Abstract
Objective:
The objective of this study was to describe the medication errors in hospitalized patients, comparing those in neonates with medication errors across the age spectrum.
Method:
In tier 1, PubMed, Embase and Google Scholar were searched, using selected MeSH terms relating to hospitalized paediatric, adult and elderly populations. Tier 2 involved a search of the same electronic databases for literature relating to hospitalized neonatal patients.
Results:
A total of 58 articles were reviewed. Medication errors were well documented in each patient group. Overall, prescribing and administration errors were most commonly identified across each population, and mostly related to errors in dosing. Errors due to patient misidentification and overdosing were particularly prevalent in neonates, with 47% of administration errors involving at least tenfold overdoses. Unique errors were identified in elderly patients, comprising duplication of therapy and unnecessary prescribing of medicines. Overall, the medicines most frequently identified with error across each patient group included: heparin, antibiotics, insulin, morphine and parenteral nutrition. While neonatal patients experience the same types of medication errors as other hospitalized patients, the medication-use process within this group is more complex and has greater consequences resulting from error. Suggested strategies to help overcome medication error most commonly involved the integration of a clinical pharmacist into the treating team.
Conclusion:
This review highlights that each step of the medication-use process is prone to error across the age spectrum. Further research is required to develop targeted strategies relevant to specific patient groups that integrate key pharmacy services into wards.
Keywords: medication error, medication safety, neonates, NICU
Introduction
Medication errors are common in hospitalized patients and are a high priority in healthcare systems worldwide [Fortescue et al. 2003; Wiedenmayer et al. 2006; Roughead et al. 2013]. Defined as any mistakes that occur during the medication-use process, medication errors can arise in the course of prescribing, dispensing, transcribing, administering and monitoring medicines [European Medicines Agency, 2015]. Often, these errors are preventable and result in increased patient morbidity and mortality as well as increased healthcare costs and unnecessary hospitalization [European Medicines Agency, 2015]. While the problem of medication errors has been widely reported in published literature, of particular concern are those that occur in neonatal medicine [Kaushal et al. 2001; Fortescue et al. 2003; Stavroudis et al. 2010]. The neonatal population is particularly vulnerable to further risk of harm resulting from medication errors due to their physiological inability to buffer errors [Kaushal et al. 2001]. Medication errors with potential to cause harm are eight times more likely to occur in the neonatal intensive care unit (NICU) compared with adult wards [Kaushal et al. 2001; Stavroudis et al. 2010]. Furthermore, it is reported that medication errors comprise 84.2% of all medical errors within the NICU [Stavroudis et al. 2010].
There are few studies that compare medication errors across different patient populations, particularly with respect to the neonatal patient group. Each hospitalized patient population has different pharmacotherapeutic needs, and it is important to establish whether there are different medication errors in each group. As such, this lack of information limits the ability of healthcare systems to develop targeted strategies to decrease the incidence of error.
The purpose of this review is to determine a medication error profile that characterizes the types of medication errors that are experienced by different hospitalized patient populations across the age spectrum. The review explores whether there are any medication errors unique to the neonatal population, and establishes whether there are differences in error type between populations. Furthermore, the review identifies the medicines that are most commonly associated with error in each patient group.
Methods
A comprehensive search of the literature was performed using the following electronic databases: Medline, Embase, Google Scholar. Relevant literature, including reviews, original studies and other articles pertaining to medication safety issues and medication errors, were extracted.
Search strategy
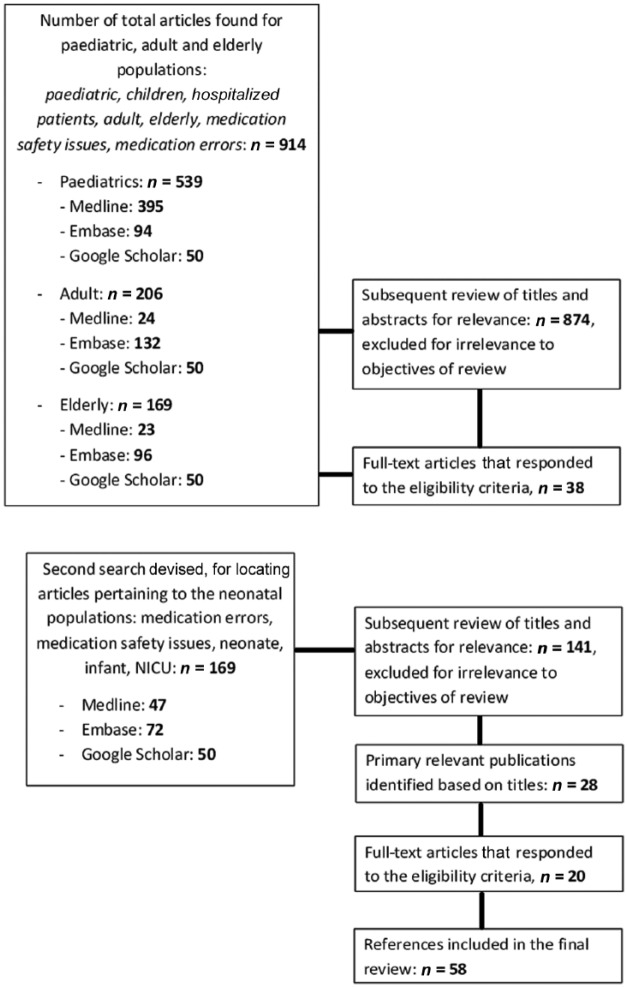
A two-tiered search strategy was used (Figure 1). In tier 1, a generalized search was performed to find literature relevant to the paediatric, adult and elderly patient populations using the MeSH terms paediatric, children, hospitalized patients, adult, elderly, medication safety and medication errors. Subsequent to finding the bulk of the literature, tier 2 of the search was dedicated to finding articles specific to the neonatal population utilising the following MeSH terms: medication errors, medication safety, neonate, infant and NICU. Inclusion criteria for the searches restricted the content to the following: types or nature of medication errors, hospitalized patients, and written in the English language. All full-text articles were retrieved and all evaluations pertaining to the types of medication errors in the NICU were included in the review. Manual bibliographic searches of all relevant articles were also performed in order to identify any articles that were not found in the electronic searches.
Figure 1.
Search Strategy.
Structure of review
The patient populations have been classified into four broad age headings: neonates (0–28 days of age), children or paediatrics (1–18 years), adults and the elderly. Neonatal data were gathered from articles that specifically studied the NICU, or had the NICU as part of their study group. The review included paediatric studies that assessed medication errors on paediatric intensive care units (PICUs), emergency and general paediatric wards. The literature reporting on the adult population comprised studies conducted in intensive care units (ICUs), surgical and medical wards and emergency departments. Articles on the elderly patient group reported on errors in geriatric wards and acute-care wards.
Medication errors have been identified and reported within each phase of the medication-use process, including prescription, transcription, dispensing, administration and monitoring [Bates et al. 1995; Kaushal et al. 2001; Pallas et al. 2008; Stavroudis et al. 2010]. Definitions of the types of medication error associated with each phase are presented in Table 1.
Table 1.
