Abstract
Background
Clustering of lifestyle risk behaviours is very important in predicting premature mortality. Understanding the extent to which risk behaviours are clustered in deprived communities is vital to most effectively target public health interventions.
Methods
We examined co-occurrence and associations between risk behaviours (smoking, alcohol consumption, poor diet, low physical activity and high sedentary time) reported by adults living in deprived London neighbourhoods. Associations between sociodemographic characteristics and clustered risk behaviours were examined. Latent class analysis was used to identify underlying clustering of behaviours.
Results
Over 90% of respondents reported at least one risk behaviour. Reporting specific risk behaviours predicted reporting of further risk behaviours. Latent class analyses revealed four underlying classes. Membership of a maximal risk behaviour class was more likely for young, white males who were unable to work.
Conclusions
Compared with recent national level analysis, there was a weaker relationship between education and clustering of behaviours and a very high prevalence of clustering of risk behaviours in those unable to work. Young, white men who report difficulty managing on income were at high risk of reporting multiple risk behaviours. These groups may be an important target for interventions to reduce premature mortality caused by multiple risk behaviours.
Keywords: population-based and preventative services, public health, socioeconomic factors
Introduction
Clustering of lifestyle risk behaviours is critical to health. A longitudinal study in Norfolk, UK,1 which followed 20 244 men and women for an average of 11 years found that those who had all four lifestyle risk behaviours (smoking and non-adherence to government guidelines on alcohol consumption, diet and physical activity, respectively) were four times more likely to have died at follow-up compared with those who had none of the lifestyle risk behaviours. Similar patterns of mortality risk for clustered behaviours have been reported in a study of 11 European countries2 and in US cohorts.3,4 We therefore need to urgently know the extent of clustering in the English population and think hard about whether policies focussed on behaviour change in isolation from one another, either national or local, are really going to work.
A recent Kings Fund analysis5 of Health Survey for England data on lifestyle risk behaviours has thrown light on the distribution of lifestyle health risks in the English population, how they cluster in different populations and how this has changed over time. The core findings of the King's Fund study5 are first that risk factors do cluster systematically by age, socioeconomic class, education and to some extent gender. Furthermore, a study of adults in the east of England has demonstrated that clustering of risk behaviours is more prevalent in deprived areas.6
The King's Fund study5 argued that in the new public health system both central and local government need to be much smarter in their understanding of clustering, and the policy and practice response to it if the government's stated aim of improving the health of the poorest fastest’7 is to be met. It also argued that local areas could make much more effective use of their own health and lifestyle surveys by applying ‘a clustering lens’ to how lifestyles are distributed to understand the nature of clustering in local areas and what this implies for local policies and practice. This paper takes on that challenge for deprived neighbourhoods in London, using data from a 2008 household survey of >4000 residents in 40 of London's most deprived neighbourhoods.
Materials and methods
Data source
Data were taken from the adult baseline survey of the Well London cluster randomized trial (CRT), details and results of which are reported elsewhere.8–10 Within the Well London CRT, a pair of census lower super output areas (LSOAs) among the 11% most deprived (based on the English Indices of Multiple Deprivation) across London were selected in each of 20 London boroughs. This study used data from the household adult survey collected in all of the 40 selected LSOAs during 2008.
