Abstract
This secondary data analysis examined effects of an abstinence contingency on participation in a therapeutic workplace. Participants exposed to a pay reset after drug use did not differ in overall attendance from participants who were not exposed to a pay reset after drug use; however, they initially worked less after a pay reset than participants who did not receive a pay reset, and their attendance increased as their pay increased. Overall participation was not influenced by the abstinence contingency, but transient decreases in attendance occurred.
Keywords: abstinence reinforcement, contingency management, employment, reset, therapeutic workplace
The therapeutic workplace was designed to promote drug abstinence, education, and job-skills development in unemployed adults with long histories of drug addiction (Silverman, 2004; Silverman, DeFulio, & Sigurdsson, 2012). Therapeutic workplace participants are paid for working in a model workplace, but they must provide drug-negative urine samples to gain access to the workplace and maintain maximum pay. Participants who provide a drug-positive urine sample are not allowed to work until they provide a drug-negative sample; they then receive a temporary decrease in pay, which can again increase each day that the participant provides a drug-negative sample. This escalating schedule of reinforcement was adapted from the procedures developed by Higgins et al. (1991). Because many participants lack basic academic and job skills, the intervention has two phases through which participants can progress sequentially. In the initial phase, a participant’s “job” is to participate in an education and job-skills training program. After participants acquire needed skills and become abstinent, they can progress to the second phase in which they can perform real jobs.
The employment-based abstinence contingency, in which participants who provide a drug-positive urine sample are suspended from work and receive a temporary pay decrease (i.e., the suspension-plus-reset contingency), can initiate (Silverman et al., 2007) and maintain (DeFulio, Donlin, Wong, & Silverman, 2009) drug abstinence. However, this contingency can have deleterious effects on workplace participation. In a clinical trial that examined whether the therapeutic workplace could promote cocaine abstinence in methadone patients, the suspension-plus-reset contingency increased cocaine abstinence but also reduced workplace attendance (Silverman et al., 2007). Specifically, the percentage of days attended during the 26-week intervention was significantly lower among participants who were exposed to the contingency than for participants who were given unconstrained access to the workplace (39% and 71%, respectively). Because the goal of the training phase of the therapeutic workplace is to promote drug abstinence and skills development, identification of methods to minimize the decrease in attendance following the implementation of abstinence contingencies is needed.
This report describes an analysis of data from a clinical trial that used a modified employment-based abstinence contingency. Under this modified reset-only contingency, participants received a temporary pay decrease if they did not meet a drug-abstinence requirement; however, they were not suspended from work. This reset-only contingency promoted abstinence from opiates and cocaine (Holtyn et al., 2014a, 2014b); however, a detailed analysis of effects of the contingency on workplace participation was not reported. The present analysis examined global effects of the reset-only contingency on overall attendance and hours worked as well as local effects immediately after a reset.
METHOD
The original trial on which this analysis is based examined whether the therapeutic workplace could promote drug abstinence and methadone treatment enrollment among unemployed and out-of-treatment adults who injected drugs. The primary outcomes and detailed methods have been reported elsewhere (Holtyn et al., 2014a, 2014b). Methods pertaining to the present analysis are described below.
Design and Description of Conditions
During a 4-week induction, participants could attend the training phase of the therapeutic workplace for 4 hr every weekday and were encouraged to enroll in methadone treatment. Participants could earn $8 per hour in base pay plus approximately $2 per hour for their performance on training programs. They were paid in vouchers that were exchangeable for goods and services. Urine samples were collected and tested for opiates and cocaine on Mondays, Wednesdays, and Fridays. Every Monday, each participant’s methadone program was contacted to confirm enrollment in methadone treatment. Participants (N = 98) who completed the induction period were randomly assigned to one of three conditions (abstinence, methadone, and work reinforcement; methadone and work reinforcement; or work reinforcement) and were invited to attend the workplace for an additional 26 weeks.
