Abstract
BACKGROUND AND OBJECTIVE:
Although children with isolated skull fractures rarely require acute interventions, most are hospitalized. Our aim was to safely decrease the hospitalization rate for children with isolated skull fractures.
METHODS:
We designed and executed this multifaceted quality improvement (QI) initiative between January 2008 and July 2015 to reduce hospitalization rates for children ≤21 years old with isolated skull fractures at a single tertiary care pediatric institution. We defined an isolated skull fracture as a skull fracture without intracranial injury. The QI intervention consisted of 2 steps: (1) development and implementation of an evidence-based guideline, and (2) dissemination of a provider survey designed to reinforce guideline awareness and adherence. Our primary outcome was hospitalization rate and our balancing measure was hospital readmission within 72 hours. We used standard statistical process control methodology to assess change over time. To assess for secular trends, we examined admission rates for children with an isolated skull fracture in the Pediatric Health Information System administrative database.
RESULTS:
We identified 321 children with an isolated skull fracture with a median age of 11 months (interquartile range 5–16 months). The baseline admission rate was 71% (179/249, 95% confidence interval, 66%–77%) and decreased to 46% (34/72, 95% confidence interval, 35%–60%) after implementation of our QI initiative. No child was readmitted after discharge. The admission rate in our secular trend control group remained unchanged at 78%.
CONCLUSIONS:
We safely reduced the hospitalization rate for children with isolated skull fractures without an increase in the readmissions.
Approximately 500 000 children visit the emergency department (ED) annually for evaluation of head trauma, resulting in nearly 50 000 admissions and $1 billion in health care expenditures.1–4 Among children with minor head trauma and abnormal neuroimaging, skull fractures are the most common traumatic finding.5–7 Children with isolated skull fractures, defined as a skull fracture without intracranial hemorrhage, are at exceedingly low risk for clinical decompensation.8–12 Despite this low risk, hospitalization rates for children with isolated skull fractures approaches 80% nationally.8 Because hospitalization is associated with increased cost,8 as well as the potential for medication errors13 and nosocomial infections,14 children should be hospitalized only when indicated. Although some children with isolated skull fractures may require hospital admission for on-going symptoms or evaluation of nonaccidental trauma,15–18 outpatient care with close follow-up is a safe option for many.10
At our study institution, the baseline hospitalization rate for children with isolated skull fractures was similar to the national average.8 We hypothesized that we could safely reduce hospitalization rates without impacting quality of care. Our quality improvement (QI) aim was to reduce hospital admissions for isolated skull fractures by at least 20% over a 2-year period.
Methods
Setting
We performed this study in the ED of a tertiary care children’s hospital with ∼60 000 ED visits annually and a level 1 trauma center designation. The ED is staffed by board-certified pediatric emergency medicine physicians, general pediatricians, and pediatric emergency medicine fellows as well as pediatric and emergency medicine residents. Pediatric neurosurgical consultation is available 24 hours a day, 7 days a week at the discretion of the ED providers.
Study Design
We designed and executed a multifaceted QI initiative to decrease hospital admissions for children with isolated skull fractures between January 2008 and July 2015. We measured the impact of this QI initiative on rates of hospitalization for children with isolated skull fractures. Starting on August 1, 2013, we obtained informed consent from a parent or guardian to perform a single telephone follow-up. The institutional review board at Boston Children’s Hospital approved the study protocol.
Study Patients
We included children ≤21 years of age who presented to the ED with minor blunt head trauma and an arrival Glasgow Coma Score ≥14. We identified all children with an ED discharge diagnosis of skull fracture (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes 800.00–800.09). We performed manual medical record review to confirm eligibility. We defined an isolated skull fracture as a fracture of the skull calvarium without concurrent intracranial injury or hemorrhage. We included skull fractures diagnosed by computed tomography (CT) scan or skull radiograph, even if imaging was performed before ED arrival. We included skull fractures diagnosed clinically (without additional neuroimaging) if concern for intracranial hemorrhage was low. We included children with other minor injuries that did not require hospitalization (eg, simple lacerations or uncomplicated extremity fractures). We excluded children with injuries that would require inpatient care, such as solid organ injuries, as well as children with skull fractures depressed greater than the table-width of the skull.
