Abstract
Plication procedures for the correction of Peyronie’s disease (PD) curvature are management options for PD patients. There are basically three types of procedures: excisional corporoplasty, incisional corporoplasty, and plication-only. This review is a compilation of English literature, peer-reviewed, published articles addressing these types of operations for Peyronie’s curvature correction, not congenital curvature. According to the urology literature, this surgical type was initially used for correction of curvature associated with hypospadias repair or congenital penile curvature. The procedures also, for the most part, historically became an alternative for plaque excision and graft repair, because of the difficulty with such repairs and the often-resultant erectile dysfunction (ED). A brief section traces some of the origins of these various repairs, followed by a brief section on the selection criteria for these types of surgery for the patient with PD penile curvature. We also review the significant articles in which the three types were presented with modifications. Finally, several articles that compare the various surgical repairs are summarized in the order that they appear in the literature. These types of surgery have become a mainstay for the surgical correction of penile curvature due to PD.
Keywords: Peyronie’s disease management, surgical correction for Peyronie’s disease, excisional corporoplasty, incisional corporoplasty, plication procedures for Peyronie’s disease
History of plication type repair for Peyronie’s disease (PD)
In 1965, Nesbit described a repair of congenital curvature of the penis in which elliptical wedges of tissue were removed opposite the curvature in three patients (1). In the first patient, a plication procedure using a series of silk sutures had failed after 6 months, leading to a second operation in which ellipses of tunica albuginea were made. Pryor and Fitzpatrick, in 1979, reported, essentially, the Nesbit procedure as a new approach to penile deformity correction in patients with PD (2). They used this procedure in 23 patients, and saw one recurrence after 3 months due to the use of an absorbable suture. Of 19 patients, who had poor erections before surgery, 16 reported return of function. The time of follow-up was not stated in the article.
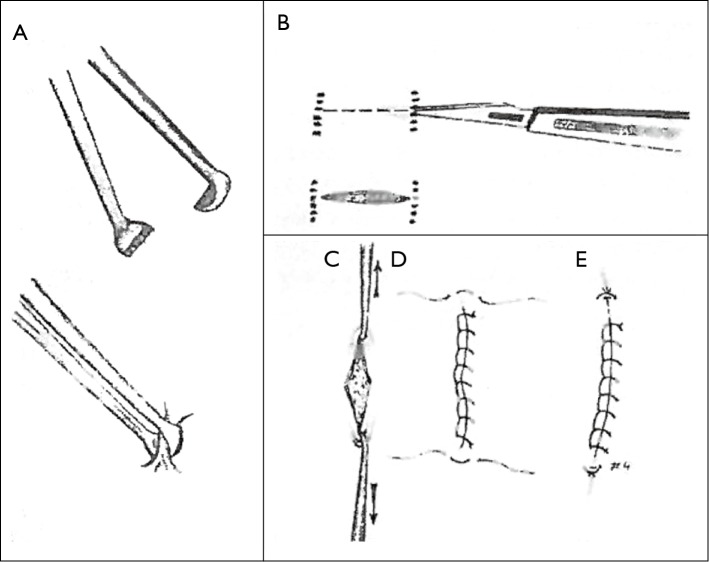
In a 1973 Journal of Urology article, Saalfeld et al. reported modifications in corporoplasty for congenital ventral curvature of the penis from an operation in one patient consisting of a vertical incision opposite the plaque with a horizontal closure, essentially a Heineke-Mikulicz repair (3). Yachia reported in 1990 on his particular modification of the Heineke-Mikulicz repair in penile deformity surgery in ten patients (4) (Figure 1). It is interesting that Yachia originally reported his type of repair in patients with congenital curvature of the penis, as did Nesbit. Licht and Lewis, in 1997, reported on a minor modification of the Yachia procedure (5).
Figure 1.
Significant parts of the original Yachia procedure. (A) Use of Allis clamps to premark the area of longitudinal incision; (B) the incision; (C) use of small skin hooks to convert the incision for horizontal closure; (D) closure complete; and (E) tucking sutures to smooth out edges of the repair [Reprinted with permission (4)].
Early plication procedures that avoided tunica albuginea incisions were reported by Essed and Schroeder (6) and by Ebbehøj and Metz in 1985 (7). In the former report, a simple plication procedure to correct penile curvature using non-absorbable suture was reported in five patients. In the latter report, 25 patients were corrected by a series of one to four double crossover 2–0 prolene sutures (selected when thinner suture failed). None reported penile shortening or erectile dysfunction (ED). Midline penile incisions were made after administration of local penile anesthetic blocks, and an erection was induced with a roller pump during surgery. In 1991, Knispel et al. modified the Essed-Schroeder technique by inverting the plication suture knots (8). Donatucci and Lue in 1992 reported on six patients, using various incisional approaches and a papaverine-induced erection, a series of plication procedures using 1–0 Ticron or Tavdec to correct penile curvature (9). Follow-up ranged from 12 to 24 months.
Indications and informed consent for plication type procedures for correction of PD penile curvature
The indications for surgery for PD penile curvature have been stated in several publications, including a surgical algorithm (10-13). The 2010 document by Ralph et al. is from the PD consensus panel held in Paris in 2010 (12). The latest document from the Madrid international consensus conference in 2015 has not been published yet. Basically for the surgery approach, the patient must be beyond the active inflammatory state, which usually means plaque and deformity have been present for 12 months, there is no pain in penis at rest, and there is no active continuing worsening of the plaque or curvature. The degree of curvature should impede adequate sexual penetration. In the 1997 surgical algorithm paper, the indication for plication procedures were subjective full erectile capacity or objective full erection following penile injection with a vasoactive agent, simple curvature less than 60 degrees, and no hourglass or hinge effect (10). The authors in this 1997 article do not recommend plication procedures for those with complex bi-directional curvature. The consensus panel in 2010 also recommended surgery for patients with extensive plaque calcification (12). The panel also recommends surgical approach for patients who want the most rapid and reliable result. Kadioglu et al. modified the 12-month recommendation with the presence of a stable plaque for 3 months (11).
In the 2012 Mobley et al. review, the published indications for plication procedures included patients with adequate potency, rigidity, penile length (>13 cm), predicted postoperative length loss of less than 20%, and penile curvature less than 60 degrees (13). They state that, at their institution, it was their belief that patients with more extensive curvature approaching 90 degrees, and even in those with hourglass or wasp waist deformity, were still candidates for plication procedures. At our institution we would offer the Yachia procedure (which is our preferred surgical plication procedure) in those with curvatures greater than 60 degrees, but do not recommend this procedure to patients with short penises nor those with hourglass deformities. Distal dorsal hinging just below the glans producing extreme difficulty in intromission also do very well from our modification of the Yachia procedure. Also, the senior author of this chapter disagrees with the concept that plication procedures are the only shortening procedures. In this author’s long-time experience with penile surgery including plaque excision or incision with grafting, placement of penile prostheses with or without PD, and revascularization surgery, the patient will often complain of significant penile shortening. Therefore we have chosen in this chapter to entitle these procedures as plication surgery with subdivision into excisional and incisional corporoplasty procedures or plication without incision procedures. We certainly do not agree that the plaque excision with grafting procedures be considered penile lengthening procedures.
Patients who present for surgery for PD should have a thorough history and genitourinary physical examination. We routinely perform vasoactive penile duplex Doppler ultrasound examinations on each patient who will undergo surgery for PD at our institution in order to access the plaque, the penile vasculature, and the nature of the deviation of the penis (degree deformity and direction of the curvature) when erect due to the plaque. Patients will also occasionally bring with them a photo of their deviation of the penis with erection. However, we still want to observe the full nature of the deviation in our clinic setting, which we do on the day of the Doppler ultrasound study. For those who do not have access to penile Doppler ultrasound the use of an office vasoactive agent injection to produce an erection is also acceptable. Stretched penile length measurements are also recommended. Some have mentioned using vacuum devices to access the curvature, but this is usually less than optimal.
