Abstract
Objective
To determine the effect of nursing guide application developed for the present study and to evaluate the Early Warning Scoring System (EWSS) in post-anaesthesia care unit (PACU).
Methods
The study was carried out as a randomised-controlled experimental study. The study sample comprised of 123 adult patients having thoracic and abdominal surgery between January 2011 and April 2011 in the Anaesthesiology and Reanimation Department of a training and research hospital. Patients were randomised during the pre-operative period; the patients who were followed-up according to the EWSS and a nursing guide constituted the study group (SG=63) and the patients whose EWSS score was calculated but routine follow-up in PACU was not intervened constituted the control group (CG=60).
Results
During the PACU, complications developed in in 34.92% of SG patients and in 30.00% of CG patients. Of the SG patients, 95.45% developing complications and of the CG patients, 22.22% developing complications were treated in the first 10 minutes, and it was determined that in 61.12% of CG patients, complications were not treated. There was a significant difference between the SG and CG patients in terms of treatment duration against complications (p<0.05).
Conclusion
The EWSS and nurse’s guide provides early determination and treatment of patients developing complications. Thus, it is recommended to use the EWSS and a nursing guide in PACU.
Keywords: Early warning scoring system, post-anaesthesia care, nurse’s guide, nursing interventions, high-risk patients
Introduction
The period in the post-anaesthesia care unit (PACU) is critical for the patients. During the PACU period, patients are continuously kept under the control of nurses. The aims of the nursing care during this period include monitoring patient until stable status can be achieved, determining the potential problems in addition to the problems resulted from the anaesthetic and surgical intervention, and applying an appropriate intervention (1–4). Patient’s vital functions may be improved rapidly, reliably, and as comfortable as possible by performing a careful and systematic assessment and timely intervention. The post anaesthetic care protocols, which have been developed by the Turkish Society of Anaesthesiology and Reanimation (TSAR) are being widely used in our country. The parameters that followed-up and recorded in PACU within the context of these protocols include heart rate and rhythm, arterial blood pressure, body temperature, depth, type, and respiratory rate, blood oxygen saturation level with pulse oximetry, pain, nausea and vomiting, level of consciousness and sedation, medications and their time of administration, name of the nurse, name of the physician who ordered the treatments, drug side-effects, fluid therapy and amount of the fluid administered, amount of urine, amount of drainage, and bleeding control (5).
The most common complications during PACU period include hypoxia, hypotension, hypertension, shock, bleeding, rhythm disturbances, nausea, vomiting, and changes in consciousness (1). The early identification of the patients at high risk not only allows immediate treatment but also accelerates recovery. In PACU patients, early detection of the potential complications may become possible by applying the scoring systems, which provide a systemic approach for assessment of patients with risks and helps early identification of patients with worsening clinical status (6, 7). The one among the scoring systems that have been developed for this purpose is the Early Warning Scoring System (EWSS) criteria (Table 1) (8–12). The EWSS is currently being used-by assessment of physiologic parameters of the patients (systolic blood pressure, body temperature, heart rate, respiratory rate, level of consciousness, blood oxygen saturation) - in surgical wards and emergency units of Europe and North America for early recognition of the critically ill patients and to help their early transfer to the intensive care unit (ICU) (3, 4, 6, 9, 13–15). This system improves patient care while reducing the rate of cardiac arrest and mortality, duration of critical care, and number of re-admission to ICU (16). The EWSS provides immediate intervention to patients with worsening clinical status by calling for the emergency team, which was comprised of one anaesthesiologist and one nurse. In the study of Gardner-Thorpe et al. (17), the EWSS and the derived algorithm allowed to make early diagnosis more accurately in the postoperative period.
Table 1.
Early Warning Scoring System (EWSS)
| Score | 3 | 2 | 1 | 0 | 1 | 2 | 3 |
|---|---|---|---|---|---|---|---|
| Heart rate | <40 | 40–50 | 51–100 | 101–110 | 111–129 | >130 | |
| Respiratory rate | <8 | 9–14 | 15–20 | 21–29 | >30 | ||
| Body temperature (°C) | <35 | 35–37.5 | >37.4–38.4 | >38.5 | |||
| Systolic blood pressure (mmHg) | <70 | 71–80 | 81–100 | 101–199 | >200 | ||
| Oxygen saturation | <92 | 92–94 | 94–96 | 96–100 | |||
| Respond to stimulus (AVPU scale) | Awake | Voice alert | Pain alert | Unresponsive |
The studies published within the last 20 years have revealed that the use of EWSS in intensive care, emergency, and surgery units is effective in terms of both evaluating the physiologic condition of patients and preventing the loss of time and labour of healthcare team (3, 4, 9–11, 13–16, 18). In one of the limited number of studies in our country, the association between the EWSS score and mortality rate was investigated and mortality rate was found to be higher in the patients with EWSS score ≥5 compared to those with EWSS ≤5 (19).
