Abstract
Background:
The application of second-generation constrained condylar knee (CCK) prostheses has not been widely studied. This retrospective study was carried out to evaluate the clinical and radiographic outcomes of a second-generation CCK prosthesis for complex primary or revision total knee arthroplasty (TKA).
Methods:
In total, 51 consecutive TKAs (47 patients) were performed between June 2003 and June 2013 using second-generation modular CCK prostheses. The follow-up was conducted at 3rd day, 1st, 6th, and 12th months postoperatively and later annually. Anteroposterior (AP), lateral, skyline, and long-standing AP radiographs of the affected knees were taken. The Hospital for Special Surgery (HSS) Knee Score, the Knee Society Knee Score (KSKS), the Knee Society Function Score (KSFS), and range of motion (ROM) were also recorded. Heteroscedastic two-tailed Student's t-tests were used to compare the HSS score and the Knee Society score between primary and revision TKAs. A value of P < 0.05 was considered statistically significant.
Results:
Four knees (two patients) were lost to follow-up, and 47 knees (31 primary TKAs and 16 revision TKAs) had a mean follow-up time of 5.5 years. The mean HSS score improved from 51.1 ± 15.0 preoperatively to 85.3 ± 8.4 points at the final follow-up (P < 0.05). Similar results were observed in terms of the KSKS and KSFS, which improved from 26.0 ± 13.0 to 80.0 ± 12.2 and from 40.0 ± 15.0 to 85.0 ± 9.3 points, respectively (P < 0.05). No significant difference in the HSS, KSKS, KSFS, or ROM was found between primary and revision TKAs (P > 0.05). Two complications were observed in the revision TKA group (one intraoperative distal femur fracture and one recurrence of infection) while one complication (infection) was observed in the primary TKA group. No prosthesis loosening, joint dislocation, patella problems, tibial fracture, or nerve injury were observed. Radiolucent lines were observed in 4% of the knees without progressive osteolysis.
Conclusions:
Second-generation modular CCK prostheses are a safe and practical treatment for both primary and revision knees that cannot be balanced. However, further studies focusing on different types of constrained prostheses are required to validate these results.
Keywords: Clinical Effectiveness, Constrained Condylar, Total Knee Arthroplasty
INTRODUCTION
Complex primary total knee arthroplasty (TKA) and revision TKA are associated with high incidence of complications including severe loss of host bone stock quantity and quality, ligamentous instability, and extensor mechanism failure or malalignment, which continue to present numerous challenges for surgeons.[1,2,3,4] Constrained condylar knee (CCK) prostheses are designed to manage these challenges.
So far, two generations of CCK prostheses are designed. Although the first-generation CCK prostheses have proven to be successful in managing some of the challenges of complex primary TKA and revision TKA including soft tissue instability and bone deficiency, previous studies have reported that first-generation CCK prostheses are associated with a high rate of aseptic loosening.[4,5,6,7,8,9] In addition, patella tracking is also problematic in these prostheses.[10] Lachiewicz and Soileau[11] performed 44 TKAs using first-generation CCK prostheses and reported that patella complications (fracture or osteonecrosis) were observed in 16.6% of knees.
The second-generation CCK prosthesis (LCCK, NexGen®, USA) is developed as a modular, non-hinged, and semi-constrained implant. It has a redesigned, deepened femoral notch and a relatively higher and broader tibial insert spine, which provides better medial-lateral stability (allowing 3° of varus-valgus tilt and 5° of internal-external rotation) than that of first-generation CCKs. Furthermore, it is developed with modular femoral and tibial stems, which allows the option of press fit fixation.[11] However, to the best of our knowledge, only a few studies of second-generation CCK prostheses have been published, with a limited number of patients and relatively short follow-up.[11,12] There is also lack of studies comparing the outcomes between primary TKA and revision TKA using second-generation CCK prostheses. This retrospective study was conducted to evaluate the clinical and radiographic outcomes of second-generation CCK prosthesis for complex primary and revision TKAs.
