Abstract
Context
Early identification efforts are essential for the early treatment of the symptoms of autism but can only occur if robust risk factors are found. Children with autism often engage in repetitive behaviors and anecdotally prefer to visually examine geometric repetition, such as the moving blade of a fan or the spinning of a car wheel. The extent to which a preference for looking at geometric repetition is an early risk factor for autism has yet to be examined.
Objectives
To determine if toddlers with an autism spectrum disorder (ASD) aged 14 to 42 months prefer to visually examine dynamic geometric images more than social images and to determine if visual fixation patterns can correctly classify a toddler as having an ASD.
Design
Toddlers were presented with a 1-minute movie depicting moving geometric patterns on 1 side of a video monitor and children in high action, such as dancing or doing yoga, on the other. Using this preferential looking paradigm, total fixation duration and the number of saccades within each movie type were examined using eye tracking technology.
Setting
University of California, San Diego Autism Center of Excellence.
Participants
One hundred ten toddlers participated in final analyses (37 with an ASD, 22 with developmental delay, and 51 typical developing toddlers).
Main Outcome Measure
Total fixation time within the geometric patterns or social images and the number of saccades were compared between diagnostic groups.
Results
Overall, toddlers with an ASD as young as 14 months spent significantly more time fixating on dynamic geometric images than other diagnostic groups. If a toddler spent more than 69% of his or her time fixating on geometric patterns, then the positive predictive value for accurately classifying that toddler as having an ASD was 100%.
Conclusion
A preference for geometric patterns early in life may be a novel and easily detectable early signature of infants and toddlers at risk for autism.
It is undeniable that early treatment can have a significant positive impact on the long-term outcome for children with an autism spectrum disorder (ASD).1–3 Early treatment, however, generally relies on the age at which a diagnosis can be made, thus pushing early identification research into a category of high public health priority. Unfortunately, easily implemented methods for facilitating early identification remain to be found.
Eye tracking technology holds promise as an objective method for characterizing the early features of autism because it can be implemented with individuals of virtually any age or functioning level. Historically, the bulk of eye tracking studies have been conducted with older children, adolescents, and adults with autism.4–10 In one of the first studies on this topic, Klin and colleagues 10 showed that when watching a socially intense movie, adults with autism predominantly looked at the mouth region of the actors whereas typical subjects looked at the eye region. Bringing this effort into the childhood years, Jones and colleagues 11 later showed that even 2-year-olds with autism spent more time fixating on the mouth region than the eyes during face viewing. They raised the provocative possibility that how social images are visually examined could be an early warning sign for autism.
Continuing with the idea that reduced fixation time on the eye region could be diagnostically revealing, Merin and colleagues 12 studied 6-month-olds at risk for autism by virtue of having a sibling with the disorder and found abnormalities similar to the Jones et al experiment: in contrast to typical infants, baby siblings at risk for having an ASD spent more time looking at the mouth region than the eyes. Given the young age of the baby sibling sample, the eventual diagnoses of these infants were not known at the time. In a follow-up study that used virtually the identical sample of baby siblings, Young and colleagues 13 examined the clinical outcome of these subjects and found that, contrary to their expectations, eye gaze patterns at 6 months did not predict diagnostic outcome. That is, many of the baby siblings who had reduced examination of the eye region at 6 months were not considered to have autism later in childhood. This makes sense given that even typically developing (TD) 3- and 6-month-old infants have been shown to be highly inconsistent in where they look during face viewing in comparison with older infants.14 Furthermore, the infant brain is undergoing an explosion of activity during the first year of life, a period when the number of synapses reaches a peak in many areas that is twice that of the adult 15 and brain volume doubles in size in comparison with birth.16 Given the active pace of brain development during the infancy period combined with high intersubject variability of eye tracking patterns to faces during this time, examining the percentage of time an infant attends to the eye region of a face may not be stable enough to make diagnostically predictive claims, especially at the individual subject level.
An alternative method to investigate early indicators of autism is to measure a very simple behavior: preference. Using a preferential looking paradigm wherein 2 images are placed side by side, Klin and colleagues 17 found a statistically reduced preference for biological motion in 2-year-olds with autism. Specifically, the 2-year-olds with autism in that study looked less often at point-light displays depicting well-known motions such as pat-a-cake and more often at inverted point-light displays than developmentally delayed (DD) and TD contrast groups. Thus, what infants prefer to look at when given a choice between 2 images may turn out to be a more clearly observable indicator of risk than how they look at a single image. When given the direct choice, TD infants and toddlers prefer to look at social images, such as faces, over nonsocial images.18,19 It is unknown if this same preference exists in toddlers at risk for autism. Interestingly, in the first prospective study of infants at risk for an ASD, social behavior was not different from normal during the first 6 months of life.20,21 Infants in that study cooed and smiled at examiners and were indistinguishable from TD infants at that age.22 At 12 months of age, however, deviances in social behavior were evident in the at-risk group, suggesting that the 1-year period marks an age where social defects and possibly social preference behaviors may become clearly observable, a finding consistent with retrospective studies.23–25
Many children with autism engage in a variety of repetitive behaviors 26 and, anecdotally, often prefer to attend to visual repetition, such as the moving blade of a fan or the spinning of a car wheel. In fact, individuals with autism have a noted strength in visuospatial abilities, particularly when considered relative to other abilities within the same individual. For example, high-functioning adults 27 and children 28 with autism are reported to be faster at finding a hidden object in an embedded figure task than TD individuals. Furthermore, adults with autism are better at remembering geometric patterns they have seen in the past than typical adults.29 It is thought that enhanced visuospatial abilities in autism may stem from a local processing bias.30,31 The early developmental profile of unusual preferences for visual repetition in autism is largely unknown and unexplored. If given the direct choice, would children with autism prefer to attend to highly repetitive images such as repeating geometric shapes rather than social images, and if so, would such a preference be evident early in development?
We hypothesized that, as a group, toddlers and young children at risk for autism would spend a greater amount of time examining dynamic geometric images (DGI) than dynamic social images (DSI) and that this preference would be observable as early as 1 year of age. Furthermore, because individuals with autism have deficits in shifting visual attention 32–37 and have been known to exhibit longer disengagement latencies,20,38 we additionally hypothesized that such individuals might show a reduction in the number of saccades overall when analyzing a visual scene.
To test this possibility, a preferential looking paradigm was developed that examined looking time toward highly salient social images, such as children dancing and doing yoga, in comparison with highly salient geometric images, such as repeating and moving concentric circles. Past studies have suggested that using highly salient or attention-directing stimuli may be critical for maximizing the potential for more typical patterns of brain activity in autism.39,40 To consider how a preference for geometric patterns may change during development, a wide age range of toddlers with an ASD spanning from 14 to 42 months were studied. Finally, to examine the degree to which preference patterns are related to delayed language or cognitive development rather than autism per se, a contrast group consisting of children with DD matched in ability to the ASD group was included.
