Abstract
Background
The prevalence of BRCA1/2 variants in Chinese breast cancer patients varies among studies. Germline or somatic BRCA1/2 mutations are associated with sensitivity to poly(ADP-ribose) polymerase-1 inhibitors and DNA-damaging agents. We aimed to investigate the distribution of both somatic and germline BRCA1/2 variants in unselected Chinese breast cancer patients, and explore their roles in tumor phenotype and disease prognosis.
Methods
507 breast cancer patients, unselected for family history of breast cancer or age at diagnosis, were prospectively enrolled from West China Hospital between Feb. 2008 and Feb. 2014. BRCA1/2 variants in the exons/flanking regions were detected in fresh-frozen tumors using next-generation sequencing and confirmed by independent methods. Germline/somatic status was validated by Sanger sequencing in paired blood/normal tissue.
Results
BRCA1/2 pathogenic or likely pathogenic (P/LP) variants were detected in 50 patients (9.9%), including 40 germline carriers (18 in BRCA1, 22 in BRCA2), 9 patients with somatic variants (3 in BRCA1, 6 in BRCA2), and 1 patient with concurrent germline/somatic variants in BRCA2. The triple-negative (21.4%) and Luminal B (9.7%) subtypes had higher rates of BRCA1/2 variants. In patients with disease stage 0~II, presence of a germline or somatic BRCA1 P/LP variant increased the risk of relapse as compared to non-carriers [univariate hazard ratio (HR): 3.70, P = 0.04]. Germline BRCA1 P/LP variants, which were associated with aggressive tumor phenotypes, predicted worse disease-free survival in the subgroup of stage 0~II (HR: 4.52, P = 0.02) and N0 (HR: 5.4, P = 0.04) compared to non-carriers.
Conclusion
A high frequency of germline and somatic BRCA1/2 P/LP variants was detected in unselected Chinese breast cancer patients. Luminal B subtype should be considered as a high-risk population of BRCA1/2 mutation, in addition to triple-negative breast cancer. BRCA1 status was associated with aggressive tumor phenotype and worse disease progression in early stage breast cancer patients.
Introduction
Germline mutations in breast cancer susceptibility genes BRCA1 and BRCA2 confer a high risk of breast and ovarian cancer. At the age of 70 years old, the mean cumulative breast cancer risks for BRCA mutation carriers are 47%-66% (BRCA1) and 40%-57% (BRCA2) in western countries [1]. Around 25% of familial breast cancer (FBC) may be attributed to inherited mutations in BRCA1 and BRCA2 [2]. The prevalence of germline BRCA1/2 mutations in Chinese breast cancer patients varies among the previous studies (1.8%~18.2%)[3–5], largely due to differences in patient selection criteria, sensitivity and specificity of detection assays, and mutation calling methods. Therefore, the prevalence of BRCA1/2 mutation in unselected Chinese breast cancer patients has not been fully explored.
BRCA1 and BRCA2 play important roles in maintaining genome integrity by acting at different stages in the DNA damage response and DNA repair processes [6]. Recent clinical evidence showed that cancer patients with BRCA1/2 mutations (germline or somatic) were particularly sensitive to poly(ADP-ribose) polymerase inhibitors (PARPi)[7–8] and DNA damaging chemotherapy (e.g., platinum [9]). In a phase 2 trial, Ledermann and colleagues [10] reported that olaparib maintenance monotherapy significantly prolonged progression-free survival (PFS) in patients with platinum-sensitive recurrent serous ovarian cancer. Further subgroup analysis suggested that the patients with a germline or somatic BRCA1/2 mutation had the most profound benefit from olaparib, which significantly extended their median PFS by 6.9 months, as compared to 1.9 months increase in wild-type BRCA patients. Based on these findings, the European Medicines Agency (EMA) included both germline and somatic BRCA1/2 mutation patients with ovarian cancer for olaparib maintenance monotherapy. Other additional study of sporadic cancers with a somatically mutated BRCA gene showed the similar phenotype (BRCAness) to germline BRCA tumors, in terms of their treatment susceptibility to DNA-damaging agents [11]. Thus, it is equally important to detect germline and somatic BRCA mutations to identify the population that would most benefit from the DNA-damaging therapy.
In breast cancer patients, the relationship between BRCA status and prognosis was complex [12–14]. Triple-negative breast cancer patients carrying founder BRCA1 mutations were likely to had a decreased risk of distant recurrence and breast cancer-specific mortality compared to BRCA1 non-carriers [15]. On the other hand, a recent meta-analysis from 13 studies of 10,016 women with breast cancer [16] concluded that BRCA1 mutation carriers had a worse overall survival but similar progression-free survival, compared to non-carriers; while BRCA2 mutation was not associated with breast cancer prognosis.
In this single-center observational study, we aimed to investigate the prevalence of both somatic and germline BRCA1/2 variants in unselected Chinese breast cancer patients, and explore their role in tumor phenotype and disease prognosis. We evaluated the frequency of likely pathogenic or pathogenic BRCA1/2 variants in tumor tissues from 507 Chinese breast cancer patients using next generation sequencing (NGS). All these variants were subsequently confirmed in the tumors and the paired blood/normal tissues by Sanger sequencing or other methods. We further assessed the clinical characteristics of BRCA1 and BRCA2 carriers by germline/somatic status. The disease-free survival (DFS) and overall survival (OS) patterns for genetically different patients were also explored.
Materials and Methods
Study patients and samples
Patients pathologically diagnosed with breast cancer were prospectively registered in the Breast Cancer Information Management System (BCIMS) at West China Hospital, Sichuan University since 2008. Medical records, diagnostic pathology reports, treatments records were reviewed and collected by oncologists. All patients were followed by outpatient visit or telephone at 3 to 4-month intervals within 3 years after diagnosis, 6-month intervals within 4–5 years, and then annually. Between Feb. 2008 and Feb. 2014, there were a total of 5103 patients registered, about 600 to 900 new cases per year. The rate of loss to follow-up was around 10% and less than 5% in patients diagnosed between 2008~2009 and 2010~2014, respectively.
This study aimed to fully understand the distribution of BRCA1/2 gene variants, both somatic and germline, in unselected breast cancer patients, as well as their potential impact on disease prognosis. Among the registered patients, 4791 cases who had undergone surgery in the Department of Thyroid and Breast Surgery between Feb. 2008 and Feb. 2014, regardless of their family history of breast cancer or age at diagnosis, were recruited. However, 3779 patients who were unable to provide sufficient amount of frozen tumor tissue or didn’t have complete clinical information, were excluded from this study. Another 422 patients without the matched frozen distal adjacent normal tissue or peripheral blood were also excluded. The neoplastic cellularity of tumor tissue section from 83 patients didn’t meet the quality control criteria of 50% or greater tumor content. Finally, 507 patients were eligible for BRCA test and clinical characteristics analysis. Survival analysis was performed on 426 patients of stage 0~III, excluding 5 patients with stage IV, 4 patients with unspecified stage, and 72 patients with the variants of uncertain significance (VUS). This study was approved by the Clinical Test and Biomedical Ethics Committee of West China Hospital, Sichuan University. Written informed consent was provided by all the patients.
Targeted DNA sequencing and variant interpretation
Details of the comprehensive NGS workflow for testing and analyzing tumor BRCA1/2 variants were described in the S1 Method and our previous work [17]. Briefly, tumor DNA samples were screened for variants in all coding exons and the splice boundaries (-20/+10 bp) of BRCA1 and BRCA2 genes using NGS on a MiSeq system (Illumina, USA). All variant candidates were successfully validated in tumors using Sanger sequencing, or the MassARRAY system (Sequenom, USA), or long-range PCR. Somatic or germline status was confirmed by testing the paired blood or normal tissue sample using Sanger sequencing.