In another descriptive study conducted on the EWSS use in PACU, it was found that the EWSS use was helpful in identification of patients with worsening status (20).
There are a limited number of studies on systems that will be used by nursing staff and will help as a guidance calling for emergency team during the care period, which is a critical course following anaesthesia and where early management of the patients with worsening status is crucially important. To this end, our study was designed to be performed in PACU.
The aim of the present study was to determine the effect of nurse’s guide-which was developed for the present study - on the outcomes patients who were being assessed according to the EWSS criteria in PACU (Figure 1).
Figure 1.
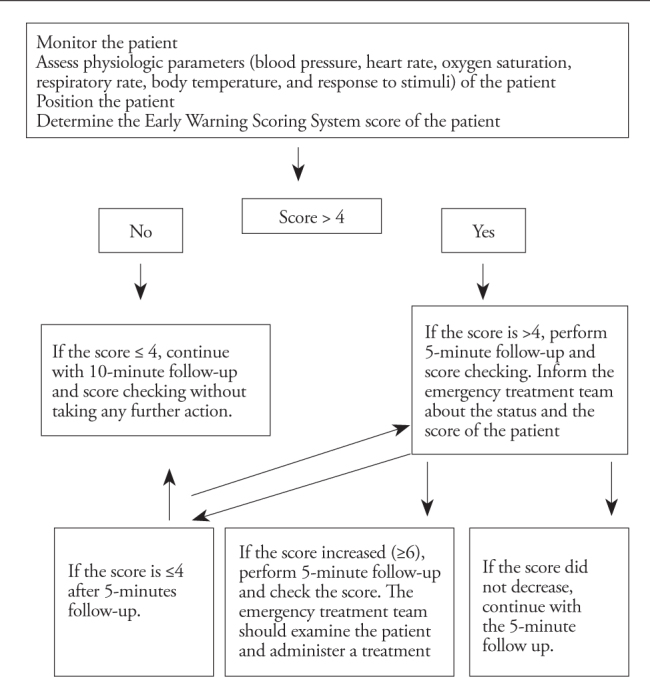
Nursing Guide used in the patients who were followed-up with Early Warning Scoring System in the post-anaesthesia care unit (adapted for the present study using the references 3, 22, 23)
Methods
Before initiating to the study, an approval from the Ethics Committee of Gülhane Military Medical Academy (decision number 1491–13, October 2010/160) was obtained. The present randomised-controlled study was performed in a PACU of anaesthesiology and reanimation department of a training and research hospital between January 2011 and April 2011. The study flow diagram was constituted by referring the recommended CONSORT guidelines (Figure 2) (21).
Figure 2.
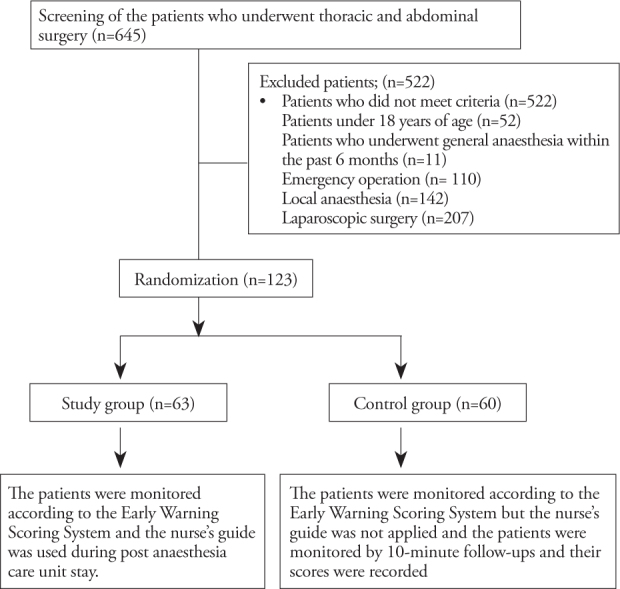
Study flow diagram
The population of the study was comprised of all patients who underwent thoracic and abdominal surgeries and followed-up in the PACU between the dates given above (n=645). The study population was comprised of the patients who were 18 years and over, volunteered to take part in the research, underwent abdominal or thoracic surgery under general anaesthesia, had no previous operations performed under general anaesthesia in the past 6 months, and had no life-threatening surgical complications during the operation (n=123). The patients were randomly allocated into the study (n=63) and control (n=60) groups by drawing lots (Figure 2).
