Abstract
All-trans retinoic acid (ATRA) induces differentiation in various cell types and has been investigated extensively for its effective use in cancer prevention and treatment. Relapsed or refractory disease that is resistant to ATRA is a clinically significant problem. To identify the molecular mechanism that bridges ATRA differentiation and resistance in cancer, we selected the multidrug-resistant leukemia cell line HL-60[R] by exposing it to ATRA, followed by sequential increases of one-half log concentration. A cytotoxicity analysis revealed that HL-60[R] cells were highly resistant to ATRA, doxorubicin, and etoposide. A comparative genome hybridization analysis of HL-60[R] cells identified gains of 4q34, 9q12, and 19q13 and a loss of Yq12 compared with in the parental HL-60 cell line. Transcriptional profiles and functional pathway analyses further demonstrated that 7 genes (FEN1, RFC5, EXO1, XRCC5, PARP1, POLR2F, and GTF2H3) that were relatively up-regulated in HL-60[R] cells and repressed in cells with ATRA-induced differentiation were related to mismatch repair in eukaryotes, DNA double-strand break repair, and nucleotide excision repair pathways. Our results suggest that transcriptional time series profiles and a functional pathway analysis of drug resistance and ATRA-induced cell differentiation will be useful for identifying promyelocytic leukemia patients who are eligible for new therapeutic strategies.
The leukemia from which the human HL-60 cell line was derived was classified in 1976 as acute progranulocytic leukemia (APL) and had several atypical features1,2,3; it has been used extensively as an in vitro model for studying cell growth and differentiation. In the presence of all trans-retinoic acid (ATRA), HL-60 cells undergo myeloid differentiation, which involves reorganization of the nucleus and cytoplasm, migration, and eventual apoptosis4. ATRA treatment was also found to increase APL cells' adhesion and invasion capabilities5. Previous studies have focused on the nuclear and cytoskeletal changes and the kinetics of protein changes in HL-60 cells with ATRA-induced differentiation6,7. A high proportion of patients with APL experience complete remission after treatment with ATRA8,9,10; however, continuous treatment causes a progressive reduction in plasma drug concentrations, which can cause clinical relapse and ATRA resistance11.
To overcome these pharmacologic effects and understand the molecular mechanisms of drug resistance so that we can initiate large-scale studies of chronic treatment with ATRA in patients with APL, we selected multi-drug-resistant (MDR) HL-60[R] cells from those that had been exposed to 10 nM ATRA after being treated with 1.0 μM ATRA for 6 days, followed by sequential increases of one-half log concentration every 2 weeks. Some retardation of growth, attended by the presence of a variable fraction of differentiated cells, was noted from inception, as determined using Gallagher's method12. This was most marked at 1.0 μM ATRA; at this concentration, a progressively expanding cell population formed in 3 months. The HL-60[R] cells were maintained at an ATRA concentration of 1.0 μM for 6 months. A bioactivity analysis showed that the cells were about 120 times more resistant to ATRA than were the parental cells. We collected all the RNA samples, from HL-60 cells with differentiation induced by 1.0 μM ATRA for 2 days, 4 days, and 6 days to MDR HL-60[R] cells with ATRA selected for 1 month, 3 months, and 6 months, and analyzed their transcriptional time series profiles, which would be undertaken to comprehensively identify defects acquired in ATRA resistance and the ATRA-induced cell differentiation response by identifying pathways that are commonly deregulated during drug resistance.
Results
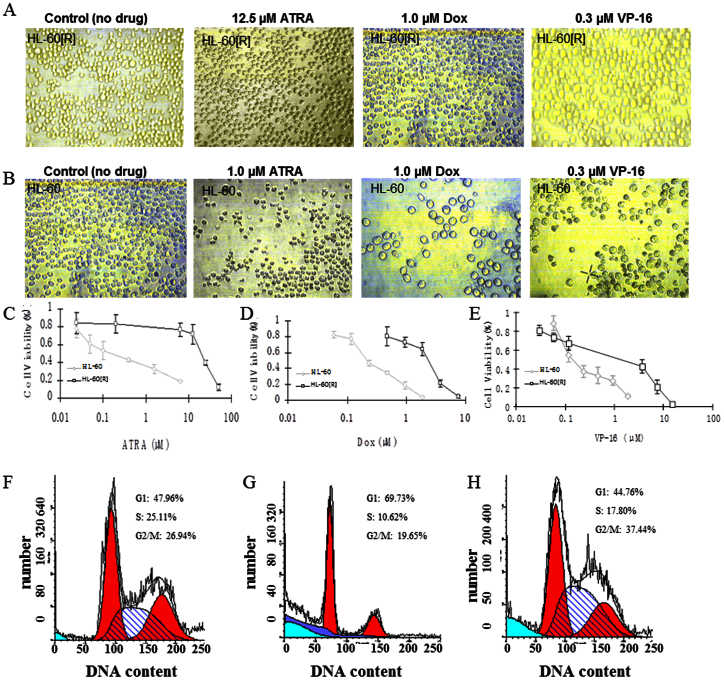
Cytotoxicity analysis of resistant HL-60[R] cells and HL-60 cells using MTT and cell cycle assays
Resistant HL-60[R] cells were derived from their parental HL-60 cells that had been treated with stepwise increasing concentrations of ATRA and maintained in 1.0 μM ATRA for 6 months. The cytotoxicities of ATRA, doxorubicin (Dox), and VP-16 (etoposide) were determined in MDR HL-60[R] cells and drug-sensitive parental HL-60 cells. MDR HL-60[R] cells were highly resistant to ATRA, doxorubicin, and VP-16 (Fig. 1A and B), with lethal doses (IC50) of 24.61 μM, 3.02 μM, and 3.12 μM, respectively. On the other hand, the IC50 of HL-60 cells treated with ATRA, doxorubicin, and VP-16 were 0.20 μM, 0.22 μM, and 0.12 μM, respectively (Fig. 1C–E and Table 1). ATRA had significant effects on HL-60 cells, and these changes in cell growth also determined the percentage of cells that were arrested at the G1/G0 phase of the cell cycle (Fig. 1F and G). However, HL-60[R] cells were not arrested at G1/G0 after 1.0 μM ATRA treatment (Fig. 1H) because of their resistance.