Data Collection
We reviewed the medical record of all eligible patients and abstracted clinical and demographic factors as well as patient management, including neuroimaging with results, specialty consultations, surgical interventions, and ED disposition. We reviewed all return visits within 72 hours of the index ED visit. Beginning on August 1, 2013, we performed a single standardized telephone follow-up 2 weeks after initial evaluation for children without suspected or confirmed child abuse whose caregivers had provided informed consent to assess the need for subsequent rehospitalization.
Outcome Measure
Our primary outcome was admission to a medical or surgical hospital service (including observation status) from the ED. Our balancing measure was hospital readmission, defined as a return to the ED with subsequent hospital admission (as defined above) within 72 hours of the index ED visit.
Intervention
Planning the Intervention
We designed a QI initiative for children with an isolated skull fracture as part of a larger effort to improve the care of children with minor blunt head trauma in the context of an ED quality program.19 The objective of this program is the creation and implementation of local, evidence-based guidelines for common conditions and rare conditions with significant morbidity and mortality. The goals of these guidelines are to increase evidence-based care and decrease care variability. The aim of our skull fracture QI initiative was to reduce hospital admissions by at least a 20% absolute reduction from baseline and to sustain this reduction. Because there was no benchmark admission rate, we chose 20% as a meaningful, but obtainable goal.
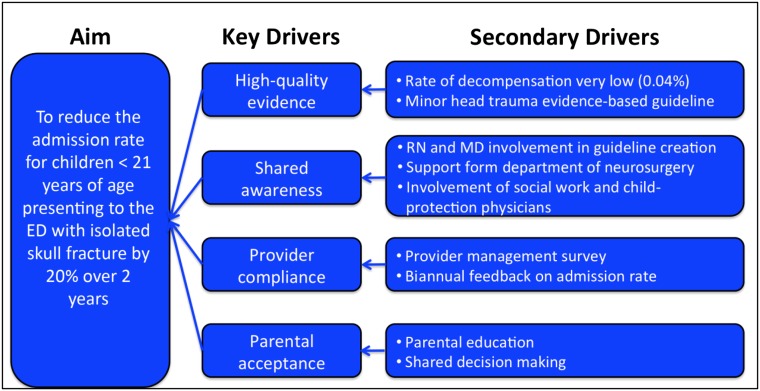
Key Drivers
To this end, we identified the following key drivers of care in the following domains: high quality evidence, provider compliance, shared awareness, and parental acceptance (Fig 1). We identified key drivers through brainstorming with stakeholders. We targeted these key drivers in our 2 QI interventions.
FIGURE 1.
Key driver diagram.
Evidence-Based Guideline
First, we developed and implemented an evidence-based guideline for the management of children with minor head trauma that included specific guidelines for the management of isolated skull fractures (Supplemental Fig 5). Routine neurosurgical consultation was not suggested. Social work evaluation was recommended for any child when there was concern for nonaccidental trauma, especially for children under 2 years of age. The guideline recommended that children with a normal mental status, a nonfocal neurologic examination, no on-going symptoms, and low concern for nonaccidental trauma should be discharged from the ED with close primary care follow-up. Although the published evidence does not support differential management,12 we recognized the difficulties in assessment of the youngest infants with skull fractures. This, coupled with analysis of provider acceptability, led to suggested hospitalization for infants under 2 months of age, although we included children of all ages in our analyses.
We developed the evidence-based guideline in an iterative process with involvement of key stakeholders from multiple disciplines, including ED physicians and nurses, neurosurgeons, and social workers. After initial development, we held educational conferences for divisional faculty, fellows, and nursing, highlighting current evidence as well as institutional experience. Feedback from this session was then used to refine the guideline. In October 2011, the guideline was made available in all of the patient-care areas, in an easily accessible online library, and nested within the electronic medical record “Minor Head Trauma” order-set used to order neuroimaging studies. To reinforce awareness of, and compliance with, this guideline, we held multiple educational initiatives, sent electronic reminders, and provided biannual department-wide updates.
