Abstract
Background:
The impact of moving to a neighborhood more conducive to utilitarian walking on the risk of incident hypertension is uncertain.
Objective:
Our study aimed to examine the effect of moving to a highly walkable neighborhood on the risk of incident hypertension.
Methods:
A population-based propensity-score matched cohort study design was used based on the Ontario population from the Canadian Community Health Survey (2001–2010). Participants were adults ≥ 20 years of age who moved from a low-walkability neighborhood (defined as any neighborhood with a Walk Score < 90) to either a high- (Walk Score ≥ 90) or another low-walkability neighborhood. The incidence of hypertension was assessed by linking the cohort to administrative health databases using a validated algorithm. Propensity-score matched Cox proportional hazard models were used. Annual health examination was used as a control event.
Results:
Among the 1,057 propensity-score matched pairs there was a significantly lower risk of incident hypertension in the low to high vs. the low to low-walkability groups [hazard ratio = 0.46; 95% CI, 0.26, 0.81, p < 0.01]. The crude hypertension incidence rates were 18.0 per 1,000 person-years (95% CI: 11.6, 24.8) among the low- to low-walkability movers compared with 8.6 per 1,000 person-years (95% CI: 5.3, 12.7) among the low- to high-walkability movers (p < 0.001). There were no significant differences in the hazard of annual health examination between the two mover groups.
Conclusions:
Moving to a highly walkable neighborhood was associated with a significantly lower risk of incident hypertension. Future research should assess whether specific attributes of walkable neighborhoods (e.g., amenities, density, land-use mix) may be driving this relationship.
Citation:
Chiu M, Rezai MR, Maclagan LC, Austin PC, Shah BR, Redelmeier DA, Tu JV. 2016. Moving to a highly walkable neighborhood and incidence of hypertension: a propensity-score matched cohort study. Environ Health Perspect 124:754–760; http://dx.doi.org/10.1289/ehp.1510425
Introduction
There is growing interest in the impact of the built environment on the promotion of physical activity (McCormack and Shiell 2011; Witten et al. 2012) and the prevention of cardiovascular diseases (Ludwig et al. 2011; Sallis et al. 2012; Kumanyika et al. 2008). In particular, living in walkable neighborhoods (i.e., neighborhoods with shorter, more connected streets and with greater access to a variety of shops and other amenities within walking distance) has been associated with increased walking and decreased prevalence of obesity and other cardiovascular risk factors, including hypertension (Berry et al. 2010; Booth et al. 2013; Giles-Corti et al. 2008; Hirsch et al. 2013, 2014a, 2014b, 2014c; Mujahid et al. 2008; Müller-Riemenschneider et al. 2013). A recent analysis by our group using a similar representative sample of the Ontario population from Statistics Canada’s Canadian Community Health Survey found that living in higher Walk Score areas was significantly associated with more utilitarian walking and a decreased prevalence of obesity (Chiu et al. 2015). A major limitation of past work on neighborhood walkability and health outcomes, such as hypertension, has been the reliance on cross-sectional data (Casagrande et al. 2011; Müller-Riemenschneider et al. 2013). The use of these data raises methodological concerns regarding the potential for reverse causation—the outcome potentially preceding or causing the exposure instead of the other way around. Moreover, earlier studies have not been able to adequately adjust for important individual characteristics [e.g., income, education, marital status, body mass index (BMI)] that differ between people who live in low- and those in high-walkability neighborhoods and might influence their risk of hypertension independent of physical activity.
We conducted a population-based cohort study using propensity-score matching methods to examine the risk of incident hypertension among individuals who moved from a low- to a high-walkability neighborhood compared with individuals who moved from a low- to another low-walkability neighborhood.
Methods
Walk Score
Several walkability indices have been created for individual study settings (Booth et al. 2013; Frank et al. 2010; Toronto Public Health 2012); however, Walk Score’s Street Smart Walk Score (henceforth called Walk Score) is currently the only walkability index that is publicly available for all postal codes and ZIP codes in Canada, the United States, and Australia (http://www.walkscore.com). The Walk Score has been shown to be a valid measure for estimating neighborhood walkability in multiple geographic locations and at multiple spatial scales in the United States as measured based on significant moderate Spearman correlations with geographic information system–derived walkability indicators (Duncan et al. 2011). The Walk Score is based on walking distances from a given location to a diverse set of nearby amenities, including grocery stores, restaurants, shopping, coffee shops, banks, parks, schools, book stores and libraries, and entertainment. The points for each type of amenity are added and then normalized to yield a score from 0 to 100 with penalties of up to 5% applied for areas with lower street connectivity (Walk Score 2014).
Data Sources and Study Cohort
The study was conducted at the Institute for Clinical Evaluative Sciences (ICES), a repository of linked administrative health databases, including individual-level data for hospital discharges and Ontario Health Insurance Plan (OHIP) physician and laboratory claims and the Canadian Institute for Health Information (CIHI) Discharge Abstract Database for hospital admissions for people in Ontario, Canada (unpublished data).
The study population consisted of Ontario participants of Statistics Canada’s Canadian Community Health Surveys (CCHS) (2001–2010) (Thomas and Wannell 2009). These surveys used a complex sampling strategy to collect sociodemographic and health information from a representative sample of Canadians ≥ 12 years of age living in private dwellings (including apartments). The surveys excluded institutionalized individuals, individuals living on Aboriginal reserves, full-time members of the Canadian forces, and residents of certain remote regions. The individual response rates in the different CCHS surveys ranged from 75.1% to 94.4%. More details about these surveys are found elsewhere (Desmeules 2004).
The outcome—incident hypertension—was derived through linkage of the survey data to the population-based Ontario Hypertension Database, which uses a validated algorithm of one CIHI hospital admission with a hypertension diagnosis or one OHIP claim with a hypertension diagnosis followed within 2 years by another OHIP claim or one CIHI hospital admission (specificity, 95%; sensitivity, 72% validated using primary care charts) (Tu et al. 2007, 2008).
