Abstract
Duration of Initiative
48 months and currently ongoing.
Setting
The Houston Methodist Hospital System and affiliated hospitals (3 facilities with 2 hospital-run skilled nursing facilities in and around Houston), St. Joseph’s Regional Health Center (1 acute care hospital and 2 skilled nursing facilities in Bryan, Texas), Hospital Corporation of America (2 acute care facilities in Houston, 1 acute care facility in McAllen, Texas [Rio Grande Valley]), Kindred Healthcare (2 long term acute care facilities in Houston), Select Medical Specialty Hospitals (2 long term acute care facilities in Houston).
Whom This Should Concern
Hospital administrators, quality and safety officers, performance improvement and patient safety professionals, clinic managers, infection control and prevention staff, and other physicians, nurses, and clinical staff.
Driving Forces
Sepsis is the 11th leading cause of death in the United States, ranking 10th in people 65 years of age and older.1 In 2011 septicemia was the most costly and third most common reason for hospitalizations, accounting for 1,094,000 hospital stays and $20.3 billion in aggregate hospital costs 2–4; the average cost for an admission for sepsis was $18,600.4 The Surviving Sepsis Campaign, launched in 2002,5 sparked many hospitals to create programs to improve the care and, hopefully, the outcomes of patients with sepsis. Although they shared common goals, programs differed in approaches to achieving the goals. Like the international sepsis performance improvement initiative that was linked to the Surviving Sepsis Campaign,6 the individual programs for which results have been reported show improvements in the processes of sepsis care,7,8 if not both processes and outcomes.9–11
Sepsis programs continue to be established across the United States,12 and hospitals are expected to monitor their processes of sepsis care and begin reporting on these processes to the Centers for Medicare & Medicaid Services (CMS) for severe sepsis and septic shock cases discharged on or after October 1, 2015, the beginning of federal Fiscal Year [FY] 2016 (ending September 30, 2016). The measure was adopted in the FY 2015 inpatient Prospective Payment System final rule for FY 2017.13–15 This places additional emphasis on the importance of recognizing patients with severe sepsis or septic shock as early as possible. In October 2015 CMS hosted a Sepsis Coalition Town Hall, which was extremely well attended by a national audience. The conference was geared toward improving the care of patients with sepsis. One of the authors [S.L.J.] presented some lessons learned and key challenges at the Region VI Sepsis Coalition Town Hall that followed the national webinar. There were two key themes in questions from the audience: (1) what can be done to reduce sepsis mortality and (2) how can such initiatives be implemented. This article presents the “how to” for one such program, which was implemented across the 15 facilities that comprise the Texas Gulf Coast Sepsis Network (TGCSN) and are part of the Sepsis Early Recognition and Response Initiative (SERRI) project.
Sepsis and the sequelae in its survivors are major concerns for CMS—the primary payer for 75% of sepsis-related hospitalizations.2 CMS insures adults ≥ 65 years of age and disabled Americans through the federally funded Medicare program, as well as indigent Americans, through the federal- and state-funded Medicaid program. In 2013 there were 52 million Medicare and 57 million Medicaid beneficiaries, and CMS covered 36% of national health care expenditures.16 From 2008 through 2011, Medicare inpatient reimbursements for a diagnosis-related group (DRG) linked to sepsis totaled $17.7 billion, 5% of which was for stays classified as high-cost outliers.17 A high proportion of sepsis survivors suffer persistent sequelae such as renal failure and cognitive decline and require high levels of postdischarge care.18,19
The 2010 Affordable Care Act created the Innovation Center at CMS,20 authorizing it to explore initiatives that could improve care, improve health, and reduce costs. In answer to its November 2011 call, the Innovation Center received 2,960 applications and funded 107. In this article, we describe one of those—the ongoing (July 2012—June 2016) multicenter SERRI. SERRI is based on a program developed by the convener facility, Houston Methodist Hospital (HMH), which reduced sepsis mortality and costs.21,22 Like many other hospitals, HMH began in the mid-2000s to devise and implement approaches to improving the detection and treatment of sepsis in its inpatients. The evolution, elements, and outcomes of the HMH program have been reported.22
Initiative Description
Design, Sites and Target Population, and Projected Impacts
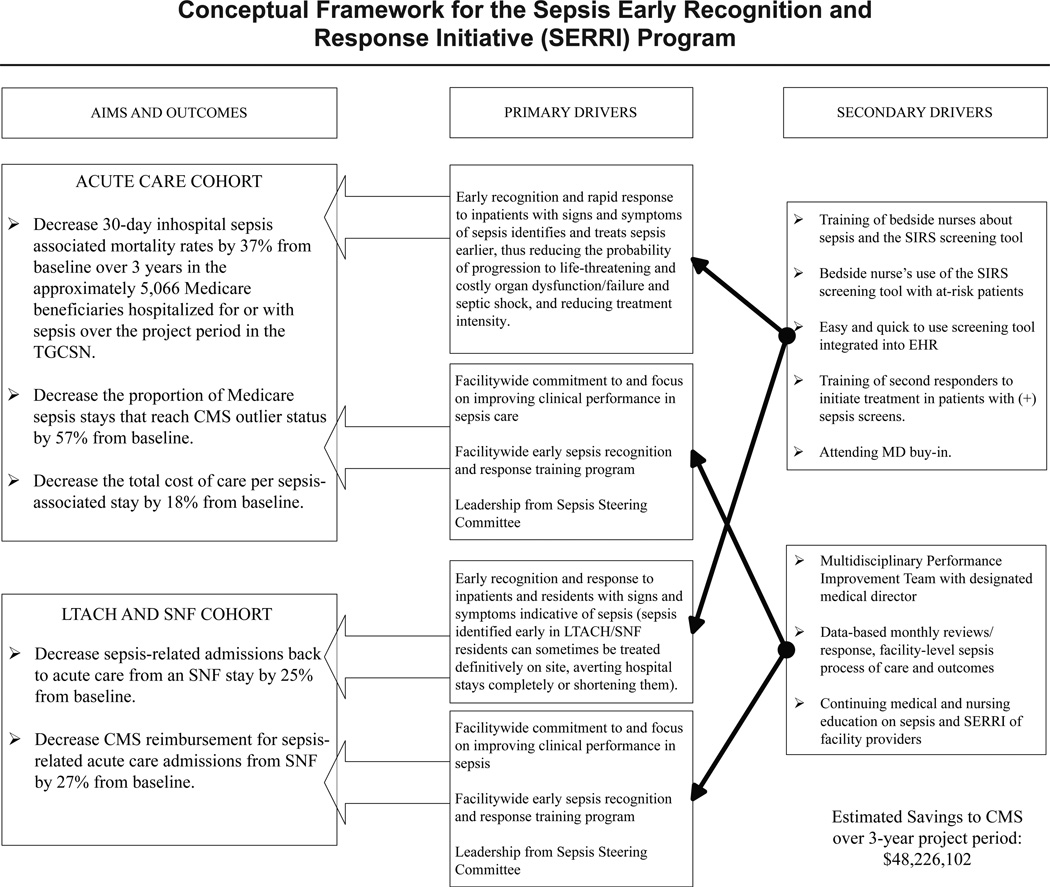
Figure 1 (page 124) depicts SERRI’s conceptual framework and projected impacts on lives saved and costs avoided. The study design incorporates pre- and postimplementation analyses of outcomes and resource use at participating facilities and concurrent comparisons between participating facilities and similar but nonparticipating facilities. Pre-post analyses will include all adults treated for sepsis, while concurrent analyses will include only CMS beneficiaries. The cost analyses will be conducted from the perspective of the primary payer (CMS or another third party insurer); from the hospital perspective, payers’ costs constitute the revenues they receive.
