Abstract
Background
Mechanical thrombectomy (MT) using stent-retrievers has been proven to be a safe and effective treatment in acute ischemic stroke (AIS), particularly in large vessel occlusion. Other than patient characteristics, time to recanalization is the most important factor linked to outcome. MT is usually performed in a dedicated angiography suite using a floor- and/or ceiling-mounted biplane angiographic system. Here we report our first experience of MT with a new combined CT and mobile C-arm X-ray device setup.
Methods
Patients with AIS underwent stroke imaging (non-contrast enhanced CT, CT perfusion, and CT angiography) using a commercially available 64-slice CT scanner which was modified for combined use with a C-arm system. In patients with large vessel occlusion, MT was conducted without further patient transfer within the CT imaging suite using a mobile C-arm X-ray device equipped with a 30×30 cm (12×12 inch), 1.5×1.5 k full-view flat detector which was positioned between the gantry and patient table. The safety and feasibility of this new system was assessed in preliminary patients.
Results
Angiographic imaging quality of the mobile C-arm was feasible and satisfactory for diagnostic angiography and MT. Using this setup, time between stroke imaging and groin puncture (picture-to-puncture time) was reduced by up to 35 min (including time for preparation of the patient such as intubation).
Conclusions
MT using a combined CT/C-arm system is safe and feasible. The potential advantages, particularly time saving and ensuing improvement in patient outcome, need to be assessed in a larger study.
Keywords: Thrombectomy, Stroke, CT, Technology, Angiography
Introduction
Ischemic stroke caused by large vessel occlusion is associated with poor outcome with high rates of death and disability.1 Recent studies have indicated safety and efficacy of mechanical thrombectomy (MT) in the treatment of acute ischemic stroke (AIS).2–6 Baseline National Institutes of Health Stroke Scale (NIHSS) score, age, and degree of recanalization are independent predictors of clinical outcome in patients undergoing MT.7 Time to recanalization is crucial for a good clinical outcome as well,8–11 and is the strongest modifiable factor beyond patient characteristics. Factors influencing time to recanalization can be divided into pre-hospital factors (eg, detection of symptoms, contact of the emergency medical service, hospital transfer) and in-hospital (mostly logistic) factors.
Several studies have already indicated that a single or combined logistic measure can be implemented and may shorten time to recanalization by reducing door-to-puncture time and/or picture-to-puncture (P2P) time.9 12–14 A further reduction in P2P time and time to recanalization may be achieved by merging stroke imaging and MT in a dedicated combined imaging and treatment suite. This would deem patient transfer from imaging suite to angiography suite unnecessary, decrease logistic effort, and save time.
A combination of imaging and angiography could be achieved by angiographic or flat-panel CT in the angiography suite. Flat-panel CT is already used in peri-interventional visualization of complications (eg, intracranial hemorrhage) and perfusion imaging,15–18 but image quality is not yet sufficient to rule out small intracranial hemorrhage19 or to detect early signs of an ischemic stroke. These imaging findings, however, are essential for the indication of intravenous thrombolytics and MT and, therefore, flat-panel CT so far cannot replace conventional CT or MRI of AIS.
To combine both imaging modalities we aimed to perform diagnostic angiography and MT on the table of the CT scanner in a dedicated setting. This was achieved by a new mobile C-arm X-ray device (Cios Alpha; Siemens AG, Healthcare Sector, Erlangen, Germany) using full-view flat detector technology and adapted to the spiral CT system. Here we report the technical setup, system performance, and preliminary clinical experience.
Methods
The mobile C-arm X-ray device (Cios Alpha)
The Cios Alpha is a commercially available mobile C-arm X-ray device and a mobile monitor cart. The device is equipped with a 30×30 cm (12×12 inch), 1.5×1.5 k full-view flat detector and a 25 kW power generator. A motorization package and a remote control unit allow direct control of the C-arm in a sterile field during endovascular therapy. The monitor cart mounts two high-brightness high-contrast thin-film transistor (TFT) monitors, the data interface, and storage unit.