Germline variants were interpreted according to the American College of Medical Genetics and Genomics (ACMG) [18]. Briefly, variants that produce premature termination codons which are associated with non-functional or truncated proteins were classified as pathogenic (P) variants: such as nonsense mutations, frameshift mutations, splice site mutations and exonic deletions. Some missense mutations were considered as likely pathogenic (LP) variants based on available evidence indicating a strong likelihood of their association with disease. Variants with undetermined clinical significance were classified as VUS: such as novel point mutations, certain missense variants, and variants located in intronic regions. Similarly, inactivating somatic variants were considered as pathogenic variants: such as nonsense mutations and frameshift mutations, while somatic variants with uncertain clinical significance were considered as VUS: such as missense variants.
LOH analysis
The heterozygosity state of the BRCA1/2 pathogenic/likely pathogenic (P/LP) variants was determined by Sanger sequencing using the genomic DNA from tumors and paired blood/normal tissue. Loss of heterozygosity (LOH) in tumor was defined as the presence of heterozygosity in the blood/normal tissue, but not in the tumor. LOH analysis was performed in 40 patients carrying germline BRCA1/2 P/LP variants.
Clinical and survival data
Clinical and pathological characteristics of 507 patients were extracted from the BCIMS (S1 Table). Immunohistochemistry (IHC) scoring for estrogen receptor (ER), progesterone receptor (PR) was performed according to the Guidelines for Testing of ER and PR in Breast Cancer [19]; IHC and fluorescence in situ hybridization scoring for human epidermal growth factor receptor-2 (HER2) was conducted following the Guidelines for HER2 Detection in Breast Cancer[20]. Standard therapy was defined as administration of comprehensive therapy according to National Comprehensive Cancer Network Guidelines (NCCN, http://www.nccn.org) and St. Gallen International Expert Consensus[21]. In this study, 426 patients of stage 0~III were followed for up to seven years (median, 39.3 months). The last follow-up date was April 1, 2015. DFS was defined as the interval between surgery date and first relapse of cancer, breast cancer-related death, or last follow-up. OS was defined as the interval between surgery date and death as a result of disease, or last follow-up.
Statistical analysis
Comparison of clinical characteristics between patients with and without BRCA1/2 variants (non-carriers) was performed using two-tailed t-tests, Pearson Chi-Square tests, or Fisher’s exact tests as appropriate (SPSS version 20; SPSS, Chicago, IL). Missing data was not included in the analysis. Survival analyses were performed using univariate and multivariate Cox proportional hazards regression models (SPSS version 20). The log-rank test and Kaplan-Meier plots were used to visualize survival characteristics (STATA version 12; StataCorp, College Station, TX). A two-sided test P values < 0.05 were considered as statistically significant.
Results
Prevalence and characteristics of BRCA1/2 variants
The prevalence, classification and germline/somatic status of the BRCA1/2 variants identified in this cohort were summarized in Table 1. Among the 507 unselected breast cancer patients, 40 (7.9%) had a germline BRCA1/2 P/LP variant, and 9 (1.8%) had a somatic BRCA1/2 pathogenic variant. 1 (1.8%) patient had two pathogenic BRCA2 variants: 1 germline and 1 somatic. Thus, the total percentage of patients with germline or somatic BRCA1/2 P/LP variants was 9.9%.
Table 1. Distribution of germline or somatic BRCA1/2 variants in 507 breast cancer patients.
| Gene | Pathogenic/Likely pathogenic (P/LP) variant | Variant of uncertain significance (VUS) b | ||
|---|---|---|---|---|
| Patient No. | Percentage a | Patient No. | Percentage a | |
| Germline | ||||
| BRCA1 | 18 | 3.6% | 16 | 3.2% |
| BRCA2 | 22 | 4.3% | 43 | 8.5% |
| BRCA1 and BRCA2 concurrent | 0 | 0.0% | 3 | 0.6% |
| Subtotal | 40 | 7.9% | 62 | 12.2% |
| Somatic | ||||
| BRCA1 | 3 | 0.6% | 3 | 0.6% |
| BRCA2 | 6 | 1.2% | 5 | 1.0% |
| Subtotal | 9 | 1.8% | 8 | 1.6% |
| Germline and somatic concurrent | ||||
| BRCA1 | 0 | 0.0% | 0 | 0.0% |
| BRCA2 | 1 | 0.2% | 0 | 0.0% |
| BRCA1 and BRCA2 concurrent | 0 | 0.0% | 1 | 0.2% |
| Subtotal | 1 | 0.2% | 1 | 0.2% |
| Total | 50 | 9.9% | 71 | 14.0% |
a The percentage of carriers out of 507 breast cancer patients.
b One BRCA2 VUS was not listed in this table due to its unknown germline/somatic status.
The variant data has been submitted to NCBI ClinVar database (http://www.ncbi.nlm.nih.gov/clinvar/, Submission ID: SUB1362368, Submission name: Chinese507BC_BRCA).
Germline BRCA1/2 variants
Germline BRCA1 P/LP variants were simultaneously detected in tumors and paired blood/normal tissue from 18 (3.6%) patients, and the germline BRCA2 P/LP variants were found in 22 (4.3%) patients. Among them, LOH in tumor was identified in 11 (61.1%) BRCA1 carriers and 13 (59.1%) BRCA2 carriers, respectively. There are 39 unique germline P/LP variants in this cohort. Half of them (20/39) are novel, including 14 frameshift insertion/deletion, 4 nonsense mutation, 1 splice site mutation, and 1 missense mutation (S2 Table). Also, we found a BRCA1 founder mutation (c.981_982del), which was previously reported in Southern Chinese breast cancer patients [22]. In addition, 12.2% of the patients in this cohort had germline VUS in BRCA1/2 genes (Table 1 and S2 Table).
Next, we compared the clinical characteristics between 40 germline BRCA variants carriers and 385 non-carriers (Table 2). The BRCA1/2 carriers (mean±standard deviation: 46.6±8.5 years), especially BRCA2 (46.2±8.0 years), had an earlier onset age than non-carriers (50.7±10.3 years), which supports BRCA genes as potential cancer risk factors. The majority of BRCA1 (18/18) and BRCA2 (19/22) carriers were identified from the patients without family history of breast or ovarian cancer. The remaining 3 BRCA2 carriers were found among the 16 FBC patients.
Table 2. A comparison between clinical characteristics of germline BRCA1/2 variant carriers and non-carriers.