Figure 1.
SERRI’s conceptual framework is shown, along with the projected impacts on lives saved and costs avoided in the acute care cohort, which were extrapolated from the convener hospital (Houston Methodist Hospital) experience from 2009 through 2011. Projected outcomes for the postacute care sites were based on 2011 data provided by 14 such sites (not all of which elected to be SERRI participants) showing that, per 1,000 long term acute care hospitals (LTACHs), and skilled nursing facilities (SNFs) stays of Medicare beneficiaries, there were 200 returns to acute care hospitals within 30 days of LTACH and SNF admission, and that nearly two thirds were due to suspected sepsis. As the figure shows, a set of primary and secondary drivers was projected to reduce from their respective baselines the following: (1) in the acute care cohort, inpatient sepsis death rates by 37%, the proportion of sepsis-associated Medicare stays reaching high-cost outlier status by 57%, and the total cost of care per sepsis-associated stay by 18%; and (2) in the postacute care cohort, sepsis-associated returns to acute care hospitals from LTACHs and SNFs by 25%, and Centers for Medicare & Medicaid Services (CMS) reimbursement for sepsis-associated acute care admissions from LTACHs and SNFs by 27%. SIRS, systemic inflammatory response syndrome (a manifestation of early sepsis); TGCSN, Texas Gulf Coast Sepsis Network; EHR, electronic health record.
The original participants are the 15 facilities of the TGCSN, which has a wide geographic reach within and outside the nine-county Houston metropolitan area, and spans the continuum of care, including 7 acute care hospitals, 4 long term acute care hospitals (LTACHs), and 4 skilled nursing facilities (SNFs), large and small, teaching and nonteaching, and for-and not-for-profit (Appendix 1 and Appendix 2, available in online article). At HMH—1 of the 7 acute care hospitals—the SERRI award enabled expansion of the HMH sepsis program to additional clinical units. Two new acute care sites joined SERRI in mid-2014.
The target population consists of adults admitted to a TGCSN facility, not limited to Medicare and Medicaid beneficiaries, divided into acute care and postacute care cohorts. The acute care cohort has three subcohorts: sepsis present-on-admission (POA), medical hospital-acquired sepsis, and surgical hospital-acquired sepsis. For the acute care cohort, the SERRI Program Office uses routinely collected hospital claims data; that is, elements found in the hospital discharge abstract (Uniform Billing Form 04) for analysis of outcomes and resource utilization. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes are, for septicemia and/or sepsis, 038.0–038.9 and 995.91; for severe sepsis, 995.92; and for septic shock, 785.52. (These codes have been used for sepsis statistics for the United States 19 and in other recent large studies.23,24) Patients with a sepsis code with a POA “no” indicator are assigned to the medical or surgical hospital-acquired subcohort by whether their stay was classified into a “medical” or “surgical” DRG.25–27
Site-Specific Implementation
The intervention’s key elements are based on those developed and implemented at the convener facility,22 as follows: (1) leadership; (2) education of bedside nurses and second responders; (3) incorporation of a five-item bedside systemic inflammatory response syndrome (SIRS)/sepsis screening tool 21 into electronic health record (EHR) systems (bedside nurses can complete a screen in < 1 minute; a score ≥ 4 triggers evaluation by a second responder); and (4) audit and feedback of process and outcome data. Table 1 (page 125) presents a synopsis of the screening tool and the second response protocols, which are fully described and/or shown elsewhere.22 Elements of the intervention were modified to accommodate differences in mission, staffing, clinical processes, and medical record systems; launch dates were staggered according to site-specific needs (Appendix 3, available in online article).
Table 1.