The study data were collected in regard to preoperative, intraoperative, and postoperative periods. Within the scope of the present study, opinions and suggestions on the EWSS and nurse’s guide of the nurses working in the PACU were investigated.
The implementation of the study and data collection
Preoperative period
On the day before the operation, the investigators visited the patients who were deemed eligible for the study; they informed the patients about the study procedures and obtained their consent. The preoperative data (name-surname, gender, date of birth, education level, weight, height, medical diagnosis, previous operations, presence of chronic diseases, drug use, and the American Society of Anaesthesiologist (ASA) classification) were recorded during this visit. The randomisation of the patients was performed during the preoperative period. The patients were requested to draw one of the two sealed envelopes; one denoting the study group and the other denoting the control group. To achieve equal distribution of the patients to the groups, randomisation was performed after the total number of patients who would undergo the operation at the same day was determined. If the total number of the patients was 6 on a certain day and 3 of them drew the study group envelope, the rest of the patients were just allocated to the control group without drawing envelopes. The day after, the patients were followed in the PACU according to the allocated way of practice.
Intraoperative Period
After the patient was admitted to the PACU, the data regarding to the intraoperative period (surgical procedure, duration of anaesthesia, and complications related to anaesthesia) were obtained from the patient’s counselling chart and the doctor who performed anaesthesia to the patient.
Post-Anaesthesia Care Unit
These data were obtained after the patient was admitted to the PACU. The applications in the PACU and data collection tools were performed in four steps, as described below.
a) The EWSS score of the patients were calculated using Table 1.
The Ramsay Sedation scoring was performed using Table 2. The Ramsay sedation score was used to evaluate the patients’ level of sedation.
Table 2.
The Ramsay Sedation Score
| 1 | 2 | 3 | 4 | 5 | 6. |
|---|---|---|---|---|---|
| Anxious and restless | Cooperative and awake | Responding to verbal commands | Responding to mild stimulus | Responding to deep stimulus | Unresponsive to deep stimulus |
The nursing guide was used in the study (Figure 1). This guide was prepared for developing a standard in care by referring to the published literature and consulting experts’ opinion (3, 22, 23).
According to the study follow-up procedure, if the patient’s EWSS score was ≤4, a 10-minute follow-up was performed. If the EWSS score was 5, 5-minute follow up was performed; if the score did not change after the follow-up, 5-minute follow-ups were continued; however, if the score decreased to ≤4, 10-minute follow-up was performed. If the score increased, 5-minute follow-up was continued and the emergency team was called to evaluate the patient (the members of the emergency team were informed about the study).
b) Patients’ outcome registry form (included the duration of PACU stay, complications developing in the PACU, time to treatment for complications, and the treatments performed).
c) Checklist for interventions performed by the nurse (included tasks performed by the nurses such as recording of saturation, blood pressure, heart rate, respiration, body temperature, consciousness level, fluid balance, pain, positioning the patient, and drug administration).
d) A survey was used to obtain the opinions and suggestions of the nurses regarding the application of the EWSS and nursing guide.
The survey for nurses working in PACU about their opinion on the EWSS and nursing guide
-
Have you ever been informed about the Early Warning Scoring System?
If the answer is “yes”, where did you receive this information?
-
Please choose the most appropriate answer for you.
Applying the Early Warning Score System;
Is helpful in recognizing the patients with worsening status.
Made me feel safe
Made me feel that patients received care in safety
Is easy because it does not necessitate any invasion.
Decreased my workload.
Have you ever met any difficulties while applying the Early Warning Scoring System in PACU? Please explain
-
Please choose the most appropriate answer for you.
Applying the nurses’ guide;
Is directive
Made me feel safe
Decreased my workload
Made me feel that patients received care in safety
Is the nurses’ guide clear and apprehensible?
-
Do you think that the Early Warning Scoring System is appropriate for use in post-anaesthesia care unit?
If yes, why?
If no, why?
Your suggestions and comments.
All of the patients were scored according to the EWSS during the PACU period. The patients in the control group (CG) did not receive any intervention according to the nursing guide even if they had high scores. The patients in the study group (SG) received the necessary intervention as indicated in the nursing guide.
Nurses’ Implementations of the EWSS and Nnursing Guide in PACU
The investigator informed the nurses working at PACU about the EWSS and nursing guide and demonstrated its use to them. Accordingly, the nurses followed-up the study patients. They also filled-in the survey form in regard to their opinions about the use of EWSS and nurse’s guide.
Statistical Analysis
Descriptive statistics were expressed as numbers and percentages (%), minimum and maximum values, and mean ± standard deviation (X±SD). The comparison of parametric means was performed using Student’s t test and the comparison of percentages were performed using chi-square test. A p value of less than 0.05 was considered statistically significant.