Figure 1. Cytotoxicity and flow cytometry analysis of HL-60[R] and HL-60 cells treated with 3 drugs (ATRA, doxorubicin [Dox], and VP-16).
(A) HL-60[R] cells treated with 12.5 μM ATRA, 1.0 μM doxorubicin, and 0.3 μM VP-16. (B) HL-60 cells treated with 1.0 μM ATRA, 1.0 μM doxorubicin, and 0.3 μM VP-16. Percentage of HL-60 and HL-60[R] cell viability after ATRA (C), doxorubicin (D), and VP-16 (E) treatment, as determined by MTT assay. Flow cytometry analysis of the effect of ATRA on the cellular DNA content of HL-60 and HL-60[R] cells. (F) HL-60 cells without ATRA. (G) HL-60 treated with 1.0 μM ATRA. (H) MDR HL-60[R] cells maintained in 1.0 μM ATRA.
Table 1. Cytotoxicity studies on HL-60 and HL-60[R] cells by MTT assay (IC50).
| HL-60 | HL-60[R] | ||
|---|---|---|---|
| Drug | IC50 | IC50 | Resistance indexa |
| ATRA | 0.20 μM | 24.61 μM | 123.05 |
| Dox | 0.22 μM | 3.02 μM | 13.73 |
| VP-16 | 0.12 μM | 3.12 μM | 26.00 |
aResistance index, ratio between the IC50 value of MDR HL-60[R] and parental HL-60 cells.
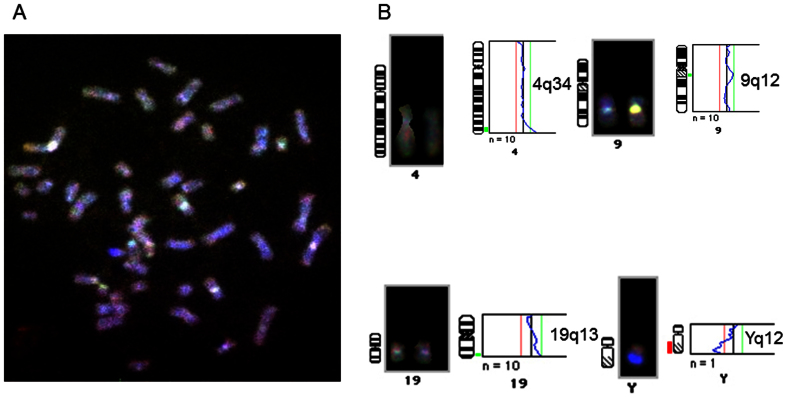
CGH studies of chromosomal gains, losses, and amplifications in HL-60[R] cells
The CGH results of MDR HL-60[R] and HL-60 cells, including 1 example of a CGH ratio profile, are shown in Fig. 2; genetic imbalances were present in HL-60 and MDR HL-60[R] cells. We identified 4 genetic changes in the MDR HL-60[R] cell line, including 1 loss (Yq12) and 3 gains (4q34, 9q12, and 19q13), compared with in its parental HL-60 cell line. We also confirmed that ZNF230, NUP62, E2-EPF, and CNOT3, which are located in 19q13, were up-regulated in MDR HL-60[R] cells compared to in their parental HL-60 cells (Table S1).
Figure 2. CGH analysis of MDR HL-60[R] and HL-60 cell lines.
(A) Representative image of CGH: MDR HL-60[R] to HL-60, (HL-60[R] labeled [spectrum green]/HL-60 labeled [spectrum red]). (B) CGH analysis shows that HL-60[R] cells have 3 chromosomal gains (4q34, 9q12, and 19q13) and 1 chromosomal loss (Yq12) compared with parental HL-60 cells.
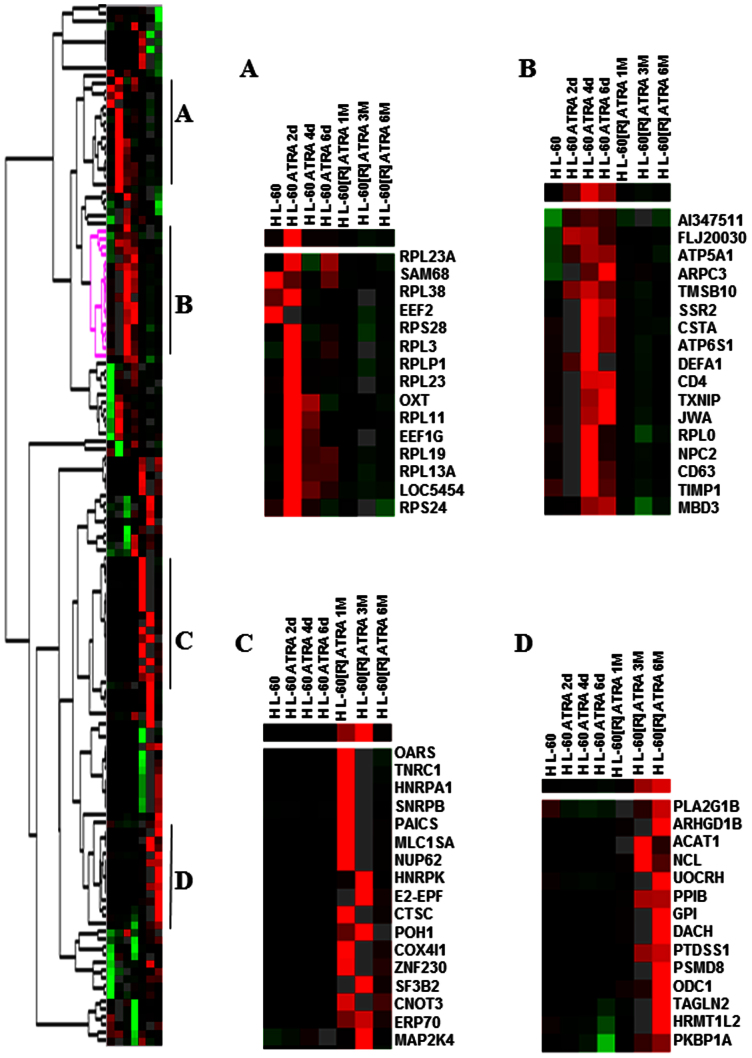
Hierarchical cluster analysis of differentially expressed genes regulated by ATRA treatment in resistant HL-60[R] and parental HL-60 cells
Using a hierarchical clustering analysis, we compared the similarities in the expression patterns of the 210 differentially expressed genes, which were differentially expressed in more than 3 samples at 7 time points (HL-60 cells treated with 1.0 μM ATRA for 2 days, 4 days, or 6 days and HL-60[R] cells maintained with 1.0 μM ATRA for 1 month, 3 months, or 6 months, compared to their parental HL-60 cells). A more than 2.0-fold change in the transcription level was used as the cut-off value for identifying the differentially expressed genes. The dendrogram, part of which is shown in Figure 3, demonstrates the relationships between genes, as calculated by the clustering algorithm. A gradual change over the 7 time points was observed after treatment with ATRA. The genes could be divided into 4 clusters. Cluster A included those genes for which mRNA levels peaked at day 2 of treatment (Fig. 3, Cluster A), including 10 ribosomal protein genes (RPL23A, RPL38, RPS28, RPL3, RPLP1, RPL23, RPL11, RPL19, RPL13A, and RPS24) and 2 eukaryotic translation elongation factors (EEF1G and EEF2) that were up-regulated by ATRA treatment (80.0% of genes in Cluster A). These genes were involved in protein synthesis and metabolism. Cluster B included genes that were expressed maximally at day 4 or day 6 (Fig. 3, Cluster B); these were biomarkers of differentiation, such as known ATRA differentiation molecules (JWA, ARPC3, TMSB10, TXNIP, and DEFA1) and CD antigens (CD4 and CD63)4. Cluster C included genes for which mRNA levels increased after ATRA treatment at 1 month, 3 months, or 6 months (OARS, TNRC1, HNRPA1, SNRPB, PAICS, MLC1SA, HNRPK, E2-EPF, CTSC, NUP62, POH1, COX4I1, ZNF230, SF3B2, ERP70, CNOT3, and MAP2K4). Cluster D included genes for which mRNA levels increased gradually over the treatment time course and were expressed maximally at 6 months (PLA2G1B, ARHGD1B, ACAT1, NCL, UOCRH, PPIB, GPI, DACH, PTDSS1, PSMD8, ODC1, TAGLN2, HRMT1L2, and PKBP1A) (Fig. 3, Cluster D). These genes are related to DNA repair, cell survival, metabolism, and drug resistance and were over-expressed in MDR HL-60[R] cells.
