Abstract
Purpose
Fewer emergency department (ED) visits may be a potential indicator of quality of care during the end of life. Receipt of palliative care, such as that offered by the adult Palliative Care Service (PCS) in Halifax, Nova Scotia, is associated with reduced ED visits. In June 2004, an integrated service model was introduced into the Halifax PCS with the objective of improving outcomes and enhancing care provider coordination and communication. The purpose of this study was to explore temporal trends in ED visits among PCS patients before and after integrated service model implementation.
Methods
PCS and ED visit data were utilized in this secondary data analysis. Subjects included all adult patients enrolled in the Halifax PCS between January 1, 1999 and December 31, 2005, who had died during this period (N = 3221). Temporal trends in ED utilization were evaluated dichotomously as preintegration or postintegration of the new service model and across 6-month time blocks. Adjustments for patient characteristics were performed using multivariate logistic regression.
Results
Fewer patients (29%) made at least one ED visit postintegration compared to the preintegration time period (36%, p < 0.001). Following adjustments, PCS patients enrolled postintegration were 20% less likely to have made at least one ED visit than those enrolled preintegration (adjusted OR 0.8; 95% confidence interval 0.6–1.0).
Conclusion
There is some evidence to suggest the introduction of the integrated service model has resulted in a decline in ED visits among PCS patients. Further research is needed to evaluate whether the observed reduction persists.
Introduction
Emergency departments (EDs) tend to be fast-paced, stressful environments where the focus is on diagnosis and treatment for acute or traumatic events.1,2 Most EDs are not designed to provide quality end-of-life care. ED physicians have little information at their disposal to guide their decisions with respect to end-of-life care and cannot provide the privacy and support required by dying patients and their families and caregivers.1,3,4 Many patients present to the ED seeking symptom relief, caregiver reassurance, and support; others are forced to visit the ED because death is imminent and they are unable or unwilling to die at home.1,3,5
Fewer ED visits during the last month of life is identified as a potential indicator of quality of care during the end of life.6,7 However, there is evidence indicating visits during the terminal period may be increasing among patients with advanced chronic disease.8,9 In 2001, 27% of patients with cancer in Ontario made at least one ED visit during their last 2 weeks of life.10
Palliative care programs or services (PCS) have been associated with a reduction in the number of ED visits made by enrolled patients.11–14 In Nova Scotia, Canada, patients with advanced cancer were 15% less likely to make at least one visit to the ED during the last 6 months of life if enrolled with a comprehensive PCS, even after controlling for many potentially influential covariates.13
The adult PCS in Halifax, Nova Scotia, based at the Queen Elizabeth II Health Sciences Centre (QEII HSC), has been providing clinical care to the local community for over 21 years. Initial electronic data collection began in 1983.15 Over time the program has expanded to provide service delivery to all sectors of the community and in 1997 saw approximately 62% of all adults who died due to cancer in the Halifax Regional Municipality.16 A multidisciplinary team follows patients across care settings, including the home, an outpatient clinic, an inpatient palliative care unit, and throughout the QEII HSC hospital sites. Today the PCS is expected to meet the needs of terminal adult patients throughout the Capital District Health Authority (CDHA). In June 2004, changes were introduced with the launch of the integrated service model (ISM) with the objectives to improve outcomes for patients and families and enhance coordination and communication among care providers. Key features of the newly named Capital Health Integrated Palliative Care Service (CHIPCS) include a shared care service model in the community emphasizing coordinated care among all health providers. Primary components include the creation of geographic community care teams composed of family physicians, home care coordinators, home visiting nurses, and hospital-based palliative care home consult physicians and nurses. Access to palliative care consult teams was simplified, assessment tools and care plans standardized, data collection centralized, and a traveling integrated home chart introduced. Governance committees were put into place and a memorandum of understanding between the Nova Scotia provincial home care program and district health services agreed upon.17 There is no standardized ISM in Canada. Regions across Canada use a variation of the ISM. Because health care is provincially administered, the ISM used by CHIPCS is considered the standard for Nova Scotia.
Given the key features of this integrated model and the program objective to improve patient and caregiver outcomes, we postulated that changes in home management of PCS patients could potentially lead to a reduction in the use of the ED. The objective of this study was to examine temporal trends in ED visits among PCS patients following enrollment and to examine the effect of the implementation of the ISM.