Provider Survey
We designed a survey to be completed by every ED attending provider caring for a child with an isolated skull fracture. Starting in August 1, 2013, attending providers were surveyed at the time of admission regarding decision-making. We developed the survey to reinforce awareness of the evidence-based guideline, increase guideline adherence, and understand barriers to guideline adherence while identifying focus areas for future QI efforts.
Methods of Evaluation and Statistical Analyses
First, we compared the patients presenting in the preimplementation period (January 1, 2008–September 30, 2011) to those in the postimplementation period (October 1, 2011–June 30, 2015). We used χ2 analyses for categorical variables and Mann–Whitney tests for continuous variables.
We used standard QI science statistical methods to monitor the impact of our QI interventions on hospital admission rates over time. We used a p-chart with control limits set at 3 σ.20 Given the number of children with isolated skull fractures, we selected a quarter of a year (ie, 3 months) as our primary unit of time. We used standard statistical process control methods to determine if changes in hospitalization rates were attributed to natural variation (ie, common cause variation) or the result of our interventions (ie, special cause variation). Second, we used a cumulative summation (CUSUM) chart to examine the effect of our initiative on the total number of admissions prevented. The CUSUM methodology allows detection of small changes in outcomes over time, much earlier than they would be detectable by using standard process control methods.21 We chose this methodology given the infrequent nature of isolated skull fractures and our desire to rapidly assess the effectiveness of our interventions.
Next, we investigated whether national hospital admission rates for children with isolated skull fractures had changed over the study period. For this comparison, we used the Pediatric Health Information System, an administrative database that contains inpatient, ED, ambulatory surgery, and observation encounter–level data from >45 tertiary care pediatric hospitals.8,22 For this study, data from 37 hospitals that provided reliable ED data for each of the years in the study period (2008–2015) were included. We identified all children ≤21 years of age with an ED primary diagnosis code of skull fracture (utilizing the same ICD-9-CM codes as above) without a concurrent diagnosis code for intracranial injury (ICD-9-CM codes 800.1–800.9X and 801.X–804.X).8 Using a general estimating equation with clustered robust SEs to adjust for study center, we compared trends over the study period in hospital admission rates after adjusting for patient age.
We used ChartRunner Lean (version 3.0; PQ Systems, Dayton, OH) for creation of the statistical process control charts and Stata (version 12; Stata Corp, College Station, TX) for the CUSUM charts. We used SPSS (version 22.0; IBM SPSS Statistics, IBM Corporation, Armonk, NY) for other analyses.
Results
We identified 438 children who presented with a skull fracture, of whom 117 (27%) were excluded after manual medical record review. Among the 321 included children, 183 (57%) presented during 1 of the 18 preimplementation quarters and 138 (43%) presented during 1 of the 15 postimplementation quarters.
First, we compared the demographic and clinical characteristics of children presenting in the preimplementation and postimplementation periods (Table 1). In the postimplementation period, fewer children had public insurance. As recommended by the evidence-based guideline, the frequency of neurosurgical consultations decreased in the postimplementation period. The proportion of children with an isolated skull fracture who had evaluation by the social work or child protective teams was unchanged.
TABLE 1.
Comparison of Patient Characteristics Between the Preimplementation and Postimplementation Periods
| Characteristic | Preimplementation Period (N = 183), n (%) | Postimplementation Period (N = 138), n (%) | P |
|---|---|---|---|
| Patients per quarter, median (IQR) | 10 (7–14) | 10 (5–11) | .61 |
| Demographics | |||
| Age (mo), median (IQR) | 10 (5–26) | 11 (6–43) | .28 |
| Male | 110 (60) | 81(59) | .82 |
| Race | |||
| White | 142 (78) | 77 (56) | <.001 |
| Black | 9 (5) | 9 (6) | |
| Other/unknown | 32 (17) | 52 (38) | |
| Public insurance | 80 (44) | 46 (33) | .038 |
| Transferred from another hospital | 96 (53) | 67 (49) | .27 |
| Radiologic method of diagnosisa | |||
| Cranial CT scan | 171 (96) | 130 (94) | .50 |
| Skull radiograph | 25 (14) | 14 (11) | .27 |
| Cranial MRI | 0 (0) | 1 (1) | .27 |
| Consultations | |||
| Neurosurgery | 136 (74) | 75 (54) | <.001 |
| Social work/child protection | 57 (31) | 42 (30) | .50 |
| Skeletal survey performed | 21 (12) | 14 (10) | .42 |
IQR, interquartile range.