Definitions and contributing factors for medication error across the medication-use process.
| Definitions of the different types of medication errors | |
|---|---|
| Prescribing | All errors that occur during the decision process and in prescribing/ordering a medication for a patient. Includes: dose errors, wrong drug, wrong regimen and inappropriate drug. |
| Transcription | All errors associated with the transfer of verbal or written information from an order sheet or prescription to patient, medication chart or medical records. Includes: discrepancies in drug name, formulation, route, dose, dosing regimen and omission. |
| Dispensing | All errors that occur during the interpretation of medication prescriptions by the pharmacy staff and the subsequent selection, preparation, labelling and distribution of medication. |
| Administration | All errors that occur whilst a medication is being administered to a patient. Includes: omission, wrong drug, wrong dose, wrong time and wrong route. |
| Monitoring | All errors associated with the monitoring of clinical and/or laboratory data that assess the patient’s response to the administered drug therapy i.e. through therapeutic drug-monitoring practices. Includes: error in interpreting results, wrong dose suggestions, omission of suggestions and wrong drug suggestions to reverse condition. |
| Contributing factors for medication error in each patient group | |
| Neonate | Higher number of medications, lack of physician experience, high-intensity physician workloads, length of stay, low birth weights, gestational ages, similar-sounding or identical names and surnames, multiple-birth babies (i.e. twins), inability to communicate, more vascular lines, long hospitalizations and dispensing medications 2 hours after being ordered. |
| Paediatric | Seriously ill patients, inexperienced physicians, human error, equipment dysfunction and communication failures. |
| Adult | Polymedication prescriptions, physicians’ lack of pharmacology knowledge, stressful and high-paced work environment, staff performance deficits, failure to consider patient information, memory lapses and dose-checking processes. |
| Elderly | Taking five or more medications, prescribed nine or more medications, hospitalizations 13 days or longer, incidence of more than one chronic disease and multiple pathologies. |
Results
Electronic and manual searches identified a total of 58 full-text articles, from a range of countries. Most of the literature came from the USA (20 of 58), with others from Spain, Iran, Finland, Australia, UK, Italy, Turkey, Argentina, Brazil, Denmark, Switzerland, New Zealand, Morocco, India and Canada.
Overall, medication errors were well documented in each patient group, however, comparative studies between patient populations were not widely identified.
Neonatal population
Among the 20 articles reviewed, the majority used a prospective chart review method to collect data and just over half of the studies were conducted in the USA (10 of 18) [Raju et al. 1989; Vincer et al. 1989; Kaushal et al. 2001; Carroll et al. 2003; Chappell and Newman, 2004; Cordero et al. 2004; Gray and Goldmann, 2004; Gray et al. 2006; Simpson et al. 2004; Suresh et al. 2004; Kunac and Reith, 2005; Van Den Anker, 2005; Ligi et al. 2008; Pallas et al. 2008; Campino et al. 2009; Jain et al. 2009; Stavroudis et al. 2010; Antonucci and Porcella, 2012; Dabliz and Levine, 2012; Sorrentino and Alegiani, 2012]. A summary of the errors reported are presented in Table 2. The prescribing phase was associated with the highest incidence of medication errors, comprising 14–74% of total error reports [Kaushal et al. 2001; Cordero et al. 2004; Gray and Goldmann, 2004; Simpson et al. 2004; Suresh et al. 2004; Pallas et al. 2008; Campino et al. 2009; Jain et al. 2009; Stavroudis et al. 2010; Antonucci and Porcella, 2012; Sorrentino and Alegiani, 2012]. The most frequently reported error within this phase involved incorrect dosing, with 42% of errors relating to overdoses or underdoses [Jain et al. 2009]. Ten articles reported that dosing errors occurred because of miscalculation of doses and incorrect placement of decimal points or units of measurement [Kaushal et al. 2001; Cordero et al. 2004; Simpson et al. 2004; Van Den Anker, 2005; Pallas et al. 2008; Campino et al. 2009; Jain et al. 2009; Stavroudis et al. 2010; Antonucci and Porcella, 2012; Dabliz and Levine, 2012]. One Indian-based study reported that as a result of a dosing error, an infant received a tenfold increase in the delivery of morphine [Jain et al. 2009]. The consequences of such significant dosing inaccuracies involved long-term injury, including developmental problems, toxic effects requiring active intervention, as well as death [Folli et al. 1987; Raju et al. 1989; Vincer et al. 1989; Frey et al. 2000, 2002; Ross et al. 2000; Kaushal et al. 2001; Simpson et al. 2004; Suresh et al. 2004]. Errors in prescribing were attributed to lack of physician experience, high-intensity physician workloads as well as the lack of neonate-specific drug protocols or policies on the ward [Gray and Goldmann, 2004; Jain et al. 2009]. This is an important issue within the NICU, as the majority of literature highlights that due to the lack of evidence-based information, physicians do not have a reliable source of information to refer to, leading to the prescribing of off-label and unlicensed medicines and subsequent erroneous prescribing decisions [Kaushal et al. 2001; Suresh et al. 2004; Kunac and Reith, 2005; Van Den Anker, 2005; Campino et al. 2009; Stavroudis et al. 2010; Antonucci and Porcella, 2012; Dabliz and Levine, 2012; Sorrentino and Alegiani, 2012]. Other common prescribing errors reported only within the neonatal population included: incorrect use of units (i.e. grams instead of milligrams) and wrong administration route [Kaushal et al. 2001; Cordero et al. 2004; Gray and Goldmann, 2004; Simpson et al. 2004; Van Den Anker, 2005; Pallas et al. 2008; Campino et al. 2009; Jain et al. 2009; Antonucci and Porcella, 2012; Dabliz and Levine, 2012].
Table 2.
Medication errors specific to neonatal patients.
| Neonates | |
|---|---|
| Prescribing | Wrong route Wrong use of units i.e. milligrams instead of grams Lack of neonate-specific drug protocols or information |
| Transcription | Wrong weight Wrong dosage regimen Wrong units |
| Dispensing | Providing the correct drug in the wrong packaging Incorrect calculations or doses Late dispensing of medications Incorrect dilutions in manufacture of drugs |
| Administration | Patient misidentification Additional dose of drug Wrong dilution Parents administering unauthorized nutrients |
| Monitoring | Nil specific compared with other populations |
Transcription-based medication errors (range 12–18.4% of total errors) were related to mistakes in the transfer of patient information to patient medication charts [Kaushal et al. 2001; Carroll et al. 2003; Suresh et al. 2004; Stavroudis et al. 2010; Sorrentino and Alegiani, 2012]. Two types of transcribing errors were identified: omissions and commissions (recording incorrect patient information), comprising 18.6% and 18.2% of errors, respectively [Carroll et al. 2003]. Specifically in the NICU, these types of errors included: the use of the incorrect units, omission or incorrect recording of patient characteristics (i.e. weights, allergies), and omission of recording administered dose [Kaushal et al. 2001; Carroll et al. 2003; Suresh et al. 2004; Stavroudis et al. 2010; Sorrentino and Alegiani, 2012. Carroll and colleagues identified that these types of documentation errors were more likely to occur in those neonatal patients with higher numbers of medicines, vascular lines and longer hospitalizations [Carroll et al. 2003].
Dispensing errors comprised 11.9–25% of total errors and were most frequently associated with mistakes in labelling and dilution of formulations [Gray and Goldmann, 2004; Suresh et al. 2004; Van Den Anker, 2005; Jain et al. 2009; Stavroudis et al. 2010; Antonucci and Porcella, 2012; Sorrentino and Alegiani, 2012]. Seven articles identified errors in this phase, which also included: late dispensing, providing the correct drug in the wrong packaging and incorrect calculations or doses [Gray and Goldmann, 2004; Suresh et al. 2004; Van Den Anker, 2005; Stavroudis et al. 2010; Sorrentino and Alegiani, 2012]. Van den Anker, in particular, emphasized the importance of timely dispensing of medicines, and associated a delayed dispensing time of more than two hours with an increased risk of medication errors occurring [Van Den Anker, 2005].