METHODS
PARTICIPANTS
Subjects were recruited from 2 sources: general community referral (eg, Web site) and a general population-based screening method called the 1-Year Well-Baby Check-Up Approach (K.P., C. Carter, PhD, M. Weinfeld, PhD, J.D., R.H., R. Bjork, MD, N. Gallagher, BA, unpublished data, 2006–2009). Using this method, toddlers at risk for an ASD, language delay, and DD as young as 12 months were identified with a broadband screening instrument, the Communication and Symbolic Behavior Scales Developmental Profile Infant-Toddler Checklist,41,42 and were recruited and tracked every 6 months until their third birthday. This method thus allowed for the prospective study of autism beginning at 12 months of age. Typically developing controls were obtained from community referrals. All toddlers participated in a series of tests across multiple 2-hour sessions that included the Autism Diagnostic Observation Schedule–Toddler Module (ADOS-T), newly validated for use with infants as young as 12 months,43 and the Mullen Scales of Early Learning.44 Parents were also interviewed with the Vineland Adaptive Behavior Scales.45 Toddlers participated in additional behavioral (eg, play) and biological (eg, magnetic resonance imaging) tests as part of a larger study. (For more information, see www.autismsandiego.org.) All standardized assessments were administered by 2 highly experienced PhD-level psychologists with more than 10 years’ combined experience in autism.
Overall, 138 toddlers aged 12 to 43 months participated. Twenty-eight (10 with an ASD, 11 with TD, 7 with DD) were excluded from final analyses because of noncompliance during testing, which almost always resulted in less than 50% valid trials. The final group of 110 toddlers consisted of 37 with an ASD (27 with autistic disorder, 9 with pervasive developmental delay not otherwise specified, 1 with ASD features), 51 with TD, and 22 with DD (12 with language delay, 10 with global developmental delay). While several of the toddlers with an ASD were only a year old at the time of testing, all but 1 have been tracked and diagnosed using the ADOS-T until at least age 24 months, an age shown to be reliable for the diagnosis of autism.20,43,46–49 Final diagnoses for participants with an ASD older than 30 months were confirmed with the Autism Diagnostic Interview-Revised.50 Toddlers were determined to have language delay if 1 or both of the language subtest scores of the Mullen Scales of Early Learning were more than 1 SD lower than expected values for that age (ie, a t score <40). Toddlers were determined to have global DD if scores were more than 1 SD lower than expected values on 3 or more of the subtests of the Mullen Scales of Early Learning and the overall developmental quotient was more than 1 SD lower than expected values (ie, <85) (Table).
Table.
Participant Characteristics
| Mean (SD) [Range] | |||||
|---|---|---|---|---|---|
| P Value | |||||
| Characteristic | ASD (n=37) |
DD (n=22) |
TD (n=51) |
||
| ASD vs TD | ASD vs DD | ||||
| Sex, M/F, No. | 30/7 | 16/6 | 35/17 | .15 | .46 |
| Age, mo | 26.7 (7.7) [14–42] | 22.7 (8.5) [12–41] | 24.6 (8.2) [12–43] | .21 | .07 |
| Mullen verbal DQ | 63.5 (21.4) | 69.4 (18.6) | 108 (17.5) | <.001 | .19 |
| Mullen nonverbal DQ | 78.4 (21.6) | 81.5 (28.5) | 118 (19.7) | <.001 | .64 |
| Vineland Adaptive Behavior Scales 45 standard score | 87.7 (12.8) | 84.3 (12.8) | 103.1 (9.9) | <.001 | .46 |
| ADOS-T social affect score | 12.5 (4.3) | 5.2 (3.0) | 1.5 (1.4) | <.001 | <.001 |
| ADOS-T restricted repetitive score | 4.1 (2.0) | 0.95 (1.2) | 0.32 (0.67) | <.001 | <.001 |
| ADOS-T total score | 16.7 (4.7) | 6.18 (3.5) | 1.86 (1.9) | <.001 | <.001 |
Thirty-seven TD toddlers were matched on a 1-1 basis to toddlers with an ASD based on age (±3 months) and sex. The remaining 14 TD toddlers were matched based on the chronological age range of the ASD group. Subjects with DD served as a contrast group and were matched to the ASD group based on chronological age, verbal and nonverbal developmental quotient as assessed by the Mullen Scales of Early Learning, and overall functioning as assessed by the Vineland Adaptive Behavior Scales. There were no significant differences in any of these measures between the ASD and DD groups. As expected, the TD group had a significantly higher verbal developmental quotient, nonverbal developmental quotient, and adaptive behavior score and significantly lower ADOS-T scores than the ASD group. This study was approved by the University of California, San Diego Human Subjects Research Protection Program. Legal guardians of all participants gave written informed consent.
APPARATUS, STIMULI, AND EYE TRACKING PROCEDURE
Apparatus
A Tobii T120 eye tracker (Tobii, Danderyd, Sweden, www.tobii.com) was used to measure toddlers’ fixations and number of saccades in response to a visual stimulus. The binocular eye tracker used infrared light sources and cameras that are integrated into a 17-in-thin film transistor monitor. Using corneal reflection techniques, the Tobii eye tracker records the X and Y coordinates of toddlers’ eye position at a frequency of 120 Hz (ie, 7200 data collections/min). Two additional small cameras were placed on top of the eye tracking monitor to obtain video of each toddler’s behavior during the experiment at all times.
Stimuli
Toddlers were presented with a movie consisting of DGI on 1 side and DSI on the other. The DGI were produced from recordings of animated screen saver programs. The DSI were produced from a series of short sequences of children doing yoga (Yoga Kids 3; Gaiam, Boulder, Colorado, http://www.gaiam.com, created by Marsha Wenig, http://yogakids.com/), which included images of children moving in a dramatic manner (eg, waving arms and appearing as if dancing). Audio information was discarded. The final presentation stimulus was composed of 2 rectangular areas of interest horizontally distributed containing DGI and DSI in which scenes changed in a simultaneous, time-linked fashion (Figure 1). To control for preference that may be mediated by spatial location, the side of presentation of DGI and DSI scenes was randomized across subject and diagnosis so that 50% of toddlers saw a movie containing DSI on the left. The final movie contained a total of 28 scenes with single-scene duration varying from 2 to 4 seconds for a total presentation time of 60 seconds at 24 frames per second.
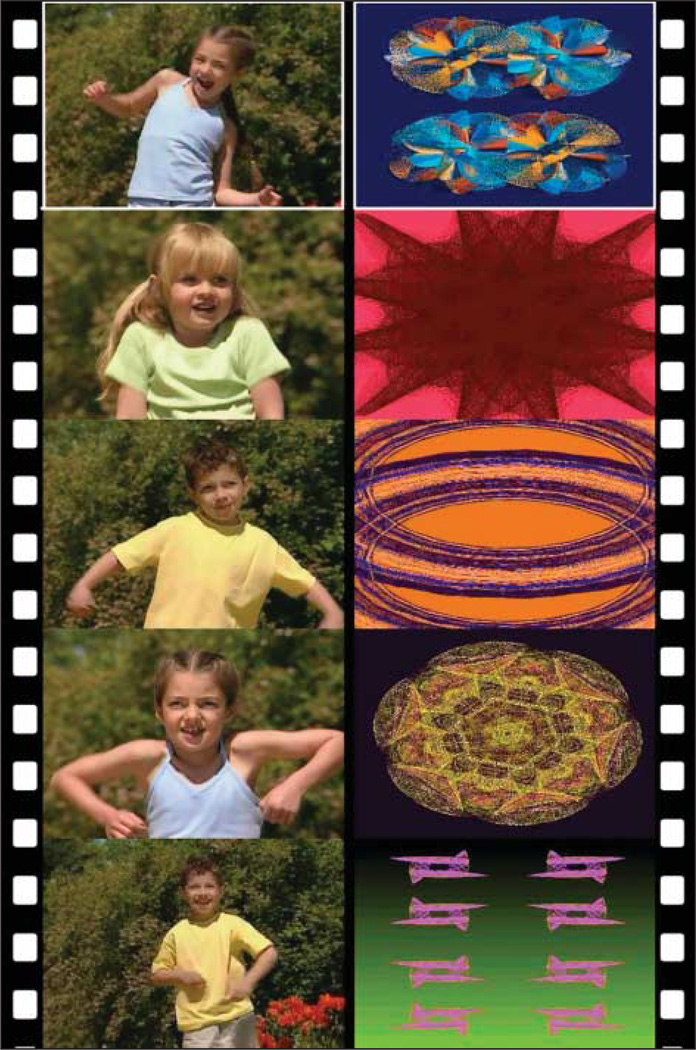
Figure 1.