Defining risk behaviours
The Well London baseline survey data set contains information about five unhealthy behaviours: (i) smoking status, (ii) alcohol consumption, (iii) low fruit/vegetable consumption, (iv) low levels of physical activity and (v) sedentary time. Current smoking behaviour was ascertained by a simple yes/no question ‘are you a daily smoker?’, as commonly used in the Health Survey for England.11 Self-reported alcohol consumption was recorded using an item from previous studies of health behaviours in London,12 dichotomized as 1 = ‘drink heavily’, ‘drink quite a lot’ or ‘drink a moderate amount’; 0 = ‘drink a little’, ‘hardly drink at all’ or ‘never drink alcohol’. Validated measures of healthy eating (food frequency questionnaire adapted from the Health Survey for England 200811) were used to create a binary indicator for meeting the Department of Health's recommended minimum of five portions of fruit or vegetables per day.13 The international physical activity questionnaire—short form (IPAQ-SF)14—was used to generate a binary variable analogous to meeting the levels of physical activity (5 × 30 min of at least moderate intensity) recommended by the chief medical officer for England:15,16 1 = does not meet physical activity recommendations; 0 = meets physical activity recommendations. Data on sedentary time was obtained using a single item from the IPAQ-SF that asks respondents to recall the total time they have spent sitting at any time on a weekday. More than 4 h sitting time per day is generally considered excessive;17 therefore, a binary variable was generated using IPAQ-SF data: 1 = more than 4 h sitting time on a weekday; 0 = 4 h or less sitting time on a weekday.
Data analyses
Data on the five risk behaviours were used to derive variables to describe the number of risk behaviours in each respondent (0–5) and patterns of risk behaviours (all possible combinations of risk behaviours). Logistic regression models were used to examine associations between risk behaviours, each sociodemographic factor. Ordered logistic regression models were used to examine associations between sociodemographic factors and number of risk behaviours (count of risk behaviours). Robust standard errors were used to account for within neighbourhood clustering of the sample. Logit regression models were used to examine relationships between risk behaviours. Odds ratios (OR) from these logit regression models were converted into predicted probabilities .
We used latent class analyses to discover underlying clustering of people according to the multiple risk behaviours they adopt. We tested the data for two, three, four and five classes. While there were from two to four classes, the models showed significant differences, and there were no differences between solutions with four classes and five classes. Therefore, we chose the four classes. We studied the behavioural profile of each class by looking at the proportion of individuals exhibiting the different behaviours. We also used multinomial logistic regression with robust standard errors to predict the relative risk of belonging to the different classes based on sociodemographic variables. All data analyses were conducted in Stata v.11 and Mplus v.7.
Missing data
Descriptive analyses were conducted using complete cases. Analyses in other steps were conducted using multiple imputation to account for missing data. Details of how the multiple imputation models were specified have been published previously.9 Proportions of missing data are shown in Supplementary data, File S1.
Results
Ninety-three per cent of men and 92% of women reported at least one risk behaviour and 70% of men and 66% of women reported two or more than two risk behaviours. Supplementary data, File S2 show the proportion of men and women who reported zero to five risk behaviours.
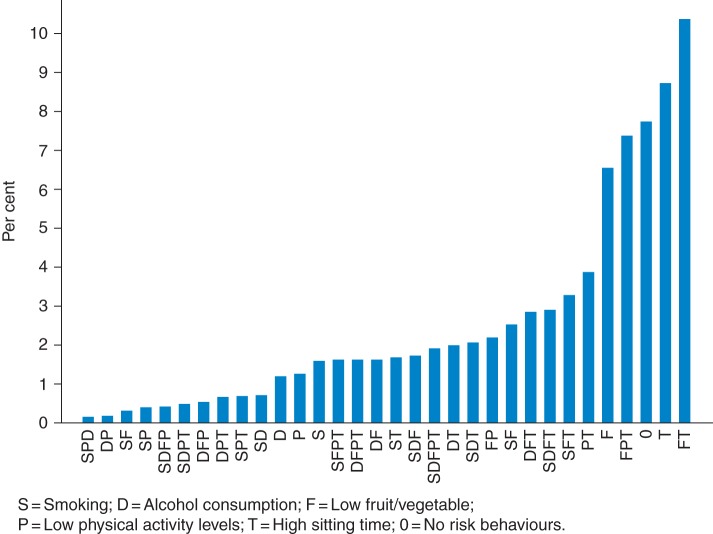
Figure 1 shows the prevalence of all possible combinations of risk behaviours, where for example, ‘S’ represents daily smoking but no other risk behaviours and ‘SD’ represents daily smoking and moderate/high alcohol consumption but no other risk behaviours. Low fruit and vegetable consumption together with high sedentary time was the most commonly reported combination of risk behaviours for both men (9.6%) and women (11.4%). In Supplementary data, Files S3 and S4, these figures are presented using only the four risk behaviours included in the King's Fund analysis (without the addition of sedentary time).