Seven studies reported on administration errors in neonates and the prevalence had a range of 31–63% of total error reports [Raju et al. 1989; Vincer et al. 1989; Chappell and Newman, 2004; Suresh et al. 2004; Ligi et al. 2008; Stavroudis et al. 2010; Sorrentino and Alegiani, 2012]. Almost two thirds (60.3%) of administration errors were caused by nurses, with the most common errors associated with incorrect administration time [Raju et al. 1989; Kaushal et al. 2001; Gray and Goldmann, 2004; Suresh et al. 2004; Kunac and Reith, 2005; Ligi et al. 2008; Stavroudis et al. 2010; Antonucci and Porcella, 2012; Sorrentino and Alegiani, 2012]. One USA-based observational study also reported that parents of NICU patients contributed to the incidence of medication errors by administering unauthorized medicines and incorrectly preparing nutrients for feeding [Suresh et al. 2004]. Other neonatal-specific administration errors included: incorrect preparation or dilution of medication and administering an extra dose of medication [Raju et al. 1989; Kaushal et al. 2001; Gray and Goldmann, 2004; Suresh et al. 2004; Kunac and Reith, 2005; Ligi et al. 2008; Stavroudis et al. 2010; Antonucci and Porcella, 2012; Sorrentino and Alegiani, 2012]. These errors were most commonly associated with the following risk factors: length of stay, low birth-weights and early gestational ages [Ligi et al. 2008]. A significant issue for the NICU related to the level of product manipulation required to improve the compatibility of medicines to the unique characteristics of neonatal patients. This was emphasized by Chappell and Newman who stated that 31% of intravenous medicines were prescribed for neonatal patients at doses less than one tenth of a vial, resulting in a significantly high susceptibility for the incidence of tenfold or 100-fold dosing errors upon administration [Chappell and Newman, 2004; Ligi et al. 2008; Jain et al. 2009]. Similarly, Ligi and colleagues reported that 47% of administration errors in the NICU were tenfold dosing errors [Ligi et al. 2008]. Medicines most commonly associated with dosing inaccuracies were identified as intravenous (IV) formulations of: frusemide, benzylpenicillin, diamorphine, gentamicin and insulin [Chappell and Newman, 2004]. The resulting harm was reported as ranging from minor harm, requiring increased monitoring and specific treatment, to serious harm and death [Suresh et al. 2004].
Several studies also emphasized the incidence of patient misidentification errors during the administration phase [Vincer et al. 1989; Gray and Goldmann, 2004; Suresh et al. 2004; Van Den Anker, 2005; Stavroudis et al. 2010; Antonucci and Porcella, 2012; Dabliz and Levine, 2012; Sorrentino and Alegiani, 2012]. Dabliz and Levine estimated that 25% of medication errors within the NICU were attributed to administering medication to the wrong patient [Dabliz and Levine, 2012]. The most common causes of misidentification were similar-sounding or identical names and surnames, difficulties in distinguishing multiple-birth babies (i.e. twins and triplets) and inability to communicate with patients [Gray et al. 2006]. Furthermore, it was reported that identification bands on wrists and ankles were often removed in order to place IV lines or to take blood samples, and were forgotten to be replaced leading to increased risk for misidentification [Antonucci and Porcella, 2012; Dabliz and Levine, 2012].
Errors pertaining to the monitoring phase were uncommon, comprising only 1.4% of all errors [Suresh et al. 2004]. These types of errors often involved the incorrect interpretation of laboratory results, omission of therapeutic drug monitoring and missing the symptoms of adverse events [Kaushal et al. 2001; Suresh et al. 2004].
Paediatric
Among the 17 articles reviewed, prescription errors were the most commonly reported type of medication error [Folli et al. 1987; Aneja et al. 1992; Wilson et al. 1998; Kozer et al. 2002; Fortescue et al. 2003; Taylor et al. 2005; Condren et al. 2010; Al-Jeraisy et al. 2011]. Accounting for 10–74% of total error reports, these types of errors were most commonly identified via retrospective and prospective reviews of patient charts and medication incident reports [Folli et al. 1987; Aneja et al. 1992; Wilson et al. 1998; Frey et al. 2000, 2002; Ross et al. 2000; Kozer et al. 2002; Fortescue et al. 2003; Taylor et al. 2005; Otero et al. 2008; Condren et al. 2010; Wong et al. 2009; Ghaleb et al. 2010; Al-Jeraisy et al. 2011; Belela et al. 2011; Ozkan et al. 2011; Manias et al. 2014]. Overall, dosing errors were the most common type reported, making up 82.6% of prescribing errors [Folli et al. 1987; Aneja et al. 1992; Wilson et al. 1998; Kozer et al. 2002; Fortescue et al. 2003; Wong et al. 2009; Al-Jeraisy et al. 2011]. Significant overdoses by as much as ten-times over the normal dosage range were identified, with Ross and colleagues attributing a third of these errors to dose miscalculations by clinicians [Ross et al. 2000; Fortescue et al. 2003]. The consequences of these errors were reported as involving elevated serum levels of medicines, leading to moderate-level and life-threatening toxicities [Wilson et al. 1998; Kozer et al. 2002]. These symptoms subsequently led to increased patient monitoring, length of stay, hospital costs and in-hospital deaths [Kozer et al. 2002]. Paediatric prescribing errors were more frequent in seriously ill patients, and were most likely to be caused by trainee doctors [Kozer et al. 2002; Al-Jeraisy et al. 2011]. Condren and colleagues identified that prescribing errors, including dosing mistakes and incomplete medication orders, were present in 9.7% of new prescriptions in a paediatric acute-care clinic [Condren et al. 2010].
Transcription errors were not commonly reported within paediatric studies, with only three articles acknowledging their incidence [Frey et al. 2000, 2002; Fortescue et al. 2003]. These types of errors made up 5.8% of all medication errors, and included: punctuation mistakes (i.e. writing ‘3’ instead of ‘0.3’), omission of medication, wrong unit of measurement (i.e. g instead of mg) and incorrect doses [Frey et al. 2000, 2002; Fortescue et al. 2003].
Errors within the dispensing phase were not considered to be significant sources of error, accounting for only 2.7–7.0% of errors in paediatric patients. Four studies identified that labelling mistakes were the most common sources or error as well as the dispensing of incorrect quantities of medication and supplying incorrect medications [Wilson et al. 1998; Ross et al. 2000; Frey et al. 2002; Belela et al. 2011].
Medication errors occurred frequently within the administration phase, comprising 12.8–73% of total reported errors [Frey et al. 2002; Ghaleb et al. 2010; Belela et al. 2011; Ozkan et al. 2011]. The administration of incorrect doses was the most commonly reported error, and specifically related to tenfold overdoses [Wilson et al. 1998; Frey et al. 2000, 2002; Ross et al. 2000; Kozer et al. 2002; Fortescue et al. 2003; Otero et al. 2008; Wong et al. 2009; Ghaleb et al. 2010; Belela et al. 2011; Ozkan et al. 2011]. A Canadian retrospective cohort study reported that children were at a greater risk of being administered tenfold overdoses than adults because the volume of a dose that was ten-times the normal range for paediatric patients would still look like a relatively small volume of stock solution [Kozer et al. 2002]. Wong and colleagues stated that an overdose of potent medications in children (e.g. sedatives), may cause respiratory depression and have a critical effect on neurological outcomes [Wong et al. 2009]. Medicines most commonly associated with tenfold dosing errors included: digoxin, morphine, gentamicin and indomethacin [Kozer et al. 2002]. Two articles also identified errors in incorrectly administering pharmacotherapy to the wrong patient, who had no therapeutic need for the medication [Wong et al. 2009; Manias et al. 2014]. Contributing factors to the incidence of administration errors were identified as including human error, equipment dysfunction and communication failures [Frey et al. 2000].
None of the studies based in paediatric wards identified monitoring errors as a part of the medication error profile.
