Abstract
Objective
Spontaneous intracranial hypotension (SIH) is most commonly caused by cerebrospinal fluid (CSF) leakage. Therefore, we hypothesised that patients with orthostatic headache (OH) would show decreased optic nerve sheath diameter (ONSD) during changes from supine to upright position.
Methods
Transorbital B-mode ultrasound was performed employing a high-frequency transducer for ONSD measurements in the supine and upright positions. Absolute values and changes of ONSD from supine to upright were assessed. Ultrasound was performed in 39 SIH patients, 18 with OH and 21 without OH, and in 39 age-matched control subjects. The control group comprised 20 patients admitted for back surgery without headache or any orthostatic symptoms, and 19 healthy controls.
Results
In supine position, mean ONSD (±SD) was similar in patients with (5.38±0.91 mm) or without OH (5.48±0.89 mm; p=0.921). However, in upright position, mean ONSD was different between patients with (4.84±0.99 mm) and without OH (5.53±0.99 mm; p=0.044). Furthermore, the change in ONSD from supine to upright position was significantly greater in SIH patients with OH (−0.53±0.34 mm) than in SIH patients without OH (0.05±0.41 mm; p≤0.001) or in control subjects (0.01±0.38 mm; p≤0.001; area under the curve: 0.874 in receiver operating characteristics analysis).
Conclusions
Symptomatic patients with SIH showed a significant decrease of ONSD, as assessed by ultrasound, when changing from the supine to the upright position. Ultrasound assessment of the ONSD in two positions may be a novel, non-invasive tool for the diagnosis and follow-up of SIH and for elucidating the pathophysiology of SIH.
Introduction
Spontaneous intracranial hypotension (SIH) is an increasingly recognised syndrome with the hallmark of orthostatic headache (OH). Pathophysiology suggests spontaneous leakage of cerebrospinal fluid (CSF) through a spinal meningeal fistula.1 Diagnosis of SIH remains challenging and the criteria of the international headache society are evolving.2 3 A simple, cost-effective, non-invasive, and repeatable diagnostic tool that would aid in diagnosis, follow-up, and understanding of the pathophysiology of SIH would be useful.
High resolution transorbital sonography of the optic nerve sheath diameter (ONSD) is increasingly used for the assessment of raised intracranial pressure.4 Sonographic measurements showing increased ONSD in patients with raised intracerebral pressure (ICP) were confirmed using high-resolution MRI.5 6 Literature on ultrasound diagnostics in patients with SIH is very sparse and consists only of a case study and an investigation in 10 patients on the effect of epidural blood patch on ONSD and ophthalmic venous flow.7–9 Up to now, all measurements reported in the literature were only performed with patients lying supine, and no measurements were made after change to the upright position.
Based on pathophysiological considerations, we hypothesised that there is a change in ONSD from supine to upright position and that this change should be more pronounced in patients with acute OHs.
In the current study we evaluated the diagnostic value of ONSD by performing two high-resolution orbital ultrasound assessments, in supine and upright positions, in three groups: symptomatic and asymptomatic SIH patients, and controls.
Methods
Subject groups
Ultrasound of the ONSD is part of our routine diagnostic workup in all patients presenting with SIH in our departments.
We included all patients (18 years or older) with confirmed SIH from January 2013 to December 2014. SIH was diagnosed according to criteria of the international headache society.2 These criteria are: (A) any headache fulfilling criterion C; (B) low CSF pressure (<60 mm H2O) and/or evidence of CSF leakage on imaging; (C) headache has developed in temporal relation to the low CSF pressure or CSF leakage, or has led to its discovery; (D) not better accounted for by another International Classification of Headache Disorders 3rd edition (ICHD-3) diagnosis. All patients with confirmed SIH had evidence of CSF leakage on imaging as required by criterion (B) in the International Headache Classification.2 Imaging findings included subdural fluid collections, enhancement of the pachymeninges, sagging of the brain, or a fluid collection circumscribing the spinal dural sac in T2-weighted MRI (see online supplementary tables S1A, B).
Exclusion criteria included any pathology (ie, erosions) of the upper eyelid, any eye surgery within the previous 6 months, and recent head or neck trauma or conditions not allowing positional changes. Patients with postdural puncture headache and patients who had recent spinal surgery potentially affecting CSF dynamics were excluded.