| Characteristics | Non-carriers No. (n = 385) | Germline BRCA1/2 P/LP variants carriers No. (n = 40) | Germline BRCA1/2 VUS carriers No. (n = 62) | |||||
|---|---|---|---|---|---|---|---|---|
| BRCA1/2 (n = 40) | P a | BRCA1 (n = 18) | P a | BRCA2 (n = 22) | P a | |||
| Age at diagnosis (y, mean±SD) | 50.7±10.3 | 46.6±8.5 | 0.01 | 46.9±9.4 | 0.13 | 46.2±8.0 | 0.05 | 48.5±9.2 |
| Family history of breast cancer | ||||||||
| Yes | 12 | 3 | 0.16 | 0 | 1.00 | 3 | 0.04 | 1 |
| No | 373 | 37 | 18 | 19 | 61 | |||
| Menopause at diagnosis | ||||||||
| Postmenopause | 176 | 13 | 0.10 | 6 | 0.29 | 7 | 0.19 | 23 |
| Premenopause | 206 | 27 | 12 | 15 | 39 | |||
| Molecular subtype | ||||||||
| Luminal A | 49 | 1 | < 0.001 | 0 | < 0.001 | 1 | 0.41 | 10 |
| Luminal B | 218 | 21 | 4 | 17 | 35 | |||
| HER2+ | 57 | 1 | 0 | 1 | 8 | |||
| TN | 48 | 14 | 11 | 3 | 6 | |||
| ER-PR+ | 13 | 3 | 3 | 0 | 3 | |||
| ER | ||||||||
| Positive (>1%) | 274 | 22 | 0.03 | 4 | < 0.001 | 18 | 0.28 | 47 |
| Negative | 111 | 18 | 14 | 4 | 15 | |||
| PR | ||||||||
| Positive (>1%) | 266 | 22 | 0.07 | 6 | 0.002 | 16 | 0.72 | 43 |
| Negative | 119 | 18 | 12 | 6 | 19 | |||
| Ki67 | ||||||||
| <14% | 68 | 1 | 0.01 | 0 | 0.05 | 1 | 0.15 | 12 |
| ≥14% | 315 | 39 | 18 | 21 | 50 | |||
| HER2 | ||||||||
| Positive | 130 | 2 | < 0.001 | 0 | 0.003 | 2 | 0.02 | 18 |
| Negative | 255 | 38 | 18 | 20 | 44 | |||
| Histology | ||||||||
| DCIS | 3 | 0 | 0.05 | 0 | 0.34 | 0 | 0.28 | 2 |
| Invasive ductal carcinoma | 341 | 40 | 18 | 22 | 53 | |||
| Other Invasive carcinomas | 41 | 0 | 0 | 0 | 7 | |||
| Histological grade | ||||||||
| I/II | 126 | 8 | 0.06 | 1 | 0.01 | 7 | 0.73 | 25 |
| III | 230 | 31 | 16 | 15 | 33 | |||
| T | ||||||||
| Tis/T1 | 128 | 11 | 0.76 | 4 | 0.70 | 7 | 1.00 | 20 |
| T2 | 227 | 26 | 13 | 13 | 36 | |||
| T3 | 17 | 1 | 1 | 0 | 3 | |||
| T4 | 11 | 0 | 0 | 0 | 3 | |||
| No. of lymph node involvement | ||||||||
| 0 | 166 | 22 | 0.28 | 11 | 0.32 | 11 | 0.71 | 33 |
| 1~3 | 133 | 10 | 4 | 6 | 22 | |||
| ≥4 | 85 | 7 | 3 | 4 | 7 | |||
| M | ||||||||
| M0 | 381 | 38 | 0.07 | 16 | 0.02 | 22 | 1.00 | 62 |
| M1 | 3 | 2 | 2 | 0 | 0 | |||
| Clinical stage | ||||||||
| 0/I | 60 | 7 | 0.13 | 2 | 0.04 | 5 | 0.62 | 12 |
| II | 227 | 22 | 11 | 11 | 40 | |||
| III | 93 | 7 | 3 | 4 | 10 | |||
| VI | 3 | 2 | 2 | 0 | 0 | |||
| Standard therapy | ||||||||
| Yes | 15 | 2 | 0.67 | 0 | 1.00 | 2 | 0.23 | 4 |
| No | 370 | 38 | 18 | 20 | 58 | |||
a P-value calculated comparing with non-carriers by two-tailed t-tests, Pearson Chi-Square tests, or Fisher's Exact tests as appropriate. Unknown data were not included in the analysis.
Among different molecular subtypes, germline BRCA1/2 P/LP variants were preferentially detected in the patients with triple-negative (14/70; 20.0%) and Luminal B (21/290; 7.2%) breast cancer, as compared to the patients of Luminal A (1/60; 1.7%) and HER2 positive (1/67; 1.5%). Interestingly, we found that in TNBC subtype, 11 out of the 14 patients with BRCA1/2 P/LP variants were BRCA1 carriers. Vice Versa in Lumina B subtype, 17 out of the 21 patients with BRCA1/2 P/LP variants were BRCA2 carriers. BRCA1 carriers were more likely associated with ER negative (77.7% vs. 28.8%, P<0.001), PR negative (66.7% vs. 30.9%, P = 0.002), HER2 negative (100.0% vs. 66.2%, P = 0.003), and Ki67 overexpression (100.0% vs. 82.2%, P = 0.05) as compared to non-carriers.
Furthermore, we found that BRCA1 carriers had a higher chance of the histological grade III tumors than non-carriers. Metastasis at diagnosis was found in 2 patients of the 16 BRCA1 carriers, again significantly higher than that of non-carriers (3/384). In addition, all the germline BRCA1/2 P/LP variants were found in the patients with invasive ductal carcinoma. No significant differences were found in tumor size, lymph node involvement, or menopause at diagnosis.
Somatic BRCA1/2 variants
9 somatic pathogenic variants were detected in tumors, which didn’t appear in paired blood/normal tissues: 3 (0.6%) in BRCA1 gene and 6 (1.2%) in BRCA2 gene. Among those 9 unique variants, 4 frameshift insertion/deletions are novel (S2 Table). Only 1.6% of the 507 patients had somatic VUS in BRCA1/2 genes (Table 1 and S2 Table).
In addition, patients with somatic BRCA1/2 P variants were all HER-2 negative (P = 0.03; Table 3), but had no significant differences in other clinical characteristics, compared to non-carriers.
Table 3. A comparison between clinical characteristics of patients with somatic BRCA1/2 variants and non-carriers.
| Characteristics | Non-carriers No. (n = 385) | No. of patients with somatic BRCA1/2 P variants (n = 9) | No. of patients with Somatic BRCA1/2 VUS (n = 8) | |||||
|---|---|---|---|---|---|---|---|---|
| BRCA1/2 (n = 9) | P a | BRCA1 (n = 3) | P a | BRCA2 (n = 6) | P a | |||
| Age at diagnosis (y, mean±SD) | 50.7±10.3 | 49.7±10.4 | 0.77 | 42.0±12.1 | 0.15 | 53.5±7.9 | 0.51 | 51.5±6.0 |
| Family history of breast cancer | ||||||||
| Yes | 12 | 0 | 1.00 | 0 | 1.00 | 0 | 1.00 | 0 |
| No | 373 | 9 | 3 | 6 | 8 | |||
| Menopause at diagnosis | ||||||||
| Postmenopause | 176 | 5 | 0.74 | 1 | 1.00 | 4 | 0.42 | 4 |
| Premenopause | 206 | 4 | 2 | 2 | 4 | |||
| Molecular subtype | ||||||||
| Luminal A | 49 | 0 | 0.29 | 0 | 0.11 | 0 | 0.63 | 0 |
| Luminal B | 218 | 7 | 1 | 6 | 7 | |||
| HER2+ | 57 | 0 | 0 | 0 | 0 | |||
| TN | 48 | 1 | 1 | 0 | 1 | |||
| ER-PR+ | 13 | 1 | 1 | 0 | 0 | |||
| ER | ||||||||
| Positive(>1%) | 274 | 7 | 1.00 | 1 | 0.20 | 6 | 0.19 | 7 |
| Negative | 111 | 2 | 2 | 0 | 1 | |||
| PR | ||||||||
| Positive(>1%) | 266 | 7 | 0.73 | 2 | 1.00 | 5 | 0.67 | 5 |
| Negative | 119 | 2 | 1 | 1 | 3 | |||
| Ki67 | ||||||||
| <14% | 68 | 2 | 0.67 | 1 | 0.45 | 1 | 1.00 | 0 |
| ≥14% | 315 | 7 | 2 | 5 | 8 | |||
| HER2 | ||||||||
| Positive | 130 | 0 | 0.03 | 0 | 0.55 | 0 | 0.18 | 2 |
| Negative | 255 | 9 | 3 | 6 | 6 | |||
| Histology | ||||||||
| DCIS | 3 | 0 | 1.00 | 0 | 1.00 | 0 | 0.52 | 0 |
| Invasive ductal carcinoma | 341 | 8 | 3 | 5 | 8 | |||
| Other Invasive carcinomas | 41 | 1 | 0 | 1 | 0 | |||
| Histological grade | ||||||||
| I/II | 126 | 2 | 0.50 | 1 | 1.00 | 1 | 0.67 | 2 |
| III | 230 | 7 | 2 | 5 | 6 | |||
| T | ||||||||
| Tis/T1 | 128 | 0 | 0.10 | 0 | 0.65 | 0 | 0.30 | 1 |
| T2 | 227 | 9 | 3 | 6 | 7 | |||
| T3 | 17 | 0 | 0 | 0 | 0 | |||
| T4 | 11 | 0 | 0 | 0 | 0 | |||
| No. of lymph node involvement | ||||||||
| 0 | 166 | 4 | 0.56 | 2 | 0.45 | 2 | 0.77 | 2 |
| 1~3 | 133 | 2 | 0 | 2 | 2 | |||
| ≥4 | 85 | 3 | 1 | 2 | 4 | |||
| M | ||||||||
| M0 | 381 | 9 | 1.00 | 3 | 1.00 | 6 | 1.00 | 8 |
| M1 | 3 | 0 | 0 | 0 | 0 | |||
| Clinical stage | ||||||||
| 0/I | 60 | 0 | 0.48 | 0 | 1.00 | 0 | 0.74 | 1 |
| II | 227 | 6 | 2 | 4 | 3 | |||
| III | 93 | 3 | 1 | 2 | 4 | |||
| VI | 3 | 0 | 0 | 0 | 0 | |||
| Standard therapy | ||||||||
| Yes | 370 | 38 | 0.67 | 18 | 1.00 | 20 | 0.23 | 58 |
| No | 15 | 2 | 0 | 2 | 4 | |||
a P-value calculated comparing with non-carriers by two-tailed t-tests and Fisher's Exact tests as appropriate. Unknown data were not included in the analysis.
