Abstract
The temporal discrimination threshold (TDT) is the shortest interstimulus interval at which a subject can perceive successive stimuli as separate. To investigate the effects of aging on TDT, we studied tactile TDT using the method of limits with 120% of sensory threshold in each hand for each of 100 healthy volunteers, equally divided among males and females, across ten age groups, from 18 to 79 years. Linear regression analysis showed that age was significantly related to left hand mean, right hand mean and mean of two hands with R-square equal to 0.08, 0.164 and 0.132, respectively. Reliability analysis indicated that the three measures had fair-to-good reliability (intraclass correlation coefficient: 0.4-0.8). We conclude that TDT is affected by age and has fair-to-good reproducibility using our technique.
Keywords: temporal discrimination threshold, aging, age effects, timing, time perception
1. Introduction
Aging is accompanied by changes in brain physiology. Age-related changes in brain physiology may make individuals more susceptible to disease, influence disease progression or response to treatment. It would be important to study the effects of aging on any diagnostic tool probing brain physiology.
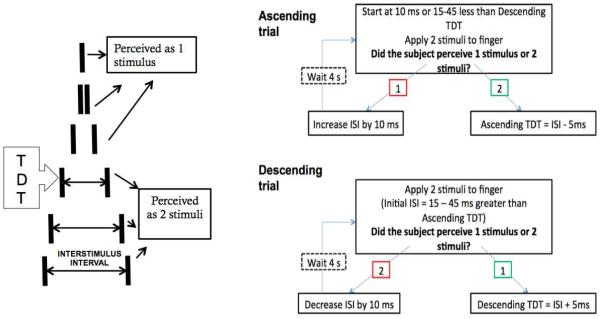
Fundamental to our sense of reality, both internal and external environments, is the experience of time. Temporal discrimination is the ability to detect elapsed time, specifically to perceive sequential stimuli. The temporal discrimination threshold (TDT) is the shortest interstimulus interval at which a subject can perceive successive stimuli as separate (Fig. 1). Stimuli can be tactile, visual or auditory. Elevated values have been described in lesions in internal capsule, posterior parietal cortex lesions, caudate nucleus, putamen, medial thalamus, and lenticular nucleus (Lacruz et al., 1991), cerebellar atrophy (Manganelli et al., 2013), and in Parkinson disease, especially those with PINK1 mutations (Fiorio et al., 2008b), with a single dose of levodopa improving the TDT abnormality (Di Biasio et al., 2015, Lyoo et al., 2012, Conte et al., 2010, Lee et al., 2005, Artieda et al., 1992), while deep brain stimulation is associated with prolonged TDT (Conte et al., 2010). Even higher TDTs, sufficient to differentiate from Parkinson patients, were reported in multiple system atrophy (Rocchi et al., 2013). In dystonia, increased TDT (Conte et al., 2014b, Bradley et al., 2012, Scontrini et al., 2009, Fiorio et al., 2008a, Fiorio et al., 2003, Sanger, et al., 2001, Bara-Jimenez, et al., 2000, Tinazzi et al., 1999) is not only prevalent, but considered to be an endophenotype in autosomal dominant primary torsion dystonia, seen even in unaffected carriers (Kimmich et al., 2011, Bradley et al., 2009, Fiorio et al., 2007). That TDT is highly associated with particular gene mutations has led to interest in developing TDT as a useful tool in performing genetic studies. TDT has been shown to differentiate between dystonic tremor (having elevated TDT) and essential tremor (Tinazzi et al., 2013). It has also been demonstrated to be elevated in isolated head and voice tremors (Conte et al., 2015), psychogenic dystonia (Morgante et al., 2011) and psychogenic tremor (Tinazzi et al., 2014).
Figure 1.
The temporal discrimination threshold (TDT), the shortest interstimulus interval (ISI) that a subject can perceive successive stimuli, is tested using six trials of alternating ascending and descending limits.
Tactile TDT testing holds promise as a clinical probe in that it is easily performed, quick, and generally comfortable. Particularly in dystonia, it is useful because it has been shown to be unaffected by botulinum toxin (Scontrini, et al., 2011) or pallidal stimulation (Sadnicka et al., 2013). However, there is great variety in technique as reported in the literature, there are no clear guidelines on normative values, and reproducibility data are scarce. Furthermore, age effects on tactile TDT are not known. Hoshiyama et al. (2004) studied 80 healthy volunteers from age 18 to 82 and found that TDT increased with age only in subjects older than 65 years. Aging is associated with poorer auditory temporal discrimination (Fostick and Babkoff, 2013, Schneider et al., 2002, Snell and Frisina, 2000), which is believed to play a role in speech perception decline in the elderly.
To investigate the effects of aging on tactile TDT, we studied 100 healthy volunteers from age 18 to 79 years.
2. Materials and methods
2.1 Subjects
One hundred neurologically healthy subjects were recruited in ten age groups of five males and five females each. Age grouping was 18-24, 25-30, 31 – 36, 37-42, 43-49, 50-55, 56-60, 61-66, 67-72, and 73 -79 years old.
None of the subjects had history of any neurologic or psychiatric illness, including neuropathy, tremor, brain tumor, stroke, epilepsy or seizures, major depression or any major mental disorders (axis I disorders according to the Diagnostic and Statistical Manual of Mental Disorders, 4th ed.), had a head injury where there was a loss of consciousness, alcoholism, using illegal drugs, or CNS acting medications. Patients with peripheral sensory neuropathy, tremor or focal neurologic findings documented on clinical exam were excluded. Patients with known or suspected family history of Parkinson disease or dystonia were excluded. Healthy volunteer status was based on interview and examination by neurologists. All subjects gave written informed consent consistent with the Declaration of Helsinki, which was approved by the CNS Institutional review Board of the National Institutes of Health, Bethesda, MD.