Setup of the mobile C-arm X-ray device within the CT imaging suite
The CT imaging suite is equipped with a commercially available 64-slice SOMATOM Definition AS CT scanner (Siemens AG, Healthcare Sector, Forchheim, Germany). The CT patient table is installed 95 cm (37.4 inch) away from the gantry, in contrast to the standard setup (30 cm (11.8 inch)), thus enabling the C-arm of the Cios Alpha to be positioned in the gap between the gantry and patient table during MT (figure 1A). Horizontal and orbital movements of the C-arm are unrestricted whereas angular movement of the C-arm is limited to 20° in the anterior or posterior direction to avoid collision of the C-arm with the patient, gantry or patient table. For direct remote control of the patient table, CT scanner and C-arm, two remote control units for both the C-arm and CT scanner (i-Control; Siemens AG, Healthcare Sector, Forchheim, Germany) are mounted to the side rail of the patient table. These switches allow the neurointerventionalist to move the CT scanner, maneuver the C-arm, and move the patient table in almost the same mode as in the existing standard biplane angiographic setup (figure 1B). Two ceiling-mounted monitors (part of the Adaptive three-dimensional Intervention Suite; Siemens AG, Healthcare Sector, Erlangen, Germany) were installed to replace the monitor cart within the CT imaging suite. The monitor cart is stationed in an adjacent room allowing concurrent viewing and, if necessary, data processing without exposure to X-rays. In case of a malfunction of the ceiling-mounted monitors, the monitor cart can be brought immediately to the CT imaging room. To protect the neurointerventionalist from radiation, an adjustable ceiling-mounted upper body protective shield and a lower body X-ray protective shield are in place. For the treating anesthesiologist or neurointensivist, a mobile height-adjustable full body X-ray protective shield is available for upper and lower body protection from radiation.
Figure 1.
(A) Setup of the CT/C-arm intervention suite with the Cios Alpha in its operating position (partially covered by the height-adjustable upper body and the mobile lower body X-ray protection shields). (B) Setup in use during mechanical thrombectomy. Note: The remote controls for the C-arm and the CT (center, bottom) can be mounted in alternative order to the side rail of the CT table.
Pre- and post-interventional management
On admission, a stroke neurologist performed physical neurologic examinations and detailed assessment of the NIHSS score in the emergency room. Patients with suspected AIS and an NIHSS score of ≥10 received a standardized stroke imaging protocol consisting of a non-contrast enhanced cranial CT (CCT), CT perfusion of the brain as well as CT angiography of the aortic arch, cervical, and intracranial arteries. During the intervention, patients received standardized peri-interventional management and monitoring of physiological target values according to in-house standard operating procedures and the discretion of the treating neurointensivist adapted to the patient and situation. To detect possible peri-procedural complications, CCT and/or CT perfusion could be repeated.
All patients were initially observed in a neurologic intensive care unit after the interventional procedure. Transfer to the stroke unit occurred as soon as possible depending on the clinical condition of the patient. Follow-up CT or MRI was routinely performed at 20–36 h after treatment, or earlier if neurologic deterioration occurred. Post-interventional NIHSS and modified Rankin Scale scores were assessed by detailed physical examinations performed by an independent stroke neurologist at discharge.
Results
Patients
We report our preliminary clinical experience with the CT/C-arm stroke system in three patients starting in October 2014. The decision to perform the procedure on the new system and the choice of the endovascular devices was made by the respective neurointerventionalist and neurologist.
Case 1
An 84-year-old man presented with low-grade right-sided weakness and reduced sense of sensation which had worsened until arrival at the hospital (NIHSS 17). He had a medical history of hypertension and diabetes mellitus type 2, but was otherwise previously independent.