For those patients choosing penile plication procedures the informed consent should include the following: possible penile shortening due to the nature of the surgery, recurrent curvature of greater than 20 degrees, some loss of penile sensation (often temporary if circumcision incision is used), ability to palpate or have pain from permanent suture knots (particularly in plication only procedures), diminished rigidity with erection and, rarely, ED secondary to the surgery. See the discussion below for reported incidences of these sequelae of peer reviewed published plication procedures.
Excisional corporoplasty and Heineke-Mikulicz procedures and modifications
As mentioned previously in the chapter, Nesbit, in 1965, was the first to describe his version of incisional corporoplasty where ellipses of tunica were excised and the defect repaired to shorten the convex side of the penis, correcting the curvature (1). In 1984, Coughlin et al. published in the Journal of Urology a series of 12 patients who underwent a Nesbit plication that was modified by burying the end knots when closing the ellipsoid incisions to prevent postoperative palpation of suture material (14). See below in the comparative surgery section a review describing the difference between standard Nesbit repairs and the use of buried suture. Also, in 1984 Goldstein et al. published the use of the Nesbit procedure for correction of penile curvature in 19 men, including 15 with Peyronie’s plaque and two with post fracture of the penis curvature with retention of potency. Good correction of the curvature in all 19 followed from 6 months to 10 years (15). Also in 1985, Porst and others confirmed the usefulness of the Nesbit procedure in a small number of men with PD (16). Kelâmi et al. later, in 1987, added a small modification to the Nesbit technique by applying sequential Allis clamps to the convex side of the penis, allowing visualization of the final surgical result, prior to making any incision and end plication closure to smooth the result (17) (Figure 2).
Figure 2.
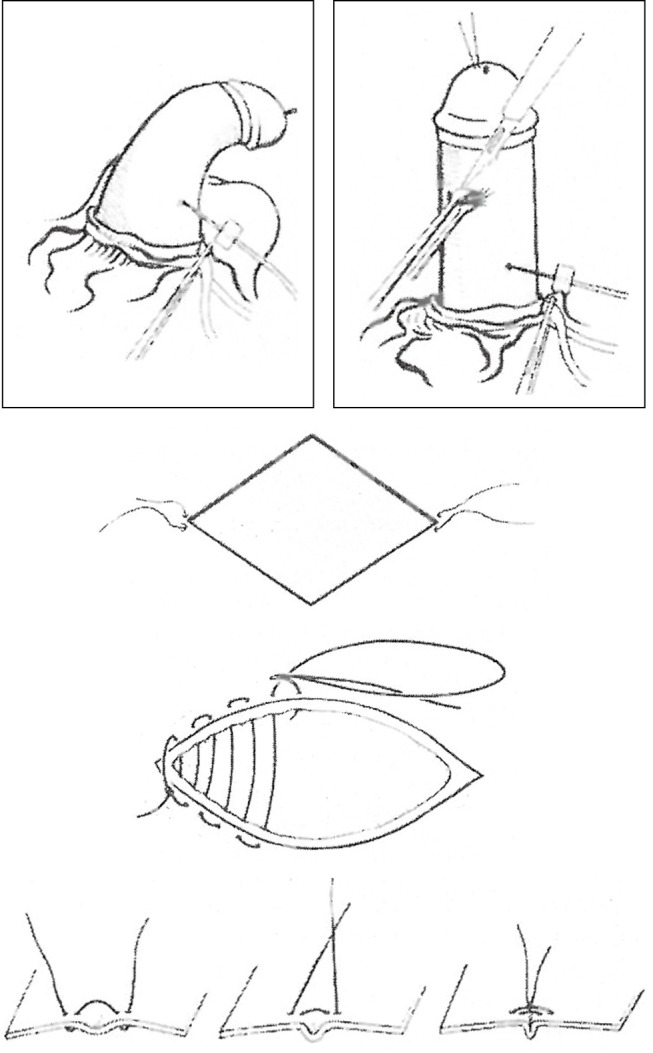
Significant parts of the Nesbit Kelami surgical repair for penile curvature repair in Peyronie’s disease (PD) (Permission is granted by John Wiley & Sons, Inc. All Rights Reserved.) [Reprinted with permission (17)].
Over the past 5 decades since Nesbit first published on his corporoplasty, many groups have looked at the efficacy of this surgery for the correction of penile curvature and three of these are discussed here. In 1995, Ralph et al. published an article looking at the results of the Nesbit operation from 1977 to 1992 in 359 patients (18). There had been previous earlier reports of results from this same group, but this was the latest and best reported. The median follow-up was 21 months and the degree of curvature prior to surgery was reported at 68 degrees. Results were categorized into excellent, satisfactory, or poor based on three criteria: penile deformity (degrees), quality of erection, and ability to perform coitus. Of the 359 patients, 237 (66%) reported excellent results, 58 (16%) reported satisfactory results, and 64 (18%) reported poor results. Interestingly, Ralph et al. found that prior to 1985, only 74% of patients reported a successful result whereas after 1985, this number increased to around 90%. The authors postulate the reason for this discrepancy is poor patient selection prior to 1985, meaning a Nesbit operation was performed on patients with poor pre-op erectile function instead of either just implanting a penile prosthesis or combining the two procedures. Penile Doppler revolutionized the work-up for PD after 1985, allowing physicians to select veno-occlusive disease as the culprit of poor erections that may have been blamed on the PD in years past.
Another study by Syed et al. looked at the results of the Nesbit procedure in 57 patients with PD from 1991 to 2000 (19). Questionnaires were sent out and had a return rate of 76.4% (42 of the 57 patients). Of the 42 responders, 26 reported a straight penis and 12 reported only a minor residual curvature of <30 degrees. The authors state that of the four patients with a poor result, two had undergone previous Nesbit repairs and had ongoing disease progression, and one had snapped the sutures during an erection (absorbable sutures used). Fifty percent of the patients reported no change in penile length, whereas the other 50% noticed the shortening effect of the procedure. Only 5 of the 21 patients who complained about penile shortening stated it was unacceptable. Nine patients reported sensory changes in the glans penis after the operation; however, the authors state multifactorial reasons for these results, such as previous ED or concomitant circumcision. Interestingly, the authors state in the introduction that although there have been many modifications to the standard Nesbit corporoplasty for correction of Peyronie’s curvature, the outcome results remain similar to the original.
Another large group of 279 patients surgically treated for Peyronie’s penile curvature was reported by Savoca et al. in 2004 (20). He mentions in his description that standard Nesbit procedure was used with a single, double, or multiple ellipses with need for Yachia supplementation in 42 patients. No details are presented for the different operative classes. An overall 86.3% of the patients had complete correction of their curvature, and 83.5% were satisfied with the outcomes of surgery at a median follow-up of 89 months. Post-operative significant penile shortening of 1.5 to 3 cm was present in 36 patients (16.5%) and, in 2 patients, shortening of greater than 3 cm was reported (0.9%). At long-term follow-up (mean 89 months), 25 patients (11.5%) reported worsening of erection and 3 patients reported, (1.4%) complete loss of erection, assessed by the IIEF.
In a 2001 article published in the British Journal of Urology, Andrews et al. set out to analyze the reasons for a poor result after a Nesbit procedure in 51 patients (21). The authors looked at degree of recurrent penile deformity post-op, as well as timing of recurrence (immediate, early and late), quality of erection, and penile shortening. The conclusion was that immediate recurrence of penile deformity was likely due to surgical error and incomplete correction of deformity intra-op, whereas early recurrence was likely due to use of absorbable suture with poor tensile strength and late recurrence a sequelae of reactivation of the disease/new disease formation. There were very few patients that reported poor erectile function post-op and the authors go on to state only that a thorough work-up of penile physiology should be done pre-operatively with vasoactive agents and Doppler ultrasound to give patients an overall picture of erectile function prior to surgery. This not only gives patients a realistic expectation, but may also change the surgical approach (i.e., Nesbit vs. IPP placement). In terms of penile shortening, patients had to report a >2 cm loss in penile length to be categorized as a poor result. Andrews et al. state that this could be due to poor surgical technique (excising more tunica than is needed) vs. penile shortening as a consequence of severe postoperative hematoma, a previous Nesbit procedure or simply progression of the PD.
