Abstract
Background
The developmental pathways associated with an enhanced risk for future alcohol use disorders (AUDs) continue to be a topic of both interest and debate. In this research, internalizing and externalizing disorders were evaluated as prospective predictors of the index AUD episode onset, separately within three developmental periods: early-to-middle adolescence (age 13.0 to 17.9), late adolescence (18.0 to 20.9), and early adulthood (21.0 to 30.0).
Methods
Participants (N = 816) were initially randomly selected from nine high schools in western Oregon and subsequently interviewed on four separate occasions between ages 16 and 30, during which current and past AUDs were assessed as well as a full range of psychiatric disorders associated with internalizing and externalizing psychopathology domains.
Results
In adjusted analyses for each of the three developmental periods investigated, externalizing domain psychopathology from the most proximal adjoining developmental period predicted time to AUD onset. Distal externalizing psychopathology also predicted time to AUD onset among early adult onset cases. Proximal or distal internalizing psychopathology, in comparison, was not found to be a significant predictor of AUD onset in adjusted analyses for any of the developmental periods examined.
Conclusions
Findings overall suggest that externalizing developmental histories are robust predictors of AUD onset within the age range during which index episodes are most likely to occur, and that gender does not moderate this association.
Keywords: Alcohol use disorders (AUDs), predictors, psychopathology, externalizing, internalizing, gender
1. INTRODUCTION
Contemporary epidemiological perspectives suggest that developmental pathways for alcohol use disorders (AUDs) are established well before problematic alcohol use begins (Clark, 2004), and likely causally related to processes that increase vulnerabilities to externalizing and internalizing psychiatric disorders (Hussong et al., 2011; Sher et al., 2005; Vanyukov et al., 2012). The internalizing-externalizing organizational model of psychopathology (Achenbach, 1966; Krueger, 1999) is a statistically-derived framework that accounts well for the covariation among psychiatric symptoms and disorders among children and adults in cross-sectional and longitudinal studies (e.g., Achenbach, 1966; Caspi et al., 2014; Farmer et al., 2013b; Kessler et al., 2011; Krueger and Markon, 2006), and has been suggested as a guiding framework for research on common causal pathways that account for lifetime disorder comorbidity (Kessler et al., 2011; Krueger, 1999), including AUDs (Hussong et al., 2011).
Externalizing disorders and their precursors are associated with oppositional, aggressive, impulsive, disruptive, and rule-breaking behavior. Prospective studies have documented that externalizing tendencies or disorders robustly predict the future onset of alcohol use problems or AUDs (Chassin et al., 2004; Elkins et al., 2006; Englund et al., 2008; Feingold et al., 2015; Fergusson et al., 2007; Grekin et al., 2006). Internalizing disorders and their precursors, in contrast, are associated with depression, anxiety, fear, rumination, and distress. Compared to externalizing developmental pathways, the role of internalizing pathways in the development of AUDs has been little researched (Hussong et al., 2011). Although internalizing symptoms or disorders are often concomitants with alcohol use problems or disorders in cross-sectional research (e.g., Burns and Teesson, 2002; Hasin et al., 2007; Kessler et al., 2005), prospective studies on the risk posed by internalizing tendencies or disorders on future alcohol use problems or AUDs have produced mixed findings (Boschloo et al., 2013; Buckner et al., 2008; Buckner and Turner, 2009; Crum and Pratt, 2001; Elkins et al., 2006; Gilman and Abraham, 2001; Grekin et al., 2006; Kushner et al., 1999; Trautmann et al., 2015; Zimmermann et al., 2003).
There are three primary aims associated with this study. First, this research evaluated whether risk for index AUD episodes within each of the developmental periods examined was associated with prior externalizing or internalizing disorders. Three developmental periods corresponding to AUD onset were defined: early-to-middle adolescence (age 13.0 to 17.9), late adolescence (18.0 to 20.9), and early adulthood (21.0 to 30.0). Outcomes from the analyses associated with this aim are expected to elucidate the relative contributions of externalizing and internalizing disorders in the prediction of AUD risk as well as the developmental specificity versus generality of these predictors. Second, for the two latter developmental periods studied, we evaluated whether distal externalizing and internalizing disorders from earlier developmental periods also predicted risk for AUDs. Findings from these analyses are expected to highlight whether risk factors that occurred later versus earlier in development are most relevant in the prediction of subsequent AUD risk. Third, important differences in the development and course of AUDs among men and women have been reported (Ammon et al., 2008; Kessler et al., 1994; Nolen-Hoeksema, 2004). Consequently, in the present research, we explored whether gender moderates observed effects.
This study builds on existing studies in the following ways. First, this research was conducted with a large representative community sample. Many earlier studies that have sought to identify externalizing or internalizing predictors of AUDs utilized high-risk, treatment, or convenience samples (e.g., university students). Second, it is often unclear from existing prospective studies if risk-based evaluations of internalizing and externalizing disorders are referenced to the first or subsequent episode of problematic drinking or an AUD. This is an especially important consideration when evaluating risk factors for versus consequences of AUDs, as AUDs are known to increase risk for future internalizing disorders (Fergusson et al., 2011) as well as externalizing disorders, especially other substance use disorders (Kandel et al., 1992). Third, rather than limiting prediction models to single diagnostic categories, externalizing and internalizing disorder domains in the present research are represented by several individual disorders, thus resulting in broader coverage of content domains associated with risk-related pathways. Fourth, studies that have examined internalizing tendencies or disorders as risk factors for future AUDs often do not statistically control for externalizing features or disorders, and vice versa (Hussong et al., 2011). In the present research, we evaluated adjusted prediction models that controlled for demographic and psychosocial variables as well as the disorder domain that was not the primary predictor variable modeled in the analysis.
2. MATERIALS AND METHODS
2.1. Participants
2.1.1. Participant sampling, composition, and retention
At the first wave of data collection (T1; ~ age 16), the sample consisted of 1,709 adolescents randomly selected from 9 high schools that were representative of urban and rural districts in western Oregon. About one year later (T2), 1,507 (88%) of these persons were reassessed. At T3 (~ age 24), a sampling stratification procedure was introduced whereby eligible participants included all non-white participants to enhance ethnic diversity and all persons with a positive history of a psychiatric diagnosis by T2 (n = 644) and a randomly selected subset of participants with no history of a psychiatric or substance use disorder by T2 (n = 457 of 863 persons). Of these 1,101 eligible persons, 941 (85%) completed T3. The T4 assessment period was conducted approximately 6 years after T3 (~ age 30). From the 941 eligible persons who completed T3, 816 (87%) completed the T4 assessment. Earlier analyses of participant attrition (Farmer et al., 2013a; Lewinsohn et al., 1993; Rohde et al., 2007) revealed minimal sample bias related to study discontinuation.
By age 30.0, 34.3% of the weighted T4 panel had a DSM-III-R or DSM-IV lifetime AUD diagnosis (43.0% male, 95% confidence interval [CI95] = 37.4 - 48.5; 27.6% female, CI95 = 23.4 - 31.8; p < .05). For those with a lifetime AUD episode by age 30.0, the mean age at time of first AUD onset was 20.2 years of age (SD = 3.9).
2.1.2. Weighting procedures based on stratification implemented at T3
As a result of the unequal stratified sampling strategy implemented at T3, Caucasian participants without a psychiatric diagnosis by T2 were under-sampled at T3 and T4. To adjust for this sampling procedure, Caucasian participants with no lifetime diagnosis by T2 were assigned a weight that reflected the probability of this subgroup being sampled during T3 and T4 assessments (see Farmer et al., 2013a for details). All findings subsequently presented (e.g., rates, ratios) were based on weighted data, with references to the numbers of cases based on unweighted data.
