Abstract
Objective
Postoperative vomiting (POV) is one of the most common problems following general anaesthesia, and many factors, either solely or in combination, may play a role in aetiology. Acupuncture is a technique that the World Health Organization has accepted as a complementary treatment. This study presents our experience with acupuncture for POV treatment in a study of paediatric tonsillectomy cases.
Methods
The study included ASA I–II patients (n=70) aged 2–14 years who underwent tonsillectomy and/or adenoidectomy under general anaesthesia. The patients were randomly divided into the following two groups: control and study group. In the study group, an acupuncture needle was intraoperatively applied to the P6 acupuncture point for 20 min. Antiemetics were not administered to either group because of the standard applications in the preoperative period. The patients were postoperatively evaluated by nurses who were unaware about the techniques used in either group.
Results
No statistically significant difference was determined between the groups with regard to age, sex, nature of the operation, duration of anaesthesia, duration of the operation, surgical method and ASA scores. A statistically significant difference was determined between the groups with respect to vomiting rates. The acupuncture group presented with 0.28-times fewer vomiting episodes than the control group.
Conclusion
The results of the study demonstrate that acupuncture has an apparent antiemetic efficacy in POV. Its routine use for POV may improve postoperative comfort and reduce drug use for prophylactic or therapeutic purposes.
Keywords: Acupuncture, postoperative vomiting, adenoidectomy, tonsillectomy
Introduction
Despite several preventative approaches and treatments, postoperative nausea and vomiting (PONV) still poses a significant source of postoperative discomfort (1, 2). Several contributing factors may be responsible for postoperative emesis, including age, type of surgery, anaesthetic agents, anxiety or pain level (1, 2). Tonsillectomy and/or adenoidectomy in the paediatric age group present a high percentage of PONV, accounting for 70% of cases (2–4). Different treatments or prophylaxis modalities have been suggested; however, currently, there is no universally accepted approach for reducing PONV incidence (5–7).
Acupuncture is an ancient technique has been used for medical purposes in China for 2000 years (1, 2). Following the approval of this technique by WHO as a complementary measure in treating some medical conditions, including PONV, many centres have utilised acupuncture in addition to standard medical approaches (5). In paediatric patients, acupuncture currently has a limited volume of practice in medical or surgical conditions (8). This study aimed to investigate the effect of acupuncture to relieve postoperative vomiting (POV) following tonsillectomy and/or adenoidectomy in a paediatric population.
Methods
This randomised and single-blind study was conducted in collaboration with the Otolaryngology and Anaesthesiology Clinics of our hospital. The study protocol was reviewed and approved by the Ankara Children’s Health and Diseases Haematology and Oncology Training and Research Hospital Ethical committee for Clinical Research. The study comprised 70 paediatric patients in the ASA I–II category (aged 2–14 years) who underwent tonsillectomy and/or adenoidectomy under general anaesthesia. Patients with previous antiemetic use, drug hypersensitivity, car sickness or history of gastroesophageal reflux were excluded from the study. A total of 70 patients were included: 35 subjects in each of the control and study groups. The main indications for removal of tonsils or/and adenoid tissue were recurrent (five or more attacks in the recent year) tonsillitis, upper airway obstruction findings whether or not accompanied by obstructive sleep apnoea and serous otitis media of three or more months of duration.
Tonsillectomy was performed by cold knife dissection or bipolar diathermy techniques. The classic curettage technique was employed for adenoidectomy. After randomization, subjects in both groups were pre-medicated with oral midazolam. They were admitted to the operating room 20 min after pre-medication. The patient’s age, sex, ASA, surgical technique, type of anaesthesia and duration of surgery were recorded. After ECG, pulse oximetry and non-invasive blood pressure monitoring, anaesthesia induction was initiated with a gas mixture of 8% sevoflurane, 50% O2 and 50% nitrous oxide to all patients. Maintenance dose was administered with 2%–3.5% sevoflurane. An intravenous fluid infusion of 3.33% dextrose and 0.3% sodium chloride (8–10 mL kg−1) was initiated via a 22-G cannula, and then, fentanyl citrate was administered. Before starting the surgery, tramadol hydrochloride was administered to all patients for postoperative analgesia.