Method
Subjects
All patients enrolled in the adult PCS in Halifax, Nova Scotia, between January 1, 1999 and December 31, 2005 who had died during this 7-year period were initially considered as subjects for this retrospective, population-based study. We will refer to the years prior to the implementation of the new ISM as preintegration and the time period from integration onward (June 2004) as postintegration. To ensure each patient had the potential to visit the ED at least once during the period from PCS enrollment to death, patients who spent the full time period as a hospital inpatient were excluded. Also excluded were patients enrolled in the service with residence in a geographic region beyond the maximum boundary commonly served by the QEII HSC ED. Although some living outside the catchment area may have visited the QEII HSC ED, providers in the ED and the PCS felt it more likely this group of patient’s would have sought immediate help in community hospitals much nearer to their home.
Data
Data pertaining to enrolled patients were extracted from the PCS database. Variables included each patient’s enrollment date, gender, birth date, death date, location of death, postal code, diagnosis, caregiver status, reason for referral, and a unique patient identifier. Transition information in the PCS database allowed for the calculation of total hospital in-patient time following PCS admission. Income information is not captured, therefore, data from the 2001 Canadian Census associated with each subject’s residential postal code was used to develop an ecological indicator of “neighborhood” income as well as a census indicator of urban or rural residency. When applying such measures, interpretation of the findings is best limited to the community where people live and not to individuals.18–20
During the time period of this study, ED visits were captured within the Emergency Department Information System of the QEII HSC. ED visit information included the date, time of day, mode of arrival, diagnosis, major complaint, and outcome. For each eligible subject, the total ED visits made to the QEII HSC ED from the initial date of PCS enrollment to their date of death were counted and linked to PCS information via each patient’s unique identifier. Due to the highly skewed distribution displayed, total ED visits were dichotomized for subsequent analysis (no visits versus at least one visit).
Temporal trends in ED visits before and after the implementation of the ISM to the PCS were evaluated in two ways. First, each patient’s year of enrollment was dichotomized as being either before the introduction of the ISM, (preintegration: enrollment January 1999 to May 31, 2004) or following (postintegration: enrollment from June 1, 2004 to December 31, 2005). Next, each calendar year of enrollment was split into 1 of 14 6-month time blocks (January 1 to May 31, 1999–2005; June 1 to December 31, 1999–2005) in order to illustrate a more detailed representation of ED utilization over time. Six-month time blocks were selected since survival among patients in the PCS following enrollment tends to be relatively short and few survive more than 6 months.21,22
To account for the variability in the number of days each patient would have had the “potential” to visit the ED, a variable capturing the total days of ED “potential” time was created. Patients spending more time in the PCS and not as a hospital inpatient would have a greater potential of having made at least one ED visit. Total ED “potential” time was defined as the number of days between PCS enrollment to date of death (survival) minus the total number of days each patient spent as a hospital inpatient.
Analysis
Initial descriptive analysis (frequencies, measures of central tendency and dispersion) of study variables was followed by cross tabulations to assess the association of patient and ED visit characteristics to enrollment period. Differences between categorical variables were assessed using χ2 analysis; for continuous variables, Student’s t tests or Wilcoxon rank sum tests were used. To examine the association of enrollment period on having made at least one ED visit, univariate and multivariate logistic regression techniques were used. Enrollment period was treated first as a dichotomy (postintegration versus preintegration) and then as 6-month time blocks. Manual backwards elimination modeling was used to develop the most parsimonious multivariate model of at least one ED visit and time period of PCS enrollment. Patient variables included in the initial multivariate model began with all factors found to be significantly associated with ED visits at the p = 0.1 level in the unadjusted analyses. All patient characteristics retained in the final adjusted model were significant at the p = 0.05 level of significance. Statistical analyses were performed using SAS 9.0.23
Ethical approval was provided by the Research Ethics Board of the CDHA, Nova Scotia.
Results
In total, 5965 patients were enrolled with the PCS and died over the 7-year study period. Of this group, 1521 who did not live within the maximum geographical boundary commonly serviced by the program were excluded. An additional 1223 were deemed ineligible because they were hospital inpatients from the date of PCS enrollment to death and did not have ED visit potential. Exclusion of these patients resulted in 3221 eligible study subjects. Overall, 2033 ED visits were made by patients during the study period.
