Abstract
Objective
Recently, to further enhance the potential in the management of difficult airways, the highly angulated D-Blade was added to the C-MAC system. The purpose of this study was to investigate the laryngoscopic view and intubation parameters using the new C-MAC D-Blade in comparison to the conventional C-MAC video laryngoscope and Macintosh direct laryngoscope in simulated easy and difficult airways.
Methods
We recruited 26 experienced anaesthesia providers into a randomized trial. Each performed tracheal intubation of a Laerdal SimMan® manikin with each laryngoscope in the following laryngoscopy scenarios: (1) normal airway, (2) cervical spine immobilization, and (3) tongue edema. The intubation times, success rates, number of intubation attempts, laryngoscopic views, and severity of dental compression were recorded.
Results
In all scenarios, video laryngoscopes provided better laryngeal exposure than the ML and appeared to produce less dental pressure. In the cervical spine immobilization scenario, D-Blade caused less dental pressure and showed better Cormack-Lehane (CL) classes than the other devices (p<0.001). There were no differences between video laryngoscopes in success of tracheal intubation (p>0.05). The CMAC provided the most rapid intubation. The rate of failure was 19% with ML. In the tongue edema scenario, the CMAC provided the most rapid and successful intubation (p<0.001). There were no differences between video laryngoscopes in laryngoscopic views according to CL classification and dental pressure (p>0.05). The rate of failure was 46% with the ML and 7% with the D-Blade.
Conclusion
The CMAC D-Blade caused less dental pressure than the conventional C-MAC and ML in the cervical immobilization scenario. The conventional CMAC performed better than the D-Blade and ML in the tongue edema scenario. These two video laryngoscopes may complement each other in various difficult airway situations.
Keywords: Difficult laryngoscopy, video laryngoscopy, manikin, equipment
Introduction
The vast majority of patients is intubated using standard direct laryngoscopes in daily anaesthesia practice, and the Macintosh laryngoscope is the most commonly used device. Despite advancements in predicting a difficult airway, the efficacy of routine preoperative tests are still limited (1, 2). Difficult intubation and failed tracheal intubation are among the major causes of morbidity and mortality associated with anaesthesia (3, 4). Indirect laryngoscopes improve the view and increase the success of intubation in cases when direct glottic view is difficult to obtain (5). In recent years, video laryngoscopy has gained an increasingly important role in the management of difficult and emergent laryngoscopy (6). This method allows for better visualization of anatomical structures, and it can be used as an educational tool (7). The mouth and pharyngeal tract is not necessary to view the glottis by indirect laryngoscopy. Bringing the pharyngeal and laryngeal axes, which have a close degree of slope to the same plane, is adequate to view the glottis (8). Many indirect laryngoscopes with different shapes and imaging technologies have been produced recently due to these advantages.
The C-MAC (Karl Storz, Tuttlingen, Germany) incorporates a standard Macintosh blade with a camera placed at its tip and a video display unit (9). Therefore, the C-MAC can be used both as a standard direct laryngoscope and as an indirect laryngoscope. Many previous studies showed that a limited laryngeal view with direct laryngoscopy was improved with C-MAC (10–12).
Recently, the producers of the C-MAC have produced C-MAC D-Blade, which has a highly angulated video laryngoscopic blade. The D-Blade is half-moon-shaped and can be used with the C-MAC system (Figure 1). This equipment was added to the C-MAC system to increase the potential to manage difficult airways and to introduce an alternative blade that can be used in extremely difficult conditions (13). Although the C-MAC D-Blade has been shown in recent trials to be beneficial in difficult airway conditions (14), present knowledge about the use of the D-Blade in different difficult laryngoscopy conditions is limited.
Figure 1.
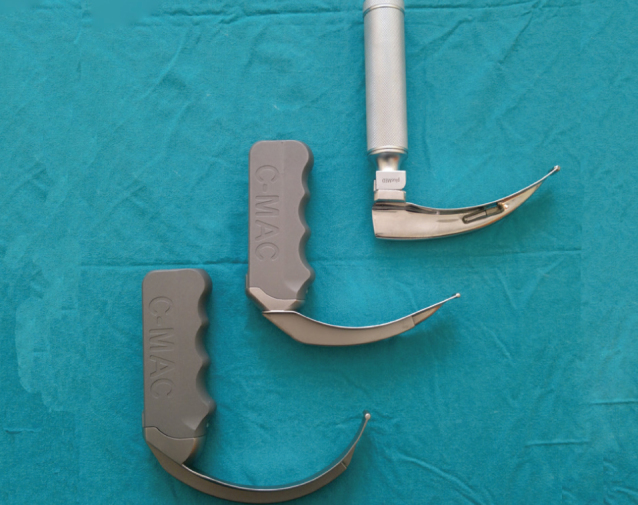
From left to right: (a) C-MAC D-Blade videolaryngoscope (b) Conventional C-MAC videolaryngoscope, (3) Macintosh laryngoscope
The purpose of this randomized controlled study was to compare the video laryngoscopes C-MAC D-Blade and conventional C-MAC with the Macintosh laryngoscope when used by experienced anaesthetist in an atomically correct manikin during simulated easy and difficult airways. Primary end-points were intubation time, success rate, number of intubation attempts, and laryngoscopic view.
Methods
After ethics board approval (Konya University, 13.3.2012/No: 2313) and written informed consent were obtained, 26 anaesthesia providers with at least 4 years of experience were included in the study. This group consisted of 16 staff anaesthesiologists and 10 residents. All residents were in the final year of their education, and all participants had performed at least 1000 intubations with the Macintosh laryngoscope. None of the participants had clinical experience with the use of C-MAC and D-Blade.
