Abstract
Cervical cancer is a common and deadly disease, especially in developing countries. We developed and implemented an interactive, tablet-based educational intervention to improve cervical cancer knowledge among women in rural Malawi. Chichewa-speaking adult women in six rural villages participated. Each woman took a pre-test, participated in the lesson, and then took a post-test. The lesson included information on cervical cancer symptoms, causes, risk factors, prevention, and treatment. Over the 6-month study period, 243 women participated. Women ranged in age from 18 to 77 years. Only 15% had education beyond primary school. Nearly half of participants (48%) had heard of cervical cancer prior to viewing the lesson. For these women, the median number of correct responses on the pre-test was 11 out of 20; after the lesson, they had a median of 18 correct responses (p<0.001). After the intervention, 93% of women indicated a desire for cervical cancer screening. Despite lack of familiarity with computers (96%), most women (94%) found the tablet easy to use. A tablet-based educational program was an effective, feasible and acceptable strategy to disseminate cervical cancer information to women with low education in rural Malawi. This method may be appropriate to distribute health information about other health topics in low-resource settings.
Keywords: patient education, eHealth, reproductive health, cervical cancer, global health, Malawi, HPV, screening
INTRODUCTION
Cervical cancer is a common disease and deadly unless diagnosed early. Each year around 500,000 new cases are diagnosed worldwide, 80% of which occur in developing countries [1]. Sub-Saharan Africa has a particularly high rate of cervical cancer; in Malawi, 75.9 out of every 100,000 women develop cervical cancer each year [2]. Screening is key to decreasing cervical cancer morbidity and mortality, however, only 3% of women in Malawi have ever been screened [3]. By the time cervical cancer is detected, most women have advanced disease, and prognosis is poor [4]. Treatment is also available only in large urban hospitals, and remains out of reach for most women. For these reasons, 80% of Malawian women who develop cervical cancer die from this disease [1].
Studies in Malawi suggest that while women are widely aware of cervical cancer, they hold a great deal of false information on the causes, symptoms, screening and treatment of this disease [5–7]. Therefore, educational efforts to correct misinformation, especially as screening becomes more widely available, may greatly impact women’s decision to seek screening. In recent years in the United States, educational interventions administered on portable tablet computers have been used for patient education on various diagnoses and therapies, including diabetes, prostate cancer, and contraception [8–10]. These programs bring unique advantages: mobility, fidelity, and cost-effectiveness [8–12]. However, little research has assessed whether tablet-based educational interventions are acceptable, feasible, or effective outside of the US, especially in rural areas.
We developed and tested a tablet-based educational intervention for rural Malawian women, to inform this population about the causes, symptoms, screening, and treatment of cervical cancer. We hypothesize that interactive educational messages delivered via tablet can be an effective and feasible method to disseminate information about cervical cancer and other reproductive health topics to populations in rural Africa.
MATERIALS AND METHODS
In this study, we assessed a new cervical cancer educational intervention. Participants completed a pretest on cervical cancer knowledge, participated in the tablet-based educational program, and then completed a posttest. We evaluated knowledge before and after the intervention.
Study Team
The study was conducted through a collaboration between Ohio State University, the University of Malawi College of Medicine, and the non-profit organization Child Legacy International. As part of an earlier study, this team had observed that cervical cancer was a dominant health concern for women in this community; the educational intervention was developed to respond to these concerns.
Study Setting and Population
The study was conducted from July–December 2014 in six villages in Central Malawi. The selected villages surround a health facility, Child Legacy International, in a rural district of Lilongwe; the facility serves a catchment area of 68 villages and more than 20,000 people. The six study villages were chosen for convenience based on their proximity to the health facility. Every household in each selected village was approached to recruit participants. All Chichewa-speaking women aged 18 or older were eligible to participate.
Educational Program and Survey Materials
The content of the educational program included: 1) anatomical and etiological information; 2) information on local availability of screening and treatment; and 3) correction of misconceptions about cervical cancer causes, screening and treatment. Misconceptions addressed by the program had been identified from the published literature [5–6] and from formative focus groups with the target population. The content was developed in English, reviewed by a cervical cancer expert outside the primary study team, and translated into Chichewa. All content was video- and audio-recorded, and transferred into Keynote (Apple Inc., Cupertino, CA) for presentation. The content of the video, both in English and Chichewa, was piloted extensively by staff at the health facility to ensure that all information was presented in a culturally appropriate manner.