Figure 1 illustrates the creation of the study cohort. The cohort was restricted to CCHS respondents ≥ 20 years of age at their survey date who had a valid Ontario health card number and who did not have previous hypertension (as ascertained by self-report or through linkage to the Ontario Hypertension Database). For each study participant, we ascertained longitudinal annual postal codes of residence starting from the year of interview by linking our CCHS study population data set to the Registered Person’s Database (RPDB) from the Ontario Ministry of Health and Long-term Care (MOHLTC) (Health Analytics Branch 2012). The RPDB includes postal codes for all Ontario residents and is updated on 1 July of each year via linkage to other administrative databases at the Institute for Clinical Evaluative Sciences. The annual postal codes were then linked to a file purchased from Walk Score® (which contained Walk Scores as of 2012) to assign a Walk Score for each annual postal code, the smallest unit for which geographical information was available from the CCHS survey. Postal codes are defined by Canada Post Corporation for the efficient sorting and delivery of mail and represent small geographical units which may be made up of a specific city block in urban areas (one side of a street between two intersecting streets) or a rural community in rural areas. The cohort was limited to individuals who at the time of the survey were living in a low-walkability neighborhood and who subsequently moved neighborhoods following the interview date. Individuals were classified as either moving from a low- (defined as Walk Score < 90) to a high-walkability (defined as Walk Score ≥ 90) postal code (i.e., low to high group) or from a low- to a different low-walkability postal code (i.e., low to low group). Included in our definition of low-walkability postal codes are those defined by Walk Score as “Car-Dependent” (0-49), “Somewhat Walkable” (50–69) and “Very Walkable” postal codes (70–89). Our high-walkability postal code corresponds to “Walker’s Paradise” areas as defined by Walk Score (http://www.walkscore.com). The date of first move was defined as the index date. Individuals were followed using administrative health databases from index date to the date of incident hypertension and were censored at date of death (from the RPDB), date of move outside of Ontario, end of study date (1 July 2012), or date when an individual in the low to low group had a subsequent move to a high-walkability (Walk Score ≥ 90) postal code or when an individual in the low to high group had a subsequent move back to a low-walkability (Walk Score < 90) postal code.
Figure 1.
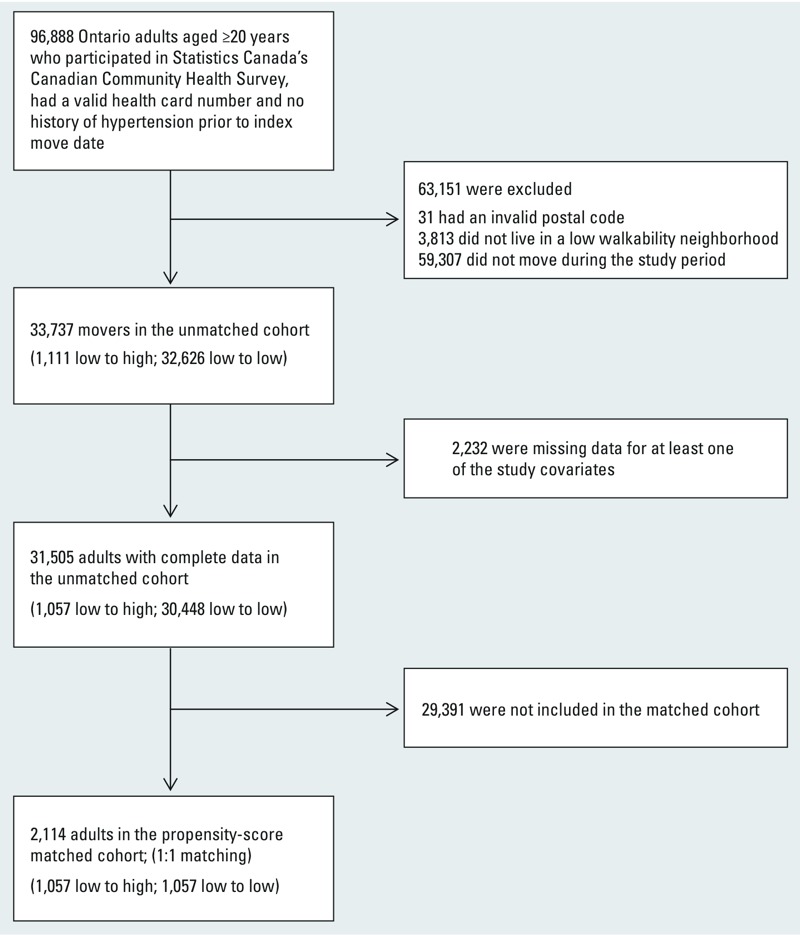
Study flow diagram. Low- and high-walkability areas were defined as Walk Score of < 90 and ≥ 90, respectively.
Study Covariates
The following covariates based on self-reported data collected at the time of survey were used to calculate propensity scores: age (used to calculate age at index date); sex; education (< secondary school vs. ≥ secondary school); marital status (married/common law vs. single/widowed/divorced); immigrant status (immigrant vs. non-immigrant); race/ethnicity (i.e., white, Chinese, South Asian, black, other); current smoking; diabetes (physician diagnosed); BMI (from self-reported weight and height); psychosocial stress (i.e., feeling extremely/quite a bit vs. not at all/not very/a bit stressed in most days); inadequate leisure physical activity (i.e., participating in at most 15 min of daily physical activity); alcohol consumption [i.e., regular drinker (≥ once per month), occasional drinker (> once per year but < once per month), or never in the past 12 months)]; and inadequate fruit and vegetable consumption (i.e., eating fruits or vegetables less than three times per day). We also included index year, as well as Statistics Canada’s 2006 census-derived area-based income quintiles (household-size adjusted income averaged at the dissemination area level, which generally includes a population of 400–700 individuals) and urban (≥ 10,000 population) or rural (< 10,000 population) dwelling at index date in the propensity-score models. The covariates were chosen based on a priori hypotheses and walkability literature, as well as all available factors associated with walkability and/or hypertension based on previous studies. A separate multivariable Cox proportional-hazards model using the unmatched sample was also constructed including all of the covariates mentioned above.