Table 1 summarizes patient characteristics by enrollment to the PCS before or after implementation of the ISM. Overall, 35% of eligible patients made at least one visit to the ED after enrollment to the service. Significantly fewer patients (29%) made at least one ED visit postintegration compared to the preintegration time period (36%, p < 0.001). Patients enrolled preintegration or postintegration differed significantly (p < 0.05) with respect to gender, diagnosis, pain as a primary reason for referral, and ED potential days. A greater proportion of males and patients with cancer and comorbidities were enrolled in the service postintegration. Fewer patients during the postintegration period were referred to the PCS due to pain. Survival time and hence, ED potential time varied widely between the two time periods. This was not unexpected given the short calendar time period represented by the postintegration period (19 months) compared to the preintegration (65 months) and the criterion that PCS patients had to have died during the 7-year time period for inclusion in the study.
Table 1.
Characteristics of Eligiblea Patients Admitted to the Adult Palliative Care Service (PCS) by Admission Preintegration or Postintegrated Service Implementation (N = 3221)
| Characteristic | Number of patients (%)
|
|
|---|---|---|
| Preintegration (January 1999 to June 2004) (n = 2615) | Postintegration (July 2004 to December 2005) (n = 606) | |
| Emergency department visits* | ||
| None | 1674 (64.0) | 431 (71.1) |
| At least one | 941 (36.0) | 175 (28.9) |
| Emergency department visits* | ||
| Mean (standard deviation) | 0.7 (1.3) | 0.5 (0.9) |
| Median (range) | 0 (0–14) | 0 (0–8) |
| Gender↑ | ||
| Female | 1343 (51.4) | 282 (46.5) |
| Male | 1271 (48.6) | 324 (53.5) |
| Age, years | ||
| <65 | 841 (32.2) | 189 (31.2) |
| 65–74 | 689 (26.4) | 164 (27.1) |
| 75–84 | 743 (28.5) | 168 (27.7) |
| 85+ | 337 (12.9) | 85 (14.0) |
| Age, years | ||
| Mean (standard deviation) | 69.8 (13.5) | 70.6 (13.5) |
| Median (range) | 72 (16–108) | 72 (16–99) |
| Location of death | ||
| Hospital death (not in PCP unit) | 670 (25.6) | 146 (24.1) |
| Palliative care unit | 668 (25.6) | 175 (28.9) |
| Home | 1175 (45.0) | 264 (43.6) |
| Long-term care facility | 101 (3.9) | 21 (3.5) |
| Census residency indicator | ||
| Urban | 2192 (86.3) | 507 (85.2) |
| Rural | 349 (13.7) | 88 (14.8) |
| Neighborhood income quintile | ||
| Low | 516 (20.3) | 114 (19.2) |
| Lower middle | 485 (19.1) | 113 (19.0) |
| Middle | 514 (20.2) | 126 (21.2) |
| Upper middle | 504 (19.8) | 120 (20.2) |
| Upper | 522 (20.5) | 122 (20.5) |
| Diagnostic summary↑↑ | ||
| Cancer only | 2213 (85.4) | 376 (62.5) |
| Other disease, no cancer | 254 (9.8) | 65 (10.8) |
| Cancer and comorbidities | 126 (4.9) | 161 (26.7) |
| Caregiver relationship | ||
| Spouse or common law spouse | 1339 (54.2) | 312 (55.8) |
| Child | 765 (31.0) | 178 (31.8) |
| Parents/other relations | 282 (11.4) | 51 (9.1) |
| Friend/other | 86 (3.5) | 18 (3.2) |
| Caregiver lives with patient | ||
| Yes | 1646 (62.9) | 389 (64.2) |
| No | 969 (37.1) | 217 (35.8) |
| Primary reasons for referral to PCS (responses are not exclusive) | ||
| Pain§ (yes) | 1099 (42.0) | 220 (36.3) |
| Other symptoms (yes) | 1294 (49.5) | 298 (49.2) |
| Survival↑↑ (days from admission to PCS to death) | ||
| Mean (standard deviation) | 145.2 (210.2) | 79.1 (81.2) |
| Median (range) | 72 (1–2236) | 50.5 (1–484) |
| Total acute hospital (inpatient) days | ||
| Mean (standard deviation) | 16.2 (33.8) | 13.9 (24.4) |
| Median (range) | 6 (0–979) | 5 (0–227) |
| “ED Potential”↑↑ days (total survival–total inpatient days) | ||
| Mean (standard deviation) | 129 (202.7) | 65.2 (74.6) |
| Median (range) | 57 (1–2223) | 38.5 (1–484) |
| “ED Potential”↑↑ days (categorized) | ||
| 1–31 | 898 (34.3) | 260 (42.9) |
| 32–93 | 760 (29.1) | 208 (34.3) |
| 94+ | 957 (36.6) | 138 (22.8) |
Residents of geographic region served by the Halifax PCS and having at least 1 day “ED potential.”