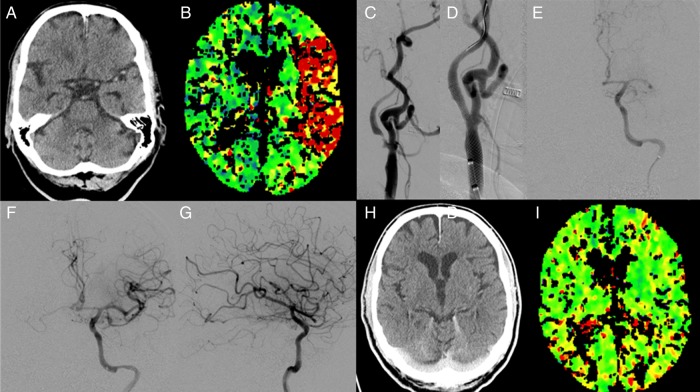
CT showed a dense artery sign in the left middle cerebral artery (MCA) and a significant increase in time to peak perfusion in the corresponding territory (figure 2A, B). CT angiography revealed an occlusion of the left MCA (image not shown) and the decision for MT was made. Initiation of general anesthesia and intubation on the CT table was followed by sterile draping and skin disinfection of the right-sided groin for puncture and placement of an 8 F introducer into the femoral artery. With support of a SIM2 angiographic catheter, a balloon guide catheter (Cello 8 F, Covidien, Dublin, Ireland) was placed in the left common carotid artery. Angiographic imaging showed a left-sided high-grade cervical internal carotid artery stenosis (80%, figure 2C). Interventional therapy started with an angioplasty of the stenosis using a 3×20 mm PTA balloon which was followed by placement of a carotid Wallstent (7×40 mm; Boston Scientific, Marlborough, Massachusetts, USA) (figure 2D). Afterwards the internal carotid artery could be passed by a 5 F distal access catheter (Sofia, MicroVention, Tustin, California, USA). Angiographic imaging confirmed an occlusion of the MCA (M1 segment, figure 2E), which was subsequently passed by a guidewire and microcatheter (Traxcess, Rebar-18 Microcatheter, Covidien) to deploy a stent-retriever device (Solitaire 2, 6×20 mm, Covidien). After a single mechanical retrieval maneuver, the clot in the M1 segment was removed completely (Thrombolysis In Cerebral Infarction (TICI) grade 3; figure 2F, G). Post-interventional CT imaging showed no signs of intracranial hemorrhage and a symmetric perfusion (figure 2H, I).
Figure 2.
(A) Dense artery sign in the left middle cerebral artery (MCA). (B) Increase of time-to-peak in CT perfusion in the left MCA territory. (C, D) A high-grade stenosis of the left cervical internal carotid artery before and after stent-assisted angioplasty. (E) Intracranial occlusion of the left MCA (M1 segment). (F, G) Left MCA after clot retrieval. (H, I) CT and CT perfusion after treatment without a sign of infarct demarcation or perfusion deficit.
Case 2
A 51-year-old man without relevant comorbidity was found unconscious at home with unknown time of onset of symptoms and intubated on site by the emergency medical service.
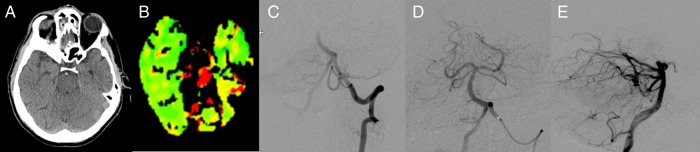
Stroke imaging revealed a dense artery sign at the tip of the basilar artery (BA) and a matching increase in time to peak perfusion (figure 3A, B). After standardized preparation for vascular arterial access, a 7 F long sheath was placed in the left subclavian artery allowing a 5 F vertebral angiographic catheter to be positioned in the left vertebral artery. Angiographic imaging confirmed a BA occlusion (figure 3C). A distal access catheter (Sofia) was placed into the root of the BA. The occlusion was passed by a guidewire and microcatheter (Traxcess, Rebar-18 Microcatheter) which were placed into the left posterior cerebral artery. A stent-retriever device (Solitaire 2, 6×20 mm) was deployed and a single mechanical retrieval maneuver removed the clot completely (TICI grade 3; figure 3D, E).
Figure 3.
(A) Non-contrast enhanced CT reveals a dense artery sign in the basilar artery. (B) CT perfusion shows a significant reduction of perfusion of the pons and the superior cerebellar artery territory on both sides. (C) Angiographic imaging shows an occlusion of the basilar tip. (D, E) Posterior circulation after mechanical thrombectomy without evidence of a remaining occlusion.
