Abstract
Background
Risk stratification is an important goal of cardiac noninvasive tests (NITs), yet little contemporary data exist on the prognostic value of different NITs by patient sex.
Objectives
To compare the results and prognostic information derived from anatomic versus stress testing in stable men and women with suspected coronary artery disease.
Methods
In 8966 PROMISE trial patients tested as randomized (4500 computed tomographic angiography [CTA], 52% female; 4466 stress testing, 53% female), we assessed the relationship between sex and NIT results using logistic regression, and the relationship between sex and a composite of death, myocardial infarction, and unstable angina hospitalization using Cox proportional hazards models.
Results
In women, a positive CTA (≥70% stenosis) was less likely than a positive stress test (8% vs. 12%, adjusted OR 0.67 [95% CI 0.55-0.82]). Compared with negative tests, a positive CTA was more strongly associated with subsequent clinical events than a positive stress test (CTA adjusted HR 5.86 [95% CI 3.32-10.35]; stress adjusted HR 2.27 [95% CI 1.21-4.25]; adjusted p=0.028). Men were more likely to have a positive CTA than stress test (16% vs. 14%, adjusted OR 1.23 [95% CI 1.04-1.47]). Compared with negative tests, a positive CTA was less strongly associated with subsequent clinical events than a positive stress test in men, although this difference was not statistically significant (CTA adjusted HR 2.80 [95% CI 1.76-4.45]; stress adjusted HR 4.42 [95% CI 2.77-7.07]; adjusted p=0.168). Negative CTA and stress tests were equally likely to predict an event in both sexes (adjusted p-values=NS). A significant interaction between sex, NIT type, and test result (p=0.01) suggests that sex and NIT type jointly influence the relationship between test result and clinical events.
Conclusions
The prognostic value of an NIT result varies by test type and patient sex. Women appear to derive more prognostic information from a CTA, while men tend to derive similar prognostic value from both test types.
Keywords: coronary artery disease, gender, risk stratification, noninvasive testing
Two major goals of noninvasive tests (NITs) in patients with chest pain are the diagnosis of obstructive coronary artery disease (CAD) and risk stratification, as both diagnostic and prognostic information are essential to optimally guide subsequent management (1). Careful analyses of diagnostic accuracy have shown different test performances not only by modality but also by patient sex (2). These sex-related differences may be due to reasons as varied as baseline differences in electrocardiography (ECG) characteristics, breast attenuation, smaller coronary vessel size, and the higher prevalence of microvascular coronary dysfunction in women, giving rise to a higher rate of false positive test results in women (2-4).
Given these well-established variations by sex in diagnostic test performance, it is reasonable to postulate that NITs may also provide different prognostic information in women and in men. This in turn may result in differences in the relative value of anatomic versus stress testing for patients of each sex. Although older studies have compared the prognostic value of stress testing within each sex, there are few contemporary data on this issue (5-7). Furthermore, recent observational studies on the prognostic value of computed tomographic angiography (CTA) do not include sex-specific analyses (8,9). A fuller understanding of the prognostic performance of these tests could aid in selecting the diagnostic evaluation strategy for both women and men.
The Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE) randomized 10,003 outpatients with stable symptoms suggestive of CAD to a strategy of either functional or anatomic (CTA) testing (10). Over a median follow-up period of 25 months, there was no difference between testing arms in clinical events overall or by sex. However, the primary analysis did not compare the prognostic capabilities of the 2 types of tests in either women or men. Given the high percentage (53%) of women enrolled in this trial and the randomized selection of test type, it is an ideal setting in which to explore the associations between test results and clinical events in each sex. We hypothesized that the 2 types of NITs, anatomical and stress testing, would have different likelihoods of being positive in women and in men, and that the relationships between a positive test result and a clinical event, compared with those of a negative test result, would be jointly influenced by patient sex and NIT type.
Methods
Study Cohort and Design
The PROMISE trial was a pragmatic comparative effectiveness trial that randomized stable symptomatic patients without known CAD requiring noninvasive testing to either an initial strategy of anatomic (CTA) or stress testing (10,11). For patients in the stress testing arm, the choice of test was left up to the clinician (exercise ECG, stress echocardiography, or stress nuclear). Randomization was stratified by study site and by the stress test type prespecified by the provider.
All tests were performed and interpreted by local physicians who were responsible for all subsequent clinical decisions. We defined a positive CTA to be one that showed obstructive CAD (i.e., ≥70% stenosis in at least one epicardial artery or ≥50% stenosis in the left main). An exercise ECG was considered positive if there were ST-segment changes consistent with ischemia during stress or early termination (<3 minutes) due to reproduction of symptoms, arrhythmia, and/or hypotension. A stress echocardiography or stress nuclear test was considered positive if there was inducible ischemia in at least one coronary territory (anterior, inferior, or lateral), or early termination of exercise stress (<3 minutes) due to ST changes consistent with ischemia, symptom reproduction, arrhythmia, and/or hypotension.
This secondary analysis included those patients who were tested as randomized and who had interpretable results, defined as not missing and not indeterminate. The primary endpoint was the same as that of the overall trial (a composite of death from any cause, myocardial infarction [MI], or unstable angina hospitalization), except that the major procedural complication component was omitted because it was not believed to be related to the prognostic value of the test. A composite of time to cardiovascular death or MI was a secondary outcome.
Statistical Analyses
Baseline characteristics were described using mean ± SD for continuous variables and percentages for categorical variables. Characteristics were compared between patients in each NIT arm by sex using chi-square testing for categorical variables and the Wilcoxon rank sum test for continuous variables.