Other modifications to the Nesbit procedure have been published, including one in the Journal of Urology in 1997 by Rehman et al. that incorporates a shaving technique of the tunica albuginea (postulated to decrease bleeding and damage to spongy erectile tissue) used along with standard Nesbit ellipsoid incisions (22). In this study published in 1997, 26 PD patients underwent this modified Nesbit procedure. Follow-up ranged from 1 to 5 years, and the authors reported that results at prolonged follow-up showed 19 patients (78%) had an excellent result; however the remaining 7 had recurrence of curvature (5 patients with <30 degrees, 2 patients with >30 degrees). Seventy-seven percent of the patients reported overall satisfaction with the procedure on follow-up questionnaire.
In 2001, Colpi et al. presented at a Congress of the European Society for Sexual and Impotence Research a modification to the Nesbit procedure which they termed a “penile septoplasty”, where ventral curvature of the penis is repaired by first elevating the neurovascular bundle on the dorsal surface along with the deep vein of the penis and then making diamond shaped cuts from the intercavernous septum with transverse closure. The authors postulated that this would prevent complaints of post-surgical palpation of suture by patients. In a follow-up article in 2009, they stated this modification had been performed on 51 patients from 2001 to 2007 with excellent results (follow-up points at 3, 6, 12, and 18 months) (23). 49 of the patients were very satisfied, with only two showing partial satisfaction. No neurovascular lesions occurred, and there was no new onset of ED noted. These authors gave credit to a previously published paper by Giammusso et al., which used a similar approach, but this group had performed a modification of the Yachia procedure and performed this dorsal vein excision in the midline for only four patients with PD (24).
Rolle et al. submitted a modification of the Nesbit procedure to the Journal of Urology in 2005 where Allis clamps were used to grasp the convex side of the penis for straightening prior to incision as in the Nesbit-Kelami technique; however the authors then placed two U-shaped knots, one on either side of the Allis clamps, to plicate the tunica before incision (25). The Allis clamps are then removed and assurance is made that correction of the curvature remains with the U-shaped knots in place. This is all performed with a constant erect penis. Tunica is then excised over the U-shaped knots and approximated in a horizontal fashion. Rolle et al. proposed this modification so that the surgeon can make exact corrections of the curvature in real time, even re-passing the plication sutures if needed until satisfactory correction of the curvature is attained. This publication showed a total of 50 patients underwent this modified Nesbit procedure between the years 1995 to 2004 with follow-up at 1, 6 and 12 months. The results show no recurrent curvature and 94% overall patient satisfaction (3% unsatisfied with amount of penile shortening).
More recently, Schwarzer and Steinfatt published a modification to the Nesbit procedure that involves making multiple U-shaped flaps of tunica on the convex side of the penis and sliding them up and under the tunica, towards the glans in 37 patients with PD (26). They then sutured the now doubled-up tunica with a watertight closure using synthetic absorbable suture. This modification was utilized on 50 patients with congenital or Peyronie’s penile curvature disorders from 2008 to 2011 with a mean follow-up of 23 months, showing an overall “strong” or “very strong” satisfaction response of 87%. Ninety-six percent reported no sensation of suture induration and 87% had no worsening in ED.
In 1973, Saalfeld et al. published an article in the Journal of Urology describing three patients who underwent corporoplasty to correct penile curvature (3). The first of the three underwent a standard Nesbitt plication. The second patient underwent a Nesbit plication where a series of ellipses of tunica were removed from the dorsal surface of the penile shaft and closed transversely. Saalfeld then added the modification of making a total of four transverse incisions on the ventral aspect of the penis and closing them longitudinally with the intention to gain length on the ventral side. In the remaining patient, a Heineke-Mikulicz repair was essentially used by making two longitudinal dorsal incisions, one on either side of the neurovascular bundle with transverse closure. Again on the third patient, Saalfeld et al. instituted ventral transverse incisions and closed them longitudinally in an attempt to gain ventral length. The authors state all three types of repairs were successful, but do not state length of follow-up or degree of correction of curvature. They also do not state if the ventral lengthening incisions made a difference in outcomes and this modification is not seen in later literature.
In 1984, Lemberger et al. also applied the Heineke-Mikulicz repair to 19 patients with a mean follow-up of 10 months (range, 4–22 months) (27). The results showed 18 patients with straight erections at that time (1 patient with continued curvature, but who was satisfied with the result). However, the authors noted that no objective method was used for assessing correction of curvature. Sassine et al. later published results on a series of 55 patients (23 with PD curvature) in 1994 with congenital and acquired penile curvature over a 10-year period who underwent what they labeled the “Saalfeld procedure”, showing 52 of the 55 (95%) had a good cosmetic and functional outcome as evidenced by recovery of normal sexual activity (28). They also mentioned the use of absorbable sutures and stated their series did not encounter loosening of the sutures or recurrence of the curvature.
Responding to complaints of palpation of suture postoperatively, Daniel Yachia published his modification on the Heineke-Mikulicz repair for PD in the Journal of Andrology in 1990 (4). He describes a repair in which he made longitudinal incisions that were closed transversely with running delayed-absorption monofilament sutures without burying the knots; however, he then placed additional burying plication sutures at each end of the incision to cover up the protruding edges.
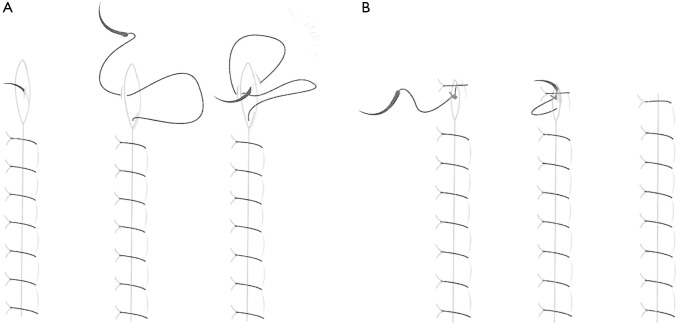
In 1997, Litch and Lewis reported a modification to the Yachia in 30 patients where end knots were buried and no extra end plication sutures were placed (5). A 19-gauge butterfly needle is placed into the corpora at the base of the penis, once the circumcision incision and degloving is made, for saline infusion with a roller pump during the procedure to produce an erection, without the need for neither a tourniquet nor the use of intracavernous smooth muscle relaxing agents. Also the use of Allis clamps to correct the curvature opposite the plaque outlines where the vertical incisions are to be made. Permanent suture (3–0 polypropylene) is used to close horizontally with burying the knots at each end. Figures 3 and 4 illustrate details of the procedure. The authors compared these 30 patients to 28 patients who received a standard Nesbit procedure. The results showed that the modified Yachia procedure achieved an overall higher rate of correction of curvature, and also a higher rate of satisfaction compared to the standard Nesbit. See more details of this comparative study in the section below.
Figure 3.

Licht Lewis Yachia modifications Illustration of penile degloving, placement of a sutured tied in 19 gauge butterfly needle for connection to an infusion pump to produce an intra-operative erection, placement of Allis clamps to mark the extent for the needed correction.
Figure 4.
Licht Lewis modification of the Yachia procedure. (A) Details of the end closure of the running suture, loop is kept outside while the needle is passed out upper or lower edge of the incision then brought back inside of the midline of the incision; (B) knot tied to the loop inside, passed out the incision from the inside beyond the edge of the incision to bury the knot.
Daitch et al. in 1999 reported the results of, basically, the Yachia procedure in 19 patients with PD curvature and 9 with congenital curvature that were followed for an average of 24.1 months (range, 11–46 months) (29). Penile straightening was excellent in 25 patients and good (less than 20 degrees of residual curvature) for a total response of 96% with the same percentage reporting no change in erectile rigidity. When 14 patients treated for Peyronie’s curvatures were contacted at long-term follow-up, 93% reported excellent straightening with one patient reporting less than 20 degrees of residual curvature; 93% also reported no change in post-operative rigidity. Eight patients noted penile shortening (57%). Eleven of the 14 men were satisfied or very satisfied, two were neutral and two were dissatisfied.