The three intubating devices (Figure 1) that we compared were:
Standard Macintosh laryngoscope, size 3 (Heine Optotechnik, Munich, Germany).
Storz C-MAC video laryngoscope, size 3 (Karl Storz GmbH, Tuttlingen, Germany).
Storz C-MAC D-Blade video laryngoscope (Karl Storz GmbH, Tuttlingen, Germany)
All anaesthetists were briefed about the study. Before starting the trial, a 30-minute standard education session was provided for all of the participants by one instructor. The education started with the screening of a computer-based presentation about the use of indirect laryngoscopes, which lasted 5 minutes. Consequently, each participant was permitted to attempt five intubations on the SimMan manikin (Laerdal Medical), on which the study was performed. The instructor provided constructive feedback. No presentation or demonstration was performed about the Macintosh, but five attempts at intubation were permitted.
All intubations were performed using a 7.0-mm cuffed tracheal tube. A semi-rigid stylet was introduced into the intubation tube. The stylet had a hockey stick shape (distal tip of 8 mm was angled at 100°) for the C-MAC and D-Blade. This configuration was previously demonstrated to facilitate intubation with the C-MAC and Glidescope with a more angled blade (15). A lubricant (Laerdal Medical), a 10-mL syringe to inflate the cuff of the tube, and an Ambu® resuscitator balloon (Ambu, Kopenhag, Denmark) were kept ready to be used in each trial. The design of the study was a randomized crossover trial consisting of three groups and three periods. Each anaesthesiologist performed tracheal intubations in one easy and two difficult laryngoscopy scenarios with each piece of equipment.
Airway scenarios were determined as:
Normal airway
Cervical spine immobilization with hard cervical collar and pharyngeal obstruction
Tongue edema
Difficult laryngoscopy scenarios were selected among the configurations of difficult but feasible situations (16, 17).
Each participant was requested to draw a letter from one opaque envelope indicating the equipment he/she would use and a letter indicating the level of difficulty for the airway to prevent bias due to learning and to provide randomization of the participants’ turns to use the equipment. All participants used the equipment in the same order during the study period. The participants were blinded to the level of difficulty of the airway, and they were prevented from seeing each other.
The primary endpoints were the duration of a successful trial of intubation, the rate of successful intubations, the number of attempts of intubations, and the number of the views obtained. Unsuccessful intubation was defined as no intubation in 120 seconds and/or the necessity to attempt an intubation more than three times. One unsuccessful trial of intubation was defined as removal of the equipment from the mouth and its replacement. The duration of intubation was defined as the time starting from the introduction of the equipment into the mouth through the teeth to the time of first successful inflation of the lungs. The duration was measured by the same investigator in all of the trials, and all measurements were performed with a mobile phone chronometer (Nokia, Finland). Cormack-Lehane grade (18) and percentage of glottic opening (POGO) (19) scores were recorded for each attempt. Cormack-Lehane and POGO scores were recorded by the investigator when the glottic opening was seen on the video monitor (by C-MAC and D-Blade). The time of the view of the glottic opening, which was seen during the use of Macintosh laryngoscope, was recorded by the participating anaesthesiologist. To aid in obtaining the best laryngeal view, a pillow was placed under the manikin, and a “sniffing position” was obtained. In addition, the participants were allowed to apply the maneuvers they desired.
Secondary endpoints included the number of optimization maneuvers required (change of head position, application of external laryngeal pressure) to aid tracheal intubation, the severity of dental compression, and the difficulty of use of each laryngoscope. The severity of dental compression was evaluated by an independent investigator by visual grading of the pressure applied to the upper teeth (0=none, 1=moderate, 2=severe). The number of additional maneuvers required was recorded by the investigator, too. After the completion of each scenario, each participant was asked to score the ease of the use of the laryngoscopes using a visual analog scale (VAS) (from 0=very easy to 100=very difficult) scoring system. The sample size was calculated by reference to previous studies (15, 20). Assuming a difference of success rate of 33% between the two devices in the tongue edema scenario and 80% power (a=0.05 and b=0.2), we calculated that 26 participants would be needed for the study.
Statistical analysis
The data were evaluated using the SPSS 15 (Statistical Package for the Social Sciences Inc., Chicago, IL, USA) statistical program. No cross-comparisons were made between the results of different laryngoscopy scenarios. Data for the rate of successful intubation were analyzed using the chi-square test. The Friedman test was used to analyze repeated measures, with “device” as the repeated measure. If a statistically significant finding was observed, post hoc analyses were carried out using the Wilcoxon signed-ranks tests with a Bonferroni correction. Continuous data are presented as mean (standard deviation, SD), ordinal data are presented as median (inter-quartile range), and categorical data are presented as number (%). In all analyses, a P-value <0.05 was accepted as statistically significant.
Results
Participants’ characteristics
A total of 26 anaesthesia providers (n=8 females, n=18 males, mean experience: 6.6±2.4 years and mean age: 33.2±4.3 years) were included in the study. None of the participants had prior experience in the use of indirect laryngoscopes. Only successful intubations were used to compare the durations of intubation attempts.
