Abstract
Background and Aims
Low-quality bowel preparation reduces efficacy of colonoscopy. We aimed to summarize effects of bowel preparation on detection of adenomas, advanced adenomas and colorectal cancer.
Methods
A systematic literature search was performed regarding detection of colonic lesions after normal and low-quality bowel preparation. Reported bowel preparation quality was transformed to the Aronchick scale with its qualities “excellent”, “good”, “fair”, “poor”, and “insufficient” or “optimal” (good/excellent), “suboptimal” (fair/poor/insufficient), “adequate” (good/excellent/fair) and “inadequate” (poor/insufficient). We identified two types of studies: i) Comparative studies, directly comparing lesion detection according to bowel preparation quality, and ii) repeat colonoscopy studies, reporting results of a second colonoscopy after previous low-quality preparation.
Results
The detection of early adenomas was reduced with inadequate vs. adequate bowel preparation (Odds Ratio (OR) 0.53, CI: 0.46–0.62, p<0.001). The advanced adenomas were affected less in comparison (0.74, CI: 0.62–0.87, p<0.001). The large number of subjects considered in the present meta-analysis resulted in smaller confidence intervals compared to earlier studies. Classifying the bowel-preparation quality as suboptimal vs. optimal led to the same qualitative conclusion (OR: 0.81, CI: 0.74–0.89, p<0.001 for early adenomas, OR: 0.94, CI: 0.87–1.01, n.s. for advanced adenomas). Bowel preparation was equally important for right-sided/ flat/ serrated vs. other lesions in most observational studies but more relevant in some repeat colonoscopy studies; data regarding carcinoma detection were insufficient.
Conclusion
Inadequate bowel preparation affects detection of early colonic lesions stronger than advanced lesions.
Introduction
Colorectal cancer (CRC) remains the second most common cancer in women and the third most common in men [1]. In industrialized countries the lifetime incidence for patients at average risk is approximately 5%, and more than 600’000 patients die from this cancer every year [2].
CRC incidence and mortality can be reduced by endoscopic screening since precancerous lesions (early and advanced adenomas) can be detected and removed during the intervention [3,4]. In a large randomized study one-time screening with sigmoidoscopy resulted in a 23% decrease in CRC incidence and a 31% decrease in CRC mortality after a follow up of 11 years [3]. The protective effect of colonoscopy so far has not been tested in randomized trials but should exceed the effect of sigmoidoscopy since the whole colon is visualized. Nevertheless, colonoscopy is regarded as the most effective CRC screening strategy by gastroenterologists and professional organizations [2,5,6].
A high quality of colonoscopy is decisive for maximum protection from CRC. Interval carcinoma refer to carcinoma detected before the recommended surveillance interval and might be responsible for up to 10% of all CRCs [7–9]. Adenoma detection rate (ADR) is inversely correlated with interval cancer development [9,10] and widely used as a surrogate for the quality of colonoscopy [11]. Many factors including experience of the endoscopist, withdrawal time, and quality of bowel preparation are associated with ADR [11].
Suboptimal bowel preparation has been reported in as much as 20% of all colonoscopies [12,13], possibly reducing ADR. The best strategy after such a colonoscopy remains unclear: Even though poor bowel preparation reduces protection from CRC, an immediate repetition of colonoscopy clearly offers less benefit then the original intervention. Clarity regarding effects of bowel preparation on differential detection of adenomas, advanced adenomas and CRC is needed to enable an informed decision regarding repetition of colonoscopy. Missing early colonic lesions will be inconsequential in the majority of cases since only a minority will ever transform to cancer. However, detection of advanced lesions will critically impact the future clinical course and detection of these lesions accounts for the largest impact of colonoscopy on CRC prevention. However, a previous meta-analysis demonstrated widely overlapping confidence intervals for the detection of early vs. advanced lesions [16].
We decided to perform another systematic review and meta-analysis regarding the effect of bowel preparation, considerably expanding the previous meta-analysis [16]. Our analysis revealed a stronger effect of bowel preparation on the detection of advanced vs. early colonic lesions.
Materials and Methods
Between November 1st and November 7th 2014 we performed a systematic PubMed literature research regarding the impact of quality of bowel preparation on detection of lesions. The following search strategy was used: (Adenoma detection OR polyp detection) AND bowel preparation, colonoscopy AND Boston bowel preparation scale (BBPS), colonoscopy AND Ottawa scale, colonoscopy AND Aronchick scale, and colonoscopy AND tandem colonoscopy (S1 file). The abstracts of all publications were screened and potentially relevant papers retrieved. In addition, a search within the reference list of several publications including a recent meta-analysis [16] identified 3 additional relevant articles.
Inclusion criteria
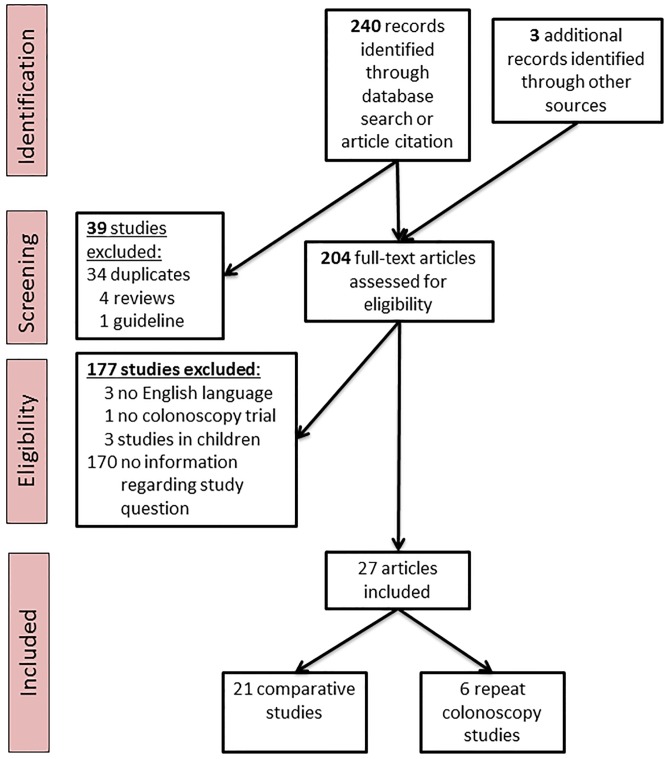
Our analysis identified two study types: Comparative studies (for which adenoma/polyp detection rates were compared according to bowel preparation quality within a given study population) and repeat-colonoscopy studies (for which after low-quality colonoscopy the investigation was repeated). The study selection process is shown in Fig 1. Independent sets inclusion criteria were defined: Comparative studies were included if the following criteria were met: i) bowel preparation was defined and reported. ii) adenoma or polyp detection was reported as raw numbers and/or odds ratios for at least two qualities of bowel preparation [16]. Repeat colonoscopy studies were included if: i) Colonoscopy was repeated for at least a fraction of patients, ii) bowel preparation was defined and reported for the first and second colonoscopy, iii) the first and the second colonoscopy reported lesion detection rates and/or miss rates (defined by the number of detected lesions in the second colonoscopy divided by the sum of lesion in both colonoscopies).