Synopsis of Screening and Response Protocols, Sepsis Early Recognition and Response Initiative (SERRI)
| Screening for Systemic Inflammatory Response Syndrome (SIRS) (First Response) | |
|---|---|
| First responder personnel | Bedside nurses (acute care hospitals); bedside nurses or patient care assistants (postacute care sites) |
| Timing | Every 12 hours from the time of admission; clock-time for screening decided on by unit nurses |
| Elements | Heart rate, temperature, respiratory rate, latest white blood cell (WBC) count, presence of altered mental status. Deviations from normal range are awarded points and a total score is computed; for acute care hospitals only, a total score of ≥ 4 is interpreted as positive for SIRS and initiates contact of the second responder.* |
| Evidence or guidelines for elements |
Elements derived from clinical syndrome described as SIRS; modified in prior testing at the SERRI convener facility; approach to scoring based on that used in the Acute Physiology and Chronic Health Evaluation (APACHE) severity of illness rating system1 |
| Actions | None if score < 4; if score ≥ 4, second responder is contacted immediately. |
| Other | Screening tool is integrated into the electronic health record of most SERRI partners; a few partners use a Web-based or paper format. |
| Responding to a Patient with a Positive Screen (Second Response) | |
| Second responder personnel | Nurse practitioners (some acute care hospitals); charge nurses or rapid response teams |
| Timing | Within one hour of detection of positive screen |
| Elements | Physical examination and search for source of infection; laboratory work, including cultures and sensitivities; fluid resuscitation; antibiotics; nursing interventions |
| Evidence or guidelines for elements |
Based on the 2008 and subsequent recommendations for goal-directed therapies from the Surviving Sepsis Campaign; 20082 and 20123 International Guidelines for Management of Severe Sepsis and Septic Shock; and recommendations of an expert panel of acute care surgeons at the SERRI convener facility (Houston Methodist Hospital) |
| Actions | Decision about need for transfer to ICU; notification of attending physician; evaluation for possible infection; early goal-directed interventions (collection of blood and fluids for culture before start of antibiotics; stat fluid resuscitation; administer antibiotics within 1 hour); reassessment after interventions |
| Other | Nurse practitioners (NPs) in Texas can be credentialed as independent practitioners; at the convener facility and some other SERRI acute care sites, the NPs, using second response/sepsis evaluation and treatment protocols approved by the hospital medical staff, can institute these protocols without waiting for the approval of the attending physician. |
For the skilled nursing facility/long term acute care hospitals, the positive screen threshold was lowered to ≥ 3 shortly after the initiative’s introduction because most patients in those sites would not have had a WBC count measured in the previous 24 hours.
References
Knaus WA, et al. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13:818–829.
RP, et al. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36: 296–327. Erratum in Crit Care Med. 2008;36:1394–1396.
Dellinger RP, et al.; Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup. Surviving Sepsis Campaign: International guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39:165–228.
Leadership
Leadership of the overall SERRI program is invested in the SERRI Program Office (at HMH), facility administrators, and the CMS Innovation Center, interacting regularly through several mechanisms; for example, SERRI Executive Committee, Site Liaisons, webinars, periodic reports, milestone-based subcontracts. Leadership at participating sites is invested in a multidisciplinary Sepsis Care Management Performance Improvement (CMPI) Committee.
Education and Training
Two sets of clinical staff must be trained at each site: those who use the screening tool with patients at the bedside (first responders), and those who evaluate patients who have a positive screen and initiate diagnostic and treatment protocols for sepsis (second responders). Training of site personnel occurred before the screening of the site’s patients began and is an ongoing activity at each site because of staff turnover. Continuing education credits are awarded for the training.
A site’s first responders are trained by local educators who have completed a mandatory online training module and a two-hour in-person “Train-the-Trainer” session given by the SERRI Site Liaisons. Site educators evaluate the success of their training of local first responders by means of a standardized posttest. The prelaunch training schedule for first responders was left to a site’s discretion, with the provision that > 85% of the site’s bedside nurses would be trained within the four weeks preceding the site’s launch date. (If training preceded the launch by more than four weeks, retraining was necessary.)
The education and training of second responders consists of an online sepsis course (SimSuite “Sepsis Comprehensive,” Medical Simulation Corporation [MSC], Denver) and a four-hour simulation training workshop at HMH’s Methodist Institute for Technology, Innovation, and Education (MITIE). First-time pass rates on pre- and posttests have been higher among second responders from acute care sites than from postacute care sites (data not provided).
Incorporation of Screening Tool into Electronic Medical Record Systems
Information technology differs across sites (Appendix 1). All six acute care hospitals (now eight, since mid-2014) and two SNFs were able to integrate the tool into their EHR systems (Appendix 3), but two LTACHs and two SNFs use the Web-based version (shown previously 22), and two LTACHs use paper.
Audit and Feedback of Process and Outcome Metrics
Sepsis early recognition measures, reviewed weekly or quarterly by unit and site, include total number of screens performed; number of unique patients screened, and number of patients with positive screens. Response measures include, for example, percentage of patients with positive screens who were evaluated by a second responder; and time elapsed between a positive screen and notification of a second responder. For most sites screening data can be retrieved electronically; however, chart review is required for response measures.
TGCSN sites submit to the Program Office anonymized data derived from their discharge/claims databases, allowing analysis of, for the acute care cohort and subcohorts, inpatient death rates, distribution of sepsis stages, length of stay, CMS financial outlier status, distribution of sepsis-associated stays across DRGs, revenue (amount reimbursed for a stay), and discharge disposition (for example, home, LTACH); and, for the postacute care cohort, admission to acute care from an LTACH or SNF. Outcomes and costs (revenues) are compared between screened and not-screened patients by linking discharge/claims data with screening data. Outcomes and cost (revenue) analyses are reported quarterly to the sites and to CMS.
Addressing Barriers
Developing Site-Specific Implementation Plans
To initiate planning for local implementation, the SERRI Program Director [S.L.J.] and Associate Program Director [L.K.] held a series of meetings and follow-up communications with upper-level leadership at each site. The purpose of these meetings was multifold: to establish relationships, provide an overview of the SERRI program, introduce the screening tool and its implications for information technology infrastructure, describe anticipated clinical outcomes of SERRI participation, discuss federal policies and procedures pertaining to subcontract awards, and communicate the importance of identifying and appointing personnel for key SERRI roles: educators, first and second responders, physician and nurse champions, and Sepsis CMPI Committee members. Participants in these planning meetings represented all key stakeholders: chief executive officers, chief nursing officers, physicians, infection prevention specialists, performance improvement and quality management directors, education directors, nurse educators and managers, nurse practitioners (NPs), pharmacy leaders, and information technology directors.