Scenario 1-Normal airway
There was a significant difference in the durations of successful intubation attempts between devices (Figure 2). Post hoc comparison revealed no difference between the C-MAC and Macintosh laryngoscopes (p=0.1), both being faster than the D-Blade (p<0.01). All anaesthetists successfully intubated the manikin with each device. There were no differences in the number of tracheal intubation attempts or optimization maneuvers required for each device (Table 1). The severity of dental compression was significantly lower with the C-MAC and the D-Blade compared with the Macintosh (Table 1). The C-MAC and the D-Blade produced significantly better Cormack and Lehane grades and POGO scores than the Macintosh (p=0.002) (Table 1). There were no significant differences in laryngoscopic views between the video laryngoscopes. The anaesthetists rated the D-Blade laryngoscope as more difficult to use than the C-MAC and the Macintosh (Figure 3). There was no difference in difficulty scores between the Macintosh and the C-MAC (p=0.8).
Figure 2.
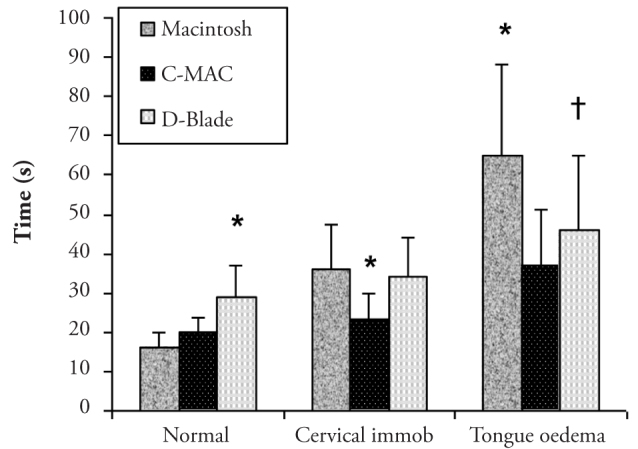
Mean time required to successfully intubate the trachea with each device in each scenario. Error bars indicate SD. *p<0.05 compared with all other laryngoscopes. †p<0.05 compared with C-MAC laryngoscope
Table 1.
Tracheal intubation data for normal airway scenario. Data are reported as median (IQR [range]) or as number (%)
| Macintosh | C-MAC | D-Blade | p value | |
|---|---|---|---|---|
| Overall success rate (%) | 26 (100) | 26 (100) | 26 (100) | 1.0 |
| Number of intubation attempts (%) | ||||
| 1 | 23 (89) | 25 (96.2) | 22 (85) | 0.3 |
| 2 | 3 (11) | 1 (3.8) | 4 (15) | |
| 3 | 0 | 0 | 0 | |
| Summary | 1 (1–1 [1–2]) | 1 (1–1 [1–1]) | 1 (1–1 [1–2]) | |
| Cormack and Lehane grade | ||||
| 1 | 18 (69.2) | 24 (92.3) | 26 (100) | <0.001 |
| 2. | 8 (30.8) | 2 (7.7) | 0 | |
| 3. | 0 | 0 | 0 | |
| 4. | 0 | 0 | 0 | |
| Summary | 1 (1–2 [1–2])*† | 1 (1–1 [1–2]) | 1 (1–1 [1–1]) | |
| POGO score | 70 (20–80 [10–90])*† | 100 (90–100 [40–100]) | 100 (100–100 [100–100]) | <0.001 |
| Number of optimization maneuvers (%) | ||||
| 0 | 24 (92.3) | 26 (100) | 26 (100) | 0.1 |
| 1 | 2 (7.7) | 0 | 0 | |
| 2 | 0 | 0 | 0 | |
| Summary | 0 (0–0 [0–1]) | 0 (0–0 [0–0]) | 0 (0–0 [0–0]) | |
| Severity of dental compression (%) | ||||
| 0 | 10 (38.5) | 20 (76.9) | 18 (69.2) | 0.03 |
| 1 | 16 (61.5) | 6 (23.1) | 8 (30.8) | |
| 2 | 0 | 0 | 0 | |
| Summary | 1 (0–1 [0–1])*† | 0 (0–0.25 [0–1]) | 0 (0–1 [0–1]) | |
p<0.05 compared with C-MAC laryngoscope;
p<0.05 compared with D-Blade laryngoscope.
POGO: Percentage of glottic opening
Figure 3.
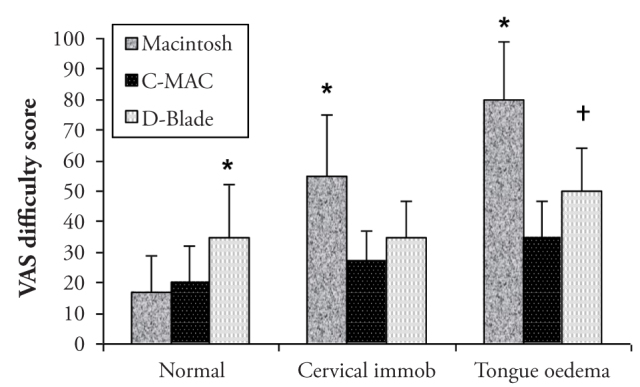
Mean VAS device difficulty score for each laryngoscope in each scenario. Error bars indicate SD. *p<0.05 compared with all other laryngoscopes. †p<0.05 compared with C-MAC laryngoscope
Scenario 2: Cervical spine rigidity and pharyngeal obstruction
There was a significant difference in the duration of successful intubation attempts between devices (Figure 2). Post hoc analysis revealed that the time taken to intubate was shorter with the C-MAC than with the Macintosh (p<0.01) and D-Blade (p<0.01), whereas the latter two did not differ (p=0.3). The rate of successful intubation was significantly different between the indirect laryngoscopes and the Macintosh. The C-MAC and D-Blade were successful in 100% of intubation attempts compared with 84% with the Macintosh (Table 2). The number of intubation attempts or optimization maneuvers required for the C-MAC and D-Blade was less than that required for the Macintosh (Table 2). The severity of dental compression was significantly lower with the D-Blade and significantly greater with the Macintosh laryngoscope compared with the C-MAC laryngoscope (Table 2). The C-MAC and D-Blade produced significantly better Cormack and Lehane grades and POGO scores than the Macintosh. There were no significant differences in the laryngoscopic views between the video laryngoscopes (Table 2). The anaesthetists rated the Macintosh laryngoscope as more difficult to use than the C-MAC and the D-Blade (p<0.001) (Figure 3). There was no difference in difficulty scores between the C-MAC and D-Blade (p=0.4).
