Abstract
Background
Over the past two decades there have been increasingly long waiting times for heart transplantation. We studied the relationship between heart transplant waiting time and transplant failure (removal from the waitlist, pre-transplant death, or death or graft failure within one-year) to determine the risk that conservative donor heart acceptance practices confer in terms of increasing the risk of failure among patients awaiting transplantation.
Methods
We studied a cohort of 28,283 adults registered on the United Network for Organ Sharing (UNOS) heart transplant waiting list between 2000 and 2010. We used Kaplan-Meier methods with inverse probability censoring weights to examine the risk of transplant failure accumulated over time spent on the waiting list (pre-transplant). In addition, we used transplant candidate blood type as an instrumental variable to assess the risk of transplant failure associated with increased wait time.
Results
Our results show that those who wait longer for a transplant have greater odds of transplant failure. While on the waitlist, the greatest risk of failure is during the first 60 days. Doubling the amount of time on the waiting list was associated with a 10% (1.01, 1.20) increase in the odds of failure within one year after transplantation.
Conclusions
Our findings suggest a relationship between time spent on the waiting list and transplant failure, thereby supporting research aimed at defining adequate donor heart quality and acceptance standards for heart transplantation.
INTRODUCTION
Heart transplantation remains the only curative therapy for a growing number of patients with end-stage heart disease1. Unfortunately, only 2,500 heart transplants are performed annually in the United States2, in large part due to a severe shortage of donor organs. Over the past two decades, use of available hearts for transplantation has decreased substantially, from a high of 38% in 2000 to 32% in 2010, with a nadir of 29% in 20063. Concurrently, the number of new active candidates on the adult heart transplant waiting list has increased substantially in recent years: in 2013, 3293 new candidates were for listed for transplantation, representing a 32%increase since 2003. Half of all candidates listed in 2012–2013 received atransplant within 9.3 months, an increase from 5.3 months in 2004–2005. The median waiting time for candidates listed in the highest priority category increased from 1.9 to 2.6 months since 2004–2005, while median waiting time for candidates listed in the intermediate priority category increased notably from 2.7 to 8.5 months during the same period.
There are several potential explanations for the decline in donor heart use, including the increased availability and use of mechanical circulatory support (such left ventricular assist devices) as an alternative to heart transplantation4. There is also potential risk aversion, as transplant centers are primarily judged on short-term outcomes, and hearts with undesirable features such as older donor age or echocardiographic abnormalities are often turned down for concern that their use may result in adverse recipient outcomes5,6.
The goal of this is analysis is to understand the impact of increased waiting time on a patient's risk of transplant failure. There are many challenges in using observational data to assess the relationship between waiting time and transplant failure: sicker patients may die sooner; “pickier” physicians may wait for better hearts for their patients; or healthier patients may be perceived as able to wait longer. To account for these concerns we used a mixed methods approach to study the relationship between heart transplant waiting time and transplant failure to determine the risk associated with increasing the amount of time spent waiting to receive a transplant.
MATERIALS AND METHODS
Data
Cohort
This study used adult heart transplant waiting list and post-transplant survival data obtained from the United Network for Organ Sharing (UNOS). The UNOS heart transplant registry contains data regarding every organ donation and transplant occurring in the United States since 1986. Heart transplant candidate data are submitted by the transplant center to UNOS at the time of listing, and are updated at the time of transplantation. After transplantation, centers are required to submit data to UNOS at 1-year post-transplant, and annually thereafter.7All individuals between 18 and 70 years of age who were placed on the heart transplant waiting list from January 1, 2000 to December 31, 2010 were available for analysis. Follow-up extended through December 31, 2011, providing a minimum of one year of potential follow-up. Patients who received multi-organ transplants or who were listed as “inactive” were excluded. “Inactive” is the designation for patients who are temporarily removed from the heart transplant waiting list due to health conditions or personal circumstances.
Detailed information on a subset of the heart transplant donors in this cohort were obtained from the Donor Network West (DNW) and were used for testing certain analytic assumptions. The DNW database is a research database created by the study investigators in collaboration with colleagues at DNW—an organ procurement organization based in Northern California. The database, described elsewhere8, contains detailed data on demographic variables, cause of death, health-related behaviors, and past medical history collected on 2,048 consecutive donors managed by DNW from 2001–2008. All data were collected via manual review of the donor medical records. The UNOS and DNW databases were linked using the UNOS ID number, a unique identifier assigned to each potential organ donor in the United States.
This study was approved by DNW and by the Stanford University Institutional Review Board.
Outcomes
Our primary goal was to assess failure of the transplant process. We considered outcomes during two different time periods: pre-transplant and post-transplant. For the pre-transplant period, UNOS provides waitlist removal codes for all heart transplant candidates on the waiting list, as well as the date of death, when applicable. We defined pre-transplant failure as removal from the heart transplant waiting list for worsening medical condition or death. We combined worsening medical condition with death, since removal for this reason is an indication that a patient is too sick to receive a transplant, and therefore represents failure of the transplant process. For the post-transplant period, UNOS provides annual follow-up data for all heart transplant recipients, as well as the date of death or graft failure, when applicable. Similarly, we considered graft failure or death as post-transplant failures.