Abstinence, methadone, and work reinforcement participants (n = 33) had to provide opiate- and cocaine-negative urine samples and had to enroll in methadone treatment. The drug-abstinence requirement used a reset-only contingency: If participants provided an opiate- or cocaine-positive urine sample (i.e., urinary morphine and benzoylecgonine concentrations had to be less than 300 ng/ml or at least 20% lower per day since the last sample) or failed to provide a sample, their base pay rate was temporarily reduced from $8 to $1 per hour. After the reset, the participant’s base pay increased by $1 per hour to the maximum of $8 per hour for every day that the participant met the abstinence requirement and attended the workplace. Methadone and work reinforcement participants (n = 35) only had to enroll in methadone treatment; these participants could work and earn wages at the maximum pay rate even if their urine samples tested opiate or cocaine positive. Work reinforcement participants (n = 30) could work and earn wages at the maximum pay rate even if they were not enrolled in methadone treatment and their urine samples tested opiate or cocaine positive.
Methadone Treatment
Most participants enrolled in methadone treatment; there were no significant between-condition differences in enrollment. Participants in the abstinence, methadone, and work reinforcement and the methadone and work reinforcement conditions were exposed to a suspension-plus-reset contingency: If participants were not enrolled in methadone treatment, they were not allowed access to the workplace until they enrolled and their base pay rate was temporarily reduced. Participants in these two conditions experienced very few resets for failing to enroll, and those resets were not included in the analyses below.
Data Analysis
Overall attendance for each participant was calculated as the number of days he or she attended the workplace divided by the number of available workdays. Number of hours worked for each participant was calculated based only on days that he or she attended the workplace to provide a measure of engagement when a participant was in the workplace. Global measures of attendance and hours worked were analyzed using one-way ANOVAs.
To identify local effects of the reset-only contingency, attendance and hours worked after a reset were examined. However, a reset occurred whenever abstinence, methadone, and work reinforcement participants provided a drug-positive sample or failed to provide a sample. Thus, effects of the reset contingency are confounded with active drug use and missed urine samples. For this reason, we compared attendance and hours worked the day before and the day after a pay reset (for the abstinence, methadone, and work reinforcement participants) and a sham reset (for the methadone and work reinforcement and work reinforcement participants). A pay reset occurred when a participant’s base pay was decreased to $1 per hour due to the reset-only contingency. A sham reset occurred when a participant’s base pay would have been reduced to $1 per hour if the participant had been under the reset-only contingency. Although both reset types involved active drug use and missed urine samples, only the pay reset involved a pay decrease. For each condition, attendance and hours worked before and after a reset were compared using paired t tests. Then, for the abstinence, methadone, and work reinforcement condition, attendance and hours worked at the different base pay rates for participants who transitioned from $1 per hour to $8 per hour were analyzed using repeated measures ANOVA. Bonferroni’s post-hoc tests were used for comparisons between the $8 per hour pay rate (before and after a reset) and the other pay rates ($2 to $7).
RESULTS AND DISCUSSION
There were no significant differences among the abstinence, methadone, and work reinforcement, methadone and work reinforcement, and work reinforcement participants in the overall percentage of days attended (70.4%, 69.6%, and 68.4%, respectively; F = 0.08, p = .92) and hours worked (2.7, 2.9, and 2.8, respectively; F = 2.36, p = .10); however, effects were evident immediately after a pay reset. Figure 1 shows attendance and hours worked the day before and the day after a pay or sham reset. Abstinence, methadone, and work reinforcement participants worked significantly fewer days and hours after a pay reset than they did before the reset. In comparison, methadone and work reinforcement and work reinforcement participants worked a similar number of days and hours before and after a sham reset. This suggests that the pay reset, and not active drug use or missed urine samples, caused the effect on attendance and hours worked.
Figure 1.