The video began with a short tutorial showing the participant how use the device and interact with the screen. During the lesson, the participant encountered 12 “opportunities for interaction.” About half of these opportunities allowed the participant to move forward or backward in the lesson by touching the screen with her finger or a stylus. The other half of the opportunities for interaction came in the form of “quiz” questions, separate from the pre/post testing, to engage the participant in learning. For example, after learning in the video about risk factors for cervical cancer, the participant was asked “True or False, HPV is a virus that is passed between sex partners during sex.” The participant then had the option to choose an answer on the screen. If the participant answered incorrectly, she had the opportunity to try again. If the participant had any trouble with the device during the opportunities for interaction, research staff were available to aid her.
Data Collection
In each study village, we held two meetings prior to the start of data collection – one with the village chief and one with women – to introduce the research team and explain the study objectives. All meetings were conducted in Chichewa, and all study materials were administered by native Chichewa speakers.
Following these meetings, a trained study staff member went door-to-door to recruit eligible participants individually from each household. After providing verbal consent, each participant completed a 15-minute, interviewer-administered pretest (available upon request) to assess demographic information and cervical cancer knowledge. The pretest was administered using the electronic data capture system MagPi (Magpi, Washington, DC). Participants who reported they had heard of cervical cancer completed the full pretest (“pretest-posttest group”). By design, participants who reported they had never heard of cervical cancer (even with careful probing by the interviewer) subsequently skipped nearly all questions related to cervical cancer knowledge in the pretest and completed a shortened version that captured only demographic data. These participants are referred to as the “posttest-only” group.
Following the pretest, each participant engaged in the 30-minute tablet-based educational program. If the participant encountered problems with the administration of the program, the interviewer aided her and made note of difficulties.
At the end of the educational program, the interviewer administered a 15-minute posttest, again using Magpi, to measure changes in cervical cancer knowledge, as well as to assess the feasibility and acceptability of the tablet-based educational program. All participants completed the full posttest, regardless of pretest completion. After the posttest, participants were given 1,000 Malawian Kwacha (MK) (~$3 USD at the time of the study) for their time.
Pretest and posttest data were uploaded nightly to the secure Magpi website.
Data Analysis
Demographic data are reported as frequency and percent (categorical data), and median and interquartile range (IQR) (continuous data). Pretest-posttest and posttest-only groups were compared with chi-square tests and Mann-Whitney U tests for categorical and continuous variables, respectively.
We graded the cervical cancer knowledge questions out of a total score of 20. To compare pretest and posttest scores, we used a paired t-test to test. For the pretest-posttest group, we used McNemar’s test to compare individual questions on the pretest and posttest. Additionally, we compared posttest answers to each individual question between the two groups (pretest-posttest and posttest-only) using Mann-Whitney U tests.
For acceptability and feasibility questions, we calculated frequency and percent. Data analysis was performed using Stata 13.1 (StataCorp, College Station, Texas).
Ethical approval
This project received ethical approval from the Ohio State University Institutional Review Board and the University of Malawi College of Medicine Research and Ethics Committee.
RESULTS
Between July and December 2014, 243 women participated in the study. No eligible woman declined enrollment. Of participating women, 117 had heard of cervical cancer prior to the study (pretest-posttest group). The remaining 126 women completed a shortened version of the pretest (posttest-only group).
Study Sample Characteristics
The ages of the 243 participants ranged from 18 to 77 years with a median age of 29 (IQR: 21 to 43 years). A majority (59%) of women were married, 16% were single and the remaining 24% were divorced or widowed. Most women had received little schooling, with only 15% reaching higher than primary school and 21% with no schooling at all. Three-quarters of women reported a household monthly income of 20,000 MK (≈ $42) or less (Table 1).
Table 1.