Figure 3. Cluster image demonstrating different classes of gene expression profiles in HL-60 and HL-60[R] cells after ATRA treatment.
We selected 210 genes whose RNA levels changed in response to 1.0 μM ATRA in HL-60 and HL-60[R] cells. (A) Cluster genes for which mRNA levels peaked at day 2 of ATRA treatment; (B) cluster genes that were expressed maximally at day 4 or day 6 of ATRA treatment; (C) cluster genes for which mRNA levels increased the ATRA treatment at 1 month, 3 months, or 6 months; and (D) cluster genes for which mRNA levels increased gradually over the ATRA treatment time course and were expressed maximally at 6 months.
Gene expression profiles in MDR HL-60[R] and HL-60 cells with ATRA-induced differentiation
The gene expression profiles of MDR HL-60R cells were compared to those of parental HL-60 cells. A more than 2.0-fold change in the transcription level was used as the cut-off value to identify the differentially expressed genes (p ≤ 0.05). We found that compared to their parental HL-60 cells, 104 genes were relatively up-regulated in ATRA-resistant HL-60[R] cells and repressed in cells with ATRA-induced differentiation; 69 genes were relatively repressed in HL-60[R] and up-regulated in differentiated HL-60 cells; 6 genes (IFNGR1, TGIF, SPAG9, CSF2RB, LRRFIP1, and SLC21A3) were up-regulated in both resistant and differentiated cells; and 20 genes were repressed in both resistant and differentiated cells (Table S1). The over-expressed genes in MDR HL-60[R] are related to DNA repair, stress response, drug resistance, the ubiquitin-proteasome pathway, and protein synthesis and metabolism, including anti-oxidation, oxidative phosphorylation, and the mitochondrial pathway.
Functional networks and pathways of ATRA-induced drug resistance were analyzed by the IPA
The genetic networks and cellular pathways were derived using the IPA program by analyzing 104 genes that were up-regulated in ATRA-resistant HL-60[R] cells. A more comprehensive network and pathway analysis of all deregulated genes revealed their association with 3 important network functions and 5 critical canonical pathways, all of which are relevant to the development of ATRA-resistant cancer. The differently expressed genes constituted about half the total molecules involved and the network-associated cellular functions and include those related to RNA post-transcriptional modification; DNA replication, recombination, and repair; cell death and survival; lipid metabolism; molecular transport; developmental disorders; hereditary disorders; and metabolic disease in resistant HL-60[R] cells (Table 2). These genes are expected to be affected in HL-60[R] cells. They belong to 5 canonical signaling pathways that are commonly deregulated in ATRA resistance (Table 3). Although only 10 (FEN1, RFC5, EXO1, XRCC5, PARP1, NME1, SET, TSTA3, POLR2F, and GTF2H3) were up-regulated in HL-60[R] cells and repressed in ATRA-induced differentiated cells with the signaling pathways (eukaryote mismatch repair, DNA double-strand break repair, granzyme A signaling, GDP-L-fucose biosynthesis I, and the nucleotide excision repair pathway), each has documented functions in controlling cell growth, and the DNA repair pathway has been implicated to play roles in ATRA-resistant HL-60[R] cells.