Association of BRCA1/2 P/LP variants with survival
Survival analysis was conducted among 426 patients of stage 0~III, including 19 BRCA1 carriers (16 germline, 3 somatic), 27 BRCA2 carriers (20 germline, 6 somatic, 1 concurrent) and 380 non-carriers. The standard comprehensive therapy patterns were similar between BRCA1/2 carriers and non-carriers (Tables 2 and 3). In BRCA1 group, relapse occurred in 3 germline carriers, and no death were reported; while no relapse or death occurred in the BRCA2 group during the follow-up period. In the non-carriers group, 35 relapses and 20 deaths occurred.
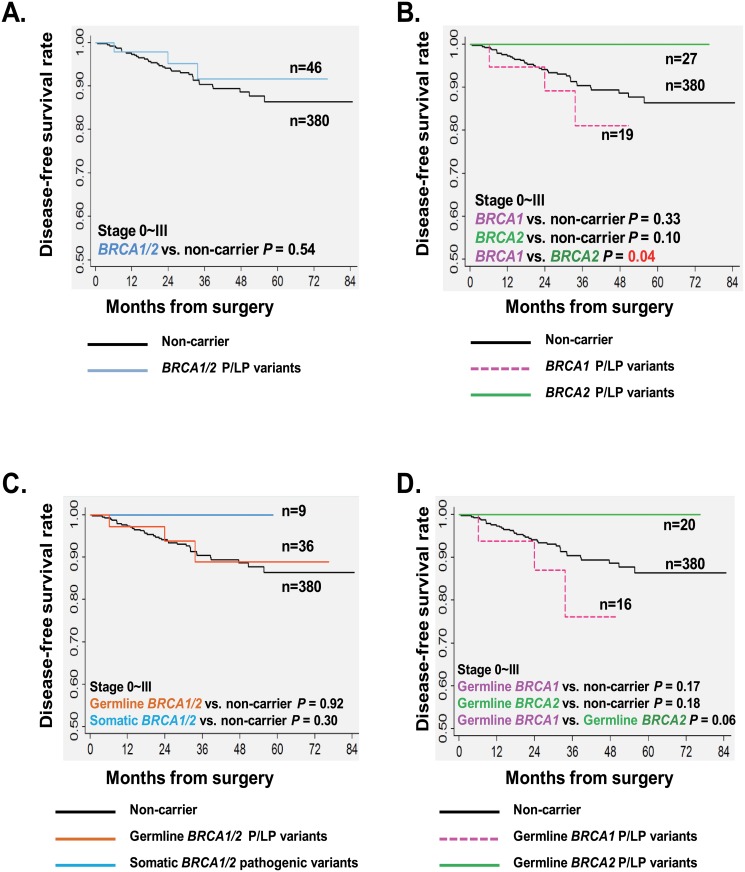
Disease-free survival of stage 0~III patients
As shown in Fig 1A, the stage 0~III patients with a germline or somatic BRCA1/2 P/LP variant had a similar estimated 3-year DFS rate with non-carriers (91.7%±4.7% vs. 90.4%±1.7%; log-rank P = 0.54). Interestingly, BRCA1 carriers (germline or somatic) had an inferior 3-year DFS rate than BRCA2 carriers (81.1%±10.2% vs. 100%; log-rank P = 0.04; Fig 1B). In univariate Cox proportional hazards regression models, the presence of a germline or somatic BRCA1/2 variant was not associated with DFS [hazard ratio (HR) for BRCA1/2 = 0.69, P = 0.54; HR for BRCA1 = 1.78, P = 0.34; HR for BRCA2 = 0, P = 0.98; Table 4]. Instead, postmenopause (HR = 2.22, P = 0.02), and higher tumor grade (HR for grade III = 3.54, P = 0.008) predicted high risks of relapse; while early disease stages predicted lower risks of relapse (HR for stage 0/I = 0.15, P = 0.01; HR for stage II = 0.39, P = 0.004; Table 4).
Fig 1. Impact of BRCA1/2 P/LP variants on the DFS of BC patients with stage 0~III.
Kaplan-Meier survival analysis; P values calculated using a log-rank analysis. Estimated DFS of breast cancer patients with stage 0~III by BRCA status: (A) BRCA1/2 P/LP variants (germline or somatic); (B) BRCA1 and BRCA2 P/LP variants (germline or somatic); (C) Germline and somatic BRCA1/2 P/LP variants; (D) Germline BRCA1 and germline BRCA2 P/LP variants.
Table 4. Impact of BRCA1/2 P/LP variants and other variables on the DFS and OS of breast cancer patients (Stage 0~III).