Characteristics of participating women (n=243)
| Total | Participants who had heard of cervical cancer prior to intervention (Pretest- posttest group) |
Participants who had NOT heard of cervical cancer prior to intervention (Posttest-only group) |
P- value | ||||
|---|---|---|---|---|---|---|---|
| N=243 | (%) | N=117 | (%) | N=126 | (%) | ||
| Village | <0.001 | ||||||
| Village 1 | 48 | (20) | 45 | (38) | 3 | (2) | |
| Village 2 | 75 | (31) | 25 | (21) | 50 | (40) | |
| Village 3 | 25 | (10) | 6 | (5) | 19 | (15) | |
| Village 4 | 32 | (13) | 12 | (10) | 20 | (16) | |
| Village 5 | 20 | (8) | 10 | (9) | 10 | (8) | |
| Village 6 | 43 | (18) | 19 | (16) | 24 | (19) | |
| Marital Status | 0.307 | ||||||
| Single | 40 | (16) | 23 | (20) | 17 | (13) | |
| Married | 144 | (59) | 64 | (55) | 80 | (63) | |
| Divorced or widowed | 59 | (24) | 30 | (26) | 29 | (23) | |
| Highest level of schooling | 0.001 | ||||||
| None | 51 | (21) | 13 | (11) | 38 | (30) | |
| Standard 1–3 | 44 | (18) | 19 | (16) | 25 | (20) | |
| Standard 4–8 | 112 | (46) | 62 | (53) | 50 | (40) | |
| More than elementary | 36 | (15) | 23 | (20) | 13 | (10) | |
| Employed | 0.021 | ||||||
| Yes | 206 | (85) | 92 | (79) | 114 | (90) | |
| No | 14 | (6) | 11 | (9) | 3 | (2) | |
| In School | 23 | (9) | 14 | (12) | 9 | (7) | |
| Monthly Income | 0.352 | ||||||
| Less than 20,000 MK (»$42) | 176 | (74) | 87 | (78) | 89 | (71) | |
| 20,000–40,000 MK (»$42–85) | 56 | (24) | 22 | (20) | 34 | (27) | |
| More than 40,000 MK (»$85) | 5 | (2) | 3 | (3) | 2 | (2) | |
| Median | (IQR) | Median | (IQR) | Median | (IQR) | ||
| Age | 29 | (21–43) | 25 | (20–38) | 34.5 | (23–46) | <0.001 |
Data gathered July–December 2014 from women 18 years and older in rural Malawian villages.
We observed some significant differences in the demographic characteristics of women in the pretest-posttest group versus the posttest-only group (Table 1). Specifically, younger women, women who had attended more school, and women from one of the six villages more frequently answered that they had previously heard of cervical cancer, and thus were in the pretest-posttest group.
Pretest and Posttest Cervical Cancer Knowledge
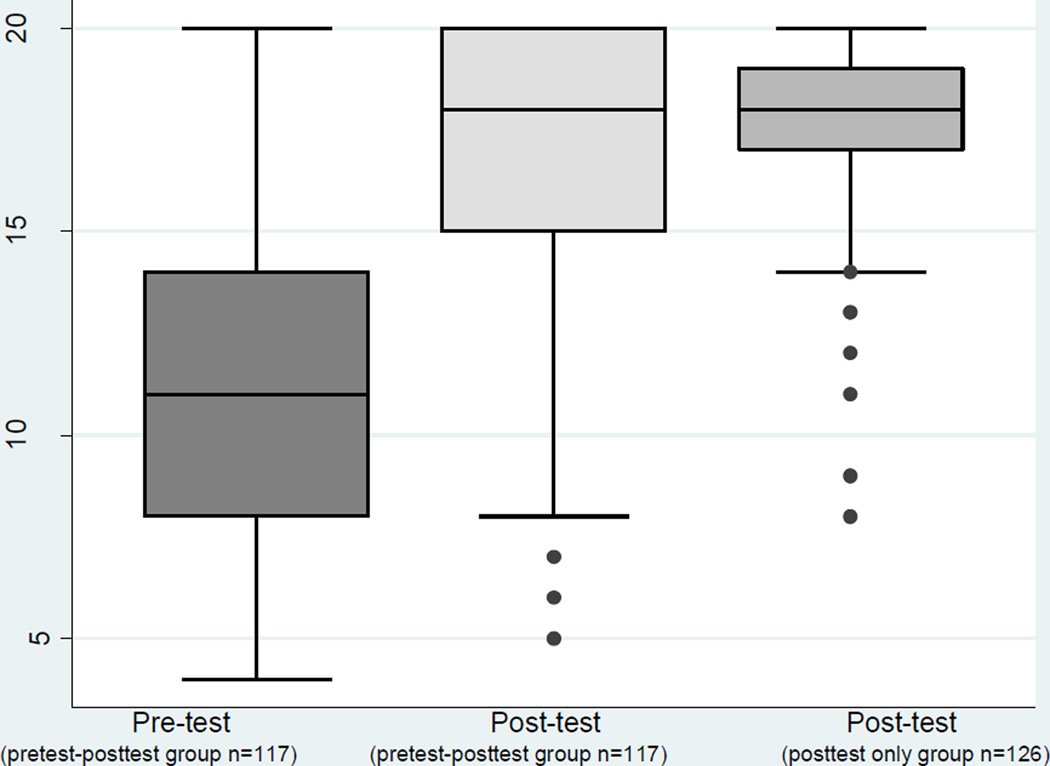
Both the pretest and posttest asked about cervical cancer anatomy, symptoms, cause, risk factors, prevention, and treatment. Each question was given equal weight, and the final scores are reported out of 20. For the pretest-posttest group, the median pretest score was 11 and the median posttest score was 18 (p<0.001). The mean pre-post difference for these 117 subjects was −5.73 (95% CI: −6.38, −5.09). For the posttest-only group, the median posttest score was also 18 (Fig 1).