Results
The patients in the study and control groups were similar in terms of descriptive features and no significant difference was found between the groups in terms of these features (p>0.05). There was a significant difference between the study and control groups in regard to the rate of previous operation (p<0.05) (Table 3).
Table 3.
Descriptive features of the study and control groups and their comparisons (n=123)
| Descriptive Features | Study Group (n=63) n |
% | Control Group (n=60) n |
% | p |
|---|---|---|---|---|---|
| Age groups | |||||
| 59 and below | 48 | 76.20 | 44 | 73.30 | 0.718* |
| 60 and above | 15 | 23.80 | 16 | 26.70 | |
| Gender | |||||
| Female | 26 | 41.26 | 23 | 38.33 | 0.739* |
| Male | 37 | 58.74 | 37 | 61.67 | |
| Education Level | |||||
| Elementary | 14 | 22.22 | 17 | 28.33 | 0.672* |
| High school | 24 | 38.09 | 23 | 38.34 | |
| University and higher | 25 | 36.96 | 20 | 33.33 | |
| BMI | |||||
| Normal | 33 | 52.38 | 28 | 46.67 | 0.520* |
| Overweight | 22 | 34.93 | 24 | 40.00 | |
| Obese | 8 | 12.69 | 8 | 13.33 | |
| Previous operations | |||||
| Present | 25 | 39.68 | 8 | 13.33 | 0.001* |
| Absent | 38 | 60.32 | 52 | 86.67 | |
| Diagnosis | |||||
| Cancer | 39 | 61.91 | 38 | 63.34 | 0.870* |
| Other | 24 | 38.09 | 22 | 36.66 | |
| Clinical Name | |||||
| General surgery | 37 | 58.73 | 36 | 60.00 | 0.868* |
| Thoracic surgery | 20 | 32.75 | 16 | 26.66 | |
| Gynaecology | 1 | 1.58 | 1 | 1.67 | |
| Urology | 5 | 7.94 | 7 | 11.67 | |
| ASA | |||||
| I | 45 | 71.43 | 48 | 80.00 | 0.185* |
| II | 15 | 23.80 | 12 | 20.00 | |
| III | 3 | 4.76 | 0 | 0 | |
| Chronic disease | |||||
| Present | 16 | 25.39 | 7 | 11.70 | 0.051* |
| Absent | 47 | 74.61 | 53 | 88.30 | |
| Number of chronic disease***** | |||||
| 1 | 11 | 68.75 | 5 | 71.44 | 0.963* |
| 2 | 3 | 18.75 | 1 | 14.28 | |
| 3 | 2 | 12.50 | 1 | 14.28 | |
| Continuous drug use | |||||
| Present | 15 | 23.81 | 6 | 10.00 | 0.079* |
| Absent | 48 | 76.19 | 54 | 90.00 | |
| Total | 63 | 100 | 60 | 100 | |
| Age | 45,23±18,59**** | 46,93±16,14**** | 0.574** | ||
| Min–Max:20–84 | Min–Max:19–77 | ||||
| BMI*** | 25,21±4,12**** Min–Max: 16,54–34,89 |
25,68±3,82**** Min–Max: 20,28–42,06 |
0,560** | ||
Chi-square- test,
Independent samples t test
Body Mass Index (BMI)
Mean, standard deviation
The percentage was calculated on the basis of the number of patients with chronic disease
Table 4 shows the comparison of the groups regarding the data on the PACU period. There were significant differences between the study and control groups with respect to the time to the treatment of complications and the duration of the PACU stay (p<0.05) (Table 4).
Table 4.
Data regarding the recovery period of the study and control patients (n=123)
| Data regarding recovery period | Study Group (n=63) n |
% | Control Group (n=60) n |
% | P |
|---|---|---|---|---|---|
| Complications | |||||
| Present | 22 | 34,92 | 18 | 30,00 | 0,560* |
| Absent | 41 | 65,08 | 42 | 70,00 | |
| Developing Complications*** | |||||
| Respiratory distress | 17 | 77,28 | 12 | 66,67 | 0,288* |
| Pain | 1 | 4,54 | 2 | 11,11 | |
| Hypotension | 1 | 4,54 | 2 | 11,11 | |
| Nausea and vomiting | 3 | 13,64 | 2 | 11,11 | |
| Time to treatment of complications (minutes) | |||||
| Untreated | 0 | 0 | 11 | 61,12 | <0,001* |
| 0–10 min | 21 | 95,45 | 4 | 22,22 | |
| 11 min and above | 1 | 4,55 | 3 | 16,66 | |
| Treatments administered to the complications | |||||
| Interventions for respiration | 14 | 63,63 | 2 | 28,57 | 0,202* |
| Drug+fluid therapy | 4 | 18,19 | 3 | 42,86 | |
| Drug therapy+positioning | 2 | 9,09 | 2 | 28,57 | |
| Examination request**** | 2 | 9,09 | 0 | 0 | |
| Recovery duration (minute) | 52,46±17,95*****
Range: 25–95 |
45,33±17,12*****
Range: 30–110 |
0,026** | ||
Chi-square- test,
Independent samples t test
The percentage was calculated on the basis of the number of patients developing complications.
