Abstract
Introduction and Rationale
Influenza and pneumonia remain serious health concerns for long-term care (LTC) residents. Vaccination of LTC residents and health care workers are reasonable preventive strategies, although most facilities fall short of Healthy People 2010 goals. Improving immunization rates across multiple LTC facilities remains an elusive challenge. This quality improvement study sought to improve immunization rates across 6 LTC facilities and identify persistent barriers to better performance.
Methods
In 2002, 6 facilities associated with the University of Pittsburgh Institute on Aging established a quality improvement network addressing immunization rates. The facilities were provided with a written educational toolkit and shared information through an e-mail distribution list. To help determine optimal program structure in future years, 3 of the facilities participated in a single half-day collaborative training session. Change in immunization rates from baseline to year 2 were compared between those participating in the collaborative training and those not participating. Barriers to improved performance were sought from all groups through focus group analysis.
Results
Facilities participating in the single collaborative training program improved immunization rates modestly, whereas facilities not participating in the collaborative training saw decreases in immunization rates. Staff turnover was cited as a significant barrier to improved performance.
Discussion
It may be possible to improve immunization rates in LTC facilities, at least modestly, using a collaborative training process. Staff turnover may be an important barrier to improved LTC immunization rates.
Keywords: Nursing homes, immunizations, influenza, health care workers, pneumococcal vaccine
Influenza and pneumonia collectively represent the eighth leading cause of death and the leading cause of vaccine-preventable deaths in the United States.1 and 2 Most influenza and pneumonia deaths occur in older adults and disproportionately affect those residing in long-term care (LTC) facilities. Influenza case fatality rates range between 5% and 55% and pneumococcal case fatality rates of 27% have been reported in nursing homes.2 and 3 Both conditions are also responsible for as many as 430,000 hospitalizations, a rate that appears to be increasing.4, 5 and 6
Immunizing residents against influenza and pneumococcal disease may help to reduce outbreaks, hospitalizations, pneumonia, and death.7 and 8 As a result, Healthy People 2010 has set resident immunization goals of 90% for influenza and pneumococcal vaccinations.9 Despite the clear impact of these conditions and the established goals, only 60% to 66% of institutionalized adults are immunized each year against influenza and 38% against pneumococcal disease.10
Health care worker (HCW) immunization has been advocated by many organizations, including the Advisory Committee on Immunization Practices, to reduce the transmission and consequences of influenza in health care settings. Several studies suggest mortality may be reduced by as much as 40% when HCWs are immunized against influenza.11, 12 and 13 Despite current research and recommendations, HCW influenza immunization rates remain unchanged at 37% to 40% over the past decade.10, 14, 15 and 16
Since the mid 1990s, the University of Pittsburgh Institute on Aging has focused on improving influenza and pneumococcal immunization rates. Pilot work showed that organizational change within a single facility was possible and sustainable.17 A significant question was whether we could translate immunization strategies to other facilities so as to improve influenza and pneumococcal immunization rates. The primary objective of this quality improvement project was to improve immunization rates among health care workers for influenza and among residents for influenza and pneumococcal vaccines in a network of collaborating nursing homes. The secondary objective was to identify barriers to immunization by conducting focus groups in collaborating nursing homes to help improve immunization rates in subsequent studies.
Methods
The University of Pittsburgh Institute on Aging established an influenza and pneumococcal immunization program in 2002 whose purpose it was to assist LTC facilities in improving immunization rates among residents and HCWs. It was initiated in response to the Long-Term Care Resident and Employee Immunization Act 95, a regulation passed in Pennsylvania in March 2002 requiring LTC facilities to offer influenza vaccine to all residents and HCWs, and pneumococcal vaccine to residents. Six LTC facilities in western Pennsylvania participated in this program.
Between March 2002 and October 2003, participating facilities assembled immunization teams of at least 4 staff members. The teams assessed their facility's baseline immunization program, calculated immunization rates, and planned and implemented changes to their immunization programs.