Adult
Among the 11 articles reviewed, the most common study designs were prospective observational studies [Bates et al. 1995; Calabrese et al. 2001; Barker et al. 2002; Van Den Bemt et al. 2002; Winterstein et al. 2004; Lisby et al. 2005; Kopp et al. 2006; Bohomol et al. 2009; Jennane et al. 2011; Zeraatchi et al. 2013; Saghafi and Zargarzadeh, 2014]. Bates and colleagues estimated that 6.5 of 100 adult admissions experienced a medication error and that at least 28% were preventable [Bates et al. 1995]. Most errors occurred within the prescribing phase, making up 56–72.5% of total reported medication errors [Bates et al. 1995; Winterstein et al. 2004]. Examples of these errors included: the prescribing of 100 vials of tramadol instead of 100mg and ranitidine erroneously prescribed via nasogastric tube instead of intravenously [Bohomol et al. 2009]. Overall, incorrect dosing was the most commonly reported prescribing error [Bates et al. 1995; Winterstein et al. 2004; Lisby et al. 2005; Kopp et al. 2006; Bohomol et al. 2009; Jennane et al. 2011; Zeraatchi et al. 2013; Saghafi and Zargarzadeh, 2014]. Bohomol and colleagues, Winterstein and colleagues and Kopp and colleagues emphasized that prescribing errors were mostly caused by physicians’ lack of detailed pharmacology knowledge and failure to comprehensively consider patient information [Winterstein et al. 2004; Kopp et al. 2006; Bohomol et al. 2009]. Furthermore, a quantitative study that analysed patient prescriptions and incident reports in a Brazilian ICU highlighted that patients with polymedication prescriptions admitted to the stressful and fast-paced environment of the ICU were more prone to experiencing prescribing errors [Bohomol et al. 2009]. The consequences of medication error were reported as including uncontrolled pain and infection due to underdosing, renal failure and elevated serum levels, resulting in increased monitoring and additional treatment [Winterstein et al. 2004; Bohomol et al. 2009].
Transcription errors were well documented within the adult population, particularly within the Danish and Moroccan studies, and the percentage of reported errors had a range of 6–60% of all total medication errors [Bates et al. 1995; Winterstein et al. 2004; Lisby et al. 2005; Kopp et al. 2006; Bohomol et al. 2009; Jennane et al. 2011; Zeraatchi et al. 2013; Saghafi and Zargarzadeh, 2014]. The most commonly reported error related to errors in transferring information into patient charts [Bates et al. 1995; Lisby et al. 2005; Kopp et al. 2006; Jennane et al. 2011; Zeraatchi et al. 2013]. Nursing staff were responsible for 40% of transcription errors, due to erroneous interpretations of prescriptions by nurses [Lisby et al. 2005; Zeraatchi et al. 2013].
Overall, the dispensing phase was not a major source of medication errors, comprising 2.2–34% of all errors [Lisby et al. 2005; Kopp et al. 2006; Saghafi and Zargarzadeh, 2014]. The most frequently reported error was associated with mistakes in the preparation of doses for patients [Bates et al. 1995; Lisby et al. 2005; Kopp et al. 2006].
The administration phase comprised 14.6–41% of all medication errors in adult wards [Calabrese et al. 2001; Barker et al. 2002; Van Den Bemt et al. 2002; Kopp et al. 2006; Zeraatchi et al. 2013; Saghafi and Zargarzadeh, 2014]. A US-based, prospective, observational study set in adult medical and surgical ICUs identified that one medication error occurred for every five doses of medication administered [Kopp et al. 2006]. The most frequently reported errors involved the administration of medications at the wrong time and omission of administering doses, accounting for 43% and 30% of administration errors, respectively [Calabrese et al. 2001; Barker et al. 2002; Van Den Bemt et al. 2002; Lisby et al. 2005; Kopp et al. 2006; Bohomol et al. 2009]. The consequences of late or omitted administration of critical medicines such as anti-infectives and anticoagulants were reported as leading to suboptimal management of infection, blood pressure and blood clotting, threatening the success of treatment [Bohomol et al. 2009]. The overdosing of medications was also emphasized as a serious error within adult critical care wards, with Winterstein and colleagues documenting nephrotoxic effects as a result of overdosing antibiotics [Winterstein et al. 2004]. Nurses were responsible for generating 40% of administration errors and contributing factors included staff performance deficits, memory lapses and faulty dose-checking processes [Winterstein et al. 2004; Kopp et al. 2006; Zeraatchi et al. 2013].
Errors in the monitoring phase were uncommon, identified in only two studies [Bohomol et al. 2009; Jennane et al. 2011]. These errors were described as the failure to assess patient responses to prescribed medications, including laboratory results and clinical markers within therapeutic drug-monitoring practices [Bohomol et al. 2009; Jennane et al. 2011].
Elderly
Among the 10 articles reviewed, medication errors were most commonly identified through prospective observational studies, and retrospective review of charts and incident reports [Briggs, 2006; Picone et al. 2008; Ben-Yehuda et al. 2011; Henri et al. 2012; Maher and Hajjar, 2012; Zakharov et al. 2012; Buck et al. 2013; García-Aparicio and Herrero-Herrero, 2013; Ernawati et al. 2014; Metsälä and Vaherkoski, 2014]. The median age of elderly participants ranged from 68 to 84 years of age [Picone et al. 2008; Ben-Yehuda et al. 2011; Buck et al. 2013; García-Aparicio and Herrero-Herrero, 2013; Ernawati et al. 2014]. Medication errors in the prescribing phase had a range of 1.6–46% of the total reported errors [Picone et al. 2008; Ben-Yehuda et al. 2011; Ernawati et al. 2014]. Incorrect dosing was most commonly reported, comprising 49% of prescribing errors [Briggs, 2006; Picone et al. 2008; Ben-Yehuda et al. 2011; Maher and Hajjar, 2012; Buck et al. 2013; García-Aparicio and Herrero-Herrero, 2013; Ernawati et al. 2014; Metsälä and Vaherkoski, 2014]. A unique error commonly reported in the elderly population involved the prescribing of inappropriate medications [Briggs, 2006; Picone et al. 2008; Ben-Yehuda et al. 2011; Maher and Hajjar, 2012; Buck et al. 2013; García-Aparicio and Herrero-Herrero, 2013; Ernawati et al. 2014; Metsälä and Vaherkoski, 2014]. Described as the ordering of medications that are unnecessary, ineffective or unsafe, these errors most often occur in elderly patients who present with multiple pathologies, requiring multiple medications [Maher and Hajjar, 2012]. The consequences of these errors were reported as involving serious adverse drug events and prolonging hospitalizations [Maher and Hajjar, 2012]. Furthermore, Ernawati and colleagues found that physicians often only partially complete patient medication histories, leading to the prescribing of duplicate therapies because of the inadequate gathering of patient information [Ernawati et al. 2014].
Transcribing errors were well documented in elderly patients, and were discussed by four articles. The percentage range of total errors was 15–54%, and the most commonly reported error related to discrepancies in doses between prescriptions and patient charts [Picone et al. 2008; Ben-Yehuda et al. 2011; Maher and Hajjar, 2012; Ernawati et al. 2014]. A cohort study set in a 37-bed ward in Israel and involving 137 patients detected that the number of medications being taken was related to a higher risk of transcribing errors [Ben-Yehuda et al. 2011]. Specifically, patients prescribed nine or more medications and whose hospitalizations were 13 days or longer were at a higher risk [Ben-Yehuda et al. 2011]. The medications most commonly associated with this type of error included: simvastatin, valsartan and paracetamol [Ernawati et al. 2014]. Ernawati and colleagues commented that there was a need for accuracy during the transcribing process in order to prevent subsequent administration errors [Ernawati et al. 2014].
