Improving healthcare services can all too easily become synonymous with the use of certain in vogue tools for improving quality. Trigger tools, run charts and driver diagrams are just three examples of techniques used by frontline staff who are undertaking improvement work. Educators seeking to teach improvement are similarly faced with long lists of possible approaches and techniques with which to fill their course descriptions. As a consequence the temptation for improvement leaders and teachers is to include yet another technique in an already crowded curriculum, to add in more ‘stuff’.
But what if focusing so much on the tools is actually unhelpful? What if our attempts to create better and safer organisations is muddled rather than enhanced by the growing interest in so many techniques? Could we be putting off the very people we need to engage by the use of what can be seen as jargon? Might it lead people to see improvement as an event or a ‘project’ rather than as a way of working?
Sure, knowledge and skill are vitally important and we must be able to measure the impact of any changes over time. But maybe we need a way of framing improvement, that is, somewhere between the abstract ambition of ‘improvement’ and the specific methods which have come to be known as the tools of quality improvement.
Healthcare services will never realise their full potential until improvement becomes part of every worker's day job1 rather than a temporary phenomenon. For such a paradigm shift to occur, caregivers will need to learn and, most importantly, unlearn behaviours. At the individual level considerable habit change will be required. Within teams and across organisations such habits will become enshrined in new patterns of social interaction.
From techniques to habits
At The Health Foundation, we have recently been wondering how the conversation might change if it were framed in terms of the kinds of habits which successful improvers demonstrate.2 If we could agree on the kinds of habits which seem to matter, then it might be easier to consider which knowledge and what skills will be needed according to specific contexts. And then (and only then) it may become clearer to frontline staff which improvement tools they will wish to use. By the same token, if we are clearer about what the habits of improvers are, it might be easier for educators to select pedagogies most suited to the cultivation of these target habits.
A theory of change3 to underpin this line of argument looks like this:
If:
we clearly articulate the range habits which improvers need to have, and the knowledge and skills which will help them improve care.
Then:
we can more precisely specify the learning required and the best learning methods.
So that:
all caregivers embrace an ethic of learning, and considerable value is created for all those who create, deliver and use care services.
By articulating a set of habits it becomes easier to decide which techniques or skills and what knowledge needs to be learned rather than simply creating an ever-longer list of improvement methods. The frame becomes a means by which conversations can be had between frontline staff and curriculum and course developers to understand needs better.
Once the learning has been specified it is possible to have more informed conversations about which teaching and learning methods are likely to be most effective. With professional bodies we will then need to consider the timing of any learning, whether it is part of initial training and certification or ongoing professional development (and, potentially, revalidation). If communication is truly effective and if those who lead the National Health Service and other health services across the world can create the conditions in which learning can flourish, then improvement capability, hand in hand with ongoing learning, should be being cultivated.
And—a big ‘and’—through the staff's and patients’ lived experiences of an ‘ethic of learning’, safety and value are ultimately created.
The habits of improvers
Spend any time with someone for whom improvement really is an intrinsic part of their job and you realise that they are special. Improvers are constantly curious, wondering if there is a better way of doing something. They always want to extract the learning from any experience. Never content with keeping ideas to themselves, they are out there talking to and persuading others that an issue is worth exploring. They have well-honed influencing skills. Aware of the likelihood of disagreement they are prepared for and deal well with conflict. They have a positive mindset which can remain resilient in the face of inevitable adversity. They are constantly generating ideas and then inviting critical scrutiny of their thinking. They see strength in collaboration. Above all they see the health and social care systems and all the people who use and help to design them as complex systems. As a consequence they look to make connections, to build alliances and synthesise ideas in order to gain maximum acceptance of any planned change.