Patients in the control group did not receive any antiemetic medication. For patients in the study group, a stainless steel acupuncture needle, measuring 0.25×0.25 mm, was inserted in the P6 acupuncture point (Nei Guan), which is 2-cm below the transverse crease of the wrist P7, between the palmaris longus and flexor carpi radialis tendons on the line connecting P3 and P7 for at least 20 min during the surgery by a certified anaesthesiologist (Figure 1).
Figure 1.
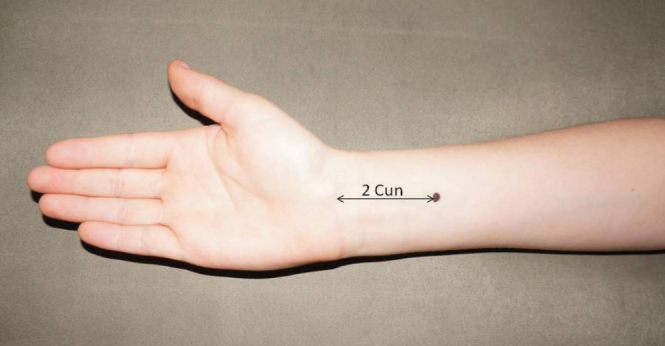
P6 (Nei Guan): 2-cm below the transverse crease of the wrist P7, between palmaris longus and flexor carpi radialis tendons, on the line connecting P3 and P7
All operations were performed by the same two-person surgical team. To prevent gastric distension, an orogastric catheter was inserted for aspiration of fluid and accumulated blood, and before airway reflexes returned, the catheter was removed. Patients with sufficient respiration were extubated.
All patients were postoperatively kept under close observation for 24 h by the ward nurses who were blinded to the applied technique. Thereafter, the patients were discharged when they met the discharge criteria. Because of the difficulty in understanding the expression and description of nausea in children, nausea was not considered. The incidents of vomiting were recorded in detail during the hospital stay. In refractory cases (three or more times of vomiting), ondansetron was administered to relieve symptoms.
Statistical analysis
Data were collected from patients who were operated in our otorhinolaryngology clinic. Type I error was set at 0.05, power was 80% and 20% lower expectation was expected for patients who underwent acupuncture compared with patients who received the standard treatment. The required sample size was calculated as 35 patients per group.
Data analysis was performed using Statistical Package for the Social Sciences version 11.5, (SPSS Inc; Chicago IL, USA). To compare differences between the control and study groups, for independent samples, t-test was used for continuous data with normal distribution, Mann–Whitney U test was used for continuous data with non-normal distributions or ordinal data and chi-square test or Fisher’s exact test was used for categorical data. Bivariate logistic regression analysis was used to investigate significant risk factors for vomiting.
For descriptive statistics, means±standard deviation was expressed for continuous data with a normal distribution, median and minimum–maximum values were expressed for continuous data with non-normal distribution and frequencies and percentages were provided for categorical data. A p value of <0.05 was accepted as statistically significant.
Results
There was no statistically significant difference between the groups in terms of age, sex, anaesthesia time, surgical procedure, surgery duration, type of surgical technique and ASA scores (Table 1). The POV rate was 22.9% in the study group and 51.4% in the control group. The POV rate difference between the groups was statistically significant (p<0.05). The possibility of POV incidences was 0.28-times lower in the study group than the control group (95% CI, 0.1–0.79; p<0.05) (Table 1).
Table 1.