In 2013, Lopes et al. published the largest series at the time on the results of Yachia for treating Peyronie’s curvatures (30). The study followed 117 patients for an average of 14 months, between the years 1991 and 2009. Mean outcome measures were overall satisfaction, quality of erections, degree of curvature and complications (including hematomas and paresthesia of the glans). The authors found an overall satisfaction rate of 92.9% (88.4% complete satisfaction and 4.5% partially satisfied). For those that reported dissatisfaction with the procedure (7.1%), most were unhappy due to complaints of penile shortening, hypoesthesia of the glans, and recurrence of deformity. Twenty-two patients developed recurrent deformity at 12-month follow-up; however this only compromised intercourse in 7 of these patients.
From unpublished data from our institution that have been presented to regional and national urology meetings, we have results of analysis of a group from 94 patients having the Yachia procedure performed by the senior author of this chapter from October 1998 through April of 2012. We had adequate follow-up in 73 patients (79%), and 45 patients were reached for a telephone survey at a mean follow-up of 4.6±3.7 years. Forty-one (56%) of the patients had prior medical therapy before surgery and 8 patients had prior surgery for PD. The median pre-operative curvature was 60 degrees (range, 15–90 degrees) and was most commonly lateral in 49% of the patients; post-operative, the median curvature was 0 degrees (range, 0–45 degrees). Using a 5-point Likert scale for each of the questions on the telephone survey, the following results were obtained by a non-surgeon questioner: 87% were improved, 89% reported no pain, 93% reported penile shortening, 78% would have the surgery again, and satisfaction was a median value to 3.5 (range, 1–5).
Imbrication (plication only) procedures and modifications
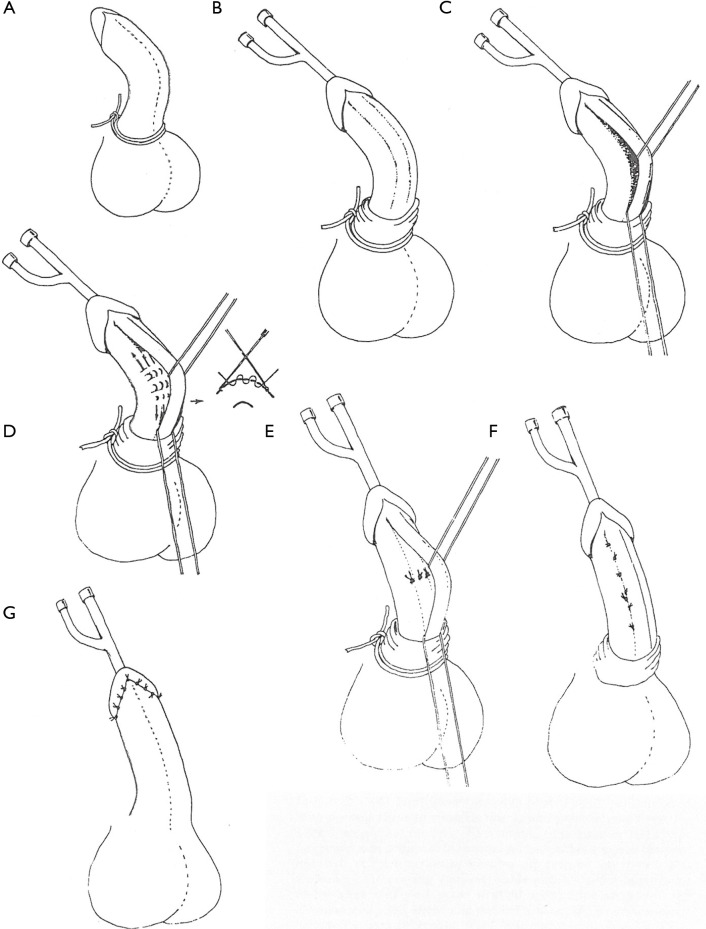
While Nesbit would be credited for the excisional corporoplasty that bears his name, he was also among the first to describe a plication procedure for congenital penile curvature in the same paper from 1965 (1). This was performed in one patient, using heavy silk suture, but he abandoned this method due to recurrence of curvature on short-term follow-up. In the year 1985, two papers were published in Urology on treating penile curvature by plication. Essed and Schroeder were first to take up the mantle of plication-only procedure for the treatment of PD when they published a short series of five patients in June of that year (6). They described their technique as reeving on the convex aspect of the curvature (Figure 5). They reported that all five patients were able to resume sexual activity but as is common with all Peyronie’s procedures, a slight penile shortening occurred. One patient with a short penis found this disturbing. A month later, Ebbehof and Metz published in Urology a larger series of 25 patients treated with their technique of plication in both congenital and acquired penile curvature (7). Four points on the tunica albuginea were grasped in the form of a square similar to a figure-8 stitch and plicated together to straighten the penis. See Figure 6 from that article. They found that one to four plications were needed to correct the curvature. However, their paper does not describe preoperative angle of curvature, indications for surgery, length of follow-up nor patient satisfaction rates.
Figure 5.
Parts of the Essed/Schroeder plication procedure for penile curvature surgery. (A) Tourniquet at base of penis as penis is injected with normal saline to visualize degree of curvature (injection needle not shown); (B) circumcision with penile degloving with indwelling catheter; (C) dissection of urethra off corpora cavernosa; (D) placement of reeving non-absorbable sutures after identification of points that will result in penile straightening; (E) straightened penis after tying reeving sutures; (F) urethra sutured back to corpora cavernosa; and (G) closure of the skin incision [Reprinted with permission (6)].
Figure 6.

Illustration of the double crossover stitch for the Ebbehof/Metz with four grasping points [Reprinted with permission (7)].
Klevmark et al. contributed their version of the plication technique in 1994 (31). A longitudinal incision was made on the penile shaft over the convexity of the curvature and dissected down to the tunica albuginea. Using 2–0 Prolene the tunica was seized in four areas with a width of 5 mm and plicated together over a 1-cm length to straighten the penis by 30 degrees. See Figure 7 from that article. Fifty-seven patients with PD, averaging 56 years of age, underwent this procedure with a 2-year follow-up. Preoperatively, only 8% of the patients were able to have satisfactory intercourse; 82% improved to have successful intercourse postoperatively. There was no incidence of new ED or chronic pain. Five patients had recurrences of curvature early (prior to 2–3 months), who were subsequently re-operated successfully. They recommended retaining 10–15 degree angulation to avoid unnecessary pain and stress on the suture, although not all patients were satisfied with this residual curvature.
Figure 7.
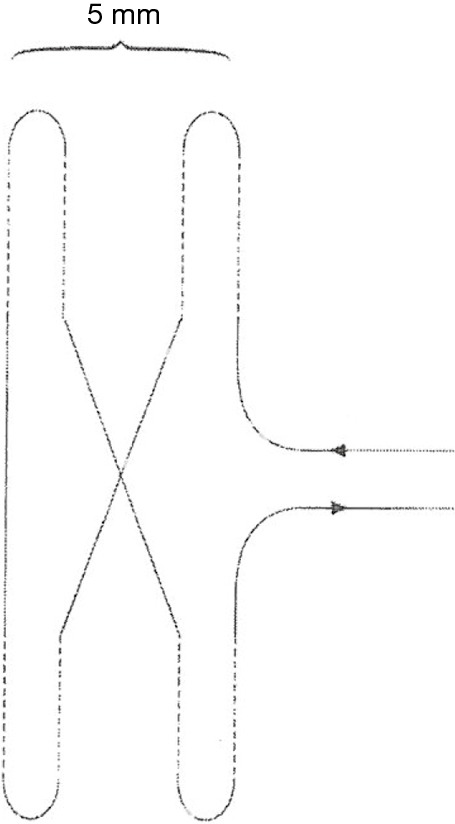
The suture technique used by Klevmark et al. for plication, the broken line indicates where the suture (2/0 Prolene) seizes the tunic. The suture must be narrow, approximately 5 mm, to avoid reduction in penile circumference. One cm height of suture corrects 30 degree angulation (Permission is granted by John Wiley & Sons, Inc. All Rights Reserved.) [Reprinted with permission (31)].