To determine whether the likelihood of a positive test differed by type of NIT (CTA vs. stress test) in women and in men, we performed multivariable logistic regression analyses. To further determine whether these relationships were independent of risk factors, the model was adjusted by patient age, race, baseline cardiac risk factors (history of hypertension, dyslipidemia, diabetes, tobacco use, family history of premature CAD, absence of regular exercise, CAD equivalent [defined as history of cerebrovascular disease, peripheral arterial disease, and/or diabetes], body mass index), global estimates of cardiovascular disease as derived from the Framingham Risk Score (12), the ASCVD Pooled Cohort Risk Score (13), and the updated Diamond and Forrester Risk Score (14), typicality of chest pain, and physician's estimation of the likelihood of significant CAD. A 2-way interaction between type of NIT and sex was included to determine whether the relationship between NIT type and test positivity was modified by patient sex.
To assess the prognostic value of each type of NIT for women and for men, multivariable Cox regression models were used to examine the relationship between test result, test type, patient sex, and both the primary composite outcome and the secondary outcome of time to cardiovascular death or MI. This model included a 3-way interaction between patient sex, test type, and test result to determine whether the relationships between test result and outcomes were modified jointly by sex and NIT type. Because the comparison of interest (patients with positive test results vs. patients with negative test results) was a nonrandomized comparison, we computed direct adjusted event curves to control for possible confounders of the relationship between test result and the primary composite outcome (14). The event curves and the above Cox regression models were adjusted for the same clinical factors as in the test positivity analysis. To further investigate how negative test results affect the prognostic value of each type of NIT, Cox regression models were developed to examine the relationship between NIT type and the primary composite outcome in women and in men with a negative test result.
All statistical calculations were carried out using SAS version 9.4 (SAS Institute, Cary, North Carolina).
Results
Baseline Characteristics
Among the 8966 PROMISE patients who received the NIT type to which they were randomized and had interpretable results, CTA was performed in 4500 (52% female) and stress testing in 4466 (53% female; Online Figure 1). Although randomization was not stratified by sex, the characteristics of women in the 2 testing arms were relatively similar, as were those of men (Table 1).
Table 1.
Baseline Characteristics of Women and Men by Randomization Group
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| All Women (N=4720) | CTA (N=2332) | Stress Test (N=2388) | P-value | All Men (N=4246) | CTA (N=2168) | Stress Test (N=2078) | P-value | |
| Demographics | ||||||||
| Age, mean (SD), yrs | 62.4 (7.8) | 62.2 (7.7) | 62.6 (7.9) | 0.07 | 58.9 (8.3) | 58.6 (8.2) | 59.2 (8.4) | 0.008 |
| Age ≥65 y | 1627 (34.5%) | 780 (33.4%) | 847 (35.5%) | 0.14 | 961 (22.6%) | 471 (21.7%) | 490 (23.6%) | 0.15 |
| Racial or ethnic minority | 1052 (22.4%) | 547 (23.6%) | 505 (21.3%) | 0.06 | 913 (21.6%) | 471 (21.9%) | 442 (21.4%) | 0.70 |
| Cardiac risk factors | ||||||||
| Hypertension | 3137 (66.5%) | 1534 (65.8%) | 1603 (67.1%) | 0.33 | 2673 (63.0%) | 1359 (62.7%) | 1314 (63.2%) | 0.71 |
| Diabetes | 1025 (21.7%) | 500 (21.4%) | 525 (22.0%) | 0.65 | 883 (20.8%) | 436 (20.1%) | 447 (21.5%) | 0.26 |