Table 2. Genetic networks associated with ATRA-induced cell differentiation and drug resistance.
| Top 3 ATRA networks | Score | Focus molecules | Molecules in network |
|---|---|---|---|
| Resistance | |||
| RNA post-transcriptional modification; DNA replication, recombination, and repair; cell death and survival | 55 | 24 | Akt, CD3, CD14, Ck2, CLK2, CLNS1A, CSTF2, CTDP1, cytochrome C, DDX1, EXO1, GTF2H3, histone h3, Holo RNA polymerase II, Hsp70, Hsp90, HSPA4, IFN β, ILF2, NME1, PI4KB, POLR2F, POLR3F, PRMT5, RNA polymerase II, SRPK1, SRSF3, TCEA1, TRA2B, TRAP1, TSTA3, ubiquitin, VDAC2, XRCC5, YWHAQ |
| DNA replication, recombination, and repair; lipid metabolism; molecular transport | 43 | 20 | 26s proteasome, caspase, Cg, CRABP2, cyclin A, DUSP3, EIF2S1, EIF3B, ERK1/2, FEN1, GM-CSF, GRK6, Igm, Ikβ, LAMP2, Lh, LIG1, MAP2K1/2, Mek, MMRN1, NFYA, PARP1, PEBP1, PSMB6, PSMC1, PTPRCAP, Rar, Rfc, RFC5, RUNX1, SCARB1, Sos, TCR, TMPO, UNG |
| Developmental disorder, hereditary disorder, metabolic disease | 30 | 15 | ADSL, ARL4D, ATP5G3, CAND2, CNOT3, CNOT10, CNOT11, DENND4A, DFNA5, DRG2, EML4, GBF1, GNPDA1, GNPDA2, MAN1B1, MTRR, MYO1D, PCBD1, PCK2, PGM1, RAVER1, RNF38, RNF114, RNF219, SEC62, SEC63, SPG21, SUPV3L1, TBCE, TMEM230, TNKS1BP1, TRIM52, UBC, UEVLD, ZNF263 |
| Differentiation | |||
| Cellular compromise, developmental disorder, hereditary disorder | 48 | 21 | Actin, ALB, Ap1, APOC2, CD3, CORT, DTNA, EIF2S1, ERK1/2, F actin, FBN1, FGR, FHL3, growth hormone, insulin, KLK7, KLKB1, laminin, LDL, Lh, MAP2K1/2, Mlc, MSMO1, MYO5A, NID1, NPPA, PAK1, PI3K (complex), POU2F1, PRKG1, RAB27A, SLC12A7, STX6, TGFβ, TXNIP |
| Small molecule biochemistry, neurological disease, cell death and survival | 44 | 19 | Acot1, ACOT8, AMY2B, ARMCX5, ATF5, β-estradiol, CLCA1, CLPTM1, DDIT4, DHCR7, FOS, H1FX, HTT, IL2RB, KCNAB2, MAN1A2, MST1R, NAP1L3, NEDD9, PET112, PLXNB3, REST, SLCO2B1, SPOCK1, ST8SIA5, STEAP1, THRSP, TNF, TP73, TXNIP, UBC, VASH1, VEZF1, ZNF217, ZNF616 |
| Infectious disease, cellular movement, hematological system development and function | 17 | 9 | 26s proteasome, ACO1, adenosine, Akt, APC, CEACAM6, ERK, F2RL1, FOXF1, GLS, GOT, IFN, IgG, IL-1, IL-12 (complex), IL2RB, IL3RA, interferon alpha, Jnk, KISS1, LTB, MAP3K8, Mapk, MYD88, NADPH oxidase, NF-κB (complex), NLRP3, NOX4, P38 MAPK, Pkc(s), Ras, STC2, TRAP1, uric acid, VEGF |
Table 3. Top 5 canonical pathways involving genes that are differently expressed in ATRA- differentiated HL-60 and -resistant HL-60[R] cells, as determined by Ingenuity Pathway Analysis.
| Top 5 ATRA pathways | p value | Ratio | Molecules |
|---|---|---|---|
| Resistance | |||
| Mismatch repair in eukaryotes | 4.75E-05 | 1.25E-01 | FEN1, RFC5, EXO1 |
| DNA double-strand break repair | 1.77E-03 | 1.00E-01 | XRCC5, PARP1 |
| Granzyme A signaling | 3.27E-03 | 1.00E-01 | NME1, SET |
| GDP-L-fucose biosynthesis I | 9.00E-03 | 1.43E-01 | TSTA3 |
| Nucleotide excision repair pathway | 1.09E-02 | 5.56E-02 | POLR2F, GTF2H3 |
| Differentiation | |||
| FcY receptor-mediated phagocytosis in macrophages and monocytes | 2.01E-03 | 2.83E-02 | MYO5A, PAK1, FGR |
| L-glutamine biosynthesis II (tRNA-dependent) | 5.38E-03 | 9.09E-02 | PET112 |
| Glutamine degradation I | 5.38E-03 | 2.00E-01 | GLS |
| IL-12 signaling and production in macrophages | 5.63E-03 | 1.91E-02 | ALB, MYD88, APOC2 |
| Acute phase response signaling | 1.06E-02 | 1.66E-02 | KLKB1, ALB, MYD88 |
Discussion
We challenged the MDR cancer cells in our study with retinoic acid, doxorubicin and found that they involved the activation of different mechanisms of drug metabolism and were dependent on the bioactivities of certain cancer cell lines. ATRA is known to induce the in vitro and in vivo differentiation of APL cells and favor their release from the bone marrow into the blood at the initiation of therapy. In the presence of ATRA, HL-60 human promyelocytic cells underwent myeloid differentiation. MDR HL-60[R] cells, which were highly resistant to ATRA, did not undergo cell differentiation. We demonstrated that MDR HL-60[R] cells were more than 122-, 12-, and 25-fold resistant to ATRA, doxorubicin, and VP-16, respectively, compared to parental HL-60 cells (Table 1). In addition, cell cycle arrest was not induced at the G1/G0 phase of the cell cycle in HL-60[R] cells but was induced in parental HL-60 cells with 1.0 μM ATRA treatment. Next, a CGH analysis of MDR HL-60[R] cells identified gains of 4q34, 9q12, and 19q13 and a loss of Yq12 as the most prominent alterations compared with in parental HL-60 cells. It is well recognized that resistant cells with genetic alterations possess a growth or survival advantage that leads to clonal expansion. To understand the molecular mechanism by which MDR is induced by ATRA in HL-60[R] cells, we used a DNA microarray to monitor the changeable gene expression profiles, from the cell differentiation induced by ATRA to the development of MDR; we also analyzed the functional networks and pathways of ATRA-induced cell differentiation and drug resistance.
