Abstract
Objective
This study aimed to investigate the efficacy of femoral block and unilateral spinal anaesthesia on analgesia, haemodynamics and mobilization during endovenous ablation in patients with lower extremity venous insufficiency.
Methods
Forty patients of ASA physical status I and II, with ages ranging between 30 and 45 years, and who were scheduled for endovenous laser ablation for varicose veins were prospectively enrolled in this study. Patients were randomized into a unilateral spinal anaesthesia group (group HS, n=20) or a femoral block group (group F, n=20). Group HS received 7.5–10 mg of heavy bupivacaine for unilateral spinal anaesthesia, while group F received 100 mg prilocaine for femoral block with ultrasound guidance. The level of motor blockage (Bromage score), visual pain score, mean heart rate and mean arterial pressures were recorded at postoperative 0, 1, 2, 3d and 6 h, respectively.
Results
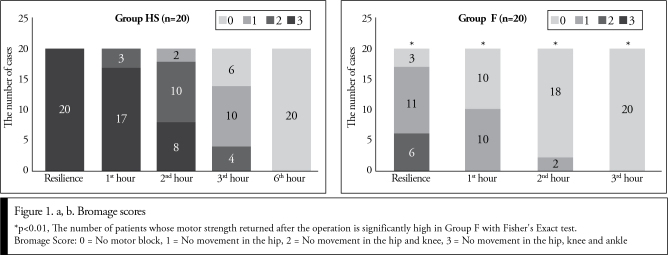
Perioperative visual pain score values in both groups were <4. None of the groups required an additional analgesic agent. Bromage scores were significantly lower in group F than in group HS during the postoperative period (p<0.01). Motor function returned to normal in all patients at 3 h in group F and at 6 h in group HS. Postoperative mean heart rate and arterial pressure did not differ between the groups (p>0.05).
Conclusion
In patients with lower extremity venous insufficiency who were undergoing endovenous laser ablation, an ultrasound-guided femoral block provided similar analgesia with that of unilateral spinal anaesthesia. In group F, the duration of anaesthesia and mobilization time was shorter.
Keywords: Varicose vein, laser ablation, nerve block, spinal block
Introduction
Endovascular laser ablation method is a minimally invasive alternative method to surgery in the treatment of superficial venous insufficiency (1–5). In this procedure, occlusion is generated by creating thermal damage to the endothelium. The process is performed under tumescent anaesthesia (TA) implemented by surgeons. With TA, pain is eliminated as well as normal tissues are protected from the excessive heat generated during the laser application. However, pain may occur because of a large number of TA injections administered along the large and small saphenous veins. Although such pain can be tolerated by some patients, the others may have a bad experience. Especially during venous catheterization, spasms may develop and the pain becomes more severe because of local anaesthesia itself or its high volume (1).
The characteristic of not delaying the mobilization is the most important one sought in the anaesthesia method to be selected for endovascular laser ablation. Delay in mobilization increases the risk of deep vein thrombosis. On the other hand, deep anaesthesia may cause unwanted damage to the saphenous and sural nerves (6). Various anaesthesia methods such as general anaesthesia, epidural anaesthesia, hemi-spinal anaesthesia, femoral block, sciatic block and conscious sedation have been administered during endovenous laser ablation (1–8). General anaesthesia has side effects such as nausea, vomiting, sore throat and myalgia; spinal blocks have side effects such as postoperative lumbar pain, postdural headache and postdural hypotension; conscious sedation has side effects such as respiratory depression and extension of the time of discharge (9, 10).
The sensory innervation of the femoral nerve includes the skin and muscles in the proximal anterior aspect of the knee and makes the interventions possible on both large and small saphenous veins (5). Ultrasound-guided peripheral blocks are preferred because they increase the quality and success of the block, prevent the side effects and decrease the implementation time (11).
The purpose of the study is to compare the effects of unilateral spinal anaesthesia and femoral nerve block on perioperative analgesia, haemodynamic parameters and after ablation procedures with endovenous laser in patients with venous insufficiency of the lower extremity.