METHODS
Materials
This study was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University, School of Medicine. Written informed consents were obtained from all patients. In total, 51 consecutive TKAs (35 were primary TKA [primary group] and 16 revision TKA [revision group]) were performed by the same surgeon (Rong-Xin He) between June 2003 and June 2013 using a second-generation modular CCK prosthesis. The indications for implanting a CCK prosthesis were similar to those described by Insall,[13] Donaldson et al.,[6] and Sculco:[9,14] medial collateral ligament insufficiency, severe bone loss, and severe valgus deformity.
Two patients (four knees) died after a <2-year follow-up. The remaining 45 patients (47 knees) comprised 32 females and 15 males with an average age of 65.4 years (range, 43–87 years). Thirty-five (68.6%) were primary TKAs and 16 (31.4%) were revision TKAs. In primary TKA group, severe varus deformity with an average angle of 24.4° ± 4.6° was observed in nine knees. In revision group, severe varus deformity with an average angle of 23.8° ± 4.8° was observed in four knees. Ten knees with an average angle of 25.0° ± 6.7° in primary TKA group were considered to have severe valgus deformity while no cases of severe valgus deformity were observed in revision TKA group. Ten of the revision surgeries were due to aseptic loosening while the remaining six were due to infection [Table 1].
Table 1.
Demographic data for patients underwent primary and revision TKAs with second-generation modular CCK prostheses
| Items | Primary TKA (n = 31) | Revision TKA (n = 16) |
|---|---|---|
| Patients (knees) | 29 (31) | 16 (16) |
| Age (years), mean ± SD | 64 ± 12 | 67 ± 8 |
| Follow-up (months), mean ± SD | 68.6 ± 21.8 | 61.1 ± 21.7 |
| Male/female, n | 9/22 | 6/10 |
| Severe varus deformity, n | 9 | 4 |
| Severe valgus deformity, n | 10 | 0 |
TKA: Total knee arthroplasty; SD: Standard deviation; CCK: Constrained condylar knee.
Operative procedures
Primary total knee arthroplasties
All primary TKAs were performed via a standard-length midline skin incision and a modified medial parapatellar approach.[13] Before and after bone resection, the ligament-balancing techniques described by Insall et al.[15] were applied to determine the use of CCK prosthesis components. The second-generation CCK prosthesis was only implanted if intraoperative stability could not be obtained with a posterior-stabilized (PS) prosthesis. Ligament and retinacular release of the patella, as described by Insall,[13] were performed for patients with severe valgus or varus deformity. Uncemented 100-mm tibial and femoral stem extensions were routinely used for additional fixation. Patella resurfacing with an all-polyethylene component was performed if the articular surface of the patella was severely damaged.
Revision total knee arthroplasties
Of the 16 revision TKAs, ten were due to aseptic loosening and involved procedures similar to those in the primary TKAs as described above. A longitudinal midline skin incision was carefully created without overlapping the previous incision. The other six revision TKAs were due to periprosthetic infection, and the two-stage revisions were performed. The bone defects were completely excavated or exposed, and bone allograft or tibial augment implants were used to manage the large segmental defects. After pulse lavage irrigation of the remaining cut bone surfaces, the condylar prosthesis was implanted. Uncemented 100-mm tibial and femoral stem extensions were routinely used.