Exposure of Interest
The exposure of interest was time (in days) on the heart transplant waiting list. This was calculated from the date of listing to the date of removal from the waiting list. In an experimental study we would be able to randomly assign patients to different waiting times (or strategies) and observe the relationship with transplant failure. With observational data, this is not possible and we can only analyze the observed waiting time.
Use of Blood Type
As others have noted, patient blood type can serve as a natural randomizer for time to receive a transplant9, making it well suited to serve as an instrumental variable (IV). There are three primary assumptions for an IV approach to be appropriate10: these are (1) the IV (blood type) is associated with the treatment of interest (time on wait list), (2) the IV is not related to any measured and unmeasured confounders, (3) and the IV is related to the outcome only through the treatment.
Heart transplants are allocated according to blood type (ABO-identical or compatible)11, such that type AB patients can receive a donor heart of any blood type. Given this matching criterion, type O candidates will typically wait longer to receive a suitable heart than candidates of other blood types (assumption 1)12–15. However, there is no biological reason to suspect that candidates with different blood types will be more or less likely to die on the waitlist or have different transplant outcomes (assumption 3). A concern is that blood type will differ by race (potential violation of assumption 2) or patients with type O blood may receive lower quality hearts (potential violation of assumption 3). We addressed these potential violations analytically.
Additional Covariates
We abstracted covariates available at the time of placement on the waitlist. These included age, sex, race (White, Black, Asian, Hispanic, Other), insurance payor, wait list priority status, body mass index, diabetes and use of extracorporeal membrane oxygenation, left ventricular assist device, and mechanical ventilation. Time on the wait list will differ based on one's initial listing status. At the time of listing, patients are placed into one of three priority categories based on their clinical acuity (1A-highest, 1B-intermediate, and 2-lowest priority). To assess whether effects differed based on priority status, we stratified all analyses based on initial listing status.
Analytic Framework
Our primary interest was to understand the impact of time spent waiting for a transplant on mortality or transplant failure. To do so, we first assessed whether patients who are “randomly” assigned to wait longer for a transplant have worse outcomes. Next, to further understand the role of waiting time, we considered that patients could fail either before receiving or after receiving a transplant. As such we considered two distinct analytic periods: pre-transplant and post-transplant, and assessed the impact of time spent waiting on failure during each of these periods.
Overall Analysis
To establish the relationship between wait time and transplant failure, we used patients' blood type as a randomizer. We estimated the cause-specific hazard ratio for time to transplant based on blood type. Since we were interested in the observed rate of transplantation, this hazard is more appropriate than the alternative subdistribution hazard – the alternative hazard in the presence of competing events16,17. We next regressed the probability of being alive at one-year after listing onto blood type. We used both failure during the pre- and post-transplant periods to define the overall outcome. This is an analysis of the natural experiment. While this does not provide an estimate of a causal parameter, under the IV assumptions it establishes the relationship between the exposure (waiting time) and outcome (survival).
Pre-transplant analysis
After establishing the impact of waiting time, we estimated the cumulative risk of failure over time spent waiting. To do so, we estimated the Kaplan-Meier curve for time to failure while on the waitlist. The Kaplan-Meier estimate provides a non-parametric function for the change in probability of failure over time, i.e. a function of spending time on the waitlist. One challenge in estimating the Kaplan-Meier curve is that those who are transplanted are informatively censored, leading to a biased estimate. Therefore, we estimated the Kaplan-Meier curve with inverse probability censoring weights18. Specifically, we used a Cox Proportional Hazards model to calculate transplant (censoring) probabilities over time, adjusting for the baseline clinical covariates. For computational purposes, we coarsened time into 7 day increments. We used these survival probabilities to calculate stabilized inverse probability censoring weights. We then used these weights to estimate the Kaplan-Meier function.
Post-transplant analysis
To assess the impact of time spent waiting on post-transplant outcomes, we studied the patients who received a transplant and regressed the probability of not having a failure by one-year post-transplant onto time spent waiting. One challenge in such an analysis is the potential for unmeasured confounding. Specifically, it is possible that patients with “pickier” or more selective physicians spend more time on the waitlist. The UNOS data does not have high quality data on donor heart characteristics or function (while the DNW database described above does). Therefore, we utilized patient blood type as an IV. Since the analysis is conditional on being transplanted, one way to interpret the IV estimate is as the increased odds of failure of two people about to receive a transplant, with one person having spent more time than the other on the waitlist. Patients with AB blood type will have a short-listing strategy, those with O blood type will have a long-listing strategy, and those with A or B blood type will have an intermediate-listing strategy.