Some children had >1 type of imaging study.
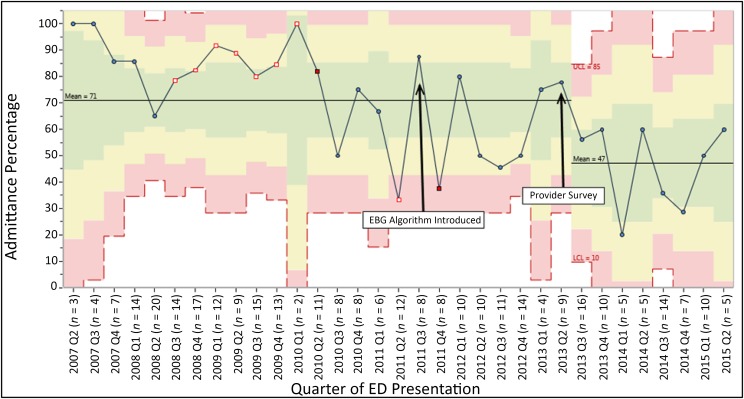
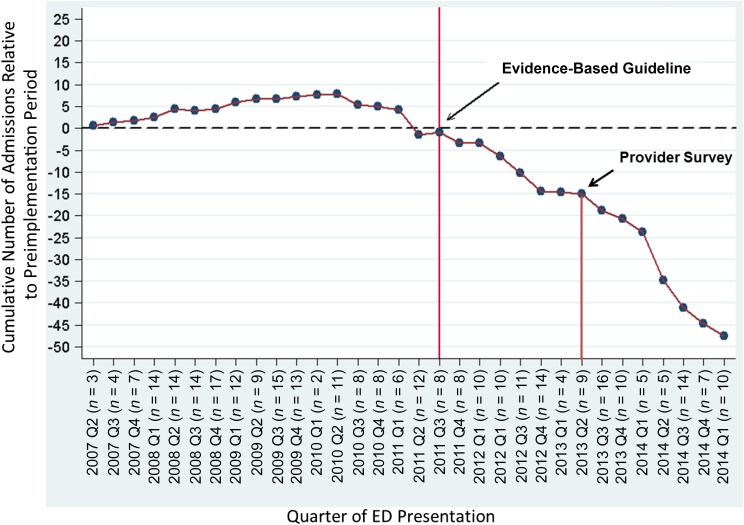
We next examined hospital admission rates over time. Baseline hospital admission rate at our hospital was 71% (95% confidence interval, 66%–77%). Using standard statistical process control methodology, the hospital admission rate did not show special cause variation immediately after guideline implementation; however, we observed a 24% reduction after the addition of the provider survey (Fig 2). Analysis by the CUSUM method shows that hospital admissions began to decline immediately after implementation of the guideline, and this trend continued over the study period, leading to 48 potential admissions avoided (Fig 3). Overall, admission rates were similar for children across age groups (58% for <2 years vs 61% for ≥2 years, P = .18).
FIGURE 2.
Statistical process control chart (p-chart) showing the hospital admission rate for children with isolated skull fracture over the study period.
FIGURE 3.
CUSUM: hospital admissions prevented over time.
After beginning our second QI intervention, we completed telephone follow-up interviews with parents/guardians of 54 of the 75 (72%) eligible children with an isolated skull fracture. Using a combination of medical record review and telephone follow-up, we did not identify any child who required hospital readmission or neurosurgical intervention.