Fig 1. Distribution of Pretest and Posttest scores.
In this box chart, the length of each box represents the interquartile range, and the horizontal line inside the box represents the median. The “whiskers” represent the upper and lower bounds of the data. The dots represent outliers, or anything greater or less than 3/2 the interquartile range.
There is a significant improvement in test scores after the intervention (p<0.001). There is no significant difference in posttest scores between those who had heard of cervical cancer before the intervention (pretest-posttest group) and those who had not (posttest-only group).
For the pretest-posttest group, a question-by-question analysis was conducted to understand increases in knowledge following the educational program (Table 2). We observed significant improvement on most questions. For example, for the question “Can cervical cancer be prevented?” 32% of pretest and 88% of posttest participants chose the correct response (“Yes”). In the section about risk factors, one question asked “Eating contaminated meat - Does this increase, decrease, or not change a woman’s chance of getting cervical cancer?” About one third (35%) of pretest participants, vs. 73% of posttest participants, chose the correct response (“Neither increases nor decreases”). The only question which did not show significant improvement was: “Having sex with multiple sex partners - Does this increase, decrease, or not change a woman’s chance of getting cervical cancer?”: because 97% of pretest participants chose the correct response, (“Increase”), there was no room for significant improvement.
Table 2.
Cervical cancer knowledge before and after the tablet-based educational intervention (n=243)
| Correct on pretest (pretest- posttest group) |
Correct on posttest (pretest- posttest group) |
McNemar's P-value* |
Correct on posttest (posttest- only group) |
P- value** |
||||
|---|---|---|---|---|---|---|---|---|
| N=243 | (%) | N=117 | (%) | N=126 | (%) | |||
| Where is the cervix located? (Participant shown diagram of female reproductive tract) | 65 | (56) | 108 | (92) | <0.001 | 112 | (89) | 0.364 |
| What are the symptoms of cervical cancer? | 43 | (37) | 85 | (73) | <0.001 | 95 | (75) | 0.626 |
| Can cervical cancer be prevented? | 38 | (32) | 103 | (88) | <0.001 | 114 | (90) | 0.539 |
| What is/are the cause/s of cervical cancer? | 48 | (41) | 105 | (90) | <0.001 | 122 | (97) | 0.027 |
| Is cervical cancer caused by HIV, the AIDS virus? | 95 | (81) | 106 | (91) | 0.034 | 117 | (93) | 0.523 |
| Is there a test to find signs of cervical cancer before a woman notices any symptoms of disease? | 77 | (66) | 108 | (92) | <0.001 | 118 | (94) | 0.682 |
| Where is the closest place to get this test? | 20 | (17) | 85 | (73) | <0.001 | 110 | (87) | 0.004 |
| If a woman is found to have cervical cancer, does treatment exist? | 74 | (63) | 114 | (97) | <0.001 | 123 | (98) | 0.927 |
| Can cervical cancer be cured? | 43 | (37) | 96 | (82) | <0.001 | 107 | (85) | 0.548 |
| Risk factor identification: State whether the following increase, decrease, or do getting cervical cancer. | ||||||||
| Being coughed or sneezed on by a person who has cervical cancer | 68 | (58) | 96 | (82) | <0.001 | 104 | (83) | 0.921 |
| Smoking cigarettes or pipes | 84 | (71) | 107 | (91) | <0.001 | 110 | (87) | 0.297 |
| Eating contaminated meat | 41 | (35) | 85 | (73) | <0.001 | 95 | (75) | 0.626 |
| Working with farm animals | 74 | (63) | 92 | (79) | 0.002 | 114 | (90) | 0.010 |
| Having sex with multiple sex partners | 115 | (97) | 116 | (99) | 0.317 | 125 | (99) | 0.958 |
| Drinking water from the same cup as a person who has cervical cancer | 75 | (64) | 94 | (80) | <0.001 | 114 | (90) | 0.025 |
| Sex without a condom | 109 | (92) | 116 | (99) | 0.020 | 114 | (90) | 0.003 |
| Having sex with a circumcised man | 35 | (30) | 90 | (77) | <0.001 | 91 | (72) | 0.402 |
| Taking certain medications | 52 | (44) | 81 | (69) | <0.001 | 95 | (75) | 0.284 |
| Using contraception to prevent pregnancy | 61 | (52) | 86 | (74) | <0.001 | 108 | (86) | 0.018 |
| If a woman's mother has cervical cancer | 77 | (65) | 92 | (79) | 0.004 | 115 | (91) | 0.006 |
Data gathered July–December 2014 from women 18 years and older in rural Malawian villages.