Routine closure was performed over a closed-suction drain, which was removed 24 h postoperatively. To reduce postoperative hemorrhage, tranexamic acid was injected into the wound immediately after closure and a bulky compression dressing was applied. Rehabilitation using a continuous passive-motion machine and formal physical therapy was performed 24 h postoperatively. All patients were administered cefuroxime at a dose of 1.5 g twice a day for postoperative periprosthetic infection prophylaxis. Rivaroxaban was applied at a dose of 10 mg/d for venous thromboembolism prophylaxis. Duplex ultrasonography was routinely performed before discharge.[16]
Follow-up
The patients, knees, and radiographs were evaluated preoperatively at 3rd day, 1st, 6th, and 12th months after the operation, and annually thereafter at the outpatient department of our hospital. The Hospital for Special Surgery (HSS) Knee Score and the Knee Society Score (KSS) were recorded. The clinical results were rated as excellent (≥85 points), good (70–84 points), fair (60–69 points), or poor (< points) according to the HSS scoring system. Anteroposterior (AP), lateral, skyline, and long-standing AP radiographs were evaluated for axial alignment, radiolucent lines, and bone-graft incorporation using the Knee Society Scoring System.[17] The patellofemoral axial position was evaluated using the method described by Bindelglass and Vince.[18]
Statistical methods
The SPSS version 18.0 statistical software package (IBM Corp., Armonk, NY, USA) was used for the statistical analysis. Data are presented as mean ± standard deviation (SD). The preoperative and postoperative HSS scores, KSS, and range of motion (ROM) were analyzed using paired t-tests. Heteroscedastic two-tailed Student's t-tests were used to compare the HSS score and KSS between primary and revision TKAs. A value of P < 0.05 was considered statistically significant.
RESULTS
In total, 47 knees (45 patients) underwent follow-up for 2–12 years (mean, 5.5 years), and complete clinical and radiographic results were recorded. Bone allografts were applied in three primary TKAs and two revision TKAs while tibial augment implants were applied in five primary TKAs and four revision TKAs to manage bone defects [Figures 1 and 2].
Figure 1.
(a) A female aged 70 years underwent a revision TKA due to aseptic loosening: (a1) The preoperative radiographic view showed aseptic loosening of the tibial component; (a2) The postoperative view showed that a tibial augment implant was applied to manage the severe bone loss. (b) A male aged 78 years underwent a primary TKA due to severe posttraumatic bone loss: (b1) The preoperative radiographic view showed severe bone loss; (b2) The postoperative view showed that a second-generation CCK prosthesis was applied to manage the severe bone loss. TKA: Total knee arthroplasty; CCK: Constrained condylar knee.
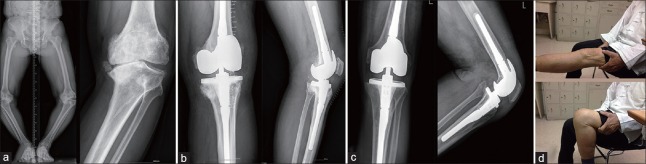
Figure 2.
A male aged 78 years underwent a primary TKA due to severe varus deformity. (a) AP and lateral views of the left knee preoperatively. (b) AP and lateral views of the left knee postoperatively. (c) AP and lateral views of the left knee at the last follow-up. (d) Range of motion in the left knee at the last follow-up. AP: Anteroposterior; TKA: Total knee arthroplasty.
Clinical results
The mean HSS scores improved from 51.1 ± 15.0 points preoperatively to 85.3 ± 8.4 points at the final follow-up (P < 0.05). Similar results were observed in terms of the Knee Society Knee Score (KSKS) and the Knee Society Function Score (KSFS), which improved from 26.0 ± 13.0 to 80.0 ± 12.2 points and from 40.00 ± 14.96 to 85.00 ± 9.27 points, respectively (P < 0.05). The average ROM improved from 81.4° ± 15.2° to 90.9° ± 15.9° (P < 0.05). No significant difference in the HSS score, KSKS, KSFS, or ROM was found between primary and revision TKAs (P > 0.05) [Table 2]. Using the HSS scoring system, 29 (62%) knees had an excellent result, 14 (30%) had a good result, 2 (4%) had a fair result, and 2 (4%) had a poor result. Overall, 43 knees (92%) had good or excellent results. No knees exhibited varus-valgus instability in flexion or extension.
Table 2.