2.1.3. Reference sample for this research
The reference sample for this study varied according to the research question. Demographic predictors of AUD onset were evaluated using data from the complete T4 panel (n = 816). Psychiatric predictors of early-to-middle adolescent AUD onset (between ages 13.0 and 17.9) were evaluated using data from participants without an incidence of AUD between ages 0 and 12.9 (n = 810), with AUD episodes occurring at or after age 18.0 right-censored.1, 2 Psychiatric predictors of late adolescent AUD onset (between ages 18.0 and 20.9) were evaluated with data from participants without an incidence of AUD before age 18.0 (n = 730), with AUD episodes occurring at or after 21.0 right-censored. Finally, psychiatric predictors of early adult AUD onset (between ages 21.0 and 30.0) were evaluated with data from participants without an incidence of AUD before age 21.0 (n = 641).
2.2. Diagnostic Assessments
2.2.1 Definitions of internalizing and externalizing disorder domains and subdomains
When evaluating predictors of AUD onset, internalizing and externalizing disorder domain scores were categorically modeled, whereby a value of 0 was assigned if no disorder associated with a given domain was diagnosed within the timeframe specified and a value of 1 assigned if one or more domain-related disorders was diagnosed at any time within the indicated timeframe. Based on our earlier research with the OADP sample (Farmer et al., 2009, 2013b; Seeley et al., 2011), DSM-defined disorders that contributed to the internalizing domain, further distinguished by DSM-defined subdomains, were: mood disorders (major depressive; dysthymia; bipolar spectrum disorders), anxiety disorders (separation anxiety, simple/specific phobia, generalized anxiety, obsessive–compulsive, panic, agoraphobia without panic, post-traumatic stress, social phobia), and bulimia nervosa (as the sole exemplar of eating disorders). Disorders that contributed to the definition of the externalizing domain, further distinguished by DSM-defined subdomains, were: disruptive behavior disorders (attention deficit/hyperactivity, oppositional defiant, conduct) and non-alcohol-related substance use disorders (i.e., other SUDs), which incorporated cannabis use disorders and hard drug use disorders, with the latter category including the abuse or dependence of substances other than cannabis and alcohol.
2.2.2 Diagnostic assessments
One objective of each assessment wave was to determine current and past episodes of DSM-defined psychiatric disorders and SUDs for each participant. At the time of study entry (T1), participants were individually evaluated for current (last 12 months) as well as past (lifetime) AUDs and individual internalizing and externalizing disorders. During subsequent assessments (T2 - T4), participants were evaluated for current AUDs and other individual disorders as well as any other episodes that may have emerged or persisted since the last interview.
During T1, T2, and T3, participants were interviewed with the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS), an interviewer administered semi-structured diagnostic interview that assesses symptom features of DSM-defined disorder categories and produces information that allows for diagnostic decisions consistent with criteria specified in the DSM. The version of the K-SADS used in the present research combined features of the Epidemiologic and Present Episode versions (Chambers et al., 1985; Orvaschel et al., 1982). Follow-up diagnostic assessments at T2 and T3 also involved the joint administration of the Longitudinal Interval Follow-Up Evaluation (LIFE; Keller et al., 1987) that, in conjunction with the K-SADS, provided detailed information related to the presence and course of disorders since participation in the previous diagnostic interview. The T4 assessment included administration of the LIFE and the administration of the Structured Clinical Interview for Axis I DSM-IV Disorders–Non-Patient Edition (SCID-NP; First et al., 1994). Like the K-SADS, the SCID-NP is an interviewer administered semi-structured interview for assessing psychiatric symptoms and evaluating diagnostic criteria consistent with DSM specifications.
Diagnostic interviewers and reliability assessors were carefully trained and supervised, with most having advanced degrees in mental health-related disciplines (see Rohde et al., 2007, for details on assessor training and supervision). All interviews were either audio- or videotaped, and interviews from each assessment wave were randomly selected for reliability assessments by a second interviewer. Diagnostic agreement was good to excellent across assessment waves (median kappa = .77 for 9 separate diagnostic categories excluding AUD; see Farmer et al., 2009 and Seeley et al., 2011).
2.2.3 Assessment and specification of AUDs
In DSM-III-R and DSM-IV, SUDs are arranged hierarchically into abuse and dependence categories, whereby dependence takes precedence over abuse when criteria for both conditions are satisfied. This modeling of SUDs has been challenged by data that fail to support the alcohol abuse/dependence distinction as operationalized in DSM-III, DSM-III-R and DSM-IV (Hasin et al., 2013; Slade et al., 2009), with the abuse/dependence distinction eliminated from DSM-5 as a result. Consequently, for the analyses described below, we combined DSM-III-R and DSM-IV alcohol abuse and dependence diagnoses into a single category (AUDs) to indicate syndromal alcohol use that has resulted in significant functional impairment. Diagnostic agreement among raters for AUD diagnoses since the previous interview was adequate to excellent at each wave (kappas: T1 = .76, T2 = .89, T3 = .69, T4 = .79). In the present research, the onset of the index AUD episode is referenced to the age (in months) at which the disorder was diagnosed. The intraclass correlation (ICC) that indexed rater agreement for age of disorder onsets in instances where both raters agreed on the occurrence of an index AUD episode was high (ICC = .92).
2.3. Childhood and Adolescent Predictors of Time to AUD Onset
In a set of prospective analyses described below, we evaluated the degree to which internalizing and externalizing disorders were predictors of AUD onset. AUD onset was differentiated according to early-to-middle adolescent onset (ages 13.0 to 17.9), late adolescent onset (ages 18.0 to 20.9), and early adult onset (ages 21.0 to 30.0). Age 21 was used as a boundary age for the last two developmental periods because this age demarcates illicit from licit use of alcohol. In models predicting early-to-middle adolescent AUD onset, we evaluated disorders occurring during childhood (ages 8.0 to 12.9) as predictors. In models predicting late adolescent AUD onset, we separately evaluated disorders occurring during early-to-middle adolescence (proximal) and childhood (distal) as predictors. For models predicting early adult AUD onset, we separately evaluated disorders occurring during late adolescence (proximal), early-to-middle adolescence (distal) and childhood (distal) as predictors.
2.4. Potential Confounders
We evaluated several demographic variables as predictors of AUD onset functions, and included these putative confounders as covariates in adjusted analyses to better isolate unique associations between internalizing and externalizing disorders and AUD onset. Putative confounders included participant characteristics (i.e., gender; race/ethnicity; puberty onset [early, on time, late] based on procedures described in Graber et al., 1997; self-reports of repeating a grade before age 12) and family characteristics assessed at T1 (dual versus single parent household; at least one parent completed college; mean age of heads of household at T1; number of older siblings).3 In adjusted analyses, we also controlled for the disorder domain that was not the main focus of the analysis (e.g., when isolating the predictive effects associated with internalizing disorders, externalizing disorders were controlled).
2.5. Statistical Analyses
Separate non-parametric tests of rate differences in internalizing and externalizing disorder occurrences within the preceding developmental period(s) are presented as a function of the presence versus absence of an initial AUD diagnosis in the reference developmental period. To fully exploit longitudinal information available from our data set, we also examined the prediction of AUD onset with Cox PH modeling procedures. Hazard ratios (HR) and corresponding 95% confidence intervals (CIs) produced from these analyses are based on the ratio of AUD onset probabilities, specifically differences in hazard rates as a linear function of the predictor variables. HR values therefore reflect any differences in hazard functions, and specify the increased likelihood of developing an AUD within a unit of time (months) as a function of the presence versus absence of prior internalizing or externalizing disorders. In the prediction models tested, HR values greater than 1.0 and whose 95% CIs do not include a value of 1.0 indicate that participants with a disorder history represented by the predictor have significantly greater odds of being diagnosed with an AUD during any month-length interval within the developmental period examined when compared to those without disorder histories represented by the predictor. An HR value of 2.0 associated with a given disorder predictor, for example, indicates a two times greater odds of being diagnosed with an AUD during any month-length interval within the developmental period examined when compared to those without an earlier history of a disorder from that domain. In our set of separate analyses of predictors of AUD risk during discrete developmental periods, persons who were diagnosed with AUDs in earlier developmental periods were removed from analyses involving subsequent developmental periods because the event being predicted (i.e., the emergence of the index AUD episode) had already occurred.