At the beginning of the project, participating facilities were provided with a copy of the American Medical Directors Association Immunization Toolkit.18 An e -mail distribution list was created to facilitate communication, reinforce project goals, and share the successes and failures of participating facilities. Examples of issues communicated through the distribution list included the release of the Centers for Medicare & Medicaid Services Standing Orders Program, updates on local and national influenza activity, and details of Act 95. Three of the 6 facilities were randomly selected to participate in a single half-day collaborative training program held in October 2002 (hereafter referred to as collaborative versus noncollaborative facilities). The collaborative training program, based on the Institute for Healthcare Improvement model,19 provided didactic education, a review of baseline immunization rates, training in barrier identification, and goal setting.
Education focused on the impact and prevention of influenza and pneumococcal disease in the LTC setting and was presented by a LTC infectious disease specialist (R.M.). Acontent expert in LTC quality improvement (D.A.N.) facilitated barrier identification. Barriers were assessed by use of a Trotter matrix tool.20 The matrix listed the major tasks of immunization programs. Each immunization team assigned a rating to these tasks using a 5-point Likert scale (see Appendix 1). Based on the matrix assessments, teams defined program interventions, specified process and outcome measurements, and set completion time frames. No additional collaborative sessions were held. Immunization rates were obtained for all facilities by self-report. Baseline data for 2002 and follow-up data for 2003 were collected and compared to evaluate the program. The denominator for the resident immunizations was all residents residing in the facility as of March 2002 for the baseline period and as of March 2003 for the follow-up period. The numerator was the total number of residents residing in the facility as of March of the given year who had received influenza or pneumococcal vaccines. The denominator for employees was all health care workers currently employed at the facility as of March 2002 for the baseline period and as of March 2003 for the follow-up period. The numerator represented all of these health care workers who received the current season influenza vaccine by March of the given year. The primary outcomes were the change in immunization rates over time for the combined collaborative groups compared with the combined noncollaborative groups. Rates are also presented for each individual facility. The small number of facilities in this pilot quality improvement initiative precludes rigorous analysis, and so only descriptive results are presented.
At the end of the project, immunization team members from each facility were invited to participate in a focus group session. The focus group reviewed the project outcomes and identified significant immunization barriers still remaining.21
The University of Pittsburgh Institutional Review Board (IRB) staff deemed the project a quality improvement study exempt from IRB review.
Results
All 6 facilities were community-based, nonprofit facilities located in southwestern Pennsylvania. They were located in both urban and suburban settings, and 2 had unionized staff. Facility size ranged from 59 to 202 beds. None of the facilities used standing orders or a vaccine declination form during the project. Table 1describes the 6 facilities. Because this was a quality improvement initiative rather than a research study, information on resident and HCW demographics, HCW tenure, and HCW turnover was not collected or analyzed.
Changes in vaccination rates are shown in Table 2. The HCW influenza immunization rate improved 10% in the collaborative group and decreased in the noncollaborative group. All 3 facilities in the collaborative group improved their HCW immunization rates although the amount varied. Only 1 of the noncollaborative facilities, Facility F, improved its HCW immunization rate (17%). Only 1 facility in the collaborative group exceeded the Healthy People 2010 goal for HCW of 60%.
Table 2.
Vaccination Rates
| Health Care Worker Influenza Vaccination Rates | |||
|---|---|---|---|
| Facility | 2002, % | 2003, % | Raw Change, % |
| Collaborative Group Rate | 39.2 | 50.1 | 10.9 |
| Facility A | 56.9 | 67.2 | 10.3 |
| Facility C | 14.3 | 36.2 | 21.9 |
| Facility E | 46.4 | 46.8 | 0.4 |
| Noncollaborative Group Rate | 29.3 | 25.8 | −3.5 |
| Facility B | 23.1 | 12.5 | −10.6 |
| Facility D | 47.1 | 30.3 | −16.7 |
| Facility F | 17.8 | 34.7 | 16.9 |
| Resident Influenza Vaccination Rates | |||
|---|---|---|---|
| Facility | 2002, % | 2003, % | Raw Change, % |
| Collaborative Group Rate | 73.8 | 77.8 | 4.0 |
| A–Collaborative | 61.9 | 88.7 | 26.8 |
| C–Collaborative | 86.4 | 91.5 | 5.1 |
| E–Collaborative | 73.1 | 53.2 | −19.9 |
| Noncollaborative Group Rate | 78.9 | 58.2 | −20.8 |
| B–Noncollaborative | 76.7 | 89.3 | 12.6 |
| D–Noncollaborative | 95.9 | 31.2 | −64.7 |
| F–Non-collaborative | 64.2 | 54.0 | −10.3 |
| Resident Pneumococcal Vaccination Rates | |||
|---|---|---|---|
| Facility | 2002, % | 2003, % | Raw Change, % |
| Collaborative Group Rate | 16.0 | 45.9 | 29.9 |
| A–Collaborative | 40.3 | 79.0 | 38.7 |
| C–Collaborative | 5.1 | 25.4 | 20.3 |
| E–Collaborative | 2.6 | 33.2 | 30.6 |
| Non-Collaborative Group Rate | 20.2 | 6.3 | −13.9 |
| B–Noncollaborative | 47.8 | 14.0 | −33.8 |
| D–Noncollaborative | 6.2 | 4.3 | −2.0 |
| F–Noncollaborative | 6.6 | 0.6 | −6.0 |
Resident influenza immunization rates improved slightly by 4% in the collaborative group, whereas the noncollaborative group declined by 20%. Baseline resident influenza vaccination rates were consistently higher than those for HCW or pneumococcal vaccination. Similar to HCW immunization, 1 facility in the collaborative group reached the Healthy People 2010 goal of 90%.