Sample stimuli illustrating 5 movie frames (Yoga Kids 3; Gaiam, Boulder, Colorado, http://www.gaiam.com, created by Marsha Wenig, http://yogakids.com/) contained within the larger movie with dynamic geometric images on the right and dynamic social images on the left. Half of the subjects viewed the movie with this orientation and the other half, with the side of dynamic geometric images and dynamic social images reversed. The areas of interest are depicted by the white box highlighted on the first frame. Eye tracking data were recorded at 120 Hz for a total of 7200 data collections across the 1-minute movie.
Procedure
Toddlers were seated on their parent’s lap 60 cm in front of the eye tracking monitor. Parents were read a series of standardized instructions describing the eye tracking procedure. The lights were off during testing and a partition separated the operator from the toddler. To obtain calibration information, toddlers were first shown images of an animated cat that appeared in 1 of 9 locations on the screen. During this procedure, the eye tracker measured characteristics of the toddler’s eyes (eg, corneal light reflection) and used them together with a 3-dimensional eye model to calculate the gaze data. Quality of calibration was displayed as green lines with varying lengths, with shorter lines indicating better calibration. If an infant’s calibration was poor, the procedure was repeated as necessary.
Using a “live tracker” included in the Tobii software (Tobii Studio version 1.3) that superimposes the toddler’s eye tracking data on the test image in real time, the operator observed the infant’s gaze position and head position on a secondary monitor during the experimental procedure, making note of deviation from an established working range of positions. The operator also monitored the child’s behavior by observing the realtime video recording. If the infant’s eyes were no longer picked up by the live tracker, or if the infant attempted to get out of his or her mother’s lap as indicated by the video recording, then the process was repeated, including pretrial calibration.
DEPENDENT VARIABLES AND STATISTICAL ANALYSES
Fixation Time
Using Tobii software, fixation data were calculated using a 35-pixel radius filter. Time spent fixating and number of saccades within each area of interest were tabulated for each subject. Offscreen fixations (ie, when a participant looked away from the movie) were determined by fixation coordinates that fell outside the areas of interest. Any subject with total fixation time less than 30 seconds (ie, 50% of the experiment) was excluded from analyses. There was a significant difference in total viewing time between groups (F3,106=3.2; P=.02; mean viewing time: ASD, 49.4 seconds; TD, 53.7 seconds; and DD, 48.1 seconds). To compare percentage of fixation time within DGI between the 3 diagnostic groups, a 1-way analysis of variance was performed (diagnostic group [3 levels] × percentage of DGI fixation time [1 level]). Significant effects were followed by planned contrasts using t tests. To determine the specific percentage of fixation time within DGI that would best discriminate toddlers with an ASD from toddlers with DD and TD, a receiver operating characteristic curve was generated that graphically displayed a plot of the true positives vs false positives using SPSS statistical software (SPSS, Chicago, Illinois, http://www.spss.com/statistics). To determine if a preference for geometric patterns or DSI became stronger or weaker with development, percentage of fixation time on DGI was correlated with age for toddlers within each diagnostic group using Pearson product-moment correlations. Bonferroni correction was used with a significance level set at P < .0125 for all post hoc comparisons.
Time Course Analysis
To determine if each toddler’s preference was stable across the experiment or changed with time, fixation time data were divided into thirds (ie, percentage of fixation on geometric patterns from 0–19.99 seconds, 20–39.99 seconds, and 40–60 seconds) for each participant and plotted as an average for each major diagnostic group. A repeated-measures analysis of variance was used to examine differences between each of the 3 periods.
Number of Saccades
To determine if the overall number of saccades was different between groups, the total number of saccades divided by the total looking time was determined for each toddler.
Test-Retest Reliability
A subset of 41 toddlers (16 with an ASD, 5 with DD, and 20 with TD) returned for a second eye tracking session 1 to 14 months following the first session (mean [SD], 7.79 [3.2] months later). Test-retest reliability was calculated as the percentage of preference difference between test time 1 and test time 2.
RESULTS
A PREFERENCE FOR DGI IN A SUBGROUP OF TODDLERS WITH AUTISM
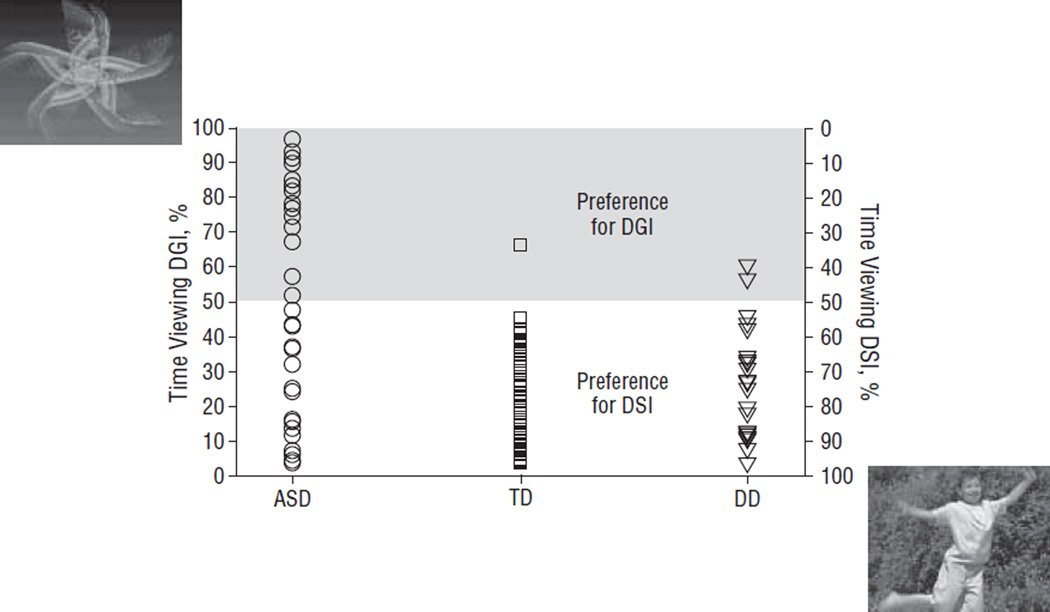
Overall, the percentage of time that toddlers spent viewing DGI was significantly different between diagnostic groups (F2,107=11.8; P< .001). As a group, toddlers with an ASD spent significantly more fixation time on DGI than TD toddlers (t86=4.5; P<.001) and toddlers with DD (t57=2.7; P= .009). Forty percent of the ASD group spent greater than 50% of viewing time fixated on DGI in contrast to only 1.9% of TD toddlers and 9% of toddlers with DD. Of the 15 toddlers with an ASD who preferred DGI, more than half spent more than 70% of their time visually examining DGI, with several toddlers exceeding 90% DGI viewing time, a pattern not found in any other group (Figure 2 and Figure 3). As is visually apparent in Figure 2, and confirmed with a receiver operating characteristic curve analysis (area under the curve=0.686 ±0.06; P < .001), when 68.6% geometric pattern viewing time was used as a cutoff, the positive predictive value for an ASD was 100%. Furthermore, a preference for geometric patterns was found in several subjects with an ASD younger than 18 months, with the youngest age being 14 months.