Fig 1. PRISMA flow diagram.
For a separate analysis addressing differential detection of flat/serrated and/or right-sided lesions studies were included if: i) Bowel preparation was defined and reported and ii) data for a comparison with either all polyps/adenomas and/or left-sided, pedunculated or non-serrated lesions was available.
Only studies for which an adult study population was evaluated by complete colonoscopy and only articles in English published before November 2014 were considered. If the same study population had been analyzed more than once only the latest analysis was included. Review and data extraction of each study was performed by two authors (BM and MCS or AK); discrepancies were resolved after discussions. All relevant data were retrieved from the original publications; the authors of the respective studies were not contacted in case of missing, incomplete or incomprehensible data.
Studies differed regarding their outcomes: Colonic lesions were either summarized as polyps, referring to protruding lesions detected during endoscopy without histological information or adenomas, for which histological confirmation was required. Similarly, advanced lesions were either summarized as advanced polyps, referring to lesions ≥1cm diameter without histological information or advanced adenomas. The latter category included lesions with villous/ tubulovillous or serrated histology irrespective of its size or tubular adenomas with a diameter ≥1cm. If data regarding both, adenoma and polyp detection, were available, only adenoma data were considered. We included data regarding polyp/adenoma detection using the following hierarchy: Odds Ratio (OR) derived from a multivariate analysis, OR from a univariate analysis, raw numbers.
Analysis of bowel preparation
The Aronchick scale [17] was the most frequently used bowel preparation scale (Table 1) and the 5 preparation qualities “excellent”, “good”, “fair”, “poor”, and “insufficient” were used throughout this study. In addition we compared “optimal” (defined as “excellent” or “good”) with “suboptimal” (“fair”, “poor”, or “insufficient”) and “adequate” (“excellent”, “good”, or “fair”) with “inadequate” (“poor” or “insufficient”) preparations. BBPS was converted to the Aronchick scale using data from Lai et al. [18]. Only one publication used the Ottawa scale and due to limited data only conversion to the broad categories optimal/ suboptimal was possible [19]. No study used the Chicago scale. Unique scales were also converted to the Aronchick scale. In several publications these scales had not been strictly defined and in a conservative approach only a conversion to broad categories (optimal/ suboptimal or adequate/ inadequate) was done.
Table 1. Bowel preparation scales and definitions used.
| Aronchick scale [17] |
| excellent: a small volume of clear liquid or >95% of surface seen |
| good: large volume of clear liquid covering 5–25% of the surface but >90% of surface seen |
| fair: some semisolid stool, >90% of surface seen |
| poor: semisolid stool could not be sucked away, <90% of surface seen |
| inadequate: repeat preparation needed |
| Boston Bowel Preparation Scale (BBPS) [33, 40] |
| Score 3 segments of the colon |
| 0: Unprepared colon segment with mucosa not well seen due to solid stool that cannot be cleared |
| 1: Portion of mucosa of the colon segment seen, but other areas are not well seen due to staining, residual stool and/ or opaque liquid |
| 2: Minor amount of residual staining, small fragments of stool and/ or opaque liquid but mucosa of colon segment well seen |
| 3: Entire mucosa of the colon well seen with no residual staining, small fragments of stool and/ or opaque liquid. Comment: |
| score reaches from 0–9 (for each colon segment separate scores, e.g., 2+2+3 = 7) |
| Other definitions |
| Optimal = good + excellent |
| Suboptimal = insufficient + poor + fair |
| Adequate = fair + good + excellent |
| Inadequate = insufficient + poor |
Quality of included studies
The quality of all included studies was evaluated following a strategy adapted from a previous meta-analysis [16]: i) Adenoma detection: 1 point was given if adenoma detection and 0 points if only polyp detection had been reported. ii) Study population: 2 points if the study population consisted only of patients referred for CRC screening, 1 point if only patients for CRC screening and adenoma surveillance were considered, and 0 points if patients with symptoms or indications other than CRC screening and adenoma surveillance were also included. iii) Study design: 1 point for a prospective, 0 point for a retrospective study design. iv) Bowel preparation: 1 point if training, exercises or internal validations for the respective bowel preparation scale had been performed. v) Confounders: 2 points were given if the study controlled for all crucial confounders: age, gender and colon withdrawal time. 1 point if the study controlled for any confounders.
Statistical analysis
Meta-analysis
The meta-analysis was performed to summarize early and advanced adenoma detection in all studies included. Unless otherwise mentioned, meta-analysis was performed comparing two kinds of bowel preparations at a time. For this pairwise comparison, the total number of subjects who had either of the two described qualities of preparation as well as the number of patients for whom at least one adenoma was detected was tabulated. The number of studies included as well as the number of patients in these sub-categories are reported (Fig 2 and S1 Fig). For our meta-analysis we used a random-effects model weighing the contributions from different studies based on both the intra-study and inter-study variances. StatsDirect software version 3.0.150 (StatsDirect Ltd., Sale, Cheshire, UK; www.statsdirect.com) was used and Forest plots as well as funnel plots were generated. The overall OR, confidence intervals (CI), and p-values obtained from a random-effects model were reported. Bias assessment graphs were also generated but indicated a lack of bias according to visual inspection (S2 Fig). The number of studies included was not sufficient to obtain a reliable bias-estimator such as the Begg-Mazumdar estimator (typically requiring more than 25 high quality studies) and no such analysis was performed.
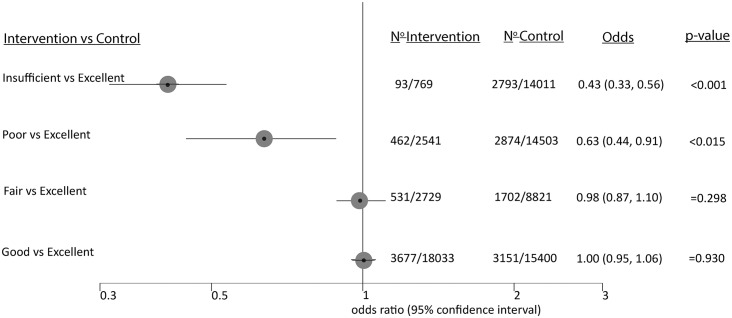
Fig 2. Effects of insufficient, poor, fair and good bowel preparation compared to an excellent preparation on overall detection of colonic lesions in a network meta-analysis.