Resident pneumococcal vaccination rates increased in the collaborative group by almost 30%, and they declined by 14% in the noncollaborative group. Baseline pneumococcal immunization rates were very low across the facilities; none of the facilities came close to reaching the 90% Healthy People 2010 pneumococcal immunization goal.
Persisting barriers identified by the focus group are shown in Figure 1 . All of these immunization barriers are commonly cited, with the exception of one: staff turnover.
Fig. 1.
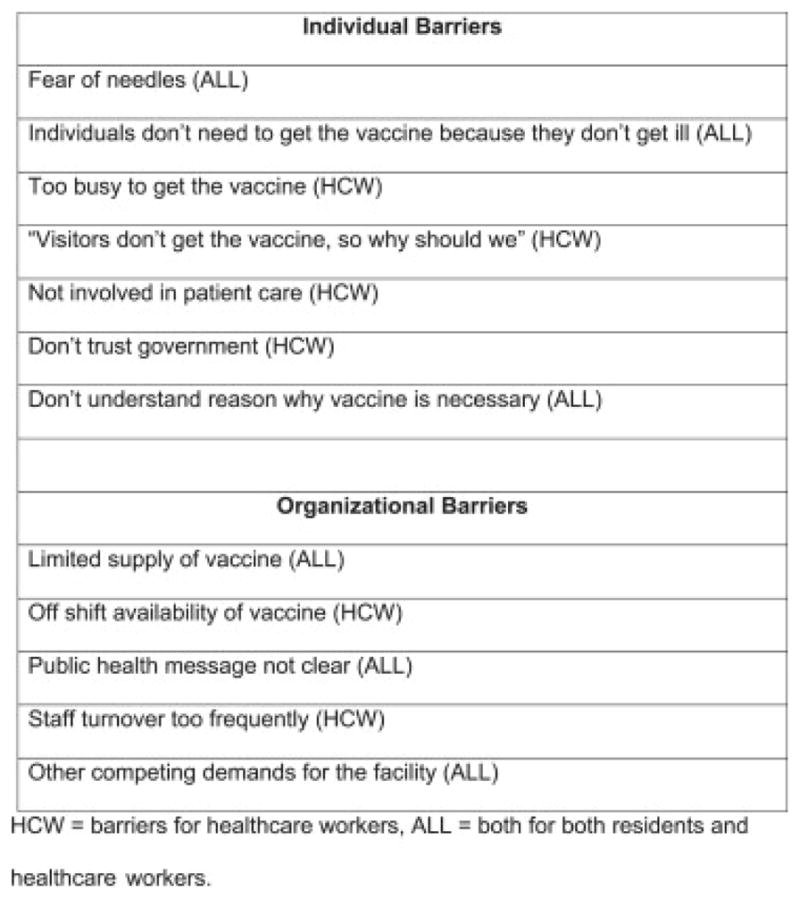
Individual and organizational barriers to immunization identified by focus group process.