2.2 Temporal Discrimination Threshold (TDT) Procedure
Participants were seated in a comfortable chair with their testing hand on a table, palm facing up. All measurements were carried out in a quiet room at a temperature of 21-23 degrees centigrade. Each index finger was wiped clean with alcohol, then scrubbed with abrasive gel and wiped clean. The right index finger was tested before the left index finger for all participants. Prior to each index finger being tested, ring electrodes were placed in the distal and proximal interphalangeal creases with conductive gel, and tightened to a snug fit without causing any discomfort to the participants. The stimulation intensity for testing was set for each person individually at 120% of sensory threshold, defined as the minimum intensity where 10 out of 10 stimuli were perceived by the subject, determined by increasing the intensity of the stimulus from 2mA in increments of 0.2 mA.
Two painless electrical stimuli with varying interstimulus intervals (ISI) were used to determine the TDT of the index finger for each participant. Each stimulus consisted of a square wave pulse of 0.2 ms duration. Each participant was familiarized with the sensation of a single pulse (“one”) using ISI 0 ms, and the sensation of two pulses (“two”) using ISI 300 ms. Participants were informed that the ISI would be varied. Participants were asked to respond verbally by saying either “one” or “two” to indicate the number of pulses they perceived. Pairs of pulses were given at 4-second intervals to allow sufficient wash out period. Each participant’s TDT was determined by the method of limits, with three ascending trials and three descending trials. Each ascending trial was followed by a descending trial for a total of six trials for each index finger. For ascending trials, ISI was increased from 0 ms in increments of 10 ms until two stimuli were perceived, and the ascending TDT was recorded as the smallest 10 ms increment that the subject was able to perceive two stimuli minus 5 ms. For descending trials, the ISI was increased 45 ms beyond the ascending TDT and the ISI was decreased by 10 ms until only one stimulus was perceived. The descending TDT was recorded as the highest 10 ms decrements plus 5 ms. The mean over the six trials was taken as the TDT. The TDT was considered valid when the participant consistently reported two stimuli with an ISI longer than the threshold for ascending trials, and consistently reported one stimulus with an ISI shorter than the threshold for descending trials. For each trial, at least three catch events consisting of an ISI 0 ms are included at random intervals to prevent perseverative responses and catch subject’s attention.
2.3 Reproducibility testing
Sixteen participants were retested following exactly the same protocol at least one week after the first test. No feedback was given from previous testing. Of these sixteen participants, ten were retested again at least one week after the second test.
2.4 Statistical analysis
Linear regression analysis was performed to examine the relationship between age and the following three TDT test outcomes: mean of left hand (L-mean), mean of right hand (R-mean), and mean of two hands (LR-mean). L-mean (or R-mean) was the mean of three ascending TDT and three descending TDT measures from left (or right) hand. LR-mean was the mean of R-mean and L-mean. Gender, handedness, and test stimulus were considered as covariates. The reliability or the reproducibility of TDT measurements was assessed by intraclass correlation coefficient (ICC) using the 16 subjects with test and retest measures. P=0.05 was used as a significance level. All statistics were performed using Statistical Analysis System 9.2 (SAS Institute, Inc, Cary, NC).
3. Results
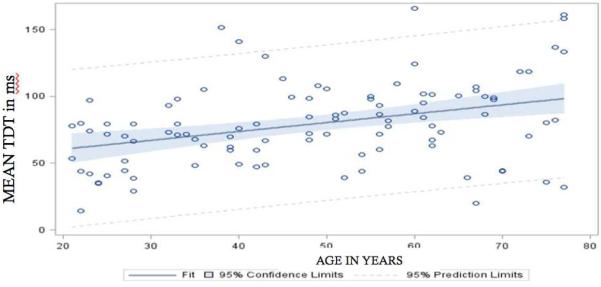
We recruited 100 healthy volunteers, 50% male, 2% Asian, 29% African-American, 69% Caucasian. 5% were Hispanic. 94% were right hand dominant. Repeated measures ANOVA showed no effect of gender, race, ethnicity or handedness on mean TDT. Test stimulus also had no effect on the mean TDT for each hand, and thus was dropped from the model. Linear regression analysis showed that age was significantly related to TDT (Table 1) with a 0.66 ms mean increase for every year increase in age (Figure 2). This yielded an equation for TDT with age correction= 47.28 + 0.66*age. Correction for age also improved standard deviation from 31.14 ms (without age correction) to 11.33 ms (with age correction).
Table 1.
Linear regression analysis showed that age was significantly related to temporal discrimination threshold (TDT).
| TDT measurement |
R-square | Regression coefficient |
|---|---|---|
| RIGHT hand | 0.164 | 0.75 (p<0.0001) |
| LEFT hand | 0.08 | 0.57 (p=0.0039) |
| Mean | 0.132 | 0.66 (p=0.0002) |
Figure 2.
Nomogram showing increasing age correlating with increasing TDT.
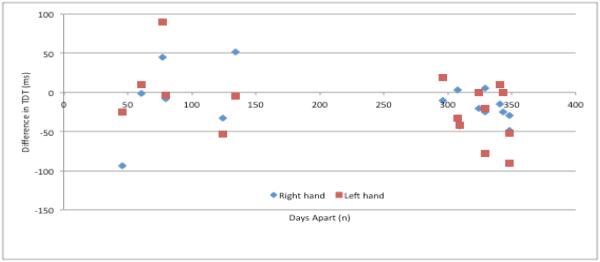
Reliability analysis was performed using the 16 participants with test and re-test measures. ICC was in the range of 0.4 to 0.8 indicating the test-retest reliability was fair-to-good (Table 2). Length of time between tests did not seem to impact TDT reproducibility (Figure 3).