Control Event
We assessed annual health examination as the control event. Control or tracer events have been used in previous studies to detect possible biases by testing for the lack of association between the exposure and the control event when there is expected to be no association. (Hackam et al. 2006). Annual health examination, a general health assessment for patients with no apparent physical or mental illness, was chosen as the control event to examine possible differences in health care seeking behavior using an event unlikely to be related to hypertension or physical activity. We used the same propensity score–matched cohort as the main analysis and linked to the OHIP database to ascertain time to the first annual health examination during the follow up period.
Statistical Analyses
SAS v. 9.3 (SAS Institute Inc.) and R v. 3.1.2 (R Core Team 2014) were used for statistical analysis. All tests were two-sided and p < 0.05 was considered statistically significant. Study data sets were linked using unique encoded identifiers and analyzed at the ICES. All estimates were weighted using Statistics Canada’s original survey weights to generate results that are representative of the overall Ontario population.
Propensity Score–Matched Analysis
A propensity score for the probability of moving from a low- to a high-walkability postal code was estimated for each individual using a weighted logistic regression model including the 16 study covariates previously stated. We created a propensity score–matched cohort by attempting to match each participant in the low to high group to an individual in the low to low group. A nearest-neighbor-1:1-greedy matching algorithm was applied to match participants on the basis of the logit of their propensity score, with a caliper width equal to 0.2 times the standard deviation of the logit of the propensity score (Austin 2011; Austin and Small 2014). Balance of baseline covariates between the exposed and control groups in the matched sample was assessed using standardized differences, with standardized differences of < 0.1 for each covariate being used to indicate good balance (Austin 2009). We also assessed whether the groups were balanced on other health status and individual income variables that were not used to derive propensity scores, including self-reported health, mental health, and continuous individual-level income.
The effect of moving to a high-walkability neighborhood (compared with moving to a low-walkability neighborhood) was estimated using a Cox proportional hazards model that regressed the hazard of incident hypertension on the exposure group. To account for the paired nature of the matched sample, robust sandwich-type variance estimators were used to assess the statistical significance of the estimated hazard ratio (Austin 2013). Survival curves were produced using Kaplan–Meier methods. All analyses were weighted by the survey sample weights and appropriate propensity-score matching and bootstrap methods for complex survey design were applied (Austin and Small 2014; Zanutto 2006).
Unmatched Sample and Sensitivity Analyses
To assess whether results were consistent using the entire sample of survey respondents, we also calculated adjusted Cox proportional hazard ratios and bootstrapped p-values for the incidence of hypertension among the larger unmatched sample (low to low n = 32,626; low to high n = 1,111). This was important in order to verify that results were consistent using traditional multivariable regression methods. Adjusted survival curves were produced using the corrected group prognosis method (Makuch 1982; SAS Institute Inc. 2014). For sensitivity analyses, we calculated Cox proportional hazard ratios for a) a sample limited to only those who lived in non-rural postal codes at the time of the survey and censoring occurring upon moving to a rural postal code (n = 26,048), and b) a sample where a cut point of Walk Score 70 was used instead of 90 (n = 26,563) to dichotomize high- and low-walkability neighborhoods.
Ethics Committee Approval
Our study was approved by the Research Ethics Board at Sunnybrook Health Sciences Centre. Informed consent for the use of data for research purposes was obtained from all survey participants by Statistics Canada.
Results
Study Population
The unmatched sample included a total of 33,737 adults (before excluding participants with missing covariate data): 1,111 in the low to high group and 32,626 in the low to low group. The baseline characteristics of the unmatched sample are displayed in Table S1. In the unmatched sample, the movers in the low- to low-walkability group were on average older (39.9 years vs. 37.0 years) and less likely male (48.3% vs. 51.7%) than those in the low- to high-walkability group. Levels of less than secondary school education (11.3% vs. 5.5%), the prevalence of overweight/obesity (43.6% vs. 33.0%) and diabetes (1.9% vs. 0.6%), as well as leisure physical activity (inactive 51.1% vs. 46.5%) and alcohol consumption (regular drinker; 64.2% vs. 72.9%) were similar between the low- to low- and the low- to high-walkability groups, respectively.
Propensity-Score Matched Analysis
After propensity-score matching, a total of 1,057 (95%) low to high movers were matched to 1,057 low to low movers. The matched sample was balanced, with standardized differences ≤ 0.01 for all comparisons (Table 1). The matched cohort was followed for up to 10 years, with a mean length of follow-up of 4.3 years (median, 4.0; range, 0.03–11.0) in the low to low group compared with 3.0 years (median, 2.0; range, 0.03–11.0) in the low to high group. Mean individual-level income was well balanced between the two study groups ($34,311 in the low to low group vs. $37,030 in the low to high group). The proportion of individuals in middle and high income area–based income quintiles was also well balanced (49.1% in the low to low group vs. 49.2% in the low to high group) (Table 1). The mean Walk Score before move in the low to low movers was 39.7 (median, 41; range, 0–89) compared to 50.2 (median, 55; range, 0–89) in the low to high movers. The mean post-move Walk score in the low to low movers was 40.0 (median, 41.0; range, 0–89) compared with 94.4 (median, 94; range, 90–100) in the low to high movers.
Table 1.