Function parameters preoperatively and at the last follow-up for patients underwent primary and revision TKAs (mean ± SD)
| Parameter | Primary TKA (n = 31) | Revision TKA (n = 16) | t | P |
|---|---|---|---|---|
| Range of motion (°) | ||||
| Preoperative | 78.4 ± 15.2 | 87.1 ± 13.9 | −1.96 | 0.74 |
| Last follow-up | 89.9 ± 15.8 | 92.8 ± 16.5 | −0.57 | 0.66 |
| HSS score | ||||
| Preoperative | 47.4 ± 15.5 | 58.1 ± 11.3 | −2.44 | 0.13 |
| Last follow-up | 84.6 ± 9.6 | 86.9 ± 5.4 | −1.06 | 0.06 |
| Knee Society Knee Score | ||||
| Preoperative | 27.3 ± 14.3 | 23.6 ± 10.1 | 1.01 | 0.22 |
| Last follow-up | 79.3 ± 13.9 | 81.4 ± 8.3 | −0.64 | 0.08 |
| Knee Society Function Score | ||||
| Preoperative | 39.8 ± 16.1 | 40.3 ± 13.1 | −0.11 | 0.24 |
| Last follow-up | 84.5 ± 10.8 | 85.9 ± 5.2 | −0.61 | 0.28 |
TKA: Total knee arthroplasty; SD: Standard deviation; HSS: Hospital for Special Surgery.
Radiographic results
A radiographic review of the components showed no radiolucent lines in 45 knees, and two knees (4%, one femur and one tibia component) had at least 1 mm of radiolucency in a single zone in one component. The radiolucency of the tibia was localized to the medial tibial plateau, and the femoral radiolucency was localized to the anterior femoral condyle. None of the surviving knees showed evidence of radiolucent lines in the patellar component, and neither complete bone-cement radiolucency nor progressive radiolucency was observed. Using the method described by Bindelglass and Vince,[18] no patella was noted to have >5° of tilt on tangential radiographs.
Thirteen knees with massive bone loss of the distal femur or proximal tibia were reconstructed with tibial augment implants or a bulk structural allograft. All cortical bone grafts appeared to be radiographically united to the host bone. None of these knees showed evidence of graft subsidence or bone cement radiolucency.
Complications
Two complications were observed in revision TKA group (one intraoperative distal femur fracture and one recurrence of infection) while one complication was observed in primary TKA group (infection). None of the patients experienced complications relating to prosthesis loosening, joint dislocation, patella problems, tibial postfracture, or nerve injury.
Three patients (3 knees) developed complications. The first patient was a 46-year-old woman in revision TKA group, who was left with severe bone loss and developed a longitudinal bone fracture at the distal end of the femur when the femoral component was inserted. The fracture was reduced intraoperatively and fixed with cerclage. Eight months postoperatively, the fracture had healed with good alignment and positioning. The second patient was a 78-year-old woman who had previously undergone right legacy CCK arthroplasty for osteoarthritis with severe valgus deformity. She developed a Staphylococcus aureus infection two-years postoperatively. The initial prosthesis was removed, and a vancomycin-loaded cement spacer was implanted. After a 6-week courseof intravenous vancomycin, a knee culture was negative. Four months after the initial removal of the prosthesis, the patient underwent revision surgery by the same surgeon, using a LCCK prosthesis, and finally the infection was controlled. The third patient was a 66-year-old woman who developed recurrence of an infection 4 years postoperatively. She was treated with the same method described above by the same surgeon. Until the final follow-up, no recurrence of infection was observed. No other revision or reoperation were performed.
DISCUSSION
It is unusual to require the use of a prosthesis with more constraints than the PS prosthesis in most primary and revision TKAs. However, a CCK prosthesis is required for certain indications,[19] including medial collateral insufficiency, severe bone loss, and severe valgus deformity as described by Insall et al.,[19] and Donaldson et al.[6]
Few studies have described the results of second-generation CCK prosthesis components. The high failure rates of complex primary and revision TKAs prompted a review of our experience of using CCK prosthesis.[3,4,20,21] In this series of 31 primary and 16 revision TKAs using legacy CCK prosthesis, 47 knees underwent complete clinical and radiographic follow-up over a mean of 5.5 years.