Comparing paired pretest and posttest answers in the pretest-posttest group
Comparing posttest answers of the pretest-posttest group and the posttest-only group
We also performed a question-by-question analysis comparing posttest answers between the two groups (pretest-posttest and posttest-only). Those in the posttest-only group – who had not heard of cervical cancer prior to the study – performed significantly better than women in the pretest-posttest group on some questions about the causes and risk factors of cervical cancer (Table 2).
Cervical Cancer Screening
On the posttest, 226 participants (93%) stated that they would like to obtain cervical cancer screening. Of the 17 who did not want screening, all explained that they were either too old or not having sex, and thus did not feel at risk for cervical cancer. These women had a median age of 61 and most (76%) were either divorced or widowed.
On both the pretest and posttest, women were asked, “What factors would encourage you to get cervical cancer screening?” On the posttest, women most commonly answered that experiencing the symptoms of cervical cancer would encourage them to get screening (n=65, 29%). Participants also stated that a screening test that is provided without paying a fee (12%), painless (11%), and at a nearby location (10%) are encouraging factors. Participants were also asked, “What factors would discourage you from getting cervical cancer screening?” Some women identified distance from the testing site (8%) or fear that the screening test was dangerous (6%) as discouraging factors. However, most women did not identify any factors that would discourage them from screening.
Acceptability and Feasibility
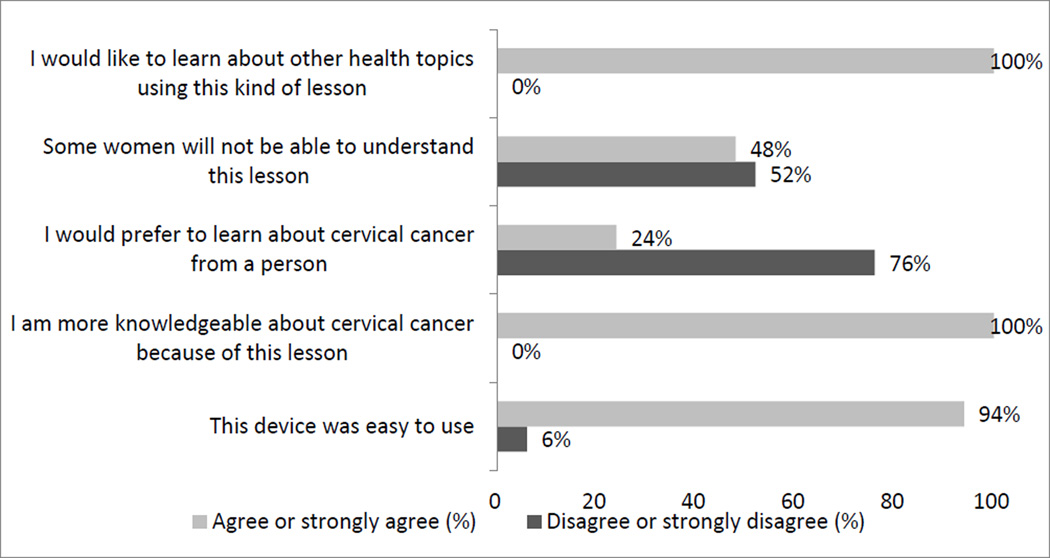
All participants answered multiple questions about the acceptability and feasibility of the tablet-based lesson. The majority of participants had not used a computer (96%) or smart phone (88%) prior to the study. Most women preferred the tablet to learning from a person (76%), and all participants wanted to learn about other health topics from the tablet (100%) (Fig 2). In a free-response section at the end of the posttest, women showed overwhelming enthusiasm for the lesson and requested that the research team return with similar lessons.
Fig 2. Acceptability and feasibility of the educational intervention.
The tablet-based lesson was highly acceptable and easy to use.
Ease of tablet use was evaluated in two ways. First, the research assistant recorded how many times he or she needed to aid the participant during each of the “opportunities for interaction.” Out of the 12 opportunities of interaction, participants needed assistance a median of 2 times per lesson. Ease of use was also evaluated by asking participants how easy or difficult it was to use the device and to interact with the screen: 94% found the device easy to use, and 82% specifically found touching the screen easy.