Baseline characteristics of the propensity-score matched cohort.
| Sociodemographic characteristics | Low to low walkability (n = 1,057) | Low to high walkability (n = 1,057) | Standardized difference |
|---|---|---|---|
| Age at index date (years) [mean (median)] | 36.8 (33) | 37.0 (34) | < 0.01 |
| Age at index date (grouped) (years) | |||
| 20–34 | 55.6 | 54.0 | < 0.01 |
| 35–45 | 19.0 | 22.2 | < 0.01 |
| ≥ 46 | 25.4 | 23.9 | < 0.01 |
| No. of years between interview and index dates [mean (median)] | 2.9 (2) | 3.2 (2) | 0.01 |
| Male sex (%) | 49.3 | 52.7 | < 0.01 |
| Area-based income quintile at index date | |||
| 1 (lowest) | 27.3 | 26.4 | < 0.01 |
| 2 | 23.6 | 24.4 | < 0.01 |
| 3 | 15.2 | 14.3 | < 0.01 |
| 4 | 13.7 | 13.6 | < 0.01 |
| 5 (highest) | 20.2 | 21.3 | < 0.01 |
| Individual-level income ($) [mean (median)] | 34,311 (28,000) | 37,030 (30,000) | < 0.01 |
| Less than secondary school education | 4.0 | 5.0 | < 0.01 |
| Married or common-law | 29.5 | 32.4 | < 0.01 |
| Urban dwelling at index date | 92.3 | 93.8 | < 0.01 |
| Immigrant | 33.3 | 34.5 | < 0.01 |
| No. of years in Canada (among immigrants) [mean (median)] | 16.1 (12) | 15.8 (13) | < 0.01 |
| Race/ethnicity | |||
| White | 70.0 | 71.5 | < 0.01 |
| South Asian | 1.6 | 2.9 | < 0.01 |
| Chinese | 4.7 | 3.8 | < 0.01 |
| Black | 7.7 | 5.6 | < 0.01 |
| Other | 16.1 | 16.2 | < 0.01 |
| Current smoker | 26.6 | 28.6 | < 0.01 |
| Prevalent diabetes | 0.3 | 0.7 | < 0.01 |
| BMI (kg/m2) [mean (median)] | 24.0 (23) | 24.0 (24) | < 0.01 |
| Overweight (BMI ≥ 25 kg/m2) | 34.7 | 33.1 | < 0.01 |
| Obese (BMI ≥ 30 kg/m2) | 7.7 | 7.1 | < 0.01 |
| Psychosocial stress | 29.7 | 30.2 | < 0.01 |
| Leisure physical activity | |||
| Active | 34.1 | 29.4 | 0.01 |
| Moderate | 21.1 | 24.7 | < 0.01 |
| Inactive | 44.8 | 45.9 | < 0.01 |
| Leisure physical activity (≤ 15 min/day)a | 60.4 | 62.0 | < 0.01 |
| Alcohol consumptionb | |||
| Regular drinker | 72.5 | 74.3 | < 0.01 |
| Occasional drinker | 13.1 | 11.8 | < 0.01 |
| Nondrinker | 14.4 | 13.9 | < 0.01 |
| Inadequate fruits and vegetables (< 3 times per day) | 22.6 | 25.0 | < 0.01 |
| No. of times consumed fruits and vegetables per day [mean (median)] | 4.9 (4) | 5.0 (5) | < 0.01 |
| Poor/fair self-rated overall health | 6.4 | 6.9 | < 0.01 |
| Poor/fair self-rated mental health | 4.3 | 4.5 | < 0.01 |
| Low- and high-walkability areas were defined as Walk Score of < 90 and ≥ 90, respectively. Data were derived from the Ontario components of Canadian Community Health Survey (2001–2010) linked to the Ontario Hypertension Database. Estimates are percentages or mean (median). All estimates were weighted by the survey sample weight. In all comparisons of characteristics, the groups were well balanced (standardized differences in the mean ≤ 0.01 for all comparisons). aLeisure physical activity [average daily energy expenditure (active: ≥ 3.0 kcal/kg/day; moderately active: 1.5–2.9 kcal/kg/day; inactive: < 1.5 kcal/kg/day)] bAlcohol consumption (regular drinker: at least once per month; occasional drinker: less than once per month; nondrinker: never in the past year from survey date). | |||
There was a significantly lower risk of incident hypertension in the low to high versus low to low groups [hazard ratio (HR) = 0.46; 95% confidence interval (CI): 0.26, 0.81, p < 0.01]. The crude hypertension incidence rates were 18.0 per 1,000 person-years (95% CI: 11.6, 24.8) in the low to low movers compared with 8.6 per 1,000 person-years (95% CI: 5.3, 12.7) in the low to high movers (p < 0.001). Figure 2 displays the event-free Kaplan–Meier curves for the two study groups.
Figure 2.
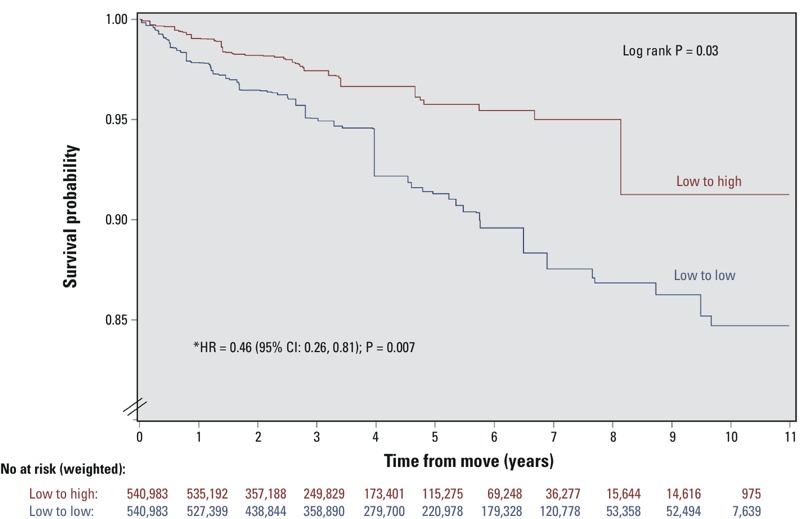
Event-free survival for incident hypertension in a propensity score–matched cohort of participants who moved from low- to high-walkability areas vs. from low- to low-walkability areas. Low- and high-walkability areas were defined as Walk Score of < 90 and ≥ 90, respectively. The p-value tests the difference between the Kaplan–Meier survival curves using the log-rank test. All estimates were weighted by the survey sample weights and bootstrap methods were applied. The hazard ratios, 95% confidence intervals, and p-values were derived from a Cox proportional hazards model performed on the propensity score–matched study sample of 1,057 pairs of participants balanced on age, sex, income, education, marital status, urban/rural residence, immigrant status, race/ethnicity, smoking, diabetes, BMI, stress, leisure physical activity, alcohol consumption, fruit and vegetable consumption, and index year.