| Metabolic syndrome | 1761 (37.3%) | 857 (36.7%) | 904 (37.9%) | 0.43 | 1626 (38.3%) | 816 (37.6%) | 810 (39.0%) | 0.37 |
| Dyslipidemia | 3258 (69.0%) | 1621 (69.5%) | 1637 (68.6%) | 0.48 | 2812 (66.2%) | 1408 (64.9%) | 1404 (67.6%) | 0.07 |
| Cerebrovascular disease | 220 (4.7%) | 103 (4.4%) | 117 (4.9%) | 0.43 | 140 (3.3%) | 71 (3.3%) | 69 (3.3%) | 0.93 |
| Peripheral artery disease | 86 (1.8%) | 42 (1.8%) | 44 (1.8%) | 0.92 | 75 (1.8%) | 32 (1.5%) | 43 (2.1%) | 0.14 |
| History of heart failure | 186 (3.9%) | 90 (3.9%) | 96 (4.0%) | 0.77 | 150 (3.5%) | 73 (3.4%) | 77 (3.7%) | 0.55 |
| Current or former smoker | 2162 (45.8%) | 1068 (45.8%) | 1094 (45.8%) | 0.70 | 2420 (57.0%) | 1224 (56.5%) | 1196 (57.6%) | 0.02 |
| Family history of premature CAD | 1602 (34.1%) | 815 (35.1%) | 787 (33.1%) | 0.15 | 1237 (29.2%) | 645 (29.9%) | 592 (28.6%) | 0.35 |
| History of depression | 1226 (26.0%) | 599 (25.7%) | 627 (26.3%) | 0.65 | 625 (14.7%) | 286 (13.2%) | 339 (16.3%) | 0.004 |
| Participate in physical activity | 2215 (47.0%) | 1101 (47.3%) | 1114 (46.7%) | 0.70 | 2393 (56.5%) | 1211 (56.0%) | 1182 (57.0%) | 0.51 |
| BMI (kg/m2) | 30.4 (6.5) | 30.4 (6.4) | 30.4 (6.6) | 0.93 | 30.5 (5.4) | 30.4 (5.4) | 30.5 (5.4) | 0.36 |
| Cardiac risk scores, mean (SD) | ||||||||
| Framingham risk score | 15.0 (9.9) | 14.7 (9.5) | 15.3 (10.2) | 0.17 | 28.7 (16.3) | 28.2 (16.2) | 29.2 (16.3) | 0.02 |
| ASCVD Pooled Cohort Risk prediction | 12.5 (11.4) | 12.1 (10.9) | 12.9 (11.8) | 0.06 | 16.9 (11.5) | 16.5 (11.4) | 17.3 (11.5) | 0.01 |
| Diamond and Forrester (2011) | 28.4 (12.3) | 28.1 (12.1) | 28.6 (12.5) | 0.29 | 60.3 (17.5) | 60.0 (17.7) | 60.5 (17.2) | 0.13 |
| Presenting symptoms | ||||||||
| Chest pain | 3455 (73.2%) | 1744 (74.8%) | 1711 (71.7%) | 0.02 | 3067 (72.3%) | 1578 (72.9%) | 1489 (71.7%) | 0.40 |
| Aching/dull | 808 (23.4%) | 418 (24.0%) | 390 (22.8%) | 0.42 | 847 (27.6%) | 424 (26.9%) | 423 (28.4%) | 0.34 |
| Crushing/pressure/squeezing/tightness | 1832 (53.0%) | 921 (52.8%) | 911 (53.2%) | 0.80 | 1413 (46.1%) | 754 (47.8%) | 659 (44.3%) | 0.05 |
| Provider characterization of chest pain | 0.88 | 0.72 | ||||||
| Typical | 526 (11.1%) | 261 (11.2%) | 265 (11.1%) | 501 (11.8%) | 260 (12.0%) | 241 (11.6%) | ||
| Atypical | 3671 (77.8%) | 1818 (78.0%) | 1853 (77.6%) | 3317 (78.1%) | 1683 (77.6%) | 1634 (78.6%) | ||
| Physical exam, mean (SD) | ||||||||
| Systolic BP (mmHg) | 131.0 (17.1) | 130.8 (16.8) | 131.1 (17.4) | 0.76 | 131.6 (15.9) | 131.4 (16.1) | 131.8 (15.8) | 0.32 |
| Diastolic BP (mmHg) | 77.6 (10.2) | 77.4 (10.1) | 77.7 (10.3) | 0.21 | 80.1 (10.2) | 80.2 (10.2) | 80.1 (10.2) | 0.83 |
Data are n (%) unless otherwise indicated.
BMI = body mass index; BP = blood pressure; CAD = coronary artery disease; CTA = computed tomographic angiography.
Effect of Sex and Test Type on Test Result
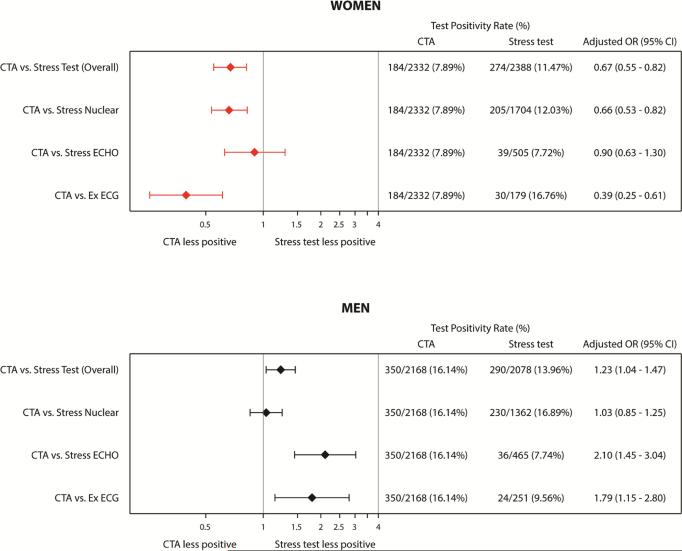
There were 456 women (9.7% of 4720 women total) who had a positive test result, with a significantly smaller proportion of positive CTAs compared to positive stress tests (8% vs. 12%, p<0.001; Table 2). The significance of this difference persisted after adjustment for clinical factors, with women being less likely to have a positive CTA than a positive stress test (adjusted OR 0.67 [95% CI 0.55-0.82]; p<0.001; Table 3). Specifically, CTA was less likely to be positive compared to exercise ECG (OR 0.39 [95% CI 0.25-0.61]; p<0.001) and nuclear stress testing (OR 0.66 [95% CI 0.53-0.82]; p<0.001), but not compared to stress echocardiography (OR 0.90 [95% CI 0.63-1.30]; p=0.58; Figure 1).
Table 2.