Table 2.
Testing 16 participants twice, and 10 participants thrice showed fair-to-good reliability based on the intra-class correlation coefficient (Fleiss JL, 1986).
| # of subjects |
# of testings |
RIGHT Hand ICC |
LEFT Hand ICC |
RIGHT Hand ICC Minus First trials |
LEFT Hand ICC Minus First Trials |
|---|---|---|---|---|---|
| 16 | 2 | 0.40 | 0.43 | 0.51 | 0.45 |
| 10 | 3 | 0.53 | 0.62 | 0.56 | 0.62 |
Figure 3.
Length of time between testing did not affect TDT reproducibility.
5. Discussion
Our findings show that age affects TDT with a 0.66 ms increase for every year increase in age. This means that an age gap of 10 years has a difference of 6.60 ms, and, with a testing protocol that moves in 10 ms intervals, that it takes an age gap of at least 31 years to effect a two step increase in the TDT. Using this age gap leads to an age grouping similar to that used by Bradley et al., who divided groups by age less than 50, and age 50 years old and above (Bradley, et al., 2009). Their results of mean TDT 22.85 ms with standard deviation of 8.00 ms for healthy volunteers less than 50 years old were much smaller than our study’s mean TDT 71.62 with standard deviation of 29.98. Similarly, for their 50 years old and above healthy volunteers, their mean TDT was 30.87 ms with standard deviation of 5.48 ms, again much smaller than our study’s mean 87.33 with a standard deviation of 34.27. It is not clear why the TDT values from Bradley et al. are so much shorter than ours, but there were methodological differences; they changed their ISIs by 5 ms, while we changed ours by 10 ms, and they used a stimulus intensity of sensory threshold while we used 1.2X sensory threshold. Hoshiyama et al. studied 45 healthy volunteers from 40 to 82 years old, using 1.3 to 1.5X sensory threshold stimulus, with 1 msec ISI changes, and showed that TDT increases with aging only after age 65(Hoshiyama et al., 2004). Their mean TDT for finger measurements was 26.10 ms (range (20 to 44 ms), while for their participants 65 years old and above, mean TDT was 46.50 ms +/− 11.10 ms. With investigators who used a similar change in ISI of 10 ms, we do get similar results with respect to mean TDT and standard deviation (Conte et al., 2014b, Rocchi et al., 2013, Fiorio et al., 2008a).
According to the Scalar Expectancy Theory or the Scalar Timing Theory, the temporal processing system can be broken into three stages: clock, memory, and decision (Gibbon, 1977). In the clock stage, a person’s attention to a to-be-timed signal allows pacemaker pulses to be collected in an accumulator. The pacemaker is an entity that produces timed pulses at a defined rate, while an accumulator is a register used to contain the results of the operation. After some time or accumulated pulses, if the corresponding to-be-timed signal acquires a new form, such as feedback or another signal, then there is transfer of the contents of the accumulator, or the experienced duration, from working to reference or long-term storage memory; this is the memory stage. When the corresponding experienced duration is presented to the accumulator again, there is the decision stage, where a comparator judges the current contents of the accumulator against the reference memory. Variability in timing perception can then be attributed to changes in the function of attention, pacemaker, memory, or decision (for a thorough review, see Allman and Meck, 2012). How these elements may be affected by the aging process leading to prolonged TDT is unclear. Since our experiment is fairly short, ~ 15 to 20 minutes, and we have not observed any differences in reaction times between our participants across the ages, we argue that attention is probably not a crucial factor to explain prolonged TDT with aging. Since we have also shown that TDT measurements using our technique have fair reliability, unaffected by length of time between testings, we also argue that memory or decision stages likely are not the crucial factors. Hence, to the extent that the Scalar Expectancy Theory is correct, we consider the pacemaker as the crucial factor to explain our aging results.
Prolonged TDT in dystonia is likely related to an underlying GABA-ergic mechanism with failure of inhibition (Scontrini et al., 2009). Paired somatosensory evoked potential studies showed that TDT values correlated with P27 suppression at short latency, which is mediated by GABA-ergic mechanism (Tamura et al., 2008). The short intracortical inhibition (SICI) is a measure of inhibitory effects in the motor cortex mediated by GABA-ergic mechanisms, specifically GABA-A (Di Lazzaro et al., 2007), and is abnormally decreased in people with dystonia(Avanzino et al., 2008,Avanzino et al., 2011,Espay et al., 2006, Quartarone et al., 2008,Tokimura et al., 2000). A recent study among 64 healthy volunteers from age 20 to 88 showed that SICI decreases by 1.6% with every year increase in age (Heise et al., 2013). Thus, with increasing age, there is prolonged TDTs and decreased SICI, both of which have underlying GABA-ergic mechanisms, and also both seen in dystonia.
Participants in a duration discrimination task were also found to underestimate comparison intervals with increasing resting state GABA in the visual cortex as measured by magnetic resonance spectroscopy (Terhune et al., 2014). Increased GABA, also evidenced by magnetic resonance spectroscopy, in the sensorimotor cortex was correlated with improved discrimination using vibrotactile tasks in 16 healthy volunteers (Puts, et al., 2011). Thus a decrease in GABA could explain an abnormal TDT.
GABA-ergic interneurons are lost in ageing so indeed may explain functional deficits (Lehmann et al., 2012). More evidence for a GABA deficit is that Mora et al., based on rat brain microdialysis studies, showed that dopamine and GABA release in the nucleus accumbens is decreased during aging (Mora et al., 2008).