DISCUSSION
We aimed to study the effectiveness, feasibility, and acceptability of a tablet-based educational intervention in a low-resource setting. Our intervention was effective, with significant improvements in posttest scores both among women with prior knowledge of cervical cancer and those who had never heard of this disease. An important finding was that posttest knowledge appeared to be the same for these two groups of women, suggesting that tablet-based education is equally effective irrespective of baseline knowledge. Question-by-question analysis showed significant improvement in all areas of knowledge. Our intervention was also feasible. Despite very limited prior use of technology, participants required only modest assistance in operating the tablet and reported that the tablet was easy to use. Finally, our intervention was acceptable. Participants enjoyed using the device and enthusiastically indicated that they would like to learn about more health topics using this approach.
Cervical cancer is a common and deadly disease in developing countries. Malawi in particular has an extremely high rate of cervical cancer, with an estimated age standardized rate of 75.9 per 100,000 [2]. Screening is one key component to cervical cancer prevention, but screening in Malawi is limited due to lack of knowledge about cervical cancer [3–6]. In our study, roughly half of enrolled women had never heard of cervical cancer prior to their participation. Older women and women with little schooling were less likely to have heard of cervical cancer. Interestingly, in one village, nearly all women had heard of cervical cancer: with further investigation, we discovered that a woman from this village recently died from cervical cancer. This finding highlights the importance of social networks in the spread of health knowledge, a concept that is supported in the literature [13].
Other studies have identified misconceptions about cervical cancer, including misunderstanding about pathogenesis, susceptibility, risk factors, and treatment of the disease [5–6, 14]. Similarly, we found low understanding of nearly all aspects of cervical cancer, including a number of misconceptions that, to our knowledge, have not been previously identified. For example, prior to the intervention many women thought that eating contaminated meat increased a woman’s chances of developing cervical cancer. Our intervention was successful at debunking this myth. The pretest also revealed interesting baseline knowledge about medications and contraception. Many women thought that common medications, both traditional and modern (such as aspirin and antibiotics), could modify cervical cancer risk. Many women also thought that modern methods of contraception, specifically oral contraceptive pills and birth control injections, affected cervical cancer risk. The relationship between hormonal contraception and cervical cancer has been debated in the literature, with some finding an increase and some finding no change [15–17]. However, it is generally accepted that the benefits of contraception outweigh any potential increased risk of cervical cancer [17]. The appropriate way to address women’s understanding of hormonal contraception in relation to cervical cancer risk is an area for further research.
In our study, all areas of cervical cancer knowledge showed improvement on the posttest. Interestingly, the posttest-only group had higher median scores on a number of questions than the pretest-posttest group. Those with prior incorrect knowledge may have a harder time internalizing new information compared to those with no baseline knowledge [18], possibly explaining the slightly improved performance of the posttest-only group.
In addition to an increase in knowledge, participants showed a great interest in obtaining cervical cancer screening following the intervention. The lesson promoted screening using visual inspection of the cervix with acetic acid (VIA), the recommended method of screening in low-resource areas [1]. Screening is generally recommended from age 30–50, with the highest rate of cervical cancer at ages 30–39 [19]. However, there is still a high rate of cervical cancer both below 30 and above 50, and there are no official age recommendations or limits for screening in Malawi. Therefore, we did not specify an age of screening in our intervention. Despite this, some of the older women indicated that they would not need screening because of their age. If screening of women over age 50 becomes feasible, an intervention targeted to women in this age group may be necessary.
Health education has been shown to be effective through many avenues, including promoting a healthy lifestyle [20], improving rates of disease screening [21], and increasing compliance with treatment [22]. Cervical cancer is just one example of a prevalent and deadly health problem that can be ameliorated through education. Technology-based methods such as computer-based and text message-based educational interventions have been studied throughout Africa for other healthcare topics and have shown great promise [12, 23–24]. In recent years, educational interventions administered on portable tablet computers have been developed and bring unique advantages: mobility, interactivity, and cost-effectiveness [8–11, 24]. However, little research has assessed whether tablet-based educational interventions are acceptable, feasible, or effective outside of the US, especially in rural areas. Our study is one of the first to look at tablet-based education in a low-resource setting. Participants had extremely low levels of technology use prior to our study, yet they found the tablet highly acceptable. About half of the participants stated that others may have difficulty with the device. However this is consistent with the idea that people often overestimate their own abilities compared to others, a phenomenon called “illusory superiority.” In reality, women only needed modest assistance with the device and found it easy to use. Participants enjoyed the lesson and expressed desire for future educational content to be delivered in this fashion. In addition to having great potential utility in rural Africa, the standardization of educational information permitted by tablet-based programs may also have value in higher-resource settings, including in medical clinics [25–26] or schools [27–28] in the US.