Test Results and Event Rates by Sex and Test Type
| Women (N=4720) | Men (N=4246) | |||||
|---|---|---|---|---|---|---|
| CTA (N=2332) | Stress (N=2388) | P-value | CTA (N=2168) | Stress (N=2078) | P-value | |
| Positive Test Result | 184/2332 (7.9%) | 274/2388 (11.5%) | <.001 | 350/2168 (16.1%) | 290/2078 (14.0%) | 0.046 |
| Multi vessel disease/Ischemia | 78/184 (42.4%) | 190/274 (69.3%) | 188/350 (53.7%) | 165/290 (56.9%) | ||
| Single vessel disease/Ischemia | 106/184 (57.6%) | 84/274 (30.7%) | 162/350 (46.3%) | 125/290 (43.1%) | ||
| Negative Test Result | 2148/2332 (92.1%) | 2114/2388 (88.5%) | <.001 | 1818/2168 (83.9%) | 1788/2078 (86.0%) | 0.046 |
| Nonbstructive CAD/Abnormal ECG with normal imaging or scar without ischemia | 1185/2148 (55.2%) | 197/2114 (9.3%) | 1276/1818 (70.2%) | 226/1788 (12.6%) | ||
| Normal anatomy/no abnormalities | 963/2148 (44.8%) | 1917/2114 (90.7%) | 542/1818 (29.8%) | 1562/1788 (87.4%) | ||
| Revascularization within 90 days | 82/2332 (3.5%) | 45/2388 (1.9%) | <.001 | 191/2168 (8.8%) | 102/2078 (4.9%) | <.001 |
| Primary Composite Endpoint: Time to Death/MI/UAH (%) | 57/2332 (2.4%) | 55/2388 (2.3%) | 0.750 | 80/2168 (3.7%) | 73/2078 (3.5%) | 0.757 |
| Individual Components (%) | 0.007 | 0.778 | ||||
| All Cause Death | 28/57 (49.1%) | 29/55 (52.7%) | 34/80 (42.5%) | 34/73 (46.6%) | ||
| MI | 5/57 (8.8%) | 15/55 (27.3%) | 19/80 (23.8%) | 14/73 (19.2%) | ||
| UAH | 24/57 (42.1%) | 11/55 (20.0%) | 27/80 (33.8%) | 25/73 (34.2%) | ||
| Secondary Composite Endpoint: Time to CV Death/MI (%) | 21/2332 (0.9%) | 35/2388 (1.5%) | 0.073 | 39/2168 (1.8%) | 35/2078 (1.7%) | 0.775 |
| Individual Components (%) | 0.203 | 0.331 | ||||
| CV Death | 15/21 (71.4%) | 19/35 (54.3%) | 19/39 (48.7%) | 21/35 (60.0%) | ||
| MI | 6/21 (28.6%) | 16/35 (45.7%) | 20/39 (51.3%) | 14/35 (40.0%) | ||
CV = cardiovascular; MI = myocardial infarction; UAH = Hospitalization for unstable angina.
Table 3.
Association Between Noninvasive Test Type and Positive Test Results in Women and in Men
| Positive Test Rate, No. of Positive Tests/Sample Size (%) | CTA versus Stress Test Unadjusted* | CTA versus Stress Test Adjusted† | ||||
|---|---|---|---|---|---|---|
| Model/Comparison | CTA | Stress Test | Odds Ratio (95% CI) | P-value | Odds Ratio (95% CI) | P-value |
| Interaction between randomized arm and sex | --- | < 0.001 | --- | < 0.001 | ||
| CTA versus stress test in women | 184/2332 (7.89%) | 274/2388 (11.47%) | 0.66 (0.54 - 0.80) | < 0.001 | 0.67 (0.55 - 0.82) | < 0.001 |
| CTA versus stress test in men | 350/2168 (16.14%) | 290/2078 (13.96%) | 1.19 (1.00 - 1.41) | 0.047 | 1.23 (1.04 - 1.47) | 0.019 |
Unadjusted models contained sex, randomized testing arm, and interaction term.
Adjusted for age, race, body mass index, coronary artery disease (CAD) equivalent, Framingham risk score (12), ASCVD (13), Diamond and Forrester (14), hypertension, dyslipidemia, diabetes, family history of premature CAD, sedentary lifestyle, smoking, typicality of chest pain, and physician's estimation of likelihood of significant CAD.
CTA = computed tomographic angiography; NIT = noninvasive test.
Figure 1. Adjusted Association Between Noninvasive Test Type and Test Results in Women and Men Tested as Randomized.
Adjusted for age, race, body mass index, coronary artery disease (CAD) equivalent, Framingham risk score (12), ASCVD score (13), 2011 Diamond and Forrester score (14), hypertension, dyslipidemia, diabetes, family history of premature CAD, sedentary lifestyle, smoking, typicality of chest pain, and physician's estimation of likelihood of significant CAD. CTA = computed tomographic angiography; ECG = electrocardiography.
In contrast, 640 men (15.1% of 4246 men total) had a positive test, with a marginally greater proportion of CTAs being positive compared to stress tests (16% vs. 14%, p=0.047; Table 2). After adjustment for clinical factors, men were more likely to have a positive CTA than a positive stress test (adjusted OR 1.23 [95% CI 1.04-1.47]; p=0.019) (Table 3). Specifically in men, CTA was more likely to be positive compared to exercise ECG (OR 1.79 [95% CI 1.15-2.80]; p=0.01) and stress echocardiography (OR 2.10 [95% CI 1.45-3.04]; p<0.001), but not compared to nuclear stress testing (OR 1.03 [95% CI 0.85-1.25]; p=0.75; Figure 1). The likelihood of a positive test was strongly influenced by patient sex such that the effect of test type on test result was different for women compared with men (interaction p<0.001).
Effect of Sex and Test Type on the Prognostic Value of Noninvasive Testing
During the median 25 months of study follow-up, 112 women (2.4%; 57 in CTA arm, 55 in stress test arm) and 153 men (3.6%; 80 in CTA arm, 73 in stress test arm) had a primary endpoint event (Table 2). Overall, a positive NIT was strongly predictive of the composite endpoint of all-cause death/MI/hospitalization for unstable angina compared with a negative NIT (HR 3.37 [95% CI 2.59-4.38]). An analysis of the interaction between sex, NIT type, and test result revealed that sex and NIT type jointly modified the association of test result (positive vs. negative) with the risk of experiencing the primary composite endpoint (adjusted interaction p=0.010; Table 4). Thus, the influence of test type on the relationship between test result and outcome was different for women compared with men.