χ2 tests of association, student t tests or Wilcoxon rank sum scores:
p < 0.001;
p < 0.05;
p < 0.0001;
p < 0.01.
Characteristics of ED visits by preintegration or postintegration are presented in Table 2. Among those who made at least one ED visit, the mean number of visits did not differ significantly (p = 0.06). No differences were evident between the timing of ED visits (day of week, hour), mode of arrival or visit outcome. A significant difference was evident with respect to the major complaint for the visit (p < 0.0001). Although shortness of breath was the most common major complaint recorded during the preintegration period, the proportion citing this complaint declined markedly postintegration.
Table 2.
Characteristics of Emergency Department Visits Made by Patients Admitted to the Palliative Care Service by Admission Preintegrated or Postintegrated Service Implementation
| Characteristic | Number of ED visits (%)
|
|
|---|---|---|
| Preintegration (January 1999 to June 2004) (n = 1750) | Postintegration (July 2004 to December 2005) (n = 283) | |
| Total ED visits (by unique patients) | ||
| 1 | 581 (61.7) | 110 (62.9) |
| 2 | 172 (18.3) | 41 (23.4) |
| 3 | 89 (9.5) | 16 (9.1) |
| 4 or more | 99 (10.5) | 8 (4.6) |
| Mean (standard deviation [SD]) | 1.9 (1.8) | 1.6 (1.1) |
| Median (range) | 1.0 (1–18) | 1.0 (1–8) |
| Day of week presenting to ED | ||
| Monday | 248 (14.2) | 32 (11.3) |
| Tuesday | 259 (14.8) | 43 (15.2) |
| Wednesday | 231 (13.2) | 35 (12.4) |
| Thursday | 235 (13.4) | 40 (14.1) |
| Friday | 250 (14.3) | 47 (16.6) |
| Saturday | 257 (14.7) | 32 (11.3) |
| Sunday | 270 (15.4) | 54 (19.1) |
| ED registration during weekend | ||
| Yes | 527 (30.1) | 86 (30.4) |
| No | 1223 (69.9) | 197 (69.6) |
| ED after-hours registration (17:00–7:59) | ||
| Yes | 851 (48.6) | 137 (48.4) |
| No | 899 (51.4) | 146 (51.6) |
| Mode of arrival to ED | ||
| Transport self | 120 (6.9) | 18 (6.4) |
| By a relative | 616 (35.2) | 96 (33.9) |
| Emergency medical care | 977 (55.9) | 159 (56.2) |
| Friend | 30 (1.7) | 7 (2.5) |
| Other/taxi/police | 5 (0.3) | 3 (1.1) |
| Major complainta,* | ||
| Shortness of breath | 387 (22.1) | 17 (6.0) |
| Abdominal pain | 169 (9.7) | 32 (11.3) |
| Pain (not abdominal) | 267 (15.3) | 34 (12.0) |
| Nausea/vomiting | 82 (4.7) | 14 (5.0) |
| Fever | 42 (2.4) | 11 (3.9) |
| Weakness/fatigue/malaise | 131 (7.5) | 21 (7.4) |
| Confusion/unconscious/dizzy | 84 (4.8) | 22 (7.8) |
| Blocked tubes (feeding/catheters/drains) | 68 (3.9) | 14 (5.0) |
| Bleeding | 83 (4.7) | 13 (4.6) |
| Falls/fractures/trauma/lacerations | 29 (1.7) | 9 (3.2) |
| Other | 408 (23.3) | 96 (33.9) |
| Diagnosis | ||
| Respiratory system | 330 (18.9) | 52 (18.4) |
| Neoplasms | 221 (12.6) | 20 (7.1) |
| Mental disorders | 14 (0.8) | 1 (0.4) |
| Circulatory system | 93 (5.3) | 10 (3.5) |
| Digestive system | 74 (4.2) | 7 (2.5) |
| Genitoruinary system | 63 (3.6) | 4 (1.4) |
| Musculoskeletal system | 56 (3.2) | 8 (2.8) |
| Injury and poisoning | 127 (7.3) | 21 (7.4) |
| General symptoms, ill defined | 358 (20.5) | 66 (23.3) |
| Other | 69 (3.9) | 11 (3.9) |
| Outcome | ||
| Admitted | 923 (52.7) | 151 (53.4) |
| Treatment completed/d/c/home | 721 (41.2) | 104 (36.8) |
| Treatment discontinued | 31 (1.8) | 7 (2.5) |
| Patient expired-died | 12 (0.7) | 2 (0.7) |
| Clinic appointment scheduled | 10 (0.6) | 1 (0.4) |
| Surgery required—sent to OR | 3 (0.2) | 2 (0.7) |
| Left against medical advice | 2 (0.1) | 0 (0.0) |
| Missing | 48 (2.7) | 16 (5.7) |
The complaint data filed was available only as free text to which category groupings were applied.