In the 1990’s other series were published. Nooter et al. in 1994 reported on a series of patients having the Essed plication in 33 patients with acquired penile curvatures, with an average age of 54.4 years and average angle of curvature of 63.3 degrees, using non-absorbable polyester 3–0 Tevdex with a follow-up of 40 months (32). The majority had good preoperative rigidity of erections, but 21 reported difficulty with intercourse. Twelve of this group of PD patients found intercourse impossible due to curvature or ED. Eighteen of 21 patients reported intercourse improved post-operatively. Eighteen noticed penile shortening, with two patients reporting severe shortening attributed to recurrent PD and re-plication surgeries. Complications included four out of seven uncircumcised patients requiring secondary circumcision and unexplained paresthesia in four patients.
Geertsen et al. in 1996 reported a series of 28 patients with PD who had tunical plication procedure in the manner of Ebbehof and Metz, but exposing the site of surgery correction by making a semi-circumferential incision overlying the site of maximum convexity (33). 2–0 Prolene sutures were used to correct the curvature with knots inverted. Mean age of this group was 60.5 years and mean follow-up was 34 months with a median deviation of 60 degrees (range, 30–90 degrees). Preoperatively, 24 patients were unable to have intercourse and four could have intercourse, but it was painful. Post-operatively, 16 were able to have intercourse without difficulty, while four suffered post-operative tolerable pain with intercourse. Late post-operative pain was attributable to suture in five patients and uncharacteristic pain in the penis /scrotum in five patients. Sixteen patients found the penis insufficiently straight but not enough to interfere with intercourse. The surgeons accepted 15–20 degree deviation post-operatively as a normal variant. Overall, 15 men (54%) were very satisfied with the functional and cosmetic result; eight (28%) were satisfied, and five (18%) were not satisfied at all.
In 1998, Thiounn et al. reported using the Ebbehof/Metz procedure in 29 PD patients using 3–0 Prolene suture with a mean follow-up of 18 months (34). Twenty men (81%) had satisfactory cosmetic results and 18 (62%) had satisfactory functional results. There were recurrences of curvature in six patients, four attributed to suture failure and two to recurrence of the disease. Five patients reported penile shortening, but none found it bothersome or interfering with intercourse, and two reported glans paresthesia. In this series where results in congenital curvature were also reported in 25 patients, the authors found plication somewhat less effective for PD patients.
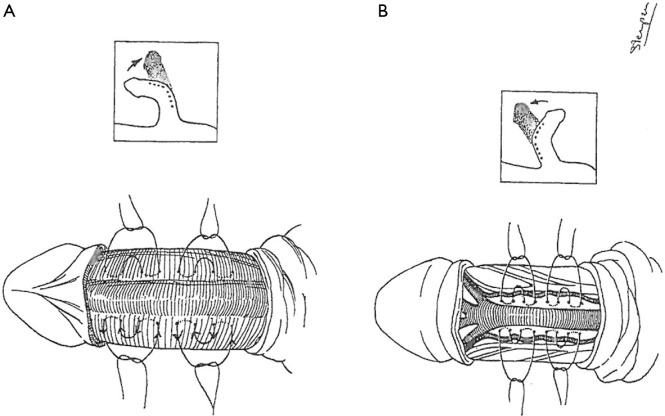
In 1998, Baskin and Lue published a series on ten patients with congenital curvatures who underwent what was then called “multiple parallel plications” (35). Gholami and Lue then followed this in 2002 with a large series of both congenital and acquired curvature patients, and a modified version of the multiple parallel plications, now formalized as the 16-dot plication technique (36). A surgical pen was used to mark the center of the curvature on its convexity as well as the entry and exit points with 16 dots (two pairs) or 24 (three pairs depending on the length of curvature) about 0.5 cm apart. Then 2–3 pairs of 2-O braided polyester sutures were placed through the full thickness of the tunica albuginea. These were tied in five knots with minimal tension to prevent tissue strangulation (Figure 8). From Dec 1995 to November 2000, 132 patients, with age ranging from 16 to 79 years, underwent the 16-dot plication procedure. Only 16 were patients with congenital curvature. The majority (81%) complained of difficulty with intercourse or partner discomfort. Penile curvature ranged from 30–120 degrees (average 64) with 34% noted to have more than one direction curvature. Preoperative erections were good in 63% while the remainder required assistance with sildenafil or injection therapy. At 6 months follow-up, 93% reported straight erections while 7% complained of slight curvature; four patients had worsening ED. At mean follow-up of 2.6 years, 15% of 124 patients had recurrence of curvature with four patients complaining of severe curvature. Four of the congenital group and eight of the acquired curvature group had failed prior Nesbit procedures and all 12 were satisfied with straight penises postoperatively. Forty-one percent of the patients reported penile shortening with loss of 0.5 to 1.5 cm in length and 7% found the length loss affected sexual activity. Other common complaints included bother from suture knots (12%), pain with erection (11%), narrowing or indentation of the penis (9%), paresthesia (6%), hematoma (4%), and pain when flaccid (1%). Eight patients complained of worst erections at long-term follow-up (mean 2.6 years). Overall satisfaction with the procedure was 96%.
Figure 8.
Details from the Lue 16-dot plication procedure. (A) 16-dot repair of dorsal curvature with periurethral sutures of 2–0 Ticron. Procedure done with midline raphe incision (circumcision used for illustration purposes; (B) 16-dot repair of ventral curvature. Peri-dorsal vein sutures without dissection of neurovascular bundles [Reprinted with permission (36)].
In 2000, Friedrich et al. presented a long-term follow-up of 12 of 16 patients who had Essed-Schroeder operations for acquired curvature caused by PD from 1994 to 1999 with a median follow-up time of 22 months (37). Of these 12 patients, six reported impaired rigidity and two reported recurrences of their penile curvature. Only seven reported good functional result. They compared these results to those who received corrective surgery by the same operation for congenital curvature, and these fared much better than the PD patients.
Chahal et al. reported in 2001 a long-term follow-up of patients having an Essed/Schroder plication procedure (44/65 patients returning a questionnaire) at a mean time of 4.1 years (range, 0.5–7.25 years) (38). Twenty-four patients (55%) were currently sexually active and two (5%) reported their erections had improved after surgery. Twenty-five (57%) reported a mild residual curvature after surgery and six reported a severe persistent curvature, making penetration difficult. Forty (90%) reported penile shortening after surgery with 22 (55%) considering this as significant. Seven (16%) complained of significant penile pain and discomfort during intercourse. Fifteen (34%) reported “new nodules”, that were not possible to distinguish between suture nodules or new Peyronie’s plaques. Half of the patients had significant stress because of their disease, with 57% reporting deterioration in their quality of life since surgery. Only 14% of the 38 partners reporting felt that there had been a significant improvement in sexual performance while eight (21%) felt there had been slight improvement. Only 23 (52%) would recommend the surgery to other patients with similar problems.
In 2004 Van Der Horst et al. reported on results and quality of life from the patient’s perspective. This was based on a standardized questionnaire in 50 patients having an Essed-Schroeder plication with a knot burying technique (39). Twenty-eight of these patients had PD curvature with a mean angle of 72 degrees (range, 30–90 degrees). Sixty-one percent were capable of sexual intercourse before surgery; 90% afterwards. In three patients intercourse was still impaired. Seventy-four percent reported a shorter penis after surgery. Five patients reported improved erectile function after correction, but ten patients reported persistent ED, 50% each moderate or slight impairment. Five men reported no improvement in curvature after surgery. Sixteen patients would choose the same operation again, six were undecided, and three would not. Four patients required reoperation, one for granuloma and three for recurrence of deviation. Nineteen patients were moderately to very satisfied, and nine patients were dissatisfied with the result of surgery. Twenty patients reported an improvement in sexuality and none complained of a decrease in sexual satisfaction. Pain during intercourse was reduced in 4 of 13 of the patients. Impairment of penile sensibility was reported in 28%. Of the patients’ partners, 78% were satisfied with the outcome. In an earlier publication, the same group had compared the use of two types of suture, non-absorbable polypropylene and polytetrafluoroethylene, in the same group of patients and concluded that the latter was the preferable suture (40).