3. RESULTS
3.1. Demographic Predictors of Time to AUD Onset
By age 30.0, 34.3% of the weighted T4 panel had a lifetime AUD diagnosis. Demographic variables were individually evaluated as predictors of AUD onset with Cox PH regression methods. Findings from these analyses, which were conducted with the entire sample, are presented in Table 1. Male gender, ethnic/racial minority status, and late versus on-time puberty by T1 were each significantly associated with AUD onset. All demographic variables, regardless of their individual significance, were included among the covariates used in adjusted analyses reported below.
Table 1.
Descriptive Statistics for Demographic Variables and Bivariate Associations with Time to AUD Onset through Age 30 (n = 816)
| Predictor | Descriptive Statistics:
% [CI95] and M
(SD) |
Associations with Time to AUD Onset HR [CI95] |
|||
|---|---|---|---|---|---|
| No AUD (n = 513) | AUD (n = 303) | Test Statistica | p-value | ||
| Participant Characteristics | |||||
| Male, % [CI95] | 38.1 [33.7, 42.7] | 54.9 [48.9, 60.7] | 20.93 | <.001 | 1.68 [1.32, 2.15] |
| Non-white, % [CI95] | 6.6 [5.0, 8.6] | 10.0 [7.3, 13.5] | 3.88 | .049 | 1.44 [1.02, 2.02] |
| Pubertal timing, % [CI95] | |||||
| Early (n = 153) vs. on-time (n = 567) | 18.9 [15.4, 22.9] | 22.5 [17.6, 28.2] | 1.22 | .270 | 1.24 [0.90, 1.71] |
| Late (n = 96) vs. on-time (n = 567) | 12.3 [9.3, 16.0] | 18.6 [13.9, 244] | 4.16 | .042 | 1.46 [1.03, 2.08] |
| Early (n = 153) vs. late (n = 96) | 62.5 [53.6, 70.5] | 56.0 [45.7, 65.8] | 0.91 | .339 | 0.86 [0.56, 1.29] |
| History of repeating grade before age 12 | 11.1 [8.6, 14.3] | 10.3 [7.3, 14.4] | 0.12 | .725 | 0.91 [0.63, 1.33] |
| Family Demographic Variables | |||||
| Dual versus single parent household, % [CI95] | 58.7 [54.2, 63.1] | 55.1 [49.1, 60.9] | 0.92 | .336 | 0.86 [0.68, 1.10] |
| At least one parent completed college, % [CI95] | 44.1 [39.6, 48.7] | 44.3 [38.4, 50.3] | 0.01 | .968 | 1.01 [0.79, 1.29] |
| Mean parent age at T1, M (SD) | 42.4 (6.0) | 42.1 (5.9) | 0.71 | .476 | 0.99 [0.97, 1.01] |
| Number of older siblings, M (SD) | 0.9 (1.1) | 0.9 (1.1) | 0.70 | .484 | 0.97 [0.87, 1.08] |
Note. HR = hazard ratio; CI95 = 95% confidence interval. Bolded table entries denote statistically significant effects.
Likelihood ratio chi-square and independent observation t-tests were conducted on categorical and continuous variables, respectively.
3.2. Childhood Predictors of AUD Onset During Early-to-Middle Adolescence
For those with initial AUD episode onsets during early-to-middle adolescence (n = 80), the mean onset age of the first episode was 15.9 years (SD = 1.3; Mdn = 16.0). Table 2 presents the period prevalence rates of internalizing and externalizing disorders separately within the childhood developmental period among participants without and with an initial AUD onset during early-to-middle adolescence. Rates of externalizing domain disorders in childhood were significantly higher among those with than without an AUD onset during this developmental period. Significant externalizing subdomains included childhood disruptive behavior disorders and other SUDs. Non-significant trend effects (p ≤ .06) were noted for any internalizing domain disorder or any mood disorder, with the direction of the association indicating marginally higher rates of these disorders in the AUD onset group.
Table 2.
Period Prevalence Rates of Internalizing and Externalizing Psychopathology and Associations with Initial AUD Onset during Early-To-Middle Adolescence
| Predictor | Period
Prevalence % [CI95] |
Adjusted Associations with Time to AUD Onset during Early-To-Middle Adolescence HR [CI95] |
|||
|---|---|---|---|---|---|
| No AUD (n = 730) | AUD (n =80) | Likelihood Ratio χ2 |
p-value | ||
| Childhood Psychopathology | |||||
| Internalizing domain | 10.6 [8.8, 12.9] | 17.9 [11.1, 27.5] | 3.60 | .058 | 1.46 [0.79, 2.71] |
| Mood disorders | 5.7 [4.4, 7.3] | 11.2 [6.1, 19.7] | 3.54 | .060 | 1.43 [0.66, 3.09] |
| Anxiety disorders | 6.7 [5.3, 8.5] | 10.1 [5.3, 18.4] | 1.23 | .267 | 1.38 [0.67, 2.87] |
| Bulimia nervosa | 0.0 | 0.0 | NA | NA | NA |
| Externalizing domain | 3.4 [2.4, 4.6] | 13.5 [7.4, 23.2] | 12.47 | <.001 | 3.65 [1.84, 7.25] |
| Disruptive behavior disorders | 2.8 [1.9, 4.0] | 8.9 [4.5, 17.0] | 6.94 | .009 | 2.99 [1.35, 6.64] |
| Other substance use disorders | 0.7 [0.3, 1.4] | 4.5 [1.4, 14.0] | 5.48 | .019 | 3.68 [1.00, 13.56] |
Note. Bolded table entries denote statistically significant effects.
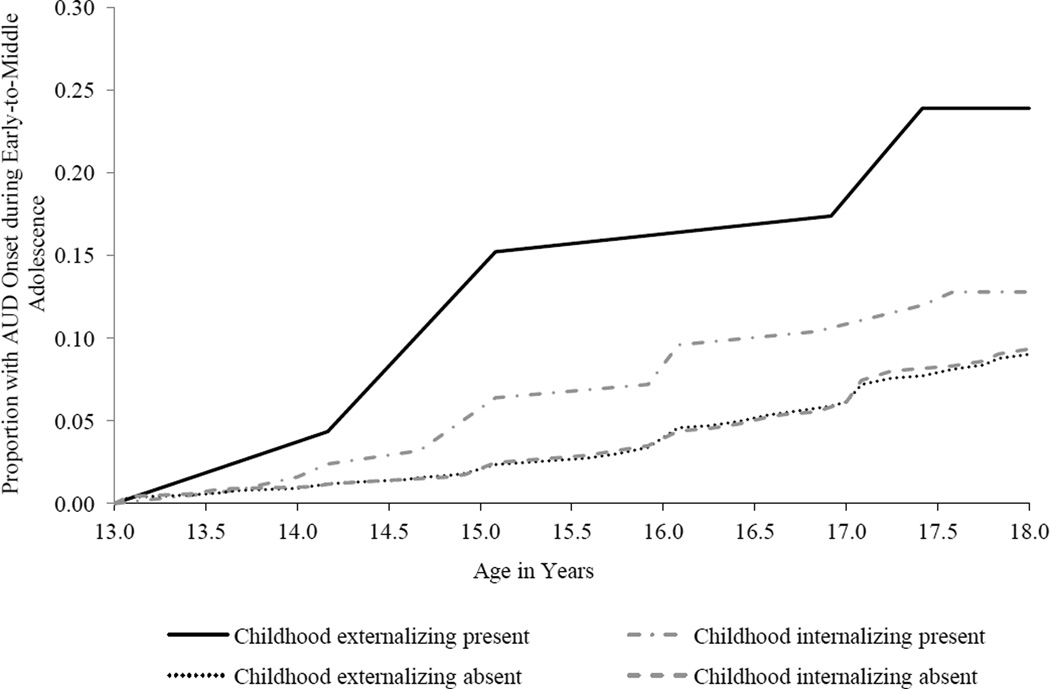
The far right column of Table 2 presents adjusted analyses that evaluated internalizing and externalizing disorder domains and subdomains as predictors of initial AUD onset during early-to-middle adolescence. These data correspond to the additive effects of individual psychiatric disorder domains after variance associated with putative confounders and the corresponding non-targeted psychiatric disorder domain were both controlled. Before evaluating the unique effects associated with internalizing and externalizing disorders, an internalizing by externalizing interaction term was included in the model to test the homogeneity of regression assumption. The interaction term was non-significant, indicating that the homogeneity assumption had been met, and was subsequently eliminated from the statistical models.4 Significant effects were noted for any externalizing domain disorder and the disruptive behavior disorder subdomain. The effect for other SUDs, however, was trend-level (p = .05). Cumulative hazard functions for AUD onset during early-to-middle adolescence by disorder domain during childhood are presented in Figure 1.
