] [Google Scholar]
- Albasser M. M., Amin E., Lin T. C. E., Iordanova M. D., Aggleton J. P. (2012). Evidence that the rat hippocampus has contrasting roles in object recognition memory and object recency memory. Behavioral Neuroscience, 126(5), 659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh J. E. (2004). Role of extracellular signal regulated kinase 5 in neuronal survival. European Journal of Biochemistry, 271(11), 2056–2059. [DOI] [PubMed] [Google Scholar]
- Chen J., Nagayama T., Jin K., Stetler R. A., Zhu R. L., Graham S. H., et al. (1998). Induction of caspase-3-like protease may mediate delayed neuronal death in the hippocampus after transient cerebral ischemia. The Journal of Neuroscience, 18(13), 4914–4928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinh C., Haake S., Chen S., Hoang K., Nong E., Eshraghi A., et al. (2008). Dexamethasone protects organ of corti explants against tumor necrosis factor-alpha–induced loss of auditory hair cells and alters the expression levels of apoptosis-related genes. Neuroscience, 157(2), 405–413. [DOI] [PubMed] [Google Scholar]
- Dirnagl U., Iadecola C., Moskowitz M. A. (1999). Pathobiology of ischaemic stroke: an integrated view. Trends in Neurosciences, 22(9), 391–397. [DOI] [PubMed] [Google Scholar]
- Erfani S., Khaksari M., Oryan S., Shamsaei N., Aboutaleb N., Nikbakht F. (2015). Nampt/PBEF/Visfatin Exerts Neuroprotective Effects Against Ischemia/Reperfusion Injury via Modulation of Bax/Bcl-2 Ratio and Prevention of Caspase-3 Activation. Journal of Molecular Neuroscience, 56(1), 1–7. [DOI] [PubMed] [Google Scholar]
- Erfani S., Khaksari M., Oryan S., Shamsaei N., Aboutaleb N., Nikbakht F., et al. (2015). Visfatin reduces hippocampal CA1 cells death and improves learning and memory deficits after transient global ischemia/reperfusion. Neuropeptides, 49, 63– 8. [DOI] [PubMed] [Google Scholar]
- Gao X., Xu X., Pang J., Zhang C., Ding J., Peng X., et al. (2007). NMDA receptor activation induces mitochondrial dysfunction, oxidative stress and apoptosis in cultured neonatal rat cardiomyocytes. Physiological Research, 56(5), 559. [DOI] [PubMed] [Google Scholar]
- Gheibi S., Aboutaleb N., Khaksari M., Kalalian-Moghaddam H., Vakili A., Asadi Y., et al. (2014). Hydrogen sulfide protects the brain against ischemic reperfusion injury in a transient model of focal cerebral ischemia. Journal of Molecular Neuroscience, 54(2), 1–7. [DOI] [PubMed] [Google Scholar]
- Giffard R. G., Yenari M. A. (2004). Many mechanisms for hsp70 protection from cerebral ischemia. Journal of Neurosurgical Anesthesiology, 16(1), 53–61. [DOI] [PubMed] [Google Scholar]
- Guo M., Lin V., Davis W., Huang T., Carranza A., Sprague S., et al. (2008). Preischemic induction of TNF-α by physical exercise reduces blood–brain barrier dysfunction in stroke. Journal of Cerebral Blood Flow & Metabolism, 28(8), 1422–1430. [DOI] [PubMed] [Google Scholar]
- Hoffman-Goetz L., Spagnuolo P. (2007). Effect of repeated exercise stress on caspase 3, Bcl-2, HSP 70 and CuZn-SOD protein expression in mouse intestinal lymphocytes. Journal of Neuroimmunology, 187(1), 94–101. [DOI] [PubMed] [Google Scholar]
- Jia J., Hu Y. S., Wu Y., Liu G., Yu H. X., Zheng Q. P., et al. (2009). Pre-ischemic treadmill training affects glutamate and gamma aminobutyric acid levels in the striatal dialysate of a rat model of cerebral ischemia. Life Sciences, 84(15), 505–511. [DOI] [PubMed] [Google Scholar]
- Jones N. M., Bergeron M. (2004). Hypoxia-induced ischemic tolerance in neonatal rat brain involves enhanced ERK1/2 signaling. Journal of Neurochemistry, 89(1), 157–167. [DOI] [PubMed] [Google Scholar]
- Khaksari M., Aboutaleb N., Nasirinezhad F., Vakili A., Madjd Z. (2012). Apelin-13 protects the brain against ischemic reperfusion injury and cerebral edema in a transient model of focal cerebral ischemia. Journal of Molecular Neuroscience, 48(1), 201–208. [DOI] [PubMed] [Google Scholar]