| Variables | DFS | OS | ||||
|---|---|---|---|---|---|---|
| #Cases (events) | HR (95% CI) a | P | #Cases (deaths) | HR (95% CI) a | P | |
| Germline and somatic combined variants | ||||||
| Non-carrier | 380 (35) | 1 | 380 (20) | 1 | ||
| BRCA1/2 | 46 (3) | 0.69 (0.21–2.25) | 0.54 | 46 (0) | 0 | 0.30 |
| BRCA1 | 19 (3) | 1.78 (0.55–5.81) | 0.34 | 19 (0) | 0 | 0.51 |
| BRCA2 | 27 (0) | 0 | 0.98 | 27 (0) | 0 | 0.42 |
| Germline variants | ||||||
| Non-carrier | 380 (35) | 1 | 380 (20) | 1 | ||
| BRCA1/2 | 36 (3) | 0.94 (0.29–3.06) | 0.92 | 36 (0) | 0 | 0.37 |
| BRCA1 | 16 (3) | 2.22 (0.68–7.26) | 0.19 | 16 (0) | 0 | 0.55 |
| BRCA2 | 20 (0) | 0 | 0.97 | 20 (0) | 0 | 0.50 |
| Somatic variants | ||||||
| Non-carrier | 380 (35) | 1 | 380 (20) | 1 | ||
| BRCA1/2 | 9 (0) | 0 | 0.49 | 9 (0) | 0 | 0.60 |
| Age at diagnosis | 426 (38) | 1.01 (0.98–1.05) | 0.38 | 426 (20) | 1.03 (0.99–1.08) | 0.11 |
| Menopause at diagnosis | ||||||
| Postmenopause | 188 (24) | 2.22 (1.15–4.29) | 0.02 | 188 (15) | 3.81 (1.38–10.49) | 0.01 |
| Premenopause | 235 (14) | 1 | 235 (5) | 1 | ||
| Molecular subtype | ||||||
| Luminal A | 49 (2) | 0.28 (0.06–1.3) | 0.10 | 49 (1) | 0.26 (0.03–2.34) | 0.23 |
| Luminal B | 241 (16) | 0.48 (0.21–1.12) | 0.09 | 241 (8) | 0.46 (0.14–1.53) | 0.20 |
| HER2+ | 59 (8) | 1.00 (0.37–2.66) | 1.00 | 59 (4) | 0.95 (0.24–3.83) | 0.95 |
| TN | 60 (8) | 1 | 60 (4) | 1 | ||
| ER-PR+ | 17 (4) | 1.9 (0.57–6.31) | 0.30 | 17 (3) | 2.62 (0.58–11.75) | 0.21 |
| Histological grade | ||||||
| I/II | 133 (5) | 1 | 133 (3) | 1 | ||
| III | 264 (33) | 3.54 (1.38–9.07) | 0.008 | 264 (17) | 2.92 (0.86–9.99) | 0.09 |
| Clinical stage | ||||||
| 0/I | 67 (2) | 0.15 (0.04–0.67) | 0.01 | 67 (0) | 0 | 0.96 |
| II | 256 (18) | 0.39 (0.2–0.74) | 0.004 | 256 (8) | 0.26 (0.11–0.64) | 0.003 |
| III | 103 (18) | 1 | 103 (12) | 1 | ||
| Standard therapy | ||||||
| No | 16 (3) | 1 | 16 (2) | 1 | ||
| Yes | 410 (35) | 0.32 (0.1–1.03) | 0.06 | 410 (18) | 0.22 (0.05–0.97) | 0.05 |
a Univariate Cox proportional hazards regression models
Next, we investigated the impact of the germline and somatic variants separately. Interestingly, the germline BRCA1 carriers showed a lower 3-year DFS rate than the germline BRCA2 carriers (76.2%±12.6% vs. 100%; log-rank P = 0.06; Fig 1D). However, there were no significant difference among 3-year DFS rates for germline BRCA1/2 group (88.8%±6.3%), somatic BRCA1/2 group (100%) and non-carriers (90.4%±1.7%) (Fig 1C). No significant association was found between the risk of relapse with germline BRCA1/2 variants or somatic ones in this general population of stage 0~III (Table 4).
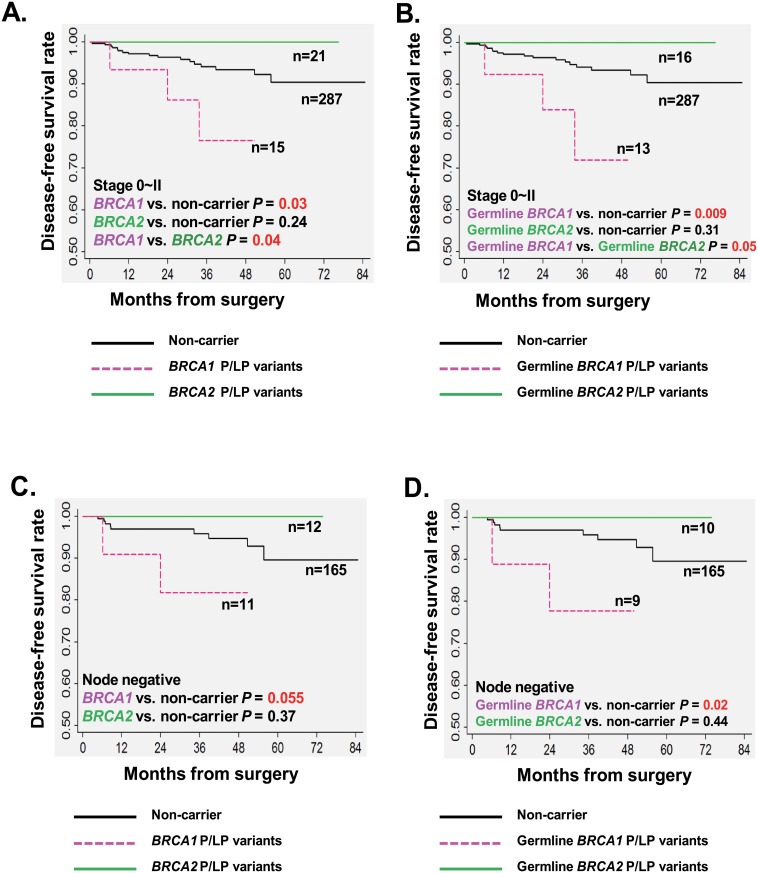
Disease-free survival of subgroups by clinical stage
We further conducted stratified survival analysis by disease stages. In the subgroup with a relatively earlier stage (0~II), we observed that 3-year DFS rate of the 15 BRCA1 carriers (germline or somatic) was significantly worse than 287 non-carriers (76.6%±12.1% vs. 94.1%±1.6%; log-rank P = 0.03), and also worse than 21 BRCA2 carriers (germline or somatic) (76.6%±12.1% vs. 100%; log-rank P = 0.04; Fig 2A). Moreover, the univariate analysis demonstrate that BRCA1 variants significantly increased the relapse risk by 3.7 fold as compared to non-carriers [HR = 3.70; 95% confidence interval (CI) = 1.08–12.76; P = 0.04; Table 5]. However, the statistical significance didn’t maintain when HR was adjusted by classic prognostic factors, including age at diagnosis, molecular subtype, tumor grade and administration of standard therapy (HR = 2.06;95% CI = 0.48–8.8;P = 0.33; Table 5).
Fig 2. Impact of BRCA1/2 P/LP variants on the DFS of subgroups with early stage.
Kaplan-Meier survival analysis; P values calculated using a log-rank analysis. Estimated DFS of breast cancer patients with stage 0~II by BRCA status: (A) BRCA1 and BRCA2 P/LP variants (germline or somatic); (B) Germline BRCA1 and BRCA2 P/LP variants. Estimated DFS of breast cancer patients with node negative disease by BRCA status: (C) BRCA1 and BRCA2 P/LP variants (germline or somatic); (D) Germline BRCA1 and BRCA2 P/LP variants.
Table 5. Impact of BRCA1/2 P/LP variants on the DFS of breast cancer patients from subgroups of stage 0~II and III.
| P/LP variants | #Cases (events) | HR (95% CI) a | P a | Adjusted HR (95% CI) b | P b |
|---|---|---|---|---|---|
| Stage 0~II | |||||
| Germline and somatic variants combined | |||||
| Non-carrier | 287 (17) | 1 | 1 | ||
| BRCA1 | 15 (3) | 3.70 (1.08–12.76) | 0.04 | 2.06 (0.48–8.8) | 0.33 |
| BRCA2 | 21 (0) | 0 | 0.98 | 0 | 0.99 |
| Germline variants | |||||
| Non-carrier | 287 (17) | 1 | 1 | ||
| BRCA1 | 13 (3) | 4.52 (1.31–15.61) | 0.02 | 2.72 (0.65–11.44) | 0.17 |
| BRCA2 | 16 (0) | 0 | 0.98 | 0 | 0.99 |
| Somatic variants | |||||
| Non-carrier | 287 (17) | 1 | 1 | ||
| BRCA1/2 | 6 (0) | 0 | 0.66 | 0 | 1.00 |
| Stage III | |||||
| Germline and somatic variants combined | |||||
| Non-carrier | 93 (18) | 1 | 1 | ||
| BRCA1 | 4 (0) | 0 | 0.55 | 0 | 0.99 |
| BRCA2 | 6 (0) | 0 | 0.51 | 0 | 0.99 |
a Univariate Cox proportional hazards regression models
b Multivariate Cox proportional hazards regression models. HR was adjusted by age at diagnosis, molecular subtype (Luminal A, Luminal B, TNBC, HER2+ and ER-PR+), tumor grade (grade I/II and III) and administration of standard therapy.