Control Event
There was no significant difference in the hazard of annual health examination (HR = 1.01; 95% CI: 0.85, 1.22, p = 0.88) between the two study groups. Figure 3 displays the Kaplan–Meier curves for this relationship.
Figure 3.
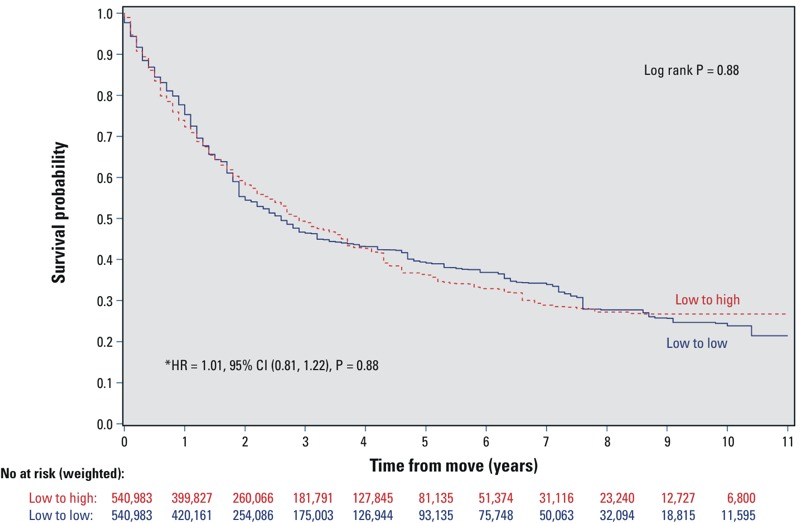
Kaplan–Meier survival curves for annual health examination in a propensity score–matched cohort of movers from low- to high-walkability areas vs. from low- to low-walkability areas. Low- and high-walkability areas were defined as Walk Score of < 90 and ≥ 90, respectively. Kaplan–Meier survival curves were weighted using survey weights. The p-values test the differences between the Kaplan–Meier survival curves using the log-rank test. The hazard ratios, 95% confidence intervals, and p-values were derived from Cox proportional hazards models performed on the propensity score–matched study sample, which was balanced on age, sex, income, education, marital status, urban residence, immigrant status, race/ethnicity, smoking, diabetes, BMI, stress, leisure physical activity, alcohol consumption, fruit and vegetable consumption, and index year.
Unmatched Sample and Sensitivity Analyses
Similar results to the main analysis were obtained when hazard ratios were calculated for the unmatched sample adjusted for the same 16 covariates included in the propensity score matched analysis (HR = 0.57; 95% CI: 0.35, 0.85, p = 0.01) (see Table S2 and Figure S1), and for the sample that excluded rural dwellers (HR = 0.58; 95% CI: 0.36, 0.86, p = 0.02).
When the threshold for what constituted a “high” walkability area was lowered from Walk Score 90 to 70, as expected, we found an attenuated but still negative association of moving to a highly walkable neighborhood on hypertension incidence among the unmatched sample adjusted for the same 16 covariates (HR = 0.81; 95% CI: 0.66, 1.02, p = 0.06).
Discussion
In this large population-based sample, we found that moving to an area with a very high Walk Score (indicating a neighborhood that is very conducive to utilitarian walking) was associated with a significantly lower risk of hypertension. People who moved from low- to high-walkability areas had a 54% lower risk of incident hypertension than their counterparts in the propensity score–matched low- to low-walkability group. There was no significant difference in the hazards of the control event—annual health examination—between the two study groups.
Our findings are consistent with earlier evidence that increased neighborhood walkability is associated with increased walking (Owen et al. 2010; Sundquist et al. 2011) and lower prevalence of obesity and hypertension (Berry et al. 2010; Mujahid et al. 2008; Müller-Riemenschneider et al. 2013). A recent study of adults in Australia followed participants moving to a new residential development over a 7-year period and found that neighborhood walkability, access to public transit stops, and having a variety of local destinations were predictors of whether participants walked for transportation in their neighborhood (Knuiman et al. 2014). A systematic review of experimental and observational studies examining the association between built environments and physical activity found that neighborhood amenities, street connectivity, and population density (similar attributes used to derive the Walk Score) were important determinants of physical activity, particularly transportation or utilitarian walking (McCormack and Shiell 2011). Moreover, other survey-based studies have reported that movers walked and biked more 1 year post-move if the neighborhood to which they moved included an increase in the mix of businesses within walking distance of their residence (Cao et al. 2007; Handy et al. 2006). Because of the impracticability and cost of a randomized control trial to answer our research question, we performed a propensity score–matched analysis of prospective data using a natural history experiment of people’s moving patterns. Our study findings are analogous and consistent in magnitude and direction to two randomized studies that have suggested that neighborhood environments can directly influence health and reduce risk of hypertension (He et al. 2000; Ludwig et al. 2011). One such study, phase one of the Trials of Hypertension Prevention, found a 77% reduction in the odds of hypertension among those receiving the lifestyle intervention, which included brisk walking (He et al. 2000). Similarly, the Moving to Opportunity project found that the opportunity to move from a neighborhood with a high level of poverty to one with a lower level of poverty was associated with a reduction in the prevalence of extreme obesity and diabetes, thus suggesting that neighborhood characteristics have the potential to improve cardiovascular health (Ludwig et al. 2011).