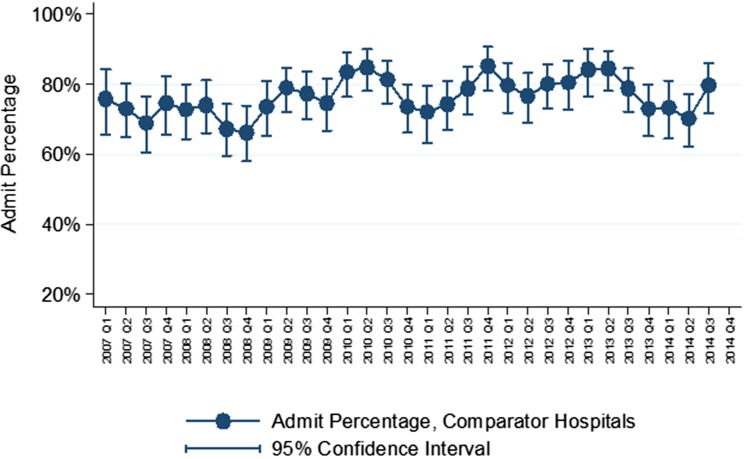
To evaluate for secular trends, we examined hospital admission rates for children with isolated skull fractures presenting to the ED of 37 comparative pediatric hospitals (Fig 4). After clustering by hospital, we found no change in hospital admission rates at comparator hospitals over time (adjusted odds ratio 1.01; 95% confidence interval 0.99–1.04).
FIGURE 4.
Trends in quarterly hospital admission rate for children with isolated skull fractures at Boston Children’s Hospital and the 37 other hospitals contributing to the Pediatric Health Information System administrative database.
Finally, we report the indications for hospital admission collected on the attending provider survey (Table 2). Young age was the most common primary indication, followed by request by a medical or surgical consulting service. Child protective or social concerns were the primary indication for hospital admission in 9% of patients. Although admission rates for patients transferred to our ED decreased between the preimplementation and postimplementation period (84% vs 59%, P = .001), transfer with expectation of admission was the primary indication for admission in 29% of children in the postimplementation period. Taken together, the primary indication for admission diverged from our evidenced-based guideline for 25% of children.
TABLE 2.
Indications for Hospital Admission for 45 Patients Admitted After Implementation of the Evidence-Based Guideline With Completed Provider Surveys
| Primary Indication for Hospital Admission, N (%) | Additional Indications for Hospital Admission, N (%)a | |
|---|---|---|
| Young age | 11 (24) | 5 (11) |
| Consultant request | 10 (22) | 10 (22) |
| Persistent symptoms | 6 (13) | 5 (11) |
| Concern for hemorrhage on imagingb | 4 (9) | 1 (2) |
| Transfer with expectation of admission | 4 (9) | 9 (20) |
| Social or child protection concerns | 4 (9) | 5 (11) |
| Clinical concern | 3 (7) | 3 (6) |
| Otherc | 3 (3) | 3 (6) |
| No follow-up available | 1 (2) | 0 (0) |
| Family or patient preference | 1 (2) | 2 (4) |
| Concern for clinical deterioration | 0 (0) | 12 (26) |
| Distance from hospital | 0 (0) | 4 (9) |
Numbers total >100% as patients can have >1 additional indication for hospital admission.
Ultimately determined on final report not to be a hemorrhage by neurosurgery or attending neuroradiologist.
Other indicates included: question of open fracture, concern for cerebrospinal fluid leak, question of cranial nerve palsy, for MRI, worrisome mechanism and > 1 fracture.
Discussion
We designed and implemented a QI initiative for the management of children with isolated skull fracture in a single pediatric trauma center. Our QI efforts were associated with an ∼25% reduction in hospital admissions without a concurrent increase in 72-hour readmission rates. Admission rates for children with isolated skull fractures at other similar pediatric institutions over the same time period remained constant, supporting the conclusion that the reduction we observed was due to our QI efforts and not the result of a national secular trend. One-quarter of children admitted for isolated skull fractures meet criteria for outpatient management, suggesting further reductions in hospital admission rates may be possible.
Most children hospitalized for isolated skull fracture are discharged within 24 hours, and few require any acute interventions.8–12 Among children with isolated skull fractures who had repeat neuroimaging, few had additional traumatic findings12 and none required further neurosurgical intervention.9,12 Similar to previously published data, none of the children in our study required any acute interventions, and the majority of hospitalized children were discharged the following day. The direct health care cost to care for a child with an isolated skull fracture is significantly higher for children who are hospitalized when compared with those who are discharged.8 Although we did not perform a cost-effectiveness analysis, a reduction in hospital admission rates could significantly reduce the costs to care for children with isolated skull fractures.