Figure 2.
Scatterplot illustrating the percentage of fixation time on both dynamic geometric images (DGI) and dynamic social images (DSI) for each toddler with an autism spectrum disorder (ASD), typically developing (TD) toddler, and toddler with developmental delay (DD). Total percentage of time viewing DGI and DSI sums to 100% for each toddler. For example, a toddler who spends 80% of viewing time on DGI (as noted on the y-axis on the left) thus spends 20% of viewing time on DSI (as noted on the y-axis on the right). A toddler who spends more than 50% of viewing time on DGI is considered a “geometric responder” and a toddler who spends more than 50% of viewing time on DSI is considered a “social responder.”
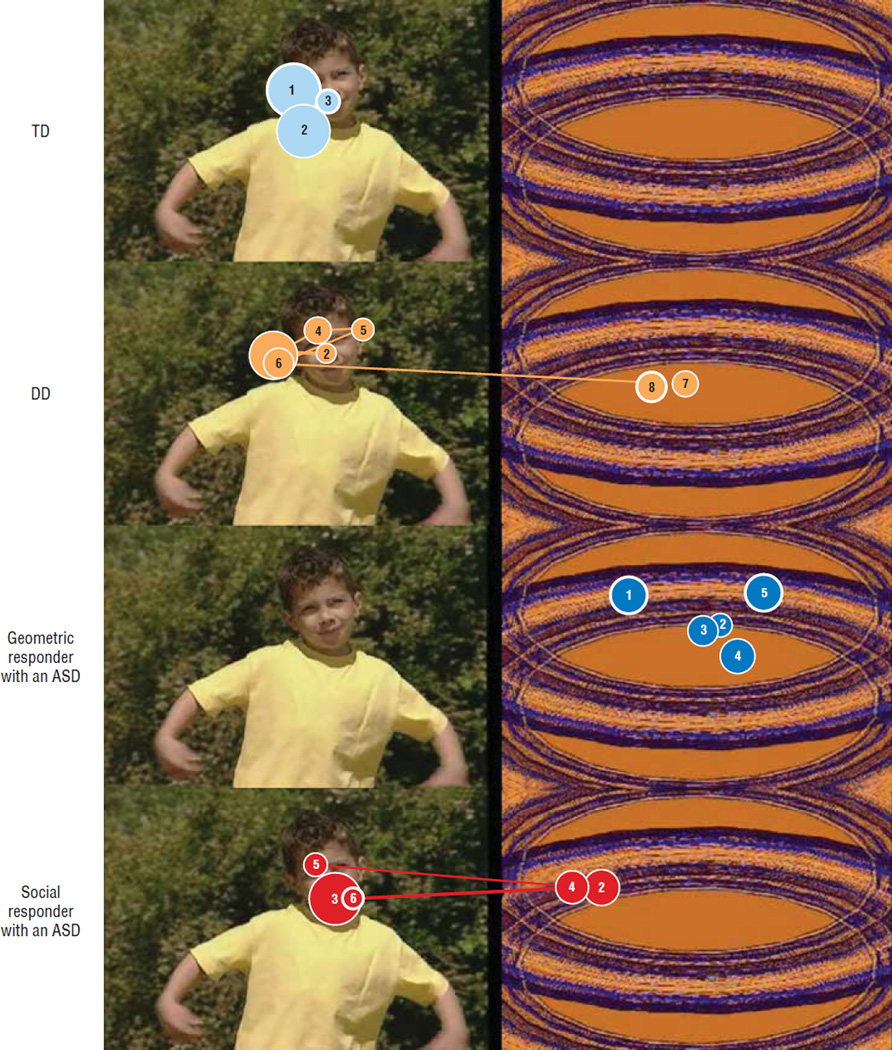
Figure 3.
Example scan paths for a typically developing (TD) toddler, toddler with developmental delay (DD), geometric responder with an autism spectrum disorder (ASD), and social responder with an ASD across a 3-second scene overlaid on a single movie scene (Yoga Kids 3 ; Gaiam, Boulder, Colorado, http://www.gaiam.com, created by Marsha Wenig, http://yogakids.com/). The numbers inside the circles represent the order of saccades, with larger circles representing longer fixation times.
An examination of the relationship of age on preference revealed no significant correlation between percentage of time viewing DGI (or DSI) and age, for any diagnostic group (ASD: r=0.06;P=.74;DD: r=0.05;P=.80; TD: r=0.11; P = .43). When age was used as a covariate in the overall analysis of variance, the main effect of age in the model was very low (F1,106= 0.51; P =.47) while the main effect of group was still highly significant (F2,106= 10.9; P< .001).
Excluding 1 TD toddler who preferred geometric patterns, 50% of viewing time on DSI marks the end of the range for TD toddlers, who all preferred DSI. Using this as a boundary, we next identified 2 subgroups within the larger ASD group: those who preferred DSI (ie, spent >50% of viewing time within DSI) and those who preferred DGI (ie, spent >50% of viewing time within DGI). Considering “geometric” and “social” responders with an ASD as separate groups, we next asked if the overall clinical characteristics differed between these 2 subgroups. Independent-sample t tests revealed no difference between geometric and social responders with an ASD on the social affect (t35 = 1.6; P = .10), restricted and repetitive (t35=−1.2;P = .23), or overall (t35 = 0.91;P = .36) ADOS-T scores. There were also no differences in the visual reception (t35 = −0.99; P = .32), fine motor (t35 =−1.7; P=.32), receptive language (t35=−0.98; P = .33), expressive language (t35=−0.42; P=.67), or early learning composite (t35=−1.2; P = .22) scores.