Chest x-ray, arterial blood gas
Mean, standard deviation
Since the patients in the study group received treatment and 5-minute follow-up as well as they were not discharged from the PACU unless their EWSS scores decreased below 4, they had a longer time of the PACU stay.
At the time of admission to the PACU, the mean EWSS score of the study group was 5.06±1.13; whereas, it was 5.23±0.96 in the control group. Throughout the PACU stay, the mean EWSS of the study group was 4.41±0.73 whereas it was 4.63±0.84 in the control group (p>0.05). During discharge from the PACU, the mean EWSS of the study group was 3.79±0.74 whereas it was 4.21±1.10 in the control group; the difference was significant (p<0.05).
At the time of admission to the PACU, the mean Ramsay Sedation Score of the study group was 3.03±0.17 and 3.01±0.12 in the control group (p>0.05).
When the EWSS scores during the PACU stay were compared according to gender, the mean EWSS score was 4.64±0.79 in males and 4.33±0.75 in females; the difference was significant (p<0.05). There were no significant differences between the mean EWSS scores of the study and control groups in terms of age group, ASA classification, duration of anaesthesia, presence of chronic disease, and body-mass index (BMI) (p>0.05). There were also no significant differences between the mean EWSS scores of the groups during the discharge from the PACU regarding gender, age group, ASA classification, duration of anaesthesia, presence of chronic disease, and BMI (p>0.05).
There was a significant difference between the study and control groups in regard to the mean number of applications performed by nurses (saturation, heart rate, blood pressure, level of consciousness, pain follow-up, drug administration) (p<0.05) (Table 5).
Table 5.
Number of interventions performed by nurses in the post-anaesthesia care unit (n=123)
| Nurses’ interventions | Study group (n=63) ±SD** |
Control group (n=60) ±SD** |
test | p |
|---|---|---|---|---|
| Saturation monitoring | 8.04±3.53 | 5.48±1.73 | t*=5.063 | <0.001 |
| Heart rate monitoring | 8.04±3.53 | 5.48±1.73 | t*=5.063 | <0.001 |
| Blood pressure monitoring | 8.04±3.53 | 5.48±1.73 | t*=5.063 | <0.001 |
| Respiration monitoring | 8.04±3.53 | 5.48±1.73 | t*=5.063 | <0.001 |
| Body temperature monitoring | 8.04±3.53 | 5.48±1.73 | t*=5.063 | <0.001 |
| Consciousness monitoring | 8.04±3.53 | 5.48±1.73 | t*=5.063 | <0.001 |
| Fluid balance monitoring | 8.04±3.53 | 5.48±1.73 | t*=5.063 | <0.001 |
| Pain monitoring | 8.04±3.53 | 5.48±1.73 | t*=5.063 | <0.001 |
| Positioning | 1.06±1.26 | 1.00±1.02 | t*=1.615 | 0.109 |
| Drug administration | 1.06±1.26 | 1.08±0.96 | t*=2.557 | 0.012 |
| Calling for physician | 1.90±0.99 | 1.71±0.90 | t*=1.096 | 0.0275 |
Independent samples t test,
Mean, standard deviation
When the responses given by the nurses to the survey (mentioned in the methods section) on their opinions about the EWSS and the nursing guide analysed, all nurses (n=4) responded to “Applying the EWSS” as “is helpful in early recognizing the patients with worsening status”, three responded as “made me feel safe” and “made me feel that patients received care in safety”, two responded as “is easy because it does not necessitate any intervention” and “decreased my workload”, one responded as “increased my workload”. Three of the nurses mentioned that they did not meet any difficulties while applying the EWSS in PACU. In regard to the nursing guide survey, the answers to “Applying the guide” were as follows; three responded as “is directive”, two responded as “made me feel safe”, “decreased my workload”, and “made me feel that patients received care in safety”. All of the nurses (n=4) were in the opinion that the nursing guide was clear and apprehensible.