The baseline hospitalization rate at the study institution was similar to the national average (80% at pediatric centers).8 Recent studies have reported a slightly lower admission rate, but excluded children transferred to a tertiary hospital after neuroimaging was performed.12 Approximately half of our patients were transferred to the study site ED with neuroimaging obtained at the referring institution. Parental and provider expectations often impact the subsequent care at the referral center.23
Clinicians caring for children with isolated skull fractures must carefully consider the possibility of nonaccidental trauma. The American Academy of Pediatrics recommends hospitalization for children undergoing evaluation and treatment of suspected abuse or neglect.24 However, reported rates of inflicted injury among children with an isolated skull fracture vary widely.15–18,25,26 Many children with isolated skull fractures do not undergo further evaluation for nonaccidental trauma, and additional fractures are identified in only a small fraction of those undergoing skeletal survey.16,17,26 Importantly, the majority of children with confirmed nonaccidental trauma were under 6 months of age, with at least 1 concerning factor on history and physical examination. Red flags for child abuse include delays in seeking care, unknown injury mechanism, changing history, bruises, or complex skull fracture.16,17 Although children with suspected inflicted injury require additional child protective evaluation, children with an isolated skull fracture and no red flags may be safely managed without hospital admission.
We learned many valuable lessons from our QI efforts that may be generalizable to other centers. First, as children with isolated skull fractures are encountered relatively infrequently, robust, locally-sensitive implementation of an evidence-based guideline may be an effective way to change practice, as individual provider clinical experience may be limited. In a previous study of 88 children with isolated skull fractures, the introduction of an evidence-based guideline was associated with a reduction in hospital admissions.27 Second, involvement of key stakeholders from all of the typically involved clinical disciplines improved the uptake of the new guideline. For our guideline, we involved individuals from nursing, neurosurgery, and social work to gain critical support for standardizing care for these patients. Third, we learned the importance of frequent updates and ongoing provider education about the care of children with infrequent conditions. Lastly, we also note the value of using complimentary QI tools for analysis. The addition of the CUSUM methodology allowed us to detect improvement earlier in the initiative.
Importantly, implementation of our QI initiative was not without challenges. First, during guideline development, key stakeholders expressed concerns about discharging the youngest infants with skull fractures. We modified the guideline to suggest routine admission for these infants to increase provider acceptance of the guideline. Second, the skull fracture QI initiative was embedded in a minor head trauma guideline (on the second page), which focused on initial CT decision-making.28 Because isolated skull fractures occur much less commonly than minor blunt head trauma, increasing provider awareness of the guidelines for children with isolated skull fractures created a challenge. Once we identified this barrier (the second page effect), we held focused educational sessions for the providers, increased frequency of electronic reminders, and designed a provider survey to increase awareness of the skull fracture guideline. We developed the provider survey to reinforce and increase guideline awareness of the evidence-based guideline. Additionally, data gathered from the provider survey are being used to understand barriers to practice change while identifying focus areas for future interventions.
Our study has limitations. First, because our QI initiative occurred at a single center, our results might not be generalizable to other EDs. Because our institution has a robust ED-based QI program with considerable provider buy-in, implementation of a similar program outside of this context may be more challenging. Second, because we did not perform telephone follow-up interviews for all study patients, we relied on medical record review to identify hospital readmissions. Although we may have missed children who returned to an alternate hospital, no child reached by telephone follow-up sought care at another hospital. Third, we are unable to determine whether any discharged children with isolated skull fractures had undetected child abuse. However, the rate of child protective evaluations and of skeletal surveys was unchanged, suggesting continued provider vigilance. Lastly, although no child with an isolated skull fracture required neurosurgery, our study was not powered to detect these rare events. However, in a previous examination of almost 4000 children with isolated skull fractures, only 1 required neurosurgery, demonstrating the rarity of these events.8
Conclusions
We created and implemented a multifaceted QI initiative that included an evidence-based guideline developed with key stakeholder collaboration as well as a provider survey. Through this initiative, we safely reduced hospital admissions rates for children with isolated skull fractures without an increase in hospital readmission.