Because participating sites differ in organization, financing, mission, and other factors, we assumed that they would have to tailor the four key elements of the SERRI intervention in order to implement the program. To help the sites develop their implementation plans, the SERRI Associate Program Director and Site Liaisons conducted implementation assessment meetings at each site with nursing leaders, nurse educators, and others in key roles in frontline implementation. Sites had to decide, based on their personnel infrastructure and staffing patterns, the types of personnel who would serve as sepsis educators, first responders (bedside RNs or licensed vocational nurses), and second responders (NPs, on-call physician house staff, charge nurses, members of rapid response teams) (Appendix 3). Information technology/screening tool issues specific to each site were handled by the SERRI Program Director. The planning process at each site culminated in an implementation plan (Appendix 4, available in online article) specifying the units and patients prioritized for the program on the basis of the site’s needs and resources; personnel to serve as first and second responders; clock-time for every-12-hourly sepsis screening on targeted units; membership of the local Sepsis CMPI Committee; and target dates for key implementation activities (for example, completion of training of bedside nurses and second responders, as well as the actual launch of the SERRI program with the site’s patients). Sites chose when during Year 1 or 2 they would launch the program; as Appendix 1 shows, all six original acute care hospitals were able to launch it during Year 1, while the postacute care sites became ready in Year 2.
The large number of people directly involved with the SERRI program at each site has led to high levels of local awareness of sepsis and of SERRI. To obtain buy-in from local stake holders less directly involved (for example, attending physicians and medical staff), during the first year of the SERRI program, the Program Director made 39 different presentations across the TGCSN sites (grand rounds; seminars, usually with continuing medical education [CME] credit available) about sepsis and the benefits of early recognition and treatment. To maintain program momentum, the SERRI Program Office and Site Liaisons interact frequently with each site, attending local Sepsis CMPI Committee meetings; communicating via e-mail, telephone, and weekly newsletters; and helping with local implementation challenges as well as additional grand rounds and seminars with CME credit available for physicians, NPs, and RNs.
Incorporating The Early Sepsis/Systemic Inflammatory Response Syndrome Screening Tool into the Electronic Medical Record Systems
The backbone of the intervention is the screening tool. Incorporating the screening tool into EHR systems was a major challenge because the sites use systems from different vendors (Appendix 1), different data and information system governance processes, and local (or corporate) information technology teams with heavy competing responsibilities.
The SERRI Program Director, a physician who is an expert in medical informatics and software design, worked closely with personnel at each site (not with software vendors) to provide technology specifications and to advise on the modifications to a site’s information technology architecture that would be required to integrate the screening tool.
Some sites had to use Web-based or paper versions of the screening tool. The inability to integrate the screening tool into the EHR system shifts onto the bedside nurse the burdens of registering patients into the screening system and recording screening results. The creation of an automated feed of patient location and demographics from a site’s electronic admit, discharge, transfer module eliminated the need for bedside nurses to manually register patients at some but not all postacute care sites. Use of the Web and paper versions of the screening tool is more labor-intensive for bedside nurses than the integrated screening tool because to perform a screen they must record vital signs in two different places—the patients’ EHR, as well as the website or paper form—which carries inherent risks for data entry lags, transposition errors, and transcription errors. Lack of an integrated tool also makes it more labor-intense for a site to obtain, analyze, and therefore respond to its aggregate screening and outcome data.
The screening tool’s scoring algorithm (shown previously 22) had to be tailored for the LTACH and SNF SERRI sites because most patients in those sites would not have had a white blood cell count measured in the previous 24 hours. For patients in LTACHs and SNFs without a recent count, a score of > 3 is considered a positive screen, prompting the nurse to obtain a white blood cell count and contact the second responder. Planning is under way for an evaluation of the positive and negative predictive values of this amended scoring algorithm in the postacute care cohort.
Results
Education of responders was the first activity undertaken when SERRI funding began in July 2012. Between then and June 2015, bedside nurses and second responders at SERRI sites had participated in 12,553 SERRI educational sessions, including, but not limited to, in-person and online training for bedside nurses, train-the-trainer sessions, simulation training, and annual competency evaluations and refresher courses. (SERRI offers 12 different educational sessions, and individuals take more than one type of session.)
Between October 2012 (the “go-live” date for screening) and June 2015, screening had been performed during 215,545 stays (208,935 acute hospital stays, 3,824 LTACH stays, and 2,779 SNF stays). A positive screen prompted an evaluation by a second responder in 25,317 of all encounters (24,519/208,935 or 11.7% of acute care stays, 715/3,834 or 18.6% of LTACH encounters, and 83/2,776 or 3.0% of SNF stays). Screening is conducted on patients treated on clinical units targeted for the SERRI program, without foreknowledge of the final diagnoses for the stay, so a large proportion of the 215,545 screened stays did not have sepsis as a discharge diagnosis. These data can be used to project the workload for second responders in acute care sites or in postacute care sites.
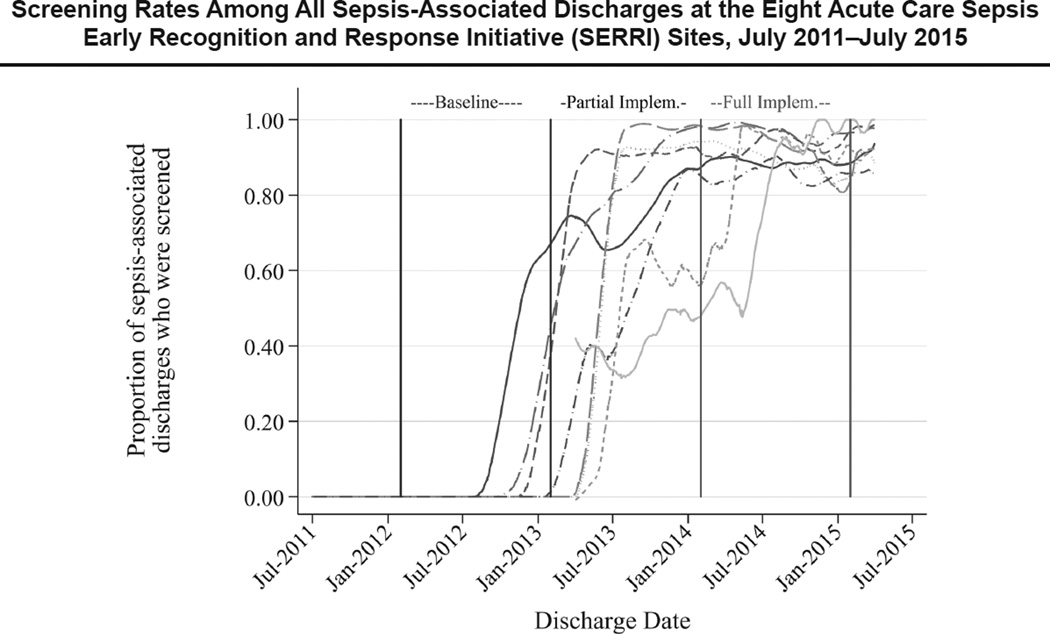
If we restrict the denominator to stays determined by final discharge diagnoses to be associated with sepsis, it is possible to determine the extent to which the screening project is reaching the patients who need it most. By January 2015, except for the two new sites that joined in mid-2014, all the acute care SERRI sites were screening more than 80% of inpatients whose stay was sepsis-associated (Figure 2, page 128). By January 2015, screening by site had reached 89%–98% of sepsis-associated stays in the postacute care sites (temporal data not shown). In calendar year 2014, the proportion of patients with a sepsis-associated stay who had been screened and had > 1 positive screen was 7,690/106,706 (7.2%) in the acute care sites, 617/3,184 (19.4%) in LTACHs, and 55/1,654 (3.3%) in the SNF setting.