Distribution of age, sex, weight, surgical procedure, anaesthesia and surgery duration, applied surgical techniques and ASA scores of all the patients
| Variables | Control group (n=35) | Study group (n=35) | p |
|---|---|---|---|
| Age* | 5.45±2.69 | 5.44±2.83 | 0.990 |
| Weight | 20.60±7.97 | 19.72±7.18 | 0.633 |
| Sex** | |||
| Female | 10 (28.6) | 15 (42.9) | 0.212 |
| Male | 25 (71.4) | 20 (57.1) | |
| Operation** | |||
| Adenoidectomy | 15 (42.9) | 15 (42.9) | 0.267 |
| Adenotonsillectomy | 9 (25.7) | 6 (17.1) | |
| Adenoidectomy+VT follow-up | 9 (25.7) | 7 (20) | |
| Adenotonsillectomy+ VT follow-up | 1 (2.9) | 6 (17.1) | |
| Adenotonsillectomy+ Paracentesis | 1 (2.9) | 0 (0) | |
| Tonsillectomy | 0 (0) | 1 (2.9) | |
| Anaesthesia duration* | 37.05±12.31 | 39.28±15.63 | 0.510 |
| Surgery duration* | 22.94±10.87 | 24.14±14.30 | 0.694 |
| ASA** | |||
| ASA I | 28 (80) | 28 (80) | 1.000 |
| ASA II | 7 (20) | 7 (20) | |
| Vomiting | |||
| Yes | 18 (51.4) | 8 (22.9) | 0.013† |
| No | 17 (48.6) | 27 (77.1) | |
mean±SD (Independent sample t-test)
Count (%) (Fisher’s exact test)
Odds ratio (95% CI): 0.28 (0.1–0.79)
There was no statistically significant differences between patients with and without POV in terms of age, sex, surgical procedure, type of anaesthesia, surgery duration, applied surgical technique and ASA scores (Table 2). Ondansetron was required for excessive nausea and vomiting in one patient in each group. Only these two refractory cases were determined.
Table 2.
Distribution of age, sex, surgical procedure, anaesthesia and surgery duration, applied surgical technique and ASA scores in vomiting and non-vomiting patients
| Vomiting | No (n=44) (62.9%) | Yes (n=26) (37.1%) | p |
|---|---|---|---|
| Age* | 5.13±2.70 | 5.99±2.83 | 0.206 |
| Sex** | |||
| Female | 19 (76) | 6 (24) | 0.090 |
| Male | 25 (55.6) | 20 (44.4) | |
| Operation** | |||
| Adenoidectomy | 20 (66.7) | 10 (33.3) | 0.426 |
| Adenotonsillectomy | 8 (53.3) | 7 (46.7) | |
| Adenoidectomy+VT follow-up | 9 (56.2) | 7 (43.8) | |
| Adenotonsillectomy+VT follow-up | 6 (85.7) | 1 (14.3) | |
| Adenotonsillectomy+ Paracentesis | 0 (0) | 1 (100) | |
| Tonsillectomy | 1 (100) | 0 (0) | |
| Anaesthesia duration* | 37.22±14.13 | 39.76±13.93 | 0.467 |
| Surgery duration* | 22.04±12.50 | 26.07±12.67 | 0.199 |
| ASA** | |||
| ASA I | 36 (64.3) | 20 (35.7) | 0.621 |
| ASA II | 8 (57.1) | 6 (42.9) | |
mean±SD (Independent sample t-test)
Count (%) (Fisher’s exact test)
The factor that affected the frequency of vomiting in postoperative nausea was determined to be acupuncture treatment.
Discussion
With many frequently performed surgeries in children, PONV is a quite common complaint, particularly in the early postoperative period (1, 2). According to Lerman et al. (9), in paediatric surgical cases over 3 years the risk of PONV is double that of the adult population. Some operations, including adenotonsillectomy, appear to increase the risk of PONV (1, 2). As reported by some studies, this risk may be as high as 70%–80% in adenotonsillectomy cases (1, 2, 4, 9, 10).
Nausea and vomiting may be caused by different factors such as postoperative opioid use, mechanical irritation of the throat or irritation of the pharyngoesophageal tract because of the swallowing of fluids containing blood during surgery (3, 9). PONV has a negative impact on patient comfort and postoperative complications, which may be attributed to surgical site irritation that is caused by regurgitated gastric fluids and/or increase of local pressure in the vascular bed. Therefore, proper and accurate handling and treatment strategies for PONV are still required (9, 10).
In this study, all the patients were pre-medicated with oral midazolam. In the literature, it has been demonstrated that a low dose of fentanyl citrate when added to sevoflurane during induction is useful in achieving haemodynamic stability and providing intubation comfort (11, 12). Therefore, in this study, fentanyl citrate (1 mcg kg−1) was added to 8% sevoflurane during induction. Previous studies have demonstrated that sevoflurane, N2O and intraoperative opioid use increased the incidence of PONV (13–16). The administration of midazolam and high concentration O2 has been reported to reduce the incidence of PONV (17, 18). As both groups in this study were administered with the same anaesthesia method, all cases were equal in terms of PONV risk factors. Therefore, the difference in the number of vomiting incidence between the groups could not be related to the anaesthetic technique or the agents used. Positive-pressure ventilation that was applied with a mask causes a predisposition to vomiting in the postoperative period (19). To avoid this effect, the accumulated air and blood in the stomach was aspirated with an orogastric catheter in both groups of this study. The catheter was removed before the airway reflexes returned to avoid nausea and vomiting that was caused by pharyngeal catheter irritation.
