ABSTRACT
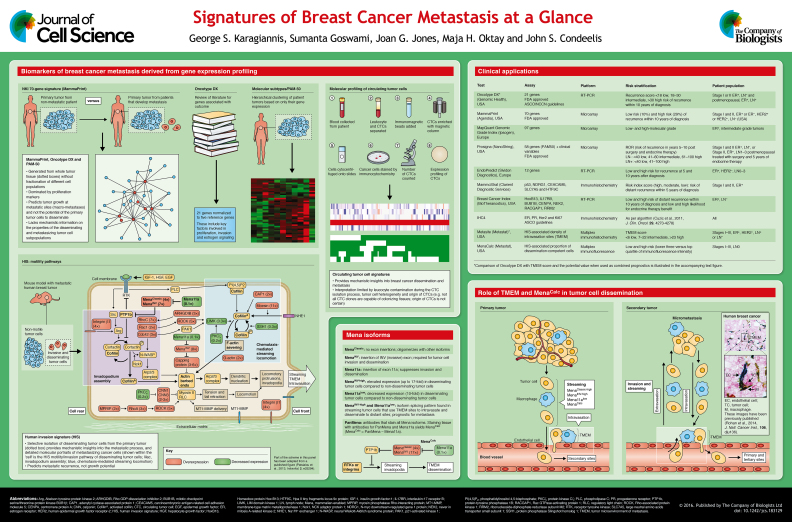
Gene expression profiling has yielded expression signatures from which prognostic tests can be derived to facilitate clinical decision making in breast cancer patients. Some of these signatures are based on profiling of whole tumor tissue (tissue signatures), which includes all tumor and stromal cells. Prognostic markers have also been derived from the profiling of metastasizing tumor cells, including circulating tumor cells (CTCs) and migratory–disseminating tumor cells within the primary tumor. The metastasis signatures based on CTCs and migratory–disseminating tumor cells have greater potential for unraveling cell biology insights and mechanistic underpinnings of tumor cell dissemination and metastasis. Of clinical interest is the promise that stratification of patients into high or low metastatic risk, as well as assessing the need for cytotoxic therapy, might be improved if prognostics derived from these two types of signatures are used in a combined way. The aim of this Cell Science at a Glance article and accompanying poster is to navigate through both types of signatures and their derived prognostics, as well as to highlight biological insights and clinical applications that could be derived from them, especially when they are used in combination.
KEY WORDS: Circulating tumor cell, CTC, Chemotaxis, Invadopodia, Human invasion signature, HIS, Intravasation, Mena, Tumor microenvironment of metastasis, TMEM
Summary: Prognostic assays based on proliferation (e.g. Oncotype DX, MammaPrint DX) combined with a prognostic derived from a signature of dissemination (e.g. TMEM score) could provide a complementary and more personalized prognostic information for breast cancer patients.
Introduction
High-throughput gene-expression profiling studies have yielded prognostic tests, such as MammaPrint-DX, Oncotype-DX and Prosigna (see below), that facilitate clinical decision making in breast cancer patients (see poster). However, these tests do not capture all of the patients who could benefit from adjuvant therapy or identify patients who do not need additional therapy [Arpino et al., 2013; Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group, 2009; Sorlie et al., 2001; Sotiriou and Pusztai, 2009; Wirapati et al., 2008]. One of the reasons for the hampered prognostic and predictive potential of these assays might be the fact that they are based on signatures that have been constructed from whole tumor tissue, which includes all tumor and stromal cells, instead of just the subpopulations of metastasizing tumor cells. To reveal the mechanisms responsible for the metastatic phenotype, gene expression has been performed on disseminating tumor cells, either circulating tumor cells (CTCs) (De Mattos-Arruda et al., 2013), or migratory–disseminating tumor cells isolated from the primary tumor (Goswami et al., 2004; Hernandez et al., 2009; Patsialou et al., 2013, 2012; Philippar et al., 2008; Roussos et al., 2011a,b,c; Wang et al., 2004, 2005, 2006, 2003; Wyckoff et al., 2011, 2000) (see poster). These signatures provide additional insights into the biological processes that are employed during metastasis, such as epithelial-to-mesenchymal transition (EMT), invasion and migration, resistance to apoptosis and anoikis, and intravasation. In this Cell Science at a Glance article and the accompanying poster, we discuss the discovery platforms and the clinical applications of clinically validated prognostic tests. We compare several prognostic tests derived from whole tissue profiling (i.e. MammaPrint DX, Oncotype DX, Prosigna) with prognostic tests derived from gene expression profiling of the metastasizing cancer cell subpopulation (e.g. migratory–disseminating tumor cells) and argue that their combined use has the potential to add additional information for treatment decisions for breast cancer patients.
Gene expression signatures for prediction of breast cancer metastasis
Signatures from whole tumor tissue
Molecular profiling of breast cancers has confirmed the existence of four major subtypes traditionally identified using immunohistochemistry: the basal-like subtype [estrogen receptor negative (ER−), progesterone receptor negative (PR−) and human epidermal growth factor receptor 2 (also known as ERBB2) negative (HER2−)], the HER2+ subtype, and two different ER+ subtypes, the luminal A (ERhigh, HER2−, low Ki67) and the luminal B (ERlow, HER2+/−, high Ki67) subtypes (Perou et al., 2000). These subtypes show diverse clinical outcome and response to therapy. For example, luminal-A breast cancers respond to hormonal therapy better than any other subtype, and also have favorable prognosis, whereas the basal-like and HER2+ subtypes are more sensitive to chemotherapy (Rouzier et al., 2005). There is new evidence that breast cancers can be subdivided in up to ten integrative clusters when copy number variation and gene polymorphism data are co-analyzed with genomic profiles (Curtis et al., 2012). However, such signatures have not yet reached clinical validation and application.
Several prognostic assays that are based on gene expression profiling of whole tumor tissue complement the molecular subtypes and address certain clinical needs, such as the identification of patient subgroups with low risk of developing metastatic disease or need for additional systemic therapy. MammaPrint DX is a 70-gene signature (also known as NKI-70) that has been developed through inkjet-synthesized oligonucleotide microarray profiling of tumors less than 5 cm in size obtained from breast cancer patients younger than 55 with lymph-node-negative disease (i.e. the disease had not spread into the axillary lymph nodes); it distinguishes patients who are likely to develop metastases from those who are likely to remain metastasis-free within five years after diagnosis (van ‘t Veer et al., 2002). MammaPrint has been validated in multiple independent validation studies (Bueno-de-Mesquita et al., 2009; Buyse et al., 2006; Mook et al., 2009, 2010; van de Vijver et al., 2002; Wittner et al., 2008), and is currently approved for stratification of patients of all ages with either hormone-receptor-positive or -negative disease and negative lymph nodes into ‘low-risk’ or ‘high-risk’ groups for developing distant metastases at 10 years after diagnosis without adjuvant chemotherapy (Curtis, 2015). The other two molecular tests, Oncotype DX and Prosigna, are primarily used for hormone-positive disease (see the summary Table on the poster for a more complete list of validated prognostic markers).
The initial breast cancer biomarker studies that eventually led to Oncotype DX started with the identification of a 250-gene signature that is associated with risk of breast cancer recurrence (Cobleigh et al., 2005; Cronin et al., 2004; Paik et al., 2004). Subsequent statistical analysis and modeling narrowed this list down to 21 candidate genes, of which 16 were cancer-related and primarily focused on the components of the estrogen receptor pathway and proliferation, and five reference genes, which were used for normalization of the gene-expression of the cancer-related genes (Paik et al., 2004). The Oncotype DX has been analytically and clinically validated in multiple studies in the past and diverse patient cohorts (Cronin et al., 2007; Esteva et al., 2005; Habel et al., 2006; Paik et al., 2006). The test result is presented as a recurrence score (RS), ranging from 0 to 100, which predicts recurrence in early-stage, node-negative ER+ disease and benefit from chemotherapy after breast surgery (Arpino et al., 2013; Brenton et al., 2005; Cobleigh et al., 2005; Daly et al., 2005; Simon et al., 2003; Stec et al., 2005). In particular, the Tailorx study demonstrated that patients with RS of 10 and below had a 98% chance of being disease free when treated with endocrine therapy only (Sparano et al., 2015). The benefit of chemotherapy in the patients with the intermediate RS (67% of patients) is still being evaluated, and in general, RS values in the intermediate range have not been useful to stratify patients as to metastatic risk.
Another prognostic test is IHC4; it is based on four widely performed immunohistochemistry measurements, those for estrogen receptor, progesterone receptor, HER2 and the proliferation marker Ki-67. IHC4 has been shown to contain the same amount of prognostic information as that of Oncotype DX RS and it correlates well with RS, and thus can be used interchangeably with RS (Cuzick et al., 2011). This suggests that these prognostics based on proliferation signatures are measuring the same biology in the whole tumor.