We recognize that there may be several other neighborhood characteristics associated with highly walkable areas that may have contributed to our findings. For example, walkable neighborhoods often have easier access to transit, and it has been shown that people who take transit generally are more likely to meet daily physical activity recommendations (Lachapelle and Frank 2009) and have a lower BMI (Flint et al. 2014; Duncan et al. 2014). We also acknowledge that there are some negative consequences to living in highly walkable areas; for example, these areas may have substantial variation in other characteristics of highly walkable areas, such as higher levels of noise and air pollution, which have been shown to negatively impact health (Frank and Engelke 2005; Moudon 2009). However, some studies have found that higher walkability areas are associated with lower levels of air pollution (Frank et al. 2006). Future studies should also consider other characteristics that may be associated with walkability and both physical and mental health, including the food environment (Rundle et al. 2009) and pollutants (Marshall et al. 2009).
This study has several strengths. First, to our knowledge, our study represents the first cohort study to investigate the association between neighborhood walkability and risk of incident hypertension in a population-based sample, thus ensuring temporality between exposure and outcome. Second, we were able to adjust for 16 important study covariates, including many of the known risk factors for hypertension. Third, to optimize the comparability of the two study groups, we designed our study population to include only those who moved during the study period. All study participants also had to have lived in a low-walkability area at baseline, thus making the two study groups more similar than if a comparison was done for movers from low- to high- versus high- to low-walkability areas. Our estimates were weighted using survey weights, which allowed estimates to be generalizable to the overall Ontario population.
This study has limitations worth noting. First, we did not have serially measured blood pressure data. We also did not have detailed dietary data (e.g., salt intake) as well as more detailed measures of physical activity. Second, people moving to high-walkability neighborhoods may be healthier and/or demonstrate more health-seeking behavior. In this study, however, the propensity score–matching method ensured that the two mover groups were balanced on several lifestyle and health status covariates. In addition, we found no differences between the two study groups for annual health examination, thus suggesting that the groups likely did not differ in their health-seeking behavior. Third, we acknowledge that based on our dichotomization of Walk Score and classification of high-walkability areas (Walk Score ≥ 90), there may have been individuals living in walkable neighborhoods that were classified as low walkability. There also may have been variations in the change in Walk Score of individuals following their move both within and between groups. Fourth, we did not have information about other built environment attributes, such as street aesthetics and safety, which may influence physical activity and in turn may influence the risk of hypertension. Fifth, there were differences in the median years of follow-up between the low to low and low to high movers groups that should be acknowledged. Finally, a key assumption of propensity score modeling is that most observed confounding is accounted for; however, there remains the possibility that there may be residual confounding among unobserved covariates, such as other geographic factors or changes in sociodemographic characteristics, that could contribute to the results of the study. Future studies could focus on the effects of subcomponents of the Walk Score (e.g., amenities, density, land-use mix) and whether the relationship between moving to areas of higher walkability and a decreased risk of hypertension might differ across age, sex, and socioeconomic groups.
Conclusions
In this large cohort study, moving to a highly walkable neighborhood was associated with a significantly lower risk of incident hypertension, a leading global burden of disease risk factor (Lim et al. 2012). Despite continued public health efforts to encourage people to participate in physical activity, only a small proportion of adults meet the minimum recommended physical activity levels to achieve health benefits (Colley et al. 2011). Thus, it becomes pertinent to emphasize that features of the built environment have the potential to encourage active living and improve population health, sentiments that are echoed by the American Heart Association (Bambs et al. 2011; Pearson et al. 2013), the World Health Organization’s European Healthy Cities Network (Edwards and Tsouros 2008), and the U.S. Surgeon General (2010). Our findings suggest that neighborhood walkability can positively affect health and may help raise awareness among the public of the importance of neighborhood environments.
Supplemental Material
Acknowledgments
We acknowledge that the data used in this publication are from Statistics Canada’s Canadian Community Health Survey. We thank all the survey participants and the staff from Statistics Canada who assisted in the data collection and management.
Footnotes
This work was supported by a fellowship to M.C. from the Canadian Institutes of Health Research (CIHR); Career Investigator Award from the Heart and Stroke Foundation of Ontario to P.C.A.; CIHR New Investigator Award to B.R.S.; Canada Research Chair in Medical Decision Science and a CIHR grant from the CIHR to D.A.R.; Canada Research Chair in Health Services Research from the CIHR and a Career Investigator Award from the Heart and Stroke Foundation of Ontario to J.V.T.; Institute for Circulatory Health-Canadian Institutes of Health Research Chronic Diseases Team grant (no. TCA 118349) to the Cardiovascular Health in Ambulatory Care Research Team (http://www.canheart.ca); and the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). Parts of this material are based on data and information compiled and provided by Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed herein are those of the author, and not necessarily those of CIHI. This study was conducted using funding entirely from public sources.
The study results and conclusions are those of the authors, and should not be attributed to any of the funding or sponsoring agencies. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. All decisions regarding study design, publication, and data analysis were made independent of the funding agencies.
The authors declare they have no actual or potential competing financial interests.