χ2 tests of association, Student’s t tests, or Wilcoxon rank sum scores:
p < 0.0001.
ED, emergency department; OR, odds ratio.
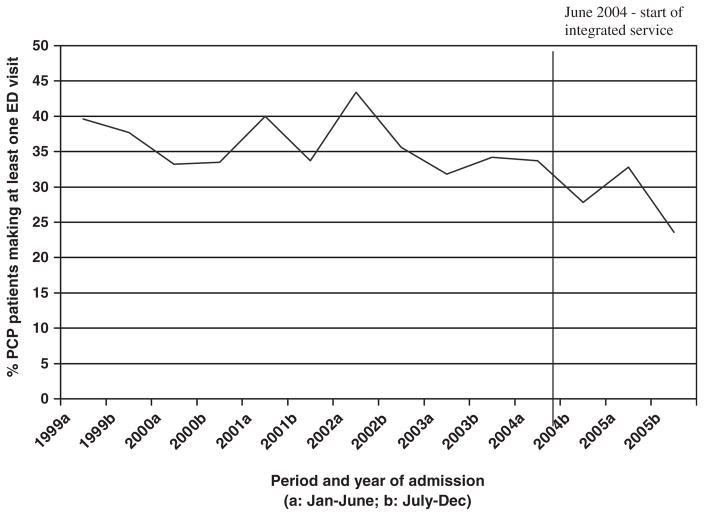
The proportion of patients who made at least one visit to the ED over the 7-year study period by 6-month time blocks is illustrated in Figure 1. A statistically significant (p = 0.008) downward trend in ED visits over time is evident.
FIG. 1.
Proportion of adult palliative care service patients making at least one emergency department (ED) visit over time. Does not account for total ED “potential” days.
Results of the logistic regression analyses assessing the effect of program enrollment period, dichotomously and by 6-month time blocks, on having made at least one ED visit after enrollment to the PCS are presented in Table 3. In the assessment of service enrollment as a dichotomy (preintervention or postintegration), patients enrolled postintegration were less likely to have made at least one ED visit than patients enrolled preintegration (adjusted odds ratio [AOR] 0.8; 95% confidence interval [CI] 0.6, 1.0). This result is after accounting for all retained significant patient covariates in the model (ED potential time, age, location of death, caregiver relationship, pain as primary reason for referral, and the census residency indicator). In the unadjusted model, enrollment period, treated as 6-month time blocks was significantly associated with ED visits. However this relationship did not remain significant after adjustments for total ED potential time and other retained patient characteristics. Nonetheless, a downward trend in the likelihood of palliative care patients making at least one ED visit after the implementation of the ISM remained evident.
Table 3.