Figure 2.
Time lines, generated using lowess smoothing of screening rates with a bandwidth of 0.10, represent the proportion of sepsis-associated discharges that had at least one sepsis screen performed during the encounter. As shown in the figure, by January 2015, except for the two new sites that joined in mid-2014, all the acute care SERRI sites were screening more than 80% of inpatients whose stay was sepsis-associated. the denominators were all sepsis-associated discharges at participating hospitals during the time points, regardless of whether the stay occurred on a unit targeted for SERRI participation.
Analyses of the demographic and clinical features and outcomes (inpatient mortality, hospital cost to primary payer, and discharge disposition of survivors) of the 5,672 sepsis-associated acute care stays that occurred at the seven original acute care sites during the baseline preimplementation year 2012 have been reported elsewhere.28 These baseline data are informative for epidemiological purposes.
Outcomes data (changes in, for example, inpatient mortality rates, costs) for the ongoing SERRI program are not yet available, and it is not yet known the extent to which the SERRI intervention will achieve the goals shown in Figure 1.
Key Learnings
Medical Informaticist and Software Designer: a Critical Component
Because participating sites use different EHR systems, getting the sepsis screening tool electronically integrated across sites was a major challenge. The design and deployment of the back end data retrieval and presentation software for audits and the feedback of data to the sites (and to CMS) were also dependent on the medical informaticist. Multicenter projects such as SERRI that involve very different sites will not be successful (or worse, may be impossible to launch) without the full involvement of an expert in medical informatics. Such experts are, unfortunately, still in short supply. Their expertise differs substantially from data scientists who manipulate large health care claims databases, expertise that is also critical in the SERRI Program Office.
Education and Training
All SERRI sites have integrated first responder training into their onboarding process for new hires; most plan to include it in annual competency evaluations for bedside nurses. The SERRI program Site Liaisons provided simulation training workshops at HMH during Year 2 to train new personnel hired as second responders. To obviate the need to travel to HMH for simulation training, and for the sustainability of the program for Year 3 and beyond, the SERRI program is providing each site with resources needed to manage its own second responder training, including an advanced simulation manikin and educational materials.
Feedback provided to the SERRI Program Office by the second responders indicated that the simulation software purchased from the vendor focused largely on patients with septic shock, neglecting training for the care of patients with early sepsis. This was a major gap, given SERRI’s focus on the early recognition and definitive treatment of sepsis before it progresses to severe sepsis and septic shock. Accordingly, SERRI’s nurse educators developed simulation scenarios addressing early sepsis and have incorporated them into second responder training.
Evaluating the Effectiveness of the “Early Detection” and “Definitive ResPonse” Elements of the Intervention
The screening tool used by the first responders was developed and its measurement properties tested in patients in the surgical ICU.21 Now that time has passed, and the tool is being used in different populations, the SERRI team is planning to analyze whether its sensitivity, specificity, and predictive values are the same as in the test population. For example, the SERRI team is investigating anecdotal reports that some inpatients undergoing cancer chemotherapy appear to have a higher-than-average false-positive screening rate, generally because they have abnormally low white blood cell counts that are treatment- rather than sepsis-related. Some elderly inpatients appear to have a higher-than-average false-negative rate because their heart rates fail to increase even when sepsis is present. Whenever a measurement tool is used under different circumstances with different populations, its measurement properties must be reassessed. Moreover, the screening tool was designed to estimate the probability that sepsis is present and relies heavily on SIRS criteria.21 Information has since emerged that the clinical constellation of signs indicative of SIRS is neither specific 29 nor sensitive 30 for sepsis.
Changing the prognosis of sepsis depends not just on early detection but also on the institution of prompt, definitive treatment.31–34 SERRI’s second responders use standardized protocols, but, for most sites, the adequacy and timing of their implementation must be obtained by means of laborious chart review (time elapsed between a positive screen [T0] and notification of a second responder; time elapsed between T0 and the arrival of the second responder; time elapsed between T0 and the orders for fluid resuscitation, cultures, lactic acid measurement, and antibiotics). The difficulty of getting these data means that it is possible to establish compliance with the sepsis care protocols (analogous to a “pill count” in a drug study) only for a sample of SERRI patients. If analyses at the end of the project appear to show that the SERRI intervention is not effective or less effective than anticipated, poor implementation of the second responder protocols will be one possible explanation that will be challenging to rule out.