Despite the absence of a universally accepted protocol to treat the condition, ondansetron, dolasetron, dexamethasone, droperidol, dimenhydrinate and perphenazine are the main agents used in medical treatment, either alone or in combination (2, 10, 20–22). As an alternative approach, Dundee et al. (7, 23) first introduced acupuncture applications for PONV in 1986 and then in 1989. It was concluded that stimulating the P6 acupuncture point resulted in a reduction of vomiting incidences (7, 23). The National Institutes of Health stated in 1998 that the stimulation of the P6 point is effective in preventing nausea and vomiting that is caused by chemotherapeutic agents (5).
The antiemetic efficacy of acupuncture in surgical cases that were performed under general anaesthesia is a debatable subject. Yentis and Shenkman (24, 25) were unable to demonstrate a significant decrease in PONV rates in paediatric tonsillectomy cases with acupuncture application to the P6 point and concluded that this finding may be because of the effect of general anaesthesia. In contrast, Streitberger et al. (26) reported that the acupuncture application with the stimulation of the P6 point was quite effective under general anaesthesia. The irritation of needle insertion, which may be problematic in paediatric cases, also appears to be eliminated with general anaesthesia.
There have been several studies regarding acupuncture applications to relieve PONV in paediatric tonsillectomy and/or adenoidectomy cases with expectations of increased postoperative patient comfort and decreased antiemetic drug use (27). Schlager et al. (28) reported that the laser acupuncture technique was effective in paediatric ocular surgery cases (strabismus) as witnessed by a decrease in the PONV rate from 85% to 25%. Rusy et al. (29) also concluded that the PONV rate decreased from 93% to 63% with the electro-acupuncture technique. The acupressure technique has also been reported to decrease PONV rates from 66.2% to 46.8% and is more effective in female children under 3 years, who have a high risk for this condition (30). The results of this study are similar with these reports. In current literature, no earlier study could be found regarding the antiemetic effects of acupuncture in Turkey, where currently standard antiemetic medical treatment protocols are in use.
According to the meta-analysis of a research conducted by Bolton et al. (2) to analyse PONV incidences in children who underwent tonsillectomy, the odds ratio (OR) was calculated as 0.23, (95% CI, 0.16–0.33), 0.36 (95% CI, 0.29–0.46), 0.11 (95% CI, 0.06–0.19), 0.15 (95% CI, 0.06–0.35), 0.25 (95% CI, 0.1–0.59) and 0.51 (95% CI 0.34–0.77) for dexamethasone, ondansetron, serotonin antagonists granisetron, tropisetron, dolasetron and metoclopramide, respectively. The odds ratio (0.28; 95% CI, 0.1–0.79) in this study was similar to these findings, which demonstrates the effectiveness of this treatment modality.
In this study, no complications were encountered, which may be attributable to the acupuncture technique. In a previously reported series of a total of 99,442 acupuncture applications, the complication rate was found to be 0.13%–0.14% (31, 32). The most frequently reported complications were dislodgement of the needle, pain, vertigo, nausea and vomiting, bleeding, fever and contact dermatitis (32, 33). The P6 point specific complications were reported as needle dislodgement, pain, local irritation and median nerve injury (33). The complication rates for current standard antiemetic medical treatment have been reported as 0.5%–6% (33). The most important aspect of acupuncture application in the paediatric age group is adequate information for the parents and their cooperation daring the planned procedure. A positive attitude of the parents appears to increase the effectiveness of the treatment (34). In our study, no negative reactions from the parents were encountered. Following a detailed information procedure, all parents provided informed consent before the study.