Table 4.
Association between NIT Result and the Primary Composite Outcome by Sex and NIT Type
| Event Rate No. of Events/Sample Size (%) | Positive vs. Negative Unadjusted* | Positive vs. Negative Adjusted† | ||||
|---|---|---|---|---|---|---|
| Sex/NIT Type | Positive Test | Negative Test | Hazard Ratio (95% CI) | P-value | Hazard Ratio (95% CI) | P-value |
| Interaction between test result, test type, and sex | --- | 0.020 | --- | 0.010 | ||
| Women | ||||||
| Association of test positivity in women randomized to CTA | 18/184 (9.78%) | 39/2148 (1.82%) | 6.39 (3.65-11.17) | <0.001 | 5.86 (3.32-10.35) | <0.001 |
| Association of test positivity in women randomized to stress test | 14/274 (5.11%) | 41/2114 (1.94%) | 2.70 (1.45-5.03) | 0.002 | 2.27 (1.21-4.25) | 0.011 |
| Difference between the association in CTA and the association in stress test | --- | 0.043 | --- | 0.028 | ||
| Men | ||||||
| Association of test positivity in men randomized to CTA | 31/350 (8.86%) | 49/1818 (2.70%) | 3.69 (2.35-5.79) | <0.001 | 2.80 (1.76-4.45) | <0.001 |
| Association of test positivity in men randomized to stress test | 33/290 (11.38%) | 40/1788 (2.24%) | 5.39 (3.39-8.56) | <0.001 | 4.42 (2.77-7.07) | <0.001 |
| Difference between the association in CTA and the association in stress test | --- | 0.249 | --- | 0.168 | ||
CTA = computed tomographic angiography; NIT = noninvasive test.
Unadjusted models contained test result, randomized testing arm, sex, and all 2-way and 3-way interaction terms.
Adjusted for age, race, body mass index, coronary artery disease (CAD) equivalent, Framingham risk score (12), ASCVD score (13), 2011 Diamond and Forrester score (14), hypertension, dyslipidemia, diabetes, family history of premature CAD, sedentary lifestyle, smoking, typicality of chest pain, and physician's estimation of likelihood of significant CAD.
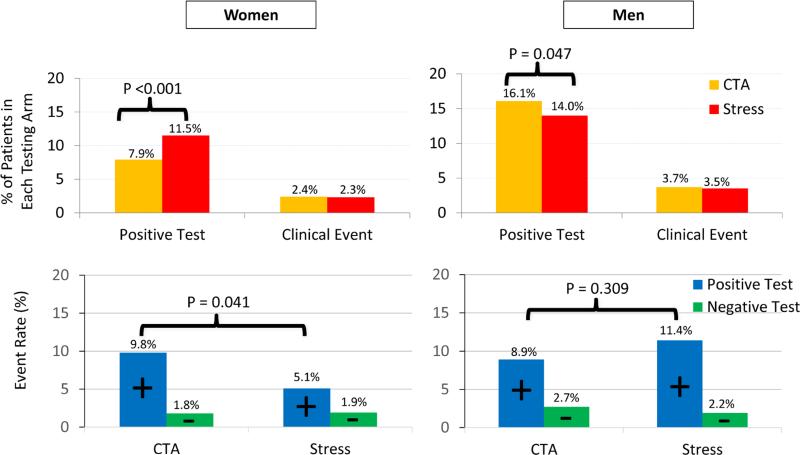
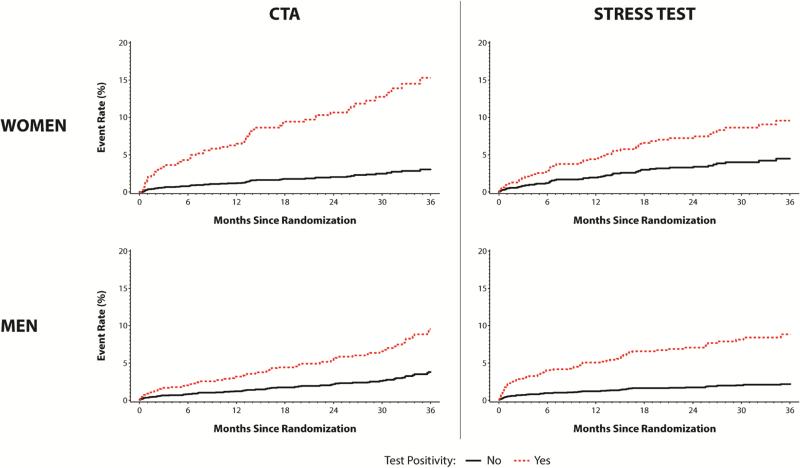
In women, the association of test results (positive vs. negative) with clinical events in CTA was stronger than the association of test results with clinical events in stress tests (unadjusted HR 6.39 [95% CI 3.65-11.17] vs. 2.70 [95% CI 1.45-5.03]; Table 4, Figure 2). This relationship persisted after adjustment for clinical factors, with a more than 2-fold greater hazard ratio for the association of test results to clinical events in CTA compared with the association of test results to clinical events in stress tests (adjusted HR 5.86 [95% CI 3.32-10.35] vs. 2.27 [95% CI 1.21-4.25]; adjusted p=0.028; Table 4, Figure 3). In contrast, in men the association of test results to clinical events in CTA was weaker than the association of test results to clinical events in stress tests (unadjusted HR 3.69 [95% CI 2.35-5.79] vs. 5.39 [95% CI 3.39-8.56]) (Table 4, Figure 2). This relationship persisted after adjustment for clinical factors, although the difference in adjusted hazard ratios did not reach statistical significance (adjusted HR 2.80 [95% CI 1.76-4.45] vs. 4.42 [95% CI 2.77-7.07]); adjusted p=0.168 (Table 4, Figure 3). There was no difference in the ability of a negative CTA and a negative stress test to predict clinical events in either women or men (adjusted HR of negative CTA vs. negative stress test in women = 0.89 [95% CI 0.57-1.38]; adjusted HR of negative CTA vs. negative stress test in men = 1.13 [95% CI 0.75-1.72]; all adjusted p-values = NS; Figure 2). In both sexes, event rates were too low to meaningfully compare prognostic value across the different modalities of stress tests. There was no interaction between patient sex, NIT type, and the relationship between a positive test and the secondary outcome of cardiovascular death or MI (unadjusted p=0.77).