A prognostic that can assist in predicting response to therapy is Prosigna, which was derived from the PAM50 signature of whole tissue (Parker et al., 2009). PAM50 is a quantitative real-time PCR (qRT-PCR)-based assay of 50 genes; it evolved from studies that have reproducibly demonstrated the prognostic significance and predictive ability of the four intrinsic subtypes of breast cancer (Bastien et al., 2012; Chia et al., 2012; Harvell et al., 2008; Kelly et al., 2012; Martín et al., 2013; Nielsen et al., 2010; Prat et al., 2014; Sorlie et al., 2001, 2003). Prosigna stratifies breast cancer patients who have been treated with surgery and endocrine therapy into risk groups regarding disease outcome for years 5–10 post surgery and endocrine therapy, which helps to reduce overtreatment with chemotherapy in patients with good prognosis (Parker et al., 2009).
Several factors partially limit the effectiveness of these whole-tissue-derived signatures in the clinical setting. First, these signatures are mostly useful for the ER+/HER2− subset of patients. Second, although the molecular signatures address a similar clinical question, that is they identify low-risk patients, which do not need systemic adjuvant treatment, there is only minimal overlap between their gene lists, thus raising questions about their biological interpretation. Third, a thorough examination of the individual genes incorporated in MammaPrint-DX, Prosigna and IHC4 and Oncotype-DX tests reveals that they are dominated by those of the estrogen receptor, progesterone receptor and proliferation pathways, with only a few exceptions for genes that might be involved in metastasis, such as matrix metalloproteinase-11 (MMP11) and cathepsin-L2 (CTSL2, also known as CTSV). Finally, these signatures mostly refer to genes that are involved in tumorigenic pathways of cancer cells with little or no regard to the tumor microenvironment, which is known to dictate tumor cell dissemination, metastasis, survival and drug resistance (Hanahan and Weinberg, 2011).
Molecular profiling of circulating tumor cells
An alternative approach to address the metastatic potential of tumors is expression profiling of circulating tumor cells (CTCs). CTCs might be more representative of disease progression and resistance to treatment than random cells taken from the primary tumor (Bidard et al., 2014; Lianidou et al., 2012; Pantel and Alix-Panabieres, 2013). Early attempts to molecularly characterize CTCs in breast cancer patients yielded poor results, primarily because of the small number of CTCs collected and the inevitable contamination by circulating leukocytes. As such, those studies mostly pursued only small numbers of gene candidates that were already known to be involved in breast cancer progression, metastasis and therapeutic resistance, rather than global transcriptional profiles (Aktas et al., 2011; Bolke et al., 2009; Gervasoni et al., 2008; Gradilone et al., 2011; Theodoropoulos et al., 2010). Recent technological advancements allow for immunomagnetic-bead- or microfluidic-based isolation of CTCs (Autebert et al., 2015; Magbanua and Park, 2013). When coupled to high-throughput microarray or RNA-sequencing technologies and unbiased bioinformatics analyses, the aforementioned obstacles are significantly surmounted (Curtis, 2015; Lianidou and Markou, 2012; Magbanua and Park, 2014). Overall, these new-generation studies have allowed single-cell and bulk-cell analyses of CTCs, which efficiently capture the transcriptional heterogeneity and identify the molecular portraits of metastasizing cells (Ascolani et al., 2015; Cassatella et al., 2012; De Mattos-Arruda et al., 2013; Fina et al., 2015; Lang et al., 2015; Lianidou et al., 2012; Polzer et al., 2014; Powell et al., 2012). For example, one study has demonstrated that CTCs express various biomarkers and mediators of EMT (Yu et al., 2013), a phenotypic change crucial for the completion of the metastatic cascade (Bill and Christofori, 2015; Hanahan and Weinberg, 2011; Kalluri, 2009; Kalluri and Weinberg, 2009; Radaelli et al., 2009). However, only certain fractions of CTCs represent clones that are capable of colonizing distant metastatic sites, and in addition, there are reported discordances between the profile of the primary tumor and CTCs, e.g. with regard to their epidermal growth factor receptor 2 (EGFR2) status. Strikingly, CTC incidence might be observed in the peripheral blood of breast cancer patients, even after removal of the primary tumor, posing additional layers of complexity with regard to the specific origin of these cells and their relationship to dissemination from the primary tumor (Baccelli et al., 2013; Bidard et al., 2014; Curtis, 2015; Lang et al., 2015; Lianidou et al., 2012; Magbanua and Park, 2014; Pukazhendhi and Glück, 2014). As such, molecular signatures derived from CTCs should always be interpreted with caution.
Molecular profiling of metastatic breast cancer cell subpopulations
A recent study has demonstrated an in-depth expression profile of breast cancer stem cells using a mass-spectrometry-based proteomic approach in an in vitro model of forced EMT induction (Lu et al., 2014). The authors identified and validated new markers of breast cancer stem cells, including the membrane glycoprotein Thy1 (also known as CD90), which was associated with recruitment of tumor-associated macrophages; specifically Thy1 contributed to the construction of a cancer stem cell niche and enhanced tumor induction and progression in patient-derived xenografts (Lu et al., 2014). In another study, by using fluorescence-activated cell sorting-based assays and gene-expression profiling at the single-cell level, Lawson et al. demonstrated that metastatic cells retained a distinct gene expression signature that is composed of stem cell-, EMT-, pro-survival- and dormancy-associated genes (Lawson et al., 2015). Overall, many biologically relevant stem-like expression signatures have been reported (Borcherding et al., 2015; Feng et al., 2014), but, to our knowledge, no definite clinical validation or meta-analysis studies have been performed to provide robust molecular profiles of breast cancer stem cells. Thus, the extent to which breast cancer stem cell incidence and/or function holds important prognostic and therapeutic information remains to be elucidated (Ali et al., 2011; Rakha et al., 2009; Shipitsin et al., 2007).
An alternative approach of capturing metastasizing tumor cells in living tumors has been previously established in studies using an in vivo invasion assay. By this approach, migrating cells are collected from the primary tumor site using chemoattractants [e.g. epidermal growth factor (EGF), hepatocyte growth factor (HGF), insulin-like growth factor-1 (IGF1) or colony-stimulating factor-1 (CSF-1)], which are involved in the migration and dissemination steps of metastasis (Hernandez et al., 2009; Roussos et al., 2011b; Wang et al., 2005, 2003; Wyckoff et al., 2011, 2000). Using this methodology, migratory–disseminating cancer cells were collected from mouse mammary cancer models and patient-derived xenografts, and subjected to comparative expression profiling with whole tumor tissue. The resulting profiles were specific to breast cancer cell invasion and dissemination and defined rodent and human invasion signatures (Goswami et al., 2009, 2004; Patsialou et al., 2013; Patsialou et al., 2012; Roussos et al., 2011b; Wang et al., 2007, 2004). These invasion signatures are enriched in genes that regulate embryonic and tissue development, EMT, cellular movement, DNA replication and repair, apoptosis-evasion and resistance to treatment (Goswami et al., 2004; Patsialou et al., 2013, 2012; Wang et al., 2003; Wyckoff et al., 2011, 2000). Notably, the disseminating cancer cell subpopulation that gave rise to this signature was more resistant to conventional chemotherapies, such as doxorubicin, etoposide and cisplatin, when compared to the bulk tumor population (Goswami et al., 2004). In the discussion below, we focus on the clinically relevant, human invasion signature (HIS) (Patsialou et al., 2013, 2012) and the HIS-derived clinically validated prognostic markers TMEM and MenaCalc.
HIS describes migration and dissemination pathways critical for breast cancer metastasis
The HIS contains 445 transcripts that are significantly altered in the migratory tumor cells, of which 185 are annotated genes with known protein products (Patsialou et al., 2013, 2012). Gene transcripts altered in the HIS are ranked according to functional categories, which provides valuable clues for the molecular events that precede tumor cell intravasation and hematogenous dissemination, and allows insight into a detailed biological context that supports tumor cell invasion and dissemination. Interestingly, in contrast to MammaPrint-DX, Oncotype-DX and Prosigna that do not provide such insight, selected genes from HIS are functionally required for in vivo invasion and hematogenous dissemination. Moreover, prominent dissemination/metastasis-associated pathways, including transforming-growth factor β (TGF-β) and HGF were found to serve as molecular hubs in the identified overrepresented pathways (Patsialou et al., 2013, 2012), further confirming that this approach provides mechanistic insights underlying breast cancer dissemination and metastasis.