We used a two-stage residual inclusion model to estimate the association between waiting time and the odds of death19,20. This model has been shown to be more appropriate than the more typical two-stage least squares model when dealing with binary data. Due to the skewness of waitlist time, we log transformed waitlist time to log2. Therefore, for the post-transplant analysis the point estimate represents the effect of doubling waiting time (e.g. 10 days to 20 days) on the odds of transplant failure. In the first stage, we regressed the exposure of interest (log time on waiting list) on the instrumental variable (blood type) and any other measured confounders (e.g. race). In the second stage, we regressed the logit of the probability of the outcome (graft failure or death) onto the residual values from the first stage and the confounders. Finally, 1000 bootstraps were performed to obtain proper standard errors.
Sensitivity Analysis
We performed several sensitivity analyses. First, we restricted the analysis to July 2006 onwards, when the national cardiac allocation system was changed to direct more donor hearts to status 1A and 1B candidates via broader regional sharing. Use of ventricular assist devices also became increasingly common during this period. Additionally, we considered two sources of residual bias. The first is race, since frequency of blood type can differ by racial group and different racial groups may experience differential post-transplant outcomes21. While all models were adjusted for race, we also performed the two-stage residual inclusion analyses stratified by race as a sensitivity analysis. The second potential source of bias involves physicians waiting for a “more desirable” heart for blood type AB candidates, knowing that these candidates will, in general, receive more organ offers. We used the DNW database to examine whether differences exist in heart transplant donor characteristics between recipients of different blood types. Finally, to assess the impact of the instrumental variable analysis, we estimated a comparable logistic regression model using waiting time as the predictor variable of interest and controlling for the same covariates.
Statistical analyses were performed using R (version 3.01)22.
RESULTS
From January 1, 2000 through December 31, 2010, 29,654 patients between 18 and 70 years of age were placed on the heart transplant waiting list. Of these, 789 were excluded from analysis for being listed with an “inactive” status (e.g. active infection or pending additional testing), four for having a transplant date before their wait list date, and 578 for being recipients of multi-organ transplants, resulting in a final cohort of 28,283 participants. Table 1 summarizes patient demographics. By December 31, 2011, 18,807 (66%) patients received a transplant, 4,743 (17%) died while on the waitlist or were removed for medical reasons, 3,024 (11%) were still active on the waitlist and 1,709 (6%) saw their condition improve. The only variable with missing data was BMI (n = 299, 1%). For simplicity we performed a single mean imputation of BMI for all analyses.
Table 1.
Characteristics of patients listed for heart transplantation, stratified by blood type
| Blood Type | O | A | B | AB | |
|---|---|---|---|---|---|
| Number of patients | 12,335 (44%) | 11068 (39%) | 3674 (13%) | 1206 (4%) | |
|
Time on waiting list (days)a |
178 (51,512) | 84 (23,288) | 80 (23,255) | 33 (10,100) | |
| Waitlist Outcome | |||||
| Transplanted | 7213 (58%) | 7960 (72%) | 2665 (73%) | 969 (80%) | |
| Died on Waitlist | 1883 (15%) | 1164 (11%) | 373 (10%) | 102 (8%) | |
| Removed from list for worsening medical condition |
669 (5%) | 382 (3%) | 132 (4%) | 38 (3%) | |
| Removed from list for improved medical condition |
900 (7%) | 574 (5%) | 191 (5%) | 44 (4%) | |
| On waitlist at end of study |
1670 (14%) | 988 (9%) | 313 (9%) | 53 (4%) | |
| Transplant Outcome | |||||
| Died within 1 year of transplant |
595 (8%) | 731 (9%) | 265 (10%) | 89 (9%) | |
| Graft failure within 1 year of transplant |
23 (<1%) | 27 (<1%) | 9 (<1%) | 4 (<1%) | |
| Demographics | |||||
| Age (years)a | 54 (44, 60) | 55 (46, 61) | 53 (43, 60) | 53 (44, 61) | |
| Sex (male) | 9200 (75%) | 8493 (77%) | 2726 (74%) | 908 (75%) | |
| Race | |||||
| White | 8502 (69%) | 8722 (79%) | 2196 (60%) | 858 (71%) | |
| Black | 2388 (19%) | 1342 (12%) | 1031 (28%) | 242 (20%) | |
| Asian | 226 (2%) | 180 (2%) | 191 (5%) | 40 (3%) | |
| Hispanic | 1065 (9%) | 680 (6%) | 219 (6%) | 53 (4%) | |
| Other | 154 (1%) | 94 (1%) | 37 (1%) | 13 (1%) | |
| Insurance payor | |||||
| Public | 3842 (31%) | 3245 (29%) | 1141 (31%) | 364 (30%) | |
| Private | 7070 (57%) | 6479 (59%) | 2121 (58%) | 702 (58%) | |
| Other | 1423 (12%) | 1344 (12%) | 412 (11%) | 140 (12%) | |
| Clinical | |||||
| Waiting list status | |||||
| 1A | 2463 (20%) | 2274 (21%) | 836 (23%) | 280 (23%) | |
| 1B | 3909 (32%) | 3372 (30%) | 1211 (33%) | 386 (32%) | |
| 2 | 5963 (48%) | 5422 (49%) | 1627 (44%) | 540 (45%) | |
| Body mass indexa (kg/m2) |
27 (24, 30) | 27 (24, 30) | 27 (23, 30) | 26 (23, 30) | |
| Diabetes | 2034 (25%) | 2772 (25%) | 897 (25%) | 288 (24%) | |
| ECMO | 71 (1%) | 83 (1%) | 25 (1%) | 13 (1%) | |
| LVAD | 687 (6%) | 572 (5%) | 216 (6%) | 55 (5%) | |
| Mechanical ventilation | 549 (4%) | 498 (4%) | 170 (5%) | 60 (5%) | |
ECMO: extracorporeal membrane oxygenation, LVAD: left ventricular assist device
Continuous variables are median and interquartile range width.