That we are able to detect direct age effects on tactile TDT may be argued to be a result of cognitive changes, but we do not think this the explanation. Though we did not perform intensive cognitive testing on our subjects, none showed any cognitive deficits in orientation, three object five-minute recall, spelling WORLD backwards, and naming. Additionally, with another sensory modality, even after controlling for cognitive functioning, Fostick and Babkoff (2013) found a significant decrease in auditory temporal gap resolution, including gap detection, with aging. They found a linear decline in accuracy of auditory gap detection with aging among 89 participants 21 to 82 years old (y=0.0014x + 0.7912, R2=0.0617).
TDT testing is a psychometric test that is inherently subjective. The reproducibility values that we have shown in this study lend to the credibility of the testing procedure. Tactile TDT was deemed a consistent measure among patients with psychogenic dystonia because of high interrater reliability for two blinded examiners with an ICC value > 0.9 for healthy volunteers and because of similar values obtained when testing psychogenic dystonia patients twice (Morgante et al., 2011). As mentioned prior, Tamura et al. showed that TDT threshold values correlated with P27 suppression in somatosensory evoked potential studies in healthy volunteers and patients with focal hand dystonia (Tamura et al., 2008). This finding also localizes TDT abnormalities at the primary somatosensory area (S1). Plasticity inducing protocols using transcranial magnetic stimulation with continuous theta burst stimulation on S1 increased TDT values, while intermittent theta burst stimulation decreased TDT values (Conte et al., 2014a, Conte et al., 2012).
Since S1 plays a major role in TDT performance, we need to know how it is affected by aging if we are to understand age effects in TDT. Comparing 16 healthy volunteers aged 26 +/− 0.8 years and 16 healthy volunteers 62 +/− 1.5 years, the N20-P25 complex had a more marked increase in amplitude after paired associative stimulation (Pellicciari, et al., 2009), an established technique to study brain plasticity. Pellicciari et al. further plotted their subjects ages with the ratios of the amplitudes of N20-P25post/pre-paired associative stimulation, and their results suggested a linear relationship between aging and paired associative stimulation changes in the elderly (r =0.48, P=0.06) but not in the young subjects (r=0.18, P=0.51)(Pellicciari, et al., 2009). S1 was thus found to have increased plasticity in the elderly. We note that the evidence pointing to decreased plasticity in aging is far more robust, however this exceptional increased S1 plasticity in aging may be explained by differential loss of GABA-ergic inhibitory interneurons (Lehmann et al., 2012) as mentioned previously. GABA-ergic postsynaptic activity is necessary for synaptic plasticity (McDonnell, et al., 2006). Further, increased TDT associated with increased S1 plasticity with aging also correlates with increased plasticity in dystonia (Quartarone and Pisani 2011, Hallett, 1998), a disorder strongly associated with increased TDT.
An fMRI study in 14 healthy volunteers showed that during temporal discrimination tasks, increased activation is found in the pre-supplementary motor area and the anterior cingulate gyri (Pastor et al., 2004), regions anterior to S1. Differences in fMRI results might perhaps be due to differences in testing methodology, where in the Pastor et al. study, a random series of paired stimuli with ISIs between 5 and 140 msec was presented, whereas in the other studies, including this one, ISIs were presented in an ascending or descending manner.
Using [18F]-N-3-fluoropropyl-2-beta-carboxymethoxy-3-beta-(4-iodophenyl) nortropane positron emission tomography studies measuring caudate and putaminal dopamine transporter uptake levels, Lyoo et al. showed that nigrostriatal dopamine deficiency is significantly associated with prolonged TDT (Lyoo et al., 2012). Several studies have also established that dopamine replacement corrects prolonged TDTs. Age-related prolonged TDT values might be due in part to the age related decline in dopamine levels (Gaspar, et al., 1991), especially in cortical regions (Inoue et al., 2001). Also tying up nicely with the hypothesis that increased S1 plasticity in aging may explain increased TDT values is that levodopa directly affects cortical plasticity, albeit studies are in M1, a region associated with decreased plasticity in the elderly (Kishore et al., 2014, Thirugnanasambandam, et al., 2011, Rogasch et al., 2009). Age-related decline in dopaminergic transmission, while associated with diminished M1 plasticity, may be associated, whether as compensatory effect or epiphenomena, with increased S1 plasticity, which is then observed as increased TDT values in the elderly. Caution is necessary in considering this hypothesis, as mechanisms underlying age-related changes in TDT, S1 plasticity, M1 plasticity and levodopa effects are still unclear and merit further research.
We acknowledge the limitation of our study in that minor subclinical peripheral neuropathy related to aging could not be excluded. Presumably, we compensated for this anyway by utilizing a testing intensity of 120% of individual sensory threshold. In analyzing our results, we found no effect of the intensity of the test stimulus used with the TDT, or a correlation between age and test stimulus intensity. At least in Parkinson disease patients, it has been shown that median nerve and cortical somatosensory evoked potential N20-P25 recovery curves after double electrical stimulation are normal, such that elevated TDT is unlikely to be due to failure of sensory transmission (Artieda et al., 1992). Also, our results need to be interpreted in the context of the technique used, that is, smaller increments or decrements of ISIs may yield more sensitive changes with respect to aging. However, we argue that our main purpose to investigate the effects of aging in TDT is to develop TDT as a convenient diagnostic tool for clinical use. In that case, it was to our interest to keep testing protocols efficient and nontedious. We note that low R squares are problematic in making precise predictions, but that we can still draw important conclusions about how changes in age are associated with changes in TDT. It is unclear how subtle age-effects on TDT is clinically relevant, but it needs to be considered in research work with TDT. That age effects are quite subtle may in fact favor the utility of TDT as a diagnostic test for various neurologic conditions that are more prevalent in the elderly. Lastly, we acknowledge that the mechanism underlying age-effects on TDT is likely multifactorial.