Dispensing errors were not considered main sources of error within the elderly population. These errors made up 2–14% of medication errors, with the most common error involving the incorrect labelling and instructions on dispensed medications [Briggs, 2006; Picone et al. 2008; Maher and Hajjar, 2012. Maher and Hajjar stated that erroneous instructions most often related to labelling medications ‘PRN’ (as required) instead of ‘once a day’ [Maher and Hajjar, 2012; Zakharov et al. 2012].
Overall, it was found that administration errors are the most common type in hospitalized elderly patients, comprising 54.2–59% of all medication errors [Briggs, 2006; Picone et al. 2008; Henri et al. 2012; Ernawati et al. 2014; Metsälä and Vaherkoski, 2014]. Older patients, suffering from more than one chronic disease and taking five or more medications were identified as being at a greater risk of experiencing these errors [Picone et al. 2008; Henri et al. 2012]. The most frequently reported administration errors were omission of administering prescribed medication and incorrect administration times [Briggs, 2006; Picone et al. 2008; Henri et al. 2012; Maher and Hajjar, 2012; Ernawati et al. 2014; Metsälä and Vaherkoski, 2014]. Zakharov and colleagues identified that nurses were responsible for 43% of administration errors [Zakharov et al. 2012]. The clinical impact of these errors on patients ranged from minor discomfort to significant morbidity and mortality [Picone et al. 2008; Henri et al. 2012]. Ernawati and colleagues conducted a 20-week prospective study in a 13-bed geriatric ward and reported that 10.3% of medication errors had a potentially significant impact, with a further 2.4% being potentially serious [Ernawati et al. 2014]. The drug classes most commonly involved in administration errors included: aminoglycosides, anticoagulants, opioid analgesics and antihypertensives [Ernawati et al. 2014].
Monitoring errors were only identified in one article by Maher and Hajjar, who reported that they were associated with inappropriate clinical monitoring practices [Maher and Hajjar, 2012]. Specifically, this error was identified as the failure to identify risk of medication toxicity in patients, which could have been prevented, reversed or reduced by earlier dose adjustments [Maher and Hajjar, 2012].
Comparison of medication commonly associated with error
This review sought to compare the medications most commonly associated with error to the A-PINCH High Risk Medicines List. Compiled by the Australian Clinical Excellence Commission, the list groups together medications that are universally considered to be high risk and are represented by the acronym A-PINCH [Clinical Excellence Commission, 2015]. Each of the medication categories listed on A-PINCH were commonly implicated in errors across each of the reviewed patient populations, including antibiotics (particularly gentamicin), heparin, insulin, potassium chloride, fentanyl, morphine, anti-arrhythmics and parenteral nutrition (Table 3).
Table 3.
Types of medications most commonly associated with error.
A-PINCH, compiled by the Australian Clinical Excellence Commission, the list groups together medications that are universally considered to be high-risk and are represented by the acronym A-PINCH: A, anti-infectives; P, potassium and other electrolytes; I, insulin; N, narcotics and other sedatives; C, chemotherapeutic agents; H, heparin and other anticoagulants [Clinical Excellence Commission, 2015].
GI, gastrointestinal; IV, intravenous; NSAIDs, nonsteroidal anti-inflammatory drugs.
Overall, the neonatal population reported issues with a broader range of agents, as well as medications that were not seen in other populations, including prostaglandins, ketamine, immunizations, milk and vecuronium. As neonatal patients are administered the majority of medications through the IV or intramuscular (IM) routes, any errors that occur will have a systemic effect. As such, tenfold errors have been reported more commonly with IV formulations and agents including: insulin, midazolam, frusemide, benzylpenicillin, gentamicin and ranitidine [Chappell and Newman, 2004]. The literature did not report any errors with antineoplastic medications or with corticosteroids, which were all commonly reported in the other three patient groups. Furthermore, it is reported that NICU patients have a high exposure to medications, and are prescribed an average of 8.6 drugs per infant, increasing the risk for experiencing adverse drug events [Daniell and Darlow, 1989; Sorrentino and Alegiani, 2012].
The elderly and adult populations experience errors within the same groups of medications, particularly cardiovascular and GI medications. Errors are associated with a wider selection of agents in these drug classes in comparison with paediatric and neonatal patients. The elderly population experienced errors with allopurinol and statins that are medications most often used in older patients.
Paediatric patients experienced the most errors with antibiotics. Due to the large age range of the population (extending from 1 to 18 years of age), some medications were also the same as those reported in the adult population including adrenaline, anticonvulsants and steroids.
Discussion
The main focus of this article was to highlight the types of medication-related safety issues that occur in hospitalized patients, in particular those within the neonatal population. To our knowledge, this is the only review to compare the types of medication errors that occur within four distinct population groups.
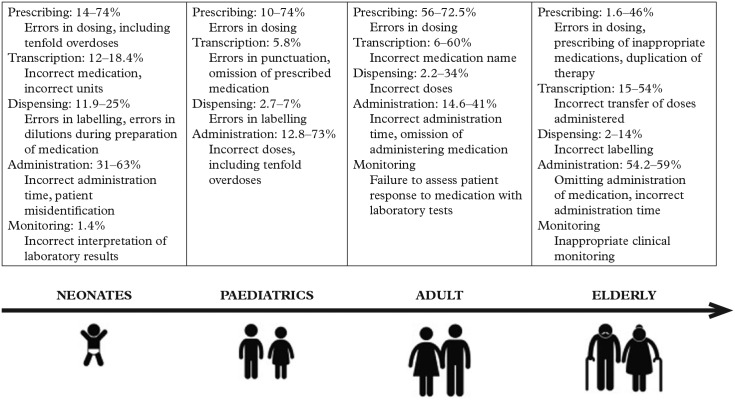
This review demonstrates that each phase of the medication-use process is susceptible to medication error, across the patient age spectrum (Figure 2). Most literature has identified errors within the prescribing and administration phases. In particular, errors relating to incorrect dosing, incorrect medications and incorrect administration time were the most frequently reported. The ranges of reported error varied greatly, which can be attributed to differences in research methods, although most studies used the chart-review method, which is more effective in detecting prescribing errors. In addition, medication error was not explicitly defined in some studies, particularly within the neonatal and paediatric studies. This may be attributed to the fact that a large proportion of medications used in young patients are prescribed off-label. As such, it is difficult to define prescribing dosing errors if doses have been adapted and extrapolated from adult guidelines.
Figure 2.
Most commonly identified medication errors across the age spectrum.
The findings suggest that there are medication errors seen in certain types of patient population more than in others. In particular, within the neonatal population errors pertaining to patient misidentification, delayed dispensing, parental involvement in administering unauthorized medications, erroneous product dilutions, as well as tenfold and 100-fold overdoses, were emphasized. Overdoses to this extent were not reported in the adult or elderly populations. The main contributing factors were identified as physician inexperience, as well as the lack of neonate-specific dosing protocols and evidence-based information on the efficacy, safety, dosing, pharmacokinetics and clinical use of medication in neonates, leading to the common use of off-label or unlicensed medications [Antonucci and Porcella, 2012]. The findings highlight that the prescribing and administration phases were most commonly associated with medication errors. Overall, the use of medication in neonates is more complex than in other patient groups [Raju et al. 2011; National Association of Neonatal Nurses, 2014]. NICU healthcare professionals are faced with limited amounts of evidence-based information supporting the use of pharmacotherapeutic interventions in neonates, as well as a narrow range of neonatal-specific formulations [Chedoe et al. 2007]. Furthermore, neonates are a nonhomogenous group, with differences in maturation of medication-sensitive organs (kidneys, GI tract and liver), weights and gestational ages, requiring individualized weight-based dosing [Gray and Goldmann, 2004; Jain et al. 2009]. (Table 4). The physiological vulnerabilities limit neonates’ ‘buffering zone’ capacity to compensate for error, leaving a narrow margin of safety [Raju et al. 2011; Antonucci and Porcella, 2012]. The resulting impact of these errors is greater than in older children or adult populations. Neonates are at the very start of the developmental age spectrum, and even minor errors can lead to short-term as well as long-term consequences affecting development [Raju et al. 2011]. As the risk of sustaining a medication error has been reported as being eight-times higher within the neonatal group than within any other population, targeted interventions to improve safety and decrease error rates should be prioritized to the neonatal population as the patients of highest risk [Kaushal et al. 2001; Stavroudis et al. 2010].