One of the prominently upregulated dissemination pathways in HIS is the mammalian-enabled (Mena, also known as ENAH)–cofilin pathway that regulates actin polymerization during chemotaxis and invasion of tumor cells (Bravo-Cordero et al., 2013; Philippar et al., 2008; Roussos et al., 2011b). Computational systems analysis of multiphoton microscope imaging datasets taken from large tumor volumes has been used to categorize the migration phenotypes of tumor cells in mammary tumors in vivo (Gligorijevic et al., 2014). High-resolution analysis of these categories indicates that the locomotion category, characterized by the streaming migration phenotype, and the invasion category, characterized by invadopodium-containing tumor cells near blood vessels and their associated intravasation, together contribute to tumor cell dissemination (Gligorijevic et al., 2014; Harney et al., 2015). Of significance, the Mena–cofilin pathway of the HIS contains the actin-binding proteins and their regulatory molecules (blue and lilac highlighted pathways in the HIS motility pathway poster panel) that define the locomotory (blue) and invasive (lilac) phenotypes of tumor cells in mammary tumors in vivo.
Mena is an actin-binding protein that is involved in the regulation of cofilin-stimulated actin polymerization, the key cofilin activity that determines chemotactic direction and invasion (Gertler and Condeelis, 2011; Philippar et al., 2008; Roussos et al., 2011a,b,c) (see poster). Subsequent investigation of the HIS gene expression pathways has revealed that differentially spliced Mena isoforms, including MenaINV, are upregulated, whereas the invasion-suppressing Mena11a isoform is downregulated in the migratory–disseminating tumor cell subpopulation (Goswami et al., 2009; Patsialou et al., 2013, 2012; Roussos et al., 2011a,b,c; Wang et al., 2004). This isoform-splicing pattern of Mena (MenaINV-high and Mena11alow) is functionally crucial for tumor cell invasion and migration during the metastatic cascade. In particular, it is required for directional cell migration in vivo, called streaming, towards chemotactic factors such as EGF and HGF, matrix degradation and transendothelial migration, as well as development of distant metastases (Patsialou et al., 2013, 2012; Patsialou and Condeelis, 2014; Philippar et al., 2008; Roussos et al., 2011a,c). In addition, MenaINV dramatically increases the sensitivity of receptor tyrosine kinases to their ligands EGF, IGF1 and HGF to increase cell protrusion and locomotion (Hughes et al., 2015b; Roussos et al., 2011a).
Identification and thorough examination of the HIS has led to development of clinically validated prognostic markers of metastasis, called MenaCalc and ‘tumor microenvironment of metastasis’ (TMEM; microanatomical structures that regulate transendothelial migration of breast tumor cells in primary tumors and possibly in secondary sites). MenaCalc is a measure of the isoform expression pattern of MenaINV-high and Mena11alow, and is commonly measured in formalin-fixed paraffin-embedded tissue as the subtraction of the immunofluorescence intensity of anti-metastatic-Mena11a antibody staining from total anti-Mena antibody staining (i.e. MenaCalc=PanMena – Mena11a), thus indirectly reflecting the expression of the invasive Mena isoforms. MenaCalc is predictive of metastatic relapse and survival in breast cancer patients (Agarwal et al., 2012; Forse et al., 2015). The relative expression of MenaINV to Mena 11a is directly related to TMEM assembly because tumor cells that both assemble and use TMEM for dissemination require the expression pattern MenaINV-high and Mena11alow (Pignatelli et al., 2014) (see poster).
TMEM sites are the sites of intravasation in polyoma middle T oncoprotein (PyMT)-induced mouse mammary tumors and patient-derived xenograft (PDX) mammary tumors, and are therefore necessary for the dissemination step of the metastatic process (Harney et al., 2015). The number of TMEM sites (TMEM score) in ER+ breast tumor tissue is predictive of an increased risk of distant metastasis. TMEM score is more strongly associated with risk of distant breast cancer metastasis than the IHC4 score and, by extension, Oncotype DX recurrence score (Rohan et al., 2014). In addition, a TMEM composite score is defined by combining the TMEM score with standard clinical variables including tumor grade, lymph node status, age, size and diagnosis year (Rohan et al., 2014). The ‘AUC’ curves [i.e. the area under the receiver operating characteristic (ROC) curve, which is the true positive rate versus false positive rate] for the TMEM composite score yield a value of 0.78 compared to those for MammaPrint (0.68), Oncotype DX (0.69) and IHC4 (0.64). These AUC values, where 0.8 is good, 0.7 is fair and 0.6 is poor discrimination (Metz, 1978), indicate that TMEM composite is better at predicting metastasis than these other prognostics (Rohan et al., 2014).
TMEM sites are composed of one Tie2high, VEGFhigh and MRC1+ perivascular macrophage, which is in physical contact with a Mena-overexpressing cancer cell, as well as an underlying endothelial cell (see poster) (Harney et al., 2015; Oktay and Jones, 2015; Pignatelli et al., 2014; Robinson et al., 2009; Rohan et al., 2014; Roussos et al., 2011c; Wyckoff et al., 2007). Previous reports on cancer angiogenesis and vasculogenesis have collectively demonstrated that newly constructed endothelia are composed of myeloid precursors expressing the receptor tyrosine kinase Tie2 (also known as TEK) (Riabov et al., 2014; Squadrito and De Palma, 2011), and, more recently, the mannose-receptor c-type 1 (MRC1) (Hughes et al., 2015a). Despite the fact that Tie2 expression has been primarily associated with endothelial precursors, it has also been linked to specific bone-marrow-derived monocyte lineages; these trans-differentiate into non-inflammatory, blood-vessel-resident macrophages that are committed to mediate proangiogenic programs and tissue remodeling, which are both frequently phenocopied by tumors (Forget et al., 2014; Pucci et al., 2009; Venneri et al., 2007).
TMEM sites enforce transient and localized blood vessel permeability through the disruption of homotypic cell–cell adhesions in the underlying endothelium (Harney et al., 2015). The detailed mechanism of TMEM function and the involvement of Mena isoforms in intravasation at TMEM sites have been described (Harney et al., 2015; Pignatelli et al., 2014; Roh-Johnson et al., 2014) and it has been shown that activation of the Tie2 signaling pathway in the perivascular macrophage stimulates the release of macrophage vascular endothelial growth factor (VEGF). VEGF in turn, promotes reversible local loss of endothelial adherens junctions at TMEM sites (Harney et al., 2015). The TMEM macrophage also initiates Mena-dependent invadopodium assembly in the TMEM tumor cell, with which it is in direct contact, thereby completing a required invasive step for transendothelial migration at TMEM sites (Pignatelli et al., 2014; Roh-Johnson et al., 2014). The resulting reversible, local permeability of the endothelium is visualized in real time by multiphoton microscopy as a dramatic release of luminal blood vessel components into the subluminal space (termed ‘bursting’). During bursting, lines of migrating cancer cells (called streaming cells; Roussos et al., 2011b) with the MenaINV-high and Mena11alow splicing pattern intravasate (Harney et al., 2015; Pignatelli et al., 2014; Roussos et al., 2011b). This finding directly links migration to dissemination (see poster). Indeed, conditional ablation of macrophages, disruption of Tie2 or VEGF-signaling, or inhibition of MenaINV-dependent invadopodium assembly dramatically inhibits TMEM assembly and function, and, consequently, tumor cell intravasation (Harney et al., 2015; Pignatelli et al., 2014).
Although the HIS contains additional prognostic markers that are currently being explored (Weitsman et al., 2014), the few that have already been investigated have provided an in-depth understanding of the process of tumor cell intravasation and dissemination, and more importantly have resulted in the development of clinically useful predictive markers of metastasis called TMEM and MenaCalc.
Clinical applications and future perspectives
Prognostic signatures derived from the study of whole tumor tissues, such as Oncotype DX, and its related test IHC4, are dominated by proliferation pathways (Paik et al., 2006), whereas signatures obtained from disseminating and metastatic tumor cell subpopulations (e.g. the HIS) are associated with cancer-progression-specific pathways, including invasion, EMT, metastasis (Patsialou et al., 2012), as well as TMEM assembly, intravasation and dissemination (Harney et al., 2015; Robinson et al., 2009; Rohan et al., 2014). The fact that most whole-tumor tissue gene-expression profiles are dominated by proliferation markers has been recently criticized, suggesting that such signatures might lose prognostic value regarding breast cancer outcome if tumors are statistically adjusted for the prevalence of proliferation-associated genes by the reference dataset (Venet et al., 2011). That is to say, any random gene set will contain a high proportion of proliferation-associated genes given that these genes are so prevalent, and have prognostic value similar to the whole-tumor tissue gene-expression profiles. However, proliferation is indeed a rate-limiting step of distant colonization (Falato et al., 2014; Nielsen et al., 2010; Wishart et al., 2014; Zurrida et al., 2013) and thus particularly important for assessment of breast cancer prognosis if combined with additional information. For these reasons, we speculate that prognostic score based on proliferation signature combined with a prognostic score derived from a signature of dissemination could provide complementary and more personalized prognostic and predictive information for breast cancer patients. An example of this is the possible combination of Oncotype Dx or IHC4, two correlated proliferation prognostics (Cuzick et al., 2011), with the TMEM prognostic marker, which provides independent prognostic information from IHC4 (Rohan et al., 2014). How a combined marker analysis of patients might be used to derive additional information about patient risk and treatment options is illustrated in the text box and accompanying chart (see Box 1).