Figure 1.
Cumulative hazard functions for alcohol use disorder (AUD) onset during early-to-middle adolescence (ages 13.0 to 17.9) by disorder domain during childhood (ages 8.0 to 12.9).
3.3. Early-to-Middle Adolescent and Childhood Psychiatric Predictors of AUD Onset During Late Adolescence
For those with an initial AUD episode onset during late adolescence (n = 89), the mean age of AUD onset was 19.2 years (SD = 0.9; Mdn = 19.0). Table 3 presents rates of internalizing and externalizing disorder occurrences for the late adolescent onset group, separately for early-to-middle adolescence and childhood. When compared to those who did not experience an initial AUD onset within this developmental period, those with index AUD episode onsets during late adolescence demonstrated significantly higher rates of early-to-middle adolescent externalizing domain disorders and, at the subdomain level, other SUDs. No significant difference between groups, however, was observed for disruptive behavior disorders or for any internalizing domain or subdomain disorders. Rates of childhood internalizing or externalizing disorders, at both the domain and subdomain levels, also did not significantly differ between those without and with initial AUD onsets during late adolescence with the exception of mood disorder rates, which were significantly lower during childhood in AUD onset group.
Table 3.
Period Prevalence Rates of Internalizing and Externalizing Psychopathology and Associations with Initial AUD Onset during Late Adolescence
| Predictor | Period
Prevalence % [CI95] |
Adjusted Associations with Time to AUD Onset during Late Adolescence HR [CI95] |
|||
|---|---|---|---|---|---|
| No AUD (n = 641) | AUD (n = 89) | Likelihood Ratio χ2 |
p-value | ||
|
Early-To-Middle
Adolescent Psychopathology |
|||||
| Internalizing domain | 24.5 [21.6, 27.8] | 27.9 [19.7, 37.8] | 0.45 | .490 | 1.32 [0.82, 2.12] |
| Mood disorders | 21.1 [18.4, 24.1] | 18.5 [12.2, 27.0] | 0.34 | .528 | 0.93 [0.54, 1.62] |
| Anxiety disorders | 6.25 [4.8, 8.2] | 8.58 [4.2, 16.9] | 0.65 | .433 | 1.53 [0.72, 3.22] |
| Bulimia nervosa | 1.1 [0.6, 2.2] | 0.8 [0.1, 5.3] | 0.09 | .723 | 0.81 [0.11, 6.23] |
| Externalizing domain | 8.5 [6.7, 10.6] | 17.9 [11.1, 27.7] | 6.95 | .010 | 2.05 [1.15, 3.67] |
| Disruptive behavior disorders | 4.1 [2.9, 5.6] | 4.7 [1.8, 11.3] | 0.07 | .784 | 0.91 [0.32, 2.59] |
| Other substance use disorders | 5.1 [3.7, 6.8] | 13.3 [7.4, 22.6] | 7.53 | .008 | 2.36 [1.19, 4.60] |
| Childhood Psychopathology | |||||
| Internalizing domain | 11.1 [9.1, 13.3] | 7.8 [3.7, 15.5] | 0.97 | .322 | 0.85 [0.40, 1.80] |
| Mood disorders | 6.2 [4.8, 8.1] | 1.5 [0.4, 6.0] | 4.40 | .013 | 0.26 [0.06, 1.08] |
| Anxiety disorders | 6.7 [5.2, 8.5] | 7.0 [3.2, 14.6] | 0.01 | .907 | 1.58 [0.70, 3.55] |
| Bulimia nervosa | 0.0 | 0.0 | NA | NA | NA |
| Externalizing domain | 3.5 [2.5, 4.9] | 2.3 [0.7, 7.0] | 0.38 | .462 | 1.15 [0.35, 3.87] |
| Disruptive behavior disorders | 3.0 [2.0, 4.3] | 1.5 [0.4, 6.0] | 0.69 | .325 | 0.56 [0.13, 2.46] |
| Other substance use disorders | 0.7 [0.3, 1.5] | 0.8 [0.1, 5.3] | 0.02 | .885 | 1.45 [0.21, 9.91] |
Note. Bolded table entries denote statistically significant effects.
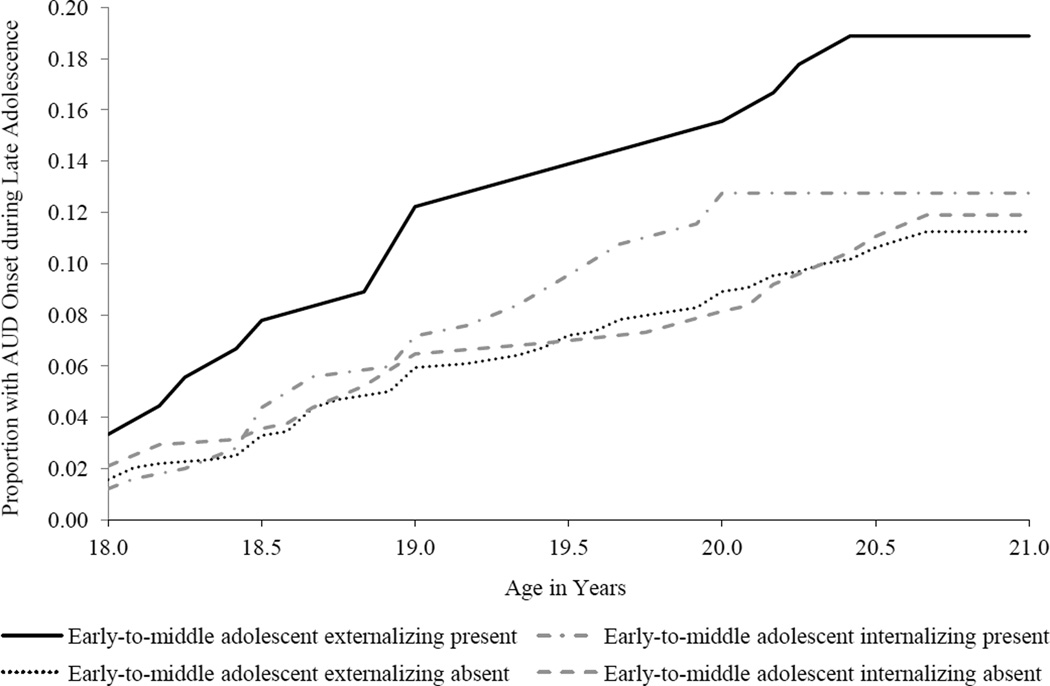
Reported under the far right column of Table 3 are adjusted analyses that evaluated internalizing and externalizing domains and subdomains as predictors of AUD onset during late adolescence. A diagnosis of any internalizing domain disorder during early-to-middle adolescence did not significantly predict AUD onset during late adolescence. The externalizing disorder domain corresponding to early-to-middle adolescence, however, was a significant predictor of late adolescent AUD onset, as was the other SUD subdomain. Cumulative hazard functions for AUD onset during late adolescence by disorder domain during early-to-middle adolescence are presented in Figure 2. As further indicated in Table 3, the presence of any childhood internalizing or externalizing domain or subdomain disorder did not achieve statistical significance in any analysis.
Figure 2.