Adjusted Odds of Making at Least One Emergency Department Visit, Changes Over Time by Period of Admission
| Period of admission | Odds ratio; 95% confidence interval
|
|
|---|---|---|
| Unadjusted | Adjusteda | |
| Period of admission | ||
| Preintegrated program | 1.0 | 1.0 |
| Postintegrated program | 0.7 (0.6, 0.9) | 0.8 (0.6, 1.0) |
| p < 0.001 | p = 0.02 | |
| Period and year of admission in 6-month time blocks | ||
| 1999a (January to June) | 1.2 (0.8, 1.8) | 1.3 (0.9, 2.0) |
| 1999b (July to December) | 1.2 (0.8, 1.8) | 1.1 (0.7, 1.6) |
| 2000a (January to June) | 0.9 (0.6, 1.3) | 0.8 (0.5, 1.2) |
| 2000b (July to December) | 0.9 (0.6, 1.3) | 0.9 (0.6, 1.4) |
| 2001a (January to June) | 1.2 (0.8, 1.8) | 1.2 (0.8, 1.8) |
| 2001b (July to December) | 1.0 (0.6, 1.4) | 0.9 (0.6, 1.4) |
| 2002a (January to June) | 1.4 (1.0, 2.1) | 1.4 (0.9, 2.1) |
| 2002b (July to December) | 1.0 (0.7, 1.5) | 1.0 (0.7, 1.5) |
| 2003a (January to June) | 0.9 (0.6, 1.3) | 0.9 (0.6, 1.3) |
| 2003b (July to December) | 0.9 (0.6, 1.3) | 1.0 (0.6, 1.5) |
| 2004ab (January to June) | 1.0 | 1.0 |
| 2004b (July to December) | 0.7 (0.5, 1.1) | 0.7 (0.5, 1.1) |
| 2005a (January to June) | 0.9 (0.6, 1.3) | 0.9 (0.6, 1.4) |
| 2005b (July to December) | 0.5 (0.3, 0.8) | 0.7 (0.4, 1.2) |
| p = 0.003 | p = 0.08 | |
Adjusted for age, location of death, caregiver relationship, census indictor of urban or rural residency, pain as primary reason for program referral and total potential days to make an ED visit.
Program implementation.
ED, emergency department.
Discussion
Although the study period after the implementation of the ISM to the PCS was limited, our results suggest patients enrolled to the service postintegration were visiting the ED less often. This is in keeping with results reported by others11,12,14 who report significantly fewer ED visits among patients receiving care from an interdisciplinary in-home palliative care team than patients provided “usual” end-of-life care. Additional data capturing patient enrollment and ED visits beyond 2005 are required in order to determine whether the decline evidenced is a function of service changes or represents random variation in ED use and/or a reflection of overall ED utilization in the general population. Administrative records within the QEII HSC (M. Greenan, personal communication, 2007) indicate ED visits among the general population of the region served declined steadily from 74,088 visits in 1999 to 58,608 in 2004, then remained stable in 2005. During this same time period we found that ED visits among PCS patients also declined from 388 in 1999 to 267 in 2004. In 2005, the first full year after the implementation of the ISM, ED visits among postintegration PCS patients decreased substantially to only 169, albeit with a great deal of variability. In contrast, ED visits by the general population did not change in 2005 from the previous year. This reduction in ED visits among postintegration PCS patients but not among the general populace supports the premise that changes in home management of PCS patients may have lead to a reduction in the use of the ED.
An objective of the ISM implementation was to improve patient and family outcomes during the end of life. One goal was to see patients being cared for in a location best suited to their desires and needs by health care providers best informed about their condition and care preferences. In the ED, privacy is limited, staff are not familiar to the patients, nor are they trained to deal with many issues associated with the end of life, and care preferences, such as advance care directives, are not always known.1,3,5 For many, reducing or eliminating unnecessary visits to the ED is viewed as an indicator of improved quality of care.6,7,24 Although there are circumstances where a visit to the ED is required and thus the best location for care, an integrated, interdisciplinary service model can, as our research and others12 suggest, reduce potentially unnecessary ED visiting.
Close attention to symptom control and anticipatory care planning, involving the patient, their family and providers in an integrated fashion are aimed at minimizing unnecessary ED use. Many ED visits tend to be made because patients and their family members are unsure of how to access care.1,3 As part of the ISM a health care provider is identified to act as the continuity person for the patient and their family. Clear instructions are provided in how to contact this provider during and after hours so that help may be obtained directly from the PCS as opposed to accessing care via the ED. Symptom management or minor adjustments to medications are common reasons for ED visits.1,3 The integrated PCS addresses these issues by providing patient and family education and coaching advice. The marked decline in breathing problem complaints postintegration may be a reflection of these initiatives.
In our previous research25 half of PCS patients visiting the ED were admitted to the hospital. In the literature, patients receiving improved home interdisciplinary services were admitted to hospital less often.12 In this study admissions remained constant while ED visits declined. We postulate that patients choosing to present to the ED were likely sicker and more appropriate for ED visits, hence the need for admission. A goal of the ISM is to reduce ED visits by patients who could receive the appropriate care via an alternative route, thus avoiding prolonged waits and care in an environment ill-prepared for end-of-life issues.