By the mid-2000s, as urologists around the world had accrued more than 20 years of experience with plication procedures as part of their armamentarium for the treatment of PD and congenital penile curvature, Laurence Levine published his review of a modification of penile plication in 2006 (41). Levine combined aspects of the Yachia transverse closure with the plication procedure and labeled this the tunica albuginea plication, or TAP procedure. For both ventral and dorsal curvatures, a circumcision incision was made after an artificial erection was induced and the penis degloved. For ventral curvatures, a segment of the deep dorsal vein dorsally contralateral to the maximum concavity was elevated and resected with circumflex and perforating veins ligated, as well as the neurovascular bund carefully mobilized to expose the dorsal tunica albuginea. A pair of transverse incisions is made directly over the septum and carried through the longitudinal tunical fibers but not through the circular fibers—thus the cavernosal space remained inviolate. The tunica is then plicated using 2-O braided polyester suture in a vertical mattress fashion to bury the knot and several 3-O PDS sutures used to reinforce the plication. For dorsal curvature, the plication is carried through on the thicker ridge of the tunica, adjacent to the urethra bilaterally. In this review, he referenced his experience with 154 consecutive TAP procedures, and highlighted reservation of plication for curvature less than 60 degrees to minimize penile length loss, as well as a 99% rate of adequate straightening to a less than 20 degree residual curve. Levine would avoid plication for severe or hourglass deformities.
In a published article in early 2006, Levine’s group analyzed factors affecting loss of length in 68 patients with PD treated with the TAP procedure that were part of the group discussed above with a mean follow-up of 29 months (42). They concluded that best measurement of curvature was obtained in the office using pharmacodynamics duplex ultrasound. Mean loss of length was 0.36 cm (range, 0–2.5 cm). The longer the penis was preoperatively, the more length was lost. Also a greater curvature assessed objectively was correlated with a greater loss of length. A ventral curvature also postoperatively was associated with greater loss. Sixty-seven of the patients (98.5%) with PD plication surgery were satisfied or extremely satisfied.
Hsieh et al. had published in 2006 very favorable outcomes for correction of congenital curvatures in 114 patients using absorbable suture with 28.1% suture failure. Of this, only half of these saw a curvature greater than 15 degrees at 6-month follow-up (43). Dugi and Morey, in 2009, reported plication with absorbable sutures, but via a minimally invasive penoscrotal approach (44). No degloving of the penis is necessary. A 2-cm longitudinal incision was made in the penoscrotal junction for dorsal curvatures where 2-O Ethibond sutures were placed in tunica albuginea in a vertical mattress pattern in a parallel series of plication. For ventral curvatures the incision was transferred 180 degrees and the sutures placed in the sulcus next to the dorsal penile vein. Each vertical mattress suture spanned a total distance of ~1.5 cm. Forty-eight patients underwent this minimally invasive technique within a 4-year period from 2005 to 2009, of which 45 were sufferers of PD. The median age was 58.7, with correction of median preoperative curvature of 45 degrees to median postoperative curvature of 15 degrees. The majority had dorsal or dorso-lateral curvature. Dugi and Morey reported 93% satisfaction after one surgery, and no worsening of penile shortening that had already occurred secondary to PD. In the last 13 patients operated on, the stretched penile length before and after surgery indicated no quantifiable shortening. Only two patients were noted to be dissatisfied: a young man with congenital curvature requiring a second plication as well as a man with PD with continued curvature and worsening ED requiring insertion of penile prosthetic. Dugi and Morey reported no delayed complications or late failures.
Comparative studies
Over the last four decades a number of articles have compared different surgical approaches to penile curvature surgery performed for PD at the same center or by the same surgeon or group. Many of these have compared a historical assessment as one surgical approach has replaced another. Most of these have not been mentioned in the sections above and are primarily presented here to represent comparative approaches for the same disorder.
In 1990, Mufti et al. performed a retrospective study comparing the three known techniques for surgical correction of PD: Nesbit’s excision, incision, and transverse closure of corpora, and a variation of the corporal plication in a small group of patients (45). Mean follow-up was 31 months. Nine (30%) underwent Nesbit procedures, 8 (27%) had Heineke/Mikulicz procedures, and 13 (43%) had plication only. Overall 19 (63%) patients improved post-operatively. There was no significant difference comparing the three approaches. Those with pain at the time of surgery had a high failure rate, suggesting persistent disease activity. Because of the simplicity of the plication approach and the outcomes being no different the authors recommended this approach.
In 1995 Poulsen and Kirkeby reported a comparison to plication of the tunica albuginea to Nesbit procedures in 57 patients with Peyronie’s curvature (46). Forty-eight men had Nesbit surgery and nine had plication. Good or acceptable results were obtained in 91% of the Nesbit group compared to 44% in the plication group (improving to 67% after a second operation—a Nesbit procedure). Post-operative erectile capacity occurred in 5 of 9 receiving plication procedures and 11 or 48 receiving the Nesbit approach.
Licht and Lewis reported in 1997 a comparison of standard Nesbit procedure (28 patients), to their modified Yachia procedure (30 patients), to plaque excision with patch repair (28 patients) in a total of 86 patients (5). Plaque excision with patch repair resulted in less elimination of curvature (61% compared to 93% for Yachia procedure and 79% for the standard Nesbit procedure), a lower rate of satisfaction (30% compared to 83% of Yachia and 79% for Nesbit), and a higher rate of post-operative ED (18% compared to none for the Yachia and only one for the Nesbit). Elimination of curvature, patient satisfaction, and post-operative ED were not statistically different between the Yachia and the standard Nesbit group. Penile shortening was higher in the Yachia group compared to the other approaches, but did not affect satisfaction (67% for Yachia, 37% for the standard Nesbit, and 30% for the plaque excision with patch repair group—the P value reached 0.007).
In 1997 Levine and Lenting published their results of surgery for PD comparing tunica albuginea plication in 22 patients with incision or partial excision of plaque with grafting with dermal grafting in 48 patients or tunica vaginalis grafting in 4 patients (10). Complete straightening occurred in 94% of the dermal graft group, in 91% of the tunica plication group, and 50% of the tunica vaginalis group. Persistent curvature occurred in three with dermal grafting, two with penile plication (less than 30 degrees), and 2 of the tunica vaginalis grafting group. Full erectile capacity occurred in 91% of the plication group, 75% of the dermal graft and two of the tunical vaginalis groups. Penile shortening occurred in two of the plication group (less than 3 cm) and nine of the dermal graft group (0.5 to 2 cm). Using this data, the authors proposed a surgical algorithm for the treatment of PD mentioned in the section above.
Popken et al., in 1998, submitted an article comparing the outcomes of this modified Nesbit technique to the original Nesbit technique (47). The study had 105 patients with penile curvature in which half underwent the original Nesbit procedure and half underwent a modified Nesbit procedure with continuous running closure of incisions with buried end knots. The authors found similar short term outcomes (<6 months post-op) in terms of complaints and patient morbidity, however long term follow-up (>6 months post-op) showed that a much larger percentage of patients who underwent the original Nesbit technique complained of palpable indurations compared to patients undergoing the modified Nesbit (45% vs. 16%).
Schultheiss et al. in 2000 expanded on Essed/Schroeder’s technique in 21 patients with PD (avg. age 49.8) from 1991 to 1996 with a mean follow-up time of 39.8 months (48). 42.9% of the Peyronie’s patients reported failure, still making intercourse painful or even impossible. A total of 76.2% stated penile shortening after surgery but only 21.3% felt bothered by this. They compared the Essed with the Nesbit corporoplasty by using a Medline search for both procedures with results from the literature presented in two excellent tables. They compared their outcomes with this published literature-derived groups. Their conclusion was that the Nesbit outcomes were better, and that their future approach at their institution would be the Nesbit approach.
In 2005 Bokarica et al. presented the results in 55 patients operated on for PD curvature, 40 with Nesbit procedures and 15 with plaque excision with polytetrafluoroethylene patch graft from 1990 to 2000 (49). The median follow-up for the Nesbit group was 84 months and 85 months for the patch graft group. ED occurred in two patients (5%) who had Nesbit operations and in one (6%) with grafting. Penile shortening occurred in all who had the Nesbit procedure and in none of the graft group. The authors concluded that the type of surgery offered to the patient with PD should depend on the degree of curvature and penile length. For Nesbit, the penile length pre-operatively should be greater than 13 cm and have a deviation of 60 degrees with grafting for those with shorter lengths and more penile deviation.