Cumulative hazard functions for alcohol use disorder (AUD) onset during late adolescence (ages 18.0 to 20.9) by disorder domain during early-to-middle adolescence (ages 13.0 to 17.9).
3.4. Late Adolescent, Early-to-Middle Adolescent, and Childhood Psychiatric Predictors of AUD Onset During Early Adulthood
For those with an initial AUD episode onset during early adulthood (n = 128), the mean age of AUD onset was 23.8 years (SD = 2.5; Mdn = 23.2). Table 4 presents rates of internalizing and externalizing disorder occurrences for the early adult onset group, separately for late adolescence, early-to-middle adolescence, and childhood.
Table 4.
Period Prevalence Rates of Internalizing and Externalizing Psychopathology and Associations with Initial AUD Onset during Early Adulthood
| Predictor | Period
Prevalence % [CI95] |
Adjusted Associations with Time to AUD Onset during Early Adulthood HR [CI95] |
|||
|---|---|---|---|---|---|
| No AUD (n = 513) | AUD (n = 128) | Likelihood Ratio χ2 |
p-value | ||
| Late Adolescent Psychopathology | |||||
| Internalizing domain | 17.9 [14.9, 21.4] | 23.0 [16.7, 30.8] | 1.54 | .188 | 1.44 [0.92, 2.24] |
| Mood disorders | 13.3 [10.7, 16.5] | 18.2 [12.5, 25.6] | 1.72 | .162 | 1.42 [0.85, 2.37] |
| Anxiety disorders | 6.6 [4.8, 9.0] | 6.0 [3.2, 11.0] | 0.05 | .796 | 0.88 [0.43, 1.82] |
| Bulimia nervosa | 0.8 [0.3, 2.0] | 1.2 [0.3, 4.7] | 0.16 | .649 | 1.58 [0.30, 8.24] |
| Externalizing domain | 4.3 [2.8, 6.5] | 15.2 [9.8, 23.0] | 15.36 | < .001 | 3.10 [1.76, 5.50] |
| Disruptive behavior disorders | 0.9 [0.5, 2.0] | 0.6 [0.1, 4.2] | 0.13 | .664 | 0.18 [0.02, 1.70] |
| Other substance use disorders | 3.8 [2.4, 6.0] | 15.2 [9.8, 23.1] | 17.75 | < .001 | 3.96 [2.22, 7.07] |
|
Early-To-Middle
Adolescent Psychopathology |
|||||
| Internalizing domain | 23.3 [20.1, 26.8] | 30.2 [23.1, 38.3] | 2.34 | .098 | 1.41 [0.94, 2.11] |
| Mood disorders | 20.1 [17.1, 23.4] | 25.9 [19.4, 33.8] | 1.90 | .128 | 1.36 [0.89, 2.09] |
| Anxiety disorders | 5.6 [4.1, 7.7] | 9.1 [5.5, 14.6] | 1.73 | .132 | 1.71 [0.93, 3.15] |
| Bulimia nervosa | 1.2 [0.6, 2.5] | 0.6 [0.1, 4.2] | 0.37 | .473 | 0.50 [0.08, 3.27] |
| Externalizing domain | 5.6 [4.1, 7.6] | 21.2 [15.0, 29.0] | 23.97 | <.001 | 3.20 [2.03, 5.07] |
| Disruptive behavior disorders | 3.2 [2.1, 4.9] | 7.8 [4.6, 13.2] | 4.42 | .015 | 1.57 [0.82, 3.04] |
| Other substance use disorders | 2.9 [1.9, 4.5] | 14.6 [9.5, 21.8] | 20.59 | <.001 | 3.50 [2.03, 6.03] |
| Childhood Psychopathology | |||||
| Internalizing domain | 10.8 [8.7, 13.4] | 12.1 [7.8, 18.2] | 0.15 | .660 | 1.26 [0.75, 2.11] |
| Mood disorders | 6.3 [4.7, 8.3] | 6.0 [3.2, 11.0] | 0.01 | .905 | 1.12 [0.53, 2.34] |
| Anxiety disorders | 6.6 [5.0, 8.6] | 7.2 [4.1, 12.5] | 0.07 | .755 | 1.15 [0.58, 2.25] |
| Bulimia nervosa | 0.0 | 0.0 | NA | NA | NA |
| Externalizing domain | 2.7 [1.7, 4.1] | 7.2 [4.1, 12.5] | 4.86 | .010 | 2.24 [1.17, 4.25] |
| Disruptive behavior disorders | 2.1 [1.3, 3.5] | 6.6 [3.7, 11.7] | 5.43 | .007 | 2.40 [1.22, 4.71] |
| Other substance use disorders | 0.5 [0.2, 1.4] | 1.2 [0.3, 4.8] | 0.56 | .373 | 1.63 [0.51, 5.18] |
Note. Bolded table entries denote statistically significant effects.
When compared to those who did not experience an initial AUD onset within early adulthood, those with AUD onsets during this period had significantly higher rates of late adolescent externalizing domain disorders and, at the subdomain level, other SUDs. Rates of late adolescent internalizing disorders at both the domain and subdomain levels, however, did not significantly differ between those without and with initial AUD onsets during this developmental period. When compared to those who did not experience an initial AUD onset during early adulthood, those with an initial AUD onset during this period experienced significantly higher rates of early-to-middle adolescent externalizing domain disorders. When externalizing subdomains were analyzed separately, rates of disruptive behavior disorders and other SUDs significantly differed between those without and with an AUD onset during early adulthood. Rates of early-to-middle adolescent internalizing disorders at both the domain and subdomain levels did not significantly differ between those without and with initial AUD onsets during early adulthood.
In the evaluation of childhood disorders, rates of childhood externalizing domain disorders and disruptive behavior disorders significantly differed between those without and with initial AUD onsets during early adulthood. Rates of childhood internalizing disorders at both the domain and subdomain levels, however, did not significantly differ between those without and with initial AUD onsets during early adulthood.
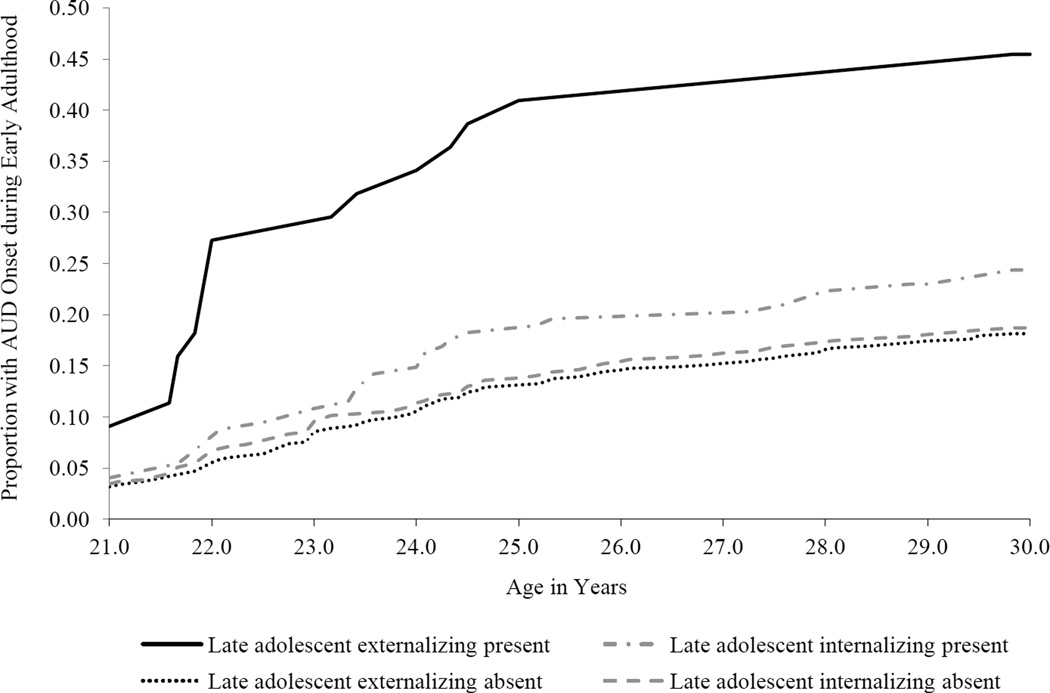
The far right column of Table 4 presents adjusted analyses that evaluated internalizing and externalizing domains as proximal and distal predictors of AUD onset during early adulthood. The externalizing disorder domain during late adolescence was significant predictor of early adult AUD onset, as was the other SUD subdomain. The internalizing domain and subdomains disorders occurring during late adolescence did not significantly predict AUD onset during early adulthood. Cumulative hazard functions for AUD onset during early adulthood by disorder domain during late adolescence are presented in Figure 3.