Methods
After the approval of the Ethics Committee (20478486-323) of the Faculty of Medicine, Celal Bayar University, 40 cases with ASA physical status I–II for whom varicose vein surgery was planned electively with unilateral lower extremity endovascular laser method in cardiovascular surgery operating room were included in the study after being informed in detail about the blocks to be performed and after receiving the written informed consent. There were clinical symptoms of chronic venous insufficiency (pain while standing) and visible signs in all cases. Insufficiency observed in deep and/or small veins and/or perforating veins by Doppler ultrasound. Inclusion criteria in the study were determined as not having central or peripheral neuropathy, diabetes, coagulation disorders, severe lung and heart function disorders and liver and kidney function disorder. The criteria of exclusion from the study were determined as failure to observe the muscle response through nerve stimulator at maximum of 0.5 mA and not being able to detect the sensory block in the innervation area through pinprick test after the administering the block.
In the operating room, balanced electrolyte solution infusion (10 mL kg−1 h−1) was started by placing an 18 G venous cannula in the forearm. Before beginning the trials of anaesthesia, all patients were administered 500 mL of maintenance fluid in 20 minutes and midazolam (0.04 mg kg−1) intravenously for sedation purposes. The heart rate (ECG), arterial oxygen saturation (SpO2) and non-invasive arterial pressure of the patients were monitored. Patients were randomized to hemi-spinal anaesthesia group (Group HS, n=20) or femoral nerve block group (Group F, n=20) in the operating room by the unilateral method of drawing lots. In patients of the group of HS, the spinal space was entered through the midline of L4–5 or L3–4 with a 22 G Quince needle in accordance with the antisepsis rules in the lateral decubitus position and unilateral spinal anaesthesia was performed with 7.5 mg of ‘heavy’ bupivacaine (Marcaine Spinal Heavy AstraZeneca Trade Inc., Levent, Istanbul, Turkey). The patients were placed in the lateral decubitus position until the anaesthesia level reached T12 level (max 10 min.). For patients receiving the femoral block, common femoral artery and vein were monitored at the inguinal ligament level in the supine position after performing antisepsis of the groin, with the linear transducer being held transversely (Sono Site Micro Maxx, L25 prob, Sono Site, Bothell, WA, USA). Later, the triangular area formed by iliac fascia, common femoral artery and iliopsoas muscle, where the femoral nerve fibres are located, lateral to the common femoral artery was monitored. A short (50 mm) needle tip (Stimplex ab.braun®, Melsungen AG, Germany) connected with the nerve stimulator (Multiplex Pajunk, Germany) was advanced using the in-plane technique under the iliac fascia. Characteristic rhythmic twitching movement of the patella (patellar dance) was observed using current of ≤0.5 mA. Following a negative aspiration test, 100 mg prilocaine (Citanest 2%, 20 mgmL−1, AstraZeneca Trade Inc., Levent, Istanbul, Turkey), which was diluted in 20 ml saline solution, was injected into the lateral aspect of the femoral artery in triangular area (anterior branch of the femoral nerve) and the rear limit of the triangle (posterior branch) (12). The effectiveness of the block was confirmed by the disappearance of the pinprick feeling in the innervation area. Anaesthesia processing time (elapsed time from taking the patients to the anaesthesia room to the confirmation of block effectiveness) and the duration of surgery were recorded.
Standard TA [lidocaine (400 mgL−1 = 0.04%) diluted in isotonic saline, epinephrine (1 mgL−1 = 1: 1,000.000) and sodium bicarbonate (10 mEqL−1)] was used during endovenous ablation. Ablation was performed to veins using 980-nm (A.R.C. Laser GmbH Nuremberg, Germany) or 810-nm (Angiodynamics, Queensbury, NY, USA) laser fibres. The patients were placed in the reverse Trendelenburg position in order to create fullness in veins. Insufficient veins were punctured using an 18 G needle under US guidance, and angled tipped guide wire was advanced through the needle until it passed the junction between the deep veins and insufficient veins. The laser catheter was placed near the junction after it was advanced using a guide wire; then guide wire was withdrawn. Tumescent solution was injected into around the vein with the guidance of US. Ablation was performed by giving 50–120 J/cm of energy depending on the diameter of reflux veins. Legs were wrapped with compression bandages after the procedure.