We performed a network meta-analysis to summarize adenoma detection according to the five qualities of the Aronchick scale with pairwise comparison of all 5 preparation qualities. For these calculations we used the algorithms by Chaimani et al. [20] and the corresponding STATA modules (http://www.mtm.uoi.gr). The analysis showed indirect effects among the categories to be irrelevant. We therefore reported the pairwise meta-analysis results relative to good or excellent preparation.
Results
Our systematic literature research identified 204 potentially relevant studies which were screened for eligibility; 27 of those fulfilled our inclusion criteria and were used in subsequent analyses (Table 2). We included studies of two different categories: i) 21 comparative (observational) studies for which adenoma/polyp detection rates were compared according to bowel preparation within given study populations, ii) 6 repeat-colonoscopy studies in which results of a second colonoscopy (tandem colonoscopy) after an initial endoscopy with less than optimal preparation were reported. Due to different study designs both types of studies are summarized separately.
Table 2. Summary of all included studies.
| Study Publication year | Quality points | Number (n) colonoscopies | Study type | Bowel preparation scale |
|---|---|---|---|---|
| Mahadev [1] 2014 | 4 | 1,649 | Comparative Retrospective | Unique |
| Kim [28] 2014 | 5 | 482 | Comparative Prospective | BBPS Aronchick |
| Holt [19] 2014 | 4 | 413 | Comparative Prospective | Ottawa |
| Singhal [23] 2014 | 1 | 297 | Repeat-colonoscopy Retrospective | Aronchick |
| Anderson [25] 2014 | 1 | 13,022 | Comparative Prospective | Unique |
| Lee [41] 2014 | 4 | 31,088 | Comparative Prospective | Unique |
| Fayad [42] 2013 | 2 | 2,163 | Comparative Retrospective | Aronchick |
| Menees [31] 2013 | 3 | 71 | Repeat-colonoscopy Retrospective | Aronchick |
| Gao [37] 2013 | 4 | 1,012 | Comparative Prospective | BBPS |
| Jover [26] 2013 | 6 | 4,539 | Comparative Prospective (RCT) | Aronchick |
| Bryant [27] 2012 | 0 | 1,785 | Comparative Retrospective | Unique |
| Adler [43] 2013 | 6 | 11,166 | Comparative Prospective | Aronchick-based |
| Chokshi [29] 2012 | 3 | 133 | Repeat-colonoscopy Retrospective | Aronchick |
| Goncalves [44] 2011 | 2 | 1,545 | Comparative Retrospective | Unique |
| Sherer [45] 2012 | 2 | 8,800 | Comparative Retrospective | Unique |
| De Jonge [39] 2012 | 2 | 4,800 | Comparative Retrospective | Unique |
| Enestvedt [46] 2011 | 4 | 190 | Comparative Prospective (RCT) | BBPS |
| Calderwood [33] 2010 | 4 | 983 | Comparative Prospective | BBPS |
| Shaukat [47] 2009 | 5 | 47,253 | Comparative Retrospective | Unique |
| Radaelli [48] 2008 | 1 | 12,835 | Comparative Consecutive | Unique |
| Froehlich [22] 2005 | 2 | 5,832 | Comparative Prospective | Unique |
| Harewood [13] 2003 | 1 | 93,004 | Comparative Retrospective | Unique |
| Pontone [49] 2014 | 1 | 190 | Comparative Retrospective | Aronchick |
| Xiang [30] 2014 | 3 | 2,093 | Repeat-colonoscopy Retrospective | Unique |
| Aslanian [50] 2013 | 4 | 502 | Comparative Prospective (RCT) | Aronchick |
| Lebwohl [12] 2011 | 1 | 216 | Repeat-colonoscopy Retrospective | Aronchick |
| Hong [21] 2012 | 5 | 277 | Repeat-colonoscopy Prospective | Aronchick |
Quality points were given for a detailed reporting of lesions, the study population, study design, validation of stool scales and correction for confounders (for details see methods). RCT: Randomized controlled trial. BBPS: Boston Bowel Preparation Scale.
Bowel preparation and overall adenoma and polyp detection
We included 21 comparative studies in our meta-analysis. Aronchick scale was used in 5 of these studies to report bowel preparation quality, 1 study used an Aronchick-based scale, 3 studies used BBPS, and 1 the Ottawa scale. 11 additional studies used unique non-validated scales. Bowel preparation quality was converted to the 5 qualities of the Aronchick scale (“excellent”, “good”, “fair”, “poor”, “insufficient”), or two pairs of broader categories “optimal” (i.e. good/excellent) vs. “suboptimal” (i.e. fair/poor/insufficient) and “adequate” (i.e. excellent/good/fair) vs. “inadequate” (i.e. poor/insufficient). When bowel preparation quality of all studies was summarized, 77% of patients had optimal preparation, and 95% had adequate preparation.
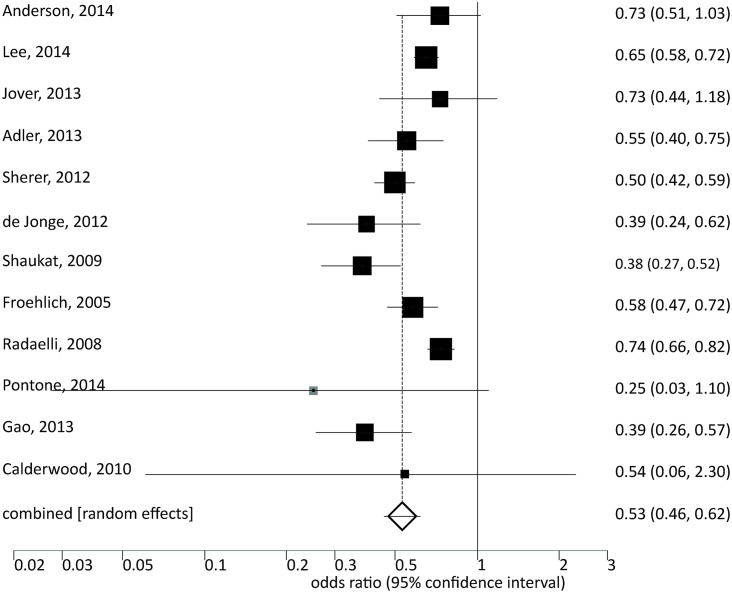
Low-quality bowel preparation was significantly associated with reduced detection of polyps or adenomas (Fig 3 and S3 Fig): For inadequate vs. adequate preparation the OR was 0.53 (CI: 0.46–0.62, p<0.001). For suboptimal vs. optimal preparation an OR of 0.81 (CI: 0.74–0.89, p<0.001) was calculated.
Fig 3. Meta-analysis of studies showing effects of inadequate vs. adequate bowel preparation regarding detection of colonic lesions.
We also summarized adenoma detection for the individual qualities of the Aronchick scale (Fig 2). Despite no difference for excellent, good, and fair bowel preparation adenoma detection decreased with poor and insufficient preparation (poor: OR 0.63, CI: .44–0.91, p<0.015; insufficient: OR 0.43, 0.33–0.56, p<0.001). However, only four studies provided data regarding insufficient bowel preparation.