What’s Next
The CMS funding period for SERRI ends in June 2016; outcome analyses of this complex project will be a major endeavor for 2016. As we have reported, reductions in sepsis-associated inpatient death rates that occurred after the establishment of the program at the convener facility have been sustained through 2014.22 The key question for SERRI, as for all multicenter health care innovations, is the extent to which a complex intervention 35 will have similar effects when its features are modified—a process called “reinvention”36—so that it can be implemented in facilities that differ substantially along multiple dimensions. The impact of reinvention is not yet known, but by tracking how SERRI’s elements were modified, we hope to identify factors in the implementation process that affect the intervention’s robustness and exportability. Regarding SERRI’s postacute care sites, they have faced greater challenges in implementing the program than the acute care sites, and although sepsis is a common reason for returns to acute care from LTACHs and nursing homes,37,38 little data exist to serve as a footing for predictions about whether SERRI will have its hoped-for effects in such facilities. For the acute care sites, we think three factors may be most important: (1) automation of sepsis/SIRS screening, (2) the frequency of audit and feedback of screening results and patient outcomes, and (3) the staffing model for second responders. The extent to which the sepsis screening tool can be automated for use by bedside nurses affects nursing workload and, consequently, the proportion of targeted patients who are screened on admission and every 12 hours, and also drives the accuracy of the screening data. The level of automation of the screening tool also affects how often unit- or site-specific data on screening results and second response parameters can be fed back to local leaders. Audit and feedback is known to be a powerful motivator of behavior change for clinicians and leaders.39 Because the frequency of feedback depends on a site’s level of automation, SERRI’s effects may differ across sites on the basis of whether the screening tool is integrated, Web-based, or paper-based. As to the staffing models of second responders, some acute care hospitals had existing departments of NPs, while others had to hire new NPs for SERRI. Postacute care sites do not have NPs, relying instead on other personnel to serve as second responders; even though all those personnel successfully completed the intensive SERRI second responder training, not all have the credentials to write orders for patients, which delays the initiation of definitive treatment until a physician can be reached. Moreover, many of them have fixed clinical assignments (such as serving as charge nurse of an intensive care unit), which could impede their ability to evaluate a patient elsewhere in the hospital and start definitive treatment within that “golden hour” after the positive screen. We believe that NPs are the optimal second responders for the SERRI program. They do much more than evaluate and start treatment in patients with positive screens: They track the patients’ progress thereafter and follow up on orders; from a programmatic viewpoint, many of these empowered individuals have emerged as energetic leaders of their site’s SERRI. However, we have heard concerns that having NPs (who are salaried by the hospital) serve as sepsis second responders inappropriately offsets the responsibility of private-practice attending physicians (who are remunerated by insurers for caring for hospitalized patients). The evolving role of clinical nurse specialists in acute care hospitals in the United States deserves more research. Financial and professional-identity considerations aside, the evaluation and treatment of patients with suspected sepsis should adhere to evidence-based guidelines, and the literature supports nurses’ possibly pivotal role in delivering such care.40
Although SERRI has been successful in improving sepsis outcomes at the convener hospital 22 and has been successfully and widely implemented at other acute care and postacute care sites, it is too early yet to know whether it will improve outcomes on a programwide basis. For health care facilities interested in improving their sepsis care and patient outcomes, it should be clear from this article that launching and sustaining the SERRI intervention requires a major commitment of time, energy, and other resources. As is true with any clinical intervention, decisions to adopt a SERRI–like approach to sepsis before the final results are in should be made with caution.
Supplementary Material
Acknowledgments
The project described is supported by Funding Opportunity Number 1C1CMS330975-01-00 from the US Department of Health and Human Services, Centers for Medicare & Medicaid Services. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the US Department of Health and Human Services or any of its agencies. The research presented here was conducted by Houston Methodist. Findings might or might not be consistent with or confirmed by the independent evaluation contractor. The authors thank the leaders of the institutional members of the Texas Gulf Coast Sepsis Network (TGCSN) and all the individuals at the TGCSN sites who are implementing this program. The individual members of the TGCSN are, from the SERRI Program Office: Stephen L. Jones, MD; Carol M. Ashton, MD; Nelda P. Wray, MD; Lisa Kiehne; Mary Hall; Juan Nicolas; Theresa Pinn; Alexis Rose; Shirley Tran; from the Acute Care SERRI sites: Anyalebechi Agnes; Brandi Baez; Tessie Bautista; Charyl Bell-Gordon; Pamela Bond; Preciosima Bongat; Tunde Breaker; Debra Cassidy; Heather Chung; Kristen Cone; Kathleen Dassler; Janie Destefano; Daniel Didonato; Maureen Disbot; Stuart Dobbs, MD; Ashely Drews, MD; Victor Fainstein, MD; Shemaiah Fernandes; Wanda Ford, MD; Ronald Galfione, MD; Ricardo Garcia, MD; Elizabeth Gigliotti; Elizabeth Gonzales; Shaikh Hai, MD; Becky Halfon; Ken Hargett; Pat Harrison; Preema Joseph; Janet Leatherwood; Ricardo Lemos, MD; Johnnie Leonard; Patricia Lewis; Brenda Martinez; Faisal Masud, MD; Katie Miles; Tiffany Mundie; Nancy Musselman; Kelli Nations; Deborah O’Briant; Robert Ochoa, MD; Valerie Parker; Nancy Reeder; Stephanie Rosser; Benjamin Saldana, MD; Roberta Schwartz; Jennifer Steele; Linda Sun; Mary Thomas; Elaine Tracy; Alex Varkey; Carl Vartian, MD; Krendi Walls; Beverly Welch; Janice Zimmerman, MD; and from the Post-Acute Care SERRI sites: Chanelle Bort; Jane Dailey; Teresa Davis; Ibrahim Garcia, MD; Robert Griffith; Kevin Grimes, MD; Naman Mahajan; Laura Rodriguez; Dava Williams. A special acknowledgement goes to Frederick A. Moore, MD; Laura J. Moore, MD; Krista L Turner, MD; S. Rob Todd, MD; and Joseph F. Sucher, MD, for their work in developing the original paper sepsis screening tool that guided the development of the Web-based and automated screening tools that are a core component of this project.
Biographies
Stephen L. Jones, MD, MSHI, is Program Director, Sepsis Early Recognition and Response Initiative (SERRI), and Chief Clinical Informatics Officer, Department of Surgery, Houston Methodist Hospital; Division Chief of Health Informatics, Center for Outcomes Research, and Research Scientist and Assistant Member, Houston Methodist Research Institute; and Assistant Professor of Medical Informatics in Surgery, Weill Cornell Medical College, New York City.