Discussion
This clinical experience report describes the results of a pilot LTC immunization quality improvement program developed by the University of Pittsburgh Institute on Aging. The initiative focused on improving 3 immunization end points: HCW influenza immunizations, resident influenza immunizations, and resident pneumococcal immunizations. Our results suggest it is possible to improve influenza and pneumococcal immunization rates across a group of facilities. The collaborative program facilities showed improvement in all 3 measured immunization outcomes whereas the noncollaborative program facilities sustained decreases in these rates. This is consistent with the prevailing assumption that providing passive information, such as through written materials and e-mail, is not enough to stimulate organizational change. We were also able to identify barriers and facilitators to immunization. Included was staff turnover, a barrier that has received little attention in the literature.
Improving immunization rates in single LTC facilities requires a focus on organizational change. Our past work and that of others has shown this is possible through measured use of quality improvement methods.17, 22, 23 and 24 From a public health perspective, however, we have a pressing need to take successful individual programs and practices and disseminate them across groups of facilities, a step that has received little attention.25 Ef forts to date have relied on either mandatory approaches such as legislative or policy changes, or voluntary approaches such as education or quality improvement collaboratives. Outcome data on the impact of legislating LTC immunizations is very limited and has not shown significant improvements in rates.26 and 27 Education and health care collaboratives have shown some promise, but their overall impact has been moderate and variable.24 and 28 Thus, gaining a better understanding of these latter approaches is important in planning future initiatives. Our work here provides preliminary feedback on the design and implementation of a pilot immunization improvement program targeting multiple facilities in western Pennsylvania.
The strengths of this program include its prospective comparative design, the creation of immunization teams at each facility, use of focus group methodology, the diverse size and nature of the facilities participating, and the program's real world practicality. Process improvement teams, through emphasis on team collaboration, have been associated with improved performance in other outcomes.29 and 30 Facilities in this study were all required to establish an immunization team responsible for planning and carrying out immunization action plans. Focus group methodology enabled us to identify a potentially important HCW immunization barrier not previously described: the impact of staff turnover. High turnover has been linked to poorer nursing home care in general,31 and it could plausibly influence immunization rates as well. Although all the facilities in this study were nonprofit status, they varied in location, size, and staff unionization. Practicality was achieved by disseminating an inexpensive and widely available evidence-based immunization toolkit; using an e-mail communication network; and, for the collaborative group, using a single half-day training session. These components optimized the amount of support provided to each facility. Used jointly, they should promote sustainability and the ability to disseminate this work to other sites.
We recognize several limitations as well. First, a potential confounding variable was enactment of the Long-Term Care Resident and Employee Immunization Act 95, in March 2002. It is doubtful this affected our results, as the noncollaborative group's immunization rates did not improve, and because data collected by Pennsylvania has failed to show any impact of Act 95 during the project period (e-mail communication to authors by Brian Showalter, Program Analyst, PA Department of Health, June 7, 2006).
Second, although the collaborative groups performed better than the noncollaborative facilities, we cannot establish a causal link to the collaborative process. Although the facilities were randomly assigned to the collaborative training process, the number of facilities was small, limiting power, and we were unable to stratify them for baseline variables such as facility size, location, and baseline immunization rates. Because this was a quality improvement initiative, we do not have demographic information on the residents or HCW including age distribution, HCW tenure, or staff turnover rates, all of which can influence immunization performance. It is possible that unmeasured confounders exist between the 2 groups that could account for the observed differences. Such limitations are common to most published collaborative reports and have been extensively addressed elsewhere.32
Third, although the collaborative group's immunization rates improved, they fell short of the Healthy People 2010 goals. No facility reached the Healthy People 2010 goal for resident pneumococcal vaccination, and only 2 facilities reached Healthy People 2010 goals for HCW and resident influenza vaccination. The low success with pneumococcal vaccination is not surprising given the very low baseline immunization rates. The facilities would have had to increase their pneumococcal immunization rates by up to 6-fold. Influenza immunizations provide a special challenge based on the perceived short immunization period. Although this program was conducted over 1 year, most providers view the influenza immunization season as running from only October to December.33, 34 and 35 Short immunization seasons leave little time for traditional quality improvement cycles. By the time initial measurements are available, most immunization opportunities are gone.28 Responding to this issue, the Centers for Disease Control and Prevention (CDC) recommends that influenza immunizations be given as soon as they become available and be continued throughout the entire influenza season, even after influenza is documented in the community.16
Fourth, we did not manage the actual programs within each facility. We do not have information on how well the immunization teams collaborated, how interventions were designed or executed, or compliance with the chosen interventions.