The heart rate and mean arterial blood pressure was measured and recorded at 5-minute intervals after the blocks. Engine block level was evaluated with Bromage scale (0: No motor block, 1: No movement in the hip, 2: No movement in the hip and knee, 3: No movement in the hip, knee and ankle) 10 minutes after the blocks were performed as well as in the 1st, 2nd, 3rd and 6th postoperative hours after arrival at the recovery room after the procedure. Foot movements were evaluated using verbal commands. At the same periods of time after the procedure, pain levels, nausea and vomiting score, HR and MAP were recorded using visual analogue scale (VAS). The VAS value was aimed to be ≤4 (0, no pain, 10 unbearable pain). If the pain score is above this, fentanyl (1 μg kg−1, i.v.) was administered in the intraoperative period and dexketoprofen 50 mg kg−1, i.v. (maximum 150 mg day−1) in the postoperative period. The nausea and vomiting symptoms of the cases were evaluated with nausea-vomiting score (1. No nausea, 2. Slight nausea. 3. Serious nausea. 4. Vomiting), if the nausea and vomiting score is 2 and above, 10 mg kg−1 i.v. of metoclopramide was administered. The doses of analgesic and antiemetic drugs consumed during the observation period were recorded. Dizziness and headache were questioned and recorded. The patients in femoral block group whose hemodynamics remained stable after walking 15–20 minutes under the supervision of a nurse were discharged. The cases of unilateral spinal anaesthesia group were discharged the next day in order to monitor the side effects of the central block. Patients (at discharge) and surgeons (after surgery) were asked to evaluate the satisfaction levels as too bad, bad, average, good, very good, and the results were recorded.
Statistical analysis
The data were evaluated using the statistical software Statistica for Windows version 6.0 (StatSoft, Inc., Tulsa, USA). The data were recorded as mean ± standard deviation (SD) or the number of cases (n). The distribution characteristics of the variables were investigated with the Kolmogorov–Smirnov test. In the comparisons among groups, Student’s t-test was used for the data with normal distribution, Mann–Whitney U-test for the data not showing normal distribution and the Fisher exact test for categorical variables. Bonferroni-corrected Wilcoxon test was used as Friedmann and post-hoc tests in the multiple comparisons within groups. Results were evaluated at 95% confidence interval and a significance level of p<0.05.
Results
Forty patients that were included in the study completed the study. In the group of femoral nerve block, occlusion of the great saphenous vein occurred in 11 cases and that of perforating veins in 9 cases. The corresponding numbers of cases in the group of hemi-spinal anaesthesia were 13 and 7. The characteristics and surgery duration of the patients were similar in the groups (Table 1). The duration of beginning the surgery was significantly longer in the group administered unilateral spinal anaesthesia than in the group administered femoral nerve block (41.4±8.1 min. and 28.5±4.1 min.; p=0.001), probably because of the waiting period in the lateral decubitus position.
Table 1.
Demographic characteristics
| Group HS (n=20) | Group F (n=20) | p | |
|---|---|---|---|
| Age (years) | 44±10 | 45±15 | 0.1 |
| Body mass index | 1.8±0.1 | 1.7±0.2 | 0.6 |
| Gender (M / F) | 14/6 | 15/5 | 0.5 |
| Concomitant Disease | |||
| Hypertension | 1 | 1 | 0.5 |
| obesity | 1 | 2 | 0.5 |
| Anaesthesia time (in minutes) | 41±8 | 28±4 | 0.02* |
| Processing time (in minutes) | 27±3 | 28±5 | 0.1 |
| Midazolam (mg) | 2.1±1.1 | 2.3±0.7 | 0.1 |
| Tumescent (mL) | 379.1±41.3 | 385.3±31.8 | 0.2 |
Student’s t-test for comparisons among groups. Values were calculated as mean ± SD.