Table 2.
Tracheal intubation data for cervival spine rigidity scenario. Data are reported as median (IQR [range]) or as number (%)
| Macintosh | C-MAC | D-Blade | p value | |
|---|---|---|---|---|
| Overall success rate (%) | 21 (80.8)*† | 26 (100) | 26 (100) | 0.007 |
| Number of intubation attempts (%) | ||||
| 1 | 13 (50) | 20 (76.9) | 18 (69.2) | 0.003 |
| 2 | 12 (42.3) | 6 (23.1) | 8 (30.8) | |
| 3 | 2 (7.7) | 0 | 0 | |
| Summary | 1.5 (1–2 [1–3])*† | 1 (1–1 [1–2]) | 1 (1–2 [1–2]) | |
| Cormack and Lehane grade | ||||
| 1 | 3 (11.5) | 21 (80.8) | 22 (84.6) | <0.001 |
| 2 | 14 (53.8) | 5 (19.2) | 4 (15.4) | |
| 3 | 9 (34.6) | 0 | 0 | |
| 4 | 0 | 0 | 0 | |
| Summary | 2 (2–3 [1–3])*† | 1 (1–1 [1–2]) | 1 (1–1 [1–2]) | |
| POGO score | 25 (0–70 [0–90])*† | 90 (80–100 [30–100]) | 100 (85–100 [30–100]) | <0.001 |
| Number of optimization maneuvers (%) | ||||
| 0 | 14 (53.8) | 24 (92.3) | 26 (100) | <0.001 |
| 1 | 10 (38.8) | 2 (7.7) | 0 | |
| 2 | 2 (7.7) | 0 | 0 | |
| Summary | 0 (0–1 [0–2])*† | 0 (0–0 [0–1]) | 0 (0–0 [0–0]) | |
| Severity of dental compression (%) | ||||
| 0 | 0 | 4 (15.4) | 10 (38.5) | <0.001 |
| 1 | 8 (30.8) | 17 (65.4) | 16 (61.5) | |
| 2 | 18 (69.2) | 5 (19.2) | 0 | |
| Summary | 2 (1–2 [1–2])*† | 1(1–1 [ 0–2 ])† | 1 (0–1 [0–1]) | |
p<0.05 compared with C-MAC laryngoscope;
p<0.05 compared with D-Blade laryngoscope.
POGO: Percentage of glottic opening
Scenario 3-Tongue edema
There was a significant difference in the duration of successful intubation attempts between devices. Statistical analysis revealed that the time taken to intubate was significantly shorter with the C-MAC (p<0.01) and significantly longer with the Macintosh (p<0.01) in comparison with the D-Blade (Figure 2). The rate of successful intubation was significantly different between the devices. The C-MAC was successful in 100% of intubation attempts, compared with 92.4% with the D-Blade and 54% with the Macintosh. There was no significant difference in the rate of success between the indirect laryngoscopes (p=0.4) (Table 3). The number of tracheal intubation attempts required was significantly lower with the video laryngoscopes compared with Macintosh laryngoscope. There were no differences in the number of tracheal intubation attempts required for the C-MAC and D-Blade (Table 3). The number of optimization maneuvers required for the D-Blade was less than that required for the Macintosh but greater than that required for the C-MAC (Table 3). The severity of dental compression was lower with the video laryngoscopes compared with the Macintosh (Table 3). The C-MAC and the D-Blade produced significantly better Cormack and Lehane grades and POGO scores than the Macintosh. There were no significant differences in the laryngoscopic views between the video laryngoscopes (Table 3). The anaesthetists found the Macintosh very difficult to use, and the D-Blade was judged to be of intermediate difficulty, whereas the C-MAC was found to be easy to use (Figure 3). Prolonged intubation times with the D-Blade were due to difficulties in inserting the device into the mouth. Prolonged intubation times with the Macintosh were due to the poor quality of laryngeal exposure.
Table 3.