TIME COURSE ANALYSIS
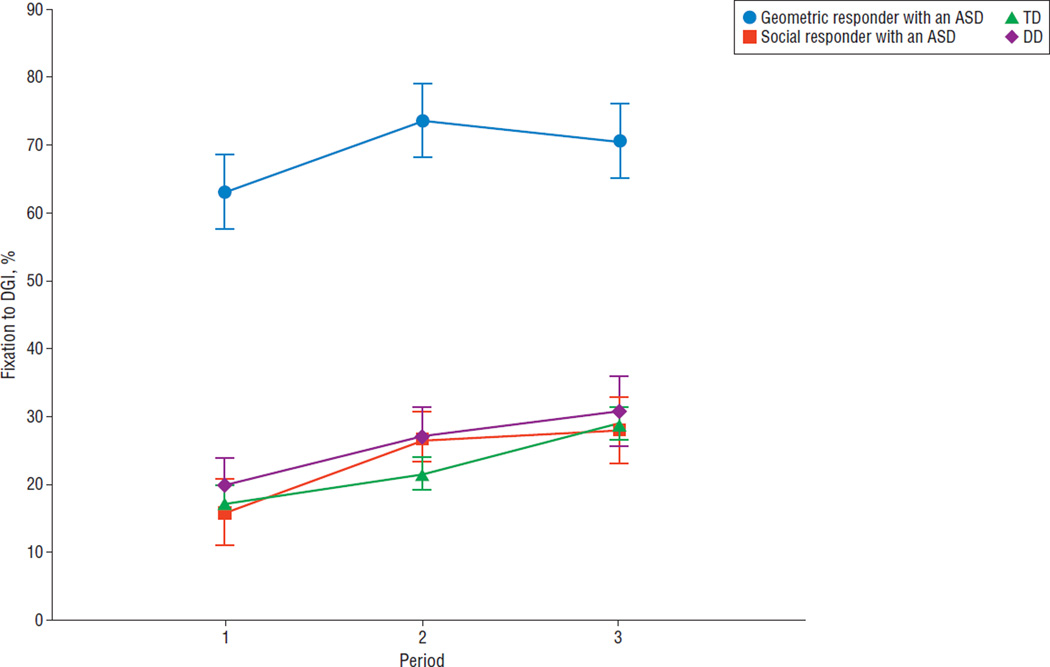
An examination of differences in fixation on DGI across time for the 4 major groups (geometric responder with an ASD, social responder with an ASD, toddlers with DD, and TD toddlers) revealed a strong main effect of group (F3,106=49; P< .001) and follow-up t tests revealed that geometric responders with an ASD spent significantly more time fixating on DGI than other groups during all 3 periods. Although there was a small, significant increase in DGI fixation across time in all groups (F2,212= 12.7; P<.001), there was no group X time interaction (F6,212= 0.667; P>.05) (Figure 4).
Figure 4.
Line graph depicting the time course of percentage of fixation on dynamic geometric images (DGI) across the 1-minute movie divided into 3 periods for geometric responders with an autism spectrum disorder (ASD), social responders with an ASD, typically developing (TD) toddlers, and toddlers with developmental delay (DD). Period 1 represents the mean percentage of fixation from 0 to 19.99 seconds, period 2 represents the mean percentage of fixation from 20 to 39.99 seconds, and period 3 represents the mean percentage of fixation from 40 to 60 seconds. Percentage of fixation on DGI was significantly different between periods 1 and 2. Error bars represent standard error of the mean.
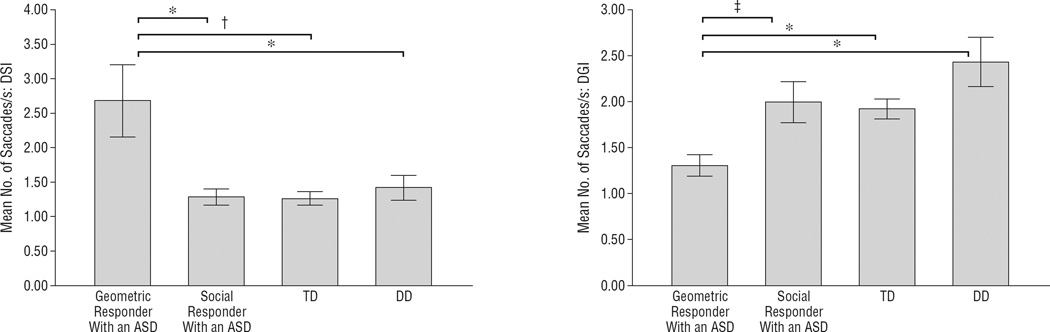
UNIQUE SACCADE PATTERN IN TODDLERS WITH AN ASD WHO PREFERRED GEOMETRIC IMAGES
The number of saccades while viewing DGI (F3,106=4.6; P = .005) and DSI (F3,106=8.9; P< .001) was significantly different between geometric responders with an ASD, social responders with an ASD, and the DD and TD groups. Follow-up t tests revealed that the geometric responders with an ASD had a unique saccade signature and exhibited significantly fewer saccades when they were viewing their preferred geometric stimuli in comparison with all other groups (all P< .01). In contrast, when the geometric responders with an ASD viewed their nonpreferred stimuli, namely the social stimuli, they exhibited a significantly greater number of saccades in contrast to TD toddlers and toddlers with DD. The significance level in contrast to social responders with an ASD was P = .02, but this did not meet the Bonferroni correction threshold of less than .0125 (Figure 5).
Figure 5.
Bar graphs illustrating the mean number of saccades during the viewing of dynamic social images (DSI) (left) or dynamic geometric images (DGI) (right). The toddlers with an autism spectrum disorder (ASD) were grouped according to movie preference (ie, geometric or social responder). When viewing social images, geometric responders with an ASD had significantly more saccades than all other groups. When viewing geometric images, geometric responders with an ASD had significantly fewer saccades. *P<.01. †P<.001. ‡P=.02. DD indicates developmental delay; TD, typically developing.
TEST-RETEST RELIABILITY
Each toddler’s preference for a particular movie type was relatively stable. The mean change in percentage of preference within our sample was 15.62% (range, 1%-36%; SD, 9.2). As revealed by the range, 1 subject changed his preference by 36%. This subject had an ASD and changed his preference from social responder on test 1 to geometric responder on test 2. A paired-sample t test revealed no significant difference between percentage of fixation on DGI between test 1 and test 2 (t40 = 1.7; P>.05).
COMMENT
Using a simple preferential looking paradigm, toddlers who were at risk for or had a confirmed ASD diagnosis spent a greater amount of time visually examining dynamic geometric images (DGI) in contrast to dynamic social images (DSI). This pattern was not found in TD controls or DD contrast groups. When the percentage of time a toddler spent fixating on geometric patterns was 69% or greater, the positive predictive validity for accurately classifying that toddler as having an ASD was 100%. Furthermore, a preference for DGI may be a risk factor for autism in that this preference was observed in a toddler at risk for an ASD as young as 14 months.
This phenomenon, however, was not ubiquitous across the entire ASD sample. While a considerable portion of the ASD sample, namely 40%, were geometric responders, in that they preferred to visually examine DGI, the remaining 60% of participants with an ASD performed similar to the TD and DD contrast groups in that they preferred DSI. A preference for geometric patterns was not associated with general cognitive delay in that there was no relationship between IQ and fixation time within the ASD group. Additionally, with 2 exceptions, none of the toddlers with DD showed a preference for DGI. This is particularly compelling given that several of the toddlers with DD had IQ scores less than 65. Given that there was also no relationship with the social affect or overall algorithm scores on the ADOS-T, it was thus not the case that toddlers with an ASD who preferred DGI had more severe symptoms in general. Instead, the findings illustrate a definable subgroup of toddlers with an ASD who may be linked to perceptual variables not examined in this study, such as superior visual acuity,51 weak central coherence,30 or enhanced perceptual processing in general.52 Alternatively, this subgroup of toddlers may be a particularly strong example of those who do not prefer biological motion, as has been recently demonstrated.17
While a preference for geometric patterns alone may be an intriguing novel identifier of early autism, results also illustrated a distinct pattern of saccades within the geometric responders. Based on research documenting deficits in shifting 32–37 and disengaging attention 20 in autism, we initially predicted that toddlers with an ASD overall would show a reduced number of saccades. Results revealed that it was only the geometric responders, not the group as a whole, who displayed a reduced number of saccades. Furthermore, this reduction in saccades was evident only when geometric responders with an ASD were viewing their preferred geometric patterns. In contrast, when geometric responders with an ASD viewed their non-preferred stimuli, namely DSI, they exhibited a significantly greater number of saccades (almost twice as many) in comparison with other diagnostic groups. A recent eye tracking study suggested that an increased number of saccades to DSI may be the result of anxiety in individuals with autism.53 Therefore, for this particular subgroup, the profile appears to be increased saccades during the viewing of nonpreferred stimuli and decreased saccades while viewing preferred stimuli. Thus, the combination of a preference for geometry combined with saccade quantity might be a particularly strong early identifier of autism.