Case 3
An 83-year-old man with moderate to severe AIS (NIHSS 17) was referred for further diagnostics and possible interventional treatment from a primary care hospital where he had already received intravenous recombinant tissue plasminogen activator.
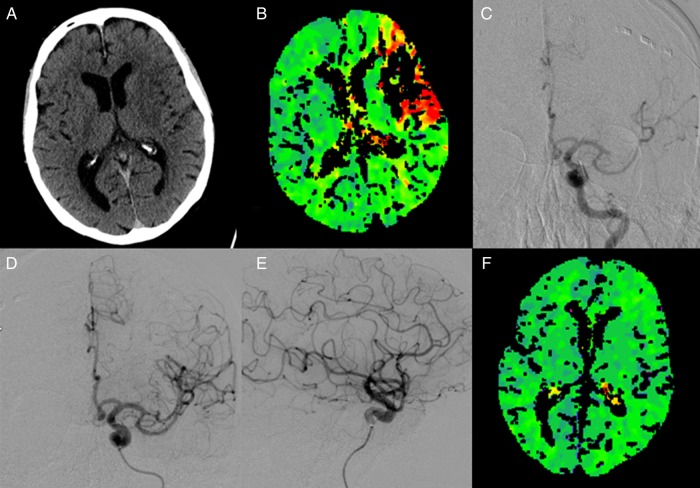
CCT was repeated because of clinical deterioration during transfer to exclude intracranial hemorrhage (figure 4A). CT perfusion and CT angiography showed a left-sided proximal M2 occlusion (superior trunk) with an equivalent decrease in brain perfusion (figure 4B). While the patient was intubated on the CT table by the neurointensivist, the neurointerventionalist concurrently started the interventional procedure by prepping the placing of an 8 F guiding catheter. A 5 F vertebral catheter was positioned in the left internal carotid artery. Angiographic imaging confirmed a distal M2 occlusion with poor leptomeningeal collaterals (figure 4C). A distal access catheter (Sofia) was placed into the internal carotid artery and the M2 occlusion was subsequently passed by a guidewire and microcatheter (Traxcess; Rebar-18). A stent-retriever device (Solitaire 2, 6×20 mm) was deployed in the occluded M2 segment. The clot was removed completely after three mechanical retrieval maneuvers leaving no perfusion deficit (TICI grade 3; figure 4D, F).
Figure 4.
(A) Non-contrast enhanced CT shows hypodensity in the lenticular nucleus and the insular cortex and excludes intracranial hemorrhage. (B) CT perfusion demonstrates a fairly large deficit in almost two-thirds of the left middle cerebral artery territory. (C) Angiographic imaging delineates a proximal M2 occlusion (superior trunk). (D, E) The superior trunk of the left middle cerebral artery is reperfused after mechanical thrombectomy. (F) Symmetric brain perfusion after thrombectomy.
Comparison with a biplane angiographic system
Since biplane angiographic systems are usually used in our center and other centers for MT, we provide preliminary technical and time relevant data from the first patients who received MT using the CT/C-arm system in comparison with a small historic patient cohort in August to October 2014 (n=16).
Median P2P time was 35 min (IQR 34–43) and median onset to recanalization (TICI 2b/3) time was 183 min (IQR 175–243) in the CT/C-arm system group. For patients who received MT using a biplane angiographic system, median P2P time aggregated to 57 min (IQR 50–71) and median onset to recanalization time totaled 250 min (IQR 214–319).
Using the CT/C-arm system, mean±SD signal-to-noise ratio (SNR) was 38 (8) and radiation dose was 4045 (834) µGy×m² compared with a mean SNR of 45 (8) and a radiation dose of 18 797 (8357) µGy×m² using the biplane angiographic system in comparable procedures.