Figure 3.
Cumulative hazard functions for alcohol use disorder (AUD) onset during early adulthood (ages 21.0 to 30.0) by disorder domain during late adolescence (ages 18.0 to 20.9).
Externalizing domain disorders during early-to-middle adolescence and childhood were also significant distal predictors of AUD onset during early adulthood. At the subdomain level of externalizing psychopathology, other SUDs during early-to-middle adolescence and disruptive behavior disorders during childhood were each significant predictors of early adult AUD onset. No internalizing disorders at the domain or subdomain levels during early-to-middle adolescence or childhood were significant predictors of AUD onset during early adulthood.
3.5. Gender Moderation
We evaluated gender as a moderator of the association between, separately, internalizing disorders and AUD onset and externalizing disorders and AUD onset in each of the developmental period analyses presented in Tables 2 through 4. Gender moderation would be evident by statistically significant gender by predictor interactions. Gender did not emerge as a significant moderator in any developmental period analysis (all ps ≥ .250).
4. DISCUSSION
This study evaluated psychiatric disorder risk factors as predictors of future AUD episode onsets, and explored whether significant predictors differed in relation to the developmental period during which AUDs first emerged. To evaluate whether predictors differed as a function of AUD onset age and to comparatively evaluate the influence of proximal and distal predictors, statistical models were generated separately for each of three developmental periods (early-to-middle adolescence, late adolescence, and early adulthood/licit alcohol use). In these models, proximal predictors corresponding to the preceding developmental period were evaluated and, for the latter two developmental periods, distal predictors pertaining to one or more developmental periods prior to the proximal developmental period were also assessed.
For each of the three developmental periods investigated, adjusted analyses revealed that proximal externalizing domain-level disorders significantly predicted AUD onset during the next developmental period. At the externalizing subdomain level of analysis, disruptive behavior disorders had more relevance as a proximal predictor of AUD onset during the earliest developmental period (i.e., early-to-middle adolescent onset) whereas other SUDs had greater relevance as proximal predictors of AUD onsets during late adolescence and early adulthood.
Although distal psychiatric disorders had no relevance for predicting AUD onsets occurring during late adolescence, distal externalizing domain-related disorders experienced during early-to-middle adolescence and childhood were each significant predictors of AUD onset during early adulthood. Significant externalizing subdomains were other SUDs during early-to-middle adolescence and disruptive behavior disorders during childhood. These findings suggest that externalizing disorders experienced early in life continue to operate as risk factors for AUD onsets during early adult years.
Internalizing disorders at both the domain and subdomain levels were not significant predictors of AUD onset during any developmental period analysis. Overall, these findings suggest that internalizing disorders independent of comorbid externalizing disorders and demographic variables do not pose a significant risk for future AUDs in community samples, and challenge notions of an internalizing developmental pathway as a risk factor for AUDs (Hussong et al., 2011). The present research, however, was framed at the disorder-level of analysis, and it is possible that more subtle forms of internalizing tendencies that do not rise to the threshold of diagnosis may pose a risk for future AUDs (e.g., Stewart et al., 1995) as might other forms of internalizing disorders not assessed here, such as some subsets of personality disorders (Røysamb et al., 2011). We also pooled individual psychiatric disorders into domains and subdomains to form inclusive diagnostic categories to increase statistical power and, consequently, may have obscured unique associations that individual disorders within these domains have with AUD onset (Hussong et al., 2011; Nichter and Chassin, 2015).
In addition to the restricted racial and ethnic diversity of the sample, there are other limitations associated with this research that should be considered. First, diagnostic data pertaining to childhood and early adolescence (> age ~ 15) were based on retrospective assessments collected at T1. Retrospective data are subject to recall-related biases that frequently result in the under-reporting of psychopathology (Haeny et al., 2014a, 2014b; Moffitt et al., 2010). Second, this study was limited by its emphasis on predictors of index AUD episodes during early adolescence through early adulthood. Existing research suggests that genetic pathways associated with adolescent and early adult onset of alcohol dependence disorder are different from alcohol dependence episodes that occur after age 30 (Kendler et al., 2011). The extent to which the present findings generalize to cases with AUD onsets after age 30 is therefore uncertain. Third, this study emphasized the prediction of AUDs based on disorders from earlier developmental periods; consequently, this research does not take into account disorders that may have preceded the onset of AUDs within the same developmental period in which the index AUD episode emerged. Finally, this study did not consider disorder severity or duration in the prediction models for either covariates or AUDs. These features of psychiatric disorders might further contribute to the prediction of AUD onsets within subsequent developmental periods.
The present research demonstrated that proximal externalizing disorders were robust predictors of AUD onset during each of the developmental periods examined. Internalizing disorders, in comparison, were not significant predictors independent of comorbid externalizing disorders or demographic variables, suggesting that histories of internalizing disorders do not constitute a heightened risk for future AUD development. Overall, study findings imply that AUD preventive efforts should primarily focus on the externalizing pathway early in development as a means for reducing overall risk.
Highlights.
We investigated psychiatric risk factors for future alcohol use disorders (AUDs).
Externalizing domain disorders predicted AUD onset in ensuing developmental periods.
Internalizing domain disorders did not significantly predict AUD onset.
Gender did not moderate observed effects in any analysis.
Acknowledgments
Author Disclosures
Role of Funding Source
National Institutes of Health grants MH40501, MH50522, and DA12951 to Peter M. Lewinsohn and R01AA020968 to Richard F. Farmer and John R. Seeley supported this research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Earlier studies with community samples demonstrated that initial AUD onsets before age 13 are rare (Cohen et al, 1993; Clark, 2004). To evaluate the prospective associations between childhood disorders and later AUD onset, 6 cases with initial AUD onsets prior to age 13 (2% of participants with a lifetime AUD) were excluded from analyses involving predictors of onset (i.e., analyses presented in Tables 2, 3, and 4). These participants, however, were included in analyses of demographic factors related to AUD onset (Table 1).
Right-censoring here refers to an exclusion from consideration any index AUD episode onsets that emerged after the cessation of the developmental period that was the primary focus of the analysis. These cases did not have an observed AUD onset time within the developmental period examined, and were right-censored based on the last known observation time.
T1 demographic data on participants and family characteristics were used in most instances. When T1 data were missing, T2 values were used. If both T1 and T2 data were missing, we imputed values using the expectation maximization algorithm implemented in the SPSS Missing Value Analysis module. T1 and T2 data were missing for pubertal timing (< 1% missing), history of repeating a grade before age 12 (< 1% missing), education levels of head of household (4% missing), and age of heads of household (< 1% missing). All putative confounders were included as auxiliary variables in the imputation procedure.
The homogeneity of regression assumption was also tested prior to performing each adjusted analysis subsequently presented. In the analyses presented in Tables 3 and 4, only one of the models tested evidenced a violation of this assumption. In this single instance, the significant interaction terms remained in the final model whereas for all other models non-significant interaction terms were removed from the final model.
Contributors
RF and JG had the initial idea and conducted background literature searches. PL and JS were involved in the original study protocol and data collection. JG and DK programmed and conducted statistical analyses. RF and JG wrote the first draft of the manuscript. RF, JG, JS, DK, KS, and PL contributed to interpreting the findings and writing further drafts of the manuscript. All authors reviewed and have approved the final manuscript.