Tracheal intubation data for tongue edema scenario. Data are reported as median (IQR [range]) or as number (%)
| Value | Macintosh | C-MAC | D-Blade | p |
|---|---|---|---|---|
| Overall success rate (%) | 14 (53.8)*† | 26 (100) | 24 (92.3) | <0.001 |
| Number of intubation attempts (%) | ||||
| 1 | 12 (46.1) | 19 (73.1) | 17 (65.4) | 0.025 |
| 2 | 8 (30.8) | 7 (26.9) | 7 (26.9) | |
| 3 | 6 (23.1) | 0 | 2 (7.7) | |
| Summary | 2 (1–2.25 [1–3])*† | 1 (1–2 [1–2]) | 1 (1–2 [1–3]) | |
| Cormack and Lehane grade | ||||
| 1 | 1 (3.8) | 22 (84.6) | 21(80.8) | <0.001 |
| 2 | 8 (30.8) | 4 (15.4) | 5 (19.2) | |
| 3 | 16 (61.5) | 0 | 0 | |
| 4 | 1 (3.8) | 0 | 0 | |
| Summary | 3 (2–3 [1–4])*† | 1 (1–1 [1–2]) | 1 (1–1 [1–2]) | |
| POGO score | 0 (0–30 [0–80])*† | 80 (70–100 [20–100]) | 95 (70–100 [30–100]) | <0.001 |
| Number of optimization maneuvers (%) | ||||
| 0 | 7 (26.9) | 22 (84.6) | 16 (61.5) | <0.001 |
| 1 | 13 (50) | 4 (15.4) | 7 (26.9) | |
| 2 | 6 (23.1) | 0 | 3 (11.5) | |
| Summary | 1 (0–1.25 [0–2 ])*† | 0 (0–0 [0–1]) | 0 (0–1 [0–2])* | |
| Severity of dental compression (%) | ||||
| 0 | 0 | 7 (26.9) | 5 (19.2) | <0.001 |
| 1 | 0 | 16 (61.5) | 16 (61.5) | |
| 2 | 26 (100) | 3 (11.5) | 5 (19.2) | |
| Summary | 2 (2–2 [2–2])*† | 1 (0–1 [0–2]) | 1 (1–1 [0–2]) | |
p<0.05 compared with C-MAC laryngoscope;
p<0.05 compared with D-Blade laryngoscope.
POGO: Percentage of glottic opening
Discussion
In this study, both video laryngoscopes provided better laryngeal views in all difficult airway simulations compared to the conventional Macintosh blade and facilitated tracheal intubation. In addition, the video laryngoscopes created a lesser degree of dental compression and were evaluated as easier to use (compared to the Macintosh laryngoscope) in the difficult airway scenarios. While the number of unsuccessful intubations was 14 by the Macintosh in the most difficult airway scenario, this number was only 2 with D-Blade. The trial of tracheal intubations with C-MAC was successful in all scenarios. To the best of our knowledge, the two video laryngoscopes studied in this trial were not compared previously in studies either on patients or on manikins, and thus, this is the first study to evaluate the D-Blade in different difficult laryngoscopy conditions. When the duration of successful tracheal intubations was evaluated, differences in the equipment were observed according to the difficulty of the scenarios. The Macintosh and C-MAC allowed quicker intubation times compared to the D-Blade in normal airway scenarios. In previous studies, the use of the Macintosh was demonstrated to produce a shorter intubation time in normal airway scenarios compared to some indirect laryngoscopes, such as the Mcgrath (21), Airtraq (16, 20), and Pentax AVS (22). Serocki et al. (14) reported that the intubation time was significantly shorter with the Macintosh laryngoscope than with the Glidescope and D-Blade in patients with expected difficult airways. This situation has been explained by the familiarity of the anaesthesiologists to the Macintosh blade. In this study, the duration of intubation was shortest with the C-MAC in the two difficult laryngoscopy scenarios. While there was no difference between the duration of intubations with the D-Blade and Macintosh in the cervical spine immobilization scenario, the duration of intubation was shorter using the D-Blade compared to using the Macintosh in the tongue edema scenario. With increasing difficulty of the laryngoscopy, the laryngeal view was worsened by the Macintosh and the duration of intubation was lengthened.
Although the anaesthesiologists were using the C-MAC video laryngoscope for the first time, they reached similar intubation times compared to intubations using the Macintosh. This was likely due to easy apprehension of the C-MAC with a Macintosh-shaped blade by the participants and due to the easier introduction of this shape of blade into the mouth compared to the half-moon shape of the D-Blade. Thus, the D-Blade may require more practice for participants to get used to it than the conventional CMAC video laryngoscope. These results are in concordance with previous studies. The C-MAC video laryngoscope provided better intubation times compared to other indirect video laryngoscopes in different laryngoscopy situations in both human and manikin studies (16, 23).
It appears as one of the most important findings of this study that the D-Blade video laryngoscope causes less dental compression compared to Macintosh and especially the conventional C-MAC video laryngoscope in the cervical immobilization scenario. Angulation of the conventional CMAC size 3 blade increased 18° to 40° in the D-Blade (13). The high blade angulation may prevent additional maneuvers and further extension of the head for visualization of the larynx. Cervical mobilization was not evaluated in this study; however, the compression applied by the laryngoscope on the upper teeth is a surrogate marker of the extension forces applied to the head. Laryngoscopy and tracheal intubation of a patient with a cervical spine injury are procedures of very high risk that can even cause neurologic deficits (24, 25). Cervical vertebra should be immobilized in those patients, which makes the viewing of the larynx by conventional laryngoscopes more difficult. Additional maneuvers are required to obtain a better view with conventional laryngoscopes. Indirect laryngoscopes in those patients not only aid in overcoming the difficulties of laryngoscopy but also provide less movement of the cervical vertebra (26, 27). With the use of video laryngoscopy in patients in need of cervical immobilization, complication rates can be decreased, and thus, success rates of intubation can be increased.