Chromosomal 19q13 has been reported to contain several genes that are important in DNA repair–specifically, nucleotide excision repair and apoptosis mechanisms such as XPD, ERCC1, and RAI. The 19q13 chromosomal region is important in cancer13. Our microarray analysis revealed that genes in the 19q13 chromosomal region–ZNF230, NUP62, E2-EPF, and CNOT3–were constitutively over-expressed in MDR HL-60[R] cells (Table S1 and Fig. 3C). NUP62 is an essential component of the nuclear pore complex and plays a novel role in centrosome integrity. Knockdown of NUP62 induced G2/M phase arrest, mitotic cell death, and aberrant centrosome and centriole formation14. E2-EPF, named UBE2S (ubiquitin-conjugating enzyme E2S), accepts ubiquitin from the E1 complex and catalyzes its covalent attachment to other proteins before elongating ubiquitin chains on APC/C substrates to promote mitotic exit15. High expression of E2-EPF was indicative of poor overall survival in a large-scale co-expression analysis of breast cancer16. It is interesting that CNOT3 has also been associated with transcription regulation and represents a novel component of the core self-renewal and pluripotency circuitry that is conserved in mouse and human embryonic stem cells with CNOT1 and CNOT217. The chromosomal gene set enrichment analysis further confirmed that genes located at 19q13 were expressed at higher levels in uterine carcinosarcoma and contributed to its poor prognosis because of its epithelial-to-mesenchymal transition characteristics18.
In our microarray, many genes involved in the retinoic acid signaling pathway (such as RARRES2, CRABP2, MYC, TGIF, SUPV3L1, SET, ILF2, PTPRCAP, GPRK6, and SEC4L) were up-regulated in MDR HL-60[R] cells. In previous studies, RARRES2 (retinoic acid receptor responder 2 or chemerin) was over-expressed in malignant mesothelioma cells19 and adrenocortical tumors20 and was a biomarker for insulin resistance in type 2 diabetes mellitus patients21. TGIF functions as a transcriptional co-repressor and regulates developmental signaling by retinoic acid; it may also repress other RXR-dependent transcriptional responses22. Moreover, TGIF's levels are inversely correlated with survival in patients with acute myelogenous leukemia, and its knockdown inhibits the differentiation of myeloid cell lines and increases apoptosis23,24. On the other hand, retinoic acid-resistant neuroblastoma cell lines also showed over-expression of MYC with ATRA in culture medium25, and SET (SET nuclear oncogene), a potential marker for HNSCC that is associated with drug resistance, is up-regulated in 97% of tumor tissue samples and HNSCC cell lineages26.
Next, we found that the genes involved in oxidative phosphorylation and metabolism (ACAT1, ATP5G3, ARF4L, HEAB, PDHA1, and GNPI) were differentially expressed in HL-60[R] cells; other genes involved in protein synthesis metabolism, such as eukaryotic translation initiation factors (EIF2S1 and EIF3S9), transcription and elongation factors (GTF3A, CNOT3, RUNX1, and TCEA1), and splicing factors (SFRS3 and SFRS10), were also over-expressed in MDR HL-60[R] cells. ACAT1 expression may be a prognostic marker in prostate cancer: it was expressed at a significantly higher level in cancerous cores than in adjacent benign cores and was specifically effective at differentiating between indolent and aggressive forms of cancer27. Moreover, targeting ACAT1 with avasimibe (ACAT inhibitor) could be an efficient treatment for glioblastoma because it can inhibit ACAT1 expression and induce cell apoptosis28. The expression of ARF4L (adenosine diphosphate-ribosylation factor 4-like), a glioma-associated antigen, is controlled by the activated Akt/mTOR pathway, which is a downstream effect of the loss of PTEN29. HEAB (cleavage and polyadenylation factor I subunit 1) is a protein-coding gene that contains an adenosine triphosphate/guanosine triphosphate-binding motif that is homologous to the adenosine triphosphate-binding transporter superfamily or guanosine triphosphate-binding proteins30. RUNX1 may play a critical role in chemotherapy response in acute megakaryocytic leukemia by regulating the phosphoinositide 3-kinase/Akt pathway31, and ectopic RUNX reduces intracellular long-chain ceramides in NIH3T3 fibroblasts and elevated extracellular sphingosine 1 phosphate. RUNX expression also opposed the activation of c-Jun-NH(2)-kinase and p38 (mitogen-activated protein kinase) and suppressed the onset of apoptosis in response to exogenous tumor necrosis factor α32. SFRS3 (SRp20) is a serine- and arginine-rich splicing factor and proto-oncogene that is critical for cell proliferation and tumor induction and maintenance. Increased expression of SFRS3 in rodent fibroblasts promoted immortal cell growth and transformation33. However, depletion of SFRS10 resulted in apoptosis of the neural progenitor cells as well as disorganization of the cortical plate34.
It is interesting that many of the genes related to DNA repair and cell survival (NME1, DDX1, YWHAQ, PSMC1, PSMB6, E2-EPF, FEN1, RFC5, EXO1, UNG, XRCC5, ADPRT, POLR2F, Rpo1-2, and GTF2H3) are over-expressed in MDR HL-60[R] cells. Of note, POLR2F, XRCC5, and NME1 were reported to be repressed in retinoid-induced cell differentiation4. Most of these genes are related to mismatch repair in eukaryotes (FEN1, RFC5, and EXO1), DNA double-strand break repair (XRCC5 and PARP1), and the nucleotide excision repair pathway (POLR2F and GTF2H3) on IPA analysis, and they are commonly up-regulated in ATRA-resistant HL-60[R] cells. Among these DNA repair genes, FEN1 (Flap endonuclease 1) is a highly conserved structure-specific nuclease that catalyzes a specific incision to remove 5′ flaps in double-stranded DNA substrates; it plays an essential role in key cellular processes, such as DNA replication, repair, and mutation35. ADPRT (PARP1) is a critical DNA repair enzyme that is involved in DNA single-strand break repair via the base excision repair pathway. PARP inhibitors have been shown to sensitize tumors to DNA-damaging agents and selectively kill BRCA-deficient cancers36,37. XRCC5 (X-Ray repair complementing defective repair in Chinese hamster cells 5) was over-expressed in cisplatin-resistant ovarian cancer cell lines38; it also affected chemosensitivity39 and was associated with the MDR phenotype40. An immunohistochemical analysis verified significant co-expression of MDR1 and NME1 in human epithelial ovarian carcinoma41. Increased NME1 mRNA levels were associated with resistance to initial chemotherapy in acute monocytic leukemia42 and helped cells become resistant to oxidative stress43. On the other hand, higher levels of UNG (uracil-DNA glycosylase) were associated with pemetrexed resistance, and induction of UNG protein confirmed that up-regulation of the base excision repair enzyme is a feature of acquired pemetrexed resistance44. DDX1 is a member of the DEAD box protein family, which has RNase activity, plays an RNA clearance role at DNA double-strand break sites, and facilitates the template-guided repair of transcriptionally active regions of the genome45.