M: male; F: female; SD: standard deviation
In the average values of heart rate and arterial pressure during and after the process, no significant change was observed in the comparisons of intra-group and intergroup (Table 2).
Table 2.
Perioperative HR and MAP values (mean±SD)
| Beginning | After the block | |||||
|---|---|---|---|---|---|---|
| 5th min | 15th min | 30th min | 60th min | *p | ||
| HR | ||||||
|
| ||||||
| Group HS | 78±8 | 76±7 | 79±9 | 75±11 | 78±10 | 0.8 |
|
| ||||||
| Group F | 77±8 | 74±9 | 78±9 | 74±9 | 77±9 | 0.6 |
|
| ||||||
| CBG | 0.8 | 0.8 | 0.4 | 0.6 | 0.7 | |
|
| ||||||
| MAP | ||||||
|
| ||||||
| Group HS | 79±12 | 79±12 | 75±9 | 76±11 | 77±5 | 0.2 |
|
| ||||||
| Group F | 82±10 | 81±9 | 79±11 | 80±10 | 80±8 | 0.1 |
|
| ||||||
| CBG | 0.4 | 0.6 | 0.2 | 0.2 | 0.2 | |
CBG: comparison between groups; Mann–Whitney U-test.
p: intergroup comparison; Friedman test, Bonferroni-corrected Wilcoxon test.
HR: heart rate, pulse min–1; MAP: mean arterial pressure; min: minutes; SD: standard deviation
Pain scores in the visual analogue scale were 0 in all patients during the process in the group administered HS. In group F, pain (VAS>4) was felt in 3 (15%) patients in the first puncture of the great saphenous veins. The guide wire was enabled to advance through the needle painlessly by administering TA to the area. Because of the failure to relieve the pain in one of these patients with TA, 0.1 μg i.v. fentanyl was administered.
VAS values were <4 in all patients in both groups (Table 3). There was no need for additional analgesic agent administration.
Table 3.
Visual analogue scale values
| Group HS (n=20) 0/1: 2/3: ≥4 |
Group F (n=20) 0/1: 2/3: ≥4 |
*p | |
|---|---|---|---|
| postoperative recovery | 20 (100): 0: 0 | 18 (90): 2 (10): 0 | 0.5 |
| 1st hour | 20 (100): 0: 0 | 16 (80): 4 (20): 0 | 0.09 |
| 2nd hour | 20 (100): 0: 0 | 19 (95): 1 (5): 0 | 0.8 |
| 3rd hour | 20 (100): 0: 0 | 20 (100): 0: 0 | 1.0 |
| 6th hour | 20 (100): 0: 0 | 20 (100): 0: 0 | 1.0 |
P Fisher’s exact test.
In the group administered unilateral spinal anaesthesia, unilateral complete motor and sensory block at T12 level were established in all cases. Complete motor block (Bromage 3) was not established in any patient in the group administered femoral nerve block. Five patients had moderate motor block (Bromage 2) and 12 patients had mild motor block (Bromage 1). Motor block did not get established (Bromage 0) in three cases. In group F, low Bromage score was found in significantly greater number of patients in the postoperative period. All patients completely regained the leg motor functions in the postoperative 3rd hour in group F and in the postoperative 6th hour in the group administered HS (Figure 1a, b).
Figure 1.
a, b. Bromage scores
*p<0.01, The number of patients whose motor strength returned after the operation is significantly high in Group F with Fisherfs Exact test.
Bromage Score: 0 = No motor block, 1 = No movement in the hip, 2 = No movement in the hip and knee, 3 = No movement in the hip, knee and ankle
Patient and surgeon satisfaction was complete in all cases. In both groups, an additional sedative dose were not required in addition to that administered initially. In the group administered HS, antiemetic agent was required in 2 (10%) patients and urinary retention developed in 1 (5%) patient (p<0.05). Dizziness and hypotension were not detected in any of the patients.