Discussion
MT using stent-retrievers has been proven to be safe and effective in stroke due to large vessel occlusions.2–4 20–22 Besides final recanalization, the time to recanalization after stroke onset is crucial for patient outcome.8 23 24 Among all in-hospital factors, logistic measures are crucial to reduce time to treatment —that is, recanalization in the endovascular setting. Here we report the first use of a combined CT/C-arm system for interventional stroke treatment in order to decrease time from CT to recanalization, increase the safety of the procedure, and extend the application of endovascular stroke treatment to a more general setting, in particular in centers lacking a dedicated neurointerventional X-ray suite.
Using the combined CT/C-arm system, the time window between symptom onset and endovascular therapy may be reduced by accelerating initiation of endovascular therapy. This affects time metrics relevant for clinical outcome such as P2P time, onset to puncture time, and onset to recanalization time.9 11–13 In these few cases, P2P time and onset to recanalization time were clearly reduced compared with large multicenter studies.3 4 Since this is a series of only three patients, these time windows should be viewed cautiously and investigated in a larger patient cohort.
While accelerating initiation of endovascular therapy is very important, the CT/C-arm system does not neglect the need for state of the art stroke imaging, which is a prerequisite for initiation of intravenous thrombolysis and MT. On the contrary, this setting allows precise pretherapeutic imaging as well as immediate, intra- or post-interventional detection and monitoring of peri-/intraprocedural complications via repeated CT scans with high imaging quality (in contrast to flat-panel CT). Furthermore, repeated CT perfusion after MT could demonstrate successful brain reperfusion, which complements angiographic findings and therefore allows a better prognostic estimation.
Performing endovascular therapy on the CT table using this combined CT/C-arm system eliminates further patient transfers. This is important because of possible time saving but, in addition, in these severely ill sometimes obese patients every transport or repositioning is very strenuous for the patient as well as for the medical personnel and can be avoided by treating the patient on the CT table.
Although all the patients in this case series were intubated prior to MT, this setting allows MT in conscious sedation as well.
Another advantage of this combined CT/C-arm system is the transformation of an interventional suite out of a pre-existing room with X-ray protection. Minor reconstruction works, including the installation of the ceiling-mounted monitors and upper body X-ray protection shield, in combination with the Cios Alpha device turned a regular CT imaging suite into a versatile CT imaging and intervention suite at our institution at relatively low cost. Furthermore, in situations where the standard angiographic suite is occupied or out of order for maintenance, this option allows endovascular therapy for procedures other than time-sensitive emergencies.
Mobile C-arm X-ray devices have been in use for years for procedures such as retrieval of foreign bodies, guidance during spinal surgery, endovascular aortic repair, and coronary bypass surgery.25–28 Perhaps because of the high image quality and technical prerequisites required, no attempt has been made to use a mobile C-arm X-ray device for MT in AIS to date. With the introduction of the Cios Alpha, technical prerequisites are available to open this new application for mobile C-arm X-ray devices. The Cios Alpha device is equipped with all necessary angiographic features including fluoroscopic imaging, subtraction imaging, and road-mapping for delineation of the vessels. Imaging quality is satisfactory for precise maneuvering of guide wires, catheters, and interventional devices at doses of radiation lower than a biplane angiographic system. Moreover, all movements of the C-arm can be done remotely from the CT table so no mechanical adjustments of the C-arm need to be made.
The gap between the CT gantry and patient table was increased by 65 cm (25.6 inch) from the standard setting to 95 cm (37.4 inch) to allow the C-arm to be placed between the table and CT gantry. This seemingly small difference allows positioning, rotation, and angulation of the C-arm device for interventional therapy. The CT scanner, patient table, and C-arm device are directly controlled remotely by the neurointerventionalist via two control units. These remote control units are mounted to the side rail of the patient table and fit into the sterile field during endovascular therapy. Together with the individually adjustable ceiling-mounted monitors and X-ray protection shield as well as remote controls, this unique setup allows state of the art endovascular therapy in almost the same manner as a primary monoplane angiographic system. Most importantly, this setup does not impede diagnostic CT examinations if no intervention is being undertaken.
Conclusion
MT using a combined CT/C-arm system is safe and feasible. The potential advantages, particularly time saving and ensuing improvement in patient outcome, need to be assessed in a larger study.