SIH patients were dichotomised into: group A, those with current severe or immediate OH (ie, within 15 min after assuming an upright position); or group B, those with no OH after assuming an upright position, but who had a history (<4 weeks) of OH that developed in less than 15 min on shifting to upright position. All consecutive patients received dynamic ultrasound assessment of the ONSD. Additionally, we examined 20 patients without headache or any orthostatic symptoms (group C1) and 19 healthy controls (C2). Group C consisted of similarly aged patients who were admitted for back surgery due to spinal stenosis or disc herniation; all their data are based on presurgical examinations. Group C2, which served as an external control, comprised healthy volunteers from Regensburg, Germany. A joint meeting between the groups from Bern and Regensburg was held prior to the start of the study to ensure consistency of examinations at the two study centres. Ultrasound was performed using the same protocol in the two centres.
Twofold assessment of the ONSD
In Bern, the change in ONSD was measured with a 7–15 MHz linear array transducer in transorbital B-mode ultrasound (IU 22 equipped with a 15L8 transducer, Philips, Amsterdam, the Netherlands). In Regensburg, the ultrasound machine was Toshiba Xario XG equipped with a high frequency linear array transducer (PLT-1204BT, Tokyo, Japan).
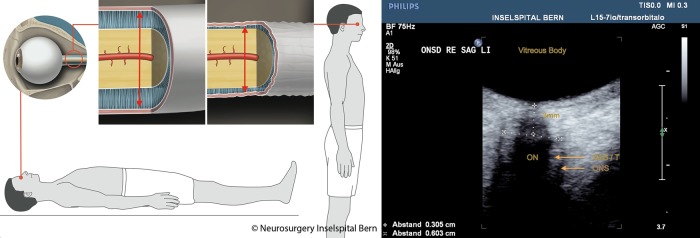
The examination was conducted first with the patient in supine position and then in upright position with the patient standing for 2 min (figure 1). The probe was placed on the temporal part of the upper eyelid using a thick layer of gel.
Figure 1.
Left: Illustration of change in diameter of the ONS in a patient with spontaneous intracranial hypotension. Right: optic nerve sheath diameter (ONSD) image from transorbital ultrasound. Illustration of the changes in the diameter of the ONS in a symptomatic patient that occur with the change from supine to upright body position. The red arrow indicates the subarachnoid space around the optic nerve measured by ultrasound. The upper left picture shows the diameter of the ONS in a symptomatic patient while supine. The upper right picture shows a decreased ONS diameter when this patient assumes upright position. Right-side image: ONSD was assessed 3 mm behind the papilla in axial and sagittal planes on both sides using a perpendicular axis. The field of view is adjusted to a depth of 40 mm. (SAS/T=subarachnoid space/trabeculae; ONS, optic nerve sheath).
Ultrasound safety and diagnostics
To comply with maximum patient safety, Mechanical Index as an on-screen parameter was reduced to 0.3, which is concordant with the guidelines of the British Medical Ultrasound Society and US Federal Drug Administration, which recommends a Mechanical Index of 0–0.3 and less than or equal to 0.23 for ultrasound of the eye.10 11
The field of view was adjusted to a depth of 40 mm and a single focal zone placed behind the orbit. The B-mode gain was reduced for optimisation of the optic nerve sheath (ONS). ONSD was measured 3 mm behind the echogenic lamina cribrosa in axial and sagittal planes to the cranium on both sides using a perpendicular axis as previously described.8 11 The documented ONSD was computed from the mean of four values for each patient, that is, two on each eye (figure 1). In both study centres, an examiner trained in ultrasound diagnostics of the ONS performed all ultrasound examinations. The examiner was not blinded with regard to the clinical presentation of the patient.
Outcome measures and statistical analysis
For this exploratory study, the primary analysis population consisted of subjects who had an ONSD assessment in supine and in upright position. The primary analysis variable was the change in the ONSD from supine to upright position.