Improving quality, safety and value in health and social care requires a kind of real-world intelligence. This has been well described by Resnick: ‘Intelligence is the habit of persistently trying to understand things and make them function better. Intelligence is working to figure things out, varying strategies until a workable solution is found.’4 One's intelligence is, Resnick suggests, the sum of one's habits of mind. Others have found the lens of habits of mind helpful in framing not just specific subjects,5–7 but creativity and learning more generally.8 9
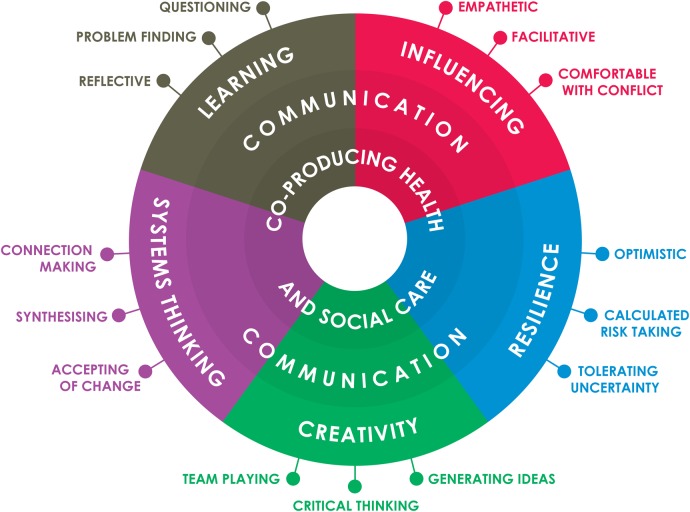
Figure 1 depicts improvers as having five core habits, each with three subelements. The whole model is premised on the idea that all care is coproduced and that communication at every turn of the process is vital. The core habits of mind (and of action) consist of learning, influencing, resilience, creativity and systems thinking. Improvers have an insatiable hunger to make things work better. Their drive for learning is a moral imperative. Improving anything is almost always a social project requiring buy-in and engagement from others. It requires people who can attract others to their cause and whose influencing skills are well honed. Resilience is vital in two senses—it calls upon the ability to bounce back from adverse events and it requires calculated risk-taking.
Figure 1.
The habits of an improver. At the centre of the figure is the goal of caregiving depicted as the coproduction of health and social care. In the middle the importance of communication in improvement is highlighted. Outside this are the five habits and attached to the outer ring are the 15 subhabits.
Creativity plays an important role in improvement work, and creative problem-solvers draw on a wide range of traditions and disciplines to ensure that the techniques and processes they use are most likely to encourage fresh thinking. Systems thinking is vital. Seeing whole systems as well as their parts and recognising complex inter-relationships, connections and dependencies is critically important, too. The interdependent nature of healthcare service work is its core property.
Attention has recently been drawn to the importance of organisational habits in creating highly reliable healthcare services.10 Cultivating the habits of reliable organisations and effective improvers at the same time can create a powerful tipping point for organisational effectiveness and collective morale.11
Pedagogies for improving quality
If reframing the way we see improvement can assist us in carefully considering which tools and methods we deploy at the frontline, it can also potentially help those who design curricula think more effectively about the teaching and learning methods they use. Cooke et al have shown us that teaching is not yet well enough done: ‘To the extent that quality and safety are addressed at all, they are taught using pedagogies with a narrow focus on content transmission, didactic sessions that are spatially and temporally distant from clinical work, and quality and safety projects segregated from the provision of actual patient care’.12
There is an idea which is potentially useful to all of us who are interested in learning which builds improvement capability—‘signature pedagogy’. First coined by Shulman in 2005, signature pedagogy refers to the types of teaching and learning which most suit or match the characteristics of a specific vocational pathway. ‘They form habits of the mind, habits of the heart and habits of the hand… signature pedagogies prefigure the cultures of professional work and provide the early socialization into the practices and values of a field’.13
So the development of the habits of improvers suggest here might be well served in general by:
sustained opportunities to observe critically and be part of improvement activities in a range of health and social care settings;
coaching and mentoring linked to improvement experiences;
peer teaching of techniques and methods;
peer critique using a range of formative methods for giving and receiving feedback;
enquiry-led approaches such as action research.
A number of educators are already well ahead in promoting these kinds of approaches.2
In healthcare a core learning method which closely matches the iterative nature of making changes and evaluating these over time is the Plan-Do-Study-Act (PDSA) cycle. Indeed the PDSA process is a kind of thumbprint for the process of improvement.14 It requires thoughtful planning, execution, evaluation of tests of change over time and actions which are then, it is hoped, better than previous ones.
But in our conversations with educators we want to go further in teasing out best pedagogies for the range of habits we believe to be desirable. We are taking each of the 15 subhabits and asking the question: how best can we teach this? How best, for example, can we learn how to:
ask better questions
be more facilitative
tolerate uncertainty
generate ideas
be accepting of change?
Such habits do not represent an alternative to knowledge or skill. Rather they are a complement. The questions above are bigger than whether or not to use a specific tool. And, there is a rich seam of literature on matching learning methods to such desired outcomes.15
The curious incident of the hands which did not get washed
Reliably safe care giving requires workers who are knowledgeable and skilled. But this is not of itself enough. We have, for example, known through the science of infection about the impact of sanitising gel or soap and water on germs. The skill of cleaning our hands has also been widespread for many generations, although there may be some technical aspects which require practice. So why, then is hand washing still not always done as it should be? The answer? Habit. Unless we have knowledge, skill and habit, then, despite good intentions, our actions may be unreliable.