For a sensitivity analysis we assessed the quality of the included studies (see legend of Table 2 and methods section). When we restricted our analysis to high-quality studies (8 studies with ≥4 quality points) our conclusions remained intact (OR suboptimal vs. optimal: 0.76, CI 0.69–0.83, p<0.001; OR inadequate vs. adequate: 0.57, CI 0.46–0.72, p<0.001; S1 Table). Similarly, restriction to studies with adenoma (not polyp) detection or to studies using Aronchick scale/ Aronchick based scale or a defined scale did not change our conclusions.
No publication bias was detected and all funnel plots for all analyses looked symmetric (see S1 Fig and data not shown).
Detection of advanced adenomas/ large polyps
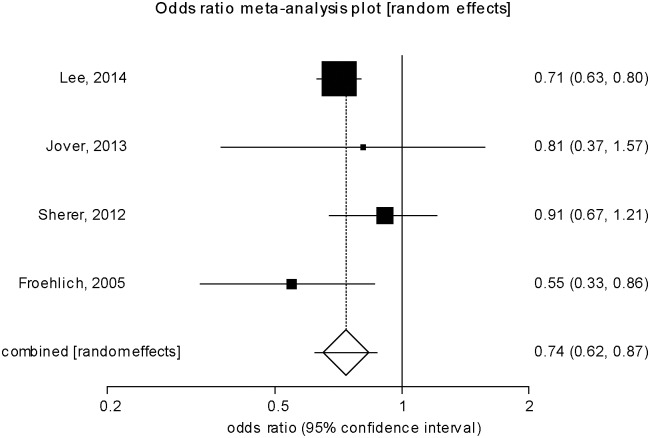
In comparative studies, low-quality bowel preparation was also associated with reduced detection of advanced lesions. In this analysis 7/11 studies defined advanced polyps by histological information, 4/11 studies by polyp size >9mm. Inadequate vs. adequate preparation significantly reduced detection of advanced lesions (OR 0.74, CI: 0.62–0.87, p<0.001; Fig 4). In comparison to early advanced colonic lesions (see above), advanced lesions are affected stronger by inadequate preparation showing non-overlapping confidence of the OR for early and advanced lesions.
Fig 4. Meta-analysis of inadequate and adequate bowel preparation regarding detection of advanced adenomas or polyps.
Suboptimal vs. optimal preparation showed a strong trend for reduced lesion detection (OR 0.94, CI: 0.87–1.01, p = 0.33; data not shown). When we compared the 5 preparation qualities of the Aronchick scale, detection of advanced lesions tended to be lower for poor and insufficient bowel preparation (poor vs. good/excellent: OR 0.79; CI: 0.53–1.19, p = 0.259; insufficient vs. good/excellent: OR 0.75; CI: 0.27–2.14, p = 0.777; S1 Fig). However, the low number of lesions (85 for poor, 4 for insufficient) limits our conclusions.
In a sensitivity analysis our conclusions remained robust when studies with and without histological information were distinguished (inadequate vs. adequate: OR advanced adenoma detection 0.76, CI: 0.65–0.89, p<0.001; OR advanced polyp detection: 0.55, CI: 0.33–0.86, p = 0.006; S2 Table). Similarly, our conclusions did not change when only high-quality studies or studies using a defined scale were considered.
Detection of early and advanced adenomas in repeat-colonoscopy studies
We included 5 repeat-colonoscopy studies (Table 3). The heterogeneous study design precluded direct comparison and meta-analysis. Results of some were reported as adenoma miss rates, defined as the number of adenomas detected during the second colonoscopy divided by the sum of all adenomas in the first and second colonoscopy. Adenoma miss rates ranging from 27%-56% for colonoscopies with poor, fair or suboptimal preparation were reported. Only one study provided an internal control with colonoscopies of good and excellent preparation with adenoma miss rates of 27% and 21%, respectively [21].
Table 3. Summary of repeat-colonoscopy studies.
| Study Publication year | Quality points | Study population Number of included patients | Number lesions analyzed | Preparation first colonoscopy | Preparation Second Colonoscopy | Time Repeat colonoscopy | Adenoma miss rate (ADR) | Advanced adenoma miss rate (Adv. ADR) |
|---|---|---|---|---|---|---|---|---|
| Studies providing analysis per adenoma (adenoma miss rate) | ||||||||
| Menees [3] 2013 | 3 | 619 Screening colonoscopies. 71 included | A: 163 AdvA: 22 | Fair | optimal: 58%, | <3y | 31% | 0% |
| fair: 21%, | ||||||||
| poor: 20% | ||||||||
| Chokshi [29] 2012 | 3 | 373 Screening colonoscopies. 133 included | A: 190 AdvA: 30 | Poor: 87% | Adequate: 77%, | Mean 340 days | 48% | 50% |
| Insufficient: 13% | inadequate: 23% | |||||||
| Lebwohl [12] 2011 | 2 | 3047 Screening and diagnostic colonoscopies. 216 included | A: 198 | Suboptimal | Excellent/Good | <3 y | Poor: 56% | Poor: 29% |
| Fair: 42% | Fair: 26% | |||||||
| Screening: 43% | Screening: 37% | |||||||
| Hong [21] 2012 | 5 | Patients scheduled for polypectomy after a first diagnostic colonoscopy.277 included | A: 714 AdvA: 184 | Excellent: 32% | Excellent/ good | <3 mo | Excellent: 21% | Excellent: 9% |
| Good: 41% | Good: 27% | Good: 17% | ||||||
| Fair: 20% | Fair: 27% | Fair: 18% | ||||||
| Inadequate: 7% | Inadequate: 47% | Inadequate: 37% | ||||||
| Studies providing analysis per patient (ADR, Adv. ADR) | ||||||||
| Singhal [23] 2014 | 1 | 10908 colonoscopies of screening and diagnostic indications 297 included | Inadequate | Optimal: 52% | <5y | First colonoscopy22% | First colonoscopy: 7.4% | |
| fair: 31%, | Repeat- colonoscopy 4% | Repeat-colonoscopy 8.4% | ||||||
| poor: 17% |
A: adenoma, AdvA: advanced adenoma, ADR: adenoma detection rate, AdvA. ADR: advanced adenoma detection rate
Advanced adenoma miss rates ranged from 0–50%. Only one study reported an internal control regarding advanced adenoma detection in a repeat-colonoscopy after a colonoscopy of excellent or good preparation reporting a miss rate of 9% and 17%, respectively [21].
All repeat-colonoscopy studies reported on a selected patient population: repeat examinations were either performed in a small subset of the original study population (Table 3) or only patients scheduled for polypectomy were included [21].