Conclusion
This study supports the effectiveness of acupuncture against POV in paediatric tonsillectomy and/or adenoidectomy cases. Once the side effects and cost effectiveness of the current prophylactic agents have been considered, it appears that acupuncture can definitely contribute to the standard treatment protocols to prevent the unnecessary use of drugs for prophylactic or therapeutic measures. To the best of our knowledge, this is the first study in Turkey to evaluate the efficacy of the acupuncture method, which was found to decrease POV frequency in paediatric tonsillectomy and/or adenoidectomy cases, which have a higher rate of POV incidence compared with other surgical interventions.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Ankara Children’s Health and Diseases Hematology and Oncology Training and Research Hospital.
Informed Consent: Written informed consent was obtained from the parents of the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - S.Ö.; Design - S.Ö.; Supervision - S.Ö.; Resources - F.S.; Materials - N.S.; Data Collection and/or Processing - S.Ö., N.S., F.S., M.A., S.S., G.K., F.A., D.T.K.; Analysis and/or Interpretation - S.Ö., F.S.; Literature Search - S.Ö., F.S.; Writing Manuscript - S.Ö.; Critical Review - N.S., F.S.; Other - S.Ö.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Myles PS, Williams DL, Hendrata M, Anderson H, Weeks AM. Patient satisfaction after anaesthesia and surgery: results of a prospective survey of 10 811 patients. Br J Anaesth. 2000;84:6–10. doi: 10.1093/oxfordjournals.bja.a013383. http://dx.doi.org/10.1093/oxfordjournals.bja.a013383. [DOI] [PubMed] [Google Scholar]
- 2.Bolton CM, Myles PS, Nolan T, Sterne JA. Prophylaxis of postoperative vomiting in children undergoing tonsillectomy: a systematic review and meta-analysis. Br J Anaesth. 2006;97:593–604. doi: 10.1093/bja/ael256. http://dx.doi.org/10.1093/bja/ael256. [DOI] [PubMed] [Google Scholar]
- 3.Furst SR, Rodarte A. Prophylactic antiemetic treatment with ondansetron in children undergoing tonsillectomy. Anesthesiology. 1994;81:799–803. doi: 10.1097/00000542-199410000-00005. http://dx.doi.org/10.1097/00000542-199410000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Stanko D, Bergesio R, Davies K, Hegarty M, Von Ungern-Sternberg BS. Postoperative pain, nausea and vomiting following adeno-tonsillectomy: a long-term follow-up. Pediatric Anesthesia. 2013;23:690–6. doi: 10.1111/pan.12170. http://dx.doi.org/10.1111/pan.12170. [DOI] [PubMed] [Google Scholar]
- 5.NIH Consensus Conference. Acupuncture. JAMA. 1998;280:1518–24. http://dx.doi.org/10.1001/jama.280.17.1518. [PubMed] [Google Scholar]
- 6.Al-Sadi M, Newman B, Julious SA. Acupuncture in the prevention of postoperative nausea and vomiting. Anaesthesia. 1997;52:658–61. doi: 10.1111/j.1365-2044.1997.143-az0147.x. http://dx.doi.org/10.1111/j.1365-2044.1997.143-az0147.x. [DOI] [PubMed] [Google Scholar]
- 7.Dundee JW, Ghaly RG, Bill KM, Chestnutt WN, Fitzpatrick KTJ, Lynas AGA. Effect of stimulation of the P6 antiemetic point on postoperative nausea and vomiting. Br J Anaesth. 1989;63:612–8. doi: 10.1093/bja/63.5.612. http://dx.doi.org/10.1093/bja/63.5.612. [DOI] [PubMed] [Google Scholar]
- 8.Ayoglu H, Bayar U, Atik L, Ozer Y, Acar A, Turan IO. The Effects of Preoperative Acupuncture Needle and Capsicum Plaster Applications of Extra 1, Pericardium 6 and Large Intestine 4 Points on Preoperative Anxiety, Postoperative Nausea-Vomiting and Analgesic Consumption. Tur Klin J Med Sci. 2009;29:1063–70. [Google Scholar]
- 9.Lerman J. Surgical and patient factors involved in postoperative nausea and vomiting. Br J Anaesth. 1992;69:24–32. doi: 10.1093/bja/69.supplement_1.24s. http://dx.doi.org/10.1093/bja/69.supplement_1.24S. [DOI] [PubMed] [Google Scholar]