References
- Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10:150–161. doi: 10.1002/pst.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin PC. The performance of different propensity score methods for estimating marginal hazard ratios. Stat Med. 2013;32:2837–2849. doi: 10.1002/sim.5705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin PC, Small DS. The use of bootstrapping when using propensity-score matching without replacement: a simulation study. Stat Med. 2014;33:4306–4319. doi: 10.1002/sim.6276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bambs CE, Kip KE, Dinga A, Mulukulta SR, Aiyer AN, Reis SE. Low prevalence of “ideal cardiovascular health” in a community-based population: the Heart Strategies Concentrating on Risk Evaluation (Heart SCORE) study. Circulation. 2011;123:850–857. doi: 10.1161/CIRCULATIONAHA.110.980151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry TR, Spence JC, Blanchard CM, Cutumisu N, Edwards J, Selfridge G. 2010. A longitudinal and cross-sectional examination of the relationship between reasons for choosing a neighbourhood, physical activity and body mass index. Int J Behav Nutr Phys Act 7 57, doi: 10.1186/1479-5868-7-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth GL, Creatore MI, Moineddin R, Gozdyra P, Weyman JT, Matheson FI, et al. Unwalkable neighborhoods, poverty, and the risk of diabetes among recent immigrants to Canada compared with long-term residents. Diabetes Care. 2013;36:302–308. doi: 10.2337/dc12-0777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao X, Mokhtarian PL, Handy SL. Do changes in neighborhood characteristics lead to changes in travel behavior? A structural equations modeling approach. Transportation. 2007;34:535–556. [Google Scholar]
- Casagrande SS, Gittelsohn J, Zonderman AB, Evans MK, Gary-Webb TL. Association of walkability with obesity in Baltimore City, Maryland. Am J Public Health. 2011;101(suppl 1):S318–S324. doi: 10.2105/AJPH.2009.187492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu M, Shah BR, Maclagan LC, Rezai MR, Austin PC, Tu JV. Walk Score® and the prevalence of utilitarian walking and obesity among Ontario adults: a cross-sectional study. Health Rep. 2015;26:3–10. [PubMed] [Google Scholar]
- Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS. Physical Activity of Canadian Adults: Accelerometer Results from the 2007 to 2009 Canadian Health Measures Survey. Ottawa, Ontario, Canada:Statistics Canada. 2011 Available: http://www.statcan.gc.ca/pub/82-003-x/2011001/article/11396-eng.htm (accessed 15 September 2015) [PubMed]
- Desmeules M. 2004. Appendix A overview of National Population Health and Canadian Community Health Surveys. BMC Women’s Health 4(suppl 1) S35, doi: 10.1186/1472-6874-4-S1-S35 [DOI] [Google Scholar]
- Duncan DT, Aldstadt J, Whalen J, Melly SJ, Gortmaker SL. Validation of Walk Score® for estimating neighborhood walkability: an analysis of four US metropolitan areas. Int J Environ Res Public Health. 2011;8:4160–4179. doi: 10.3390/ijerph8114160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Sharifi M, Melly SJ, Marshall R, Sequist TD, Rifas-Shiman SL, et al. 2014. Characteristics of walkable built environments and BMI z-scores in children: evidence from a large electronic health record database. Environ Health Perspect 122 1359 1365, doi: 10.1289/ehp.1307704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards P, Tsouros AD. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 2008. A Healthy City is an Active City: A Physical Activity Planning Guide. Available: http://www.euro.who.int/__data/assets/pdf_file/0012/99975/E91883.pdf [accessed 15 September 2015] [Google Scholar]
- Flint E, Cummins S, Sacker A. 2014. Associations between active commuting, body fat, and body mass index: population based, cross sectional study in the United Kingdom. BMJ 349 g4887, doi: 10.1136/bmj.g4887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank LD, Engelke P. Multiple impacts of the built environment on public health: walkable places and the exposure to air pollution. Int Reg Sci Rev. 2005;28:193–216. [Google Scholar]
- Frank LD, Sallis JF, Conway TL, Chapman JE, Saelens BE, Bachman W. Many pathways from land use to health: associations between neighborhood walkability and active transportation, body mass index, and air quality. J Am Plann Assoc. 2006;72:75–87. [Google Scholar]
- Frank LD, Sallis JF, Saelens BE, Leary L, Cain K, Conway TL, et al. The development of a walkability index: application to the Neighborhood Quality of Life Study. Br J Sports Med. 2010;44:924–933. doi: 10.1136/bjsm.2009.058701. [DOI] [PubMed] [Google Scholar]
- Giles-Corti B, Knuiman M, Timperio A, Van Niel K, Pikora TJ, Bull FC, et al. Evaluation of the implementation of a state government community design policy aimed at increasing local walking: design issues and baseline results from RESIDE, Perth Western Australia. Prev Med. 2008;46:46–54. doi: 10.1016/j.ypmed.2007.08.002. [DOI] [PubMed] [Google Scholar]
- Hackam DG, Mamdani M, Li P, Redelmeier DA. Statins and sepsis in patients with cardiovascular disease: a population-based cohort analysis. Lancet. 2006;367:413–418. doi: 10.1016/S0140-6736(06)68041-0. [DOI] [PubMed] [Google Scholar]
- Handy S, Cao X, Mokhtarian PL. Self-selection in the relationship between the built environment and walking: empirical evidence from Northern California. J Am Plann Assoc. 2006;72:55–74. [Google Scholar]
- He J, Whelton PK, Appel LJ, Charleston J, Klag MJ. Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension. 2000;35:544–549. doi: 10.1161/01.hyp.35.2.544. [DOI] [PubMed] [Google Scholar]
- Health Analytics Branch. 2012. Health Analyst’s Toolkit. Toronto, Ontario, Canada:Ministry of Health and Long-term Care. Available: http://www.health.gov.on.ca/english/providers/pub/healthanalytics/health_toolkit/health_toolkit.pdf [accessed 16 October 2015] [Google Scholar]