Contributor Information
Richard F. Farmer, Email: rfarmer@ori.org.
Jeff M. Gau, Email: jeffg@ori.org.
John R. Seeley, Email: jseeley@uoregon.edu.
Derek B. Kosty, Email: dkosty@ori.org.
Kenneth J. Sher, Email: SherK@missouri.edu.
Peter M. Lewinsohn, Email: pete@ori.org.
REFERENCES
- Achenbach TM. The classification of children's psychiatric symptoms: a factor-analytic study. Psychol. Monogr. 1966;80 doi: 10.1037/h0093906. (Whole No. 615). http://dx.doi.org/10.1037/h0093906. [DOI] [PubMed] [Google Scholar]
- Ammon L, Bond J, Matzger H, Weisner C. Gender differences in the relationship of community services and informal support to seven-year drinking trajectories of alcohol-dependent and problem drinkers. J. Stud. Alcohol Drugs. 2008;69:140–150. doi: 10.15288/jsad.2008.69.140. http://dx.doi.org/10.15288/jsad.2008.69.140. [DOI] [PubMed] [Google Scholar]
- Boschloo L, Vogelzangs N, van den Brink W, Smit JH, Veltman DJ, Beekman AT, Penninx BW. Depressive and anxiety disorders predicting first incidence of alcohol use disorders: results of the Netherlands Study of Depression and Anxiety (NESDA) J. Clin. Psychiatry. 2013;74:1233–1240. doi: 10.4088/JCP.12m08159. http://dx.doi.org/10.4088/JCP.12m08159. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Turner RJ. Social anxiety disorder as a risk factor for alcohol use disorders: a prospective examination of parental and peer influences. Drug Alcohol Depend. 2009;100:128–137. doi: 10.1016/j.drugalcdep.2008.09.018. http://dx.doi.org/10.1016/j.drugalcdep.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. J. Psychiatr. Res. 2008;42:230–239. doi: 10.1016/j.jpsychires.2007.01.002. http://dx.doi.org/10.1016/j.jpsychires.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns L, Teesson M. Alcohol use disorders comorbid with anxiety, depression and drug use disorders: findings from the Australian National Survey of Mental Health and Well Being. Drug Alcohol Depend. 2002;68:299–307. doi: 10.1016/s0376-8716(02)00220-x. http://dx.doi.org/10.1016/S0376-8716(02)00220-X. [DOI] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, Meier MH, Ramrakha S, Shalev I, Poulton R, Moffitt TE. The p factor one general psychopathology factor in the structure of psychiatric disorders? Clin. Psychol. Sci. 2014;2:119–137. doi: 10.1177/2167702613497473. http://dx.doi.org/10.1177/2167702613497473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M. The assessment of affective disorders in children and adolescents by semistructured interview: test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present Episode version. Arch. Gen. Psychiatry. 1985;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. http://dx.doi.org/10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- Chassin L, Flora DB, King KM. Trajectories of alcohol and drug use and dependence from adolescence to adulthood: the effects of familial alcoholism and personality. J. Abnorm. Psychol. 2004;113:483–498. doi: 10.1037/0021-843X.113.4.483. http://dx.doi.org/10.1037/0021-843X.113.4.483. [DOI] [PubMed] [Google Scholar]
- Clark DB. The natural history of adolescent alcohol use disorders. Addiction. 2004;99(Suppl 2):5–22. doi: 10.1111/j.1360-0443.2004.00851.x. http://dx.doi.org/10.1111/j.1360-0443.2004.00851.x. [DOI] [PubMed] [Google Scholar]
- Cohen P, Cohen J, Kasen S, Velez CN, Hartmark C, Johnson J, et al. An epidemiological study of disorders in late childhood and adolescence—I. Age- and gender- specific prevalence. J. Child Psychol. Psychiatry. 1993;34:851–867. doi: 10.1111/j.1469-7610.1993.tb01094.x. http://dx.doi.org/10.1111/j.1469-7610.1993.tb01094.x. [DOI] [PubMed] [Google Scholar]
- Crum RM, Pratt LA. Risk of heavy drinking and alcohol use disorders in social phobia: a prospective analysis. Am. J. Psychiatry. 2001;158:1693–1700. doi: 10.1176/appi.ajp.158.10.1693. http://dx.doi.org/10.1176/appi.ajp.158.10.1693. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, King SM, McGue M, Iacono WG. Personality traits and the development of nicotine, alcohol, and illicit drug disorders: prospective links from adolescence to young adulthood. J. Abnorm. Psychol. 2006;115:26–39. doi: 10.1037/0021-843X.115.1.26. http://dx.doi.org/10.1037/0021-843X.115.1.26. [DOI] [PubMed] [Google Scholar]
- Englund MM, Egeland B, Oliva EM, Collins WA. Childhood and adolescent predictors of heavy drinking and alcohol use disorders in early adulthood: a longitudinal developmental analysis. Addiction. 2008;103:23–35. doi: 10.1111/j.1360-0443.2008.02174.x. http://dx.doi.org/10.1111/j.1360-0443.2008.02174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer RF, Kosty DB, Seeley JR, Olino TM, Lewinsohn PM. Aggregation of lifetime axis I psychiatric disorders through age 30: incidence, predictors, and associated psychosocial outcomes. J. Abnorm. Psychol. 2013a;122:573–586. doi: 10.1037/a0031429. http://dx.doi.org/10.1037/a0031429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer RF, Seeley JR, Kosty DB, Lewinsohn PM. Refinements in the hierarchical structure of externalizing psychiatric disorders: patterns of lifetime liability from mid-adolescence through early adulthood. J. Abnorm. Psychol. 2009;118:699–710. doi: 10.1037/a0017205. http://dx.doi.org/10.1037/a0017205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer RF, Seeley JR, Kosty DB, Olino TM, Lewinsohn PM. Hierarchical organization of axis I psychiatric disorder comorbidity through age 30. Compr. Psychiatry. 2013b;54:523–532. doi: 10.1016/j.comppsych.2012.12.007. http://dx.doi.org/10.1016/j.comppsych.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feingold A, Capaldi DM, Owen LD. Proximal vs. distal predictors of alcohol use disorders and treatment utilization in at-risk men in early middle age. Compr. Psychiatry. 2015;61:64–71. doi: 10.1016/j.comppsych.2015.05.010. http://dx.doi.org/10.1016/j.comppsych.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ. Structural models of the comorbidity of internalizing disorders and substance use disorders in a longitudinal birth cohort. Soc. Psychiatry Psychiatr. Epidemiol. 2011;46:933–942. doi: 10.1007/s00127-010-0268-1. http://dx.doi.org/10.1007/s00127-010-0268-1. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM. Conduct and attentional problems in childhood and adolescence and later substance use, abuse and dependence: results of a 25-year longitudinal study. Drug Alcohol Depend. 2007;88:S14–S26. doi: 10.1016/j.drugalcdep.2006.12.011. http://dx.doi.org/10.1016/j.drugalcdep.2006.12.011. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for Axis I DSM-IV disorders, Non-patient Edition. New York: Biometrics Research Department; 1994. [Google Scholar]
- Foster KT, Hicks BM, Iacono WG, McGue M. Gender differences in the structure of risk for alcohol use disorder in adolescence and young adulthood. Psychol. Med. 2015;45:3047–3058. doi: 10.1017/S0033291715001014. http://dx.doi.org/10.1017/S0033291715001014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman SE, Abraham HD. A longitudinal study of the order of onset of alcohol dependence and major depression. Drug Alcohol Depend. 2001;63:277–286. doi: 10.1016/s0376-8716(00)00216-7. http://dx.doi.org/10.1016/S0376-8716(00)00216-7. [DOI] [PubMed] [Google Scholar]
- Graber JA, Lewinsohn PM, Seeley JR, Brooks-Gunn J. Is psychopathology associated with the timing of pubertal development? J. Am. Acad. Child Adolesc. Psychiatry. 1997;36:1768–1776. doi: 10.1097/00004583-199712000-00026. http://dx.doi.org/10.1097/00004583-199712000-00026. [DOI] [PubMed] [Google Scholar]
- Grekin ER, Sher KJ, Wood PK. Personality and substance dependence symptoms: modeling substance-specific traits. Psychol. Addict. Behav. 2006;20:415–424. doi: 10.1037/0893-164X.20.4.415. http://dx.doi.org/10.1037/0893-164X.20.4.415. [DOI] [PubMed] [Google Scholar]