6. Conclusions
We confirm previous findings that age affects TDT. Our data show that for every year increase in age, there is a 0.66 ms increase in TDT. Furthermore, we show that TDT has fair-to-good reproducibility using our testing protocol, which is convenient, quick and lends itself easily to clinical testing. We do highlight that caution and clinical correlation is necessary in interpreting results.
Temporal discrimination threshold (TDT) is the ability to detect elapsed time
TDT is increased 0.66 ms per year increase in age
TDT testing has fair-to-good reliability on repeat testing
Acknowledgments
Dr. Ramos received research support from BCN peptides, and was supported by a fellowship grant from the Dystonia Medical Research Foundation.
Dr. Hallett serves as Chair of the Medical Advisory Board for and receives honoraria and funding for travel from the Neurotoxin Institute. He may accrue revenue on US Patent #6,780,413 B2 (Issued: August 24, 2004): Immunotoxin (MAB-Ricin) for the treatment of focal movement disorders, and US Patent #7,407,478 (Issued: August 5, 2008): Coil for Magnetic Stimulation and methods for using the same (H-coil); in relation to the latter, he has received license fee payments from the NIH (from Brainsway) for licensing of this patent. He is on the Editorial Board of 20 journals, and received royalties and/or honoraria from publishing from Cambridge University Press, Oxford University Press, John Wiley & Sons, Wolters Kluwer, Springer, and Elsevier. He has received honoraria for lecturing from Columbia University. Dr. Hallett's research at the NIH is largely supported by the NIH Intramural Program. Supplemental research funds have been granted by BCN Peptides, S.A. for treatment studies of blepharospasm, Medtronics, Inc., for studies of deep brain stimulation, Parkinson Alliance for studies of eye movements in Parkinson’s disease, UniQure for a clinical trial of AAV2-GDNF for Parkinson Disease, Merz for treatment studies of focal hand dystonia, and Allergan for studies of methods to inject botulinum toxins.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
Alina Esquenazi reports no disclosures.
Monica Villegas reports no disclosures.
Dr. Wu reports no disclosures.
All authors completed this work as part of their official duties as employees of the US Federal Government: Department of Health and Human Services, National Institutes of Health.
References
- Allman MJ, Meck WH. Pathophysiological distortions in time perception and timed performance. Brain. 2012;135:656–77. doi: 10.1093/brain/awr210. Pt 3. doi:10.1093/brain/awr210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artieda J, Pastor MA, Lacruz F, Obeso JA. Temporal discrimination is abnormal in Parkinson's disease. Brain. 1992;115:199–210. doi: 10.1093/brain/115.1.199. Pt 1. [DOI] [PubMed] [Google Scholar]
- Avanzino L, Martino D, van de Warrenburg BP, Schneider SA, Abbruzzese G, Defazio G, Schrag A, Bhatia KP, Rothwell JC. Cortical excitability is abnormal in patients with the "fixed dystonia" syndrome. Mov Disord. 2008;23(5):646–52. doi: 10.1002/mds.21801. doi:10.1002/mds.21801. [DOI] [PubMed] [Google Scholar]
- Avanzino L, Tacchino A, Abbruzzese G, Quartarone A, Ghilardi MF, Bonzano L, Ruggeri P, Bove M. Recovery of motor performance deterioration induced by a demanding finger motor task does not follow cortical excitability dynamics. Neuroscience. 2011;174:84–90. doi: 10.1016/j.neuroscience.2010.11.008. doi:10.1016/j.neuroscience.2010.11.008. [DOI] [PubMed] [Google Scholar]
- Bara-Jimenez W, Shelton P, Sanger TD, Hallett M. Sensory discrimination capabilities in patients with focal hand dystonia. Ann Neurol. 2000;47(3):377–80. [PubMed] [Google Scholar]
- Bradley D, Whelan R, Kimmich O, O'Riordan S, Mulrooney N, Brady P, Walsh R, Reilly RB, Hutchinson S, Molloy F, Hutchinson M. Temporal discrimination thresholds in adult-onset primary torsion dystonia: an analysis by task type and by dystonia phenotype. J Neurol. 2012;259(1):77–82. doi: 10.1007/s00415-011-6125-7. doi:10.1007/s00415-011-6125-7. [DOI] [PubMed] [Google Scholar]
- Bradley D, Whelan R, Walsh R, Reilly RB, Hutchinson S, Molloy F, Hutchinson M. Temporal discrimination threshold: VBM evidence for an endophenotype in adult onset primary torsion dystonia. Brain. 2009;132:2327–35. doi: 10.1093/brain/awp156. Pt 9. doi:10.1093/brain/awp156. [DOI] [PubMed] [Google Scholar]
- Conte A, Ferrazzano G, Manzo N, Leodori G, Fabbrini G, Fasano A, Tinazzi M, Berardelli A. Somatosensory temporal discrimination in essential tremor and isolated head and voice tremors. Mov Disord. 2015;30(6):822–7. doi: 10.1002/mds.26163. doi:10.1002/mds.26163. [DOI] [PubMed] [Google Scholar]