Natural Experiment
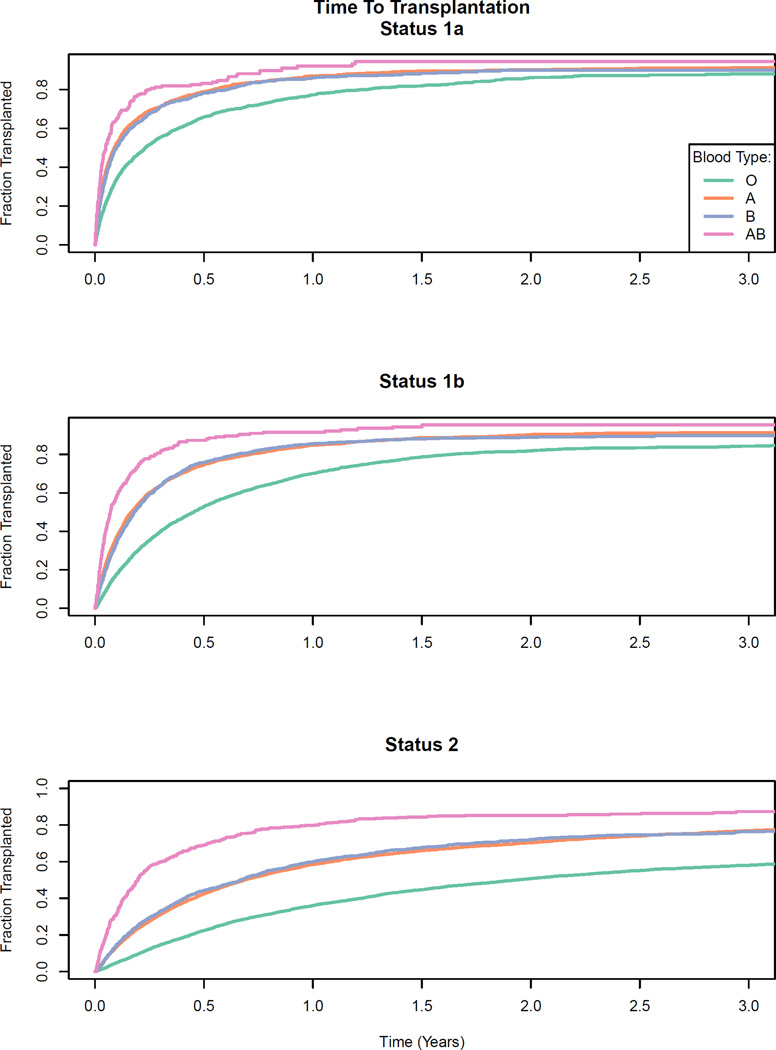
People with type O blood spent approximately five times longer on the waiting list than those with blood type AB (Table 1). After adjustment, patients with type AB blood had a cause-specific hazard ratio for transplantation of 2.88 (2.69, 3.08) compared to type O patients, and patients with blood types A and B had HRs of 1.63 (1.58, 1.68) and 1.70 (1.62, 1.78), respectively (Figure 1). We next assessed overall survival at one-year (Table 2), regardless of transplant status. Among status 1A patients (the sickest patients) Type O patients had the greatest odds of being dead at 1 year while type AB patients had the lowest. There was no observed effect among status 2 (lowest priority) patients.
Figure 1.
Relationship between heart transplant candidate blood type and time to transplantation, stratified on priority status. Type AB candidates receive a heart faster than Type O candidates.
Table 2.