All the nurses (n=4) working at the post-anaesthesia care unit had the opinion that the EWSS was inappropriate for PACU. According to the responses of the nurses to the open-ended question “Why application of the EWSS and nursing guide were inappropriate for the use in PACU”, three nurses stated that the number of nurses working in the recovery room was insufficient and they had difficulty in 5-minute follow-up because of rapid patient turnover in the unit, two nurses stated that the patients had already received care in the post-anaesthesia care unit and that the patients were immediately treated when the monitors sound an alarm, one nurse said that long-term follow-up could not be performed because the mean duration of PACU stay was 30–70 minutes. When the responses of the nurses to the open-ended question about their suggestions on the EWSS and nursing guide were evaluated, all nurses (n=4) suggested that EWSS would be helpful if the number of nurses in PACU was sufficient and they also proposed that providing a close patient monitoring, its use might also contribute positively to the patients’ outcomes, not only in PACU but also in other intensive care units.
Discussion
In the present study, the use of the EWSS and nursing guide helped early detection of complications and allowed early treatment. According to the literature, the aim of the EWSS use is early recognition of the patients with worsening status and to make early intervention (3, 6, 9, 13–16, 18, 19, 22–24). It has been indicated that the EWSS allows the healthcare personnel to diagnose and follow-up patients for the purpose of preventing surgical death, to increase awareness of the requirements of critically ill patients, and to facilitate the early recognition of patients with high risk (3, 25). In the study of Goldhill et al. (13), the EWSS use was found to decrease the mortality by allowing early recognition of the worsening patient status by healthcare personnel. In the studies by Cuthbertson et al. (4) and Burgess et al. (10), the EWSS was used for early recognition and prevention of patients with worsening clinical status and warning healthcare personnel and found to be effective. In the literature, the EWSS use had also been found to be effective as an alerting tool in recognition of patients with high risk for worsening and those who necessitate further treatment (19, 26, 27). In the study of Mcarthur-Rouse et al. (11), the EWSS use was suggested to be important in the recognition of worsening patient status by healthcare personnel, identification of the patients with risks, and calling for physician to treat patients’ early. The studies in the literature also support our results that application of the EWSS and nursing guide was effective by providing early intervention to patients and we are in the opinion that using the EWSS and nursing guide in PACU would be helpful for early intervention to patients.
The patients, whom the EWSS was applied were followed-up by 5 minute intervals when the score was higher than 4 until achieving stable parameters. Then, they were transferred to the ward from the PACU. Thus, the duration of the PACU stay was longer in the patients who were received the EWSS and nursing guide but with lower scores.
Both the present study results and literature revealed that the use of EWSS and nursing guide had important contributions in recognising and treating complications earlier by providing closer monitoring of patients (3, 6, 9,13–17, 19, 22–24).
The nurses working in post-anaesthesia care unit were also had the opinion that the use of EWSS and nursing guide was helpful and made them feel safe. However, they emphasized that the number of nurses employed should be increased when establishing such a system (the ideal is one nurse per 24 hour for each patient, the accepted limit is one nurse for two patients, and the lower limit is one nurse for three patients) (28). Moreover, an emergency treatment team should be constituted to use this system. Performing education programs for all the healthcare personnel were concluded to be helpful to obtain positive feedback from nurses about the EWSS and nurse’ guide and to facilitate the application of the system in PACUs.
Study Limitions
The patients were followed-up during their PACU stay. Since post-operative 24-hour follow-up of the patients was not performed, the effectiveness of the EWSS and nursing guide and the mortality and morbidity rates of the study population could not be identified. The sample size was limited because the number of the patients was low during the study period and the follow-up of whole study participants was performed by one investigator. Since the healthcare personnel (except nurses)-did not receive training and, according to the hospital protocols, the emergency treatment team which was comprised of an anaesthesiologist and a nurse shifted on a daily basis, the team was explained each time when they were treating a patient with a high EWSS and thus, time to treatment of complications was increased. The participation of the nurses working at PACU was limited because of the high turnover of patients in that unit.
Conclusion
The use of the EWSS and nursing guide, when monitoring patients during their PACU stay had positive effects on outcomes and provided early recognition and treatment of the complications. The use of the EWSS and nursing guide are suggested to be also continued after the patient was transferred to ward from PACU and the follow-up should be maintained in this manner up to at least 24 hours after the operation.
Footnotes
Conflict of Interest
No conflict of interest was declared by the authors.
Financial Disclosure: N/A.
Peer-review: Externally peer-reviewed.
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Gülhane Military Medical Academy.