- Conte A, Modugno N, Lena F, Dispenza S, Gandolfi B, Iezzi E, Fabbrini G, Berardelli A. Subthalamic nucleus stimulation and somatosensory temporal discrimination in Parkinson's disease. Brain. 2010;133(9):2656–63. doi: 10.1093/brain/awq191. doi:10.1093/brain/awq191. [DOI] [PubMed] [Google Scholar]
- Conte A, Rocchi L, Ferrazzano G, Leodori G, Bologna M, Li Voti P, Nardella A, Berardelli A. Primary somatosensory cortical plasticity and tactile temporal discrimination in focal hand dystonia. Clin Neurophysiol. 2014a;125(3):537–43. doi: 10.1016/j.clinph.2013.08.006. doi:10.1016/j.clinph.2013.08.006. [DOI] [PubMed] [Google Scholar]
- Conte A, Rocchi L, Nardella A, Dispenza S, Scontrini A, Khan N, Berardelli A. Theta-burst stimulation-induced plasticity over primary somatosensory cortex changes somatosensory temporal discrimination in healthy humans. PLoS One. 2012;7(3):e32979. doi: 10.1371/journal.pone.0032979. doi:10.1371/journal.pone.0032979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Biasio F, Conte A, Bologna M, Iezzi E, Rocchi L, Modugno N, Berardelli A. Does the cerebellum intervene in the abnormal somatosensory temporal discrimination in Parkinson's disease? Parkinsonism Relat Disord. 2015 doi: 10.1016/j.parkreldis.2015.04.004. doi:10.1016/j.parkreldis.2015.04.004. [DOI] [PubMed] [Google Scholar]
- Di Lazzaro V, Pilato F, Dileone M, Profice P, Ranieri F, Ricci V, Bria P, Tonali PA, Ziemann U. Segregating two inhibitory circuits in human motor cortex at the level of GABAA receptor subtypes: a TMS study. Clin Neurophysiol. 2007;118(10):2207–14. doi: 10.1016/j.clinph.2007.07.005. doi:10.1016/j.clinph.2007.07.005. [DOI] [PubMed] [Google Scholar]
- Espay AJ, Morgante F, Purzner J, Gunraj CA, Lang AE, Chen R. Cortical and spinal abnormalities in psychogenic dystonia. Ann Neurol. 2006;59(5):825–34. doi: 10.1002/ana.20837. doi:10.1002/ana.20837. [DOI] [PubMed] [Google Scholar]
- Fiorio M, Gambarin M, Valente EM, Liberini P, Loi M, Cossu G, Moretto G, Bhatia KP, Defazio G, Aglioti SM, Fiaschi A, Tinazzi M. Defective temporal processing of sensory stimuli in DYT1 mutation carriers: a new endophenotype of dystonia? Brain. 2007;130(1):134–42. doi: 10.1093/brain/awl283. doi:10.1093/brain/awl283. [DOI] [PubMed] [Google Scholar]
- Fiorio M, Tinazzi M, Bertolasi L, Aglioti SM. Temporal processing of visuotactile and tactile stimuli in writer's cramp. Ann Neurol. 2003;53(5):630–5. doi: 10.1002/ana.10525. doi:10.1002/ana.10525. [DOI] [PubMed] [Google Scholar]
- Fiorio M, Tinazzi M, Scontrini A, Stanzani C, Gambarin M, Fiaschi A, Moretto G, Fabbrini G, Berardelli A. Tactile temporal discrimination in patients with blepharospasm. J Neurol Neurosurg Psychiatry. 2008a;79(7):796–8. doi: 10.1136/jnnp.2007.131524. doi:10.1136/jnnp.2007.131524. [DOI] [PubMed] [Google Scholar]
- Fiorio M, Valente EM, Gambarin M, Bentivoglio AR, Ialongo T, Albanese A, Barone P, Pellecchia MT, Brancati F, Moretto G, Fiaschi A, Tinazzi M. Subclinical sensory abnormalities in unaffected PINK1 heterozygotes. J Neurol. 2008b;255(9):1372–7. doi: 10.1007/s00415-008-0923-6. doi:10.1007/s00415-008-0923-6. [DOI] [PubMed] [Google Scholar]
- Fleiss JL. Reliability of measurement. In: Fleiss JL, editor. The design and analysis of clinical experiments. John Wiley & Sons; New York: 1986. pp. 2–31. [Google Scholar]
- Fostick L, Babkoff H. Temporal and non-temporal processes in the elderly. Journal of basic and clinical physiology and pharmacology. 2013;24(3):191–9. doi: 10.1515/jbcpp-2013-0049. doi:10.1515/jbcpp-2013-0049. [DOI] [PubMed] [Google Scholar]
- Gaspar P, Duyckaerts C, Alvarez C, Javoy-Agid F, Berger B. Alterations of dopaminergic and noradrenergic innervations in motor cortex in Parkinson's disease. Ann Neurol. 1991;30(3):365–74. doi: 10.1002/ana.410300308. doi:10.1002/ana.410300308. [DOI] [PubMed] [Google Scholar]
- Gibbon J. Scalar Expectancy-Theory and Webers Law in Animal Timing. Psychol Rev. 1977;84(3):279–325. doi:Doi 10.1037//0033-295x.84.3.279. [Google Scholar]
- Hallett M. The neurophysiology of dystonia. Archives of Neurology. 1998;55(5):601. doi: 10.1001/archneur.55.5.601. [DOI] [PubMed] [Google Scholar]
- Heise KF, Zimerman M, Hoppe J, Gerloff C, Wegscheider K, Hummel FC. The aging motor system as a model for plastic changes of GABA-mediated intracortical inhibition and their behavioral relevance. J Neurosci. 2013;33(21):9039–49. doi: 10.1523/JNEUROSCI.4094-12.2013. doi:10.1523/JNEUROSCI.4094-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoshiyama M, Kakigi R, Tamura Y. Temporal discrimination threshold on various parts of the body. Muscle Nerve. 2004;29(2):243–7. doi: 10.1002/mus.10532. doi:10.1002/mus.10532. [DOI] [PubMed] [Google Scholar]
