Abstract
Anaesthesiologists must always prefer the safest method to minimize the risk for patients. At present, ultrasound-guided blockage of the greater occipital nerve can be performed in a safe manner. In this report, we presented our experience of ultrasound-guided blockage of the greater occipital nerve that we performed in a patient with a mass at the back of the neck who had risk of general anaesthesia because of comorbidities.
Keywords: Greater occipital nerve, ultrasound, mass excision
Introduction
Currently, regional anaesthesia techniques are improving daily. Peripheral nerve blocks affect the haemodynamic response at the minimal level, and they can be the most ideal choice for high-risk patients and who cannot tolerate minimal deterioration in the haemodynamic response (1). Therefore, regional anaesthesia techniques that can be applied in patients under high risk for general anaesthesia are mostly preferred. Innervation of the posterior area of the head and neck is provided through cervical nerves. The greater occipital nerve, which enables cutaneous innervation in the large part of the posterior scalp, consists of the dorsal ramus of C2. Nociceptive stimuli arising from the meninges in the cervical region create sensitization in the convergent neurons in the posterior horn at the C2 level. Because the branch of the greater occipital nerve originating from the C2 root is responsible for the innervation of deep paraspinal muscles and suboccipital structures, the blockade of the greater occipital nerve means blocked stimuli from these innervated regions (2, 3).
In this case report, the technique of ultrasound-guided greater occipital nerve blockade, which was applied for reducing the anaesthesia risk in a patient with a lipoma in the posterior region of the neck, is presented.
Case Presentation
A 72-year-old patient, whose body mass index was 31.3 and who had the diagnosis of mass excision in the posterior region of the neck, was scheduled to undergo an operation at the department of plastic surgery after receiving written informed consent. The neck of the patient was short, and neck extension was limited. Ultrasound-guided bilateral greater occipital nerve blockade was planned for the patient who had a history of previous chronic atrial fibrillation, type 2 diabetes mellitus (type 2 DM) and approximately 5-year chronic obstructive pulmonary disease (COPD) and hypertension; whose laboratory findings were normal and who was included in the ASA III risk group. Intravenous vascular access was established on the dorsum of the right hand with an 18-gauge (G) cannula, and 10 mL kg−1 0.9% NaCl infusion was initiated. The patient, who was administered intravenous (iv) 0.025 mg kg−1 midazolam (midazolam 5 mg/5 mL, Greece) for premedication, was taken to the operating room. Non-invasive blood pressure, electrocardiogram (ECG), heart rate and peripheral oxygen saturation (SpO2) were monitorised. After ensuring that the patient is lying in the prone position (Figure 1), the posterior region of the neck was extensively cleaned with an antiseptic solution (Betadine®, Pasig City, Philippines). Then, the image of the greater occipital nerve was obtained from the medial occipital artery at the level of the superior nuchal line with a straight ultrasound probe (Figures 2, 3). Further, 3 mL of 1% lidocaine (Aritmal 2% ampul, Turkey) was bilaterally applied around the right and left greater occipital nerves. After approximately 10 min, iv 0.025 mg kg−1 Dormicum was administered again. After ensuring pain control of the posterior region of the neck, where mass excision would be performed, the intervention was started without applying any additional anaesthetic agent. The operation lasted for approximately 40 min, and it was a painless procedure. No postoperative complication was observed. The patient was discharged from the hospital approximately 24 h later.
Figure 1.

Image of the mass in the neck
Figure 2.