Footnotes
Correction notice: This article has been corrected since it published online first. The Open Access licence has been added.
Contributors: JP, MB and MM accept full responsibility for the finished article, had access to any data, and controlled the decision to publish. JP was responsible for literature search, figures, study design, writing, data collection, data analysis, data interpretation, approval of ethics committee, patient inclusion. MM and MB had the idea for the study design and supervised data collection, data analysis, and data interpretation. CH, MP, SS, JB, PAR, and SH helped with data collection and data interpretation.
Competing interests: JP received grants from Siemens AG, Healthcare Sector, Germany during the conduct of the study.
Patient consent: Obtained.
Ethics approval: The study was conducted in accordance with the Declaration of Helsinki in its current version and the current version of ICH-GCP principles and was approved by our local ethics committee (ethics committee of the University of Heidelberg; ID S-303/2014).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Smith WS, Lev MH, English JD, et al. Significance of large vessel intracranial occlusion causing acute ischemic stroke and TIA. Stroke 2009;40:3834–40. 10.1161/STROKEAHA.109.561787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015;372:11–20. 10.1056/NEJMoa1411587 [DOI] [PubMed] [Google Scholar]
- 3.Campbell BC, Mitchell PJ, Kleinig TJ. et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015;372:1009–18. 10.1056/NEJMoa1414792. [DOI] [PubMed] [Google Scholar]
- 4.Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015;372:1019–30. 10.1056/NEJMoa1414905 [DOI] [PubMed] [Google Scholar]
- 5.Mohlenbruch M, Seifert M, Okulla T, et al. Mechanical thrombectomy compared to local-intraarterial thrombolysis in carotid T and middle cerebral artery occlusions: a single center experience. Clin Neuroradiol 2012;22:141–7. 10.1007/s00062-011-0099-9 [DOI] [PubMed] [Google Scholar]
- 6.Mohlenbruch M, Stampfl S, Behrens L, et al. Mechanical thrombectomy with stent retrievers in acute basilar artery occlusion. AJNR Am J Neuroradiol 2014;35:959–64. 10.3174/ajnr.A3796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nogueira RG, Liebeskind DS, Sung G. et al. Predictors of good clinical outcomes, mortality, and successful revascularization in patients with acute ischemic stroke undergoing thrombectomy: pooled analysis of the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) and Multi MERCI Trials. Stroke 2009;40:3777–83. 10.1161/STROKEAHA.109.561431 [DOI] [PubMed] [Google Scholar]
- 8.Khatri P, Abruzzo T, Yeatts SD, et al. Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology 2009;73:1066–72. 10.1212/WNL.0b013e3181b9c847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sun C-HJ, Nogueira RG, Glenn BA, et al. “Picture to puncture”: a novel time metric to enhance outcomes in patients transferred for endovascular reperfusion in acute ischemic stroke. Circulation 2013;127:1139–48. 10.1161/CIRCULATIONAHA.112.000506 [DOI] [PubMed] [Google Scholar]
- 10.Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929–35. 10.1016/S0140-6736(14)60584-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mazighi M, Chaudhry SA, Ribo M, et al. Impact of onset-to-reperfusion time on stroke mortality: a collaborative pooled analysis. Circulation 2013;127:1980–5. 10.1161/CIRCULATIONAHA.112.000311 [DOI] [PubMed] [Google Scholar]
- 12.Mehta BP, Leslie-Mazwi TM, Chandra RV, et al. Reducing door-to-puncture times for intra-arterial stroke therapy: a pilot quality improvement project. J Am Heart Assoc 2014;3:e000963 10.1161/JAHA.114.000963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun CH, Ribo M, Goyal M, et al. Door-to-puncture: a practical metric for capturing and enhancing system processes associated with endovascular stroke care, preliminary results from the rapid reperfusion registry. J Am Heart Assoc 2014;3:e000859 10.1161/JAHA.114.000859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Herrmann O, Hug A, Bosel J, et al. Fast-track intubation for accelerated interventional stroke treatment. Neurocrit Care 2012;17:354–60. 10.1007/s12028-012-9671-7 [DOI] [PubMed] [Google Scholar]