- Inoue M, Suhara T, Sudo Y, Okubo Y, Yasuno F, Kishimoto T, Yoshikawa K, Tanada S. Age-related reduction of extrastriatal dopamine D2 receptor measured by PET. Life sciences. 2001;69(9):1079–84. doi: 10.1016/s0024-3205(01)01205-x. [DOI] [PubMed] [Google Scholar]
- Kimmich O, Bradley D, Whelan R, Mulrooney N, Reilly RB, Hutchinson S, O'Riordan S, Hutchinson M. Sporadic adult onset primary torsion dystonia is a genetic disorder by the temporal discrimination test. Brain. 2011;134:2656–63. doi: 10.1093/brain/awr194. Pt 9. doi:10.1093/brain/awr194. [DOI] [PubMed] [Google Scholar]
- Kishore A, Popa T, James P, Yahia-Cherif L, Backer F, Varughese Chacko L, Govind P, Pradeep S, Meunier S. Age-related decline in the responsiveness of motor cortex to plastic forces reverses with levodopa or cerebellar stimulation. Neurobiol Aging. 2014;35(11):2541–51. doi: 10.1016/j.neurobiolaging.2014.05.004. doi:10.1016/j.neurobiolaging.2014.05.004. [DOI] [PubMed] [Google Scholar]
- Lacruz F, Artieda J, Pastor MA, Obeso JA. The anatomical basis of somaesthetic temporal discrimination in humans. J Neurol Neurosurg Psychiatry. 1991;54(12):1077–81. doi: 10.1136/jnnp.54.12.1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MS, Kim HS, Lyoo CH. "Off" gait freezing and temporal discrimination threshold in patients with Parkinson disease. Neurology. 2005;64(4):670–4. doi: 10.1212/01.WNL.0000151961.14861.BA. doi:10.1212/01.WNL.0000151961.14861.BA. [DOI] [PubMed] [Google Scholar]
- Lehmann K, Steinecke A, Bolz J. GABA through the ages: regulation of cortical function and plasticity by inhibitory interneurons. Neural plasticity. 2012;2012:892784. doi: 10.1155/2012/892784. doi:10.1155/2012/892784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyoo CH, Ryu YH, Lee MJ, Lee MS. Striatal dopamine loss and discriminative sensory dysfunction in Parkinson's disease. Acta Neurol Scand. 2012;126(5):344–9. doi: 10.1111/j.1600-0404.2012.01657.x. doi:10.1111/j.1600-0404.2012.01657.x. [DOI] [PubMed] [Google Scholar]
- Manganelli F, Dubbioso R, Pisciotta C, Antenora A, Nolano M, De Michele G, Filla A, Berardelli A, Santoro L. Somatosensory temporal discrimination threshold is increased in patients with cerebellar atrophy. Cerebellum. 2013;12(4):456–9. doi: 10.1007/s12311-012-0435-x. doi:10.1007/s12311-012-0435-x. [DOI] [PubMed] [Google Scholar]
- McDonnell MN, Orekhov Y, Ziemann U. The role of GABA(B) receptors in intracortical inhibition in the human motor cortex. Exp Brain Res. 2006;173(1):86–93. doi: 10.1007/s00221-006-0365-2. doi:10.1007/s00221-006-0365-2. [DOI] [PubMed] [Google Scholar]
- Mora F, Segovia G, Del Arco A. Glutamate-dopamine-GABA interactions in the aging basal ganglia. Brain research reviews. 2008;58(2):340–53. doi: 10.1016/j.brainresrev.2007.10.006. doi:10.1016/j.brainresrev.2007.10.006. [DOI] [PubMed] [Google Scholar]
- Morgante F, Tinazzi M, Squintani G, Martino D, Defazio G, Romito L, Albanese A, Di Matteo A, Quartarone A, Girlanda P, Fiorio M, Berardelli A. Abnormal tactile temporal discrimination in psychogenic dystonia. Neurology. 2011;77(12):1191–7. doi: 10.1212/WNL.0b013e31822f0449. doi:10.1212/WNL.0b013e31822f0449. [DOI] [PubMed] [Google Scholar]
- Pastor MA, Day BL, Macaluso E, Friston KJ, Frackowiak RS. The functional neuroanatomy of temporal discrimination. J Neurosci. 2004;24(10):2585–91. doi: 10.1523/JNEUROSCI.4210-03.2004. doi:10.1523/JNEUROSCI.4210-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellicciari MC, Miniussi C, Rossini PM, De Gennaro L. Increased cortical plasticity in the elderly: changes in the somatosensory cortex after paired associative stimulation. Neuroscience. 2009;163(1):266–76. doi: 10.1016/j.neuroscience.2009.06.013. doi:10.1016/j.neuroscience.2009.06.013. [DOI] [PubMed] [Google Scholar]
- Puts NA, Edden RA, Evans CJ, McGlone F, McGonigle DJ. Regionally specific human GABA concentration correlates with tactile discrimination thresholds. J Neurosci. 2011;31(46):16556–60. doi: 10.1523/JNEUROSCI.4489-11.2011. doi:10.1523/JNEUROSCI.4489-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quartarone A, Morgante F, Sant'angelo A, Rizzo V, Bagnato S, Terranova C, Siebner HR, Berardelli A, Girlanda P. Abnormal plasticity of sensorimotor circuits extends beyond the affected body part in focal dystonia. J Neurol Neurosurg Psychiatry. 2008;79(9):985–90. doi: 10.1136/jnnp.2007.121632. doi:10.1136/jnnp.2007.121632. [DOI] [PubMed] [Google Scholar]
- Quartarone A, Pisani A. Abnormal plasticity in dystonia: disruption of synaptic homeostasis. Neurobiol Dis. 2011;42(2):162–70. doi: 10.1016/j.nbd.2010.12.011. [DOI] [PubMed] [Google Scholar]