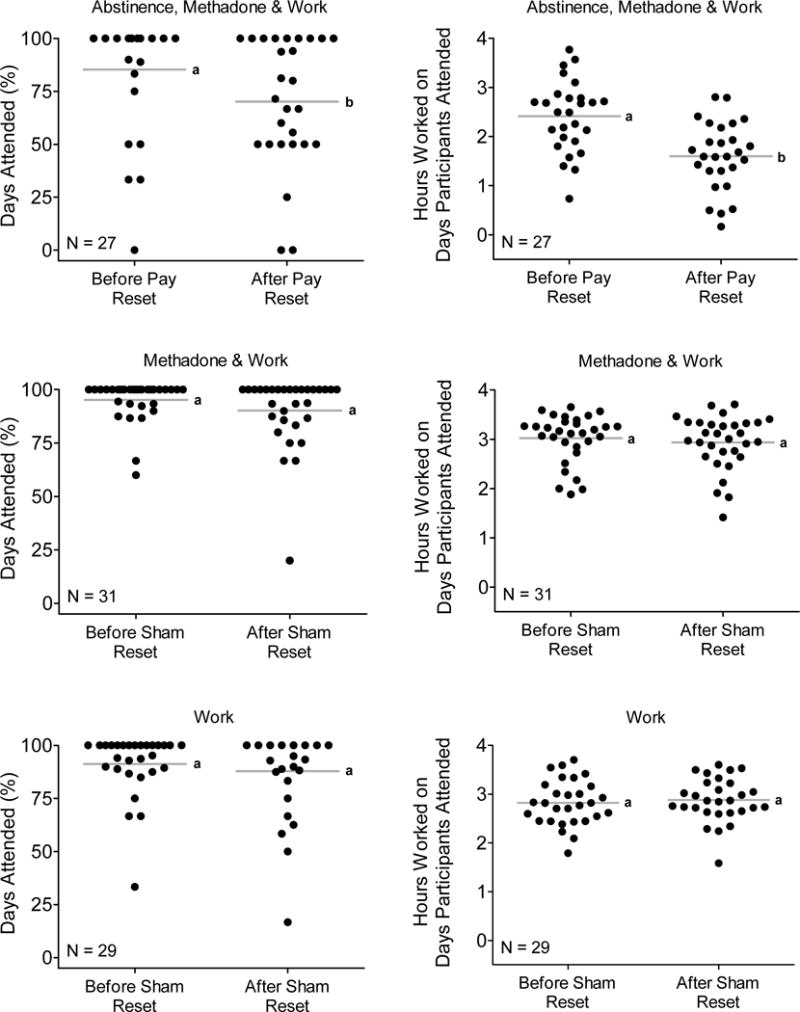
Days attended (left) and hours worked (right) the day before and the day after a pay reset (top panel: abstinence, methadone, and work participants) and a sham reset (middle and bottom panels: methadone and work and work participants, respectively). The pay reset indicates that a participant’s hourly pay was reduced to $1 per hour due to the reset-only contingency. The sham reset indicates that a participant’s hourly pay would have been reduced to $1 per hour if the participant had been under the reset-only contingency. Some of the participants never experienced a reset and were excluded from this analysis. The circles represent individual participants, and the horizontal gray lines indicate the group average. Within each graph, letters shared in common indicate no significant difference.
The decrease in attendance and hours worked immediately after the pay reset was transient. Figure 2 shows attendance and hours worked for participants who experienced a pay reset and then transitioned from $1 per hour to $8 per hour. On days that participants could earn only $1 per hour, they attended less often than when they could earn $8 per hour, both before the pay reset and after transitioning through the pay reset. Participants attended a similar percentage of days when they could earn $2 to $8 per hour. On days that participants earned only $1 per hour, they worked significantly fewer hours than when they earned $8 per hour (before the pay reset). On days that participants earned only $1 to $2 per hour, they worked significantly fewer hours than when they again earned $8 per hour. Overall, after a pay reset, the number of hours participants worked increased as a direct function of the increase in pay and remained at a similar level from $4 to $8 per hour. Hours worked at the $8 per hour pay rate did not differ before and after a pay reset.
Figure 2.