Last, participating facilities did not use standing order programs. Standing orders allow administration of influenza and pneumococcal vaccines to residents and HCW without individual physician orders.36 Information was provided to the facilities on standing order programs, but the Centers for Medicare and Medicaid services had just authorized their use at the time of this project. Participants shared concerns over the Commonwealth's acceptance of such programs and were resistant to them. Pennsylvania has since clarified acceptance of standing order programs in LTC facilities.
Long-term care facilities are complex organizations; market factors attempting to drive change may be offset by competing priorities.37 Facilities are frequently more focused on issues relating to licensure and certification than on health prevention issues such as immunization programs.38 and 39 To improve immunization rates in LTC, we will need to realign incentives. Compliance through legislative mandates is not likely31; novel approaches are needed. Addressing staff turnover is one example. High LTC staff turnover is commonplace, reduces institutional memory, and impacts overall facility quality.31 and 40 Unique strategies are required to address this barrier.
In summary, our pilot work suggests it is possible to improve influenza and pneumococcal immunization rates across a group of facilities by combining the use of published guidelines, immunization improvement teams, e-mail communication, and a brief collaborative training session. Staff turnover, competing organizational demands, and uncertain team collaboration represent plausible barriers to improving immunization rates and should be explored formally in future work.
Table 1.
Facility Characteristics
| Facility | A | B | C | D | E | F |
|---|---|---|---|---|---|---|
| Group | C | NC | C | NC | C | NC |
| Bed size | 139 | 159 | 59 | 145 | 202 | 180 |
| Location | Suburban | Urban | Urban | Urban | Suburban | Suburban |
| Unionization status | Nonunion | Union | Union | Nonunion | Nonunion | Nonunion |
| Number of staff in 2002 | 325 | 325 | 35 | 153 | 250 | 180 |
| Number of staff in 2003 | 287 | 280 | 47 | 145 | 301 | 222 |
C, collaborative participant; NC, noncollaborative participant.
Appendix 1. Examining Your Immunization Program
The following table lists some tasks important to successful vaccination programs. Think about how your facility handles each of these functions. The “Think About” column gives some ideas about what each task area addresses. Please think carefully about each task and rate how successful you think your facility is in tackling these functions using the following grading system:
= Our Performance & Comfort in This Area Need a Lot of Improvement
= Our Performance & Comfort in This Area Need Some Improvement
= Our Performance & Comfort in This Area Are Average
= Our Performance & Comfort in This Area Are Generally Good
= Our Performance & Comfort in This Area Are Very High
| TASK | THINK ABOUT…… | YOUR SCORE |
|---|---|---|
| IDENTIFYING THE IMPORTANCE OF VACCINATION |
|
|
| COMMUNICATING THE SAFETY OF THE VACCINE |
|
|
| IDENTIFYING RESIDENTS WHO SHOULD RECEIVE THE VACCINE |
|
|
| ORDERING THE VACCINE |
|
|
| CONSENT |
|
|
| DOCUMENTATION & OUTCOME MEASUREMENT |
|
|
| FEEDBACK |
|
|
| POLICY |
|
Facility
__________________________________________________________
______
Promoting LTC Vaccination Project
VACCINATION GOALS FACILITY ______________________________
By _________________, we will improve our current influenza & pneumococcal vaccination program so that we meet or exceed the following vaccination goals:
Influenza Vaccination–Residents 90%
Influenza Vaccination–Staff 60%
Pneumococcal Vaccine–Residents 90%
INDIVIDUAL FACILITY PROCESS GOALS