Transplant Failurea within 1 year of Waitlisting by Blood Type and Status
| Type Ob | Type Ac | Type Bc | Type ABc | |
|---|---|---|---|---|
| All | 21% | 0.95 (0.85, 1.06) | 1.08 (0.92, 1.27) | 0.96 (0.73, 1.25) |
| Status 1A | 34% | 0.84 (0.73, 0.97) | 0.81 (0.67, 0.98) | 0.67 (0.49, 0.91) |
| Status 1B | 23% | 0.83 (0.73, 0.93) | 0.78 (0.66, 0.92) | 0.93 (0.72, 1.22) |
| Status 2 | 14% | 0.95 (0.85, 1.06) | 1.08 (0.92, 1.27) | 0.96 (0.73, 1.25) |
Transplant failure consists of mortality, removal from waitlist for medical reasons or transplant organ failure
Baseline 1 year failure rate
Adjusted odds-ratio relative to blood type O recipients
Model adjusted for: gender, age, race, list year, payor, BMI (categorical), LVAD, ventilator, ECMO, diabetes
Failure on the Waitlist
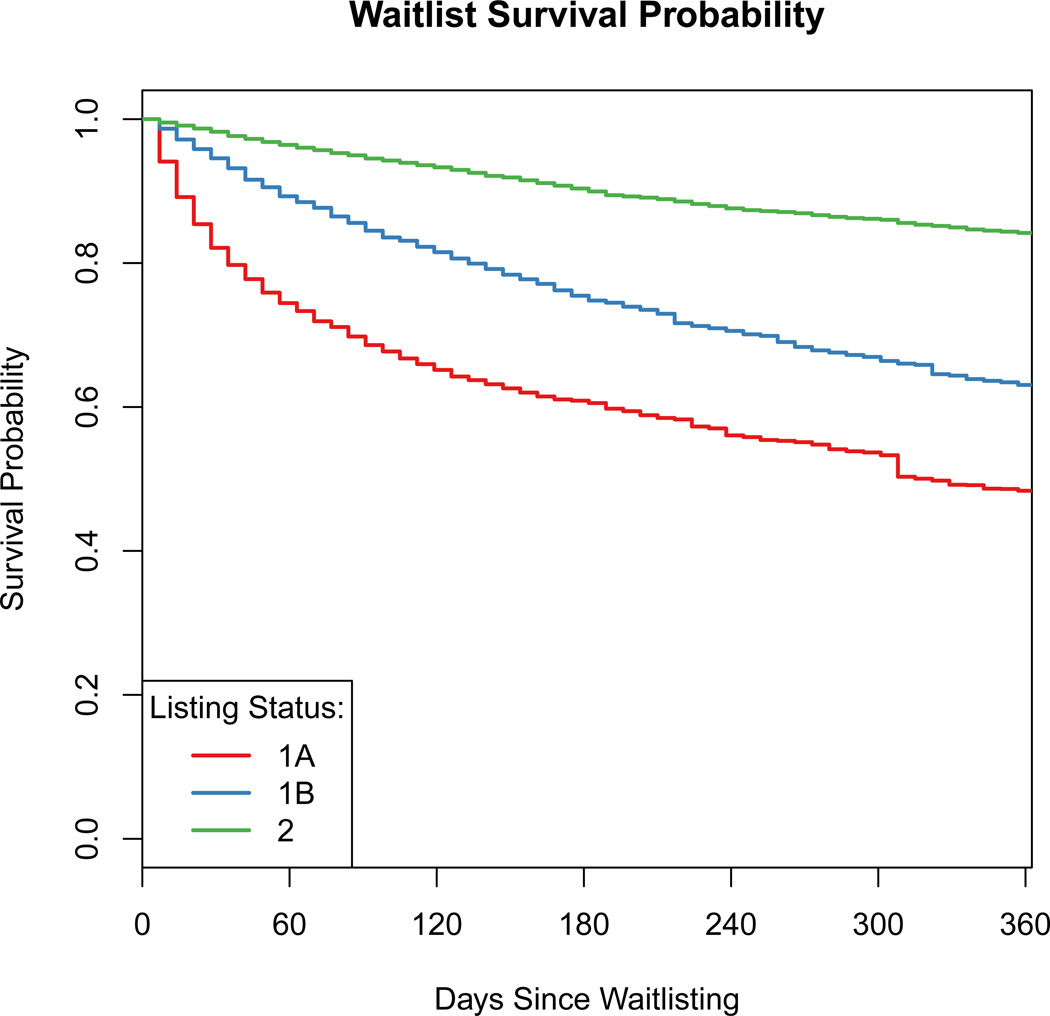
After suggesting that those who spend more time on the waitlist (Type O patients) have greater odds of being dead after one-year, we decomposed the effect of waiting time into the pre-and post-transplant periods. Figure 2 shows inverse probability censoring weights-adjusted Kaplan-Meier curves for death on the waitlist, stratified on candidate listing status, during the first year after listing. Not surprisingly, the survival probability differs based on initial status with Status 2 patients having a 35% greater survival probability than Status 1A patients (84% vs 48%). The greatest decline in survival for both Status 1A and 1B patients is during the first 60 days after listing. This corresponds well with time on the waitlist with Status 1A, 1B, and 2 patients having median waiting times of 27, 71, and 252 days respectively.
Figure 2.
Kaplan-Meier curves for death on the waitlist. Curves are adjusted for transplantation using inverse probability censoring weights, Type 1A patients (the sickest) experience the fastest drop in survival during the first 60–90 days after being listed.
Failure after Transplantation
To assess the effect of waiting time on death after transplantation, we returned to our “natural experiment,” using blood type as an IV. The first assumption in an IV analysis is that the instrument is related to the exposure (time on the waiting list), which we established above. The second assumption is that patient characteristics do not differ based on levels of the instrument. Patient characteristics stratified on blood type are shown in Table 1. Blood type did not meaningfully differ across clinical characteristics, with the expected exception of race..