Carcinoma detection
Of the comparative studies only one large study with 5832 patients [22] reported on differential carcinoma detection. In this study a non-significant paradoxical trend of lower carcinoma detection in patients with optimal vs. inadequate preparation was noted (OR 0.68; CI: 0.45–1.02, p = 0.063). All of the remaining comparative studies were either underpowered (reporting no or only 1 carcinoma case) or did not comment on carcinoma detection.
In one repeat-colonoscopy study with 150 repeat examinations, three carcinoma cases had been missed during the initial investigations and were detected during the second colonoscopy [23]. However, all carcinomas were detected in symptomatic patients and no carcinoma had been missed in patients referred for CRC screening.
Detection of right-sided, flat or serrated adenomas
We identified 11 studies addressing differential detection of right-sided, flat or serrated adenomas in patients with low quality bowel preparation (Table 4). 7 studies were comparative, 4 studies were repeat-colonoscopy studies. A heterogeneous study design and different end-points precluded a meta-analysis.
Table 4. Effects of bowel preparation on the detection of right-sided, flat or serrated polyps/ adenomas.
| Study Year of publication | Quality | n | Readout | Study results | Study conclusion |
|---|---|---|---|---|---|
| Comparative studies | |||||
| Kim [28] 2014 | 5 | 482 | Right- sided polyps | Correlation analysis: BBPS≥ 8 vs. BBPS< 8 BBPS segment scores in the right colon but not in the left colon correlated with polyp detection rates (right: r = 0.107, p = 0.018; left: r = 0.059, p = 0.198) | Bowel preparation more relevant for polyp detection in the right colon |
| de Wijkerslooth [24] 2013 | 6 | 1,354 | Proximal serrated adenoma | Multivariate analysis: Ottawa scale was associated with: | Bowel preparation equally relevant for detection of right-sided serrated adenoma vs. other adenomas |
| - overall ADR (OR 0.95; CI: 0.91–0.99) | |||||
| - but not proximal SDR (OR: 0.98; CI: 0.92–1.05) | |||||
| Anderson [25] 2014 | 1 | 13,022 | Right- sided serrated | Optimal vs. poor bowel preparation | Bowel preparation equally relevant for overall, right-sided, and serrated adenoma detection |
| - Overall ADR: 26.3% vs. 20.9% | |||||
| - Proximal ADR: 12.9% vs. 8% | |||||
| - SDR 8.8% vs. 7.5% | |||||
| no significant differences | |||||
| Lee [41] 2014 | 4 | 31,088 | Right-sided | Adequate vs. inadequate bowel preparation | Bowel preparation equally relevant for adenoma detection in the right and left colon |
| - OR overall adenoma detection 1.38 (1.23–1.54) | |||||
| - OR right sided adenoma 1.16 (1.13–1.33) | |||||
| no significant differences | |||||
| Jover [26] 2013 | 6 | 4,539 | Right-sided | No significant effects of bowel preparation on adenoma detection, similar trends for right- and left sided adenomas | Bowel preparation equally relevant for adenoma detection in the right and left colon |
| Bryant [27] 2012 | 0 | 1785 | Right- sided polyp | Adequate vs. poor preparation | Bowel preparation equally relevant for polyp detection in the right and left colon |
| - OR left-side: 1.1 (0.8–1.5) | |||||
| - OR right-side: 1.1 (0.8–1.5) | |||||
| no significant differences | |||||
| Calderwood [33] 2010 | 4 | 983 | Right-sided polyp | BBPS 0.1 vs. BBPS 2,3. Multivariate analysis | Bowel preparation equally relevant for polyp detection in the right and left colon |
| - OR right side: 1.6 (1.01–2.55) | |||||
| - OR left side: 2.6 (1.34–4.98) | |||||
| Repeat colonoscopy studies | |||||
| Xiang [30] 2014 | 3 | 2,093 | Flat adenoma | In patients with poor bowel preparation the OR for missing a flat adenoma is 4.4 (no comparison to protruding adenoma provided) | Bowel preparation relevant for flat adenoma miss rate |
| Lebwohl [12] 2011 | 1 | 216 | Proximal | Adenoma miss rate 42% for proximal and distal adenomas | Bowel preparation equally relevant for adenoma miss rate in the right and left colon |
| Singhal [23] 2014 | 1 | 297 | Right-sided | 67% of all missed adenomas were right-sided adenomas | Bowel preparation more relevant for adenoma miss rate in the right colon |
| Chokshi [29] 2012 | 3 | 133 | Right-sided | 65% of all missed adenomas and 80% of all missed advanced adenomas were in the right colon | Bowel preparation more relevant for adenoma miss rate in the right colon |
n.s. = not significant. ADR = Adenoma detection rate. Adv. ADR = Advanced adenoma detection rate. SDR = serrated adenoma detection rate. BBPS = Boston Bowel Preparation Scale.
As shown in Table 4, 6 out of 7 comparative studies [24–27] failed to detect a disproportionate effect of low bowel preparation for the detection of proximal and/ or serrated lesions. In only one study low quality preparation was associated with reduced right-sided but not left-sided polyp detection [28]. However, this study was the smallest of all comparative studies addressing this question.
In contrast, in repeat-colonoscopy studies less than optimal preparation was associated with diminished detection of flat/ serrated or right-sided lesions. In two studies approximately 65% of all missed lesions were right-sided and even 80% of all advanced adenomas missed resided in the right colon [23,29]. One tandem colonoscopy study noted an OR of 4.4 for flat adenomas compared to protruding adenomas to be missed in a poorly prepared colon [30]. In one repeat-colonoscopy study bowel preparation effected adenoma detection in the left and right colon in a similar manner [12].
Discussion
We performed a systematic literature research and meta-analysis to distinguish effects of low-quality bowel preparation on the differential detection of early, advanced colonic lesions and cancer during colonoscopy. We found that with inadequate bowel preparation, the chance of detecting early vs. advanced polyps drops by 44% and 23%, respectively. With suboptimal preparation, detection of early lesions is reduced by 20%, advanced lesions also tend do be detected less frequently. Due to consideration of a larger number of original studies and subjects, our meta-analysis demonstrates stronger effects of inadequate bowel preparation on early vs. advanced lesions which have not been apparent in a previous meta-analysis [16].
Our analysis was based on 21 studies summarizing 247,277 colonoscopies regarding overall detection of colonic lesions and 10 studies summarizing 122,958 colonoscopies regarding advanced lesions. Our and a previous meta-analysis [16] thus provide reliable estimates regarding the likelihood of missing adenoma and advanced adenomas.
In contrast, few studies addressed carcinoma detection in patients with low-quality bowel preparation. Endoscopists might feel assured that at least a cancer would have been detected but no direct evidence exist to back up such a claim. Carcinoma detection will likely be less effected than detection of advanced adenomas; however, the frequency of missed carcinoma cases remains unknown. Our study also identifies a lack of data regarding adenoma detection in the insufficiently prepared colon.