- 15.Kau T, Hauser M, Obmann SM, et al. Flat detector angio-CT following intra-arterial therapy of acute ischemic stroke: identification of hemorrhage and distinction from contrast accumulation due to blood-brain barrier disruption. AJNR Am J Neuroradiol 2014;35:1759–64. 10.3174/ajnr.A4021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rouchaud A, Pistocchi S, Blanc R. et al. Predictive value of flat-panel CT for haemorrhagic transformations in patients with acute stroke treated with thrombectomy. J Neurointerv Surg 2014;6:139–43. 10.1136/neurintsurg-2012-010644 [DOI] [PubMed] [Google Scholar]
- 17.Shinohara Y, Sakamoto M, Takeuchi H. et al. Subarachnoid hyperattenuation on flat panel detector-based conebeam CT immediately after uneventful coil embolization of unruptured intracranial aneurysms. AJNR Am J Neuroradiol 2013;34:577–82. 10.3174/ajnr.A3243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mordasini P, El-Koussy M, Brekenfeld C. et al. Applicability of tableside flat panel detector CT parenchymal cerebral blood volume measurement in neurovascular interventions: preliminary clinical experience. AJNR Am J Neuroradiol 2012;33:154–8. 10.3174/ajnr.A2715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Struffert T, Eyupoglu IY, Huttner HB, et al. Clinical evaluation of flat-panel detector compared with multislice computed tomography in 65 patients with acute intracranial hemorrhage: initial results. Clinical article. J Neurosurg 2010;113:901–7. 10.3171/2010.2.JNS091054 [DOI] [PubMed] [Google Scholar]
- 20.Mazighi M, Meseguer E, Labreuche J, et al. Bridging therapy in acute ischemic stroke: a systematic review and meta-analysis. Stroke 2012;43:1302–8. 10.1161/STROKEAHA.111.635029 [DOI] [PubMed] [Google Scholar]
- 21.Rohde S, Bosel J, Hacke W, et al. Stent retriever technology: concept, application and initial results. J Neurointerv Surg 2012;4:455–8. 10.1136/neurintsurg-2011-010160 [DOI] [PubMed] [Google Scholar]
- 22.Bosel J, Hacke W, Bendszus M, et al. Treatment of acute ischemic stroke with clot retrieval devices. Curr Treat Options Cardiovasc Med 2012;14:260–72. 10.1007/s11936-012-0172-y [DOI] [PubMed] [Google Scholar]
- 23.Saver JL. Time is brain—quantified. Stroke 2006;37:263–6. 10.1161/01.STR.0000196957.55928.ab [DOI] [PubMed] [Google Scholar]
- 24.Spiotta AM, Vargas J, Turner R, et al. The golden hour of stroke intervention: effect of thrombectomy procedural time in acute ischemic stroke on outcome. J Neurointerv Surg 2014;6:511–16. 10.1136/neurintsurg-2013-010726 [DOI] [PubMed] [Google Scholar]
- 25.Schafer S, Nithiananthan S, Mirota DJ, et al. Mobile C-arm cone-beam CT for guidance of spine surgery: image quality, radiation dose, and integration with interventional guidance. Med Phys 2011;38:4563–74. 10.1118/1.3597566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aydin U, Aydin N, Gorur A, et al. Cineangiographic intraoperative evaluation of venous grafts during coronary bypass surgery. J Card Surg 2013;28: 258–61. 10.1111/jocs.12084 [DOI] [PubMed] [Google Scholar]
- 27.Maurel B, Sobocinski J., Perini P, et al. Evaluation of radiation during EVAR performed on a mobile C-arm. Eur J Vasc Endovasc Surg 2012;43:16–21. 10.1016/j.ejvs.2011.09.017 [DOI] [PubMed] [Google Scholar]
- 28.Pandyan D, Nandakumar N, Qayyumi BN, et al. C-arm fluoroscopy: a reliable modality for retrieval of foreign bodies in the maxillofacial region. J Contemp Dent Pract 2013;14:1193–6. 10.5005/jp-journals-10024-1475 [DOI] [PubMed] [Google Scholar]