It is possible that if physicians expect type O candidates to wait longer to receive a transplant, less sick patients will be listed at a higher status in an effort to “move them up the list.” Such a scenario would be a violation of the IV assumptions. We compared the clinical characteristics of patients at time of listing stratified on blood type and listing status (eFigure 1). There was no indication that blood type O patients were less sick than blood type AB patients, with similar rates of use of mechanical ventilation and mechanical circulatory support
The third assumption is that the observed relationship between the blood type and death is only though time spent on the waitlist. This assumption is not directly testable but can be further examined. For example, it is possible that patients with type AB blood may receive “higher quality” hearts because their doctors perceive that they can afford to turn down less desirable hearts. Examination of a subset of 779 recipients on whom we obtained data on detailed donor characteristics from DNW suggested that this was not the case (eTable 1). A comparison of donor characteristics related to heart acceptance did not show differences between recipients of different blood types.
We assessed the impact of time spent waiting on post-transplant survival among the 18,807 patients who received a heart transplant. We used two-stage residual inclusion analyses to estimate the increased risk conferred on those who spend more time on the heart transplant waitlist, both at 30 days and 1 year after transplantation. We detected a slight effect on survival after heart transplantation based on the length of time spent waiting (Table 3). The results were consistent across the status categories, suggesting an overall 10% increase in the odds of death for every doubling of the time spent waiting. The results were similar for both 30 day and 1 year outcomes. The naïve logistic regression analysis suggested no relationship between waiting time and transplant failure.
Table 3.
Effect estimates on post transplant failure for doubling time spent on the heart transplant waiting list
| 3a. Outcome= Death or graft failure within 1 year post-transplant | |||
| Number of Events (%) | Logistic Regression Analysis | Instrumental Variable Analysis | |
| Overall | 2211 (12%) | 1.01 (0.99, 1.04) | 1.10 (1.01, 1.20) |
| Status 1A | 570 (15%) | 1.00 (0.95, 1.04) | 1.08 (0.89, 1.29) |
| Status 1B | 719 (11%) | 1.01 (0.97, 1.05) | 1.12 (0.96, 1.28) |
| Status 2 | 922 (12%) | 1.04 (1.00, 1.07) | 1.09 (0.95, 1.24) |
| 3b. Outcome= Death or graft failure within 30 days post-transplant | |||
| Number of Events (%) | Logistic Regression Analysis | Instrumental Variable Analysis | |
| Overall | 999 (5%) | 1.03 (0.99, 1.06) | 1.08 (0.96, 1.23) |
| Status 1A | 268 (7%) | 1.00 (0.94, 1.06) | 1.10 (0.83, 1.42) |
| Status 1B | 318 (5%) | 1.04 (0.97, 1.10) | 1.11 (0.90, 1.36) |
| Status 2 | 413 (5%) | 1.05 (1.00, 1.11) | 1.06 (0.88, 1.27) |
Model adjusted for: gender, age, race, list year, diagnosis, payor, BMI (categorical), LVAD, ventilator, ECMO, diabetes
Sensitivity Analyses
We first limited the study cohort to patients placed on the waitlist after July 2006 (n = 6,183) (eTable 2a). The adverse effect of spending additional time waiting for a transplant on the risk of death was more pronounced in these later years; however, due to the smaller sample size, the results were not statistically significant. Second, we stratified the analyses by race; only the results for Whites and Blacks are shown, due to smaller sample sizes (eTable 2b). This analysis suggests minimal racial heterogeneity. Finally, we stratified the analyses by sex, since sex-based differences in cardiovascular disease are being increasingly recognized. There was a suggestion that the post-transplant effect was stronger in men than in women (eTable 2c).
DISCUSSION
Our findings characterize the relationship between time spent waiting for a heart transplant and risk of transplant failure, either during the pre-or post-transplant periods. Overall, among the sickest patients (status 1A), those who receive a heart sooner have a greater odds of success after one-year. The mortality rate among candidates awaiting transplantation is highest during the first 60 days after listing. Among transplanted patients, those who spent double the amount of time on the waitlist had a 10% increase in the odds of transplant failure. Our results were robust when the analyses were stratified by transplant era as well as candidate race and sex.
This works highlights the challenges of analyzing observational data. In assessing the relationship between waiting time and transplant failure there is high potential for confounding and circularity. We used a mixed methods approach for our analyses. We first used blood type as a natural randomizer to establish that those who wait longer for a transplant have worse post-transplant outcomes. To further understand that relationship we partitioned time into pre-and post-transplant periods. We assessed waitlist failure by analyzing the KM curve with an IPCW estimator to account for informative censoring (due to transplantation). Finally, to determine whether patients who had to wait longer for their transplant had worse outcomes, we used blood type in an IV analysis. Since this analysis is conditional on transplantation, there is not a direct causal (manipulable) interpretation. Instead the observed association informs the difference between patients who survive a longer waiting time compared to those who are transplanted earlier.