- 10.Gallagher TQ, Hill C, Ojha S, Ference E, Keamy DG, Williams M, et al. Perioperative dexamethasone administration and risk of bleeding following tonsillectomy in children: a randomized controlled trial. JAMA. 2012;308:1221–6. doi: 10.1001/2012.jama.11575. http://dx.doi.org/10.1001/2012.jama.11575. [DOI] [PubMed] [Google Scholar]
- 11.Gupta A, Kaur R, Malhotra R, Kale S. Comparative evaluation of different doses of propofol preceded by fentanyl on intubating conditions and pressor response during tracheal intubation without muscle relaxants. Paediatr Anaesth. 2006;16:399–405. doi: 10.1111/j.1460-9592.2005.01783.x. http://dx.doi.org/10.1111/j.1460-9592.2005.01783.x. [DOI] [PubMed] [Google Scholar]
- 12.Rajan S, Gotluru P, Andews S, Paul J. Evaluation of endotracheal intubating conditions without the use of muscle relaxants following induction with propofol and sevoflurane in pediatric cleft lip and palate surgeries. J Anaesthesiol Clin Pharmacol. 2014;30:360–5. doi: 10.4103/0970-9185.137268. http://dx.doi.org/10.4103/0970-9185.137268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Apfel CC, Kranke P, Katz MH, Goepfert C, Papenfuss T, Rauch S, et al. Volatile anaesthetics may be the main cause of early but not delayed postoperative vomiting: a randomized controlled trial of factorial design. Br J Anaesth. 2002;88:659–68. doi: 10.1093/bja/88.5.659. http://dx.doi.org/10.1093/bja/88.5.659. [DOI] [PubMed] [Google Scholar]
- 14.Cohen MM, Duncan PG, DeBoer DP, Tweed WA. The postoperative interview: assessing risk factors for nausea and vomiting. Anesth Analg. 1994;78:7–16. doi: 10.1213/00000539-199401000-00004. http://dx.doi.org/10.1213/00000539-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Hartung J. Twenty-four of twenty-seven studies show a greater incidence of emesis associated with nitrous oxide than with alternative anesthetics. Anesth Analg. 1996;83:114–6. doi: 10.1097/00000539-199607000-00020. http://dx.doi.org/10.1213/00000539-199607000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Ogun CO, Duman A, Uysalel A. The effect of different anesthetic maintanences on postoperative nausea and vomiting in children undergoing adenotonsillectomies. Tur Klin J Med Sci. 2001;21:381–5. [Google Scholar]
- 17.Heidari SM, Saryazdi H, Saghaei M. Effect of intravenous midazolam premedication on postoperative nausea and vomiting after cholecystectomy. Acta Anaesthesiol Taiwan. 2004;42:77–80. [PubMed] [Google Scholar]
- 18.Greif R, Laciny S, Rapf B, Hickle RS, Sessler DI. Supplemental oxygen reduces the incidence of postoperative nausea and vomiting. Anesthesiology. 1999;91:1246–52. doi: 10.1097/00000542-199911000-00014. http://dx.doi.org/10.1097/00000542-199911000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Watcha MF, White PF. Postoperative nausea and vomiting. Anesthesiology. 1992;77:162–84. doi: 10.1097/00000542-199207000-00023. http://dx.doi.org/10.1097/00000542-199207000-00023. [DOI] [PubMed] [Google Scholar]
- 20.Gan TJ, Diemunsch P, Habib AS, Kovac A, Kranke P, Meyer TA, et al. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2014;118:85–113. doi: 10.1213/ANE.0000000000000002. http://dx.doi.org/10.1213/ANE.0000000000000002. [DOI] [PubMed] [Google Scholar]
- 21.Aydos LA, Özmert SG, Uysalel A, Tüzüner F. Comparison of ondansetron and deksamethazone’s antiemetic effects in children who underwent adenotisillectomy. Anestezi Dergisi. 1999;7:89–92. [Google Scholar]