In the subgroup analysis for stage 0~II, patients with a germline BRCA1 variant had a significantly worse 3-year DFS rate of 71.9%±14.3%, compared with 94.1%±1.6% for non-carriers (P = 0.009), and 100% for ones with a germline BRCA2 variant (P = 0.05) (Fig 2B). The presence of a germline BRCA1 variant particularly predicted an increased risk of relapse as compared to non-carriers (unadjusted HR = 4.52;95% CI = 1.31–15.61;P = 0.02; Table 5). However, no events occurred in patients with somatic BRCA1/2 variants, and no impact on the relapse risk was observed (Table 5).
On the other hand, we didn’t find any prediction role of BRCA1 or BRCA2 variants (germline or somatic) in relapse risk for the subgroup of stage III (Table 5).
Disease-free survival of subgroups by N stage
In stratified analysis by lymph node involvement, we also found an inferior DFS in 11 BRCA1 carriers (germline or somatic) than 165 non-carriers with a marginal significance in the patients without lymph node involvement (3-year DFS rate: 81.8%±11.6% vs. 95.9%±1.7%; log-rank P = 0.055; Fig 2C). A trend of an increased risk of relapse was found in BRCA1 carriers by univariate analysis (unadjusted HR = 4.08;95% CI = 0.86–19.4;P = 0.08), which was not observed in the subgroup of lymph node positive patients (Table 6). In particular, lymph node negative patients with a germline BRCA1 variant had a even worse 3-year DFS rate of 77.8%±13.9% than non-carriers (log-rank P = 0.02; Fig 2D). Germline BRCA1 variant was significantly associated with a poor DFS in the lymph node negative subgroup (HR = 5.4;95% CI = 1.12–26.00;P = 0.04; Table 6).
Table 6. Impact of BRCA1/2 P/LP variants on the DFS of breast cancer patients from subgroups of N0 and N1~3.
| P/LP variants | #Cases (events) | HR (95% CI) a | P a | Adjusted HR (95% CI) b | P b |
|---|---|---|---|---|---|
| N0 | |||||
| Germline and somatic combined variants | |||||
| Non-carrier | 165 (9) | 1 | 1 | ||
| BRCA1 | 11 (2) | 4.08 (0.86–19.4) | 0.08 | 1.7 (0.28–10.32) | 0.56 |
| BRCA2 | 12 (0) | 0 | 0.98 | 0 | 0.99 |
| Germline variants | |||||
| Non-carrier | 165 (9) | 1 | 1 | ||
| BRCA1 | 9 (2) | 5.4 (1.12–26.0) | 0.04 | 3.62 (0.47–27.63) | 0.21 |
| BRCA2 | 10 (0) | 0 | 0.99 | 0 | 0.99 |
| Somatic variants | |||||
| Non-carrier | 165 (9) | 1 | 1 | ||
| BRCA1/2 | 4 (0) | 0 | 0.70 | 0 | 0.99 |
| N1~N3 | |||||
| Germline and somatic combined variants | |||||
| Non-carrier | 215 (26) | 1 | 1 | ||
| BRCA1 | 8 (1) | 1.01 (0.14–7.47) | 0.99 | 0.7 (0.08–6.02) | 0.74 |
| BRCA2 | 15 (0) | 0 | 0.98 | 0 | 0.98 |
a Univariate Cox proportional hazards regression models
b Multivariate Cox proportional hazards regression models. HR was adjusted by age at diagnosis, molecular subtype (Luminal A, Luminal B, TNBC, HER2+ and ER-PR+), tumor grade (grade I/II and III) and administration of standard therapy.
Overall survival of stage 0~III patients
The stage 0~III patients with BRCA1/2 P/LP variants shared a similar 3-year OS rate with non-carriers (100% vs. 94.9%±1.4%; log-rank P = 0.11). We didn’t find significant association between BRCA1 or BRCA2 carriers with overall survival, regardless of their germline or somatic status (Table 4).
Discussion
This study provided new insights on the complexity of the BRCA1/2 variants in unselected Chinese breast cancer patients. Germline BRCA1/2 P/LP variants were detected in 7.9% of the 507 patients. This was higher than the germline BRCA1/2 mutation rates (2.2%) previously reported in a cohort of 645 unselected Chinese breast cancer women[4], and than that (3.0%) in 471 unselected Korea breast cancer patients using less sensitive methods[23]. In addition, the germline BRCA2 P/LP variants accounted for 18.8% (3/16) of the FBC patients in our study, and no BRCA1 variant were detected in FBC subgroup. While in a study with a larger sample size of 99 Chinese patients with hereditary breast cancer, 7.1% in BRCA1 and 11.1% in BRCA2 were found by NGS [5].
Using both tumor and paired blood/normal tissue allowed us to identify both somatic and germline mutations. We observed that somatic pathogenic variant accounted for a minor proportion of 1.8% in this cohort (BRCA1, 0.6%; BRCA2, 1.2%). The percentage was slightly lower than the previous report by The Cancer Genome Atlas (TCGA) using NGS (BRCA1, 1.4%; BRCA2, 2.0%)[24]. The majority of the races included in TCGA was Caucasian, versus Asian for our study. The genomic diversity may partly explain the various rates of somatic BRCA mutation among different races.
Among the 70 TNBC patients, there were 15 (21.4%) BRCA1/2 P/LP variants carriers (11 with germline BRCA1, 1 with somatic BRCA1, and 3 with germline BRCA2). Our results are in agreement with other studies of unselected TNBC, which demonstrated that germline BRCA1/2 mutations are enriched in TNBC patients(11.2%-18.2%)[14, 25]. Notably, the next subtype with a high rate of BRCA1/2 P/LP variants is Luminal B (9.7%, 21 germline and 7 somatic). This is potentially important as Luminal B may not be considered as a high risk group for BRCA mutation screening in current clinical practice. Interestingly, the BRCA1 variants were predominantly found in the TNBC patients, and the BRCA2 variants were mainly associated with the Luminal B subtype, respectively. We also observed that the germline BRCA1 P/LP variants have a stronger association with aggressive phenotypes, including triple-negative, tumor grade III, and advanced tumor stage M1. In the contrary, these phenotypes were not observed in the germline BRCA2 carriers. Our findings are consistent with the previous reports from Asia [26–27] and United States [28] studies.
In patients with stage 0~II disease, we observed a worse DFS in the BRCA1 (germline or somatic) carriers, as compared to the BRCA2 carriers or non-carriers. We also found a similar trend in the patients without lymph node involvement. Furthermore, the presence of germline BRCA1 P/LP variants was significantly associated with an increased risk of relapse in those two subgroups. These findings indicated that the disease progression pattern is diverse among the genetically different breast cancer patients, including those were diagnosed at an early stage. However, we didn’t find association between BRCA status and OS, which may need a long-term follow-up.
The impact of germline BRCA1/2 mutations on patient survival varies in different clinical settings. Moller et al [29] screened the whole coding sequence of BRCA1/2 in 422 FBC patients, and reported a worse 5-year OS in BRCA1 carriers, as compared to BRCA2 carriers or mutation-negative ones. And this prognosis trend maintained when BRCA1 carriers were diagnosed at an apparently early stage (ex. no lymph involvement or DCIS), which was similar to our observation in DFS. The inferior clinical outcome in BRCA1 carriers in comparison to BRCA2 might be explained by aggressive phenotypes [30]. Rennert et al [31] detected three founder BRCA1/2 mutations in 1317 Israeli women with breast cancer. Consistent with our findings, they found 10-year breast cancer-specific rates of death were similar for carriers of a BRCA founder mutation and non-carriers.