Figure 2. Comparison of Test Results and Clinical Event Rates by Test Type in Women and Men.
Clinical event rates are the primary composite outcome consisting of all-cause death, myocardial infarction, or unstable angina hospitalization. The top 2 panels compare positive test rates and event rates by sex in patients undergoing CTA vs. stress testing. In women event rates are similar in the 2 arms, but test positivity rates are higher in the stress test arm. In men event rates are also similar in the 2 arms, but test positivity rates are higher in the CTA arm. The bottom 2 panels compare event rates by positive and negative test results for each sex and by test type. Within women, the event rate with a negative CTA was similar to that with a negative stress test, but the event rate with a positive CTA was higher than that with a positive stress test. Within men, the event rate with a negative CTA was similar to that with a negative stress test, as was the event rate with a positive CTA and a positive stress test.
Figure 3. Adjusted Event Curves of the Primary Composite Outcome Comparing Positive Versus Negative Test Results by Sex and Test Type.
Event curves are shown comparing the association of positive and negative test results for each sex and by test type with the primary composite outcome of all-cause death, myocardial infarction, or unstable angina hospitalization. Curve are adjusted for age, race, body mass index, coronary artery disease (CAD) equivalent, Framingham risk score (12), ASCVD score (13), 2011 Diamond and Forrester score (14), hypertension, dyslipidemia, diabetes, family history of premature CAD, sedentary lifestyle, smoking, typicality of chest pain, and physician's estimation of likelihood of significant CAD . Interaction p = 0.010. CTA = computed tomographic angiography.
Discussion
Risk stratification is one of the primary reasons to perform noninvasive testing in patients with suspected CAD and provides important supplemental information beyond diagnosis. The current analysis suggests that women may derive greater prognostic information from a CTA, while men appear to derive similar prognostic value from a CTA and stress test. In both sexes, a negative CTA and a negative stress test appear to confer a similar likelihood of a clinical event. The durability of our findings after adjustment and the significance of the interaction terms suggest that our findings are unlikely to be due to either clinical characteristics or chance alone.
This analysis was performed in the context of the parent PROMISE trial, which found no difference in clinical events in patients randomized to the CTA versus stress testing arms overall or by sex (10). The significant interaction terms in our analyses suggest, however, that the rate of test positivity and the prognostic value of a test depend on the type of test performed and the patient's sex. Thus, although there was no difference in outcomes between the testing arms, which aggregated patients with both positive and negative test results, women with a positive CTA tended to fare worse than women with a positive stress test. Interestingly, although men randomized to the 2 testing arms had similar outcomes in the primary trial, men with a positive stress test had more clinical events than men with a positive CTA, although this difference did not reach statistical significance.
This apparent discrepancy between the nonsignificant role of sex and test type in the clinical outcomes of the overall trial and the highly significant role of sex and test type in the prognostic value of each type of test may be approached in 3 ways. First, there are many steps in the clinical pathway of a patient between the result of their diagnostic NIT and their ultimate outcome. This is especially relevant in a pragmatic, comparative effectiveness trial such as PROMISE, which did not control whether patients were referred for angiography, revascularized, prescribed appropriate pharmacological therapy, adherent to medications, able to access follow-up care, and so on. A number of care patterns could have occurred differentially by testing arm and by sex, resulting in similar clinical events despite different capabilities of the test types to predict events in women and in men.
Second, during the trial, the providers were unaware of the possible sex-based differences in prognostic value of diagnostic testing that we have demonstrated in this secondary analysis. Thus, they were not able to act on this information to influence future outcomes.
Third, it is important to note that in a setting such as PROMISE, in which event rates were similar in both testing arms in women and in men, the prognostic value of a test is at least partially determined by the number of positive tests. Thus the observed sex-based differences in prognostic capability may be related to a higher positive rate of stress testing compared with CTA in women. In the absence of angiographic data confirming or excluding obstructive CAD in the vast majority of our patients, it is impossible to determine whether these ‘excess’ positive tests represented disease that was not associated with events during trial follow-up, or if they were false positive tests.