- 22.Sheila M, Wilhelm SM, Dehoorne-Smith ML, Kale-Pradhan PB. Prevention of Postoperative Nausea and Vomiting. Ann Pharmacother. 2007;41:68–78. doi: 10.1345/aph.1H398. http://dx.doi.org/10.1345/aph.1H398. [DOI] [PubMed] [Google Scholar]
- 23.Dundee JW, Chestnutt WN, Ghaly RG, Lynas AG. Traditional Chinese acupuncture: a potentially useful antiemetic? Br Med J (Clin Res Ed) 1986;293:583–4. doi: 10.1136/bmj.293.6547.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yentis SM, Bissonnette B. P6 acupuncture and postoperative vomiting after tonsillectomy in children. Br J Anaesth. 1991;67:779–80. doi: 10.1093/bja/67.6.779. http://dx.doi.org/10.1093/bja/67.6.779. [DOI] [PubMed] [Google Scholar]
- 25.Shenkman Z, Holzman RS, Kim C, Ferrari LR, DiCanzio J, Highfield ES, et al. Acupressure–acupuncture antiemetic prophylaxis in children undergoing tonsillectomy. Anesthesiology. 1999;90:1311–6. doi: 10.1097/00000542-199905000-00015. http://dx.doi.org/10.1097/00000542-199905000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Streitberger K, Diefenbacher M, Bauer A, Conradi R, Bardenheuer H, Martin E, et al. Acupuncture compared to placebo-acupuncture for postoperative nausea and vomiting prophylaxis: A randomised placebo-controlled patient and observer blind trial. Anaesthesia. 2004;59:142–9. doi: 10.1111/j.1365-2044.2004.03577.x. http://dx.doi.org/10.1111/j.1365-2044.2004.03577.x. [DOI] [PubMed] [Google Scholar]
- 27.Fujii Y. Current management of vomiting after tonsillectomy in children. Curr Drug Saf. 2009;4:62–73. doi: 10.2174/157488609787354413. http://dx.doi.org/10.2174/157488609787354413. [DOI] [PubMed] [Google Scholar]
- 28.Schlager A, Offer T, Baldissera I. Laser stimulation of acupuncture point P6 reduces postoperative vomiting in children undergoing strabismus surgery. Br J Anaesth. 1998;81:529–32. doi: 10.1093/bja/81.4.529. http://dx.doi.org/10.1093/bja/81.4.529. [DOI] [PubMed] [Google Scholar]
- 29.Rusy LM, Hoffman GM, Weisman SJ. Electroacupuncture prophylaxis of postoperative nausea and vomiting following pediatric tonsillectomy with or without adenoidectomy. Anesthesiology. 2002;96:300–5. doi: 10.1097/00000542-200202000-00013. http://dx.doi.org/10.1097/00000542-200202000-00013. [DOI] [PubMed] [Google Scholar]
- 30.Liodden I, Howley M, Grimsgaard AS, Fønnebø VM, Borud EK, Alraek T, et al. Perioperative acupuncture and postoperative acupressure can prevent postoperative vomiting following paediatric tonsillectomy or adenoidectomy: a pragmatic randomised controlled trial. Acupunct Med. 2011;29:9–15. doi: 10.1136/aim.2010.002915. http://dx.doi.org/10.1136/aim.2010.002915. [DOI] [PubMed] [Google Scholar]
- 31.Macpherson H, Thomas K, Walters S, Fitter M. The York acupuncture safety study: prospective survey of 34000 treatments by traditional acupuncturists. BMJ. 2001;323:486–7. doi: 10.1136/bmj.323.7311.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yamashita H, Tsukayama H, Tanno Y, Nishijo K. Adverse events in acupuncture and moxibustion treatment: A six-year survey at a national clinic in Japan. J Alt Complement Med. 1999;5:229–36. doi: 10.1089/acm.1999.5.229. http://dx.doi.org/10.1089/acm.1999.5.229. [DOI] [PubMed] [Google Scholar]
- 33.Wang SM, Kain ZN. P6 Acupoint Injections Are as Effective as Droperidol in Controlling Early Postoperative Nausea and Vomiting in Children. Anesthesiology. 2002;97:359–66. doi: 10.1097/00000542-200208000-00012. http://dx.doi.org/10.1097/00000542-200208000-00012. [DOI] [PubMed] [Google Scholar]
- 34.Walach H, Falkenberg T, Fønnebø V, Lewith G, Jonas WB. Circular instead of hierarchical: methodological principles for the evaluation of complex interventions. BMC Med Res Methodol. 2006;24:6–29. doi: 10.1186/1471-2288-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]