Importantly, each toddler’s preference, be it DGI or DSI, was relatively stable across time. Additionally, there were no age effects in that there was no relationship between the quantity of looking time at DGI or DSI and age, suggesting that the current paradigm is suitable for use across at least the first 3 or 4 years of development.
Surprisingly, more than half of the toddlers with an ASD in the study behaved just like those who were TD or DD: they preferred DSI. The nature of the stimuli used may have contributed to this finding. In the past, we demonstrated that using highly compelling social images, such as images of mothers’ or children’s faces, resulted in much more normal brain activity in ASD than the use of less compelling stimuli, such as the faces of strangers.39,54 In the same way, the present study used attention-grabbing social stimuli that consisted of young children dancing and doing yoga. We can only speculate that the brain systems that are normally active in response to rich social images, such as the fusiform gyrus, cingulate, medial frontal lobes, and amygdala,55 were likely more engaged in the social responders group than in the geometric responders group. If this is true, then reanalyses of past functional magnetic resonance imaging studies with older children or adults with autism may be able to reveal distinct subgroups: those with an ASD with more “typical” social brain activity and those with less, reflecting a lifetime of differences in social preference and attention. Likewise, it may be that the neural profile of geometric responders when looking at geometric images may be stronger than social responders in brain regions classically involved in basic visual perception and attention, such as the extrastriate visual cortex and parietal lobes.56,57 While functional magnetic resonance imaging is currently not feasible with awake toddlers, other imaging modalities, such as electroencephalography and near infrared spectroscopy, hold promise for future studies aimed at revealing possible unique neural signatures between these 2 groups.
It is undeniable that eye movements guide learning.58 What an infant chooses to look at provides images and experiences from which to learn and mature. To our knowledge, the present study is the first to empirically demonstrate that this preference in a subgroup of toddlers with an ASD may begin as early as 14 months, and quite possibly even earlier. The impact of reduced social attention in favor of attention to geometry at such an early age in development can only be surmised, but it is thus no surprise that functional magnetic resonance imaging studies of older children and adults with autism often report weak or absent functional activity in brain regions involved in social processing, such as the fusiform, medial frontal lobes, amygdala, and cingulate.59–61
While the discovery of a putative new early warning sign of autism is encouraging, results should be interpreted with some caution for 2 reasons. First, approximately 20% of the overall sample was dropped from analyses because of poor compliance during testing, with the impact of such exclusion unknown. Second, participants viewed a movie that was only 1 minute. While 1 minute has been previously demonstrated to be the average attention span of a 1-year-old,62 thus suggesting that 1 minute is optimal, examining a preference for geometric patterns would be even more compelling if established across multiple testing sessions. In the present study, only one-third of the overall sample participated in test-retest reliability.
Overall, however, the present study provides strong evidence that some infants at risk for an ASD begin life with an unusual preference for geometric repetition. We believe that it may be easy to capture this preference using relatively inexpensive techniques in mainstream clinical settings such as a pediatrician’s office. Furthermore, we also believe that infants identified as exhibiting preferences for geometric repetition are excellent candidates for further developmental evaluation and possible early treatment. Mechanisms of developmental plasticity provide clear rationale that an enriched environment, such as one afforded by careful early treatment, can significantly improve brain structure and function.63,64 The discovery of an early preference for geometric repetition moves beyond the more commonly studied social defects and opens up a new line of inquiry into the early emerging developmental abnormalities in autism.
Acknowledgments
Funding/Support: This work was funded by National Institute of Mental Health grant R01-MH080134 (Dr Pierce) and National Institute of Mental Health Autism Center of Excellence grant P50-MH081755 (Eric Courchesne, PhD).
Additional Contributions: We sincerely thank all of the children and families who participated in this research. A special thank you to Eric Courchesne and Lisa Eyler, PhD, for helpful comments on drafts of the manuscript. Finally, this work would not have been possible without the support of pediatricians in San Diego. A very sincere thank you goes out to the 150 pediatricians in the University of California, San Diego Autism Center of Excellence Pediatric Network.
Footnotes
Author Contributions: Dr Pierce had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Financial Disclosure: An invention disclosure form was filed by Dr Pierce with the University of California, San Diego on March 5, 2010, as the sole inventor.
REFERENCES
- 1.Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, Donaldson A, Varley J. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics. 2010;125(1):e17–e23. doi: 10.1542/peds.2009-0958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lovaas OI. Behavioral treatment and normal educational and intellectual functioning in young autistic children. J Consult Clin Psychol. 1987;55(1):3–9. doi: 10.1037//0022-006x.55.1.3. [DOI] [PubMed] [Google Scholar]
- 3.Cohen H, Amerine-Dickens M, Smith T. Early intensive behavioral treatment: replication of the UCLA model in a community setting. J Dev Behav Pediatr. 2006;27(2 suppl):S145–S155. doi: 10.1097/00004703-200604002-00013. [DOI] [PubMed] [Google Scholar]
- 4.Dalton KM, Nacewicz BM, Johnstone T, Schaefer HS, Gernsbacher MA, Goldsmith HH, Alexander AL, Davidson RJ. Gaze fixation and the neural circuitry of face processing in autism. Nat Neurosci. 2005;8(4):519–526. doi: 10.1038/nn1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hernandez N, Metzger A, Magne´ R, Bonnet-Brilhault F, Roux S, Barthelemy C, Martineau J. Exploration of core features of a human face by healthy and autistic adults analyzed by visual scanning. Neuropsychologia. 2009;47(4):1004–1012. doi: 10.1016/j.neuropsychologia.2008.10.023. [DOI] [PubMed] [Google Scholar]