A limitation to this study is the design. As it was a pretest- posttest design with the posttest administered immediately after the lesson, it was not possible to measure long-term or sustained changes in knowledge. Participants could have retained information only over the short term, but may not have experienced a change in long-term knowledge. Additionally, we did not assess a change in screening behavior following the intervention, although plans to measure screening rates among women who received the educational lesson are currently being developed. Although there was no control group, each participant acted as her own control by taking the pretest. Despite this limitation in study design, given that our approach was a pilot study that used a new technology for this population, the design was appropriate for this study.
Our study is likely generalizable to other populations outside of the villages we sampled. The content of the intervention is likely generalizable to Malawi and other areas in Sub-Saharan Africa, with appropriate translation of content into local languages, addition of local misconceptions, and pretesting for cultural appropriateness.
CONCLUSIONS
We found that tablet-based interventions can be useful education modalities in low resource settings, such as rural Malawi. This intervention was effective, feasible, and acceptable as a method cervical cancer education. Further utilization of tablet-based education in low-resource settings is warranted for both cervical cancer education and other health topics.
Acknowledgements
The authors thank Annie-Laurie McRee for her support of this project. We also thank Jeff Rogers and the staff of Child Legacy International, particularly Gladson Mopiwa, Joana Banda, Venson Banda, Lydia Nkhoma, Mike Msesa, Jonathan Kandodo, and Patrick Nampandeni.
Funding:
This work was supported in part by the OSU College of Medicine Bennett Research Scholarship (MC) and the Ohio State Critical Difference for Women Scholarship (MC). Support for this project was also provided by the Ohio State University Institute for Population Research through a grant from the Eunice Kennedy Shriver National Institute for Child Health and Human Development of the National Institutes of Health, P2CHD058484. The content is solely the responsibility of the authors and does not necessarily represent the official view of the Eunice Kennedy Shriver National Institute for Child Health and Human Development or the National Institutes of Health.
Footnotes
Author Disclosure Statement:
No competing financial interests exist.
References
- 1.World Health Organization (WHO) Geneva: WHO; 2000. Cervical Cancer Screening in Developing Countries. [Google Scholar]
- 2.Africa Coalition on Maternal Newborn and Child Health. 2014 Africa Cervical Cancer Multi Indicator Incidence and Mortality Scorecard. [accessed 17 November 2015];2014 Available from: http://www.who.int/pmnch/media/events/2014/africa_cancer_mortality.pdf.
- 3.Bruni L, Barrionuevo-Rosas L, Albero G, et al. ICO Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in Malawi. [accessed 17 November 2015];Summary Report 2015-03-20. 2015 Available from: http://www.hpvcentre.net/statistics/reports/MWI.pdf. [Google Scholar]
- 4.Msyamboza KP, Manda G, Tembo B, et al. Cancer survival in Malawi: a retrospective cohort study. Pan Afr Med J. 2014;19:234. doi: 10.11604/pamj.2014.19.234.4675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fort VK, Makin MS, Siegler AJ, Ault K, Rochat R. Barriers to cervical cancer screening in Mulanje, Malawi: a qualitative study. Patient Prefer Adherence. 2011;5:125–131. doi: 10.2147/PPA.S17317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chadza E, Chirwa E, Maluwa A, Malata A, Kazembe A, Chimwaza A. Factors that contribute to delay in seeking cervical cancer diagnosis and treatment among women in Malawi. Health. 2012;4(11):1015–1022. [Google Scholar]
- 7.Paz-Soldan VA, Bisika T, DeGraft-Johnson J, Tsui AO. Community, social group, and individual level correlates of rural Malawian men's and women's reproductive health intentions and practices. Afr J Reprod Health. 2012;16(3):57–67. [PMC free article] [PubMed] [Google Scholar]
- 8.Sridhar A, Chen A, Forbes ER, Glik D. Mobile application for information on reversible contraception: a randomized controlled trial. Am J Obstet Gynecol. 2015;212(6):774.e1–774.e7. doi: 10.1016/j.ajog.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 9.Heisler M, Choi H, Palmisano G, et al. Comparison of community health worker-led diabetes medication decision-making support for low income Latino and African American adults with diabetes using e-health tools versus print materials: a randomized, controlled trial. Ann Intern Med. 2014;161(10 Suppl):S13–S22. doi: 10.7326/M13-3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sultan DH, Rivers BM, Osongo BO, et al. Affecting African American Men’s Prostate Cancer Screening Decision-making through a Mobile Tablet-Mediated Intervention. J Health Care Poor Underserved. 