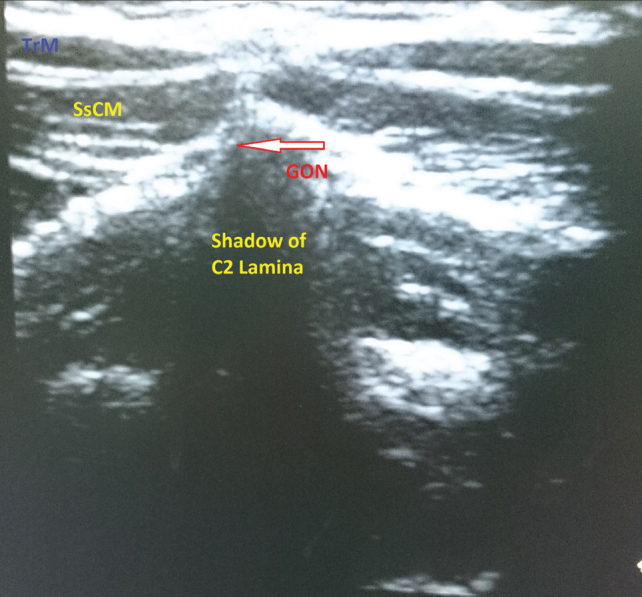
Image of the greater occipital nerve through the ultrasound linear probe
TrM: trapezius muscle; SsCM: semispinalis capitis muscle; GON: Greater Occipital Nerve
Figure 3.
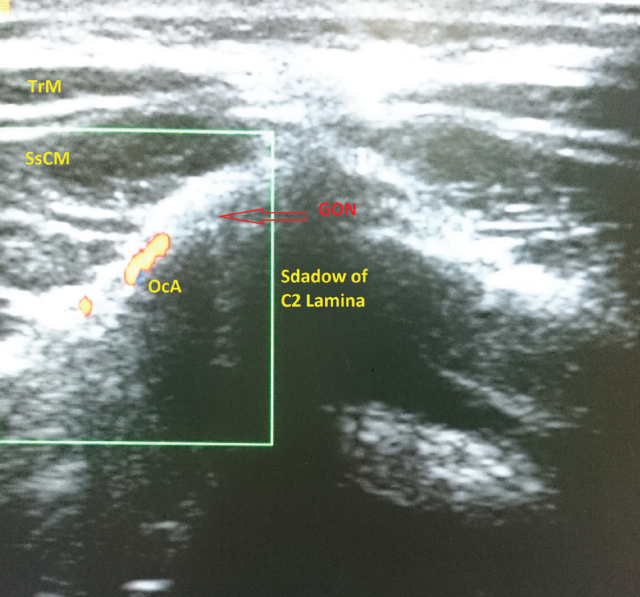
Image of the greater occipital nerve and occipital artery through the ultrasound linear probe
TrM: trapezius muscle; SsCM: semispinalis capitis muscle; GON: Greater Occipital Nerve; OcA: occipital artery
Discussion
The greater occipital nerve contains sensory fibres from the C2 and C3 segments of the medulla spinalis. It arises from the dorsal ramus of the C2 segment. It gets a thin branch from the C3 segment. It goes up over the major rectus capitis posterior muscle and passes at the level of the occipital artery medial and superior nuchal line. Then, it innervates the medial aspect of the posterior scalp up to the anterior aspect of the vertex (4, 5). The greater occipital nerve blockade inhibits the pain sensation in this region. Although the indication for the greater occipital nerve blockade is unclear, it is applied for post spinal headache, cervical headache, ‘cluster’ type headache, occipital neuralgia and migraine (6, 7).
Because the mass of our patient was 10×12 cm in size, in the medial part of the mastoid bone in the posterior neck and in size over the middle line, nerve blockade was applied bilaterally. Peripheral nerve blocks are more advantageous than general anaesthesia and central blocks because of their fewer respiratory and haemodynamic side effects, shorter recovery period and lower risk for the development of complications related to anaesthesia (1–8). Our patient was included in the obese group because of the body mass index of 31.3 and had COPD, hypertension, chronic atrial fibrillation and type 2 DM. Therefore, the risk for general anaesthesia and for being taken to the intensive care unit postoperatively was high. Ultrasound-guided bilateral greater occipital nerve block, which has fewer haemodynamic and respiratory side effects and a shorter recovery period, was applied. Because the greater occipital nerve has a superficial location, it has fewer complications. However, there is an intravascular injection risk, which can be prevented with careful aspiration. To reduce the possible complications, the patient should be questioned for previous intracranial traumas or cranial defects (9). Our patient had no history of previous cranial defects. Aspiration was carefully performed during blockade by considering the intravascular injection risk. The patient was administered lidocaine as an anaesthetic agent, and no intraoperative and postoperative complications were observed (10). Peripheral nerve blocks provide better and longer analgesia postoperatively (10). In our case, the analgesic agent was not needed for 8 h postoperatively.