- 6.Neumann D, Spezio ML, Piven J, Adolphs R. Looking you in the mouth. Soc Cogn Affect Neurosci. 2006;1(3):194–202. doi: 10.1093/scan/nsl030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sterling L, Dawson G, Webb S, Murias M, Munson J, Panagiotides H, Aylward E. The role of face familiarity in eye tracking of faces by individuals with autism spectrum disorders. J Autism Dev Disord. 2008;38(9):1666–1675. doi: 10.1007/s10803-008-0550-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freeth M, Chapman P, Ropar D, Mitchell P. Do gaze cues in complex scenes capture and direct the attention of high functioning adolescents with ASD? Evidence from eye-tracking. J Autism Dev Disord. 2010;40(5):534–547. doi: 10.1007/s10803-009-0893-2. [DOI] [PubMed] [Google Scholar]
- 9.Norbury CF, Brock J, Cragg L, Einav S, Griffiths H, Nation K. Eye-movement patterns are associated with communicative competence in autistic spectrum disorders. J Child Psychol Psychiatry. 2009;50(7):834–842. doi: 10.1111/j.1469-7610.2009.02073.x. [DOI] [PubMed] [Google Scholar]
- 10.Klin A, Jones W, Schultz R, Volkmar F, Cohen D. Visual fixation patterns during viewing of naturalistic social situations as predictors of social competence in individuals with autism. Arch Gen Psychiatry. 2002;59(9):809–816. doi: 10.1001/archpsyc.59.9.809. [DOI] [PubMed] [Google Scholar]
- 11.Jones W, Carr K, Klin A. Absence of preferential looking to the eyes of approaching adults predicts level of social disability in 2-year-old toddlers with autism spectrum disorder. Arch Gen Psychiatry. 2008;65(8):946–954. doi: 10.1001/archpsyc.65.8.946. [DOI] [PubMed] [Google Scholar]
- 12.Merin N, Young GS, Ozonoff S, Rogers SJ. Visual fixation patterns during reciprocal social interaction distinguish a subgroup of 6-month-old infants at-risk for autism from comparison infants. J Autism Dev Disord. 2007;37(1):108–121. doi: 10.1007/s10803-006-0342-4. [DOI] [PubMed] [Google Scholar]
- 13.Young GS, Merin N, Rogers SJ, Ozonoff S. Gaze behavior and affect at 6 months: predicting clinical outcomes and language development in typically developing infants and infants at risk for autism. Dev Sci. 2009;12(5):798–814. doi: 10.1111/j.1467-7687.2009.00833.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frank MC, Vul E, Johnson SP. Development of infants’ attention to faces during the first year. Cognition. 2009;110(2):160–170. doi: 10.1016/j.cognition.2008.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huttenlocher P. Neural Plasticity: The Effects of Environment on the Development of Cerebral Cortex. Cambridge, MA: Harvard University Press; 2002. [Google Scholar]
- 16.Knickmeyer RC, Gouttard S, Kang C, Evans D, Wilber K, Smith JK, Hamer RM, Lin W, Gerig G, Gilmore JH. A structural MRI study of human brain development from birth to 2 years. J Neurosci. 2008;28(47):12176–12182. doi: 10.1523/JNEUROSCI.3479-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klin A, Lin DJ, Gorrindo P, Ramsay G, Jones W. Two-year-olds with autism orient to non-social contingencies rather than biological motion. Nature. 2009;459(7244):257–261. doi: 10.1038/nature07868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Farroni T, Johnson MH, Menon E, Zulian L, Faraguna D, Csibra G. Newborns’ preference for face-relevant stimuli: effects of contrast polarity. Proc Natl Acad Sci U S A. 2005;102(47):17245–17250. doi: 10.1073/pnas.0502205102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goren CC, Sarty M, Wu PY. Visual following and pattern discrimination of facelike stimuli by newborn infants. Pediatrics. 1975;56(4):544–549. [PubMed] [Google Scholar]
- 20.Zwaigenbaum L, Bryson S, Rogers T, Roberts W, Brian J, Szatmari P. Behavioral manifestations of autism in the first year of life. Int J Dev Neurosci. 2005;23(2–3):143–152. doi: 10.1016/j.ijdevneu.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 21.Bryson SE, Zwaigenbaum L, Brian J, Roberts W, Szatmari P, Rombough V, McDermott C. A prospective case series of high-risk infants who developed autism. J Autism Dev Disord. 2007;37(1):12–24. doi: 10.1007/s10803-006-0328-2. [DOI] [PubMed] [Google Scholar]
- 22.Bryson SE, Zwaigenbaum L, Brian J, Roberts W, Szatmari P, Rombough V, McDermott C. A prospective case series of high-risk infants who developed autism. J Autism Dev Disord. 2007;37(1):12–24. doi: 10.1007/s10803-006-0328-2. [DOI] [PubMed] [Google Scholar]
- 23.Osterling J, Dawson G. Early recognition of children with autism: a study of first birthday home videotapes. J Autism Dev Disord. 1994;24(3):247–257. doi: 10.1007/BF02172225. [DOI] [PubMed] [Google Scholar]
- 24.Osterling JA, Dawson G, Munson JA. Early recognition of 1-year-old infants with autism spectrum disorder versus mental retardation. Dev Psychopathol. 2002;14(2):239–251. doi: 10.1017/s0954579402002031. [DOI] [PubMed] [Google Scholar]
- 25.Baranek GT. Autism during infancy: a retrospective video analysis of sensory-motor and social behaviors at 9–12 months of age. J Autism Dev Disord. 1999;29(3):213–224. doi: 10.1023/a:1023080005650. [DOI] [PubMed] [Google Scholar]
- 26.Mirenda P, Smith IM, Vaillancourt T, et al. Validating the Repetitive Behavior Scale-Revised in young children with autism spectrum disorder [published online April 20, 2010] J Autism Dev Disord. doi: 10.1007/s10803-010-1012-0. [DOI] [PubMed] [Google Scholar]
- 27.Jolliffe T, Baron-Cohen S. Are people with autism and Asperger syndrome faster than normal on the Embedded Figures Test? J Child Psychol Psychiatry. 1997;38(5):527–534. doi: 10.1111/j.1469-7610.1997.tb01539.x. [DOI] [PubMed] [Google Scholar]
- 28.Morgan B, Maybery M, Durkin K. Weak central coherence, poor joint attention, and low verbal ability. Dev Psychol. 2003;39(4):646–656. doi: 10.1037/0012-1649.39.4.646. [DOI] [PubMed] [Google Scholar]
- 29.Hillier A, Campbell H, Keillor J, Phillips N, Beversdorf DQ. Decreased false memory for visually presented shapes and symbols among adults on the autism spectrum. J Clin Exp Neuropsychol. 2007;29(6):610–616. doi: 10.1080/13803390600878760. [DOI] [PubMed] [Google Scholar]
- 30.Happe´ F, Frith U. The weak coherence account: detail-focused cognitive style in autism spectrum disorders. J Autism Dev Disord. 2006;36(1):5–25. doi: 10.1007/s10803-005-0039-0. [DOI] [PubMed] [Google Scholar]
- 31.Frith U. Autism: Explaining the Enigma. Oxford, England: Blackwell; 1989. [Google Scholar]
- 32.Akshoomoff NA, Courchesne E. ERP evidence for a shifting attention deficit in patients with damage to the cerebellum. J Cogn Neurosci. 1994;6(4):388–399. doi: 10.1162/jocn.1994.6.4.388. [DOI] [PubMed] [Google Scholar]
- 33.Allen G, Courchesne E. Attention function and dysfunction in autism. Front Biosci. 2001;6:D105–D119. doi: 10.2741/allen. [DOI] [PubMed] [Google Scholar]
- 34.Belmonte M. Shifts of visual spatial attention modulate a steady-state visual evoked potential. Brain Res Cogn Brain Res. 1998;6(4):295–307. doi: 10.1016/s0926-6410(98)00007-x. [DOI] [PubMed] [Google Scholar]
- 35.Townsend J, Harris NS, Courchesne E. Visual attention abnormalities in autism: delayed orienting to location. J Int Neuropsychol Soc. 1996;2(6):541–550. doi: 10.1017/s1355617700001715. [DOI] [PubMed] [Google Scholar]