The risk of missing early and advanced adenomas has also been addressed by repeat-colonoscopy studies [12,21,23,29,31] (Table 3), which was consistently higher than for comparative studies. There are several explanations for this discrepancy: i) 8–35% of early and 5–10% of advanced adenomas are missed even in a perfectly prepared colon [21,32] and this baseline adenoma miss rate would need to be subtracted from the numbers in Table 3. ii) Only a fraction of all patients eligible for repeat colonoscopy effectively underwent a repeat endoscopy. This might constitute a strong selection bias for high-risk patients. iii) Some studies reported a significant time interval between the first and second colonoscopy, allowing new lesions to appear. Comparing to repeat-colonoscopy studies, results of comparative studies were more homogenous, supported by a larger number of patients and individual studies, and seem to have higher credibility at least for patients at average risk.
After screening colonoscopy with low-quality preparation many gastroenterologists recommend an early repeat-colonoscopy [33]. However, since a significant fraction of all colon lesions will have been detected and removed during the initial exam the cost-efficiency of an immediate second endoscopy will be strongly reduced. It should be noted that even with inadequate preparation considerable efficacy of colonoscopy remains: Inadequate preparation reduces detection of overall lesions by 47% and advanced lesions by only 26%. In our opinion, our results thus argue for a repeat-colonoscopy after a delay of several years. Ultimately a cost-effectiveness analysis considering effects on both, early and advanced lesions will be needed to determine the optimal time interval of a re-colonoscopy. Clearly, different considerations apply to a symptomatic patient with a high pre-test probability of advanced lesions as these patients will likely benefit from an immediate second exam. In one repeat-colonoscopy study all patients with carcinoma that were missed in the initial colonoscopy were symptomatic patients [23].
It has been suggested that colon preparation disproportionally affects detection of flat, serrated and/or right-sided adenomas as these preferentially reside in the right colon [34] and are more difficult to detect by colonoscopy [14,15]. Therefore, these lesions might be responsible for a significant fraction of right-sided interval carcinomas. However, in our analysis the majority of all comparative studies did not find significantly diverging detection rates for adenoma subtypes in patients with different qualities of bowel preparation. In contrast, a number of small repeat colonoscopy studies described lower detection rates of right-sided lesions in a poorly prepared colon. This discrepancy might be explained by the strong selection bias in repeat colonoscopy studies with only a small fraction of all included patients undergoing repeat examinations. In addition, a long time interval (>1 year) between the index and repeat exam would favor fast growing lesions and growth rates of right-sided/flat/serrated might differ compared to pedunculated adenomas. However, one large tandem colonoscopy study described a more than 4-fold higher chance of missing a flat compared to a penduculated adenoma suggesting that detection rate differs if the analysis focuses on endoscopic appearance rather than histology or location within the colon [30]. More data are clearly needed to answer this important question.
The predictive value of preparation quality for reduction of adenoma detection will depend on inter- and intraobserver agreement as well as validity of the scale used for the description of bowel preparation. The Aronchick scale was the first scale for standardized assessment of bowel preparation [17,35]. BBPS uses similar wording as the Aronchick scale but combines 4 qualities of 3 colon segments to a single score (0–9). For BBPS online training material is available (http://www.cori.org/bbps/). The Ottawa and Chicago scale also provide semi-quantitative measurements for bowel preparation [36]. However, these scales cannot be directly converted to the Aronchick or BBPS scale since preparation quality is evaluated after sucking away all liquid material and fluid in the colon is also penalized.
Internal validation of preparation quality has not been done in most of the included studies. However, after several training sessions near-perfect interrater agreement can be achieved for BBPS [18,33,37] as well as Aronchick scale and Chicago scale [36]. In clinical practice, quality of bowel preparation should be reported for each colonoscopy as suggested by several guidelines but reporting of bowel preparation in daily practice is sometimes incomplete or suboptimal [38,39].
Our analysis has some limitations: i) The literature research was restricted to publications in English. ii) Bowel preparation has not been uniformly evaluated by a standardized scale with frequent usage of unique preparation scales. In these cases transformation to the Aronchick scale leaves some ambiguity. Moreover, most studies did not perform internal validation of the respective preparation scale. iii), while robust data could be retrieved regarding overall detection of lesions for fair and poor bowel preparation, few data exist regarding insufficient bowel preparation and detection of advanced lesions at the lower end of the preparation scale. Finally, most of the studies did not report or remained underpowered to detect enough CRC to make reliable predictions regarding missed carcinomas after low-quality preparation.
In conclusion our analysis demonstrates a stronger drop in early vs. advanced adenoma detection in the inadequately prepared colon. Therefore, considerable efficacy of colonoscopy even with inadequate bowel preparation remains since the majority of advanced lesions will still be detected. Therefore, cost-effectiveness studies will be needed to determine the best strategy for repeat-endoscopy in this situation.
Supporting Information
(TIFF)
(TIFF)
(TIF)
(PDF)
This analysis was performed using several sub-studies with different inclusion criteria. The table shows the analyses on the studies reporting the ORs for suboptimal vs. optimal bowel preparation, considering any adenoma + any polyp.
(DOC)
This table shows the analyses on the studies reporting the odds for inadequate vs. adequate bowel preparation, considering advanced adenomas + advanced polyps.
(DOC)
Abbreviations
- ADR
Adenoma detection rate
- Adv ADR
Advanced adenoma detection rate
- BBPS
Boston bowel preparation scale
- CRC
Colorectal cancer
- CI
Confidence intervals
- N.s.