Our study with 5.5-year follow-up showed that 92% of knees had good or excellent results with a CCK prosthesis, which compared favorably with previously reported studies.[4,7,10,11] Hartford et al.[4] investigated 33 TKAs (17 primary TKAs and 16 revision TKAs) using two generations of CCKs and reported that 82% had excellent or good clinical results. In their study, three failures (one recurrence of infection and two aseptic loosenings) of the entire series of 33 knees were reported in revision TKA group during the mean 5-year follow-up. Before the present study, the latest series of CCK arthroplasties was reported by Lachiewicz and Soileau.[11] Of 27 primary modular CCK arthroplasties with a mean follow-up time of 5.4 years, 12 (44%) knees were rated as excellent, 14 (52%) as good, and 1 (4%) as fair. However, the outcome with a longer follow-up than 5.5 years is still unclear and further studies with long-term follow-up are still needed.
Patella resurfacing was not routinely performed in this study. Although no ruptured patellar tendon or dislocation was discovered, previous authors have emphasized the relationship between a high rate of complications and extensor mechanism problems in revision TKA.[14,22] Stuart et al.[23] reported that an extensor mechanism problem was responsible for 41% of the 60 failures that required reoperation and highlighted the importance of patellar tracking and preservation of the patellar and quadriceps tendon insertions during revision TKA.
Eight knees (25.80%) in primary TKA group and five knees (31.25%) in revision TKA group with massive bone loss required reconstruction with bone grafts or tibial augment implants. These included 3 (9.7%) bone grafts and 5 (16.0%) tibial augment implants in primary TKA group and 2 (12.5%) bone grafts and four (25.0%) tibial augment implants in revision TKA group. Our radiographic results compared favorably with those reported by Wilde et al.,[24] supporting the use of allograft-prosthesis composites to manage massive bone loss in the proximal tibial or distal femur.
There is still controversy regarding whether to manage complex knees using a rotating-hinged knee (RHK) prosthesis or the CCK prosthesis. The RHK prosthesis is reportedly superior to the CCK prosthesis for patients with a severe deformity or instability that cannot be managed with a CCK prosthesis, especially for patients with neuromuscular deficits such as post-polio arthritis.[25] However, the RHK prosthesis is associated with a high incidence of complications and poor results over a long follow-up duration,[26,27] including infection, persistent pain, aseptic loosening, and metallic synovitis.[21,28,29] In this study, all cases were managed with CCK prostheses, and despite two cases of recurrent infection, none of the complications mentioned above were observed. Our study might indicate that for patients whose knee balance could not be gained using the PS prosthesis, a second-generation CCK prosthesis should be initially considered.
The application of femoral stems in primary TKA is also controversial. Some studies showed no benefit from the application of stem extensions[21] while others strongly recommended them.[12,30] In this study, 100-mm uncemented femoral and tibial stem extensions were routinely used in all 47 knees to provide better fixation and help protect against the occurrence of a periprosthetic fracture. At the end of the follow-up, no prosthesis loosening was observed. Together with the results of the previous studies, we recommend that a stem extension should be routinely applied for CCK arthroplasty.
We acknowledged that there were several important limitations to our study. This was a retrospective study with a relatively small group of knees, rather than a large-sample randomized controlled trial, and this decreases the robustness of the conclusions. The follow-up time (mean, 5.5 years; range, 2–12 years) was relatively short, and the results might change with a longer follow-up. In addition, we had a limited ability to assess clinical differences using different types of constrained prostheses because of the lack of available cases. Nevertheless, we compared the clinical application of a second-generation CCK prosthesis in both complex primary and revision TKAs, which might provide useful insight into the clinical efficacy of this prosthesis.
In conclusion, second-generation modular CCK prostheses are a safe and practical treatment for both primary and revision knees that cannot be balanced. It is important to realize that the results reported in this study might be design-specific; therefore, further studies focusing on different types of constrained prostheses are required to validate these results.