Benefits of reduced ED visiting are not limited to patients and their families. Fewer visits to the ED can also equate to lower health care costs, as well as greater satisfaction with care among patients and their families.11,12,14
The significant disparity in the number of days each patient had the potential to make an ED visit between the preintegration and postintegration periods, highlights the importance of statistically adjusting for this variable. Patients enrolled during the preintegration period incurred almost twice as many ED potential days than postintegration. This was due to a much longer time period being available for potential survival time, the period between initial service enrollment and death. The postintegration period was relatively short (19 months) compared to the preintegration period (65 months), as such patients who enrolled and died during the shorter postintegration period would experience a shorter survival. In addition, it is likely that patients’ enrolled postintegration would represent those with more advanced terminal disease. In our adjusted analysis, the strength of the association between ED visits and period of enrollment (preintegration or postintegration) decreased markedly from the unadjusted, but remained significant.
Our study has several limitations. First, ED information was available only from visits made to the QEII HSC ED. Although the QEII HSC ED is the largest in Nova Scotia and is located in the same site as the PCS, it is possible that some eligible patients could have made ED visits to other community EDs. Second, the postintegration time period under study was short. As discussed above, additional years of ED visit information among postintegration PCS patients is required in order to evaluate whether the decline in visits is the result of program change or random variation. As well, the study would benefit from the inclusion of a comparison group of residents during the end-of-life who are not enrolled in the PCS. We also acknowledge that other factors may also contribute to the decline in ED visits among palliative patients, such as enhanced ED services elsewhere in the region.
Conclusion
Results from this study suggest there is a decline in the number of ED visits after the implementation of an ISM to the PCS of the QEII HSC (renamed as CHIPCS). Our study is an attempt to use “real time, real-world” program data to answer questions about the effectiveness of program design and implementation. Further research will add more postintegration data. Additional information over a longer time frame postintegration is required in order to evaluate whether the observed decrease in ED visits is a persistent phenomena. We are continuing to collect such data.
Acknowledgments
This work was supported financially by a grant from the Capital Health Research Fund.
Footnotes
Author Disclosure Statement
No competing financial interests exist.
No reprints are available.
References
- 1.Chan GK. End-of-life models and emergency department care. Acad Emerg Med. 2004;11:79–86. doi: 10.1197/j.aem.2003.07.019. [DOI] [PubMed] [Google Scholar]
- 2.Chan GK. Understanding end-of-life caring practices in the emergency department: Developing Merleau-Ponty’s notions of intentional arc and maximum grip through praxis and phronesis. Nurs Philos. 2005;6:19–32. doi: 10.1111/j.1466-769X.2004.00204.x. [DOI] [PubMed] [Google Scholar]
- 3.Marco CA, Schears RM. Death, dying, and last wishes. Emerg Med Clin North Am. 2006;24:969–987. doi: 10.1016/j.emc.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 4.Heaston S, Beckstrand RL, Bond AE, Palmer SP. Emergency nurses’ perceptions of obstacles and supportive behaviors in end-of-life care. J Emerg Nurs. 2006;32:477–485. doi: 10.1016/j.jen.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 5.Tardy B, Venet C, Zeni F, Berthet O, Viallon A, Lemaire F, Bertrand JC. Death of terminally ill patients on a stretcher in the emergency department: A French specialty? Intensive Care Med. 2002;28:1625–1628. doi: 10.1007/s00134-002-1517-x. [DOI] [PubMed] [Google Scholar]
- 6.Earle CC, Park ER, Lai B, Weeks JC, Ayanian JZ, Block S. Identifying potential indicators of the quality of end-of-life cancer care from administrative data. J Clin Oncol. 2003;21:1133–1138. doi: 10.1200/JCO.2003.03.059. [DOI] [PubMed] [Google Scholar]