Fig. 1.
Prevalence of combinations of behavioural risk factors.
Evidence for the extent to which risk behaviours were ‘clustered’ is shown in Table 1 where predicted probabilities from logit regression models show the probability of a respondent reporting a specific risk behaviour given that they had reported another specific risk behaviour or combination of risk behaviours. For example, for respondents that reported moderate/high alcohol consumption (D), the probability of them reporting being a daily smoker (S) was 0.8. There are many instances shown in Table 1 where combinations of risk behaviours predicted other risk behaviours, for example, respondents who reported daily smoking and high sedentary time, the probability of reporting moderate/high alcohol consumption was 0.79.
Table 1.
Predicted probabilities for associations between risk behaviours
| Existing behaviour | Smoking (S) | Drinking (D) | Low fruit/vegetable consumption (F) | Low physical activity (P) | High sitting time (T) |
|---|---|---|---|---|---|
| S | |||||
| D | 0.8 | ||||
| F | 0.57 | 0.57 | |||
| P | 0.48 | 0.47 | 0.62 | ||
| T | 0.49 | 0.54 | 0.54 | 0.67 | |
| SD | 0.58 | 0.48 | 0.57 | ||
| SF | 0.77 | 0.49 | 0.49 | ||
| SP | 0.72 | 0.62 | 0.66 | ||
| ST | 0.79 | 0.57 | 0.55 | ||
| DF | 0.77 | 0.54 | 0.52 | ||
| DP | 0.77 | 0.67 | 0.64 | ||
| DT | 0.77 | 0.55 | 0.51 | ||
| FP | 0.48 | 0.51 | 0.65 | ||
| FT | 0.53 | 0.55 | 0.66 | ||
| PT | 0.49 | 0.47 | 0.61 | ||
| SDF | 0.54 | 0.53 | |||
| SDP | 0.54 | 0.65 | |||
| SDT | 0.55 | 0.52 | |||
| SFP | 0.76 | 0.68 | |||
| SFT | 0.77 | 0.57 | |||
| SPT | 0.71 | 0.66 | |||
| DFP | 0.74 | 0.62 | |||
| DFT | 0.76 | 0.58 | |||
| DPT | 0.74 | 0.65 | |||
| FPT | 0.5 | 0.5 | |||
| SDFP | 0.66 | ||||
| SDFT | 0.58 | ||||
| SDPT | 0.68 | ||||
| SFPT | 0.75 | ||||
| DFPT | 0.75 |
Emboldened figures represent statistically significant probabilities at P-values ≤ 0.001.
Table 2 shows the association between each risk behaviour and sociodemographic factors (logistic regression) and associations between the count of risk behaviours and sociodemographic factors (ordered logistic regression). These results show that there was considerable variation in odds ratios (and thus prevalence of different individual and multiple risk factors) across groups. In terms of individual risk factors for example, women were more likely to have low physical activity, but less likely to report smoking or moderate/high alcohol consumption than men; compared with 16–24 year olds, 25–54 year olds were more likely to report smoking and moderate/high alcohol consumption, and increasing age was associated with lower physical activity levels; those unable to work reported higher prevalences of low fruit and vegetable consumption, low physical activity, high sedentary time and were more likely to smoke than those in paid employment; and rates of moderate/high alcohol consumption were uniformly lower for all ethnic groups compared with the white ethnic group.
Table 2.