Financial support and sponsorship
This work was supported by the grant from the National Natural Science Foundation of China (No. 81572124).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Ning-Ning Wang
REFERENCES
- 1.Naudie DD, Rorabeck TC. Managing instability in total knee arthroplasty with constrained and linked implants. Instr Course Lect. 2004;53:207–15. [PubMed] [Google Scholar]
- 2.Zhou X, Wang M, Liu C, Zhang L, Zhou Y. Total knee arthroplasty for severe valgus knee deformity. Chin Med J. 2014;127:1062–6. doi:10.3760/cma.j.issn.0366-6999.20132488. [PubMed] [Google Scholar]
- 3.Vince KG, Long W. Revision knee arthroplasty. The limits of press fit medullary fixation. Clin Orthop Relat Res. 1995;317:172–7. [PubMed] [Google Scholar]
- 4.Hartford JM, Goodman SB, Schurman DJ, Knoblick G. Complex primary and revision total knee arthroplasty using the condylar constrained prosthesis: An average 5-year follow-up. J Arthroplasty. 1998;13:380–7. doi: 10.1016/s0883-5403(98)90002-x. doi:10.1016/S0883-5403(98)90002-X. [DOI] [PubMed] [Google Scholar]
- 5.Chotivichit AL, Cracchiolo A, 3rd, Chow GH, Dorey F. Total knee arthroplasty using the total condylar III knee prosthesis. J Arthroplasty. 1991;6:341–50. doi: 10.1016/s0883-5403(06)80186-5. doi:10.1016/S0883-5403(06)80186-5. [DOI] [PubMed] [Google Scholar]
- 6.Donaldson WF, 3rd, Sculco TP, Insall JN, Ranawat TC. Total condylar III knee prosthesis. Long-term follow-up study. Clin Orthop Relat Res. 1988;226:21–8. [PubMed] [Google Scholar]
- 7.Easley ME, Insall JN, Scuderi GR, Bullek TC. Primary constrained condylar knee arthroplasty for the arthritic valgus knee. Clin Orthop Relat Res. 2000;380:58–64. doi: 10.1097/00003086-200011000-00008. doi:10.1097/00003086-200011000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Kavolus CH, Faris PM, Ritter MA, Keating TC. The total condylar III knee prosthesis in elderly patients. J Arthroplasty. 1991;6:39–43. doi: 10.1016/s0883-5403(06)80155-5. doi:10.1016/S0883-5403(06)80155-5. [DOI] [PubMed] [Google Scholar]
- 9.Lachiewicz PF, Falatyn TC. Clinical and radiographic results of the Total Condylar III and Constrained Condylar total knee arthroplasty. J Arthroplasty. 1996;11:916–22. doi: 10.1016/s0883-5403(96)80132-x. doi:10.1016/S0883-5403(96)80132-X. [DOI] [PubMed] [Google Scholar]
- 10.Lachiewicz PF, Soileau TC. Ten-year survival and clinical results of constrained components in primary total knee arthroplasty. J Arthroplasty. 2006;21:803–8. doi: 10.1016/j.arth.2005.09.008. doi:10.1016/j.arth.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 11.Lachiewicz PF, Soileau TC. Results of a second-generation constrained condylar prosthesis in primary total knee arthroplasty. J Arthroplasty. 2011;26:1228–31. doi: 10.1016/j.arth.2011.05.010. doi:10.1016/j.arth.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 12.Anderson JA, Baldini A, MacDonald JH, Tomek I, Pellicci PM, Sculco TC. Constrained condylar knee without stem extensions for difficult primary total knee arthroplasty. J Knee Surg. 2007;20:195–8. doi: 10.1055/s-0030-1248042. [DOI] [PubMed] [Google Scholar]
- 13.Insall J. A midline approach to the knee. J Bone Joint Surg Am. 1971;53:1584–6. [PubMed] [Google Scholar]
- 14.Sculco TP. Total condylar III prosthesis in ligament instability. Orthop Clin North Am. 1989;20:221–6. [PubMed] [Google Scholar]