We also demonstrated that about 69 genes, including MYO5A, PAK1, FGR, PET112, GLS, ALB, MYD88, APOC2, and KLKB1, were up-regulated in HL-60 cells treated with ATRA and were repressed in HL-60[R] cells. The genes in cells with ATRA-induced differentiation were involved in cellular compromise, developmental and hereditary disorders, small molecule biochemistry, cell death and survival, cellular movement, hematological system development, and functional networks (Table 2). Next, we found that ATRA induced cell differentiation via pathways, including Fcy receptor-mediated phagocytosis in macrophages and monocytes (MYO5A, PAK1, and FGR), L-glutamine biosynthesis II (PET112), glutamine degradation I (GLS), interleukin-12 signaling and production in macrophages (ALB, MYD88, and APOC2), and acute-phase response signaling pathways (KLKB1, ALB, and MYD88) (Table 3). These functional networks and pathways will help us understand the disease response to retinoic acid's biological effects in promyelocytic leukemia chemotherapy.
In summary, in this study, we characterized the genes that are involved in DNA repair and cell survival, oxidative phosphorylation and metabolism, and the retinoic acid signaling pathways in ATRA-resistant HL-60[R] cells; we further revealed novel coordinated changes that occurred in resistant cells that allowed them to survive the cell differentiation and apoptosis elicited by ATRA chemotherapy. Thus, it is possible that blocking DNA repair and cell survival signaling pathways will not only enhance ATRA chemotherapy and improve the outcomes of patients with APL but also reduce the risk of second primary tumors.
Methods
Human myeloid leukemia HL-60 and HL-60[R] cell lines
The HL-60 cells were maintained in RPMI 1640 medium (Life Technologies, Inc.) containing 10% fetal calf serum, with penicillin, streptomycin, and glutamine added in a 5% CO2 humidified atmosphere at 37°C. The cultures were initiated at a density of 0.2 × 106 cells/ml in 10-ml cultures every 2 days. ATRA was added separately from 1.0 mM stock that had been dissolved in ethanol, stored away from light at −20°C, and used at a final concentration of 1.0 μM. The HL-60[R] cells were maintained with 1.0 μM ATRA.
Cytotoxicity assay
We performed an MTT (3-(4,5 dimethylthiazol-2-yl)-2,5 tetrazolium bromide) assay, which is based on the enzymatic (mitochondrial dehydrogenase) reduction of the tetrazolium salt, MTT, to a colored formazan product by viable cells46. Cells were plated in 96-well microassay culture plates at a cell density of 104 cells/well and grown overnight at 37°C in a 5% CO2 incubator. Test compounds were then added to the wells to achieve a final concentration of 10−6 to 10−4 M. Control wells were prepared by adding 100 μl of culture medium with no cells. The plates were incubated at 37°C in a 5% CO2 incubator for 72 h, and 20 μl of the stock MTT dye solution (5 mg/ml) was added to each well. After 4 h of incubation, 100 μl of DMSO was added to solubilize the MTT formazan. The optical density of each well was then measured with a microplate spectrophotometer at a wavelength of 570 nm. The IC50 was determined from the plots of the percentage viability vs. the dose of compound added.
Cell cycle analysis
To determine the cell cycle distribution, we plated 0.2 × 106 HL-60 and HL-60[R] cells in 60-mm dishes and treated them separately with 1.0 μM ATRA for 2 days. Cells were then collected and fixed in 95% ethanol, washed in 1% bovine serum albumin and phosphate-buffered saline, resuspended in 1.0 g/ml RNase and 50 μg/ml propidium iodide, incubated for 30 min in the dark at 37°C, and analyzed by flow cytometry using FACSCalibur. The data were analyzed using the ModFit DNA analysis program.
Comparative genomic hybridization and digital image analysis
Comparative genomic hybridization (CGH) was performed essentially as described previously47,48. The genomic DNA was prepared from HL-60 and HL-60[R] cells using the DNA Isolation Kit for Cells and Tissues (Boehringer Mannheim Corp., Indianapolis, IN, USA), according to the manufacturer's instructions. Slides were counterstained with DAPI and mounted with anti-fading solution (Vectashield; Vector, Burlingame, CA). CGH was performed using a digital image analysis system that contained a Zeiss Axioplan 2 microscope equipped with a Sensys cooled-charged device camera (Photometrics, Ltd., Tucson, AZ, USA), as previously described48. High copy number amplification of a chromosomal region was defined as a tumor:reference or HL-60[R]:HL-60 ratio of 1:50.
RNA extraction and gene expression profiling
RNA was isolated with Trizol LS (Invitrogen, Carlsbad, CA, USA) and purified using the RNeasy Mini Kit (Qiagen, Valencia, CA, USA). RNA quality was assessed using an Agilent 2100 Bioanalyzer (Agilent Technologies, Waldbronn, DE, USA). Microarray experiments were carried out using whole human genome oligonucleotide arrays with 20 μg of total RNA starting material, according to the manufacturer's protocol (National Cancer Institute [NCI] array). Total RNA from each sample was synthesized into double-stranded cDNA with SIII reverse transcriptase (Invitrogen) using an oligonucleotide d(T) primer. The double-stranded cDNA from HL-60 cells was labeled with Cy3 monofunctional reactive dye (Amersham Biosciences), and that from HL-60 [R] cells or ATRA-treated HL-60 cells was labeled with Cy5 monofunctional reactive dye (Amersham Biosciences). The probe was hybridized to an NCI oligonucleotide array (Hs-Operon V3-v1p24.gal) containing 36 K human transcripts (NCI Microarray Facility, Advanced Technology Center, Gaithersburg, MD) overnight at 42°C. For each treatment, the arrays were also queried with probes produced via reverse labeling, and the data were consistent with those obtained with initial standard labeling. Microarray slides were scanned with a GenePix 4000B microarray scanner (Axon Instruments, Union City, CA).