Although the quality of the laryngeal view obtained by both video laryngoscopes was similar in the tongue edema scenario, two anaesthesiologists were unsuccessful in tracheal intubation by the D-Blade. In addition, the number of maneuvers needed for intubation was higher compared to the C-MAC by the D-Blade. Therefore, a good quality of view does not always result in a successful tracheal intubation (14, 28). Ng et al. (23), in a study of adult patients with potentially difficult airways, demonstrated that the C-MAC allowed more rapid intubation times with fewer intubation attempts, although more grade 1 laryngoscopic views are obtained by McGrath video laryngoscopes. In another study evaluating McGrath video laryngoscopes in unexpected difficult intubations, failure was reported in 5% of the patients (29). Although good views are obtained using the GlideScope, failure of intubation was reported in 6% of the patients (30).
The use of another indirect video laryngoscope, Truview EVO2, resulted in similar difficulties (22, 31). When the blade was angled more to obtain a better view, the tip of the intubation tube, which has to be directed to the larynx at a right angle, touched the anterior wall of the trachea and hence could not be forwarded to the trachea (32). The blade of the C-MAC is very similar to the Macintosh blade, and in addition, it is thinner, and the area that might possibly come into contact with the upper incisor teeth is narrower. Therefore, a larger space is obtained to elevate the epiglottis using the lever maneuver (10). Although in this study, the tube was shaped like a hockey stick by the stylet, this shape was deformed while being passed through the narrow space, and the tip of the endotracheal tube entered the larynx with a sharper angle. Therefore, the tip of the endotracheal tube could not be easily advanced in the trachea in some of the trials, although there were good laryngeal views.
This study has several limitations. First, this study was not performed on real patients but on an airway simulator. Simulation studies can mimic very rare difficult airway situations and provide a safe environment. In addition, it is difficult to obtain a standardized clinical environment in which many different anaesthesiologists can use different equipment. Anatomically correct manikins have been validated for this use and have been shown as a reliable surrogate marker of clinical situations (15, 17, 20, 22). Secondly, our investigators were not blinded to the type of equipment that the participants used, and thus, there was a potential bias present. However, our primary endpoints were objective measurements, and there is no possibility of an effect of bias of the observer. Thirdly, our difficult scenarios might be debated, in that they were not difficult enough, since they could not provide rare situations in which intubation with the D-Blade was successful in cases in which C-MAC failed. However, these scenarios were those that were used in prior studies mimicking human anatomy. Simulation manikins that resemble human anatomy at a higher rate are required in order to mimic difficult airway situations and allow many different anatomic changes. The last limitation is the subjective measurement of equipment difficulty scores. There may be a prejudice against the new equipment; however, in accordance with the objective measurements, the C-MAC was found to be the easiest and most preferred equipment. Previous studies support the ease of use of modern video laryngoscopes and report that the mechanisms are learned in a short period of time (15, 16).
Conclusion
In conclusion, in this difficult airway simulation study, in which experienced anaesthesiologists participated, conventional C-MAC and C-MAC D-Blade video laryngoscopes were proven to be advantageous compared to the conventional Macintosh blade. Indirect laryngoscopes differed in terms of rate of intubation, success of intubation, quality of the laryngeal view, dental compression, requirement of additional maneuvers, and ease of use. Differences or advantages were more prominent with increasing degrees of difficulty. All attempts at intubation were successful in all scenarios with conventional C-MAC use. The C-MAC was defined as the easiest equipment to use in the two difficult airway scenarios. The D-Blade was the equipment causing the least upper teeth compression in the cervical immobilization scenario. The D-Blade can be preferred, especially in the tracheal intubation of patients with cervical spine injury. These two video laryngoscopes may complement each other in different difficult airway situations. Further similar clinical comparative studies in the management of difficult airways on real patients to identify the situations in which these video laryngoscopes are advantageous and disadvantageous are needed.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Konya University (13.03.2012, No:2313).