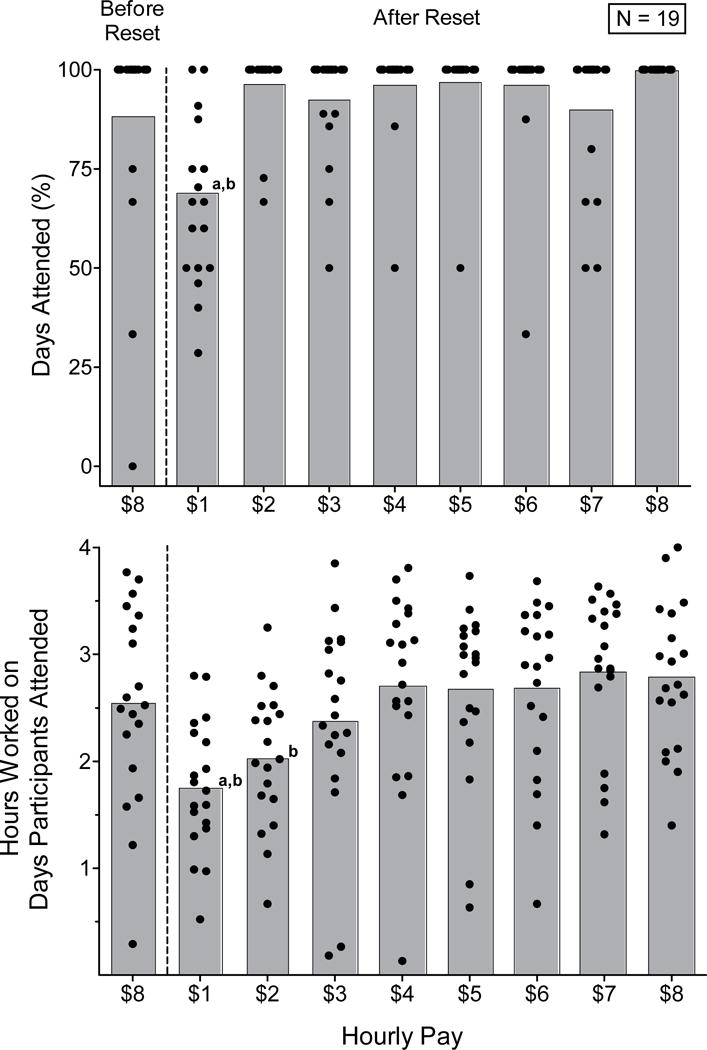
Days attended (top panel) and hours worked (bottom panel) before and after a pay reset for abstinence, methadone, and work participants (n = 19) who transitioned from $1 per hour to $8 per hour. The circles represent individual participants, and the gray bars indicate the average at each hourly pay rate. a = condition was significantly different from the $8 per hour condition before a reset. b = conditions were significantly different from the $8 per hour condition after a reset.
The finding that participants worked less after a pay reset is consistent with basic and clinical research on reinforcement magnitude. Basic research with laboratory animals responding for food (Everly, Holtyn, & Perone, 2014; Perone & Courtney, 1992) and people with intellectual disabilities responding for money (Williams, Saunders, & Perone, 2011) has shown that behavior is often disrupted when a transition occurs from a rich reinforcement context to one that is relatively lean. A similar rich-to-lean transition occurs when pay is reset and may contribute to the transient decrease in workplace participation. Clinical research also has shown low-income drug users to be sensitive to changes in reinforcement magnitude. For example, the effectiveness of abstinence reinforcement interventions is directly related to reinforcement magnitude; as the magnitude of reinforcement increases, the proportion of participants who respond to the intervention increases (Dallery, Silverman, Chutuape, Bigelow, & Stitzer, 2001). In the present study, the proportion of participants who attended the workplace also was directly related to the pay magnitude.