- 7.Earle CC. Evaluating claims-based indicators of the intensity of end-of-life cancer care. Int J Qual Health Care. 2005;17:505–509. doi: 10.1093/intqhc/mzi061. [DOI] [PubMed] [Google Scholar]
- 8.Earle CC, Neville BA, Landrum MB, Zyanian JZ, Block SD, Weeks JC. Trends in the aggresiveness of cancer care near the end of life. J Clin Oncol. 2004;22:315–321. doi: 10.1200/JCO.2004.08.136. [DOI] [PubMed] [Google Scholar]
- 9.Burge FI, Lawson B, Johnston G, Flowerdew G. Health care restructuring and family physician care for those who died of cancer. BMC Fam Pract. 2005;6:1. doi: 10.1186/1471-2296-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barbera L, Paszat L, Chartier C. Indicators of poor quality end-of-life cancer care in Ontario. J Palliat Care. 2006;22:12–17. [PubMed] [Google Scholar]
- 11.Brumley RD, Enguidanos S, Cherin DA. Effectiveness of a home-based palliative care program for end-of-life. J Palliat Med. 2003;6:715–724. doi: 10.1089/109662103322515220. [DOI] [PubMed] [Google Scholar]
- 12.Brumley R, Enguidanos S, Jamison P, Seitz R, Morgenstern N, Saito S, McIlwane J, Hillary K, Gonzalez J. Increased satisfaction with care and lower costs: Results of a randomized trial of in-home palliative care. J Am Geriatr Soc. 2007;55:993–1000. doi: 10.1111/j.1532-5415.2007.01234.x. [DOI] [PubMed] [Google Scholar]
- 13.Burge F, Lawson B, Johnston G. Family physician continuity of care and emergency department use in end-of-life cancer care. Med Care. 2003;41:992–1001. doi: 10.1097/00005650-200308000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Serra-Prat M, Gallo P, Picaza JM. Home palliative care as a cost-saving alternative: Evidence from Catalonia. Palliat Med. 2001;15:271–278. doi: 10.1191/026921601678320250. [DOI] [PubMed] [Google Scholar]
- 15.Critchley P, Lohfeld L, Maxwell D, McIntyre P, Reyno L. The challenge of developing a regional palliative care data system: A tale of two cities. J Palliat Care. 2002;18:7–14. [PubMed] [Google Scholar]
- 16.Burge F, Johnston G, Lawson B, Dewar R, Cummings I. Population based trends in referral of the elderly to a comprehensive palliative care program. Palliat Med. 2002;16:255–256. doi: 10.1191/0269216302pm550xx. [DOI] [PubMed] [Google Scholar]
- 17.McIntyre P, Pringle S, Brouse J, Archibald G, Linden B, MacDonald R, Mitchell L, Newton K, Page G, Parker S, Stockman C. Capital Health Integrated Palliative Care Service (CHIPCS) Resource Manual. Halifax, Nova Scotia: CHIPCS Care & Access Planning Team; 2004. [Google Scholar]
- 18.Finkelstein MM. Ecologic proxies for household income: How well do they work for the analysis of health and health care utilization? Can J Pub Health. 2004;95:90–94. doi: 10.1007/BF03405773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Demissie K, Hanley JA, Menzies D, Joseph L, Ernst P. Agreement in measuring socio-economic status: Area-based versus individual measures. Chronic Dis Can. 2000;21:1–7. [PubMed] [Google Scholar]
- 20.Mustard CA, Derksen S, Berthelot J-M, Wolfson M. Assessing ecologic proxies for household income: A comparison of household and neighbourhood level income measures in the study of population health status. Health Place. 1999;5:157–171. doi: 10.1016/s1353-8292(99)00008-8. [DOI] [PubMed] [Google Scholar]
- 21.Burge FI, Lawson B, Critchley P, Maxwell D. Transitions in care during the end of life: Changes experienced following enrolment in a comprehensive palliative care program. BMC Palliative Care. 2005;4:3. doi: 10.1186/1472-684X-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnston GM, Gibbons L, Burge FI, Dewar RA, Cummings I, Levy IG. Identifying potential need for cancer palliation in Nova Scotia. Can Med Assoc J. 1998;158:1691–1698. [PMC free article] [PubMed] [Google Scholar]
- 23.SAS/STAT Version 9.1 [computer program] Cary (NC): SAS Institute Inc; 2003. [Google Scholar]
- 24.Johnston G, Burge F. Analytic framework for primary clinicians providing end-of-life care. J Palliat Care. 2002;18:141–149. [PubMed] [Google Scholar]
- 25.Lawson B, Burge FI, McIntyre P, Field S, Maxwell D. Palliative care patients in the emergency department. J Palliat Care. 2008;24:247–255. [PMC free article] [PubMed] [Google Scholar]