More recently, in 2008, Taylor and Levine presented an analysis of 218 men who underwent a TAP or a partial plaque excision with human pericardial grafting (50). One hundred and forty-two patients completed survey responses at average follow-up for TAP of 72 months and the grafting group of 56 months. The degree of preoperative curvature was, of course, greater in the graft group (49 vs. 75 degrees). Residual curvature was worse with the grafting group (81% vs. 61%); rigidity was found to be as good as or better than preoperative state in 81% of the TAP group compared to 68% of the graft group but was adequate for coitus in 90% and 79% respectively. Although the TAP group expressed a slightly more percentage of post-operative length loss (69% vs. 59%) average measured length loss was 18% vs. 33%. Eighty-four percent of the TAP group and 79% of the graft group would have their respective surgery again, with 82% of the TAP group and 75% of the graft group either satisfied or extremely satisfied.
Summary
There are basically three approaches that can be labeled plication procedures for correction of PD penile curvature, excisional coroporoplasty most labeled as Nesbit or modified Nesbit procedures, incisional corporoplasty using the Heineke-Mikulicz technique most labeled Saalfeld or Yachia operations, or plication only procedures most labeled Essed/Schroeder or more recently the Lue 16 dot procedures. The latter two types of procedures are said to be less invasive and have an easier surgery, although outcomes seem to be similar. There are clearly proponents of each type and head-to-head or randomized papers comparing all three approaches are lacking in the literature. Compared to grafting procedures, these are less likely to affect erectile function but those who require grafting often have more advanced PD. All penile surgery for PD do cause some penile shortening, but certainly all plication procedures will certainly result in penile shortening, although most analyses of results suggest that perceived shortening is often greater than actually measured losses, and that some shortening is well tolerated. Those with longer pre-operative penile length are prone to have greater shortening. In the few reports comparing plication-only procedures to Nesbit type procedures, the latter is favored. A more frequent complaint for the plication-only technique is postoperative bother from knots or knot granulomas, which may be lessened by using absorbable suture or knot burying techniques. Some very long-term studies suggest that follow-up for longer than several years might result in less long-term favorable results.
Techniques for the surgery usually involve circumcision incisions with penile degloving although there have been several reports of direct penile incisions over the penis at the sites of maximum convexity or approach via penile scrotal incisions. The use of an infusion pumps to produce erections are easier to use to duplicate the penile deformity with ease of detumescence although some prefer the injection of smooth muscle relaxant agents, both obviating the bulky penile tourniquet. Allis clamps on the convex side of the deformity to correct for the curvature before surgery are good markers for length needed to correct the curvature. It is thought that 1 cm in length corrections will create for about 30 degrees of curvature and should be the maximum individual correction, using more if significant curvature remains after the first plication. Permanent 2 or 3–0 sutures are preferred by most but there have been some proponents of resorbable suture. Curvatures of greater than 90 degrees, hourglass deformities, severe plaque calcification, or those with significant ED intractable to oral or injection therapy are relative contraindication to plication type surgery.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Nesbit RM. Congenital curvature of the phallus: report of three cases with description of corrective operation. J Urol 1965;93:230-2. [DOI] [PubMed] [Google Scholar]
- 2.Pryor JP, Fitzpatrick JM. A new approach to the correction of the penile deformity in Peyronie's disease. J Urol 1979;122:622-3. [DOI] [PubMed] [Google Scholar]
- 3.Saalfeld J, Ehrlich RM, Gross JM, et al. Congenital curvature of the penis. Successful results with variations in corporoplasty. J Urol 1973;109:64-5. [DOI] [PubMed] [Google Scholar]
- 4.Yachia D. Modified corporoplasty for the treatment of penile curvature. J Urol 1990;143:80-2. [DOI] [PubMed] [Google Scholar]
- 5.Licht MR, Lewis RW. Modified Nesbit procedure for the treatment of Peyronie's disease: a comparative outcome analysis. J Urol 1997;158:460-3. 10.1016/S0022-5347(01)64502-6 [DOI] [PubMed] [Google Scholar]
- 6.Essed E, Schroeder FH. New surgical treatment for Peyronie disease. Urology 1985;25:582-7. 10.1016/0090-4295(85)90285-7 [DOI] [PubMed] [Google Scholar]
- 7.Ebbehøj J, Metz P. New operation for "krummerik" (penile curvature). Urology 1985;26:76-8. 10.1016/0090-4295(85)90264-X [DOI] [PubMed] [Google Scholar]
- 8.Knispel HH, Gonnermann D, Huland H. Modified surgical technique to correct congenital and acquired penile curvature. Eur Urol 1991;20:107-12. [DOI] [PubMed] [Google Scholar]
- 9.Donatucci CF, Lue TF. Correction of penile deformity assisted by intracavernous injection of papaverine. J Urol 1992;147:1108-10. [DOI] [PubMed] [Google Scholar]
- 10.Levine LA, Lenting EL. A surgical algorithm for the treatment of Peyronie's disease. J Urol 1997;158:2149-52. 10.1016/S0022-5347(01)68184-9 [DOI] [PubMed] [Google Scholar]
- 11.Kadioglu A, Akman T, Sanli O, et al. Surgical treatment of Peyronie's disease: a critical analysis. Eur Urol 2006;50:235-48. 10.1016/j.eururo.2006.04.030 [DOI] [PubMed] [Google Scholar]
- 12.Ralph D, Gonzalez-Cadavid N, Mirone V, et al. The management of Peyronie's disease: evidence-based 2010 guidelines. J Sex Med 2010;7:2359-74. 10.1111/j.1743-6109.2010.01850.x [DOI] [PubMed] [Google Scholar]
- 13.Mobley EM, Fuchs ME, Myers JB, et al. Update on plication procedures for Peyronie's disease and other penile deformities. Ther Adv Urol 2012;4:335-46. 10.1177/1756287212448224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coughlin PW, Carson CC, 3rd, Paulson DF. Surgical correction of Peyronie's disease: the Nesbit procedure. J Urol 1984;131:282-5. [DOI] [PubMed] [Google Scholar]
- 15.Goldstein M, Laungani G, Abrahams J, et al. Correction of adult penile curvature with a Nesbit operation. J Urol 1984;131:56-8. [DOI] [PubMed] [Google Scholar]
- 16.Porst H, Mayer R, Bach D, et al. Congenital and acquired penile curvatures: diagnosis and outcome with the Nesbit procedure. Urol Int 1985;40:206-10. 10.1159/000281081 [DOI] [PubMed] [Google Scholar]
- 17.Kelâmi A. Congenital penile deviation and its treatment with the Nesbit-Kelâmi technique. Br J Urol 1987;60:261-3. 10.1111/j.1464-410X.1987.tb05496.x [DOI] [PubMed] [Google Scholar]
- 18.Ralph DJ, al-Akraa M, Pryor JP. The Nesbit operation for Peyronie's disease: 16-year experience. J Urol 1995;154:1362-3. 10.1016/S0022-5347(01)66862-9 [DOI] [PubMed] [Google Scholar]
- 19.Syed AH, Abbasi Z, Hargreave TB. Nesbit procedure for disabling Peyronie's curvature: a median follow-up of 84 months. Urology 2003;61:999-1003. 10.1016/S0090-4295(02)02549-9 [DOI] [PubMed] [Google Scholar]