Box 1. Comparing prognostic scores based on proliferation and dissemination, and the potential value of combined marker analysis for patients.
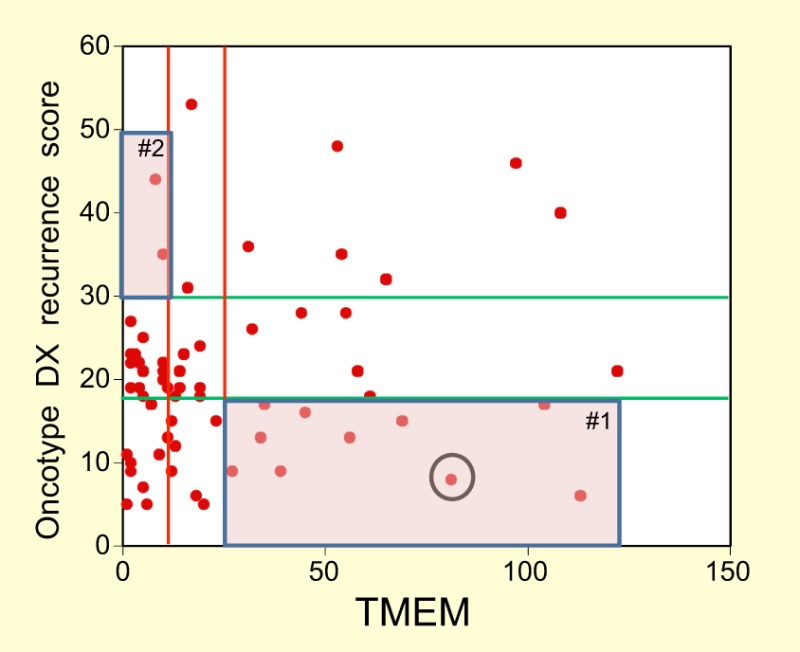
In this example, 64 randomly selected ER+ patient tissues obtained between 2008 and 2011 were evaluated for both Oncotype DX RS and TMEM score, and these scores were plotted on the y- and x-axes of the chart, respectively, along with their prognostic cut points identifying low-, medium- and high-risk patients (see accompanying chart). The R2 value for this plot is 0.11, showing that there is no correlation between TMEM density and RS, consistent with previous studies (Rohan et al., 2014). In other words, these two tests address different biological properties of the tumor, which might provide more accurate patient stratification and clinical decision making when used in combination. Additionally, in the accompanying chart, a subgroup of patients with a high Oncotype DX RS has a low TMEM score (shaded area # 2) and might have a good prognosis for dissemination, and thus less-toxic therapy could be administered. By contrast, a subgroup of patients with a low Oncotype DX RS and a high TMEM score (shaded area #1) were classified into the low-risk group based on the Oncotype DX RS alone but are at high risk for disseminated disease based on the high TMEM score. The latter would potentially benefit from more aggressive therapy. An example of the latter scenario is a 55-year-old patient (circled on the chart) with ER+ and HER2− invasive ductal carcinoma, with negative axillary lymph nodes, with an Onoctype DX score of 8 (low) and TMEM score of 81 (high) who was treated with endocrine therapy only and developed lung metastases 7 years after the primary diagnosis. This patient might have benefited from more aggressive therapy had the TMEM score been known and taken into consideration in treatment design at the time of diagnosis.
In the future, patients whose disease shows a high risk of dissemination (i.e. a high TMEM score) would need to be monitored very closely after the removal of the primary tumor. Although they might not have clinically detectable metastases at the time of initial treatment, elevated markers of dissemination (either TMEM or MenaCalc) would indicate that these patients already have cancer cells in distant organs which in time might lead to growth of metastatic tumors. These patients would be candidates for further treatment with drugs to suppress the growth of, and destroy dormant disseminated tumor cells.
In summary, future efforts should encompass further clinical validation of the use of combined signatures in larger patient cohorts. As noted in the Tailorx trial (Sparano et al., 2015), up to 67% of breast cancer patients have a disease with an intermediate Oncotype DX RS, which cannot be stratified as to the risk of recurrence by RS alone and would benefit from additional tests that measure different aspects of tumor biology, such as dissemination.
Footnotes
Competing interests
J.G.J. and S.G. have ownership interest (including patents) in MetaStat and J.G.J. is a consultant and advisory board member for the same. J.S.C. has ownership interest (including patents) in MetaStat and is a consultant and advisory board member for Deciphera Pharmaceuticals and MetaStat. No potential conflicts of interest are disclosed by the other authors.
Funding
This article was supported by a National Cancer Institute provocative question grant [grant number 1R01 CA170507-01]; the National Institutes of Health [grant numbers CA100324, CA163131, CA164468], the Integrated Imaging Program; and the Gruss Lipper Biophotonics Center. Deposited in PMC for release after 12 months.
Cell science at a glance
A high-resolution version of the poster is available for downloading at http://jcs.biologists.org/lookup/suppl/doi:10.1242/jcs.183129/-/DC1. Individual poster panels are available as JPEG files at http://jcs.biologists.org/lookup/suppl/doi:10.1242/jcs.183129/-/DC2.
References
- Agarwal S., Gertler F. B., Balsamo M., Condeelis J. S., Camp R. L., Xue X., Lin J., Rohan T. E. and Rimm D. L. (2012). Quantitative assessment of invasive mena isoforms (Menacalc) as an independent prognostic marker in breast cancer. Breast Cancer Res. 14, R124 10.1186/bcr3318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aktas B., Müller V., Tewes M., Zeitz J., Kasimir-Bauer S., Loehberg C. R., Rack B., Schneeweiss A. and Fehm T. (2011). Comparison of estrogen and progesterone receptor status of circulating tumor cells and the primary tumor in metastatic breast cancer patients. Gynecol. Oncol. 122, 356-360. 10.1016/j.ygyno.2011.04.039 [DOI] [PubMed] [Google Scholar]
- Ali H. R., Dawson S.-J., Blows F. M., Provenzano E., Pharoah P. D. and Caldas C. (2011). Cancer stem cell markers in breast cancer: pathological, clinical and prognostic significance. Breast Cancer Res. 13, R118 10.1186/bcr3061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arpino G., Generali D., Sapino A., Del Matro L., Frassoldati A., de Laurentis M., Pronzato P., Mustacchi G., Cazzaniga M., De Placido S. et al. (2013). Gene expression profiling in breast cancer: a clinical perspective. Breast 22, 109-120. 10.1016/j.breast.2013.01.016 [DOI] [PubMed] [Google Scholar]
- Ascolani G., Occhipinti A. and Liò P. (2015). Modelling circulating tumour cells for personalised survival prediction in metastatic breast cancer. PLoS Comput. Biol. 11, e1004199 10.1371/journal.pcbi.1004199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Autebert J., Coudert B., Champ J., Saias L., Guneri E. T., Lebofsky R., Bidard F.-C., Pierga J.-Y., Farace F., Descroix S. et al. (2015). High purity microfluidic sorting and analysis of circulating tumor cells: towards routine mutation detection. Lab. Chip. 15, 2090-2101. 10.1039/C5LC00104H [DOI] [PubMed] [Google Scholar]
- Baccelli I., Schneeweiss A., Riethdorf S., Stenzinger A., Schillert A., Vogel V., Klein C., Saini M., Bäuerle T., Wallwiener M. et al. (2013). Identification of a population of blood circulating tumor cells from breast cancer patients that initiates metastasis in a xenograft assay. Nat. Biotechnol. 31, 539-544. 10.1038/nbt.2576 [DOI] [PubMed] [Google Scholar]
- Bastien R. R. L., Rodríguez-Lescure A., Ebbert M. T. W., Prat A., Munárriz B., Rowe L., Miller P., Ruiz-Borrego M., Anderson D., Lyons B. et al. (2012). PAM50 breast cancer subtyping by RT-qPCR and concordance with standard clinical molecular markers. BMC Med. Genomics 5, 44 10.1186/1755-8794-5-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bidard F.-C., Peeters D. J., Fehm T., Nolé F., Gisbert-Criado R., Mavroudis D., Grisanti S., Generali D., Garcia-Saenz J. A., Stebbing J. et al. (2014). Clinical validity of circulating tumour cells in patients with metastatic breast cancer: a pooled analysis of individual patient data. Lancet Oncol. 15, 406-414. 10.1016/S1470-2045(14)70069-5 [DOI] [PubMed] [Google Scholar]
- Bill R. and Christofori G. (2015). The relevance of EMT in breast cancer metastasis: Correlation or causality? FEBS Lett. 589, 1577-1587. 10.1016/j.febslet.2015.05.002 [DOI] [PubMed] [Google Scholar]