The comparison of ONSD among groups was performed using the Wilcoxon rank-sum test (two groups) or the Kruskal-Wallis test (more than two groups). Analysis of covariance was employed for supportive evaluations and was adjusted for age and gender. For evaluation of the ONSD change, analysis of covariance was adjusted for the value in supine position. An analysis of receiver operating characteristics (ROC) curves was used to assess the diagnostic test for the presence of OHs based on ONSD. Logistic regression was used to include effects for gender, age and supine ONSD. Statistical tests were two-sided and conducted at the 5% significance level. No correction for multiplicity was used.
Ethical considerations
The analysis was carried out in accordance with Good Clinical Practice guidelines, Swiss Academy of Medical Sciences guidelines, and the Declaration of Helsinki. The ethics board of the Bern University Hospital approved the study (Bern, Switzerland, KEK-Nr. 021/14). The prospective study of healthy volunteers in Regensburg was approved by the local ethics committee (Regensburg, Germany, 14-101-0076).
Results
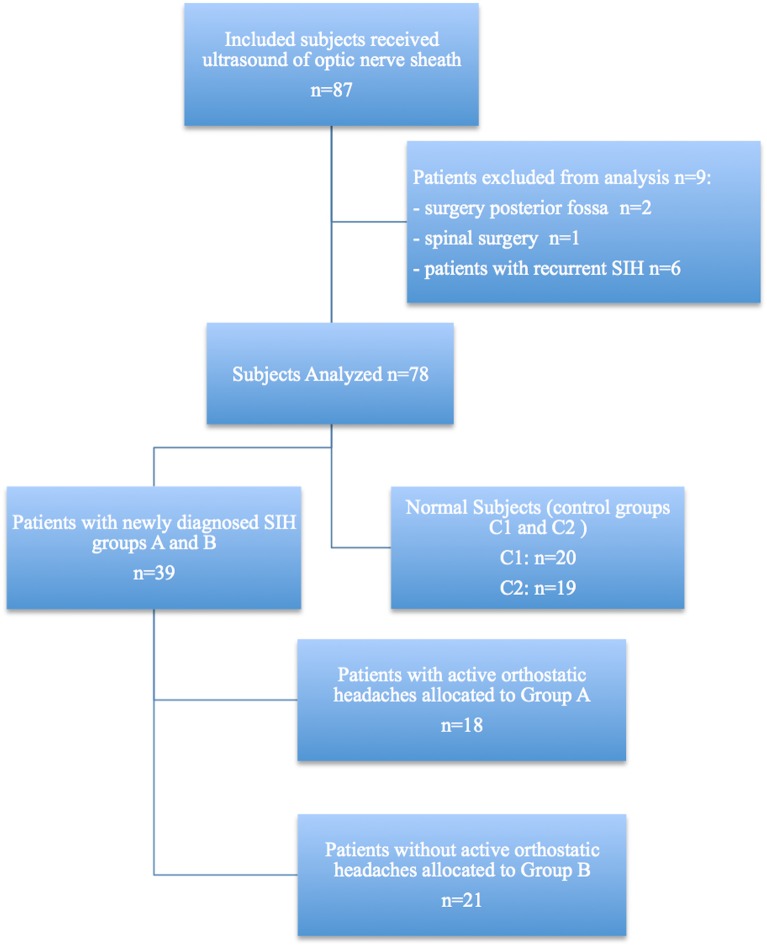
Ultrasound was performed in 48 patients plus 39 controls in the same age range. Nine patients had to be excluded from further analysis because of recent surgery with a possible effect on CSF dynamics (posterior fossa surgery, n=2; recent spinal surgery, n=1; postdural puncture headaches, n=6). Thus, 39 patients with newly confirmed SIH as well as 39 controls were included for analysis (figure 2). The demographic and clinical characteristics of the included patients are shown in online supplementary tables S1A, B.
Figure 2.
Subject disposition diagram. SIH, spontaneous intracranial hypotension.
All patients in groups A and B were selected according to the International Headache Society criteria for SIH and had confirmed diagnosis of SIH.2 At the time of the examination, 18 patients of group A (10 men, 8 women; mean age 52 (range 27–75) years) had OHs when assuming the upright position. The 21 patients comprising group B (11 men, 10 women; mean age 63 (range 39–83) years) did not have immediate (ie, within <15 min) severe OHs. The control group (C1+C2) comprised 39 patients: 20 patients (14 men, 6 women; mean age 51 (range 18–73) years) from one study centre (C1), plus 19 healthy controls (10 male, 9 female; mean age 58 (range 50–67) years) from the other study centre (C2).