Microarray data and pathway analysis
The microarray images were analyzed with GenePix 5.1 software, and the subsequent gene lists and associated expression values were loaded into mAdb (NCI Microarray Facility). Fluorescence ratios were normalized for each array using a single scaling factor so that the median fluorescence ratio of well-measured spots on each array was 1.0. After flagging the bad spots, the mean log2-transformed ratio of resistant versus sensitive cells was calculated from triplicate experiments. The mean data were calculated using the antilog as the ratio of gene expression measures of resistant cells to parental cells and analyzed using Partek Genomics Solution software, as reported in our previous studies49. To determine the specific pathways on the basis of changes in gene expression, we used the Ingenuity Pathway Analysis (IPA) (http://www.ingenuity.com) commercial gene pathway analysis web tool.
Statistical analysis
All statistical values are presented as means ± S.D. Data were analyzed using Student's t-test. The results were considered significant at p < 0.05.
Supplementary Material
Supplementary Table S1
Acknowledgments
The work described in this paper was supported by the National Natural Science Foundation of China 81271919.
Footnotes
Author Contributions Conceived and designed the experiments: J.W., S.M.L. Performed the experiments: J.W., S.M.L. Analyzed the data: W.C., J.W. Contributed reagents/materials/analysis tools: S.M.L., W.C. Wrote the manuscript: J.W., S.M.L.
References
- Collins S. J., Gallo R. C. & Gallagher R. E. Continuous growth and differentiation of human myeloid leukaemic cells in suspension culture. Nature 270, 347–349 (1977). [DOI] [PubMed] [Google Scholar]
- Collins S. J., Ruscetti F. W., Gallagher R. E. & Gallo R. C. Terminal differentiation of human promyelocytic leukemia cells induced by dimethyl sulfoxide and other polar compounds. Proc. Natl. Acad. Sci. U. S. A. 75, 2458–2462 (1978). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton W. T. Jr et al. HL-60 cell line was derived from a patient with FAB-M2 and not FAB-M3. Blood 71, 242–247 (1988). [PubMed] [Google Scholar]
- Wang J. et al. Gene expression analysis of human promyelocytic leukemia HL-60 cell differentiation and cytotoxicity induced by natural and synthetic retinoids. Life Sci. 84, 576–583 (2009). [PubMed] [Google Scholar]
- Ovcharenko A., Granot G., Shpilberg O. & Raanani P. Retinoic acid induces adhesion and migration in NB4 cells through Pyk2 signaling. Leuk. Res. 37, 956–962 (2013). [DOI] [PubMed] [Google Scholar]
- Olins A. L., Buendia B., Herrmann H., Lichter P. & Olins D. E. Retinoic acid induction of nuclear envelope-limited chromatin sheets in HL-60. Exp. Cell Res. 245, 91–104 (1998). [DOI] [PubMed] [Google Scholar]
- Olins A. L. et al. Nuclear envelope and chromatin compositional differences comparing undifferentiated and retinoic acid- and phorbol ester-treated HL-60 cells. Exp. Cell Res. 268, 115–127 (2001). [DOI] [PubMed] [Google Scholar]
- Huang M. E. et al. Use of all-trans retinoic acid in the treatment of acute promyelocytic leukemia. Blood 72, 567–572 (1988). [PubMed] [Google Scholar]
- Castaigne S. et al. All-Trans Retinoic Acid as a Differentiation Therapy for Acute Promyelocytic Leukemia .1. Clinical-Results. Blood 76, 1704–1709 (1990). [PubMed] [Google Scholar]
- Warrell R. P. Jr et al. Differentiation therapy of acute promyelocytic leukemia with tretinoin (all-trans-retinoic acid). N. Engl. J. Med. 324, 1385–1393 (1991). [DOI] [PubMed] [Google Scholar]
- Muindi J. et al. Continuous treatment with all-trans retinoic acid causes a progressive reduction in plasma drug concentrations: implications for relapse and retinoid “resistance” in patients with acute promyelocytic leukemia. Blood 79, 299–303 (1992). [PubMed] [Google Scholar]
- Gallagher R. E. et al. Characterization of differentiation-inducer-resistant HL-60 cells. Leuk. Res. 9, 967–986 (1985). [DOI] [PubMed] [Google Scholar]
- Nissen K. K., Vogel U. & Nexo B. A. Association of a single nucleotide polymorphic variation in the human chromosome 19q13.3 with drug responses in the NCI60 cell lines. Anticancer Drugs 20, 174–178 (2009). [DOI] [PubMed] [Google Scholar]
- Hashizume C. et al. Nucleoporin Nup62 maintains centrosome homeostasis. Cell Cycle 12, 3804–3816 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnett M. J. et al. UBE2S elongates ubiquitin chains on APC/C substrates to promote mitotic exit. Nat. Cell Biol. 11, 1363–1369 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke C. et al. Correlating transcriptional networks to breast cancer survival: a large-scale coexpression analysis. Carcinogenesis 34, 2300–2308 (2013). [DOI] [PubMed] [Google Scholar]
- Zheng X. et al. Cnot1, Cnot2, and Cnot3 maintain mouse and human ESC identity and inhibit extraembryonic differentiation. Stem Cells 30, 910–922 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiyoda T. et al. Expression profiles of carcinosarcoma of the uterine corpus-are these similar to carcinoma or sarcoma. Genes Chromosomes Cancer 51, 229–239 (2012). [DOI] [PubMed] [Google Scholar]
- Mohr S. et al. Microdissection, mRNA amplification and microarray: a study of pleural mesothelial and malignant mesothelioma cells. Biochimie 86, 13–19 (2004). [DOI] [PubMed] [Google Scholar]
- Fernandez-Ranvier G. G. et al. Identification of biomarkers of adrenocortical carcinoma using genomewide gene expression profiling. Arch. Surg. 143, 841–846; discussion 846 (2008). [DOI] [PubMed] [Google Scholar]