- Bolke E., Orth K., Gerber P. A., Lammering G., Mota R., Peiper M., Matuschek C., Budach W., Rusnak E., Shaikh S. et al. (2009). Gene expression of circulating tumour cells in breast cancer patients. Eur. J. Med. Res. 14, 426-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borcherding N., Bormann N., Kusner D., Kolb R. and Zhang W. (2015). Transcriptome analysis of basal and luminal tumor-initiating cells in ErbB2-driven breast cancer. Genomics Data 4, 119-122. 10.1016/j.gdata.2015.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravo-Cordero J. J., Magalhaes M. A. O., Eddy R. J., Hodgson L. and Condeelis J. (2013). Functions of cofilin in cell locomotion and invasion. Nat. Rev. Mol. Cell Biol. 14, 405-417. 10.1038/nrm3609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenton J. D., Carey L. A., Ahmed A. A. and Caldas C. (2005). Molecular classification and molecular forecasting of breast cancer: ready for clinical application? J. Clin. Oncol. 23, 7350-7360. 10.1200/JCO.2005.03.3845 [DOI] [PubMed] [Google Scholar]
- Bueno-de-Mesquita J. M., Linn S. C., Keijzer R., Wesseling J., Nuyten D. S. A., van Krimpen C., Meijers C., de Graaf P. W., Bos M. M. E., Hart A. A. M. et al. (2009). Validation of 70-gene prognosis signature in node-negative breast cancer. Breast Cancer Res. Treat. 117, 483-495. 10.1007/s10549-008-0191-2 [DOI] [PubMed] [Google Scholar]
- Buyse M., Loi S., van't Veer L., Viale G., Delorenzi M., Glas A. M., d'Assignies M. S., Bergh J., Lidereau R., Ellis P. et al. (2006). Validation and clinical utility of a 70-gene prognostic signature for women with node-negative breast cancer. J. Natl. Cancer Inst. 98, 1183-1192. 10.1093/jnci/djj329 [DOI] [PubMed] [Google Scholar]
- Cassatella M. C., Zorzino L. and Sandri M. T. (2012). Single circulating tumor cell profiling: a new perspective for targeted therapy? Future Oncol. 8, 1253-1256. 10.2217/fon.12.119 [DOI] [PubMed] [Google Scholar]
- Chia S. K., Bramwell V. H., Tu D., Shepherd L. E., Jiang S., Vickery T., Mardis E., Leung S., Ung K., Pritchard K. I. et al. (2012). A 50-gene intrinsic subtype classifier for prognosis and prediction of benefit from adjuvant tamoxifen. Clin. Cancer Res. 18, 4465-4472. 10.1158/1078-0432.CCR-12-0286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobleigh M. A., Tabesh B., Bitterman P., Baker J., Cronin M., Liu M.-L., Borchik R., Mosquera J.-M., Walker M. G. and Shak S. (2005). Tumor gene expression and prognosis in breast cancer patients with 10 or more positive lymph nodes. Clin. Cancer Res. 11, 8623-8631. 10.1158/1078-0432.CCR-05-0735 [DOI] [PubMed] [Google Scholar]
- Cronin M., Pho M., Dutta D., Stephans J. C., Shak S., Kiefer M. C., Esteban J. M. and Baker J. B. (2004). Measurement of gene expression in archival paraffin-embedded tissues: development and performance of a 92-gene reverse transcriptase-polymerase chain reaction assay. Am. J. Pathol. 164, 35-42. 10.1016/S0002-9440(10)63093-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronin M., Sangli C., Liu M.-L., Pho M., Dutta D., Nguyen A., Jeong J., Wu J., Langone K. C. and Watson D. (2007). Analytical validation of the Oncotype DX genomic diagnostic test for recurrence prognosis and therapeutic response prediction in node-negative, estrogen receptor-positive breast cancer. Clin. Chem. 53, 1084-1091. 10.1373/clinchem.2006.076497 [DOI] [PubMed] [Google Scholar]
- Curtis C. (2015). Genomic profiling of breast cancers. Curr. Opin. Obstet. Gynecol. 27, 34-39. 10.1097/GCO.0000000000000145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis C., Shah S. P., Chin S. F., Turashvili G., Rueda O. M., Dunning M. J., Speed D., Lynch A. G., Samarajiwa S., Yuan Y. et al. (2012). The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature 486, 346-352. 10.1038/nature10983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuzick J., Dowsett M., Pineda S., Wale C., Salter J., Quinn E., Zabaglo L., Mallon E., Green A. R., Ellis I. O. et al. (2011). Prognostic value of a combined estrogen receptor, progesterone receptor, Ki-67, and human epidermal growth factor receptor 2 immunohistochemical score and comparison with the Genomic Health recurrence score in early breast cancer. J. Clin. Oncol. 29, 4273-4278. 10.1200/JCO.2010.31.2835 [DOI] [PubMed] [Google Scholar]
- Daly T. M., Dumaual C. M., Dotson C. A., Farmen M. W., Kadam S. K. and Hockett R. D. (2005). Precision profiling and components of variability analysis for Affymetrix microarray assays run in a clinical context. J. Mol. Diagn. 7, 404-412. 10.1016/S1525-1578(10)60570-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Mattos-Arruda L., Cortes J., Santarpia L., Vivancos A., Tabernero J., Reis-Filho J. S. and Seoane J. (2013). Circulating tumour cells and cell-free DNA as tools for managing breast cancer. Nat. Rev. Clin. Oncol. 10, 377-389. 10.1038/nrclinonc.2013.80 [DOI] [PubMed] [Google Scholar]
- Esteva F. J., Sahin A. A., Cristofanilli M., Coombes K., Lee S.-J., Baker J., Cronin M., Walker M., Watson D., Shak S. et al. (2005). Prognostic role of a multigene reverse transcriptase-PCR assay in patients with node-negative breast cancer not receiving adjuvant systemic therapy. Clin. Cancer Res. 11, 3315-3319. 10.1158/1078-0432.CCR-04-1707 [DOI] [PubMed] [Google Scholar]
- Evaluation of Genomic Applications in Practice and Prevention (EGAPP) Working Group (2009). Recommendations from the EGAPP Working Group: can tumor gene expression profiling improve outcomes in patients with breast cancer? Genet. Med. 11, 66-73. 10.1097/GIM.0b013e3181928f56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falato C., Lorent J., Tani E., Karlsson E., Wright P. K., Bergh J. and Foukakis T. (2014). Ki67 measured in metastatic tissue and prognosis in patients with advanced breast cancer. Breast Cancer Res. Treat. 147, 407-414. 10.1007/s10549-014-3096-2 [DOI] [PubMed] [Google Scholar]
- Feng W., Gentles A., Nair R. V., Huang M., Lin Y., Lee C. Y., Cai S., Scheeren F. A., Kuo A. H. and Diehn M. (2014). Targeting unique metabolic properties of breast tumor initiating cells. Stem Cells 32, 1734-1745. 10.1002/stem.1662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fina E., Callari M., Reduzzi C., D'Aiuto F., Mariani G., Generali D., Pierotti M. A., Daidone M. G. and Cappelletti V. (2015). Gene expression profiling of circulating tumor cells in breast cancer. Clin. Chem. 61, 278-289. 10.1373/clinchem.2014.229476 [DOI] [PubMed] [Google Scholar]
- Forget M. A., Voorhees J. L., Cole S. L., Dakhlallah D., Patterson I. L., Gross A. C., Moldovan L., Mo X., Evans R., Marsh C. B. et al. (2014). Macrophage colony-stimulating factor augments Tie2-expressing monocyte differentiation, angiogenic function, and recruitment in a mouse model of breast cancer. PLoS ONE 9, e98623 10.1371/journal.pone.0098623 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Forse C. L., Agarwal S., Pinnaduwage D., Gertler F., Condeelis J. S., Lin J., Xue X., Johung K., Mulligan A. M., Rohan T. E. et al. (2015). Menacalc, a quantitative method of metastasis assessment, as a prognostic marker for axillary node-negative breast cancer. BMC Cancer 15, 483 10.1186/s12885-015-1468-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gertler F. and Condeelis J. (2011). Metastasis: tumor cells becoming MENAcing. Trends Cell Biol. 21, 81-90. 10.1016/j.tcb.2010.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gervasoni A., Monasterio Muñoz R. M., Wengler G. S., Rizzi A., Zaniboni A. and Parolini O. (2008). Molecular signature detection of circulating tumor cells using a panel of selected genes. Cancer Lett. 263, 267-279. 10.1016/j.canlet.2008.01.003 [DOI] [PubMed] [Google Scholar]
- Gligorijevic B., Bergman A. and Condeelis J. (2014). Multiparametric classification links tumor microenvironments with tumor cell phenotype. PLoS Biol. 12, e1001995 10.1371/journal.pbio.1001995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goswami S., Wang W., Wyckoff J. B. and Condeelis J. S. (2004). Breast cancer cells isolated by chemotaxis from primary tumors show increased survival and resistance to chemotherapy. Cancer Res. 64, 7664-7667. 10.1158/0008-5472.CAN-04-2027 [DOI] [PubMed] [Google Scholar]