Glossary
- CT
computed tomography
- CUSUM
cumulative summation
- ED
emergency department
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- QI
quality improvement
Footnotes
Dr Lyons conceptualized and designed the study, oversaw data collection and analyses, and wrote the first draft of the manuscript; Dr Stack conceptualized and designed the quality improvement initiative, oversaw quality improvement efforts, aided in data analysis and interpretation, and reviewed and revised the manuscript; Dr Monuteaux carried out data analyses, including comparator analyses from the Pediatric Health Information Systems database, performed statistical analyses, and reviewed and revised the manuscript; Ms Parver carried out data analyses, including creation and revision of process control charts and cumulative summation charts, performed statistical analyses with Dr Monuteaux, and reviewed and revised the manuscript; Ms Catherine Gordon and Ms Caroline Gordon carried out data collection, including performing the provider survey and patient follow-up calls, and reviewed and revised the manuscript; Dr Proctor aided in the design of the quality improvement initiative and study design, providing expert neurosurgical input, and reviewed and revised the manuscript; Dr Nigrovic designed the quality improvement initiative and study, supervised data collection and interpretation, drafted and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This project was supported by a grant from the Provider Payer Quality Initiative foundation at Boston Children’s Hospital. Dr. Lyons was supported by an NIH T32 Training Grant (5T32HD040128-12). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control Traumatic brain injury in the United States: Assessing outcomes in children. Available at: www.cdc.gov/ncipc/tbi/tbi_report/index.htm. Accessed July 1, 2013
- 2.Rutland-Brown W, Langlois JA, Thomas KE, Xi YL. Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006;21(6):544–548 [DOI] [PubMed] [Google Scholar]
- 3.Schutzman SA, Greenes DS. Pediatric minor head trauma. Ann Emerg Med. 2001;37(1):65–74 [DOI] [PubMed] [Google Scholar]
- 4.Schneier AJ, Shields BJ, Hostetler SG, Xiang H, Smith GA. Incidence of pediatric traumatic brain injury and associated hospital resource utilization in the United States. Pediatrics. 2006;118(2):483–492 [DOI] [PubMed] [Google Scholar]
- 5.Quayle KS, Jaffe DM, Kuppermann N, et al. Diagnostic testing for acute head injury in children: when are head computed tomography and skull radiographs indicated? Pediatrics. 1997;99(5). Available at: www.pediatrics.org/cgi/content/full/99/5/e11 [DOI] [PubMed] [Google Scholar]
- 6.Rosenthal BW, Bergman I. Intracranial injury after moderate head trauma in children. J Pediatr. 1989;115(3):346–350 [DOI] [PubMed] [Google Scholar]
- 7.Greenes DS, Schutzman SA. Clinical significance of scalp abnormalities in asymptomatic head-injured infants. Pediatr Emerg Care. 2001;17(2):88–92 [DOI] [PubMed] [Google Scholar]
- 8.Mannix R, Monuteaux MC, Schutzman SA, Meehan WP III, Nigrovic LE, Neuman MI. Isolated skull fractures: trends in management in US pediatric emergency departments. Ann Emerg Med. 2013;62(4):327–331 [DOI] [PubMed] [Google Scholar]
- 9.Rollins MD, Barnhart DC, Greenberg RA, et al. Neurologically intact children with an isolated skull fracture may be safely discharged after brief observation. J Pediatr Surg. 2011;46(7):1342–1346 [DOI] [PubMed] [Google Scholar]
- 10.Greenes DS, Schutzman SA. Infants with isolated skull fracture: what are their clinical characteristics, and do they require hospitalization? Ann Emerg Med. 1997;30(3):253–259 [DOI] [PubMed] [Google Scholar]