- Kluck R. M., Bossy-Wetzel E., Green D. R., Newmeyer D. D. (1997). The release of cytochrome c from mitochondria: a primary site for Bcl-2 regulation of apoptosis. Science, 275(5303), 1132–1136. [DOI] [PubMed] [Google Scholar]
- Lee M., Hyun D. H., Marshall K. A., Ellerby L. M., Bredesen D. E., Jenner P., et al. (2001). Effect of overexpression of BCL-2 on cellular oxidative damage, nitric oxide production, antioxidant defences, and the proteasome. Free Radical Biology and Medicine, 31(12), 1550–1559. [DOI] [PubMed] [Google Scholar]
- Li P., Nijhawan D., Budihardjo I., Srinivasula S. M., Ahmad M., Alnemri E. S., et al. (1997). Cytochrome c and dATP-dependent formation of Apaf-1/caspase-9 complex initiates an apoptotic protease cascade. Cell, 91(4), 479–489. [DOI] [PubMed] [Google Scholar]
- Liebelt B., Papapetrou P., Ali A., Guo M., Ji X., Peng C., et al. (2010). Exercise preconditioning reduces neuronal apoptosis in stroke by up-regulating heat shock protein-70 (heat shock protein-72) and extracellular-signal-regulated-kinase 1/2. Neuroscience, 166(4), 1091–1100. [DOI] [PubMed] [Google Scholar]
- Mattson M., Duan W., Pedersen W., Culmsee C. (2001). Neurodegenerative disorders and ischemic brain diseases. Apoptosis, 6(1–2), 69–81. [DOI] [PubMed] [Google Scholar]
- Moskowitz M. A., Lo E. H., Iadecola C. (2010). The science of stroke: mechanisms in search of treatments. Neuron, 67(2), 181–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohtsuka K., Suzuki T. (2000). Roles of molecular chaperones in the nervous system. Brain Research Bulletin, 53(2), 141–146. [DOI] [PubMed] [Google Scholar]
- Olsson T., Wieloch T., Smith M. L. (2003). Brain damage in a mouse model of global cerebral ischemia: effect of NMDA receptor blockade. Brain Research, 982(2), 260–269. [DOI] [PubMed] [Google Scholar]
- Ouyang Y. B., Voloboueva L. A., Xu L. J., Giffard R. G. (2007). Selective dysfunction of hippocampal CA1 astrocytes contributes to delayed neuronal damage after transient forebrain ischemia. The Journal of Neuroscience, 27(16), 4253–4260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paxinos G., Watson C. (2006). The rat brain in stereotaxic coordinates, Sixth Edition: hard cover edition. 6th edition U.S., Elsvier: Academic press. [Google Scholar]
- Reyes R., Jr, Wu Y., Lai Q., Mrizek M., Berger J., Jimenez D. F., et al. (2006). Early inflammatory response in rat brain after peripheral thermal injury. Neuroscience Letters, 407(1), 11–15. [DOI] [PubMed] [Google Scholar]
- Sharony R., Pintucci G., Saunders P. C., Grossi E. A., Baumann F. G., Galloway A. C., et al. (2006). Matrix metalloproteinase expression in vein grafts: role of inflammatory mediators and extracellular signal-regulated kinases-1 and-2. American Journal of Physiology-Heart and Circulatory Physiology, 290(4), H1651–H1659. [DOI] [PubMed] [Google Scholar]
- Wattenberg B., Lithgow T. (2001). Targeting of C-terminal (tail)-anchored proteins: understanding how cytoplasmic activities are anchored to intracellular membranes. Traffic, 2(1), 66–71. [DOI] [PubMed] [Google Scholar]
- White B. C., Sullivan J. M., DeGracia D. J., O’Neil B. J., Neumar R. W., Grossman L. I., et al. (2000). Brain ischemia and reperfusion: molecular mechanisms of neuronal injury. Journal of the neurological sciences, 179, 1–33 [DOI] [PubMed] [Google Scholar]
- Zamzami N., Susin S. A., Marchetti P., Hirsch T., Gómez-Monterrey I., Castedo M., et al. (1996). Mitochondrial control of nuclear apoptosis. The Journal of Experimental Medicine, 183(4), 1533–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang P., Zhang Q., Pu H., Wu Y., Bai Y., Vosler P., et al. (2011). Very early-initiated physical rehabilitation protects against ischemic brain injury. Frontiers in Bioscience (Elite Edition), 4, 2476– 2489 . [DOI] [PubMed] [Google Scholar]