Table 4.
Factors that increase therapeutic risk in neonatal patients.
|
|
|
|
|
|
|
|
|
|
Unique errors were also reported within the elderly population. Characteristics of vulnerability including polypharmacy, multimorbidities and decreased organ function were reported as important factors that increased risk of experiencing medication errors [García-Aparicio and Herrero-Herrero, 2013]. Errors pertaining to the prescribing of unnecessary medications and duplication of pharmacotherapies were almost exclusively reported within this group. Most commonly attributed to physicians, these errors were attributed to poor gathering of patient information and the failure to complete full patient medication histories upon admission. The impact of these errors most commonly related to medication toxicities as well as significant adverse effects. However, the consequences of harm are not as great compared with patients at the start of their lifespan.
An important finding of this study is that the medications most commonly associated with error in each of the patient groups were those listed within the A-PINCH. As such, medication safety interventions should focus upon these medications. When considering the neonatal population, the range of medications that are prescribed for use in the NICU are relatively limited in comparison with those used in older paediatric and adult populations [Gray and Goldmann, 2004]. However, despite this, the findings show that errors occur with a broader range of agents in the neonatal population than other hospitalized patients, indicating that the use of medications in the NICU is greater.
As medication errors can occur at any stage of the medication-use process and can be caused by a range of healthcare professionals, the strategies to improve safety must be multifactorial. Several studies recommend the use of computerized physician-order entry and the use of a single-medication therapy sheet to improve both prescribing and transcription errors [Kaushal et al. 2001; Kozer et al. 2002; Fortescue et al. 2003; Gray and Goldmann, 2004; Winterstein et al. 2004; Kunac and Reith, 2005; Lisby et al. 2005; Van Den Anker, 2005; Briggs, 2006; Campino et al. 2009; Condren et al. 2010; Wong et al. 2009; Ghaleb et al. 2010; Antonucci and Porcella, 2012; Dabliz and Levine, 2012; Maher and Hajjar, 2012; Sorrentino and Alegiani, 2012; Ernawati et al. 2014]. In addition, the formulation of population-specific quality control tools and health indicators has also been regarded as important in improving medication error rates [Bohomol et al. 2009]. However, the most commonly cited strategy identified in half of the literature across all patient groups, is the involvement of a clinical pharmacist on wards [Folli et al. 1987; Bates et al. 1995; Wilson et al. 1998; Kaushal et al. 2001; Kozer et al. 2002; Van Den Bemt et al. 2002; Fortescue et al. 2003; Gray and Goldmann, 2004; Simpson et al. 2004; Kunac and Reith, 2005; Lisby et al. 2005; Briggs, 2006; Bohomol et al. 2009; Campino et al. 2009; Condren et al. 2010; Wong et al. 2009; Ghaleb et al. 2010; Ben-Yehuda et al. 2011; Jennane et al. 2011; Antonucci and Porcella, 2012; Dabliz and Levine, 2012; Henri et al. 2012; Maher and Hajjar, 2012; Sorrentino and Alegiani, 2012; García-Aparicio and Herrero-Herrero, 2013; Ernawati et al. 2014; Metsälä and Vaherkoski, 2014]. Fortescue and colleagues report that 81% of medication errors in paediatric patients could be avoided with pharmacist monitoring [Fortescue et al. 2003]. High-intensity wards using high-risk medications, such as ICUs, may benefit the most from a ward-based clinical pharmacist [Fortescue et al. 2003]. In the NICU in particular, the integration of the pharmacist into the treating team leads to medication-use improvement [Campino et al. 2009]. Simpson and colleagues reported that following a daily cot-side review of patients, pharmacists significantly reduced monthly medication errors from 24.1 per 1000 neonatal activity days to 5.1 (p < 0.001) [Simpson et al. 2004]. Clinical pharmacy activities, such as patient medication chart reviews, medication reconciliation, as well as participating in medical ward rounds with physicians and nurses are effective in reducing errors [Fortescue et al. 2003; Simpson et al. 2004; Kunac and Reith, 2005; Briggs, 2006; Ben-Yehuda et al. 2011; Jennane et al. 2011; Dabliz and Levine, 2012; Sorrentino and Alegiani, 2012; Ernawati et al. 2014]. Furthermore, the provision of medication-specific education to the treating team can improve the quality of the healthcare delivered and promotes interdisciplinary collaboration [Kunac and Reith, 2005; Dabliz and Levine, 2012]. In adult wards, Leape and colleagues identified that pharmacist participation on ward rounds reduced the rate of preventable adverse drug events due to prescribing errors by 66% [Leape et al. 1999]. These activities allow for real-time feedback and education, leading to better prescribing decisions and greater interception of errors before they are realized [Fortescue et al. 2003; Simpson et al. 2004]. Clinical pharmacists possess specialized knowledge that is essential in preventing harm to patients as well as in minimizing hospital-associated costs from extended hospital stays and additional therapy [Folli et al. 1987].
Limitations
Differences in study methods, definitions of medication errors and definitions in error categories make direct comparison between studies difficult, particularly within the prescribing and administration phases. For example, in some studies, errors that were identified prior to the administration of medication were not included in the results and as such only actual administration errors were reported. However, most studies utilized a chart review or medication-order review method of medication-error detection, which are ultimately better at detecting prescription-based errors.
Some studies mixed population groups, for example, paediatric studies often included data from a NICU, however, did not always disclose the proportions of errors occurring in each ward. Therefore, results between the two subgroups may be hard to differentiate. There were less data available on elderly patients as most studies concentrated on medication errors that occurred outside of the hospital setting, that is, in nursing homes.
It is also possible that a large number of studies could have been excluded because they were not available in the English language.
Conclusion
Each stage of the medication-use process is prone to medication error across the age spectrum. The administration and prescribing phases were the most commonly identified phases of error and most often related to incorrect dosing, wrong prescribing or administering of drugs and wrong time of administration. While neonatal patients experience the same types of medication errors as other hospitalized patients, the medication-use process within this group is more complex and has greater consequences in the instance of error. Maintaining safe pharmacotherapeutic practices should be a major priority for all health professionals however clinical pharmacists have the potential to significantly reduce medication errors. Further research is required to develop targeted strategies relevant to specific patient groups that integrate key pharmacy services into wards, as well as quality-control tools and health indicators to prevent medication errors. Additional investigation is needed to determine the need of pharmacy services on the NICU and their impact on patient safety and care.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Contributor Information
Natalia Krzyzaniak, University of Technology, Sydney, Graduate School of Health (Pharmacy), PO Box 123, Broadway, NSW 2007, Australia.
Beata Bajorek, University of Technology, Sydney, Graduate School of Health (Pharmacy), Broadway, Sydney, NSW, Australia.