- Rocchi L, Conte A, Nardella A, Li Voti P, Di Biasio F, Leodori G, Fabbrini G, Berardelli A. Somatosensory temporal discrimination threshold may help to differentiate patients with multiple system atrophy from patients with Parkinson's disease. Eur J Neurol. 2013;20(4):714–9. doi: 10.1111/ene.12059. doi:10.1111/ene.12059. [DOI] [PubMed] [Google Scholar]
- Rogasch NC, Dartnall TJ, Cirillo J, Nordstrom MA, Semmler JG. Corticomotor plasticity and learning of a ballistic thumb training task are diminished in older adults. J Appl Physiol (1985) 2009;107(6):1874–83. doi: 10.1152/japplphysiol.00443.2009. doi:10.1152/japplphysiol.00443.2009. [DOI] [PubMed] [Google Scholar]
- Sadnicka A, Kimmich O, Pisarek C, Ruge D, Galea J, Kassavetis P, Parees I, Saifee T, Molloy A, Bradley D, O'Riordan S, Zrinzo L, Hariz M, Bhatia KP, Limousin P, Foltynie T, Rothwell JC, Hutchinson M, Edwards MJ. Pallidal stimulation for cervical dystonia does not correct abnormal temporal discrimination. Mov Disord. 2013 doi: 10.1002/mds.25581. doi:10.1002/mds.25581. [DOI] [PubMed] [Google Scholar]
- Sanger TD, Tarsy D, Pascual-Leone A. Abnormalities of spatial and temporal sensory discrimination in writer's cramp. Mov Disord. 2001;16(1):94–9. doi: 10.1002/1531-8257(200101)16:1<94::aid-mds1020>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Schneider BA, Daneman M, Pichora-Fuller MK. Listening in aging adults: from discourse comprehension to psychoacoustics. Canadian journal of experimental psychology = Revue canadienne de psychologie experimentale. 2002;56(3):139–52. doi: 10.1037/h0087392. [DOI] [PubMed] [Google Scholar]
- Scontrini A, Conte A, Defazio G, Fiorio M, Fabbrini G, Suppa A, Tinazzi M, Berardelli A. Somatosensory temporal discrimination in patients with primary focal dystonia. J Neurol Neurosurg Psychiatry. 2009;80(12):1315–9. doi: 10.1136/jnnp.2009.178236. doi:10.1136/jnnp.2009.178236. [DOI] [PubMed] [Google Scholar]
- Scontrini A, Conte A, Fabbrini G, Colosimo C, Di Stasio F, Ferrazzano G, Berardelli A. Somatosensory temporal discrimination tested in patients receiving botulinum toxin injection for cervical dystonia. Mov Disord. 2011;26(4):742–6. doi: 10.1002/mds.23447. doi:10.1002/mds.23447. [DOI] [PubMed] [Google Scholar]
- Snell KB, Frisina DR. Relationships among age-related differences in gap detection and word recognition. The Journal of the Acoustical Society of America. 2000;107(3):1615–26. doi: 10.1121/1.428446. [DOI] [PubMed] [Google Scholar]
- Tamura Y, Matsuhashi M, Lin P, Ou B, Vorbach S, Kakigi R, Hallett M. Impaired intracortical inhibition in the primary somatosensory cortex in focal hand dystonia. Mov Disord. 2008;23(4):558–65. doi: 10.1002/mds.21870. doi:10.1002/mds.21870. [DOI] [PubMed] [Google Scholar]
- Terhune DB, Russo S, Near J, Stagg CJ, Cohen Kadosh R. GABA Predicts Time Perception. J Neurosci. 2014;34(12):4364–70. doi: 10.1523/JNEUROSCI.3972-13.2014. doi:10.1523/JNEUROSCI.3972-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thirugnanasambandam N, Grundey J, Paulus W, Nitsche MA. Dose-dependent nonlinear effect of L-DOPA on paired associative stimulation-induced neuroplasticity in humans. J Neurosci. 2011;31(14):5294–9. doi: 10.1523/JNEUROSCI.6258-10.2011. doi:10.1523/JNEUROSCI.6258-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinazzi M, Fasano A, Di Matteo A, Conte A, Bove F, Bovi T, Peretti A, Defazio G, Fiorio M, Berardelli A. Temporal discrimination in patients with dystonia and tremor and patients with essential tremor. Neurology. 2013;80(1):76–84. doi: 10.1212/WNL.0b013e31827b1a54. doi:10.1212/WNL.0b013e31827b1a54. [DOI] [PubMed] [Google Scholar]
- Tinazzi M, Fasano A, Peretti A, Bove F, Conte A, Dall'Occhio C, Arbasino C, Defazio G, Fiorio M, Berardelli A. Tactile and proprioceptive temporal discrimination are impaired in functional tremor. PLoS One. 2014;9(7):e102328. doi: 10.1371/journal.pone.0102328. doi:10.1371/journal.pone.0102328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinazzi M, Frasson E, Bertolasi L, Fiaschi A, Aglioti S. Temporal discrimination of somesthetic stimuli is impaired in dystonic patients. Neuroreport. 1999;10(7):1547–50. doi: 10.1097/00001756-199905140-00028. [DOI] [PubMed] [Google Scholar]
- Tokimura H, Di Lazzaro V, Tokimura Y, Oliviero A, Profice P, Insola A, Mazzone P, Tonali P, Rothwell JC. Short latency inhibition of human hand motor cortex by somatosensory input from the hand. J Physiol. 2000;523:503–13. doi: 10.1111/j.1469-7793.2000.t01-1-00503.x. Pt 2. [DOI] [PMC free article] [PubMed] [Google Scholar]