Relationships between sociodemographic factors and risk behaviours and latent classes of risk behaviours
| Sociodemographic factor | Smoker | Moderate to high alcohol | Low fruit and vegetable | Low physical activity | High sitting time | Count of risks (ordered logistic) |
Latent class (multinomial logistic regression) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Minimal behaviours |
Smokers |
Maximal behaviours |
Sedentary lifestyle |
|||||||||||||||
| OR | OR | OR | OR | OR | OR | n | % | RRR | n | % | RRR | n | % | RRR | n | % | RRR | |
| Sex (Male) | Ref | Ref | Ref | Ref | Ref | Ref | 486 | 43.4 | Ref | 124 | 48.3 | Ref | 569 | 60.4 | Ref | 636 | 37.1 | Ref |
| Female | 0.54*** | 0.42*** | 0.98 | 1.66*** | 0.90 | 0.76*** | 634 | 56.6 | Ref | 133 | 51.8 | 0.82 | 373 | 39.6 | 0.51*** | 1080 | 62.9 | 1.34*** |
| Age (16–24) | Ref | Ref | Ref | Ref | Ref | Ref | 240 | 23.4 | Ref | 44 | 19.9 | Ref | 163 | 18.9 | Ref | 329 | 20.7 | Ref |
| 25–34 | 1.36* | 1.56** | 0.80* | 1.24 | 1.06 | 1.16 | 274 | 26.7 | Ref | 79 | 35.6 | 1.22 | 256 | 29.6 | 0.91 | 409 | 25.8 | 1.18 |
| 35–44 | 1.41* | 1.66** | 0.91 | 1.59*** | 0.93 | 1.37* | 219 | 21.3 | Ref | 42 | 18.9 | 0.69 | 229 | 27.0 | 0.89 | 317 | 20.0 | 0.99 |
| 45–54 | 1.57** | 1.58* | 0.68** | 1.60** | 0.91 | 1.17 | 132 | 12.9 | Ref | 30 | 13.5 | 0.82 | 112 | 13.0 | 0.62** | 180 | 11.3 | 0.88 |
| 55–64 | 1.19 | 1.42 | 0.88 | 2.46*** | 0.93 | 1.37* | 83 | 8.1 | Ref | 16 | 7.2 | 0.62 | 60 | 6.9 | 0.42** | 129 | 8.1 | 0.75 |
| 65+ | 0.76 | 0.91 | 1.00 | 3.54*** | 1.50* | 1.60*** | 80 | 7.8 | Ref | 11 | 5.0 | 0.47 | 44 | 5.1 | 0.26*** | 224 | 14.1 | 1.00 |
| Ethnicity (White) | Ref | Ref | Ref | Ref | Ref | Ref | 426 | 37.9 | Ref | 138 | 55.0 | Ref | 578 | 62.4 | Ref | 645 | 37.9 | Ref |
| Black | 0.35*** | 0.44*** | 1.16 | 0.99 | 0.81 | 0.54*** | 387 | 34.5 | Ref | 53 | 21.2 | 0.42** | 201 | 21.7 | 0.41*** | 585 | 34.4 | 1.24 |
| Asian | 0.26*** | 0.17*** | 0.89 | 1.06 | 0.92 | 0.43*** | 187 | 16.7 | Ref | 24 | 9.6 | 0.28** | 62 | 6.7 | 0.18*** | 328 | 19.3 | 1.21 |
| Mixed | 0.69 | 0.48** | 1.01 | 0.67 | 0.59** | 0.52*** | 65 | 5.8 | Ref | 20 | 7.9 | 0.70 | 38 | 4.1 | 0.35*** | 68 | 4.0 | 0.83 |
| Other | 0.74 | 0.52* | 0.59** | 1.09 | 0.62 | 0.46*** | 58 | 5.16 | Ref | 16 | 6.4 | 0.59 | 48 | 5.2 | 0.62 | 77 | 4.5 | 1.13 |
| Highest education level (Primary) | Ref | Ref | Ref | Ref | Ref | Ref | 98 | 9.3 | Ref | 24 | 10.0 | Ref | 74 | 8.6 | Ref | 185 | 12.4 | Ref |
| Secondary (GCSE or equivalent) | 1.09 | 1.36 | 1.57** | 0.62** | 1.09 | 1.16 | 314 | 29.7 | Ref | 97 | 40.3 | 1.13 | 297 | 34.5 | 1.13 | 515 | 34.5 | 1.01 |