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Author Contributions
Concept - B.P., A.Y.; Design - B.P., A.Y.; Supervision - B.P., A.Y.; Funding - B.P., A.Y.; Materials - B.P.; Data Collection and/or Processing - B.P.; Analysis and/or Interpretation - B.P., A.Y.,; Literature Review - B.P., A.Y.; Writer - B.P., A.Y.; Critical Review - B.P., A.Y.; Other - B.P., A.Y.
References
- 1.Özbayır T. Ameliyat Dönemi Bakımı. In: Aslan FE, Karadakovan A, editors. Dahili ve Cerrahi Hastalıklarda Bakım. Birinci basım. Adana: Özyurt Matbaacılık; 2010. pp. 314–6. [Google Scholar]
- 2.Smeltzer SC, Bare BG, Hinkle JL, Cheever KH. Postoperatif Care. In: Surrena H, editor. Brunner and Suddarth’s Textbook of Medical-Surgical Nursing. 12 edition. USA: Lippincott Williams and Wilkins Press; 2010. p. 393. [Google Scholar]
- 3.Sharpley JT, Holden JC. Introducing an early warning scoring system in a district general hospital, british association of critical care nurses. Nurs Crit Care. 2004;9:98–103. doi: 10.1111/j.1362-1017.2004.0063.x. http://dx.doi.org/10.1111/j.1362-1017.2004.0063.x. [DOI] [PubMed] [Google Scholar]
- 4.Cuthbertson BH, Boroujerdi M, McKie L, Aucott L, Prescott G. Can physiological variables and early warning scoring systems allow early recognition of the deteriorating surgical patient? Crit Care Med. 2007;35:402–9. doi: 10.1097/01.CCM.0000254826.10520.87. http://dx.doi.org/10.1097/01.CCM.0000254826.10520.87. [DOI] [PubMed] [Google Scholar]
- 5.Türk Anesteziyoloji ve Reanimasyon Derneği. Anestezi Uygulama Kılavuzları. Postanestezik Bakım. 2005. Web sitesi: http://www.tard.org.tr/kilavuz/2.pdf.
- 6.Paterson R, MacLeod DC, Thetford D, Beattie A, Graham C, Lam S, et al. Prediction of in-hospital mortality and length of stay using an early warning scoring system: clinical audit. Clin Me d. 2006;6:281–4. doi: 10.7861/clinmedicine.6-3-281. http://dx.doi.org/10.7861/clinmedicine.6-3-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tucker KM, Brewer RB, Demeritt B, Vossmeyer MJ. Prospective evaluation of a pediatric inpatient early warning scoring system. JSPN. 2009;14:79–85. doi: 10.1111/j.1744-6155.2008.00178.x. [DOI] [PubMed] [Google Scholar]
- 8.Finch A, Lambert MJ, Schaalje BG. Psychotherapy quality control: the statistical generation of expected recovery curves for integration into an early warning system. Clin Psych Psychother. 2001;8:231–42. http://dx.doi.org/10.1002/cpp.286. [Google Scholar]
- 9.Goldhill DR, McNarry AF. Physiological abnormalities in early warning scores are related to mortality in adult inpatients. Br J Anaesth. 2004;92:882–4. doi: 10.1093/bja/aeh113. http://dx.doi.org/10.1093/bja/aeh113. [DOI] [PubMed] [Google Scholar]
- 10.Burgess LP, Herdman TH, Berg BW, Feaster WW, Hebsur S. Alarm limit settings for early warning systems to identify at-risk patients. J Adv Nurs. 2009;65:1844–52. doi: 10.1111/j.1365-2648.2009.05048.x. http://dx.doi.org/10.1111/j.1365-2648.2009.05048.x. [DOI] [PubMed] [Google Scholar]
- 11.Mcarthur-Rouse F. Critical care outreach services and early warning scoring systems: a review af the literature. J Adv Nurs. 2001;36:696–704. doi: 10.1046/j.1365-2648.2001.02020.x. http://dx.doi.org/10.1046/j.1365-2648.2001.02020.x. [DOI] [PubMed] [Google Scholar]
- 12.McCabe A, Duncan H, Heward Y. Pediatric early warning systems: where do we go from here? Pediatr Nurs. 2009;21:14–7. doi: 10.7748/paed2009.02.21.1.14.c6907. [DOI] [PubMed] [Google Scholar]
- 13.Goldhill DR, McNarry AF, Mandersloot G, McGinley A. A physiologically-based early warning score for ward patients: the association between score and outcome. Anaesthe sia. 2005;60:547–53. doi: 10.1111/j.1365-2044.2005.04186.x. http://dx.doi.org/10.1111/j.1365-2044.2005.04186.x. [DOI] [PubMed] [Google Scholar]