- Syed Ikmal S. I., Zaman Huri H., Vethakkan S. R. & Wan Ahmad W. A. Potential biomarkers of insulin resistance and atherosclerosis in type 2 diabetes mellitus patients with coronary artery disease. Int. J. Endocrinol. 2013, 698567 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartholin L. et al. TGIF inhibits retinoid signaling. Mol Cell Biol. 26, 990–1001 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamid R. & Brandt S. J. Transforming growth-interacting factor (TGIF) regulates proliferation and differentiation of human myeloid leukemia cells. Mol. Oncol. 3, 451–463 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamid R., Patterson J. & Brandt S. J. Genomic structure, alternative splicing and expression of TG-interacting factor, in human myeloid leukemia blasts and cell lines. Biochim. Biophys. Acta. 1779, 347–355 (2008). [DOI] [PubMed] [Google Scholar]
- Reynolds C. P. et al. Retinoic-acid-resistant neuroblastoma cell lines show altered MYC regulation and high sensitivity to fenretinide. Med. Pediatr. Oncol. 35, 597–602 (2000). [DOI] [PubMed] [Google Scholar]
- Leopoldino A. M. et al. SET protein accumulates in HNSCC and contributes to cell survival: antioxidant defense, Akt phosphorylation and AVOs acidification. Oral Oncol. 48, 1106–1113 (2012). [DOI] [PubMed] [Google Scholar]
- Saraon P. et al. Evaluation and prognostic significance of ACAT1 as a marker of prostate cancer progression. Prostate 74, 372–380 (2014). [DOI] [PubMed] [Google Scholar]
- Bemlih S., Poirier M. D. & El Andaloussi A. Acyl-coenzyme A: cholesterol acyltransferase inhibitor Avasimibe affect survival and proliferation of glioma tumor cell lines. Cancer Biol. Ther. 9, 1025–1032 (2010). [DOI] [PubMed] [Google Scholar]
- Chi J. H. et al. Increased expression of the glioma-associated antigen ARF4L after loss of the tumor suppressor PTEN. Laboratory investigation. J. Neurosurg. 108, 299–303 (2008). [DOI] [PubMed] [Google Scholar]
- Tanabe S. et al. AF10 is split by MLL and HEAB, a human homolog to a putative Caenorhabditis elegans ATP/GTP-binding protein in an invins(10;11)(p12;q23q12). Blood 88, 3535–3545 (1996). [PubMed] [Google Scholar]
- Edwards H. et al. RUNX1 regulates phosphoinositide 3-kinase/AKT pathway: role in chemotherapy sensitivity in acute megakaryocytic leukemia. Blood 114, 2744–2752 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilbey A. et al. Runx regulation of sphingolipid metabolism and survival signaling. Cancer Res. 70, 5860–5869 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia R., Li C., McCoy J. P., Deng C. X. & Zheng Z. M. SRp20 is a proto-oncogene critical for cell proliferation and tumor induction and maintenance. Int. J. Biol. Sci. 6, 806–826 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts J. M. et al. Splicing factor TRA2B is required for neural progenitor survival. J. Comp. Neurol. 522, 372–392 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craggs T. D., Hutton R. D., Brenlla A., White M. F. & Penedo J. C. Single-molecule characterization of Fen1 and Fen1/PCNA complexes acting on flap substrates. Nucleic Acids Res. 42, 1857–1872 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandhu S. K., Yap T. A. & de Bono J. S. The emerging role of poly(ADP-Ribose) polymerase inhibitors in cancer treatment. Curr. Drug Targets 12, 2034–2044 (2011). [DOI] [PubMed] [Google Scholar]
- Lord C. J. & Ashworth A. Mechanisms of resistance to therapies targeting BRCA-mutant cancers. Nat. Med. 19, 1381–1388 (2013). [DOI] [PubMed] [Google Scholar]
- Sakamoto M. et al. Analysis of gene expression profiles associated with cisplatin resistance in human ovarian cancer cell lines and tissues using cDNA microarray. Hum. Cell 14, 305–315 (2001). [PubMed] [Google Scholar]
- Kim S. H. et al. Ku autoantigen affects the susceptibility to anticancer drugs. Cancer Res. 59, 4012–4017 (1999). [PubMed] [Google Scholar]
- Kim S. H. et al. Potentiation of chemosensitivity in multidrug-resistant human leukemia CEM cells by inhibition of DNA-dependent protein kinase using wortmannin. Leuk. Res. 24, 917–925 (2000). [DOI] [PubMed] [Google Scholar]
- Schneider J., Centeno M., Jimenez E., Rodriguez-Escudero F. J. & Romero H. Correlation of MDR1 expression and oncogenic activation in human epithelial ovarian carcinoma. Anticancer Res. 17, 2147–2151 (1997). [PubMed] [Google Scholar]
- Yokoyama A. et al. Differentiation inhibitory factor nm23 as a new prognostic factor in acute monocytic leukemia. Blood 88, 3555–3561 (1996). [PubMed] [Google Scholar]
- An R. et al. Over-expression of nm23-H1 in HeLa cells provides cells with higher resistance to oxidative stress possibly due to raising intracellular p53 and GPX1. Acta. Pharmacol. Sin. 29, 1451–1458 (2008). [DOI] [PubMed] [Google Scholar]
- Weeks L. D., Fu P. & Gerson S. L. Uracil-DNA glycosylase expression determines human lung cancer cell sensitivity to pemetrexed. Mol. Cancer Ther. 12, 2248–2260 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L., Monckton E. A. & Godbout R. A role for DEAD box 1 at DNA double-strand breaks. Mol. Cell Biol. 28, 6413–6425 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosmann T. Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J. Immunol. Methods 65, 55–63 (1983). [DOI] [PubMed] [Google Scholar]
- Guan X. Y. et al. Recurrent chromosome alterations in hepatocellular carcinoma detected by comparative genomic hybridization. Genes Chromosomes Cancer 29, 110–116 (2000). [PubMed] [Google Scholar]
- Wang J. et al. 1p31, 7q21 and 18q21 chromosomal aberrations and candidate genes in acquired vinblastine resistance of human cervical carcinoma KB cells. Oncol. Rep. 19, 1155–1164 (2008). [PubMed] [Google Scholar]
- Wang J. et al. Transcriptional analysis of doxorubicin-induced cytotoxicity and resistance in human hepatocellular carcinoma cell lines. Liver Int. 29, 1338–1347 (2009). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1