In the primary analysis population no missing ultrasound assessments were reported. No adverse events were reported.
Results of ultrasound of the ONSD
In the supine position ONSD was similar among patients with and without OH (p=0.921). The mean ONSD in supine position in patients with active OH (group A) was 5.38±0.91 mm, which was similar to values for patients with confirmed SIH but without active OH (group B), 5.48±0.89 mm.
In the upright position there was a statistically significant difference between patients with and without OH (p=0.044). Patients with active OH (Group A) had a mean ONSD of 4.84±0.95 mm, whereas patients without active OH (Group B) had a mean of 5.53±1.02 mm.
The change (Δ) in ONSD between supine and upright position was statistically significantly different between groups A and B (p<0.001). The mean difference (Δ) between supine and upright position in patients with active OH (Group A) was −0.53±SD 0.34 mm. Patients without active OHs (Group B) had a mean difference (Δ) of 0.05±0.41 mm. Comparison of patients with OH and SIH (Group A) to patients without OH (Group B), versus the controls (Groups C1 and C2 combined: 0.01±0.38 mm) showed a statistically significant difference (Δ) (p<0.001; figure 3).
Figure 3.

Bee swarm box-plot data with means and SDs showing the differences between groups. Bee swarm box-plot data with means and SDs illustrate the differences (Δ) in patients with orthostatic headaches (Group A, green), without (Group B, red) and patients without an spontaneous intracranial hypotension (SIH) diagnosis (C1, grey, internal control and C2, black, external control).
Only patients with confirmed SIH and OH had a significant decrease (−10%) of ONSD (Group A supine: 5.38±0.91 mm vs Group A upright: 4.84±0.99; p<0.001).
Analysis of covariance was used to adjust estimates for the potentially confounding effects of age and sex. Results in a model comparing groups A, B and C confirmed that the only group with a significant change in ONSD was Group A (SIH with OH; p<0.001).
We evaluated the diagnostic accuracy of the difference in ONSD with the operator: presence of OHs (Group A) against Groups B, C1 and C2. ROC analysis for difference of ONSD between supine and upright position revealed an area under the curve of 0.874 (95% CI 0.776 to 0.972; p<0.001).
Discussion
Using ultrasound measurements, we showed a significant reduction of 10.0% in the ONSD in the standing position compared to the supine position in patients diagnosed with SIH and current OHs. Unlike patients with OHs, patients diagnosed with SIH but without active OHs at the time of examination, as well as controls, did not show a significant ‘collapse’ of their ONSs when moving from a supine to an upright position. The demonstration of a collapse of the ONSD in SIH patients when changing from supine to upright position is a novel finding and assessment of the ONSD using ultrasound might become a useful diagnostic tool for diagnosis and follow-up of patients with SIH. Furthermore, our findings give intriguing insights into the pathophysiology of SIH.