References
- National Association of Neonatal Nurses (2014) Medication Safety in the Neonatal Intensive Care Unit. Chicago, IL: National Association of Neonatal Nurses. [Google Scholar]
- Ahmed M. (2008) Working as a neonatal pharmacist. Available at: http://www.pharmaceutical-journal.com/career/career-feature/working-as-a-neonatal-pharmacist/10004380.article
- Al-Jeraisy M., Alanazi M., Abolfotouh M. (2011) Medication prescribing errors in a pediatric inpatient tertiary care setting in Saudi Arabia. BMC Res Notes 4: 294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aneja S., Bajaj G., Mehandiratta S. (1992) Errors in medication in a pediatric ward. Indian Pediatrics 29: 727–730. [PubMed] [Google Scholar]
- Antonucci R., Porcella A. (2012) Current pharmacotherapy in the newborn. Res Rep Neonatol 2: 85–94. [Google Scholar]
- Barker K., Flynn E., Pepper G., Bates D., Mikeal R. (2002) Medication errors observed in 36 health care facilities. Arch Internal Med 162:1897–1903. [DOI] [PubMed] [Google Scholar]
- Bates D., Cullen D., Laird N., Petersen L., Small S., Servi D., et al. (1995) Incidence of adverse drug events and potential adverse drug events: implications for prevention. JAMA 274: 29–34. [PubMed] [Google Scholar]
- Belela A., Peterlini M., Pedreira M. (2011) Medication Errors reported in a pediatric intensive care unit for oncologic patients. Cancer Nursing 34: 393–400. [DOI] [PubMed] [Google Scholar]
- Ben-Yehuda A., Bitton Y., Sharon P., Rotfeld E., Armon T., Muszkat M. (2011) Risk factors for prescribing and transcribing medication errors among elderly patients during acute hospitalization. Drugs Aging 28: 491–500. [DOI] [PubMed] [Google Scholar]
- Berlin C., Jr (2013) Pharmacokinetics in children. Available at: https://www.msdmanuals.com/en-gb/professional/pediatrics/principles-of-drug-treatment-in-children/pharmacokinetics-in-children
- Bohomol E., Ramos L., D’Innocenzo M. (2009) Medication errors in an intensive care unit. J Adv Nursing 65: 1259–1267. [DOI] [PubMed] [Google Scholar]
- Briggs J. (2006) Strategies to reduce medication errors with reference to older adults. Nursing Standard 20: 53–57. [DOI] [PubMed] [Google Scholar]
- Buck T., Gronkjaer L., Duckert M., Rosholm J., Aagaard L. (2013) Medication reconciliation and prescribing reviews by pharmacy technicians in a geriatric ward. J Res Pharm Practice 2: 145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrese A., Erstad B., Brandl K., Barletta J., Kane S., Sherman D. (2001) Medication administration errors in adult patients in the ICU. Intensive Care Med 27: 1592–1598. [DOI] [PubMed] [Google Scholar]
- Campino A., Lopez-Herrera M., Lopez-De-Heredia I., Valls-I-Soler A. (2009) Educational strategy to reduce medication errors in a neonatal intensive care unit. Acta Paediatrica 98: 782–785. [DOI] [PubMed] [Google Scholar]
- Carroll A., Tarczy-Hornoch P., O’Reilly E., Christakis D. (2003) Resident documentation discrepancies in a neonatal intensive care unit. Pediatrics 111: 976–980. [DOI] [PubMed] [Google Scholar]
- Carvalho C., Ribeiro M., Bonilha M., Fernandes M., Jr., Procianoy R., Silveira R. (2012) Use of off-label and unlicensed drugs in the neonatal intensive care unit and its association with severity scores. J Pediatria 88: 465–470. [DOI] [PubMed] [Google Scholar]
- Chappell K., Newman C. (2004) Potential tenfold drug overdoses on a neonatal unit. Arch Dis Childhood Fetal Neonatal Ed 89: F483–F484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chedoe I., Molendijk H., Dittrich S., Jansman F., Harting J., Brouwers J., et al. (2007) Incidence and nature of medication errors in neonatal intensive care with strategies to improve safety. Drug Safety 30: 503–513. [DOI] [PubMed] [Google Scholar]
- Clinical Excellence Commission (2015) High Risk Medicines. Available at: http://www.cec.health.nsw.gov.au/programs/high-risk-medicines#P2.
- Condren M., Studebaker I., John B. (2010) Prescribing errors in a pediatric clinic. Clin Pediatrics 49: 49–53. [DOI] [PubMed] [Google Scholar]
- Conroy S. (2011) Association between licence status and medication errors. Arch Dis Childhood 96: 305–306. [DOI] [PubMed] [Google Scholar]
- Cordero L., Kuehn L., Kumar R., Mekhjian H. (2004) Impact of computerized physician order entry on clinical practice in a newborn intensive care unit. J Perinatol 24: 88–93. [DOI] [PubMed] [Google Scholar]
- Dabliz R., Levine S. (2012) Medication safety in neonates. Am J Perinatol 29: 49–56. [DOI] [PubMed] [Google Scholar]
- Daniell A., Darlow B. (1989) Audit of drug usage in a regional neonatal intensive care unit. J Paediatrics Child Health 25: 207–210. [DOI] [PubMed] [Google Scholar]
- Ernawati D., Lee Y., Hughes J. (2014) Nature and frequency of medication errors in a geriatric ward: an indonesian experience. Ther Clin Risk Management 10: 413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Medicines Agency (2015) Medication Errors. Available at: http://www.ema.europa.eu/ema/index.jsp?curl=pages/special_topics/general/general_content_000570.jsp
- Folli H., Poole R., Benitz W., Russo J. (1987) Medication Error prevention by clinical pharmacists in two children’s hospitals. Pediatrics 79: 718–722. [PubMed] [Google Scholar]
- Fortescue E., Kaushal R., Landrigan C., McKenna K., Clapp M., Federico F., et al. (2003) Prioritizing strategies for preventing medication errors and adverse drug events in pediatric inpatients. Pediatrics 111: 722–729. [DOI] [PubMed] [Google Scholar]
- Frey B., Buettiker V., Hug M., Waldvogel K., Gessler P., Ghelfi D., et al. (2002) Does critical incident reporting contribute to medication error prevention? Eur J Pediatrics 161: 594–599. [DOI] [PubMed] [Google Scholar]
- Frey B., Kehrer B., Losa M., Braun H., Berweger L., Micallef J., et al. (2000) Comprehensive critical incident monitoring in a neonatal-pediatric intensive care unit: experience with the system approach. Intensive Care Med 26: 69–74. [DOI] [PubMed] [Google Scholar]
- García-Aparicio J., Herrero-Herrero J. (2013) Medication errors detected in elderly patients admitted to an internal medicine service. Int J Clin Practice 67: 282–289. [DOI] [PubMed] [Google Scholar]
- Ghaleb M., Barber N., Franklin B., Wong I. (2010) The Incidence and nature of prescribing and medication administration errors in paediatric inpatients. Arch Dis Childhood 95: 113–118. [DOI] [PubMed] [Google Scholar]
- Gray J., Goldmann D. (2004) Medication errors in the neonatal intensive care unit: special patients, unique issues. Arch Dis Childhood Fetal Neonatal Ed 89: F472–F473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray J., Suresh G., Ursprung R., Edwards W., Nickerson J., Shiono P., et al. (2006) Patient misidentification in the neonatal intensive care unit: quantification of risk. Pediatrics 117: e43–e47. [DOI] [PubMed] [Google Scholar]
- Henri L., Dalleur O., Vaillant F., Cornette P. (2012) Medication administration errors in a geriatric ward in a Belgian hospital. Eur Geriatric Med 3: S123. [Google Scholar]
- Jain S., Basu S., Parmar V. (2009) Medication errors in neonates admitted in intensive care unit and emergency department. Indian J Med Sci 63: 145. [PubMed] [Google Scholar]