- Haeny AM, Littlefield AK, Sher KJ. Repeated diagnoses of lifetime alcohol use disorders in a prospective study: insights into the extent and nature of the reliability and validity problem. Alcohol. Clin. Exp. Res. 2014a;38:489–500. doi: 10.1111/acer.12237. http://dx.doi.org/10.1111/acer.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haeny AM, Littlefield AK, Sher KJ. False negatives in the assessment of lifetime alcohol use disorders: a serious but unappreciated problem. J. Stud. Alcohol Drugs. 2014b;75:530–535. doi: 10.15288/jsad.2014.75.530. http://dx.doi.org/10.15288/jsad.2014.75.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, O'Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, Compton WM, Crowley T, Ling W, Petry NM, Schuckit M, Grant BF. DSM-5 criteria for substance use disorders: recommendations and rationale. Am. J. Psychiatry. 2013;170:834–851. doi: 10.1176/appi.ajp.2013.12060782. http://dx.doi.org/10.1176/appi.ajp.2013.12060782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. http://dx.doi.org/10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychol. Addict. Behav. 2011;25:390–404. doi: 10.1037/a0024519. http://dx.doi.org/10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson BA, Cloninger CR, Roache JD, Bordnick PS, Ruiz P. Age of onset as a discriminator between alcoholic subtypes in a treatment- seeking outpatient population. Am. J. Addict. 2000;9:17–27. doi: 10.1080/10550490050172191. http://dx.doi.org/10.1080/10550490050172191. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Yamaguchi K, Chen K. Stages of progression in drug involvement from adolescence to adulthood: further evidence for the gateway theory. J. Stud. Alcohol. 1992;53:447–457. doi: 10.15288/jsa.1992.53.447. http://dx.doi.org/10.15288/jsa.1992.53.447. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott PA. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch. Gen. Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. http://dx.doi.org/10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner C, Dick DM. Predicting alcohol consumption in adolescence from alcohol-specific and general externalizing genetic risk factors, key environmental exposures and their interaction. Psychol. Med. 2011;41:1507–1516. doi: 10.1017/S003329171000190X. http://dx.doi.org/10.1017/S003329171000190X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch. Gen. Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. http://dx.doi.org/10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. http://dx.doi.org/10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, et al. Development of lifetime comorbidity in the World Health Organization World Mental Health Surveys. Arch. Gen. Psychiatry. 2011;68:90–100. doi: 10.1001/archgenpsychiatry.2010.180. http://dx.doi.org/10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Arch. Gen. Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. http://dx.doi.org/10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE. Reinterpreting comorbidity: a model-based approach to understanding and classifying psychopathology. Annu. Rev. Clin. Psychol. 2006;2:111–133. doi: 10.1146/annurev.clinpsy.2.022305.095213. http://dx.doi.org/10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Erickson DJ. Prospective analysis of the relation between DSM-III anxiety disorders and alcohol use disorders. Am. J. Psychiatry. 1999;156:723–732. doi: 10.1176/ajp.156.5.723. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J. Abnorm. Psychol. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. http://dx.doi.org/10.1037/0021-843X.102.1.133. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol. Med. 2010;40:899–909. doi: 10.1017/S0033291709991036. http://dx.doi.org/10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIAAA. Alcohol research: A lifespan perspective. NIAAA Publication No. 74. 2008 Retrieved 27 December 2015 at http://pubs.niaaa.nih.gov/publications/AA74/AA74.htm.
- Nichter B, Chassin L. Separate dimensions of anxiety differentially predict alcohol use among male juvenile offenders. Addict. Behav. 2015;50:144–148. doi: 10.1016/j.addbeh.2015.06.031. http://dx.doi.org/10.1016/j.addbeh.2015.06.031. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clin. Psychol. Rev. 2004;24:981–1010. doi: 10.1016/j.cpr.2004.08.003. http://dx.doi.org/10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Orvaschel H, Puig-Antich J, Chambers WJ, Tabrizi MA, Johnson R. Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. J. Am. Acad. Child Adolesc. Psychiatry. 1982;21:392–397. doi: 10.1016/s0002-7138(09)60944-4. http://dx.doi.org/10.1016/S0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR, Klein DN, Andrews JA, Small JW. Psychosocial functioning of adults who experienced substance use disorders as adolescents. Psychol. Addictive Behav. 2007;21:155–164. doi: 10.1037/0893-164X.21.2.155. http://dx.doi.org/10.1037/0893-164X.21.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Røysamb E, Kendler KS, Tambs K, Ørstavik RE, Neale MC, Aggen SH, Torgersen S, Reichborn-Kjennerud T. The joint structure of DSM-IV Axis I and Axis II disorders. J. Abnorm. Psychol. 2011;120:198–209. doi: 10.1037/a0021660. http://dx.doi.org/10.1037/a0021660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeley JR, Kosty DB, Farmer RF, Lewinsohn PM. The modeling of internalizing disorders on the basis of patterns of lifetime comorbidity: associations with psychosocial impairment and psychiatric disorders among first–degree relatives. J. Abnorm. Psychol. 2011;120:308–321. doi: 10.1037/a0022621. http://dx.doi.org/10.1037/a0022621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher KJ, Grekin ER, Williams NA. The development of alcohol use disorders. Annu. Rev. Clin. Psychol. 2005;1:493–523. doi: 10.1146/annurev.clinpsy.1.102803.144107. http://dx.doi.org/10.1146/annurev.clinpsy.1.102803.144107. [DOI] [PubMed] [Google Scholar]
- Slade T, Grove R, Teesson M. A taxometric study of alcohol abuse and dependence in a general population sample: evidence of dimensional latent structure and implications for DSM- V. Addiction. 2009;104:742–751. doi: 10.1111/j.1360-0443.2009.02498.x. http://dx.doi.org/10.1111/j.1360-0443.2009.02498.x. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Peterson JB, Pihl RO. Anxiety sensitivity and self-reported alcohol consumption rates in university women. J. Anxiety Disord. 1995;9:283–292. http://dx.doi.org/10.1016/0887-6185(95)00009-D. [Google Scholar]
- Trautmann S, Schönfeld S, Behrendt S, Heinrich A, Höfler M, Siegel S, Zimmermann P, Wittchen HU. Stress exposure and the risk for the onset of alcohol use disorders and nicotine dependence in deployed military personnel: the role of prior internalizing disorders. Addict. Behav. 2015;43:89–96. doi: 10.1016/j.addbeh.2014.12.013. http://dx.doi.org/10.1016/j.addbeh.2014.12.013. [DOI] [PubMed] [Google Scholar]
- Vanyukov MM, Tarter RE, Kirillova GP, Kirisci L, Reynolds MD, Kreek MJ, Conway KP, Maher BS, Iacono WG, Bierut L, Neale MC, Clark DB, idenour TA. Common liability to addiction and "gateway hypothesis": theoretical, empirical and evolutionary perspective. Drug Alcohol Depend. 2012;123:S3–S17. doi: 10.1016/j.drugalcdep.2011.12.018. http://dx.doi.org/10.1016/j.drugalcdep.2011.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann P, Wittchen HU, Höfler M, Pfister H, Kessler RC, Lieb R. Primary anxiety disorders and the development of subsequent alcohol use disorders: a 4-year community study of adolescents and young adults. Psychol. Med. 2003;33:1211–1222. doi: 10.1017/s0033291703008158. http://dx.doi.org/10.1017/S0033291703008158. [DOI] [PubMed] [Google Scholar]