- 15.Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg Am. 1979;61:173–80. [PubMed] [Google Scholar]
- 16.Lachiewicz PF, Kelley SS, Haden TC. Two mechanical devices for prophylaxis of thromboembolism after total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br. 2004;86:1137–41. doi: 10.1302/0301-620x.86b8.15438. doi:10.1302/0301-620X.86B8.15438. [DOI] [PubMed] [Google Scholar]
- 17.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 18.Bindelglass DF, Vince TC. Patellar tilt and subluxation following subvastus and parapatellar approach in total knee arthroplasty. Implication for surgical technique. J Arthroplasty. 1996;11:507–11. doi: 10.1016/s0883-5403(96)80101-x. doi:10.1016/S0883-5403(96)80101-X. [DOI] [PubMed] [Google Scholar]
- 19.Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–65. doi:10.1097/00003086-199910000-00002. [PubMed] [Google Scholar]
- 20.Ahlberg A, Lundén A. Secondary operations after knee joint replacement. Clin Orthop Relat Res. 1981;156:170–4. doi:10.1097/00003086-198105000-00022. [PubMed] [Google Scholar]
- 21.Goldberg VM, Figgie MP, Figgie HE, 3rd, Sobel M. The results of revision total knee arthroplasty. Clin Orthop Relat Res. 1988;226:86–92. doi:10.1097/00003086-198801000-00013. [PubMed] [Google Scholar]
- 22.Rand JA, Bryan TC. Results of revision total knee arthroplasties using condylar prostheses. A review of fifty knees. J Bone Joint Surg Am. 1988;70:738–45. [PubMed] [Google Scholar]
- 23.Stuart MJ, Larson JE, Morrey TC. Reoperation after condylar revision total knee arthroplasty. Clin Orthop Relat Res. 1993;286:168–73. doi p00003086-199301000-00025. [PubMed] [Google Scholar]
- 24.Wilde AH, Schickendantz MS, Stulberg BN, Go TC. The incorporation of tibial allografts in total knee arthroplasty. J Bone Joint Surg Am. 1990;72:815–24. [PubMed] [Google Scholar]
- 25.Morgan H, Battista V, Leopold SS. Constraint in primary total knee arthroplasty. J Am Acad Orthop Surg. 2005;13:515–24. doi: 10.5435/00124635-200512000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Inglis AE, Walker TC. Revision of failed knee replacements using fixed-axis hinges. J Bone Joint Surg Br. 1991;73:757–61. doi: 10.1302/0301-620X.73B5.1894661. [DOI] [PubMed] [Google Scholar]
- 27.Karpinski MR, Grimer TC. Hinged knee replacement in revision arthroplasty. Clin Orthop Relat Res. 1987;220:185–91. doi:10.1097/00003086-19∃000-00025. [PubMed] [Google Scholar]
- 28.Bargar WL, Cracchiolo A, 3rd, Amstutz TC. Results with the constrained total knee prosthesis in treating severely disabled patients and patients with failed total knee replacements. J Bone Joint Surg Am. 1980;62:504–12. doi:10.1016/j.knee.2003.12.007. [PubMed] [Google Scholar]
- 29.Utting MR, Newman TC. Customised hinged knee replacements as a salvage procedure for failed total knee arthroplasty. Knee. 2004;11:475–9. doi: 10.1016/j.knee.2003.12.007. doi:10.1016/j.knee.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 30.Anderson JA, Baldini A, MacDonald JH, Pellicci PM, Sculco TC. Primary constrained condylar knee arthroplasty without stem extensions for the valgus knee. Clin Orthop Relat Res. 2006;442:199–203. doi: 10.1097/01.blo.0000185675.99696.29. doi:10.1097/01.blo.0000185675.99696.29. [DOI] [PubMed] [Google Scholar]