- Goswami S., Philippar U., Sun D., Patsialou A., Avraham J., Wang W., Di Modugno F., Nistico P., Gertler F. B. and Condeelis J. S. (2009). Identification of invasion specific splice variants of the cytoskeletal protein Mena present in mammary tumor cells during invasion in vivo. Clin. Exp. Metastasis 26, 153-159. 10.1007/s10585-008-9225-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gradilone A., Raimondi C., Nicolazzo C., Petracca A., Gandini O., Vincenzi B., Naso G., Aglianò A. M., Cortesi E. and Gazzaniga P. (2011). Circulating tumour cells lacking cytokeratin in breast cancer: the importance of being mesenchymal. J. Cell Mol. Med. 15, 1066-1070. 10.1111/j.1582-4934.2011.01285.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habel L. A., Shak S., Jacobs M. K., Capra A., Alexander C., Pho M., Baker J., Walker M., Watson D., Hackett J. et al. (2006). A population-based study of tumor gene expression and risk of breast cancer death among lymph node-negative patients. Breast Cancer Res. 8, R25 10.1186/bcr1412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanahan D. and Weinberg R. A. (2011). Hallmarks of cancer: the next generation. Cell 144, 646-674. 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- Harney A. S., Arwert E. N., Entenberg D., Wang Y., Guo P., Qian B.-Z., Oktay M. H., Pollard J. W., Jones J. G. and Condeelis J. S. (2015). Real-Time imaging reveals local, transient vascular permeability, and tumor cell intravasation stimulated by TIE2hi macrophage-derived VEGFA. Cancer Discov. 5, 932-943. 10.1158/2159-8290.CD-15-0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvell D. M. E., Spoelstra N. S., Singh M., McManaman J. L., Finlayson C., Phang T., Trapp S., Hunter L., Dye W. W., Borges V. F. et al. (2008). Molecular signatures of neoadjuvant endocrine therapy for breast cancer: characteristics of response or intrinsic resistance. Breast Cancer Res. Treat. 112, 475-488. 10.1007/s10549-008-9897-4 [DOI] [PubMed] [Google Scholar]
- Hernandez L., Smirnova T., Wyckoff J., Condeelis J. and Segall J. E. (2009). In vivo assay for tumor cell invasion. Methods Mol. Biol. 571, 227-238. 10.1007/978-1-60761-198-1_15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes R., Qian B.-Z., Rowan C., Muthana M., Keklikoglou I., Olson O. C., Tazzyman S., Danson S., Addison C., Clemons M. et al. (2015a). Perivascular M2 macrophages stimulate tumor relapse after chemotherapy. Cancer Res. 75, 3479-3491. 10.1158/0008-5472.CAN-14-3587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes S. K., Oudin M. J., Tadros J., Neil J., Del Rosario A., Joughin B. A., Ritsma L., Wyckoff J., Vasile E., Eddy R. et al. (2015b). PTP1B-dependent regulation of receptor tyrosine kinase signaling by the actin-binding protein Mena. Mol. Biol. Cell 26, 3867-3878. 10.1091/mbc.E15-06-0442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalluri R. (2009). EMT: when epithelial cells decide to become mesenchymal-like cells. J. Clin. Invest. 119, 1417-1419. 10.1172/JCI39675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalluri R. and Weinberg R. A. (2009). The basics of epithelial-mesenchymal transition. J. Clin. Invest. 119, 1420-1428. 10.1172/JCI39104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly C. M., Bernard P. S., Krishnamurthy S., Wang B., Ebbert M. T. W., Bastien R. R. L., Boucher K. M., Young E., Iwamoto T. and Pusztai L. (2012). Agreement in risk prediction between the 21-gene recurrence score assay (Oncotype DX(R)) and the PAM50 breast cancer intrinsic Classifier in early-stage estrogen receptor-positive breast cancer. Oncologist 17, 492-498. 10.1634/theoncologist.2012-0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang J. E., Scott J. H., Wolf D. M., Novak P., Punj V., Magbanua M. J. M., Zhu W., Mineyev N., Haqq C. M., Crothers J. R. et al. (2015). Expression profiling of circulating tumor cells in metastatic breast cancer. Breast Cancer Res. Treat. 149, 121-131. 10.1007/s10549-014-3215-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson D. A., Bhakta N. R., Kessenbrock K., Prummel K. D., Yu Y., Takai K., Zhou A., Eyob H., Balakrishnan S., Wang C. Y. et al. (2015). Single-cell analysis reveals a stem-cell program in human metastatic breast cancer cells. Nature 526, 131-135. 10.1038/nature15260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lianidou E. S. and Markou A. (2012). Molecular assays for the detection and characterization of CTCs. Recent Results Cancer Res. 195, 111-123. 10.1007/978-3-642-28160-0_10 [DOI] [PubMed] [Google Scholar]
- Lianidou E. S., Markou A. and Strati A. (2012). Molecular characterization of circulating tumor cells in breast cancer: challenges and promises for individualized cancer treatment. Cancer Metastasis Rev. 31, 663-671. 10.1007/s10555-012-9366-8 [DOI] [PubMed] [Google Scholar]
- Lu H., Clauser K. R., Tam W. L., Fröse J., Ye X., Eaton E. N., Reinhardt F., Donnenberg V. S., Bhargava R., Carr S. A. et al. (2014). A breast cancer stem cell niche supported by juxtacrine signalling from monocytes and macrophages. Nat. Cell Biol. 16, 1105-1117. 10.1038/ncb3041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magbanua M. J. M. and Park J. W. (2013). Isolation of circulating tumor cells by immunomagnetic enrichment and fluorescence-activated cell sorting (IE/FACS) for molecular profiling. Methods 64, 114-118. 10.1016/j.ymeth.2013.07.029 [DOI] [PubMed] [Google Scholar]
- Magbanua M. J. M. and Park J. W. (2014). Advances in genomic characterization of circulating tumor cells. Cancer Metastasis Rev. 33, 757-769. 10.1007/s10555-014-9503-7 [DOI] [PubMed] [Google Scholar]
- Martín M., Prat A., Rodríguez-Lescure A., Caballero R., Ebbert M. T. W., Munárriz B., Ruiz-Borrego M., Bastien R. R. L., Crespo C., Davis C. et al. (2013). PAM50 proliferation score as a predictor of weekly paclitaxel benefit in breast cancer. Breast Cancer Res. Treat. 138, 457-466. 10.1007/s10549-013-2416-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metz C. E. (1978). Basic principles of ROC analysis. Semin. Nucl. Med. 8, 283-298. 10.1016/S0001-2998(78)80014-2 [DOI] [PubMed] [Google Scholar]
- Mook S., Schmidt M. K., Viale G., Pruneri G., Eekhout I., Floore A., Glas A. M., Bogaerts J., Cardoso F., Piccart-Gebhart M. J. et al. (2009). The 70-gene prognosis-signature predicts disease outcome in breast cancer patients with 1–3 positive lymph nodes in an independent validation study. Breast Cancer Res. Treat. 116, 295-302. 10.1007/s10549-008-0130-2 [DOI] [PubMed] [Google Scholar]
- Mook S., Schmidt M. K., Weigelt B., Kreike B., Eekhout I., van de Vijver M. J., Glas A. M., Floore A., Rutgers E. J. and van ‘t Veer L. J. (2010). The 70-gene prognosis signature predicts early metastasis in breast cancer patients between 55 and 70 years of age. Ann. Oncol. 21, 717-722. 10.1093/annonc/mdp388 [DOI] [PubMed] [Google Scholar]
- Nielsen T. O., Parker J. S., Leung S., Voduc D., Ebbert M., Vickery T., Davies S. R., Snider J., Stijleman I. J., Reed J. et al. (2010). A comparison of PAM50 intrinsic subtyping with immunohistochemistry and clinical prognostic factors in tamoxifen-treated estrogen receptor-positive breast cancer. Clin. Cancer. Res. 16, 5222-5232. 10.1158/1078-0432.CCR-10-1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oktay M. H. and Jones J. G. (2015). TMEM: a novel breast cancer dissemination marker for the assessment of metastatic risk. Biomark. Med. 9, 81-84. 10.2217/bmm.14.104 [DOI] [PubMed] [Google Scholar]