On the other hand, in the neoadjuvant chemotherapy setting, TNBC patients with germline BRCA1 mutation showed a better pathologic complete response to anthracycline with or without taxane regimens [32]. There were also other studies reported that triple-negative breast cancer (TNBC) patients with germline or somatic BRCA1/2 mutations had a significantly lower risk of relapse[14]. The Cancer Genome Atlas project and University of Washington Medical Center revealed that 6.3%-6.8% of patients with ovarian cancer carried somatic BRCA1/2 mutation [33–34]. In ovarian cancer patients, somatic mutations together with germline mutations in BRCA1/2 genes were associated with favorable survival [33, 35]. As showed by preclinical studies, tumor cells with defective homologous recombination as a result of BRCA mutation might be more sensitivity to agents that cause DNA strand breaks through intercalation with base pairs (e.g., anthracyclines) or through DNA adduct formation (e.g. platinum) [36–38]. This could partly explain different BRCA-associated prognosis observed in the general population and specific clinical settings.
There are some limitations in this study. The sample size herein (n = 507) was relatively small when considering the large diversity of documented variants (ex., over 1500 recorded in BIC database), scattered distribution of these variants in the whole coding regions, and the low frequency of BRCA1/2 P/LP variants (9.9%). In addition to the variants, to explore methylation and protein expression of BRCA1/2 genes would further provide us with understanding of the association between BRCAness and patient survival.
In summary, germline or somatic BRCA1/2 P/LP variants were detected in ~10% of the unselected breast cancer patients from a single hospital in West China. Not only TNBC but also Luminal B subtypes had high frequencies of BRCA1/2 variants. Germline BRCA1 carriers tended to have more aggressive tumor phenotypes, including triple-negative, higher tumor grade and advanced disease stage, which was not observed in germline BRCA2 carriers. On the other hand, patients with somatic BRCA1/2 variants were likely to be HER2 negative. The presence of a germline or somatic BRCA1 P/LP variant, especially the germline one, was associated with worse DFS in the patients diagnosed at early stage (Stage 0~II, or N0). These findings suggest that BRCA1 status is associated with breast cancer phenotype and disease progression, and could be potential prognostic biomarkers especially for early stage disease. It also provided clinical evidence for screening BRCA1/2 status in not only TNBC or FBC, but also Luminal B patients, which are considered as the high risk subgroups.
Supporting Information
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
We would like to acknowledge Dr. Ping He from West China Hospital for clinical information review.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by AstraZeneca (Recipient: ZH). The funder provided support in the form of salaries for authors [ZD, HD, XHZ, YS, XL, FS, XS and YG], but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section.
References
- 1.Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol. 2007;25(11):1329–33. Epub 2007/04/10. doi: 25/11/1329 [pii] 10.1200/JCO.2006.09.1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Melchor L, Benitez J. The complex genetic landscape of familial breast cancer. Hum Genet. 2013;132(8):845–63. Epub 2013/04/05. 10.1007/s00439-013-1299-y . [DOI] [PubMed] [Google Scholar]
- 3.Kim H, Choi DH. Distribution of BRCA1 and BRCA2 Mutations in Asian Patients with Breast Cancer. J Breast Cancer. 2013;16(4):357–65. Epub 2014/01/24. 10.4048/jbc.2013.16.4.357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Suter NM, Ray RM, Hu YW, Lin MG, Porter P, Gao DL, et al. BRCA1 and BRCA2 mutations in women from Shanghai China. Cancer Epidemiol Biomarkers Prev. 2004;13(2):181–9. Epub 2004/02/20. . [DOI] [PubMed] [Google Scholar]
- 5.Yang X, Wu J, Lu J, Liu G, Di G, Chen C, et al. Identification of a comprehensive spectrum of genetic factors for hereditary breast cancer in a Chinese population by next-generation sequencing. PLoS One. 2015;10(4):e0125571 Epub 2015/05/01. 10.1371/journal.pone.0125571 PONE-D-14-52603 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roy R, Chun J, Powell SN. BRCA1 and BRCA2: different roles in a common pathway of genome protection. Nat Rev Cancer. 2012;12(1):68–78. Epub 2011/12/24. doi: nrc3181 [pii] 10.1038/nrc3181 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oza AM, Cibula D, Benzaquen AO, Poole C, Mathijssen RH, Sonke GS, et al. Olaparib combined with chemotherapy for recurrent platinum-sensitive ovarian cancer: a randomised phase 2 trial. Lancet Oncol. 2015;16(1):87–97. Epub 2014/12/08. doi: S1470-2045(14)71135-0 [pii] 10.1016/S1470-2045(14)71135-0 . [DOI] [PubMed] [Google Scholar]
- 8.Tutt A, Robson M, Garber JE, Domchek SM, Audeh MW, Weitzel JN, et al. Oral poly(ADP-ribose) polymerase inhibitor olaparib in patients with BRCA1 or BRCA2 mutations and advanced breast cancer: a proof-of-concept trial. Lancet. 2010;376(9737):235–44. Epub 2010/07/09. doi: S0140-6736(10)60892-6 [pii] 10.1016/S0140-6736(10)60892-6 . [DOI] [PubMed] [Google Scholar]
- 9.Alsop K, Fereday S, Meldrum C, deFazio A, Emmanuel C, George J, et al. BRCA mutation frequency and patterns of treatment response in BRCA mutation-positive women with ovarian cancer: a report from the Australian Ovarian Cancer Study Group. J Clin Oncol. 2012;30(21):2654–63. Epub 2012/06/20. doi: JCO.2011.39.8545 [pii] 10.1200/JCO.2011.39.8545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ledermann J, Harter P, Gourley C, Friedlander M, Vergote I, Rustin G, et al. Olaparib maintenance therapy in patients with platinum-sensitive relapsed serous ovarian cancer: a preplanned retrospective analysis of outcomes by BRCA status in a randomised phase 2 trial. Lancet Oncol. 2014;15(8):852–61. Epub 2014/06/03. doi: S1470-2045(14)70228-1 [pii] 10.1016/S1470-2045(14)70228-1 . [DOI] [PubMed] [Google Scholar]
- 11.Turner N, Tutt A, Ashworth A. Hallmarks of 'BRCAness' in sporadic cancers. Nat Rev Cancer. 2004;4(10):814–9. Epub 2004/10/29. doi: nrc1457 [pii] 10.1038/nrc1457 . [DOI] [PubMed] [Google Scholar]
- 12.Goodwin PJ, Phillips KA, West DW, Ennis M, Hopper JL, John EM, et al. Breast cancer prognosis in BRCA1 and BRCA2 mutation carriers: an International Prospective Breast Cancer Family Registry population-based cohort study. J Clin Oncol. 2012;30(1):19–26. Epub 2011/12/08. doi: JCO.2010.33.0068 [pii] 10.1200/JCO.2010.33.0068 . [DOI] [PubMed] [Google Scholar]