The current results of the diameter of the ONS are in line with the reported ultrasound values in the literature of 5.4 and 5.75 mm in healthy adults, as well as MRI of 5.1 and 5.3 mm.12–16 A study by Takeuchi et al6 showed significantly smaller ONSD using MRI techniques and measured the ONSD in two slices (just behind the eyeball and 3.5 mm behind the first slice, mean 3.34 and 4.85 mm, respectively). These differences may be due to the different depth as we, and the previously mentioned groups, performed the ONSD measurements 3 mm behind the ocular bulb, as suggested by Helmke and Hansen.17 Two other studies using coronal short tau inversion recovery sequences behind the optic bulb suggested a loss of CSF signal around the optic nerve in supine position—although these were not quantitative studies and did not include control groups.14 18
The width of the ONS is related to the intracranial pressure; numerous reports and prospective studies have shown an increase of the ONSD in patients with intracranial hypertension.12 19–21 Measurements of the ONS response to increased CSF pressure by lumbar intrathecal infusion tests showed an immediate increase. However, to date, significant differences in ONSD between patients with OH, patients without OH, or healthy controls have not been found. Therefore, and based on the pathophysiology and MRI findings of SIH as summarised by Schievink et al1 and Mokri,22 we hypothesised that changes of the ONSD should be detectable when the body position is changed from supine to upright, which causes an orthostatic decrease of intracranial pressure.1 22–26 The dynamic paradigm of performing two measurements—first supine, then upright—showed a significant change in ONSD in patients with SIH. However, the change in ONSD was significant only in SIH patients when they were symptomatic, indicating a higher compliance capacity, or an ongoing loss of CSF.27 Currently the sensitivity of transorbital ultrasound for SIH seems to be rather low and would, thus, not be a suitable screening tool. However, to provide robust numbers of sensitivity and specificity, clearly a larger, possibly multicentre trial will be necessary. SIH is mainly a clinical diagnosis with the hallmark of orthostatic symptoms and MRI findings. However, SIH has a wide clinical spectrum and some patients do not show typical orthostatic symptoms or MRI findings. For these patients transorbital ultrasound may be of diagnostic help and the current data suggests that it has the potential for stratifying patients for more invasive tests and as a prognostic marker. Furthermore, dynamic ultrasound may assess the efficacy of treatment, may be used for follow-up examinations, and may provide insight into the pathophysiology of SIH.
One explanation for the collapse of the ONS could be that patients who are symptomatic with headache suffer from an ‘open’ fistula with continuous leakage of CSF. This in turn leads to a more pronounced loss of intracranial CSF and decrease of ICP while in the upright position as compared to control patients or SIH patients without headaches, eventually leading to a measurable and significant change of the subarachnoid space around the optic nerve (figure 1).
Assessing ONSD both in supine and upright positions might enhance the usefulness of ultrasound examinations of the ONS and could be a useful bedside tool for patients with OH. It has several advantages: (1) it is not affected by the normal variability of the ONS diameter between patients, (2) it ameliorates the unknown relationship between ONS diameter and CSF pressure in individual cases, and (3) it eliminates the interobserver variability of ultrasound measurements of the absolute ONSD because the same observer can perform both examinations.
The stratification of our patients is based on the hypothesis that the amount of CSF moving from the intracranial to the spinal compartment when patients shift from a supine to standing position is larger in patients with OH. Unlike patients without OH or controls, there is not enough CSF in the intracranial space to support the weight of the brain at its normal intracranial position.28 The CSF leakage causes sagging of the brain and consequent tension to pain-sensitive structures like veins and the dura mater. Thus ongoing OH serves as a surrogate marker for active disease.
Study limitations
A limitation of our study is the difficulty of SIH diagnosis. We classified our patients according to the current criteria for SIH of the International Headache Society.2 The difficulty in making a sound diagnosis is reflected by the recent evolution of the diagnostic criteria. We recently proposed a classification system for the likelihood of a spinal CSF-fistula according to imaging findings.29 Inclusion of imaging findings in the diagnosis of SIH might improve understanding of SIH. A possible bias is the composition of the two control groups. One group comprised 20 patients hospitalised prior to elective back surgery; the other comprised 19 healthy controls in a different hospital. Each of the two control groups was examined by a different ultrasound unit with a different examiner. Evaluation of control subgroups (C1 and C2), showed slightly higher ONS diameters in the C2 subgroup in both supine and upright positions (see online supplementary table S2), which may result from the different clinical units or equipment used for these subgroups. However, the mean individual difference between supine and upright position (Δ) was not notably different between the C1 and C2 subgroups (see online supplementary table S3). A technical limitation of our study is the resolution of the ultrasound technique. A 7–15 MHz linear array transducer has an axial and lateral resolution of 0.1 mm, while the mean change of the ONSD was only 0.53 mm.30 Prospective studies in patients with OH following spinal tap or epidural anaesthesia may be appropriate to confirm the results of this study.
Conclusions
In summary, this report describes a difference in the diameter of the ONS on postural changes from supine to upright positions. Therefore, transorbital ultrasound in supine and upright positions may provide a novel method for the diagnostic workup of patients suspected to have SIH. Results of the current analysis are promising and suggest the need for a larger prospective series to assess sensitivity and specificity of this novel diagnostic tool for SIH.