In the group administered femoral nerve block, 3 patients were excluded from the study because muscle movement response was not observed with nerve stimulator at a value >0.5 mA.
Discussion
Unilateral spinal anaesthesia and femoral nerve block procedures were compared during the laser ablation of insufficient great, little or perforating veins. In the group administered femoral nerve block, analgesia similar to unilateral spinal anaesthesia group was achieved in both the intraoperative and postoperative periods.
The femoral nerve (L2–L4) is the largest branch of the lumbar plexus. It is divided into two at the level of inguinal ligament. Anterior branch provides motor innervation of the sartorius and pectineus muscles and the sensory innervation of the anterior and medial aspects of the leg. The posterior branch provides motor innervation of the quadriceps muscle and sensory innervation of the medial thigh. Thus, when these two branches of the femoral nerve are blocked, the anterior and medial aspects of the whole leg that is the trace of varicose veins is numbed (13). Similar to the results of our study, it was reported that adequate analgesia was provided using the femoral block during the treatment of varicose veins with endovenous laser ablation (1–4).
Enabling rapid mobilization, the femoral block decreases the risk of deep vein thrombosis after the treatments of insufficient veins (1–4, 6). In our study, motor blockade was found in significantly lower rates in the femoral group. After the movements of the knee and the movements of the ankle completely recovered within a few hours and in the 3rd hour, respectively, after the operation, the patients were mobilized; they were discharged on the same day. Shorter start-up time of the surgery in the femoral block group also contributed to the rapid discharge of patients.
Dissatisfaction because of paraesthesia has been observed in patients who underwent femoral block (14). In this study, the implementation of the minimally invasive vascular intervention (in comparison with arthroscopy patients), TA administered during the operation with local anaesthesia and initially implemented sedation may have blocked paraesthesia symptoms in our patients.
It’s been reported that ultrasound-guided peripheral blocks increased the success and quality of the block, prevented side effects and shortened the implementation time (11). During the administration of a block, no femoral artery puncture took place in any patients. In our study, the nerve stimulator was also used along with US guidance. The rate of success was found higher in femoral blocks where motor response was achieved at lower frequencies with nerve stimulator use. Success rates of 87% and 93% were reported when motor responses in the range of 0.6–0.8 mA and 0.3–0.5 mA were achieved (14). In our study, we included the cases from whom we received a motor response at maximum 0.5 mA in order to standardize our study.
Conclusion
In patients with venous insufficiency requiring endovascular laser ablation, analgesia similar to the that achieved in unilateral spinal anaesthesia was achieved using ultrasound-guided femoral block; despite this, anaesthesia and mobilization durations were shorter in the patients undergoing femoral block.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Celal Bayar University School of Medicine.