This study did not experimentally compare the suspension-plus-reset contingency to the reset-only contingency. Nevertheless, the drug-abstinence results reported previously (Holtyn et al., 2014a, 2014b) and the present analysis suggest that a temporary pay decrease after drug use may be sufficient to promote drug abstinence without reducing overall workplace participation. Although transient decreases in workplace participation may occur, behavioral effects such as these may be an inherent and important aspect of an effective drug-abstinence contingency. Because these transient effects may provide a measure of the punitive value of the pay reset, a drug-abstinence contingency that does not produce any behavioral side effects may fail to decrease drug use. In sum, the employment-based reinforcement contingency described in the present study could be useful in achieving the goals of the therapeutic workplace to promote drug abstinence, education and job-skills development, and employment in unemployed adults with long histories of drug addiction.
Acknowledgments
This research was supported by Grants R01DA023864, R01DA019497, R01DA037314, and T32DA07209 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
Footnotes
Action Editor, Bethany Raiff
References
- Dallery J, Silverman K, Chutuape MA, Bigelow GE, Stitzer ML. Voucher-based reinforcement of opiate plus cocaine abstinence in treatment-resistant methadone patients: Effects of reinforcer magnitude. Experimental and Clinical Psychopharmacology. 2001;9:317–325. doi: 10.1037/1064-1297.9.3.317. [DOI] [PubMed] [Google Scholar]
- DeFulio A, Donlin WD, Wong CJ, Silverman K. Employment-based abstinence reinforcement as a maintenance intervention for the treatment of cocaine dependence: A randomized controlled trial. Addiction. 2009;104:1530–1538. doi: 10.1111/j.1360-0443.2009.02657.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everly JB, Holtyn AF, Perone M. Behavioral functions of stimuli signaling transitions across rich and lean schedules of reinforcement. Journal of the Experimental Analysis of Behavior. 2014;101:201–214. doi: 10.1002/jeab.74. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Delaney DD, Budney AJ, Bickel WK, Hughes JR, Foerg F, Fenwick JW. A behavioral approach to achieving initial cocaine abstinence. American Journal of Psychiatry. 1991;148:1218–1224. doi: 10.1176/ajp.148.9.1218. [DOI] [PubMed] [Google Scholar]
- Holtyn AF, Koffarnus MN, DeFulio A, Sigurdsson SO, Strain EC, Schwartz RP, Silverman K. Employment-based abstinence reinforcement promotes opiate and cocaine abstinence in out-of-treatment injection drug users. Journal of Applied Behavior Analysis. 2014a;47:681–693. doi: 10.1002/jaba.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtyn AF, Koffarnus MN, DeFulio A, Sigurdsson SO, Strain EC, Schwartz RP, Silverman K. The therapeutic workplace to promote treatment engagement and drug abstinence in out-of-treatment injection drug users: A randomized controlled trial. Preventive Medicine. 2014b;68:62–70. doi: 10.1016/j.ypmed.2014.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perone M, Courtney K. Fixed-ratio pausing: Joint effects of past reinforcer magnitude and stimuli correlated with upcoming magnitude. Journal of the Experimental Analysis of Behavior. 1992;57:33–46. doi: 10.1901/jeab.1992.57-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K. Exploring the limits and utility of operant conditioning in the treatment of drug addiction. The Behavior Analyst. 2004;27:209–230. doi: 10.1007/BF03393181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, DeFulio A, Sigurdsson SO. Maintenance of reinforcement to address the chronic nature of drug addiction. Preventive Medicine. 2012;55:S46–S53. doi: 10.1016/j.ypmed.2012.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, Wong CJ, Needham M, Diemer KN, Knealing T, Crone-Todd D, Kolodner K. A randomized trial of employment-based reinforcement of cocaine abstinence in injection drug users. Journal of Applied Behavior Analysis. 2007;40:387–410. doi: 10.1901/jaba.2007.40-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DC, Saunders KJ, Perone M. Extended pausing by humans on multiple fixed-ratio schedules with varied reinforcer magnitude and response requirements. Journal of the Experimental Analysis of Behavior. 2011;95:203–220. doi: 10.1901/jeab.2011.95-203. [DOI] [PMC free article] [PubMed] [Google Scholar]