Supplementary Material
Footnotes
Contributors: The study was designed by JB, JF, CB, AR, and HPM. Literature search and drafting of the report were performed by JF, JB, FS, HPM, and AR. Data collection was performed by JF, FS, CK, MV, ME, BS and AJ. Data analysis and/or interpretation were performed by JF, CTU, CF, AJ, PS, WJZ’G, JG, AR, JG, FS, HPM and JB. Statistical analysis was performed by CB, JF and JB. All authors reviewed the final version of the manuscript. Financial/institutional support was provided by AR and JB.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Bern University Hospital ethics committee and Regensburg local ethics committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The reviewers may view unpublished anonymised summaries of case report forms. The request should be addressed to the first author. The summaries will be available to reviewers after consent of the local ethics committee.
References
- 1.Schievink WI, Meyer FB, Atkinson JL, et al. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. J Neurosurg 1996;84:598–605. 10.3171/jns.1996.84.4.0598 [DOI] [PubMed] [Google Scholar]
- 2.Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33:629–808. 10.1177/0333102413485658 [DOI] [PubMed] [Google Scholar]
- 3.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia 2004;24(Suppl 1):9–160. 10.1111/j.1468-2982.2003.00824.x [DOI] [PubMed] [Google Scholar]
- 4.Ertl M, Barinka F, Torka E, et al. Ocular color-coded sonography—a promising tool for neurologists and intensive care physicians. Ultraschall Med 2014;5:422–31. 10.1055/s-0034-1366113 [DOI] [PubMed] [Google Scholar]
- 5.Hansen HC, Helmke K. Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: ultrasound findings during intrathecal infusion tests. J Neurosurg 1997;87:34–40. 10.3171/jns.1997.87.1.0034 [DOI] [PubMed] [Google Scholar]
- 6.Takeuchi N, Horikoshi T, Kinouchi H, et al. Diagnostic value of the optic nerve sheath subarachnoid space in patients with intracranial hypotension syndrome. J Neurosurg 2012;117:372–7. 10.3171/2012.5.JNS1271 [DOI] [PubMed] [Google Scholar]
- 7.Bauerle J, Gizewski ER, Stockhausen KV, et al. Sonographic assessment of the optic nerve sheath and transorbital monitoring of treatment effects in a patient with spontaneous intracranial hypotension: Case Report. J Neuroimaging 2011;23:237–9. 10.1111/j.1552-6569.2011.00640.x [DOI] [PubMed] [Google Scholar]
- 8.Dubost C, Le Gouez A, Zetlaoui PJ, et al. Increase in optic nerve sheath diameter induced by epidural blood patch: a preliminary report. Br J Anaesth 2011;107:627–360. 10.1093/bja/aer186 [DOI] [PubMed] [Google Scholar]
- 9.Chen CC, Luo CL, Wang SJ, et al. Colour doppler imaging for diagnosis of intracranial hypotension. Lancet 1999;354:826–9. 10.1016/S0140-6736(99)80013-0 [DOI] [PubMed] [Google Scholar]
- 10.British Medical Ultrasound Society. Guidelines for the safe use of diagnostic ultrasound equipment 2010. http://www.efsumb.org/ecmus/2011%20Guidelines%20for%20the%20safe%20use%20of%20Diagnostic%20Ultrasound%20Equipment.pdf (accessed Mar 2013).
- 11.FDA USFaDA. Ultrasound Imaging. 06/2012. http://www.fda.gov/Radiation-EmittingProducts/RadiationEmittingProductsandProcedures/MedicalImaging/ucm115357.htm (accessed Mar 2013).