The known performance characteristics of the various NITs may help explain the differences in test positivity rates that we observed between women and men. Women were less likely to have a positive CTA than a positive exercise ECG or nuclear stress test, even after adjustment for clinical factors. These findings suggest that some stress test results may be falsely positive. This would be consistent with the well-documented significant false positive rates of exercise ECG and nuclear stress testing in women (2,3). The reported high false positive rate of approximately 28% in nuclear stress testing in women without known CAD (2) is particularly relevant to our study, since the majority of patients in the functional arm received this type of test. Another reason for the higher positivity rate of stress testing in women may be the presence of ischemia in the absence of obstructive CAD, possibly due to microvascular coronary dysfunction (MCD) (16-18). The ability of stress tests to detect both obstructive and microvascular disease may have made them more likely to be positive than CTAs in women, and less likely to be associated with clinical events, since MCD has a lower event rate than obstructive disease (19). These results parallel recent data from the Rule-Out Myocardial Ischemia/Infarction by Computer-assisted Tomography (ROMICAT-II) trial, which noted greater improvement in acute chest pain care in women compared with men randomized to a CTA strategy versus usual care (20).
In contrast to the results seen in women, men in our study were less likely to have a positive stress test than a positive CTA. Multiple factors may contribute to this difference between the sexes, including the lower false positive rate of stress testing and the lower prevalence of MCD in men (3,21). The lower rate of stress test positivity compared to CTA positivity in men may be related to the known discordance between obstructive CAD and ischemia, in which only a subset of obstructive lesions show hemodynamic significance. In the Fractional Flow Reserve Versus Angiography for Multivessel Evaluation (FAME) study, which had mostly (75%) male participants, only 35% of the lesions categorized as having 50%-70% stenosis were functionally significant by fractional flow reserve (22). Although the association of CTA test results with clinical events was not significantly different from that of stress test results in men, the relationship clearly trended toward a stronger association between stress test result and clinical events. Perhaps the ability of stress tests to detect only hemodynamically significant lesions allows identification of the group of men who are most likely to have events, but with the low overall event rate, we did not have enough statistical power to detect this difference.
Our study has several strengths. PROMISE is the first, large head-to-head comparative effectiveness randomized trial of the anatomic versus stress testing strategies in stable symptomatic outpatients with adjudicated clinical events, and is therefore the first dataset that is able to rigorously address which testing strategy confers the greatest prognostic value. The trial is uniquely able to address this clinical question in women, since to our knowledge it includes the largest number of stable symptomatic women of any prospective trial of diagnostic testing to date. Our analyses harness these 2 strengths of PROMISE by focusing on within-sex differences between the 2 randomized testing groups, rather than on between-sex differences alone. Further, our sex-specific analyses provide clinically relevant information that may help to optimize testing choice in all patients, while capitalizing on the randomization between testing strategies in PROMISE.
Our study also has several caveats that should be considered when interpreting the results. Randomization was not stratified by patient sex; however, within each sex, the 2 testing arms were similar. Because less than 10% of the trial population underwent coronary angiography, we are not able to draw conclusions about the diagnostic accuracy of each testing type between sexes. Although patients were followed for a median of >2 years, there were relatively few clinical endpoint events, limiting the ability to assess prognosis by NIT type in each sex. Finally, it is unclear whether our findings would be affected by a different mix of noninvasive testing. However, this distribution of test types reflects current community practice, as PROMISE was a pragmatic trial that left the choice of stress test type and the subsequent clinical management up to the provider.
Conclusions
The choice of noninvasive test is a complex one and depends on many factors in addition to diagnostic test performance, such as local expertise and availability, prior testing data, body habitus, ability to exercise, radiation exposure, and suspicion for cardiac abnormalities other than, or in addition to, ischemia. Our data provide novel insights into the differences between stress testing and anatomic testing in men and women with respect to positivity rates and the prognostic information provided by each type of test, despite the presence of similar overall event rates with both tests. The prognostic value of a positive compared with a negative noninvasive test result varies by test type and patient sex, while the event rate associated with a negative test is similar within each sex regardless of test type. Women appear to derive more prognostic information from CTA, while men appear to derive similar prognostic value from both types of tests. Further research is necessary to determine whether these findings should guide test selection and result interpretation for patients being evaluated for suspected CAD.
Supplementary Material
Acknowledgments
Funding
This project was supported by grants R01HL098237, R01HL098236, R01HL98305, and R01HL098235 from the National Heart, Lung, and Blood Institute (NHLBI). The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents. This paper does not necessarily represent the official views of NHLBI.
Abbreviations
- CAD
coronary artery disease
- CTA
computed tomographic angiography
- ECG
electrocardiography
- MCD
microvascular coronary dysfunction
- NITs
noninvasive tests
- PROMISE
Prospective Multicenter Imaging Study for Evaluation of Chest Pain
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
DBM reported receiving personal fees from Medtronic, CardioDx, and St. Jude Medical and grant support from Eli Lilly, Bristol-Myers Squibb, Gilead Sciences, AGA Medical, Merck, Oxygen Biotherapeutics, and AstraZeneca; UH reported receiving grant support from Siemens Healthcare and HeartFlow; PSD reported receiving grant support from HeartFlow and serves on a data and safety monitoring board for GE Healthcare. No other author reported disclosures.