2014;25(3):1262–1277. doi: 10.1353/hpu.2014.0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schooley B, San Nicolas-Rocca T, Burkhard R. Patient-Provider Communications in Outpatient Clinic Settings: A Clinic-Based Evaluation of Mobile Device and Multimedia Mediated Communications for Patient Education. JMIR mHealth uHealth. 2015;3(1):e2. doi: 10.2196/mhealth.3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hall CS, Fottrell E, Wilkinson S, Byass P. Assessing the impact of mHealth interventions in low- and middle-income countries – what has been shown to work? Glob Health Action. 2014;7:25606. doi: 10.3402/gha.v7.25606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perkins JM, Subramanian SV, Christakis NA. Social networks and health: A systematic review of sociocentric network studies in low- and middle-income countries. Soc Sci Med. 2015;125:70–78. doi: 10.1016/j.socscimed.2014.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lyimo FS, Beran TN. Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: three public policy implications. BMC Public Health. 2012;12:22. doi: 10.1186/1471-2458-12-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vaisy A, Lotfinejad S, Zhian F. Risk of cancer with combined oral contraceptive use among Iranian women. Asian Pac J Cancer Prev. 2014;15(14):5517–5522. doi: 10.7314/apjcp.2014.15.14.5517. [DOI] [PubMed] [Google Scholar]
- 16.Westreich D, Jamal N, Smith SJ, et al. Injectable and oral contraception and the incidence and progression of cervical disease in HIV-infected women in South Africa. Contraception. 2014;89(4):286–291. doi: 10.1016/j.contraception.2013.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vessey M, Yeates D. Oral contraceptive use and cancer: final report from the Oxford-Family Planning Association contraceptive study. Contraception. 2013;88(6):678–683. doi: 10.1016/j.contraception.2013.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Johnson HM, Seifert CM. Sources of the continued influence effect: When discredited information in memory affects later inferences. J Exp Psychol Learn Mem Cogn. 1994;20(6):1420–1436. [Google Scholar]
- 19.World Health Organization (WHO) A demonstration project in six African countries: Malawi, Madagascar, Nigeria, Uganda, the United Republic of Tanzania, and Zambia. Geneva: WHO; 2012. Prevention of cervical cancer through screening using visual inspection with acetic acid (VIA) and treatment with cryotherapy. [Google Scholar]
- 20.Heideman WH, deWit M, Middelkoop BJ, et al. Diabetes risk reduction in overweight first degree relatives of type 2 diabetes patients: Effects of a low-intensive lifestyle education program (DiAlert) A randomized controlled trial. Patient Educ Couns. 2015;98(4):476–483. doi: 10.1016/j.pec.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 21.Schnall R, Travers J, Rojas M, Carballo-Dieguez A. eHealth interventions for HIV prevention in high-risk men who have sex with men: a systematic review. J Med Internet Res. 2014;16(5):e134. doi: 10.2196/jmir.3393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al Hayek AA, Robert AA, Al Dawish MA, Zamzami MM, Sam AE, Alzaid AA. Impact of an education program on patient anxiety, depression, glycemic control, and adherence to self-care medication in Type 2 diabetes. J Family Community Med. 2013;20(2):77–82. doi: 10.4103/2230-8229.114766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Akinfaderin-Agarau F, Chirtau M, Ekponimo S, Power S. Opportunities and limitations for using new media and mobile phones to expand access to sexual and reproductive health information and services for adolescent girls and young women in six Nigerian states. Afr J Reprod Health. 2012;16(2):219–230. [PubMed] [Google Scholar]
- 24.Bull S. Technology-based health promotion. Los Angeles, CA: SAGE Publications; 2011. [Google Scholar]
- 25.Logsdon MC, Davis D, Eckert D, et al. Feasibility of Two Educational Methods for Teaching New Mothers: A Pilot Study. Interact J Med Res. 2015;4(4):e20. doi: 10.2196/ijmr.4583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tait AR, Voepel-Lewis T, Chetcuti SJ, Brennan-Martinez C, Levine R. Enhancing patient understanding of medical procedures: evaluation of an interactive multimedia program with in-line exercises. Int J Med Inform. 2014;83(5):376–384. doi: 10.1016/j.ijmedinf.2014.01.011. Epub 2014 Feb 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Struempler BJ, Parmer SM, Mastropietro LM, Arsiwalla D, Bubb RR. Changes in fruit and vegetable consumption of third-grade students in body quest: food of the warrior, a 17-class childhood obesity prevention program. J Nutr Educ Behav. 2014;46(4):286–292. doi: 10.1016/j.jneb.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 28.Berninger VW, Nagy W, Tanimoto S, Thompson R, Abbott RD. Computer Instruction in Handwriting, Spelling, and Composing for Students with Specific Learning Disabilities in Grades 4 to 9. Comput Educ. 2015;81:154–168. doi: 10.1016/j.compedu.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]