- 36.Landry R, Bryson SE. Impaired disengagement of attention in young children with autism. J Child Psychol Psychiatry. 2004;45(6):1115–1122. doi: 10.1111/j.1469-7610.2004.00304.x. [DOI] [PubMed] [Google Scholar]
- 37.Townsend J, Courchesne E, Covington J, Westerfield M, Harris NS, Lyden P, Lowry TP, Press GA. Spatial attention deficits in patients with acquired or developmental cerebellar abnormality. J Neurosci. 1999;19(13):5632–5643. doi: 10.1523/JNEUROSCI.19-13-05632.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Elsabbagh M, Volein A, Holmboe K, Tucker L, Csibra G, Baron-Cohen S, Bolton P, Charman T, Baird G, Johnson MH. Visual orienting in the early broader autism phenotype. J Child Psychol Psychiatry. 2009;50(5):637–642. doi: 10.1111/j.1469-7610.2008.02051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pierce K, Redcay E. Fusiform function in children with an autism spectrum disorder is a matter of “who”. Biol Psychiatry. 2008;64(7):552–560. doi: 10.1016/j.biopsych.2008.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hadjikhani N, Joseph RM, Snyder J, Chabris CF, Clark J, Steele S, McGrath L, Vangel M, Aharon I, Feczko E, Harris GJ, Tager-Flusberg H. Activation of the fusiform gyrus when individuals with autism spectrum disorder view faces. Neuroimage. 2004;22(3):1141–1150. doi: 10.1016/j.neuroimage.2004.03.025. [DOI] [PubMed] [Google Scholar]
- 41.Wetherby A, Prizant B. Communication and Symbolic Behavior Scales Developmental Profile: First Normed Edition. Baltimore, MD: Paul H. Brookes; 2002. [Google Scholar]
- 42.Wetherby AM, Brosnan-Maddox S, Peace V, Newton L. Validation of the Infant-Toddler Checklist as a broadband screener for autism spectrum disorders from 9 to 24 months of age. Autism. 2008;12(5):487–511. doi: 10.1177/1362361308094501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Luyster R, Gotham K, Guthrie W, Coffing M, Petrak R, Pierce K, Bishop S, Esler A, Hus V, Oti R, Richler J, Risi S, Lord C. The Autism Diagnostic Observation Schedule-toddler module. J Autism Dev Disord. 2009;39(9):1305–1320. doi: 10.1007/s10803-009-0746-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mullen EM. In: Mullen Scales of Early Learning. AGS, editor. Circle Pines, MN: American Guidance Service; 1995. [Google Scholar]
- 45.Sparrow S, Balla D, Cicchetti D. Vineland Adaptive Behavior Scales: Survey Form Manual. Circle Pines, MN: American Guidance Service; 1984. [Google Scholar]
- 46.Cox A, Klein K, Charman T, Baird G, Baron-Cohen S, Swettenham J, Drew A, Wheelwright S. Autism spectrum disorders at 20 and 42 months of age: stability of clinical and ADI-R diagnosis. J Child Psychol Psychiatry. 1999;40(5):719–732. [PubMed] [Google Scholar]
- 47.Chawarska K, Klin A, Paul R, Macari S, Volkmar F. A prospective study of toddlers with ASD. J Child Psychol Psychiatry. 2009;50(10):1235–1245. doi: 10.1111/j.1469-7610.2009.02101.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kleinman JM, Ventola PE, Pandey J, Verbalis AD, Barton M, Hodgson S, Green J, Dumont-Mathieu T, Robins DL, Fein D. Diagnostic stability in very young children with autism spectrum disorders. J Autism Dev Disord. 2008;38(4):606–615. doi: 10.1007/s10803-007-0427-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van Daalen E, Kemner C, Dietz C, Swinkels SH, Buitelaar JK, van Engeland H. Inter-rater reliability and stability of diagnoses of autism spectrum disorder in children identified through screening at a very young age. Eur Child Adolesc Psychiatry. 2009;18(11):663–674. doi: 10.1007/s00787-009-0025-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised. J Autism Dev Disord. 1994;24(5):659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- 51.Ashwin E, Ashwin C, Rhydderch D, Howells J, Baron-Cohen S. Eagle-eyed visual acuity: an experimental investigation of enhanced perception in autism. Biol Psychiatry. 2009;65(1):17–21. doi: 10.1016/j.biopsych.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 52.Mottron L, Dawson M, Soulières I, Hubert B, Burack J. Enhanced perceptual functioning in autism. J Autism Dev Disord. 2006;36(1):27–43. doi: 10.1007/s10803-005-0040-7. [DOI] [PubMed] [Google Scholar]
- 53.Andari E, Duhamel JR, Zalla T, Herbrecht E, Leboyer M, Sirigu A. Promoting social behavior with oxytocin in high-functioning autism spectrum disorders. Proc Natl Acad Sci U S A. 2010;107(9):4389–4394. doi: 10.1073/pnas.0910249107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pierce K, Haist F, Sedaghat F, Courchesne E. The brain response to personally familiar faces in autism. Brain. 2004;127(pt 12):2703–2716. doi: 10.1093/brain/awh289. [DOI] [PubMed] [Google Scholar]
- 55.Adolphs R. The social brain: neural basis of social knowledge. Annu Rev Psychol. 2009;60:693–716. doi: 10.1146/annurev.psych.60.110707.163514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Blankenburg F, Ruff CC, Bestmann S, et al. Studying the role of human parietal cortex in visuospatial attention with concurrent TMS-fMRI [published online February 22, 2010] Cereb Cortex. doi: 10.1093/cercor/bhq015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Corbetta M, Kincade JM, Ollinger JM, McAvoy MP, Shulman GL. Voluntary orienting is dissociated from target detection in human posterior parietal cortex. Nat Neurosci. 2000;3(3):292–297. doi: 10.1038/73009. [DOI] [PubMed] [Google Scholar]
- 58.Klin A, Jones W, Schultz R, Volkmar F. The enactive mind, or from actions to cognition: lessons from autism. Philos Trans R Soc Lond B Biol Sci. 2003;358(1430):345–360. doi: 10.1098/rstb.2002.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pierce K, Müller RA, Ambrose J, Allen G, Courchesne E. Face processing occurs outside the fusiform ‘face area’ in autism. Brain. 2001;124(pt 10):2059–2073. doi: 10.1093/brain/124.10.2059. [DOI] [PubMed] [Google Scholar]
- 60.Kennedy DP, Courchesne E. Functional abnormalities of the default network during self- and other-reflection in autism. Soc Cogn Affect Neurosci. 2008;3(2):177–190. doi: 10.1093/scan/nsn011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Corbett BA, Carmean V, Ravizza S, Wendelken C, Henry ML, Carter C, Rivera SM. A functional and structural study of emotion and face processing in children with autism. Psychiatry Res. 2009;173(3):196–205. doi: 10.1016/j.pscychresns.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tamis-LeMonda CS, Bornstein MH. Language, play and attention at one year. Infant Behav Dev. 1990;13(1):85–98. [Google Scholar]
- 63.Nithianantharajah J, Hannan AJ. Enriched environments, experience-dependent plasticity and disorders of the nervous system. Nat Rev Neurosci. 2006;7(9):697–709. doi: 10.1038/nrn1970. [DOI] [PubMed] [Google Scholar]
- 64.Spires TL, Grote HE, Varshney NK, Cordery PM, van Dellen A, Blakemore C, Han-nan AJ. Environmental enrichment rescues protein deficits in a mouse model of Huntington’s disease, indicating a possible disease mechanism. J Neurosci. 2004;24(9):2270–2276. doi: 10.1523/JNEUROSCI.1658-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]