References
- 1.Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;60:e44–164. doi: 10.1016/j.jacc.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 2.Dolor RJ PM, Melloni C, Chatterjee R, et al. Comparative Effectiveness Review No. 58. (Prepared by the Duke Evidence-based Practice Center under Contract No. 290-2007-10066-I.) Agency for Healthcare Research and Quality; Rockville, MD: 2012. Noninvasive Technologies for the Diagnosis of Coronary Artery Disease in Women. [Google Scholar]
- 3.Shaw LJ, Bairey Merz CN, Pepine CJ, et al. Insights from the NHLBI-Sponsored Women's Ischemia Syndrome Evaluation (WISE) Study: Part I: gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. J Am Coll Cardiol. 2006;47(3 Suppl):S4–20. doi: 10.1016/j.jacc.2005.01.072. [DOI] [PubMed] [Google Scholar]
- 4.Dewey M, Rutsch W, Hamm B. Is there a gender difference in noninvasive coronary imaging? Multislice computed tomography for noninvasive detection of coronary stenoses. BMC Cardiovasc Disord. 2008;8:2. doi: 10.1186/1471-2261-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller TD, Roger VL, Hodge DO, Hopfenspirger MR, Bailey KR, Gibbons RJ. Gender differences and temporal trends in clinical characteristics, stress test results and use of invasive procedures in patients undergoing evaluation for coronary artery disease. J Am Coll Cardiol. 2001;38:690–7. doi: 10.1016/s0735-1097(01)01413-9. [DOI] [PubMed] [Google Scholar]
- 6.Mieres JH, Gulati M, Bairey Merz N, et al. Role of noninvasive testing in the clinical evaluation of women with suspected ischemic heart disease: a consensus statement from the American Heart Association. Circulation. 2014;130:350–79. doi: 10.1161/CIR.0000000000000061. [DOI] [PubMed] [Google Scholar]
- 7.Arruda-Olson AM, Juracan EM, Mahoney DW, McCully RB, Roger VL, Pellikka PA. Prognostic value of exercise echocardiography in 5,798 patients: is there a gender difference? J Am Coll Cardiol. 2002;39:625–31. doi: 10.1016/s0735-1097(01)01801-0. [DOI] [PubMed] [Google Scholar]
- 8.Hadamitzky M, Täubert S, Deseive S, et al. Prognostic value of coronary computed tomography angiography during 5 years of follow-up in patients with suspected coronary artery disease. Eur Heart J. 2013;34:3277–85. doi: 10.1093/eurheartj/eht293. [DOI] [PubMed] [Google Scholar]
- 9.Bamberg F, Sommer WH, Hoffmann V, et al. Meta-analysis and systematic review of the long-term predictive value of assessment of coronary atherosclerosis by contrast-enhanced coronary computed tomography angiography. J Am Coll Cardiol. 2011;57:2426–36. doi: 10.1016/j.jacc.2010.12.043. [DOI] [PubMed] [Google Scholar]
- 10.Douglas PS, Hoffmann U, Patel MR, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. 2015;372:1291–300. doi: 10.1056/NEJMoa1415516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Douglas PS, Hoffmann U, Lee KL, et al. PROspective Multicenter Imaging Study for Evaluation of chest pain: rationale and design of the PROMISE trial. Am Heart J. 2014;167:796–803. e1. doi: 10.1016/j.ahj.2014.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.D'Agostino RB, Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–53. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 13.Goff DC, Jr., Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 Suppl 2):S49–73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- 14.Genders TS, Steyerberg EW, Alkadhi H, et al. A clinical prediction rule for the diagnosis of coronary artery disease: validation, updating, and extension. Eur Heart J. 2011;32:1316–30. doi: 10.1093/eurheartj/ehr014. [DOI] [PubMed] [Google Scholar]
- 15.Zhang X, Loberiza FR, Klein JP, Zhang MJ. A SAS macro for estimation of direct adjusted survival curves based on a stratified Cox regression model. Comput Meth Programs Biomed. 2007;88:95–101. doi: 10.1016/j.cmpb.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Kuruvilla S, Kramer CM. Coronary microvascular dysfunction in women: an overview of diagnostic strategies. Expert Rev Cardiovasc Ther. 2013;11:1515–25. doi: 10.1586/14779072.2013.833854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaski JC, Rosano GM, Collins P, Nihoyannopoulos P, Maseri A, Poole-Wilson PA. Cardiac syndrome X: clinical characteristics and left ventricular function. Long-term follow-up study. J Am Coll Cardiol. 1995;25:807–14. doi: 10.1016/0735-1097(94)00507-M. [DOI] [PubMed] [Google Scholar]
- 18.Jones E, Eteiba W, Merz NB. Cardiac syndrome X and microvascular coronary dysfunction. Trends Cardiovasc Med. 2012;22:161–8. doi: 10.1016/j.tcm.2012.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharaf B, Wood T, Shaw L, et al. Adverse outcomes among women presenting with signs and symptoms of ischemia and no obstructive coronary artery disease: findings from the National Heart, Lung, and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation (WISE) angiographic core laboratory. Am Heart J. 2013;166:134–41. doi: 10.1016/j.ahj.2013.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Truong QA, Hayden D, Woodard PK, et al. Sex differences in the effectiveness of early coronary computed tomographic angiography compared with standard emergency department evaluation for acute chest pain: the Rule-Out Myocardial Infarction with Computer-Assisted Tomography (ROMICAT)-II Trial. Circulation. 2013;127:2494–502. doi: 10.1161/CIRCULATIONAHA.113.001736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaski JC, Rosano GM, Collins P, Nihoyannopoulos P, Maseri A, Poole-Wilson PA. Cardiac syndrome X: clinical characteristics and left ventricular function. Long-term follow-up study. J Am Coll Cardiol. 1995;25:807–14. doi: 10.1016/0735-1097(94)00507-M. [DOI] [PubMed] [Google Scholar]
- 22.Tonino PA, Fearon WF, De Bruyne B, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study: Fractional Flow Reserve Versus Angiography in Multivessel Evaluation. J Am Coll Cardiol. 2010;55:2816–21. doi: 10.1016/j.jacc.2009.11.096. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.