Informed Consent: This study was not performed on real patients but on an airway simulator.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - A.K.; Design - A.K., A.T.; Supervision - A.E., AK.; Funding - A.T., A.K.; Materials - A.K., A.T.; Data Collection and/or Processing - A.K., A.T., A.E.; Analysis and/or Interpretation - A.K., A.T., A.E., S.T.U.; Literature Review - A.K., A.E., A.T.; Writer - A.K., A.T.; Critical Review - A.T., A.E., S.T.U.; Other - A.K., A.T., A.E., S.T.U.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Yentis SM, Lee DJ. Evaluation of an improved scoring system for the grading of direct laryngoscopy. Anaesthesia. 1998;53:1041–4. doi: 10.1046/j.1365-2044.1998.00605.x. http://dx.doi.org/10.1046/j.1365-2044.1998.00605.x. [DOI] [PubMed] [Google Scholar]
- 2.Mashour GA, Sandberg WS. Craniocervical extension improves the specificity and predictive value of the Mallampati airway evaluation. Anesth Analg. 2006;103:1256–9. doi: 10.1213/01.ane.0000237402.03329.3b. http://dx.doi.org/10.1213/01.ane.0000237402.03329.3b. [DOI] [PubMed] [Google Scholar]
- 3.Caplan RA, Posner KL, Ward RJ, Cheney FW. Adverse respiratory events in anesthesia: a closed claims analysis. Anesthesiology. 1990;72:828–33. doi: 10.1097/00000542-199005000-00010. http://dx.doi.org/10.1097/00000542-199005000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Mort TC. Emergency Tracheal Intubation: Complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99:607–13. doi: 10.1213/01.ANE.0000122825.04923.15. http://dx.doi.org/10.1213/01.ANE.0000122825.04923.15. [DOI] [PubMed] [Google Scholar]
- 5.Su YC, Chen CC, Lee YK, Lee JY, Lin KJ. Comparison of video laryngoscopes with direct laryngoscopy for tracheal intubation: a meta-analysis of randomised trials. Eur J Anaesthesiol. 2011;28:788–95. doi: 10.1097/EJA.0b013e32834a34f3. http://dx.doi.org/10.1097/EJA.0b013e32834a34f3. [DOI] [PubMed] [Google Scholar]
- 6.Stroumpoulis K, Pagoulatou A, Violari M, Ikonomou I, Kalantzi N, Kastrinaki K, et al. Videolaryngoscopy in the management of the difficult airway: a comparison with the Macintosh blade. Eur J Anaesth. 2009;26:218–22. doi: 10.1097/EJA.0b013e32831c84d1. http://dx.doi.org/10.1097/EJA.0b013e32831c84d1. [DOI] [PubMed] [Google Scholar]
- 7.Merli G. Videolaryngoscopy: is it only a change of view? Minerva Anestesiol. 2010;76:569–71. [PubMed] [Google Scholar]
- 8.Kaplan MB, Ward D, Hagberg CA, Berci G, Hagiike M. Seeing is believing: the importance of video laryngoscopy in teaching and in managing the difficult airway. Surg Endosc. 2006;20:479–83. doi: 10.1007/s00464-006-0038-z. http://dx.doi.org/10.1007/s00464-006-0038-z. [DOI] [PubMed] [Google Scholar]
- 9.Cavus E, Thee C, Moeller T, Kieckhaefer J, Doerges V, Wagner K. A randomised, controlled crossover comparison of the C-MAC videolaryngoscope with direct laryngoscopy in 150 patients during routine induction of anaesthesia. BMC Anesthesiol. 2011;1:11–6. doi: 10.1186/1471-2253-11-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cavus E, Kieckhaefer J, Doerges V, Moeller T, Thee C, Wagner K. The C-MAC videolaryngoscope: first experiences with a new device for videolaryngoscopy-guided intubation. Anesth Analg. 2010;110:473–7. doi: 10.1213/ANE.0b013e3181c5bce5. http://dx.doi.org/10.1213/ANE.0b013e3181c5bce5. [DOI] [PubMed] [Google Scholar]
- 11.Piepho T, Fortmueller K, Heid FM, Schmidtmann I, Werner C, Noppens RR. Performance of the C-MAC videolaryngoscope in patients after a limited glottic view using Macintosh laryngoscopy. Anaesthesia. 2011;66:1101–5. doi: 10.1111/j.1365-2044.2011.06872.x. http://dx.doi.org/10.1111/j.1365-2044.2011.06872.x. [DOI] [PubMed] [Google Scholar]
- 12.Aziz MF, Dillman D, Fu R, Brambrink AM. Comparative effectiveness of the C-MAC® videolaryngoscope versus direct laryngoscopy in the setting of the predicted difficult airway. Anesthesiology. 2012;116:1–8. doi: 10.1097/ALN.0b013e318246ea34. http://dx.doi.org/10.1097/ALN.0b013e318246ea34. [DOI] [PubMed] [Google Scholar]
- 13.Cavus E, Neumann T, Doerges V, Moeller T, Scharf E, Wagner K, et al. First clinical evaluation of the C-MAC D-Blade videolaryngoscope during routine and difficult intubation. Anesth Analg. 2011;112:382–5. doi: 10.1213/ANE.0b013e31820553fb. http://dx.doi.org/10.1213/ANE.0b013e31820553fb. [DOI] [PubMed] [Google Scholar]
- 14.Serocki G, Neumann T, Scharf E, Dörges V, Cavus E. Indirect videolaryngoscopy with C-MAC D-Blade and GlideScope: A randomized, controlled comparison in patients with suspected difficult airways. Minerva Anestesiol. 2013;79:121–9. [PubMed] [Google Scholar]
- 15.McElwain J, Malik MA, Harte BH, Flynn NH, Laffey JG. Determination of the optimal stylet strategy for the C-MAC videolaryngoscope. Anaesthesia. 2010;65:369–78. doi: 10.1111/j.1365-2044.2010.06245.x. http://dx.doi.org/10.1111/j.1365-2044.2010.06245.x. [DOI] [PubMed] [Google Scholar]
- 16.McElwain J, Malik MA, Harte BH, Flynn NM, Laffey JG. Comparison of the C-MAC videolaryngoscope with the Macintosh, Glidescope, and Airtraq laryngoscopes in easy and difficult laryngoscopy scenarios in manikins. Anaesthesia. 2010;65:483–9. doi: 10.1111/j.1365-2044.2010.06307.x. http://dx.doi.org/10.1111/j.1365-2044.2010.06307.x. [DOI] [PubMed] [Google Scholar]