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – T.Ö., E.Ç.; Design – T.Ö., E.Ç., İ.T., F.N., A.Ö.; Supervision – T.Ö., İ.T.; Resources – T.Ö., E.Ç., F.N., A.Ö., İ.T.; Materials – T.Ö., E.Ç., A.Ö.; Data Collection and/or Processing – T.Ö., E.Ç.; Analysis and/or Interpretation – T.Ö., E.Ç., F.N., A.Ö.; Literature Search – T.Ö., E.Ç., F.N., A.Ö., İ.T.; Writing Manuscript – T.Ö., E.Ç.; Critical Review – İ.T.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Yilmaz S, Ceken K, Alimoglu E, Sindel T. US - guided femoral and sciatic nerve blocks for analgesia during endovenous laser. Cardiovasc Intervent Radiol. 2013;36:150–7. doi: 10.1007/s00270-012-0366-4. http://dx.doi.org/10.1007/s00270-012-0366-4. [DOI] [PubMed] [Google Scholar]
- 2.Oguzkurt L. Endovenous laser ablation for the treatment of varicose veins. Diagn Interv Radiol. 2012;18:417–22. doi: 10.4261/1305-3825.DIR.5248-11.0. [DOI] [PubMed] [Google Scholar]
- 3.Hoggan BL, Cameron AL, Maddern GJ. Systematic review of the endovenous laser therapy versus surgery for the treatment of saphenous varicose veins. Ann Vasc Surg. 2009;23:277–87. doi: 10.1016/j.avsg.2008.11.002. http://dx.doi.org/10.1016/j.avsg.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Yılmaz S, Ceken K, Alparslan A, Sindel T, Lüleci E. Endovenous laser ablation for saphenous vein insufficiency: immediate and shortterm results of our first 60 procedures. Diagn Interv Radiol. 2007;13:156–63. [PubMed] [Google Scholar]
- 5.Meier G, Buettner J. An atlas of anatomy and techniques. New York: Georg Thieme Verlag; 2007. Peripheral regional anesthesia; pp. 92–4. [Google Scholar]
- 6.Van Den Bos RR, Neumann M, De Roos KP, Nijsten T. Endovenous laser ablation-induced complications: review of the literature and new cases. Dermatol Surg. 2009;35:1206–14. doi: 10.1111/j.1524-4725.2009.01215.x. http://dx.doi.org/10.1111/j.1524-4725.2009.01215.x. [DOI] [PubMed] [Google Scholar]
- 7.Dzieciuchowicz L, Espinosa G, Grochowicz L. Evaluation of ultrasound-guided femoral nerve block in endoluminal laser ablation of the greater saphenous vein. Ann Vasc Surg. 2010;24:930–4. doi: 10.1016/j.avsg.2009.10.022. http://dx.doi.org/10.1016/j.avsg.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 8.Hakim KYK. Comparison of tumescent versus ultrasound guided femoral and obturator nerve blocks for treatment of varicose veins by endovenous laser ablation. Egyptian Journal of Anaesthesia. 2014;30:279–83. http://dx.doi.org/10.1016/j.egja.2014.01.008. [Google Scholar]
- 9.Yavaşçaoğlu B, Kaya FN, Özcan B, Uzunalioğlu S, Güven T, Yazıcı Ş, Ocakoğlu G. Erişkinlerde anestezi sonrası görülen komplikasyonların retrospektif değerlendirilmesi. Uludağ Üniversitesi Tıp Fakültesi Dergisi. 2009;35:73–8. [Google Scholar]
- 10.Doğru S, Kaya Z, Yılmaz Doğru H. Complications of spinal anaesthesia. J Contemp Med. 2012;2:127–34. [Google Scholar]
- 11.Koscielniak-Nielsen ZJ. Ultrasound-guided peripheral nerve blocks: what are the benefits? Acta Anaesthesiol Scand. 2008;52:727–37. doi: 10.1111/j.1399-6576.2008.01666.x. [DOI] [PubMed] [Google Scholar]
- 12.Kurt E, editor. Kısım 5. Bölüm: 35. Çeviri: Akkaya ÖT ve Yazıcıoğlu D. Ultrason eşliğinde Femoral Sinir Bloğu. Güneş Tıp Kitabevleri. 2. baskı. Hadzic Periferik siniri blokları ve Ultrason eşliğinde rejyonal Anestezi için Anatomi. Admir Hadzic; pp. S: 397–405. [Google Scholar]
- 13.Fingerman M, Benonis JG, Martin G. A practical guide to commonly performed ultrasound-guided peripheral-nerve blocks. Curr Opin Anaesthesiol. 2009;22:600–7. doi: 10.1097/ACO.0b013e32832f7643. http://dx.doi.org/10.1097/ACO.0b013e32832f7643. [DOI] [PubMed] [Google Scholar]
- 14.Wedel JD. Nerve blocks. In: Miller RD, editor. Anesthesia. 4th edition. Philadelphia: Churchill Livingstone; 2000. pp. 1520–48. [Google Scholar]