Carol M. Ashton, MD, MPH, now retired, was John F. Jr. and Carolyn Bookout Professor of Surgical Quality & Outcomes Science, and Research Scientist, Department of Surgery, Methodist Institute for Technology, Innovation, and Education, Houston; Co-Director, Center for Outcomes Research; and Research Professor of Medicine in Surgery, Weill Cornell Medical College.
Lisa Kiehne, MHA, is Associate Program Director, SERRI.
Elizabeth Gigliotti, NP, APRN, ACNP-BC, formerly Nurse Practitioner, Houston Methodist Hospital, is Director, Nurse Practitioner Program, Houston Methodist West Hospital.
Charyl Bell-Gordon, DNP, RN, FNP-C, CEN, NEA-BC, formerly Director, Nurse Practitioner Program, Houston Methodist Hospital, is Director, Emergency Services, Houston Methodist San Jacinto Hospital.
Theresa T. Pinn, RN, is Post-Acute Care Site Liaison;
Shirley K. Tran, RN, is Acute Care Site Liaison, SERRI;
Juan C. Nicolas is Senior Applications Analyst; and
Alexis L. Rose, PhD, is Project Director.
Beverly A. Shirkey, PhD, is Biostatistician, Center for Outcomes Research.
Maureen Disbot, RN, CCRN, formerly Vice President, Quality Operations and Patient Safety, Houston Methodist Hospital and Vice President, Clinical Analytics, Houston Methodist Hospital System, is Vice President, Quality and Patient Safety, St Joseph Health System, Eureka, California.
Faisal Masud, MD, FCCP, FCCM, is Professor of Clinical Anesthesiology, Weill Cornell Medical College, and Medical Director, Critical Care, and Associate Quality Officer, Houston Methodist Hospital.
Nelda P. Wray, MD, MPH, now retired, was Co-Director, Center for Outcomes Research; Research Scientist, Department of Surgery, Methodist Institute for Technology, Innovation and Education; and Research Professor of Medicine in Surgery, Weill Cornell Medical College.
Footnotes
Field Notes provides a forum for brief reports on in-progress innovations in quality and patient safety. Readers are invited to send Field Notes proposals to Steven Berman at sberman@jcrinc.com.
Online Only Content
http://www.ingentaconnect.com/content/jcaho/jcjqs
See the online version of this article for
Appendix 1. Characteristics of Acute Care Hospitals Participating in the Texas Gulf Coast Sepsis Network (TGCSN), 2011 Data and Facility Plans for the Sepsis Early Recognition and Response Initiative (SERRI)
Appendix 2. Characteristics of Long Term Acute Care Hospitals (LTACHs) and Skilled Nursing Facilities (SNFs) Participating in the Texas Gulf Coast Sepsis Network, 2011 Data and Facility Plans for the Sepsis Early Recognition and Response Initiative (SERRI)
Appendix 3. Tailoring and Staggering of Sepsis Early Recognition and Response Initiative SERRI) Implementation Elements to Accommodate Site-Specific Realities and Conditions
Appendix 4. Sepsis Early Recognition and Response Initiative (SERRI) Program Site Implementation Assessment
References
- 1.Murphy SL, Xu J, Kochanek KD. Deaths: Final Data for 2010. Natl Vital Stat Rep. 2013 May 8;61(4):1–118. [PubMed] [Google Scholar]
- 2.Agency for Healthcare Research and Quality. Torio CM, Andrews RM. HCUP Statistical Brief 160. [Accessed Feb 2, 2016];National inpatient hospital costs: the most expensive conditions by payer, 2011. 2013 Aug; http://www.hcup-us.ahrq.gov/reports/statbriefs/sb160.pdf. [PubMed]
- 3.Agency for Healthcare Research and Quality. Pfuntner A, Weir LM, Stocks C. HCUP Statistical Brief 162. [Accessed Feb 2, 2016];Most frequent conditions in US hospitals, 2011. 2013 Sep; http://www.hcup-us.ahrq.gov/reports/statbriefs/sb162.pdf. [PubMed]
- 4.Agency for Healthcare Research and Quality. Pfuntner A, Weir LM, Stocks C. HCUP Statistical Brief 168. [Accessed Feb 2, 2016];Costs for hospital stays in the United States, 2011. 2013 Dec; http://www.hcup-us.ahrq.gov/reports/statbriefs/sb168-Hospital-Costs-United-States-2011.pdf. [PubMed]
- 5.Marshall JC, Dellinger RP, Levy M. The Surviving Sepsis Campaign: A history and a perspective. Surg Infect (Larchmt) 2010;11:275–281. doi: 10.1089/sur.2010.024. [DOI] [PubMed] [Google Scholar]
- 6.Levy MM, et al. The Surviving Sepsis Campaign: Results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med. 2010;36:222–231. doi: 10.1007/s00134-009-1738-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Whippy A, et al. Kaiser Permanente’s performance improvement system, part 3: Multisite improvements in care for patients with sepsis. Jt Comm J Qual Patient Saf. 2011;37:483–493. doi: 10.1016/s1553-7250(11)37061-4. [DOI] [PubMed] [Google Scholar]
- 8.Seoane L, et al. Using quality improvement principles to improve the care of patients with severe sepsis and septic shock. Ochsner J. 2013;13:359–366. [PMC free article] [PubMed] [Google Scholar]
- 9.Nguyen HB, et al. Implementation of a bundle of quality indicators for the early management of severe sepsis and septic shock is associated with decreased mortality. Crit Care Med. 2007;35:1105–1112. doi: 10.1097/01.CCM.0000259463.33848.3D. [DOI] [PubMed] [Google Scholar]
- 10.Miller RR, 3rd, et al. Multicenter implementation of a severe sepsis and septic shock treatment bundle. Am J Respir Crit Care Med. 2013;188:77–82. doi: 10.1164/rccm.201212-2199OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zubrow MT, et al. Improving care of the sepsis patient. Jt Comm J Qual Patient Saf. 2008;34:187–191. doi: 10.1016/s1553-7250(08)34022-7. [DOI] [PubMed] [Google Scholar]
- 12.Rhee C, Gohil S, Klompas M. Regulatory mandates for sepsis care— Reasons for caution. N Engl J Med. 2014 May 1;370;:1673–1676. doi: 10.1056/NEJMp1400276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Medicare & Medicaid Services. [Accessed Feb 2, 2016];CMS to Improve Quality of Care During Hospital Inpatient Stays. 2014 Aug 4; https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2014-Fact-sheets-items/2014-08-04-2.html.