- 17.Savoldelli GL, Schiffer E, Abegg C, Baeriswyl V, Clergue F, Waeber JL. Comparison of the Glidescope, the McGrath, the Airtraq and the Macintosh laryngoscopes in simulated difficult airways. Anaesthesia. 2008;63:1358–64. doi: 10.1111/j.1365-2044.2008.05653.x. http://dx.doi.org/10.1111/j.1365-2044.2008.05653.x. [DOI] [PubMed] [Google Scholar]
- 18.Cormack RS, Lehane J. Difficult tracheal intubation in obstet-rics. Anaesthesia. 1984;39:1105–8. http://dx.doi.org/10.1111/j.1365-2044.1984.tb08932.x. [PubMed] [Google Scholar]
- 19.Levitan RM, Hollander JE, Ochroch EA. A grading system for direct laryngoscopy. Anaesthesia. 1999;54:1009–10. doi: 10.1046/j.1365-2044.1999.1133f.x. http://dx.doi.org/10.1046/j.1365-2044.1999.1133f.x. [DOI] [PubMed] [Google Scholar]
- 20.Maharaj CH, Higgins BD, Harte BH, Laffey JG. Evaluation of intubation using the Airtraq or Macintosh laryngoscopeby anaesthetists in easy and simulated difficult laryngoscopy -a manikin study. Anaesthesia. 2006;61:469–77. doi: 10.1111/j.1365-2044.2006.04547.x. http://dx.doi.org/10.1111/j.1365-2044.2006.04547.x. [DOI] [PubMed] [Google Scholar]
- 21.Burdett E, Ross-Anderson DJ, Makepeace J, Bassett PA, Clarke SG, Mitchell V. Randomized controlled trial of the A.P. Advance, McGrath, and Macintosh laryngoscopes in normal and difficult intubation scenarios: a manikin study. Br J Anaesth. 2011;107:983–8. doi: 10.1093/bja/aer295. http://dx.doi.org/10.1093/bja/aer295. [DOI] [PubMed] [Google Scholar]
- 22.Malik MA, O’Donoghue C, Carney J, Maharaj CH, Harte BH, Laffey JG. Comparison of the Glidescope, the Pentax AWS, and the Truview EVO2 with the Macintosh laryngoscope in experienced anaesthetists: a manikin study. Br J Anaesth. 2009;102:128–34. doi: 10.1093/bja/aen342. http://dx.doi.org/10.1093/bja/aen342. [DOI] [PubMed] [Google Scholar]
- 23.Ng I, Hill AL, Williams DL, Lee K, Segal R. Randomized controlled trial comparing the McGrath videolaryngoscope with the C-MAC videolaryngoscope in intubating adult patients with potential difficult airways. Br J Anaesth. 2012;109:439–43. doi: 10.1093/bja/aes145. http://dx.doi.org/10.1093/bja/aes145. [DOI] [PubMed] [Google Scholar]
- 24.Hastings RH, Kelley SD. Neurologic deterioration associated with airway management in a cervical spine-injured patient. Anesthesiology. 1993;78:580–3. doi: 10.1097/00000542-199303000-00022. http://dx.doi.org/10.1097/00000542-199303000-00022. [DOI] [PubMed] [Google Scholar]
- 25.Heath KJ. The effect of laryngoscopy of different cervical spine immobilisation techniques. Anaesthesia. 1994;49:843–5. doi: 10.1111/j.1365-2044.1994.tb04254.x. http://dx.doi.org/10.1111/j.1365-2044.1994.tb04254.x. [DOI] [PubMed] [Google Scholar]
- 26.McElwain J, Laffey JG. Comparison of the C-MAC, Airtraq, and Macintosh laryngoscopes in patients undergoing tracheal intubation with cervical spine immobilization. Br J Anaesth. 2011;107:258–64. doi: 10.1093/bja/aer099. http://dx.doi.org/10.1093/bja/aer099. [DOI] [PubMed] [Google Scholar]
- 27.Turkstra TP, Pelz DM, Jones PM. Cervical spine motion: a fluoroscopic comparison of the AirTraq laryngoscope versus the Macintosh laryngoscope. Anesthesiology. 2009;111:97–101. doi: 10.1097/ALN.0b013e3181a8649f. http://dx.doi.org/10.1097/ALN.0b013e3181a8649f. [DOI] [PubMed] [Google Scholar]
- 28.Malik MA, Hassett P, Carney J, Higgins BD, Harte BH, Laffey JG. A comparison of the Glidescope (R), Pentax AWS (R), and Macintosh laryngoscopes when used by novice personnel: a manikin study. Can J Anesth. 2009;56:802–11. doi: 10.1007/s12630-009-9165-z. http://dx.doi.org/10.1007/s12630-009-9165-z. [DOI] [PubMed] [Google Scholar]
- 29.Noppens RR, Mobus S, Heid F, Schmidtmann I, Werner C, Piepho T. Evaluation of the McGrath Series5 videolaryngoscope after failed direct laryngoscopy. Anaesthesia. 2010;65:716–20. doi: 10.1111/j.1365-2044.2010.06388.x. http://dx.doi.org/10.1111/j.1365-2044.2010.06388.x. [DOI] [PubMed] [Google Scholar]
- 30.Rai MR, Dering A, Verghese C. The Glidescope system: a clinical assessment of performance. Anaesthesia. 2005;60:60–4. doi: 10.1111/j.1365-2044.2004.04013.x. http://dx.doi.org/10.1111/j.1365-2044.2004.04013.x. [DOI] [PubMed] [Google Scholar]
- 31.Nasim S, Maharaj CH, Butt I, Malik MA, O’ Donnell J, Higgins BD, et al. Comparison of the Airtraq and Truview laryngoscopes to the Macintosh laryngoscope for use by Advanced Paramedics in easy and simulated difficult intubation in manikins. BMC Emerg Med. 2009;9:2. doi: 10.1186/1471-227X-9-2. http://dx.doi.org/10.1186/1471-227X-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maassen R, Lee R, Hermans B, Marcus M, van Zundert A. A comparison of three c videolaryngoscopes: the Macintosh laryngoscope blade reduces, but does notreplace, routine stylet use for intubation in morbidlyobese patients. Anesth Analg. 2009;109:1560–5. doi: 10.1213/ANE.0b013e3181b7303a. http://dx.doi.org/10.1213/ANE.0b013e3181b7303a. [DOI] [PubMed] [Google Scholar]