- 20.Savoca G, Scieri F, Pietropaolo F, et al. Straightening corporoplasty for Peyronie's disease: a review of 218 patients with median follow-up of 89 months. Eur Urol 2004;46:610-4; discussion 613-4. 10.1016/j.eururo.2004.04.027 [DOI] [PubMed] [Google Scholar]
- 21.Andrews HO, Al-Akraa M, Pryor JP, et al. The Nesbit operation for Peyronie's disease: an analysis of the failures. BJU Int 2001;87:658-60. 10.1046/j.1464-410x.2001.02176.x [DOI] [PubMed] [Google Scholar]
- 22.Rehman J, Benet A, Minsky LS, et al. Results of surgical treatment for abnormal penile curvature: Peyronie's disease and congenital deviation by modified Nesbit plication (tunical shaving and plication). J Urol 1997;157:1288-91. 10.1016/S0022-5347(01)64953-X [DOI] [PubMed] [Google Scholar]
- 23.Colpi G, Piediferro G, Castiglioni F, et al. Penile septoplasty for congenital ventral penile curvature: results in 51 patients. J Urol 2009;182:1489-94. 10.1016/j.juro.2009.06.059 [DOI] [PubMed] [Google Scholar]
- 24.Giammusso B, Burrello M, Branchina A, et al. Modified corporoplasty for ventral penile curvature: description of the technique and initial results. J Urol 2004;171:1209-11. 10.1097/01.ju.0000110297.98725.25 [DOI] [PubMed] [Google Scholar]
- 25.Rolle L, Tamagnone A, Timpano M, et al. The Nesbit operation for penile curvature: an easy and effective technical modification. J Urol 2005;173:171-3; discussion 173-4. 10.1097/01.ju.0000147160.53124.1a [DOI] [PubMed] [Google Scholar]
- 26.Schwarzer JU, Steinfatt H. Tunica albuginea underlap--a new modification of the Nesbit procedure: description of the technique and preliminary results. J Sex Med 2012;9:2970-4. 10.1111/j.1743-6109.2012.02887.x [DOI] [PubMed] [Google Scholar]
- 27.Lemberger RJ, Bishop MC, Bates CP. Nesbit's operation for Peyronie's disease. Br J Urol 1984;56:721-3. 10.1111/j.1464-410X.1984.tb06156.x [DOI] [PubMed] [Google Scholar]
- 28.Sassine AM, Wespes E, Schulman CC. Modified corporoplasty for penile curvature: 10 years' experience. Urology 1994;44:419-21. 10.1016/S0090-4295(94)80106-1 [DOI] [PubMed] [Google Scholar]
- 29.Daitch JA, Angermeier KW, Montague DK. Modified corporoplasty for penile curvature: long-term results and patient satisfaction. J Urol 1999;162:2006-9. 10.1016/S0022-5347(05)68088-3 [DOI] [PubMed] [Google Scholar]
- 30.Lopes I, Tomada N, Vendeira P. Penile corporoplasty with Yachia's technique for Peyronie's disease: Single center experience with 117 patients. Urol Ann 2013;5:167-71. 10.4103/0974-7796.115736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klevmark B, Andersen M, Schultz A, et al. Congenital and acquired curvature of the penis treated surgically by plication of the tunica albuginea. Br J Urol 1994;74:501-6. 10.1111/j.1464-410X.1994.tb00431.x [DOI] [PubMed] [Google Scholar]
- 32.Nooter RI, Bosch JL, Schröder FH. Peyronie's disease and congenital penile curvature: long-term results of operative treatment with the plication procedure. Br J Urol 1994;74:497-500. 10.1111/j.1464-410X.1994.tb00430.x [DOI] [PubMed] [Google Scholar]
- 33.Geertsen UA, Brok KE, Andersen B, et al. Peyronie curvature treated by plication of the penile fasciae. Br J Urol 1996;77:733-5. 10.1046/j.1464-410X.1996.97621.x [DOI] [PubMed] [Google Scholar]
- 34.Thiounn N, Missirliu A, Zerbib M, et al. Corporeal plication for surgical correction of penile curvature. Experience with 60 patients. Eur Urol 1998;33:401-4. 10.1159/000019624 [DOI] [PubMed] [Google Scholar]
- 35.Baskin LS, Lue TF. The correction of congenital penile curvature in young men. Br J Urol 1998;81:895-9. 10.1046/j.1464-410x.1998.00645.x [DOI] [PubMed] [Google Scholar]
- 36.Gholami SS, Lue TF. Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol 2002;167:2066-9. 10.1016/S0022-5347(05)65085-9 [DOI] [PubMed] [Google Scholar]
- 37.Friedrich MG, Evans D, Noldus J, et al. The correction of penile curvature with the Essed-Schröder technique: a long-term follow-up assessing functional aspects and quality of life. BJU Int 2000;86:1034-8. 10.1046/j.1464-410x.2000.00975.x [DOI] [PubMed] [Google Scholar]
- 38.Chahal R, Gogoi NK, Sundaram SK, et al. Corporal plication for penile curvature caused by Peyronie's disease: the patients' perspective. BJU Int 2001;87:352-6. 10.1046/j.1464-410x.2001.00114.x [DOI] [PubMed] [Google Scholar]
- 39.Van Der Horst C, Martínez Portillo FJ, Seif C, et al. Treatment of penile curvature with Essed-Schröder tunical plication: aspects of quality of life from the patients' perspective. BJU Int 2004;93:105-8. 10.1111/j.1464-410X.2004.04566.x [DOI] [PubMed] [Google Scholar]
- 40.van der Horst C, Martínez Portillo FJ, Melchior D, et al. Polytetrafluoroethylene versus polypropylene sutures for Essed-Schroeder tunical plication. J Urol 2003;170:472-5. 10.1097/01.ju.0000076370.30521.a6 [DOI] [PubMed] [Google Scholar]
- 41.Levine LA. Penile Straightening With Tunical Albuginea Plication Procedure: TAP Procedure. In: Levine LA, editor. Peyronie’s Disease: A Guide to Clinical Management. Totowa, NJ: Humana, 2006:151-9. [Google Scholar]
- 42.Greenfield JM, Lucas S, Levine LA. Factors affecting the loss of length associated with tunica albuginea plication for correction of penile curvature. J Urol 2006;175:238-41. 10.1016/S0022-5347(05)00063-7 [DOI] [PubMed] [Google Scholar]
- 43.Hsieh JT, Liu SP, Chen Y, et al. Correction of congenital penile curvature using modified tunical plication with absorbable sutures: the long-term outcome and patient satisfaction. Eur Urol 2007;52:261-6. 10.1016/j.eururo.2006.12.033 [DOI] [PubMed] [Google Scholar]
- 44.Dugi DD, 3rd, Morey AF. Penoscrotal plication as a uniform approach to reconstruction of penile curvature. BJU Int 2010;105:1440-4. 10.1111/j.1464-410X.2009.08991.x [DOI] [PubMed] [Google Scholar]
- 45.Mufti GR, Aitchison M, Bramwell SP, et al. Corporeal plication for surgical correction of Peyronie's disease. J Urol 1990;144:281-2; discussion 283. [DOI] [PubMed] [Google Scholar]
- 46.Poulsen J, Kirkeby HJ. Treatment of penile curvature--a retrospective study of 175 patients operated with plication of the tunica albuginea or with the Nesbit procedure. Br J Urol 1995;75:370-4. 10.1111/j.1464-410X.1995.tb07351.x [DOI] [PubMed] [Google Scholar]
- 47.Popken G, Wetterauer U, Schultze-Seemann W, et al. A modified corporoplasty for treating congenital penile curvature and reducing the incidence of palpable indurations. BJU Int 1999;83:71-5. 10.1046/j.1464-410x.1999.00887.x [DOI] [PubMed] [Google Scholar]
- 48.Schultheiss D, Meschi MR, Hagemann J, et al. Congenital and acquired penile deviation treated with the essed plication method. Eur Urol 2000;38:167-71. 10.1159/000020275 [DOI] [PubMed] [Google Scholar]
- 49.Bokarica P, Parazajder J, Mazuran B, et al. Surgical treatment of Peyronie's disease based on penile length and degree of curvature. Int J Impot Res 2005;17:170-4. 10.1038/sj.ijir.3901255 [DOI] [PubMed] [Google Scholar]
- 50.Taylor FL, Levine LA. Surgical correction of Peyronie's disease via tunica albuginea plication or partial plaque excision with pericardial graft: long-term follow up. J Sex Med 2008;5:2221-8; discussion 2229-30. 10.1111/j.1743-6109.2008.00941.x [DOI] [PubMed] [Google Scholar]