Conclusion
In high risk patients, the anaesthesiologist must choose the most appropriate technique for reducing complications to the minimum level. Therefore, it is suggested that ultrasound-guided bilateral greater occipital nerve block will be a good alternative to other anaesthesia techniques while planning anaesthesia administration preoperatively in high-risk patients (as long as the surgeon is suitable in terms of place and time).
Further controlled studies are needed for this technique to be used more safely and commonly.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - O.B., U.K., M.Ş:, A.A., İ.Y.; Design - O.B., U.K., M.Ş:, A.A., İ.Y.; Supervision - O.B., U.K., M.Ş:, A.A., İ.Y.; Funding - O.B., M.Ş.; Materials - O.B., İ.Y.; Data Collection and/or Processing - O.B., M.Ş., U.K.; Analysis and/or Interpretation - O.B., A.A.; Writer - O.B., U.K.; Critical Review - O.B., A.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Chia N, Low TC, Poon KH. Peripheral nerve blocks for lower limb surgery a choice anaesthetic technique for patientswith a recent myocardial infarction? Singapore Med J. 2002;43:583–6. [PubMed] [Google Scholar]
- 2.Selekler MH. Greater occipital nerve blockade: trigeminicervical system and clinical applications in primary headaches. Agri. 2008;20:6–13. [PubMed] [Google Scholar]
- 3.Ashkenazi A, Levin M. Greater occipital nerve block for migraine and other headaches: is it useful? Curr Pain Headache Rep. 2007;11:231–5. doi: 10.1007/s11916-007-0195-3. http://dx.doi.org/10.1007/s11916-007-0195-3. [DOI] [PubMed] [Google Scholar]
- 4.Matute E, Bonilla S, Girones A, Planas A. Bilateral greater occipital nerve block for post-dural puncture headache. Anaesthesia. 2008;63:557–8. doi: 10.1111/j.1365-2044.2008.05531.x. http://dx.doi.org/10.1111/j.1365-2044.2008.05531.x. [DOI] [PubMed] [Google Scholar]
- 5.Mellick L, Verma N. Headache management with occipital nerve blocks, cervical ınjections and trigger point ınjections. The Open Emergency Medicine Journal. 2010;3:32–5. http://dx.doi.org/10.2174/1876542401003010032. [Google Scholar]
- 6.Takmaz SA, Inan N, Uçler S, Yazar MA, Inan L, Başar H. Greater occipital nerve block in migraine headache: preliminary results of 10 patients. Agri. 2008;20:47–50. [PubMed] [Google Scholar]
- 7.Naja Z, Al-Tannir M, El-Rajab M, Ziade F, Baraka A. Nerve stimulator-guided occipital nerve blockade for postdural puncture headache. Pain Pract. 2009;9:51–8. doi: 10.1111/j.1533-2500.2008.00238.x. http://dx.doi.org/10.1111/j.1533-2500.2008.00238.x. [DOI] [PubMed] [Google Scholar]
- 8.Fanelli G, Casati A, Aldegheri G, Beccaria P, Berti M, Leoni A. Cardiovascular effects of two different regional anaesthetic techniques for unilateral leg surgery. Acta Anaesthesiol Scand. 1998;42:80–4. doi: 10.1111/j.1399-6576.1998.tb05084.x. http://dx.doi.org/10.1111/j.1399-6576.1998.tb05084.x. [DOI] [PubMed] [Google Scholar]
- 9.Okuda Y, Matsumoto T, Shinohara M, Kitajima T, Kim P. Sudden unconsciousness during a lesser occipital nerve block in a patient with the occipital bone defect. Eur J Anaesthesiol. 2001;18:829–32. doi: 10.1046/j.1365-2346.2001.01018.x. http://dx.doi.org/10.1097/00003643-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Çiftçioğlu M, Acar S, Gürkan Y, Solak M, Toker K. Yüksek riskli bir olguda ultrason rehberliğinde çoklu periferik sinir bloğu uygulaması Ağrı. 2012;24:90–2. doi: 10.5505/agri.2012.18291. [DOI] [PubMed] [Google Scholar]