- Jennane N., Madani N., Oulderrkhis R., Abidi K., Khoudri I., Belayachi J., et al. (2011) Incidence of medication errors in a moroccan medical intensive care unit. Int Arch Med 4: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaushal R., Bates D., Landrigan C., McKenna K., Clapp M., Federico F., et al. (2001) Medication errors and adverse drug events in pediatric inpatients. JAMA 285: 2114–2120. [DOI] [PubMed] [Google Scholar]
- Kopp B., Erstad B., Allen M., Theodorou A., Priestley G. (2006) Medication errors and adverse drug events in an intensive care unit: direct observation approach for detection. Crit Care Med 34: 415–425. [DOI] [PubMed] [Google Scholar]
- Kozer E., Scolnik D., Macpherson A., Keays T., Shi K., Luk T., et al. (2002) Variables associated with medication errors in pediatric emergency medicine. Pediatrics 110: 737–742. [DOI] [PubMed] [Google Scholar]
- Kunac D., Reith D. (2005) Identification of priorities for medication safety in neonatal intensive care. Drug Safety 28: 251–261. [DOI] [PubMed] [Google Scholar]
- Leape L., Cullen D., Clapp M., Burdick E., Demonaco H., Erickson J., et al. (1999) Pharmacist participation on physician rounds and adverse drug events in the intensive care unit. JAMA 282:267–270. [DOI] [PubMed] [Google Scholar]
- Ligi I., Arnaud F., Jouve E., Tardieu S., Sambuc R., Simeoni U. (2008) Iatrogenic events in admitted neonates: a prospective cohort study. Lancet 371: 404–410. [DOI] [PubMed] [Google Scholar]
- Lisby M., Nielsen L., Mainz J. (2005) Errors in the medication process: frequency, type, and potential clinical consequences. Int J Qual Health Care 17: 15–22. [DOI] [PubMed] [Google Scholar]
- Maher R., Hajjar E. (2012) Medication errors in the ambulatory elderly. Aging Health 8: 127–135. [Google Scholar]
- Manias E., Kinney S., Cranswick N., Williams A. (2014) Medication errors in hospitalised children. J Paediatrics Child Health 50: 71–77. [DOI] [PubMed] [Google Scholar]
- Metsälä E., Vaherkoski U. (2014) Medication errors in elderly acute care–a systematic review. Scand J Caring Sci 28: 12–28. [DOI] [PubMed] [Google Scholar]
- Otero P., Leyton A., Mariani G., Cernadas J. (2008) Medication errors in pediatric inpatients: prevalence and results of a prevention program. Pediatrics 122: e737–e743. [DOI] [PubMed] [Google Scholar]
- Ozkan S., Kocaman G., Ozturk C., Seren S. (2011) Frequency of pediatric medication administration errors and contributing factors. J Nursing Care Qual 26: 136–143. [DOI] [PubMed] [Google Scholar]
- Pallas C., De-La-Cruz J., Del-Moral T., Lora D., Malalana A. (2008) Improving the quality of medical prescriptions in neonatal units. Neonatology 93: 251–256. [DOI] [PubMed] [Google Scholar]
- Picone D., Titler M., Dochterman J., Shever L., Kim T., Abramowitz P., et al. (2008) Predictors of medication errors among elderly hospital patients. Am J Med Qual 23: 115–127. [DOI] [PubMed] [Google Scholar]
- Raju T., Thornton J., Kecskes S., Perry M., Feldman S. (1989) Medication errors in neonatal and paediatric intensive-care units. Lancet 334: 374–376. [DOI] [PubMed] [Google Scholar]
- Raju T., Suresh G., Higgins R. (2011) Patient Safety in the context of neonatal intensive care: research and educational opportunities. Pediatric Res 70: 109–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross L., Wallace J., Paton J. (2000) Medication errors in a paediatric teaching hospital in the uk: five years operational experience. Arch Dis Childhood 83: 492–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roughead L., Semple S., Rosenfeld E. (2013) Literature review: medication safety in Australia. Sydney: Australian Commission on Safety and Quality in Health Care. [Google Scholar]
- Saghafi F., Zargarzadeh A. (2014) Medication error detection in two major teaching hospitals: what are the types of errors? J Res Med Sci 19: 617. [PMC free article] [PubMed] [Google Scholar]
- Simpson J., Lynch R., Grant J., Alroomi L. (2004) Reducing medication errors in the neonatal intensive care unit. Arch Dis Childhood Fetal Neonatal Ed 89: F480–F482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorrentino E., Alegiani C. (2012) Medication errors in the neonate. J Maternal-Fetal Neonatal Med 25: 83–85. [DOI] [PubMed] [Google Scholar]
- Stavroudis T., Shore A., Morlock L., Hicks R., Bundy D., Miller M. (2010) NICU medication errors: identifying a risk profile for medication errors in the neonatal intensive care unit. J Perinatol 30: 459–468. [DOI] [PubMed] [Google Scholar]
- Suresh G., Horbar J., Plsek P., Gray J., Edwards W., Shiono P., et al. (2004) Voluntary anonymous reporting of medical errors for neonatal intensive care. Pediatrics 113: 1609–1618. [DOI] [PubMed] [Google Scholar]
- Taylor B., Selbst S., Shah A. (2005) Prescription writing errors in the pediatric emergency department. Pediatric Emergency Care 21: 822–827. [DOI] [PubMed] [Google Scholar]
- Tayman C., Rayyan M., Allegaert K. (2011) Neonatal pharmacology: extensive interindividual variability despite limited size. J Pediatric Pharmacol Ther 16: 170–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Den Anker J. (2005) Managing drugs safely. Semin Fetal Neonatal Med 10: 73–81. [DOI] [PubMed] [Google Scholar]
- Van Den Bemt P., Fijn R., Van Der Voort P., Gossen A., Egberts T., Brouwers J. (2002) Frequency and determinants of drug administration errors in the intensive care unit. Crit Care Med 30: 846–850. [DOI] [PubMed] [Google Scholar]
- Vincer M., Murray J., Yuill A., Allen A., Evans J., Stinson D. (1989) Drug errors and incidents in a neonatal intensive care unit: a quality assurance activity. Am J Dis Children 143: 737–740. [DOI] [PubMed] [Google Scholar]
- Wiedenmayer K., Summers R., Mackie C., Gous A., Everard M. (2006) Developing pharmacy practice: a focus on patient care. The Hague: World Health Organisation and International Pharmaceutical Federation. [Google Scholar]
- Wilson D., McArtney R., Newcombe R., Mcartney R., Gracie J., Kirk C., et al. (1998) Medication Errors in Paediatric Practice: Insights from a Continuous Quality Improvement Approach. Eur J Pediatrics 157: 769–774. [DOI] [PubMed] [Google Scholar]
- Winterstein A., Johns T., Rosenberg E., Hatton R., Gonzalez-Rothi R., Kanjanarat P. (2004) Nature and causes of clinically significant medication errors in a tertiary care hospital. Am J Health-Syst Pharm 61: 1908–1916. [DOI] [PubMed] [Google Scholar]
- Wong I., Wong L., Cranswick N. (2009) Minimising medication errors in children. Arch Dis Childhood 94: 161–164. [DOI] [PubMed] [Google Scholar]
- Zakharov S., Tomas N., Pelclova D. (2012) Medication errors–an enduring problem for children and elderly patients. Upsala J Med Sci 117: 309–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeraatchi A., Talebian M., Nejati A., Dashti-Khavidaki S. (2013) Frequency and types of the medication errors in an academic emergency department in iran: the emergent need for clinical pharmacy services in emergency departments. J Res Pharm Practice 2: 118. [DOI] [PMC free article] [PubMed] [Google Scholar]