not significant
- OR
Odds Ratio
- SDR
serrated adenoma detection rate
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was funded by the Swiss Cancer League (KFS-2977-08-2012) and the Horten Foundation.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61: 69–90. 10.3322/caac.20107 . [DOI] [PubMed] [Google Scholar]
- 2.Brenner H, Kloor M, Pox CP. Colorectal cancer. The Lancet. 2014; 383: 1490–502. 10.1016/S0140-6736(13)61649-9 . [DOI] [PubMed] [Google Scholar]
- 3.Atkin WS, Edwards R, Kralj-Hans I, Wooldrage K, Hart AR, Northover JM, et al. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: a multicentre randomised controlled trial. Lancet. 2010; 375: 1624–33. 10.1016/S0140-6736(10)60551-X . [DOI] [PubMed] [Google Scholar]
- 4.Manser CN, Bachmann LM, Brunner J, Hunold F, Bauerfeind P, Marbet UA. Colonoscopy screening markedly reduces the occurrence of colon carcinomas and carcinoma-related death: a closed cohort study. Gastrointest Endosc. 2012; 76: 110–7. 10.1016/j.gie.2012.02.040 . [DOI] [PubMed] [Google Scholar]
- 5.Elmunzer BJ, Singal AG, Sussman JB, Deshpande AR, Sussman DA, Conte ML, et al. Comparing the effectiveness of competing tests for reducing colorectal cancer mortality: a network meta-analysis. Gastrointest Endosc. 2015; 81: 700–9 e3 10.1016/j.gie.2014.10.033 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levin B, Lieberman DA, McFarland B, Andrews KS, Brooks D, Bond J, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008; 134: 1570–95. 10.1053/j.gastro.2008.02.002 . [DOI] [PubMed] [Google Scholar]
- 7.Shergill AK, Conners EE, McQuaid KR, Epstein S, Ryan JC, Shah JN, et al. Protective association of colonoscopy against proximal and distal colon cancer and patterns in interval cancer. Gastrointest Endosc. 2015; 82: 529–37. 10.1016/j.gie.2015.01.053 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baxter NN, Sutradhar R, Forbes SS, Paszat LF, Saskin R, Rabeneck L. Analysis of administrative data finds endoscopist quality measures associated with postcolonoscopy colorectal cancer. Gastroenterology. 2011; 140: 65–72. 10.1053/j.gastro.2010.09.006 [DOI] [PubMed] [Google Scholar]
- 9.Kaminski MF, Regula J, Kraszewska E, Polkowski M, Wojciechowska U, Didkowska J, et al. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med. 2010; 362: 1795–803. [DOI] [PubMed] [Google Scholar]
- 10.Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med. 2014; 370: 1298–306. 10.1056/NEJMoa1309086 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rembacken B, Hassan C, Riemann JF, Chilton A, Rutter M, Dumonceau JM, et al. Quality in screening colonoscopy: position statement of the European Society of Gastrointestinal Endoscopy (ESGE). Endoscopy. 2012; 44: 957–68. 10.1055/s-0032-1325686 . [DOI] [PubMed] [Google Scholar]
- 12.Lebwohl B, Kastrinos F, Glick M, Rosenbaum AJ, Wang T, Neugut AI. The impact of suboptimal bowel preparation on adenoma miss rates and the factors associated with early repeat colonoscopy. Gastrointest Endosc. 2011; 73: 1207–14. 10.1016/j.gie.2011.01.051 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harewood GC, Sharma VK, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc. 2003; 58: 76–9. . [DOI] [PubMed] [Google Scholar]
- 14.Tadros M, Anderson JC. Serrated polyps: clinical implications and future directions. Curr Gastroenterol Rep. 2013;15:342 10.1007/s11894-013-0342-4 . [DOI] [PubMed] [Google Scholar]
- 15.Gupta S, Balasubramanian BA, Fu T, Genta RM, Rockey DC, Lash R. Polyps with advanced neoplasia are smaller in the right than in the left colon: implications for colorectal cancer screening. Clin Gastroenterol Hepatol. 2012; 10: 1395–401 e2 10.1016/j.cgh.2012.07.004 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clark BT, Rustagi T, Laine L. What level of bowel prep quality requires early repeat colonoscopy: systematic review and meta-analysis of the impact of preparation quality on adenoma detection rate. Am J Gastroenterol. 2014; 109: 1714–23; 10.1038/ajg.2014.232 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aronchick C. Validation of an instrument to assess colon cleansing [abstract]. Am J Gastroenterol. 1999; 94: 2667. [Google Scholar]
- 18.Lai EJ, Calderwood AH, Doros G, Fix OK, Jacobson BC. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc. 2009; 69: 620–5. 10.1016/j.gie.2008.05.057 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holt EW, Yimam KK, Ma H, Shaw RE, Sundberg RA, Verhille MS. Patient tolerability of bowel preparation is associated with polyp detection rate during colonoscopy. J Gastrointestin Liver Dis. 2014; 23: 135–40. . [DOI] [PubMed] [Google Scholar]
- 20.Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS One. 2013; 8:e76654 10.1371/journal.pone.0076654 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hong SN, Sung IK, Kim JH, Choe WH, Kim BK, Ko SY, et al. The Effect of the Bowel Preparation Status on the Risk of Missing Polyp and Adenoma during Screening Colonoscopy: A Tandem Colonoscopic Study. Clin Endosc. 2012; 45: 404–11. 10.5946/ce.2012.45.4.404 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Froehlich F, Wietlisbach V, Gonvers JJ, Burnand B, Vader JP. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: the European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study. Gastrointest Endosc. 2005; 61: 378–84. . [DOI] [PubMed] [Google Scholar]
- 23.Singhal S, Virk MA, Momeni M, Krishnaiah M, Anand S. Impact of bowel preparation on surveillance colonoscopy interval. Scand J Gastroenterol. 2014;49:885–90. 10.3109/00365521.2014.915055 . [DOI] [PubMed] [Google Scholar]
- 24.de Wijkerslooth TR, Stoop EM, Bossuyt PM, Tytgat KM, Dees J, Mathus-Vliegen EM, et al. Differences in proximal serrated polyp detection among endoscopists are associated with variability in withdrawal time. Gastrointest Endosc. 2013; 77: 617–23. 10.1016/j.gie.2012.10.018 . [DOI] [PubMed] [Google Scholar]
- 25.Anderson JC, Butterly LF, Robinson CM, Goodrich M, Weiss JE. Impact of fair bowel preparation quality on adenoma and serrated polyp detection: data from the New Hampshire colonoscopy registry by using a standardized preparation-quality rating. Gastrointest Endosc. 2014; 80: 463–70. 10.1016/j.gie.2014.03.021 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jover R, Zapater P, Polania E, Bujanda L, Lanas A, Hermo JA, et al. Modifiable endoscopic factors that influence the adenoma detection rate in colorectal cancer screening colonoscopies. Gastrointest Endosc. 2013; 77: 381–9 e1 10.1016/j.gie.2012.09.027 . [DOI] [PubMed] [Google Scholar]
- 27.Bryant RV, Schoeman SN, Schoeman MN. Shorter preparation to procedure interval for colonoscopy improves quality of bowel cleansing. Intern Med J. 2013; 43: 162–8. 10.1111/j.1445-5994.2012.02963.x . [DOI] [PubMed] [Google Scholar]