- Paik S., Shak S., Tang G., Kim C., Baker J., Cronin M., Baehner F. L., Walker M. G., Watson D., Park T. et al. (2004). A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N. Engl. J. Med. 351, 2817-2826. 10.1056/NEJMoa041588 [DOI] [PubMed] [Google Scholar]
- Paik S., Tang G., Shak S., Kim C., Baker J., Kim W., Cronin M., Baehner F. L., Watson D., Bryant J. et al. (2006). Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J. Clin. Oncol. 24, 3726-3734. 10.1200/JCO.2005.04.7985 [DOI] [PubMed] [Google Scholar]
- Pantel K. and Alix-Panabieres C. (2013). Real-time liquid biopsy in cancer patients: fact or fiction? Cancer Res. 73, 6384-6388. 10.1158/0008-5472.CAN-13-2030 [DOI] [PubMed] [Google Scholar]
- Parker J. S., Mullins M., Cheang M. C. U., Leung S., Voduc D., Vickery T., Davies S., Fauron C., He X., Hu Z. et al. (2009). Supervised risk predictor of breast cancer based on intrinsic subtypes. J. Clin. Oncol. 27, 1160-1167. 10.1200/JCO.2008.18.1370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patsialou A. and Condeelis J. S. (2014). Metastatic cells: moving onco-targets. Oncotarget 5, 3424-3425. 10.18632/oncotarget.2057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patsialou A., Wang Y., Lin J., Whitney K., Goswami S., Kenny P. A. and Condeelis J. S. (2012). Selective gene-expression profiling of migratory tumor cells in vivo predicts clinical outcome in breast cancer patients. Breast Cancer Res. 14, R139 10.1186/bcr3344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patsialou A., Bravo-Cordero J. J., Wang Y., Entenberg D., Liu H., Clarke M. and Condeelis J. S. (2013). Intravital multiphoton imaging reveals multicellular streaming as a crucial component of in vivo cell migration in human breast tumors. Intravital 2, e25294 10.4161/intv.25294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perou C. M., Sørlie T., Eisen M. B., van de Rijn M., Jeffrey S. S., Rees C. A., Pollack J. R., Ross D. T., Johnsen H., Akslen L. A. et al. (2000). Molecular portraits of human breast tumours. Nature 406, 747-752. 10.1038/35021093 [DOI] [PubMed] [Google Scholar]
- Philippar U., Roussos E. T., Oser M., Yamaguchi H., Kim H.-D., Giampieri S., Wang Y., Goswami S., Wyckoff J. B., Lauffenburger D. A. et al. (2008). A Mena invasion isoform potentiates EGF-induced carcinoma cell invasion and metastasis. Dev. Cell 15, 813-828. 10.1016/j.devcel.2008.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pignatelli J., Goswami S., Jones J. G., Rohan T. E., Pieri E., Chen X., Adler E., Cox D., Maleki S., Bresnick A. et al. (2014). Invasive breast carcinoma cells from patients exhibit MenaINV- and macrophage-dependent transendothelial migration. Sci. Signal. 7, ra112 10.1126/scisignal.2005329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polzer B., Medoro G., Pasch S., Fontana F., Zorzino L., Pestka A., Andergassen U., Meier-Stiegen F., Czyz Z. T., Alberter B. et al. (2014). Molecular profiling of single circulating tumor cells with diagnostic intention. EMBO Mol. Med. 6, 1371-1386. 10.15252/emmm.201404033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell A. A., Talasaz A. H., Zhang H., Coram M. A., Reddy A., Deng G., Telli M. L., Advani R. H., Carlson R. W., Mollick J. A. et al. (2012). Single cell profiling of circulating tumor cells: transcriptional heterogeneity and diversity from breast cancer cell lines. PLoS ONE 7, e33788 10.1371/journal.pone.0033788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prat A., Bianchini G., Thomas M., Belousov A., Cheang M. C. U., Koehler A., Gomez P., Semiglazov V., Eiermann W., Tjulandin S. et al. (2014). Research-based PAM50 subtype predictor identifies higher responses and improved survival outcomes in HER2-positive breast cancer in the NOAH study. Clin. Cancer Res. 20, 511-521. 10.1158/1078-0432.CCR-13-0239 [DOI] [PubMed] [Google Scholar]
- Pucci F., Venneri M. A., Biziato D., Nonis A., Moi D., Sica A., Di Serio C., Naldini L. and De Palma M. (2009). A distinguishing gene signature shared by tumor-infiltrating Tie2-expressing monocytes, blood “resident” monocytes, and embryonic macrophages suggests common functions and developmental relationships. Blood 114, 901-914. 10.1182/blood-2009-01-200931 [DOI] [PubMed] [Google Scholar]
- Pukazhendhi G. and Glück S. (2014). Circulating tumor cells in breast cancer. J. Carcinog. 13, 8 10.4103/1477-3163.135578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radaelli E., Damonte P. and Cardiff R. D. (2009). Epithelial–mesenchymal transition in mouse mammary tumorigenesis. Future Oncol. 5, 1113-1127. 10.2217/fon.09.93 [DOI] [PubMed] [Google Scholar]
- Rakha E. A., El-Sayed M. E., Reis-Filho J. and Ellis I. O. (2009). Patho-biological aspects of basal-like breast cancer. Breast Cancer Res. Treat. 113, 411-422. 10.1007/s10549-008-9952-1 [DOI] [PubMed] [Google Scholar]
- Riabov V., Gudima A., Wang N., Mickley A., Orekhov A. and Kzhyshkowska J. (2014). Role of tumor associated macrophages in tumor angiogenesis and lymphangiogenesis. Front. Physiol. 5, 75 10.3389/fphys.2014.00075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson B. D., Sica G. L., Liu Y.-F., Rohan T. E., Gertler F. B., Condeelis J. S. and Jones J. G. (2009). Tumor microenvironment of metastasis in human breast carcinoma: a potential prognostic marker linked to hematogenous dissemination. Clin. Cancer Res. 15, 2433-2441. 10.1158/1078-0432.CCR-08-2179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohan T. E., Xue X., Lin H.-M., D'Alfonso T. M., Ginter P. S., Oktay M. H., Robinson B. D., Ginsberg M., Gertler F. B., Glass A. G. et al. (2014). Tumor microenvironment of metastasis and risk of distant metastasis of breast cancer. J. Natl. Cancer Inst. 106, dju136 10.1093/jnci/dju136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roh-Johnson M., Bravo-Cordero J. J., Patsialou A., Sharma V. P., Guo P., Liu H., Hodgson L. and Condeelis J. (2014). Macrophage contact induces RhoA GTPase signaling to trigger tumor cell intravasation. Oncogene 33, 4203-4212. 10.1038/onc.2013.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roussos E. T., Balsamo M., Alford S. K., Wyckoff J. B., Gligorijevic B., Wang Y., Pozzuto M., Stobezki R., Goswami S., Segall J. E. et al. (2011a). Mena invasive (MenaINV) promotes multicellular streaming motility and transendothelial migration in a mouse model of breast cancer. J. Cell Sci. 124, 2120-2131. 10.1242/jcs.086231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roussos E. T., Condeelis J. S. and Patsialou A. (2011b). Chemotaxis in cancer. Nat. Rev. Cancer 11, 573-587. 10.1038/nrc3078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roussos E. T., Goswami S., Balsamo M., Wang Y., Stobezki R., Adler E., Robinson B. D., Jones J. G., Gertler F. B., Condeelis J. S. et al. (2011c). Mena invasive (Mena(INV)) and Mena11a isoforms play distinct roles in breast cancer cell cohesion and association with TMEM. Clin. Exp. Metastasis 28, 515-527. 10.1007/s10585-011-9388-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rouzier R., Perou C. M., Symmans W. F., Ibrahim N., Cristofanilli M., Anderson K., Hess K. R., Stec J., Ayers M., Wagner P. et al. (2005). Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin. Cancer Res. 11, 5678-5685. 10.1158/1078-0432.CCR-04-2421 [DOI] [PubMed] [Google Scholar]
- Shipitsin M., Campbell L. L., Argani P., Weremowicz S., Bloushtain-Qimron N., Yao J., Nikolskaya T., Serebryiskaya T., Beroukhim R., Hu M. et al. (2007). Molecular definition of breast tumor heterogeneity. Cancer Cell 11, 259-273. 10.1016/j.ccr.2007.01.013 [DOI] [PubMed] [Google Scholar]
- Simon R., Radmacher M. D., Dobbin K. and McShane L. M. (2003). Pitfalls in the use of DNA microarray data for diagnostic and prognostic classification. J. Natl. Cancer Inst. 95, 14-18. 10.1093/jnci/95.1.14 [DOI] [PubMed] [Google Scholar]