In order to reach the goals above, we will need to improve the following processes:
| Process? | How will we measure? | By When? |
|---|---|---|
References
- 1.Kung HC, Hoyert DL, Xu J, et al. Deaths: Final data for 2005. Natl Vital Stat Rep. 2008;56:1–120. [PubMed] [Google Scholar]
- 2.Kavesh W, Drinka P, Hill T, et al. LTC Physician Information Took Kit Series: Immunization in the Long-Term Care Setting. American Medical Directors Association; Columbia, MD: 2006. [Google Scholar]
- 3.Nourti J, Butler J, Crutcher J, et al. An outbreak of multidrug-resistant pneumococcal pneumonia and bacteremia among unvaccinated nursing home residents. N Engl J Med. 1998;338:1861–1868. doi: 10.1056/NEJM199806253382601. [DOI] [PubMed] [Google Scholar]
- 4.Yoshikawa T, Ouslander J. Infection Management for Geriatrics in Long-Term Care Facilities. 2. Informa Healthcare USA, Inc; New York: 2007. [Google Scholar]
- 5.Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292:1333–1340. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- 6.Fry AM, Shay DK, Holman RC, et al. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA. 2005;294:2712–2719. doi: 10.1001/jama.294.21.2712. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Pneumococcal polysaccharide vaccine. MMWR Morbid Mortal Wkly Rep. 1989;38:64–68. [PubMed] [Google Scholar]
- 8.Loeb M, Stevenson KB SHEA Long-Term Care Committee. Pneumococcal immunization in older adults: implications for the long-term-care setting. Infect ControlHosp Epidemiol. 2004;25:985–994. doi: 10.1086/502331. [DOI] [PubMed] [Google Scholar]
- 9.Department of Health and Human Services, editor. Healthy People 2010: Understanding and Improving Health. 2. US Government Printing Office; Washington, DC: 2000. [Google Scholar]
- 10.Centers for Disease Control and Prevention. [Accessed June 19, 2009];Data. 2010 Available at http://wonder.cdc.gov/data2010.
- 11.Potter J, Stott DJ, Roberts MA, et al. Influenza vaccination of health care workers in long-term-care hospitals reduces the mortality of elderly patients. J Infect Dis. 1997;175:1–6. doi: 10.1093/infdis/175.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carman WF, Elder AG, Wallace LA, et al. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: A randomised controlled trial. Lancet. 2000;355:93–97. doi: 10.1016/S0140-6736(99)05190-9. [DOI] [PubMed] [Google Scholar]
- 13.Hayward AC, Harling R, Wetten S, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: Cluster randomised controlled trial. BMJ. 2006;333:1241. doi: 10.1136/bmj.39010.581354.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Talbot T, Bradley S, Cosgrove S, et al. Influenza vaccination of healthcare workers and vaccine allocation for healthcare workers during vaccine shortages. Infect Control Hosp Epidemiol. 2005;26:882–890. doi: 10.1086/502512. [DOI] [PubMed] [Google Scholar]
- 15.Walker F, Singleton J, Lu P, et al. Influenza vaccination of healthcare workers in the United States, 1989–2002. Infect Control Hosp Epidemiol. 2006;27:257–265. doi: 10.1086/501538. [DOI] [PubMed] [Google Scholar]
- 16.Fiore AE, Shay DK, Broder K, et al. Prevention and control of influenza: Recommendations of the Advisory Committee on Immunization Practices (ACIP), 2008. MMWR Recomm Rep. 2008;57:1–60. [PubMed] [Google Scholar]
- 17.Nace D, Hoffman E, Resnick N, et al. Achieving and sustaining high rates of influenza immunization among long-term care staff. J Am Med Dir Assoc. 2007;8:128–133. doi: 10.1016/j.jamda.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 18.American Medical Directors Association. Immunization in long term care: Focusing on influenza and pneumococcal vaccinations. American Medical Directors Association; Columbia, MD: 1998. [Google Scholar]
- 19.Institute for Healthcare Improvement. [Accessed June 19, 2009]; Available at www.ihi.org.