Over the past decade, the steady decline in use of available donor hearts, combined with an increase in new candidates listed, has resulted in increased time spent waiting for transplantation. During this time, adoption of increasingly conservative practices has reduced the proportion of donor hearts accepted for transplantation. In a prior analysis of the UNOS heart transplant registry, our group showed that the percentage of hearts accepted for transplantation from donors over 50 years of age, female donors, and donors who died of cerebrovascular causes (e.g. stroke) decreased significantly between 1995 and 2010, reflecting increasing risk aversion in the heart transplant community3. However, this decrease in the use of donor hearts with one or more “high risk” features did not result in substantially improved transplant outcomes. In fact, many previous studies have demonstrated a lack of association between donor characteristics and recipient outcomes after heart transplantation8,12,23–25 with several notable exceptions, including older donor age, especially in the setting of a prolonged ischemic time6.
Our analytic approach had several inherent strengths, including large sample size (>28,000 patients) from a well-defined population that includes almost all patients in need of a heart transplant in the United States over a 10-year period. We were able to assess the suitability of the IV via a detailed donor research database on a subset of the sample; this enabled us to compare donor characteristics between recipients of different blood types in order to determine whether donor heart quality may influence post-transplant outcomes for patients of different blood types. One interesting finding was that the results obtained from the IV and logistic regression analyses were very similar, suggesting that strong biases may not be present in this case.
There are potential limitations of our analyses. In estimating the inverse probability censoring weights we were only able to use baseline patient information. Therefore, if a patient's clinical acuity changed substantially after listing, the censoring weights may be incorrect. Moreover, the nature of the analysis only allows us to observe waitlist survival. An ideal analysis – not possible with the present data – would be to assess waitlist strategies, i.e. compare physicians who were more or less aggressive about listing their patients for transplantation and/or accepting marginal donor hearts. The post-transplant analysis approximates such a design, but since the analysis is conditional on being transplanted it is not a true causal analysis. It is possible that clinicians are aware of the differential waiting times and are either moving type O patients into a higher priority status or are more aggressive in transplanting type O patients, introducing unmeasured confounding. While a concern, the data does suggest that type AB patients of the same priority status are just as sick as type O patients and that all patients receive hearts of similar quality.
An important consideration is how to interpret these findings from a public health context. The results suggest that waiting to receive a heart has a detrimental impact on overall survival. However, this analysis does not assess the impact of being “picky” (i.e. waiting for a better heart). In fact, the IV analysis is meant to remove the impact of such confounding. Therefore, this analysis only attempts to answer half of the question: namely, what is the impact of waiting? It does not attempt to evaluate the impact of getting a 'better' heart. One way of interpreting the IV analysis is: given two people who match to a single heart, if one of them spent 30 days on the waitlist and the other spent 60 days, who would we expect to live longer with the heart? This question is likely more salient to transplant centers than to individual patients, since centers are judged on one-year outcomes after transplantation. Ultimately, this work suggests the benefits that being “picky” must beget in order to overcome the detriments of spending more time on the waitlist. However, as discussed, previous work has suggested that donor heart quality has a minimal impact on overall post-transplant survival, making this question worthy of fuller consideration, ideally in a prospective fashion.
In conclusion, we have demonstrated a positive relationship between time spent on the waiting list and mortality in heart transplant candidates. This finding is relevant in the face of a national donor shortage and conservative donor heart acceptance practices, which in combination result in increasingly long waiting times for heart transplantation. Studies such as this underscore the need for research efforts aimed at defining adequate donor heart quality and acceptance standards for heart transplantation.
Supplementary Material
Acknowledgments
We thank the anonymous reviewers and editor for their thoughtful comments. We thank Donor Network West and the United Network for Organ Sharing for access to the data required for this study. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government. This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (K25DK097279, B.A.G.) and the National Heart, Lung, and Blood Institute (K23HL091143, K.K.K.). The data reported here have been supplied by the United Network for Organ Sharing as the contractor for the Organ Procurement and Transplantation Network, and was supported in part by Health Resources and Services Administration contract 234-2005-370011C.
Contributor Information
Benjamin A. Goldstein, Department of Biostatistics and Bioinformatics, Duke University, Durham, NC.
Laine Thomas, Department of Biostatistics and Bioinformatics, Duke University, Durham, NC.
Jonathan G. Zaroff, Kaiser Northern California Division of Research, Oakland, CA
John Nguyen, Donor Network West, Oakland, CA.
Rebecca Menza, Graduate School of Nursing, Midwifery, and Health, Victoria University of Wellington, New Zealand.