- Hirsch JA, Diez Roux AV, Moore KA, Evenson KR, Rodriguez DA. Change in walking and body mass index following residential relocation: the Multi-Ethnic Study of Atherosclerosis. Am J Public Health. 2014a;104:e49–e56. doi: 10.2105/AJPH.2013.301773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch JA, Moore KA, Barrientos-Gutierrez T, Brines SJ, Zagorski MA, Rodriguez DA, et al. Built environment change and change in BMI and waist circumference: Multi-Ethnic Study of Atherosclerosis. Obesity (Silver Spring) 2014b;22:2450–2457. doi: 10.1002/oby.20873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch JA, Moore KA, Clarke PJ, Rodriguez DA, Evenson KR, Brines SJ, et al. Changes in the built environment and changes in the amount of walking over time: longitudinal results from the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2014c;180:799–809. doi: 10.1093/aje/kwu218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch JA, Moore KA, Evenson KR, Rodriguez DA, Diez Roux AV. Walk Score® and transit score and walking in the Multi-Ethnic Study of Atherosclerosis. Am J Prev Med. 2013;45:158–166. doi: 10.1016/j.amepre.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knuiman MW, Christian HE, Divitini ML, Foster SA, Bull FC, Badland HM, et al. A longitudinal analysis of the influence of the neighborhood built environment on walking for transportation the RESIDE Study. Am J Epidemiol. 2014;180:453–461. doi: 10.1093/aje/kwu171. [DOI] [PubMed] [Google Scholar]
- Kumanyika SK, Obarzanek E, Stettler N, Bell R, Field AE, Fortmann SP, et al. Population-based prevention of obesity. The need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the Expert Panel on Population and Prevention Science). Circulation. 2008;118:428–464. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]
- Lachapelle U, Frank LD. Transit and health: mode of transport, employer-sponsored public transit pass programs, and physical activity. J Public Health Policy. 2009;30(suppl 1):S73–S94. doi: 10.1057/jphp.2008.52. [DOI] [PubMed] [Google Scholar]
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, et al. Neighborhoods, obesity, and diabetes—a randomized social experiment. N Engl J Med. 2011;365:1509–1519. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makuch RW. Adjusted survival curve estimation using covariates. J Chronic Dis. 1982;35:437–443. doi: 10.1016/0021-9681(82)90058-3. [DOI] [PubMed] [Google Scholar]
- Marshall JD, Brauer M, Frank LD. 2009. Healthy neighborhoods: walkability and air pollution. Environ Health Perspect 117 1752 1759, doi: 10.1289/ehp.0900595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack GR, Shiell A. 2011. In search of causality: a systematic review of the relationship between the built environment and physical activity among adults. Int J Behav Nutr Phys Act 8 125, doi: 10.1186/1479-5868-8-125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moudon AV. Real noise from the urban environment: how ambient community noise affects health and what can be done about it. Am J Prev Med. 2009;37:167–171. doi: 10.1016/j.amepre.2009.03.019. [DOI] [PubMed] [Google Scholar]
- Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan TE, Cooper RS, Ni H, et al. Neighborhood characteristics and hypertension. Epidemiology. 2008;19:590–598. doi: 10.1097/EDE.0b013e3181772cb2. [DOI] [PubMed] [Google Scholar]
- Müller-Riemenschneider F, Pereira G, Villanueva K, Christian H, Knuiman M, Giles-Corti B, et al. 2013. Neighborhood walkability and cardiometabolic risk factors in Australian adults: an observational study. BMC Public Health 13 755, doi: 10.1186/1471-2458-13-755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the Surgeon General (U.S.) The Surgeon General’s Vision for a Healthy and Fit Nation. 2010 Available: http://www.surgeongeneral.gov/priorities/healthy-fit-nation/obesityvision_factsheet.html (accessed 15 September 2015) [PubMed]
- Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population-health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38:105–113. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson TA, Palaniappan LP, Artinian NT, Carnethon MR, Criqui MH, Daniels SR, et al. American Heart Association Guide for Improving Cardiovascular Health at the Community Level, 2013 update: a scientific statement for public health practitioners, healthcare providers, and health policy makers. Circulation. 2013;127:1730–1753. doi: 10.1161/CIR.0b013e31828f8a94. [DOI] [PubMed] [Google Scholar]
- R Core Team. Vienna, Austria: R Foundation for Statistical Computing; 2014. R: A Language and Environment for Statistical Computing. Available: http://www.R-project.org/ [Google Scholar]
- Rundle A, Neckerman KM, Freeman L, Lovasi GS, Purciel M, Quinn J, et al. 2009. Neighborhood food environment and walkability predict obesity in New York City. Environ Health Perspect 117 442 447, doi: 10.1289/ehp.11590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF, Floyd MF, Rodriguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125:729–737. doi: 10.1161/CIRCULATIONAHA.110.969022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. The PHREG Procedure. 2014 Available: http://support.sas.com/documentation/cdl/en/statug/63033/HTML/default/viewer.htm#phreg_toc.htm (accessed 15 September 2015)
- Sundquist K, Eriksson U, Kawakami N, Skog L, Ohlsson H, Arvidsson D. Neighborhood walkability, physical activity, and walking behavior: the Swedish Neighborhood and Physical Activity (SNAP) study. Soc Sci Med. 2011;72:1266–1273. doi: 10.1016/j.socscimed.2011.03.004. [DOI] [PubMed] [Google Scholar]
- Thomas S, Wannell B. Combining cycles of the Canadian Community Health Survey. Health Rep. 2009;20:53–58. [PubMed] [Google Scholar]
- Toronto Public Health. The Walkable City: Neighbourhood Design and Preferences, Travel Choices and Health. Toronto, Ontario, Canada:Toronto Public Health. 2012 Available: http://www1.toronto.ca/city_of_toronto/toronto_public_health/healthy_public_policy/hphe/files/pdf/walkable_city.pdf (accessed 20 October 2015)
- Tu K, Campbell NR, Chen ZL, Cauch-Dudek KJ, McAlister FA. Accuracy of administrative databases in identifying patients with hypertension. Open Med. 2007;1:e18–e26. [PMC free article] [PubMed] [Google Scholar]
- Tu K, Chen Z, Lipscombe LL, Canadian Hypertension Education Program Outcomes Research Taskforce Prevalence and incidence of hypertension from 1995 to 2005: a population-based study. CMAJ. 2008;178:1429–1435. doi: 10.1503/cmaj.071283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walk Score. Walk Score Methodology. 2014 Available: https://www.walkscore.com/methodology.shtml (accessed 15 September 2015)
- Witten K, Blakely T, Bagheri N, Badland H, Ivory V, Pearce J, et al. 2012. Neighborhood built environment and transport and leisure physical activity: findings using objective exposure and outcome measures in New Zealand. Environ Health Perspect 120 971 977, doi: 10.1289/ehp.1104584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanutto EL. A comparison of propensity score and linear regression analysis of complex survey data. J Data Sci. 2006;4:67–91. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