- 14.National Quality Forum (NQF) Severe Sepsis and Septic Shock: Management Bundle. [Accessed Feb 2, 2016];Measure Submission and Evaluation Worksheet 5.0. (Updated: Oct 5, 2012.) http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifer=ID&ItemID=71548.
- 15.Centers for Medicare Medicaid Services. The Joint Commission. [Accessed Feb 2, 2016];Specifications Manual for National Inpatient Quality Measures, version 5.0b. 2015. http://www.jointcommission.org/assets/1/6/NHQM_v5_0_b_PDF_11_13_2015.zip.
- 16.Centers for Medicare & Medicaid Services CMS Financial Report: Transforming Health Care for All Americans. [Accessed Feb 2, 2016];Fiscal Year 2013. 2013 Dec 16; https://www.cms.gov/CFOReport.
- 17.US Department of Health and Human Services, Office of Inspector General. [Accessed Feb 2, 2016];Medicare Hospital Outlier Payments Warrant Increased Scrutiny. Levinson DR. Nov 2013. OEI-06-10-00520. http://www.oig.hhs.gov/oei/reports/oei-06-10-00520.pdf.
- 18.Iwashyna TJ, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010 Oct 27;304:1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hall MJ, et al. Inpatient care for septicemia or sepsis: A challenge for patients and hospitals. NCHS Data Brief. 2011;(62):1–8. [PubMed] [Google Scholar]
- 20.Centers for Medicare & Medicaid Services. [Accessed Feb 2, 2016];The CMS Innovation Center. https://innovation.cms.gov/
- 21.Moore LJ, et al. Validation of a screening tool for the early identification of sepsis. J Trauma. 2009;66:1539–1547. doi: 10.1097/TA.0b013e3181a3ac4b. [DOI] [PubMed] [Google Scholar]
- 22.Jones SL, et al. Reductions in sepsis mortality and costs after design and implementation of a nursing-based early recognition and response program. Jt Comm J Qual Patient Saf. 2015;41:483–491. doi: 10.1016/s1553-7250(15)41063-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Casey DE, Jr, Chang K, Bustami RT. Evaluation of hospitalization for infections that are present on admission. Am J Med Qual. 2011;26:468–473. doi: 10.1177/1062860611409198. [DOI] [PubMed] [Google Scholar]
- 24.Liu V, et al. Hospital deaths in patients with sepsis from 2 independent cohorts. JAMA. 2014 Jul 2;312:90–92. doi: 10.1001/jama.2014.5804. [DOI] [PubMed] [Google Scholar]
- 25.Angus DC, et al. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Angus DC, Wax RS. Epidemiology of sepsis: An update. Crit Care Med. 2001;29(7 Suppl):S109–S116. doi: 10.1097/00003246-200107001-00035. [DOI] [PubMed] [Google Scholar]
- 27.Iwashyna TJ, et al. Identifying patients with severe sepsis using administrative claims: Patient-level validation of the Angus implementation of the International Consensus Conference definition of severe sepsis. Med Care. 2014;52:e39–e43. doi: 10.1097/MLR.0b013e318268ac86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jones SL, et al. Outcomes and resource use of sepsis-associated stays by presence on admission, severity, and hospital type. Med Care. doi: 10.1097/MLR.0000000000000481. Epub 2016 Jan 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Horeczko T, Green JP, Panacek EA. Epidemiology of the systemic inflammatory response syndrome (SIRS) in the emergency department. West J Emerg Med. 2014;15:329–336. doi: 10.5811/westjem.2013.9.18064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaukonen KM, et al. Systemic inflammatory response syndrome criteria in defining severe sepsis. N Engl J Med. 2015 Apr 23;372:1629–1638. doi: 10.1056/NEJMoa1415236. [DOI] [PubMed] [Google Scholar]
- 31.Yealy DM, et al. A randomized trial of protocol-based care for early septic shock. N Engl J Med. 2014 May 1;370:1683–1693. doi: 10.1056/NEJMoa1401602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mouncey PR, et al. Trial of early, goal-directed resuscitation for septic shock. N Engl J Med. 2015 Apr 2;372:1301–1311. doi: 10.1056/NEJMoa1500896. [DOI] [PubMed] [Google Scholar]
- 33.Peake SL, et al. Goal-directed resuscitation for patients with early septic shock. N Engl J Med. 2014 Oct 14;371:1496–1506. doi: 10.1056/NEJMoa1404380. [DOI] [PubMed] [Google Scholar]
- 34.Gupta RG, et al. Early goal-directed resuscitation of patients with septic shock: Current evidence and future directions. Crit Care. 2015 Aug 28;19:286. doi: 10.1186/s13054-015-1011-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Craig P, et al. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ. 2008 Sep 29;337:a1655. doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rogers EM. Diffusion of Innovations. 4th. New York City: Free Press; 1995. [Google Scholar]
- 37.Kollef MH, et al. Epidemiology, microbiology and outcomes of healthcare-associated and community-acquired bacteremia: A multicenter cohort study. J Infect. 2011;62:130–135. doi: 10.1016/j.jinf.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 38.White AC, et al. Unplanned transfers following admission to a long-term acute care hospital: A quality issue. Chron Respir Dis. 2011;8:245–252. doi: 10.1177/1479972311424514. [DOI] [PubMed] [Google Scholar]
- 39.Ivers N, et al. Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012 Jun 13;6:CD000259. doi: 10.1002/14651858.CD000259.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gurzick M, Kesten KS. The impact of clinical nurse specialists on clinical pathways in the application of evidence-based practice. J Prof Nurs. 2010;26:42–48. doi: 10.1016/j.profnurs.2009.04.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.