Kiran K. Khush, Division of Cardiovascular Medicine, Department of Medicine, Stanford University School of Medicine, Palo Alto, CA
References
- 1.Mozaffarian D, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.Lund LH, et al. The registry of the International Society for Heart and Lung Transplantation: thirty-first official adult heart transplant report--2014; focus theme: retransplantation. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2014;33:996–1008. doi: 10.1016/j.healun.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Khush KK, Zaroff JG, Nguyen J, Menza R, Goldstein BA. National decline in donor heart utilization with regional variability: 1995–2010. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2015;15:642–649. doi: 10.1111/ajt.13055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kirklin JK, et al. Fifth INTERMACS annual report: risk factor analysis from more than 6,000 mechanical circulatory support patients. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2013;32:141–156. doi: 10.1016/j.healun.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Stehlik J, et al. The Registry of the International Society for Heart and Lung Transplantation: 29th official adult heart transplant report-2012. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2012;31:1052–1064. doi: 10.1016/j.healun.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 6.Wever Pinzon O, et al. Impact of donor left ventricular hypertrophy on survival after heart transplant. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2011;11:2755–2761. doi: 10.1111/j.1600-6143.2011.03744.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dickinson DM, et al. Transplant data: sources, collection, and caveats. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2004;4(Suppl 9):13–26. doi: 10.1111/j.1600-6135.2004.00395.x. [DOI] [PubMed] [Google Scholar]
- 8.Khush KK, Menza R, Nguyen J, Zaroff JG, Goldstein BA. Donor predictors of allograft use and recipient outcomes after heart transplantation. Circ. Heart Fail. 2013;6:300–309. doi: 10.1161/CIRCHEARTFAILURE.112.000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Everhart JE, et al. Increased waiting time for liver transplantation results in higher mortality. Transplantation. 1997;64:1300–1306. doi: 10.1097/00007890-199711150-00012. [DOI] [PubMed] [Google Scholar]
- 10.Baiocchi M, Cheng J, Small DS. Instrumental variable methods for causal inference. Stat. Med. 2014;33:2297–2340. doi: 10.1002/sim.6128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jawitz OK, G Jawitz N, Yuh DD, Bonde P. Impact of ABO compatibility on outcomes after heart transplantation in a national cohort during the past decade. J. Thorac. Cardiovasc. Surg. 2013;146:1239–1245. doi: 10.1016/j.jtcvs.2013.06.040. discussion 1245–1246. [DOI] [PubMed] [Google Scholar]
- 12.Chen JM, et al. Multivariate analysis of factors affecting waiting time to heart transplantation. Ann. Thorac. Surg. 1996;61:570–575. doi: 10.1016/0003-4975(95)01031-9. [DOI] [PubMed] [Google Scholar]
- 13.Hussey JC, Parameshwar J, Banner NR UK Transplant Cardiothoracic Advisory Group (CTAG) Influence of blood group on mortality and waiting time before heart transplantation in the United kingdom: implications for equity of access. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2007;26:30–33. doi: 10.1016/j.healun.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 14.Rexius H, Nyström U, Lorentzon U, Nilsson F, Jeppsson A. The use of ABO compatible non-identical organs for cardiac transplantation: are we treating potential recipients with blood group O fairly? J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2001;20:207. doi: 10.1016/s1053-2498(00)00446-0. [DOI] [PubMed] [Google Scholar]
- 15.Sharples LD, et al. Heart transplantation in the United Kingdom: who waits longest and why. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 1995;14:236–243. [PubMed] [Google Scholar]
- 16.Lau B, Cole SR, Gange SJ. Competing risk regression models for epidemiologic data. Am. J. Epidemiol. 2009;170:244–256. doi: 10.1093/aje/kwp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prentice RL, et al. The analysis of failure times in the presence of competing risks. Biometrics. 1978;34:541–554. [PubMed] [Google Scholar]
- 18.Hernán MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiol. Camb. Mass. 2000;11:561–570. doi: 10.1097/00001648-200009000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Cai B, Small DS, Have TRT. Two-stage instrumental variable methods for estimating the causal odds ratio: analysis of bias. Stat. Med. 2011;30:1809–1824. doi: 10.1002/sim.4241. [DOI] [PubMed] [Google Scholar]
- 20.Terza JV, Basu A, Rathouz PJ. Two-stage residual inclusion estimation: addressing endogeneity in health econometric modeling. J. Health Econ. 2008;27:531–543. doi: 10.1016/j.jhealeco.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu V, Bhattacharya J, Weill D, Hlatky MA. Persistent racial disparities in survival after heart transplantation. Circulation. 2011;123:1642–1649. doi: 10.1161/CIRCULATIONAHA.110.976811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.R Core Team. R: A language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2012. at < www.R-project.org>. [Google Scholar]
- 23.Lima B, et al. Marginal cardiac allografts do not have increased primary graft dysfunction in alternate list transplantation. Circulation. 2006;114:I27–132. doi: 10.1161/CIRCULATIONAHA.105.000737. [DOI] [PubMed] [Google Scholar]
- 24.Ott GY, et al. Cardiac allografts from high-risk donors: excellent clinical results. Ann. Thorac. Surg. 1994;57:76–81. doi: 10.1016/0003-4975(94)90368-9. discussion 81–82. [DOI] [PubMed] [Google Scholar]
- 25.Weiss ES, et al. Development of a quantitative donor risk index to predict short-term mortality in orthotopic heart transplantation. J. Heart Lung Transplant. Off. Publ. Int. Soc. Heart Transplant. 2012;31:266–273. doi: 10.1016/j.healun.2011.10.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.