- 11.Dias MS, Lillis KA, Calvo C, Shaha SH, Li V. Management of accidental minor head injuries in children: a prospective outcomes study. J Neurosurg. 2004;101(1 suppl):38–43 [DOI] [PubMed] [Google Scholar]
- 12.Powell EC, Atabaki SM, Wootton-Gorges S, et al. Isolated linear skull fractures in children with blunt head trauma. Pediatrics. 2015;135(4). Available at: www.pediatrics.org/cgi/content/full/135/4/e851 [DOI] [PubMed] [Google Scholar]
- 13.Walsh KE, Landrigan CP, Adams WG, et al. Effect of computer order entry on prevention of serious medication errors in hospitalized children. Pediatrics. 2008;121(3). Available at: www.pediatrics.org/cgi/content/full/121/3/e421 [DOI] [PubMed] [Google Scholar]
- 14.Madge P, Paton JY, McColl JH, Mackie PL. Prospective controlled study of four infection-control procedures to prevent nosocomial infection with respiratory syncytial virus. Lancet. 1992;340(8827):1079–1083 [DOI] [PubMed] [Google Scholar]
- 15.Piteau SJ, Ward MGK, Barrowman NJ, Plint AC. Clinical and radiographic characteristics associated with abusive and nonabusive head trauma: a systematic review. Pediatrics. 2012;130(2):315–323 [DOI] [PubMed] [Google Scholar]
- 16.Laskey AL, Stump TE, Hicks RA, Smith JL. Yield of skeletal surveys in children ≤18 months of age presenting with isolated skull fractures. Pediatrics. 2013;162(1):86–89 [DOI] [PubMed] [Google Scholar]
- 17.Wood JN, Christian CW, Adams CM, Rubin DM. Skeletal surveys in infants with isolated skull fractures. Pediatrics. 2009;123(2). Available at: www.pediatrics.org/cgi/content/full/123/2/e247 [DOI] [PubMed] [Google Scholar]
- 18.Reece RM, Sege R Childhood head injuries: accidental or inflicted? Arch Pediatr Adolesc Med. 2000;154(1):11–15 [PubMed] [Google Scholar]
- 19.Akenroye AT, Stack AM. The development and evaluation of an evidence-based guideline programme to improve care in a paediatric emergency department. Emerg Med J. 2015;33:(2):109–117 [DOI] [PubMed] [Google Scholar]
- 20.Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12(6):458–464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grigg OA, Farewell VT, Spiegelhalter DJ. Use of risk-adjusted CUSUM and RSPRT charts for monitoring in medical contexts. Stat Methods Med Res. 2003;12(2):147–170 [DOI] [PubMed] [Google Scholar]
- 22.Kittle K, Currier K, Dyk L, Newman K. Using a pediatric database to drive quality improvement. Semin Pediatr Surg. 2002;11(1):60–63 [DOI] [PubMed] [Google Scholar]
- 23.Li J, Monuteaux MC, Bachur RG. Interfacility transfers of noncritically ill children to academic pediatric emergency departments. Pediatrics. 2012;130(1):83–92 [DOI] [PubMed] [Google Scholar]
- 24.American Academy of Pediatrics. Committee on Hospital Care and Committee on Child Abuse and Neglect . Medical necessity for the hospitalization of the abused and neglected child. Pediatrics. 1998;101(4 pt 1):715–716 [DOI] [PubMed] [Google Scholar]
- 25.Myhre MC, Grøgaard JB, Dyb GA, Sandvik L, Nordhov M. Traumatic head injury in infants and toddlers. Acta Paediatr. 2007;96(8):1159–1163 [DOI] [PubMed] [Google Scholar]
- 26.Deye KP, Berger RP, Lindberg DM; ExSTRA Investigators . Occult abusive injuries in infants with apparently isolated skull fractures. J Trauma Acute Care Surg. 2013;74(6):1553–1558 [DOI] [PubMed] [Google Scholar]
- 27.Metzger RR, Smith J, Wells M, et al. Impact of newly adopted guidelines for management of children with isolated skull fracture. J Pediatr Surg. 2014;49(12):1856–1860 [DOI] [PubMed] [Google Scholar]
- 28.Nigrovic LE, Stack AM, Mannix RC, et al. Quality improvement effort to reduce cranial CTs for children with minor blunt head trauma. Pediatrics. 2015;136(1). Available at: www.pediatrics.org/cgi/content/full/136/1/e227 [DOI] [PMC free article] [PubMed] [Google Scholar]