- 13.Huzarski T, Byrski T, Gronwald J, Gorski B, Domagala P, Cybulski C, et al. Ten-year survival in patients with BRCA1-negative and BRCA1-positive breast cancer. J Clin Oncol. 2013;31(26):3191–6. Epub 2013/08/14. doi: JCO.2012.45.3571 [pii] 10.1200/JCO.2012.45.3571 . [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez-Angulo AM, Timms KM, Liu S, Chen H, Litton JK, Potter J, et al. Incidence and outcome of BRCA mutations in unselected patients with triple receptor-negative breast cancer. Clin Cancer Res. 2011;17(5):1082–9. Epub 2011/01/15. doi: 1078-0432.CCR-10-2560 [pii] 10.1158/1078-0432.CCR-10-2560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maksimenko J, Irmejs A, Nakazawa-Miklasevica M, Melbarde-Gorkusa I, Trofimovics G, Gardovskis J, et al. Prognostic role of mutation in patients with triple-negative breast cancer. Oncol Lett. 2014;7(1):278–84. Epub 2013/12/19. 10.3892/ol.2013.1684 ol-07-01-0278 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhong Q, Peng HL, Zhao X, Zhang L, Hwang WT. Effects of BRCA1- and BRCA2-related mutations on ovarian and breast cancer survival: a meta-analysis. Clin Cancer Res. 2015;21(1):211–20. Epub 2014/10/29. 1078-0432.CCR-14-1816 [pii] 10.1158/1078-0432.CCR-14-1816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dong Z, Dong H, Zhong X, Peng Z, Zhu X, Sun Y, et al. Development of a Comprehensive NGS Workflow for the Analysis of Tumor BRCA1 and BRCA2 Mutations and Large Rearrangements. J Genet Genome Res. 2015;2(2):019. [Google Scholar]
- 18.Richards CS, Bale S, Bellissimo DB, Das S, Grody WW, Hegde MR, et al. ACMG recommendations for standards for interpretation and reporting of sequence variations: Revisions 2007. Genet Med. 2008;10(4):294–300. Epub 2008/04/17. 10.1097/GIM.0b013e31816b5cae 00125817-200804000-00009 [pii]. . [DOI] [PubMed] [Google Scholar]
- 19.Bu H, Chen J, Chen LY, Chang XQ, Deng YJ, Ding HY, et al. [Guideline for testing of estrogen and progesterone receptors in breast cancer]. Zhonghua Bing Li Xue Za Zhi. 2015;44(4):237–9. Epub 2015/05/16. . [PubMed] [Google Scholar]
- 20.Bian XW, Bu H, Chang XQ, Chen J, Ding HY, Fu L, et al. [Guidelines for HER2 detection in breast cancer, the 2014 version]. Zhonghua Bing Li Xue Za Zhi. 2014;43(4):262–7. Epub 2014/06/12. . [PubMed] [Google Scholar]
- 21.Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thurlimann B, et al. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol. 2013;24(9):2206–23. Epub 2013/08/07. doi: mdt303 [pii] 10.1093/annonc/mdt303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kwong A, Ng EK, Wong CL, Law FB, Au T, Wong HN, et al. Identification of BRCA1/2 founder mutations in Southern Chinese breast cancer patients using gene sequencing and high resolution DNA melting analysis. PLoS One. 2012;7(9):e43994 Epub 2012/09/13. 10.1371/journal.pone.0043994 PONE-D-12-00295 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim H, Cho DY, Choi DH, Choi SY, Shin I, Park W, et al. Characteristics and spectrum of BRCA1 and BRCA2 mutations in 3,922 Korean patients with breast and ovarian cancer. Breast Cancer Res Treat. 2012;134(3):1315–26. Epub 2012/07/17. 10.1007/s10549-012-2159-5 . [DOI] [PubMed] [Google Scholar]
- 24.Comprehensive molecular portraits of human breast tumours. Nature. 2012;490(7418):61–70. Epub 2012/09/25. doi: nature11412 [pii] 10.1038/nature11412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Couch FJ, Hart SN, Sharma P, Toland AE, Wang X, Miron P, et al. Inherited mutations in 17 breast cancer susceptibility genes among a large triple-negative breast cancer cohort unselected for family history of breast cancer. J Clin Oncol. 2015;33(4):304–11. Epub 2014/12/03. doi: JCO.2014.57.1414 [pii] 10.1200/JCO.2014.57.1414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu JH, Lee JW, Son BH, Kim SW, Park SK, Lee MH, et al. Characteristics of BRCA1/2 Mutation-Positive Breast Cancers in Korea: A Comparison Study Based on Multicenter Data and the Korean Breast Cancer Registry. J Breast Cancer. 2014;17(2):129–35. Epub 2014/07/12. 10.4048/jbc.2014.17.2.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li WF, Hu Z, Rao NY, Song CG, Zhang B, Cao MZ, et al. The prevalence of BRCA1 and BRCA2 germline mutations in high-risk breast cancer patients of Chinese Han nationality: two recurrent mutations were identified. Breast Cancer Res Treat. 2008;110(1):99–109. Epub 2007/09/14. 10.1007/s10549-007-9708-3 . [DOI] [PubMed] [Google Scholar]
- 28.Atchley DP, Albarracin CT, Lopez A, Valero V, Amos CI, Gonzalez-Angulo AM, et al. Clinical and pathologic characteristics of patients with BRCA-positive and BRCA-negative breast cancer. J Clin Oncol. 2008;26(26):4282–8. Epub 2008/09/10. doi: 26/26/4282 [pii] 10.1200/JCO.2008.16.6231 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moller P, Evans DG, Reis MM, Gregory H, Anderson E, Maehle L, et al. Surveillance for familial breast cancer: Differences in outcome according to BRCA mutation status. Int J Cancer. 2007;121(5):1017–20. Epub 2007/05/02. 10.1002/ijc.22789 . [DOI] [PubMed] [Google Scholar]
- 30.Liedtke C, Mazouni C, Hess KR, Andre F, Tordai A, Mejia JA, et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008;26(8):1275–81. Epub 2008/02/06. doi: JCO.2007.14.4147 [pii] 10.1200/JCO.2007.14.4147 . [DOI] [PubMed] [Google Scholar]
- 31.Rennert G, Bisland-Naggan S, Barnett-Griness O, Bar-Joseph N, Zhang S, Rennert HS, et al. Clinical outcomes of breast cancer in carriers of BRCA1 and BRCA2 mutations. N Engl J Med. 2007;357(2):115–23. Epub 2007/07/13. doi: 357/2/115 [pii] 10.1056/NEJMoa070608 . [DOI] [PubMed] [Google Scholar]
- 32.Wang C, Zhang J, Wang Y, Ouyang T, Li J, Wang T, et al. Prevalence of BRCA1 mutations and responses to neoadjuvant chemotherapy among BRCA1 carriers and non-carriers with triple-negative breast cancer. Ann Oncol. 2015;26(3):523–8. Epub 2014/12/07. doi: mdu559 [pii] 10.1093/annonc/mdu559 . [DOI] [PubMed] [Google Scholar]
- 33.Network TCGAR. Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474(7353):609–15. Epub 2011/07/02. doi: nature10166 [pii] 10.1038/nature10166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pennington KP, Walsh T, Harrell MI, Lee MK, Pennil CC, Rendi MH, et al. Germline and somatic mutations in homologous recombination genes predict platinum response and survival in ovarian, fallopian tube, and peritoneal carcinomas. Clin Cancer Res. 2014;20(3):764–75. Epub 2013/11/19. doi: 1078-0432.CCR-13-2287 [pii] 10.1158/1078-0432.CCR-13-2287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hennessy BT, Timms KM, Carey MS, Gutin A, Meyer LA, Flake DD 2nd, et al. Somatic mutations in BRCA1 and BRCA2 could expand the number of patients that benefit from poly (ADP ribose) polymerase inhibitors in ovarian cancer. J Clin Oncol. 2010;28(22):3570–6. Epub 2010/07/08. doi: JCO.2009.27.2997 [pii] 10.1200/JCO.2009.27.2997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tassone P, Tagliaferri P, Perricelli A, Blotta S, Quaresima B, Martelli ML, et al. BRCA1 expression modulates chemosensitivity of BRCA1-defective HCC1937 human breast cancer cells. Br J Cancer. 2003;88(8):1285–91. Epub 2003/04/17. 10.1038/sj.bjc.6600859 6600859 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quinn JE, Kennedy RD, Mullan PB, Gilmore PM, Carty M, Johnston PG, et al. BRCA1 functions as a differential modulator of chemotherapy-induced apoptosis. Cancer Res. 2003;63(19):6221–8. Epub 2003/10/16. . [PubMed] [Google Scholar]
- 38.Chalasani P, Livingston R. Differential chemotherapeutic sensitivity for breast tumors with "BRCAness": a review. Oncologist. 2013;18(8):909–16. Epub 2013/07/25. doi: theoncologist.2013-0039 [pii] 10.1634/theoncologist.2013-0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.