- 12.Geeraerts T, Newcombe VF, Coles JP, et al. Use of T2-weighted magnetic resonance imaging of the optic nerve sheath to detect raised intracranial pressure. Crit Care 2008;12:R114 10.1186/cc7006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rohr A, Riedel C, Reimann G, et al. Pseudotumor cerebri: quantitative in vivo measurements of markers of intracranial hypertension. Fortschr Röntgenstr 2008;180:884–90. [DOI] [PubMed] [Google Scholar]
- 14.Rohr A, Riedel C, Fruehauf A, et al. MR imaging findings in patients with secondary intracranial hypertension. AJNR Am J Neuroradiol 2011;32:1021–9. 10.3174/ajnr.A2463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bäuerle J, Lochner P, Kaps M. Intra- and Inter-and interobserver reliability of sonographic assessment of the optic nerve sheath diameter in healthy adults. J Neuroimaging 2012;22:42–5. 10.1111/j.1552-6569.2010.00546.x [DOI] [PubMed] [Google Scholar]
- 16.Steinborn M, Friedmann M, Hahn H. Normal values for transbulbar sonography and magnetic resonance imaging of the optic nerve sheath diameter (ONSD) in children and adolescents. Ultraschall Med 2015;36:54–8. 10.1055/s-0034-1385012 [DOI] [PubMed] [Google Scholar]
- 17.Helmke K, Hansen HC. Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension II. Patient study. Pediatr Radiol 1996;26:706–10. 10.1007/BF01383384 [DOI] [PubMed] [Google Scholar]
- 18.Watanabe A, Horikoshi T, Uchida M, et al. Decreased diameter of the optic nerve sheath associated with CSF hypovolemia. AJNR Am J Neuroradiol 2008;29:863–4. 10.3174/ajnr.A1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hamilton DR, Sargsyan AE, Melton SL, et al. Sonography for determining the optic nerve sheath diameter with increasing intracranial pressure in a porcine model. J Ultrasound Med 2011;30:651–9. [DOI] [PubMed] [Google Scholar]
- 20.Moretti R, Pizzi B. Optic nerve ultrasound for detection of intracranial hypertension in intracranial hemorrhage patients: confirmation of previous findings in a different patient population. J Neurosurg Anesthesiol 2009;21:16–20. 10.1097/ANA.0b013e318185996a [DOI] [PubMed] [Google Scholar]
- 21.Hansen HC, Lagreze W, Krueger O, et al. Dependence of the optic nerve sheath diameter on acutely applied subarachnoidal pressure—an experimental ultrasound study. Acta Ophthalmol 2011;89:e528–532. 10.1111/j.1755-3768.2011.02159.x [DOI] [PubMed] [Google Scholar]
- 22.Mokri B. Cerebrospinal fluid volume depletion and its emerging clinical/imaging syndromes. Neurosurg Focus 2000;9:e6 10.3171/foc.2000.9.1.6 [DOI] [PubMed] [Google Scholar]
- 23.Mokri B. Headaches caused by decreased intracranial pressure: diagnosis and management. Curr Opin Neurol 2003;16:319–26. 10.1097/00019052-200306000-00011 [DOI] [PubMed] [Google Scholar]
- 24.Mokri B. Low cerebrospinal fluid pressure syndromes. Neurol Clin 2004;22:55–74. 10.1016/S0733-8619(03)00089-6 [DOI] [PubMed] [Google Scholar]
- 25.Mokri B. Spontaneous low cerebrospinal pressure/volume headaches. Curr Neurol Neurosci 2004;4:117–24. 10.1007/s11910-004-0025-5 [DOI] [PubMed] [Google Scholar]
- 26.Mokri B. Spontaneous low pressure, low CSF volume headaches: spontaneous CSF leaks. Headache 2013;53:1034–53. 10.1111/head.12149 [DOI] [PubMed] [Google Scholar]
- 27.Levine DN, Rapalino O. The pathophysiology of lumbar puncture headache. J Neurol Sci 2001;192:1–8. 10.1016/S0022-510X(01)00601-3 [DOI] [PubMed] [Google Scholar]
- 28.Carrie LE. Postdural puncture headache and extradural blood patch. Br J Anaesth 1993;71:179–81. 10.1093/bja/71.2.179 [DOI] [PubMed] [Google Scholar]
- 29.Beck J, Gralla J, Fung C, et al. Spinal cerebrospinal fluid leak as the cause of chronic subdural hematomas in nongeriatric patients. J Neurosurg 2014;121:1380–7. 10.3171/2014.6.JNS14550 [DOI] [PubMed] [Google Scholar]
- 30.Szabo TL. Diagnostic ultrasound imaging: inside out. 2nd edn Academic Press, 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.