- 14.Tarassenko L, Hann A, Young D. Integrated monitoring and analysis for early warning of patient deterioration. Br J Anaesth. 2006;97:64–8. doi: 10.1093/bja/ael113. http://dx.doi.org/10.1093/bja/ael113. [DOI] [PubMed] [Google Scholar]
- 15.Cuthbertson BH, Smith GB. A warning on early-warning scores! Br J Anaesth. 2007;98:704–6. doi: 10.1093/bja/aem121. http://dx.doi.org/10.1093/bja/aem121. [DOI] [PubMed] [Google Scholar]
- 16.Duckitt RW, Buxton-Thomas R, Walker J, Cheek E, Bewick V, Venn R, et al. Worthing physiological scoring system: derivation and validation of a physiological early-warning system for medical admissions. An observational, population-based single-centre study. Br J Anaesth. 2007;98:769–74. doi: 10.1093/bja/aem097. http://dx.doi.org/10.1093/bja/aem097. [DOI] [PubMed] [Google Scholar]
- 17.Gardner-thorpe J, Love N, Wrıghtson J, Walsh S, Keelıng N. The value of modified early warning score (mews) in surgical in-patients: a prospective observational study. Ann R Coll Surg Engl. 2006;88:571–5. doi: 10.1308/003588406X130615. http://dx.doi.org/10.1308/003588406X130615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morgan RJ, Williams F, Wright MM. An Early Warning score for the early detection of patients with impending illness. Clin Int Care. 1997;8:100. [Google Scholar]
- 19.Armağan E, Yılmaz Y, Ölmez ÖF, Şimşek G, Gül CB. Predictive value of the modified early warning score in a Turkish emergency department. Eur J Emerg Med. 2008;15:338–40. doi: 10.1097/MEJ.0b013e3283034222. http://dx.doi.org/10.1097/MEJ.0b013e3283034222. [DOI] [PubMed] [Google Scholar]
- 20.Doğru AG, Yava A, Bilgin F, Çiçek H, Tosun N. The use of the early warning score system in assessment of patients in post anesthesia care unit. 23rd ESICM Annual Congress; Barcelona, Spain. 2010. p. 182. Congres abstract book. [Google Scholar]
- 21.Schulz KF, Altman DG, Moher D For the Consort Group. CONSORT 2010 Statement: updated guidelines for reporting paralel group randomised trials. BMJ. 2010:332–40. doi: 10.3736/jcim20100702. http://dx.doi.org/10.1136/bmj.c332. [DOI] [PubMed] [Google Scholar]
- 22.Smith GB, Osgood VM, Crane S. ALERTTM Course development group, ALERTTM - A multiprofessional training course in the care of the acutely ill adult patient resuscitation. Resusc itation. 2002;52:281–6. doi: 10.1016/s0300-9572(01)00477-4. http://dx.doi.org/10.1016/S0300-9572%2801%2900477-4. [DOI] [PubMed] [Google Scholar]
- 23.Ridley S. The recognition and early management of critical illness. Ann R Coll Surg Engl. 2005;87:315–22. doi: 10.1308/003588405X60669. http://dx.doi.org/10.1308/003588405X60669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quarterman CP, Thomas AN, McKenna M, McNamee R. Use of a patient information system to audit the introduction of modified early warning scoring. J Eval Clin Pract. 2005;11:133–8. doi: 10.1111/j.1365-2753.2005.00513.x. http://dx.doi.org/10.1111/j.1365-2753.2005.00513.x. [DOI] [PubMed] [Google Scholar]
- 25.Goldhill DR. Preventing surgical deaths: critical care and intensive care outreach services in the postoperative period. Br J Anaesth. 2005;95:88–94. doi: 10.1093/bja/aeh281. http://dx.doi.org/10.1093/bja/aeh281. [DOI] [PubMed] [Google Scholar]
- 26.Baines E, Kanagasundaram NS. Early warning scores, How do you know when patients are so ill that it’s time to act? Student BJM. 2008;16:320–1. [Google Scholar]
- 27.McGaughey J, Blackwood B, O’halloran P, Trinder TJ, Porter S. Realistic Evaluation of early warning systems and the acute life threatening events-recognition and treatment training course for early recognition and management of deteriorating ward-based patients: research proto col. J Adv Nurs. 2010;66:923–32. doi: 10.1111/j.1365-2648.2009.05257.x. http://dx.doi.org/10.1111/j.1365-2648.2009.05257.x. [DOI] [PubMed] [Google Scholar]
- 28.Yoğun bakım dergisi. Yoğun bakım serüveni: Dün Bugün. Web site: http://www.yogunbakimderg.com/sayilar/8/buyuk/6-12.pdf.