- 20.Slater R. The GE Way Fieldbook: Jack Welch's Battle Plan for Corporate Revolution. McGraw-Hill; New York: 2000. [Google Scholar]
- 21.Pope C, van Royen P, Baker R. Qualitative methods in research on healthcare quality. Qual Saf Health Care. 2002;11:148–152. doi: 10.1136/qhc.11.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bannerman B, Schram K. Influenza immunization program in long term care facilities. Can J Infect Control. 1992;7:13–15. [PubMed] [Google Scholar]
- 23.Thomas D, Winsted B, Koontz C. Improving neglected influenza vaccination among healthcare workers in long-term care. J Am Geriatr Soc. 1993;41:928–930. doi: 10.1111/j.1532-5415.1993.tb06757.x. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Interventions to increase influenza vaccination of health-care workers—California and Minnesota. MMWR Morb Mortal Wkly Rep. 2005;54:196–199. [PubMed] [Google Scholar]
- 25.Edwards N. Can quality improvement be used to change the wider healthcare system? Qual Saf Health Care. 2005;14:75. doi: 10.1136/qshc.2005.013748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dunn MK, Misra S, Habermann R, et al. Pneumococcal vaccination in nursing homes: Does policy change practice? J Am Med Dir Assoc. 2003;4:135–138. doi: 10.1097/01.JAM.0000064462.55083.DC. [DOI] [PubMed] [Google Scholar]
- 27.Grabowski DC, Castle NG. Nursing homes with persistent high and low quality. Med Care Res Rev. 2004;61:89–115. doi: 10.1177/1077558703260122. [DOI] [PubMed] [Google Scholar]
- 28.Sand K, Lynn J, Bardenheier B, et al. Increasing influenza immunization for long-term care facility staff using quality improvement. J Am Geriatr Soc. 2007;55:1741–1747. doi: 10.1111/j.1532-5415.2007.01422.x. [DOI] [PubMed] [Google Scholar]
- 29.Lawhorne LW, Ouslander JG, Parmelee PA, et al. Clinical practice guidelines, process improvement teams, and performance on a quality indicator for urinary incontinence: a pilot study. J Am Med Dir Assoc. 2008;9:504–508. doi: 10.1016/j.jamda.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 30.Rantz MJ, Hicks L, Grando V, et al. Nursing home quality, cost, staffing, and staff mix. Gerontologist. 2004;44:24–38. doi: 10.1093/geront/44.1.24. [DOI] [PubMed] [Google Scholar]
- 31.Castle NG, Engberg JA. Men Nursing home staff turnover: Impact on nursing home compare quality measures. Gerontologist. 2007;47:650–661. doi: 10.1093/geront/47.5.650. [DOI] [PubMed] [Google Scholar]
- 32.Mittman BS. Creating the evidence base for quality improvement collaboratives. Ann Intern Med. 2004;140:897–901. doi: 10.7326/0003-4819-140-11-200406010-00011. [DOI] [PubMed] [Google Scholar]
- 33.Stinchfield PK. Practice-proven interventions to increase vaccination rates and broaden the immunization season. Am J Med. 2008;121:S11–S21. doi: 10.1016/j.amjmed.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 34.Poland GA, Johnson DR. Increasing influenza vaccination rates: The need to vaccinate throughout the entire influenza season. Am J Med. 2008;121:S3–10. doi: 10.1016/j.amjmed.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 35.Davis MM, McMahon SR, Santoli JM, et al. A national survey of physician practices regarding influenza vaccine. J Gen Intern Med. 2002;17:670–676. doi: 10.1046/j.1525-1497.2002.11040.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bardenheier B, Shefer A, McKibben L, et al. Factors predictive of increased influenza and pneumococcal vaccination coverage in long-term care facilities: The CMS-CDC Standing Orders Program Project. J Am Med Dir Assoc. 2005;6:291–299. doi: 10.1016/j.jamda.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 37.Ham C. Improving the performance of health services: The role of clinical leadership. Lancet. 2003;361:1978–1980. doi: 10.1016/S0140-6736(03)13593-3. [DOI] [PubMed] [Google Scholar]
- 38.Rosen J, Mittal V, Degenholtz H, et al. Organizational change and quality improvement in nursing homes: Approaching success. J Healthc Qual. 2005;27:6–14 21,44. doi: 10.1111/j.1945-1474.2005.tb00583.x. [DOI] [PubMed] [Google Scholar]
- 39.Katz-Navon T, Naveh E, Stern Z. The moderate success of quality of care improvement efforts: Three observations on the situation. Int J Qual Health Care. 2007;19(1):4–7. doi: 10.1093/intqhc/mzl058. [DOI] [PubMed] [Google Scholar]
- 40.Decker F, Gruhn P, Matthews-Martin L, et al. Health Services Research and Evaluation. American Health Care Association; Washington, DC: 2003. Results of the 2002 AHCA Survey of Nursing Staff Vacancy and Turnover in Nursing Homes. [Google Scholar]