It is the same with improvement more widely. We need, as Perkins and colleagues have put it, a ‘sensitivity to occasion’.16 Either our action needs reliably to arise unprompted in the context in which we work because it has become a habit, or—in this case—to be prompted through awareness raising, routine practicing and the availability of basins, water and dispensers. Knowledge and skills are not enough. Unless a skill is routinely used when it is required, it is useless.
To really get the improvement habit we need to understand the habits of reliable action and also those which seem most likely to cultivate the dispositions of sustainable improvement.
Acknowledgments
The author would like to thank Hadjer Nacer, Nick Barber and Helen Crisp at the Health Foundation for their many suggestions, improvement science fellows in the UK and in Sweden, many of the thoughtful educators who shared their experiences and Paul Batalden for many years of critical friendship and wisdom on this topic.
Footnotes
Competing interests: None declared.
Provenance and peer review: Commissioned; internally peer reviewed.
References
- 1.Batalden P, Davidoff F. What is “quality improvement” and how can it transform healthcare? Qual Saf Health Care 2007;16:2–3. 10.1136/qshc.2006.022046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lucas B, Nacer H. The habits of an improver: thinking about learning for improvement in healthcare. London: The Health Foundation, 2015. http://www.health.org.uk/sites/default/files/TheHabitsOfAnImprover.pdf (accessed 25 Nov 2015). [Google Scholar]
- 3.Davidoff F, Dixon-Woods M, Leviton L, et al. . Demystifying theory and its use in improvement. BMJ Qual Saf 2015;24:228–38. 10.1136/bmjqs-2014-003627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Resnick L. Making America Smarter. Educ Week Century Ser 1999;18:38–40. [Google Scholar]
- 5.Cuoco A, Goldenberg E, Mark J. Habits of mind: an organizing principle for mathematics curricula. J Math Behav 1996;15:375–402. 10.1016/S0732-3123(96)90023-1 [DOI] [Google Scholar]
- 6.Çalik M, Coll R. Investigating socioscientific issues via scientific habits of mind: development and validation of the scientific habits of mind survey. Int J Sci Educ 2012;34:1909–30. 10.1080/09500693.2012.685197 [DOI] [Google Scholar]
- 7.Lucas B, Hanson J. Thinking like an engineer: implications for the education system. London: Royal Academy of Engineering, 2013. http://www.raeng.org.uk/publications/reports/thinking-like-an-engineer-implications-full-report.pdf (accessed 25 Nov 2015). [Google Scholar]
- 8.Lucas B, Claxton G, Spencer E. Progression in student creativity in school: first steps towards new forms of formative assessments. OECD Education Working Papers, No. 86, OECD Publishing, 2013. 10.1787/5k4dp59msdwk-en (accessed 25 Nov 2015). [DOI] [Google Scholar]
- 9.Claxton G. Building learning power. Bristol: TLO, 2002. [Google Scholar]
- 10.Vogus TJ, Hilligoss B. The underappreciated role of habit in highly reliable healthcare. BMJ Qual Saf 2016;25: 141–6.. [DOI] [PubMed] [Google Scholar]
- 11.Souba W. Health care transformation begins with you. Acad Med 2015;90:139–42. 10.1097/ACM.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 12.Cooke M, Ironside P, Ogrinc G. Mainstreaming quality and safety: a reformulation of quality and safety education for health professions students. BMJ Qual Saf 2011;20(Suppl 1):i79–82. 10.1136/bmjqs.2010.046516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shulman L. Signature pedagogies in the professions. Daedalus 2005;134:52–9. 10.1162/0011526054622015 [DOI] [Google Scholar]
- 14.Taylor MY, McNicholas C, Nicolay C, et al. . Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf 2014;23:290–8. 10.1136/bmjqs-2013-001862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lucas B, Claxton G, Spencer E. How to teach vocational education: a theory of vocational pedagogy. London: City & Guilds, 2012. http://www.skillsdevelopment.org/PDF/How-to-teach-vocational-education.pdf (accessed 21 Nov 2015). [Google Scholar]
- 16.Perkins D, Jay E, Tishman S. Beyond abilities: a dispositional theory of thinking. Merrill-Palmer Q 1993;39:1–21. [Google Scholar]