- 28.Kim EJ, Park YI, Kim YS, Park WW, Kwon SO, Park KS, et al. A Korean experience of the use of Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Saudi J Gastroenterol. 2014; 20: 219–24. 10.4103/1319-3767.136950 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chokshi RV, Hovis CE, Hollander T, Early DS, Wang JS. Prevalence of missed adenomas in patients with inadequate bowel preparation on screening colonoscopy. Gastrointest Endosc. 2012; 75: 1197–203. 10.1016/j.gie.2012.01.005 . [DOI] [PubMed] [Google Scholar]
- 30.Xiang L, Zhan Q, Zhao XH, Wang YD, An SL, Xu YZ, et al. Risk factors associated with missed colorectal flat adenoma: a multicenter retrospective tandem colonoscopy study. World J Gastroenterol. 2014; 20: 10927–37. 10.3748/wjg.v20.i31.10927 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Menees SB, Kim HM, Elliott EE, Mickevicius JL, Graustein BB, Schoenfeld PS. The impact of fair colonoscopy preparation on colonoscopy use and adenoma miss rates in patients undergoing outpatient colonoscopy. Gastrointest Endosc. 2013; 78: 510–6. 10.1016/j.gie.2013.03.1334 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Rijn JC, Reitsma JB, Stoker J, Bossuyt PM, van Deventer SJ, Dekker E. Polyp miss rate determined by tandem colonoscopy: a systematic review. Am J Gastroenterol. 2006; 101: 343–50. . [DOI] [PubMed] [Google Scholar]
- 33.Calderwood AH, Jacobson BC. Comprehensive validation of the Boston Bowel Preparation Scale. Gastrointest Endosc. 2010; 72: 686–92. 10.1016/j.gie.2010.06.068 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Okamoto M, Kawabe T, Yamaji Y, Kato J, Ikenoue T, Togo G, et al. Flat-Type Early Colorectal Cancer Preferentially Develops in Right-Sided Colon in Older Patients. Diseases of the Colon & Rectum. 2005; 48: 101–7. . [DOI] [PubMed] [Google Scholar]
- 35.Aronchick CA, Lipshutz WH, Wright SH, Dufrayne F, Bergman G. A novel tableted purgative for colonoscopic preparation: efficacy and safety comparisons with Colyte and Fleet Phospho-Soda. Gastrointest Endosc. 2000; 52: 346–52. . [DOI] [PubMed] [Google Scholar]
- 36.Gerard DP, Foster DB, Raiser MW, Holden JL, Karrison TG. Validation of a new bowel preparation scale for measuring colon cleansing for colonoscopy: the chicago bowel preparation scale. Clin Transl Gastroenterol. 2013;4:e43 10.1038/ctg.2013.16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gao Y, Lin JS, Zhang HD, Lin MX, Cheng CS, Wu SZ. Pilot validation of the Boston Bowel Preparation Scale in China. Dig Endosc. 2013;25:167–73. 10.1111/j.1443-1661.2012.01356.x . [DOI] [PubMed] [Google Scholar]
- 38.Li J, Nadel MR, Poppell CF, Dwyer DM, Lieberman DA, Steinberger EK. Quality assessment of colonoscopy reporting: results from a statewide cancer screening program. Diagn Ther Endosc. 2010; 2010 pii: 419796 10.1155/2010/419796 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Jonge V, Sint Nicolaas J, Cahen DL, Moolenaar W, Ouwendijk RJ, Tang TJ, et al. Quality evaluation of colonoscopy reporting and colonoscopy performance in daily clinical practice. Gastrointest Endosc. 2012; 75: 98–106. 10.1016/j.gie.2011.06.032 . [DOI] [PubMed] [Google Scholar]
- 40.Calderwood AH, Schroy PC 3rd, Lieberman DA, Logan JR, Zurfluh M, Jacobson BC. Boston Bowel Preparation Scale scores provide a standardized definition of adequate for describing bowel cleanliness. Gastrointest Endosc. 2014; 80: 269–76. 10.1016/j.gie.2014.01.031 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee TJ, Rees CJ, Blanks RG, Moss SM, Nickerson C, Wright KC, et al. Colonoscopic factors associated with adenoma detection in a national colorectal cancer screening program. Endoscopy. 2014; 46: 203–11. 10.1055/s-0033-1358831 . [DOI] [PubMed] [Google Scholar]
- 42.Fayad NF, Kahi CJ, Abd El-Jawad KH, Shin AS, Shah S, Lane KA, et al. Association between body mass index and quality of split bowel preparation. Clin Gastroenterol Hepatol. 2013; 11: 1478–85. 10.1016/j.cgh.2013.05.037 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Adler A, Wegscheider K, Lieberman D, Aminalai A, Aschenbeck J, Drossel R, et al. Factors determining the quality of screening colonoscopy: a prospective study on adenoma detection rates, from 12,134 examinations (Berlin colonoscopy project 3, BECOP-3). Gut. 2013; 62: 236–41. 10.1136/gutjnl-2011-300167 . [DOI] [PubMed] [Google Scholar]
- 44.Goncalves AR, Ferreira C, Marques A, Ribeiro LC, Velosa J. Assessment of quality in screening colonoscopy for colorectal cancer. Clin Exp Gastroenterol. 2011; 4: 277–81. 10.2147/CEG.S25596 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sherer EA, Imler TD, Imperiale TF. The effect of colonoscopy preparation quality on adenoma detection rates. Gastrointest Endosc. 2012; 75: 545–53. 10.1016/j.gie.2011.09.022 . [DOI] [PubMed] [Google Scholar]
- 46.Enestvedt BK, Brian Fennerty M, Zaman A, Eisen GM. MiraLAX vs. Golytely: is there a significant difference in the adenoma detection rate? Aliment Pharmacol Ther. 2011; 34: 775–82. 10.1111/j.1365-2036.2011.04795.x . [DOI] [PubMed] [Google Scholar]
- 47.Shaukat A, Oancea C, Bond JH, Church TR, Allen JI. Variation in detection of adenomas and polyps by colonoscopy and change over time with a performance improvement program. Clin Gastroenterol Hepatol. 2009; 7: 1335–40. 10.1016/j.cgh.2009.07.027 . [DOI] [PubMed] [Google Scholar]
- 48.Radaelli F, Meucci G, Sgroi G, Minoli G, Italian Association of Hospital G. Technical performance of colonoscopy: the key role of sedation/analgesia and other quality indicators. Am J Gastroenterol. 2008; 103: 1122–30. [DOI] [PubMed] [Google Scholar]
- 49.Pontone S, Leonetti G, Lamazza A, Fiocca F, Filippini A, Fanello G, et al. A Retrospective Case-Control Study Evaluating the Bowel Preparation Quality during Surveillance Colonoscopy after Colonic Resection. ISRN Gastroenterol. 2014; 2014:681978 10.1155/2014/681978 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Aslanian HR, Shieh FK, Chan FW, Ciarleglio MM, Deng Y, Rogart JN, et al. Nurse observation during colonoscopy increases polyp detection: a randomized prospective study. Am J Gastroenterol. 2013; 108: 166–72. 10.1038/ajg.2012.237 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIFF)
(TIFF)
(TIF)
(PDF)
This analysis was performed using several sub-studies with different inclusion criteria. The table shows the analyses on the studies reporting the ORs for suboptimal vs. optimal bowel preparation, considering any adenoma + any polyp.
(DOC)
This table shows the analyses on the studies reporting the odds for inadequate vs. adequate bowel preparation, considering advanced adenomas + advanced polyps.
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.