- Sorlie T., Perou C. M., Tibshirani R., Aas T., Geisler S., Johnsen H., Hastie T., Eisen M. B., van de Rijn M., Jeffrey S. S. et al. (2001). Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc. Natl. Acad. Sci. USA 98, 10869-10874. 10.1073/pnas.191367098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorlie T., Tibshirani R., Parker J., Hastie T., Marron J. S., Nobel A., Deng S., Johnsen H., Pesich R., Geisler S. et al. (2003). Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc. Natl. Acad. Sci. USA 100, 8418-8423. 10.1073/pnas.0932692100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotiriou C. and Pusztai L. (2009). Gene-expression signatures in breast cancer. N. Engl. J. Med. 360, 790-800. 10.1056/NEJMra0801289 [DOI] [PubMed] [Google Scholar]
- Sparano J. A., Gray R. J., Makower D. F., Pritchard K. I., Albain K. S., Hayes D. F., Geyer C. E. Jr., Dees E. C., Perez E. A., Olson J. A. Jr.. et al. (2015). Prospective validation of a 21-gene expression assay in breast cancer. N. Engl. J. Med. 373, 2005-2014. 10.1056/NEJMoa1510764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squadrito M. L. and De Palma M. (2011). Macrophage regulation of tumor angiogenesis: implications for cancer therapy. Mol. Aspects Med. 32, 123-145. 10.1016/j.mam.2011.04.005 [DOI] [PubMed] [Google Scholar]
- Stec J., Wang J., Coombes K., Ayers M., Hoersch S., Gold D. L., Ross J. S., Hess K. R., Tirrell S., Linette G. et al. (2005). Comparison of the predictive accuracy of DNA array-based multigene classifiers across cDNA arrays and Affymetrix GeneChips. J. Mol. Diagn. 7, 357-367. 10.1016/S1525-1578(10)60565-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theodoropoulos P. A., Polioudaki H., Agelaki S., Kallergi G., Saridaki Z., Mavroudis D. and Georgoulias V. (2010). Circulating tumor cells with a putative stem cell phenotype in peripheral blood of patients with breast cancer. Cancer Lett. 288, 99-106. 10.1016/j.canlet.2009.06.027 [DOI] [PubMed] [Google Scholar]
- van de Vijver M. J., He Y. D., van ‘t Veer L. J., Dai H., Hart A. A. M., Voskuil D. W., Schreiber G. J., Peterse J. L., Roberts C., Marton M. J. et al. (2002). A gene-expression signature as a predictor of survival in breast cancer. N. Engl. J. Med. 347, 1999-2009. 10.1056/NEJMoa021967 [DOI] [PubMed] [Google Scholar]
- van ‘t Veer L. J., Dai H., van de Vijver M. J., He Y. D., Hart A. A. M., Mao M., Peterse H. L., van der Kooy K., Marton M. J., Witteveen A. T. et al. (2002). Gene expression profiling predicts clinical outcome of breast cancer. Nature 415, 530-536. 10.1038/415530a [DOI] [PubMed] [Google Scholar]
- Venet D., Dumont J. E. and Detours V. (2011). Most random gene expression signatures are significantly associated with breast cancer outcome. PLoS Comput. Biol. 7, e1002240 10.1371/journal.pcbi.1002240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venneri M. A., De Palma M., Ponzoni M., Pucci F., Scielzo C., Zonari E., Mazzieri R., Doglioni C. and Naldini L. (2007). Identification of proangiogenic TIE2-expressing monocytes (TEMs) in human peripheral blood and cancer. Blood 109, 5276-5285. 10.1182/blood-2006-10-053504 [DOI] [PubMed] [Google Scholar]
- Wang W., Wyckoff J. B., Wang Y., Bottinger E. P., Segall J. E. and Condeelis J. S. (2003). Gene expression analysis on small numbers of invasive cells collected by chemotaxis from primary mammary tumors of the mouse. BMC Biotechnol. 3, 13 10.1186/1472-6750-3-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Goswami S., Lapidus K., Wells A. L., Wyckoff J. B., Sahai E., Singer R. H., Segall J. E. and Condeelis J. S. (2004). Identification and testing of a gene expression signature of invasive carcinoma cells within primary mammary tumors. Cancer Res. 64, 8585-8594. 10.1158/0008-5472.CAN-04-1136 [DOI] [PubMed] [Google Scholar]
- Wang W., Goswami S., Sahai E., Wyckoff J. B., Segall J. E. and Condeelis J. S. (2005). Tumor cells caught in the act of invading: their strategy for enhanced cell motility. Trends Cell Biol. 15, 138-145. 10.1016/j.tcb.2005.01.003 [DOI] [PubMed] [Google Scholar]
- Wang W., Mouneimne G., Sidani M., Wyckoff J., Chen X., Makris A., Goswami S., Bresnick A. R. and Condeelis J. S. (2006). The activity status of cofilin is directly related to invasion, intravasation, and metastasis of mammary tumors. J. Cell Biol. 173, 395-404. 10.1083/jcb.200510115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Eddy R. and Condeelis J. (2007). The cofilin pathway in breast cancer invasion and metastasis. Nat. Rev. Cancer 7, 429-440. 10.1038/nrc2148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitsman G., Lawler K., Kelleher M. T., Barrett J. E., Barber P. R., Shamil E., Festy F., Patel G., Fruhwirth G. O., Huang L. et al. (2014). Imaging tumour heterogeneity of the consequences of a PKCalpha-substrate interaction in breast cancer patients. Biochem. Soc. Trans. 42, 1498-1505. 10.1042/BST20140165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirapati P., Sotiriou C., Kunkel S., Farmer P., Pradervand S., Haibe-Kains B., Desmedt C., Ignatiadis M., Sengstag T., Schutz F. et al. (2008). Meta-analysis of gene-expression profiles in breast cancer: toward a unified understanding of breast cancer sub-typing and prognosis signatures. Breast Cancer Res. 10, R65 10.1186/bcr2124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wishart G. C., Rakha E., Green A., Ellis I., Ali H. R., Provenzano E., Blows F. M., Caldas C. and Pharoah P. D. (2014). Inclusion of KI67 significantly improves performance of the PREDICT prognostication and prediction model for early breast cancer. BMC Cancer 14, 908 10.1186/1471-2407-14-908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittner B. S., Sgroi D. C., Ryan P. D., Bruinsma T. J., Glas A. M., Male A., Dahiya S., Habin K., Bernards R., Haber D. A. et al. (2008). Analysis of the MammaPrint breast cancer assay in a predominantly postmenopausal cohort. Clin. Cancer Res. 14, 2988-2993. 10.1158/1078-0432.CCR-07-4723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyckoff J. B., Segall J. E. and Condeelis J. S. (2000). The collection of the motile population of cells from a living tumor. Cancer Res. 60, 5401-5404. [PubMed] [Google Scholar]
- Wyckoff J. B., Wang Y., Lin E. Y., Li J.-f., Goswami S., Stanley E. R., Segall J. E., Pollard J. W. and Condeelis J. (2007). Direct visualization of macrophage-assisted tumor cell intravasation in mammary tumors. Cancer Res. 67, 2649-2656. 10.1158/0008-5472.CAN-06-1823 [DOI] [PubMed] [Google Scholar]
- Wyckoff J., Gligorijevic B., Entenberg D., Segall J. and Condeelis J. (2011). The in vivo invasion assay: preparation and handling of collection needles. Cold Spring Harb. Protoc. 2011, 1232-1234. 10.1101/pdb.prot065912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu M., Bardia A., Wittner B. S., Stott S. L., Smas M. E., Ting D. T., Isakoff S. J., Ciciliano J. C., Wells M. N., Shah A. M. et al. (2013). Circulating breast tumor cells exhibit dynamic changes in epithelial and mesenchymal composition. Science 339, 580-584. 10.1126/science.1228522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zurrida S., Bagnardi V., Curigliano G., Mastropasqua M. G., Orecchia R., Disalvatore D., Greco M., Cataliotti L., D'Aiuto G., Talakhadze N. et al. (2013). High Ki67 predicts unfavourable outcomes in early breast cancer patients with a clinically clear axilla who do not receive axillary dissection or axillary radiotherapy. Eur. J. Cancer 49, 3083-3092. 10.1016/j.ejca.2013.05.007 [DOI] [PubMed] [Google Scholar]