| A’ Level or equivalent | 0.87 | 1.41 | 1.36* | 0.42*** | 1.37 | 0.96 | 298 | 28.2 | Ref | 60 | 24.9 | 0.68 | 248 | 28.8 | 1.01 | 363 | 24.3 | 0.74 |
| Higher (university degree) | 0.67** | 1.58* | 1.07 | 0.42*** | 1.50* | 0.93 | 335 | 31.7 | Ref | 59 | 24.5 | 0.58 | 236 | 27.4 | 0.78 | 414 | 27.7 | 0.83 |
| Other | 0.84 | 0.47 | 0.77 | 0.82 | 0.83 | 0.79 | 11 | 1.0 | Ref | 1 | 0.4 | 0.34 | 6 | 0.7 | 0.72 | 18 | 1.2 | 0.86 |
| Job status (Working 30+ hours/week) | Ref | Ref | Ref | Ref | Ref | Ref | 344 | 31.9 | Ref | 81 | 33.5 | Ref | 338 | 37.6 | Ref | 386 | 24.0 | Ref |
| Working under 30 h per week | 0.84 | 0.74** | 0.87 | 1.04 | 0.99 | 0.84 | 163 | 15.1 | Ref | 32 | 13.2 | 0.96 | 133 | 14.8 | 0.99 | 199 | 12.3 | 1.11 |
| Unpaid housework | 0.96 | 0.41*** | 0.75 | 1.61** | 0.52* | 0.58** | 67 | 6.2 | Ref | 22 | 9.1 | 1.57 | 37 | 4.1 | 0.78 | 84 | 5.2 | 0.99 |
| Full-time education | 0.36*** | 0.22*** | 1.23 | 1.05 | 1.04 | 0.61** | 172 | 15.9 | Ref | 19 | 7.9 | 0.47 | 53 | 5.9 | 0. 36** | 246 | 15.2 | 1.28 |
| Unemployed | 1.31 | 0.57*** | 1.43** | 1.35 | 0.95 | 1.10 | 194 | 18.0 | Ref | 67 | 27.7 | 1.53 | 202 | 22.5 | 1.18 | 300 | 18.6 | 1.21 |
| Retired | 0.62** | 0.49*** | 1.14 | 3.10*** | 1.55* | 1.26 | 88 | 8.2 | Ref | 11 | 4.5 | 0.74 | 62 | 6.9 | 1.42 | 237 | 14.7 | 2.05** |
| Unable to work/ill/disabled | 1.57* | 0.76 | 1.76** | 6.03*** | 2.67*** | 3.20*** | 22 | 2.0 | Ref | 2 | 0.8 | 0.35 | 61 | 6.8 | 2.62*** | 133 | 8.3 | 4.15*** |
| Managing on income (difficult) | Ref | Ref | Ref | Ref | Ref | Ref | 528 | 49.2 | Ref | 149 | 61.1 | Ref | 462 | 51.1 | Ref | 774 | 48.2 | Ref |
| Easy or very easy | 0.70*** | 1.12 | 0.96 | 0.94 | 1.42 | 1.04 | 546 | 50.8 | Ref | 95 | 38.9 | 0.69* | 442 | 48.9 | 0.84 | 831 | 51.8 | 1.05 |
OR, odds ratio; RRR, relative risk ratio.
*P < 0.05.
**P < 0.01.
***P < 0.001.
Results from the ordered logistic regression of the count of risk behaviours showed that women had significantly lower odds of reporting a higher number of risk behaviours than men. Compared with respondents aged 16–24 years, those aged 35–44, 55–64 and over 65 years had higher odds of reporting more risk behaviours. White respondents had significantly higher odds of reporting more risk behaviours compared with all other ethnic groups. Respondents who reported being unable to work, ill or disabled had more than three times higher odds of reporting more risk behaviours compared with those working >30 h per week. We did not find evidence of associations between education status or ease of managing on income and total number of risk behaviours reported.
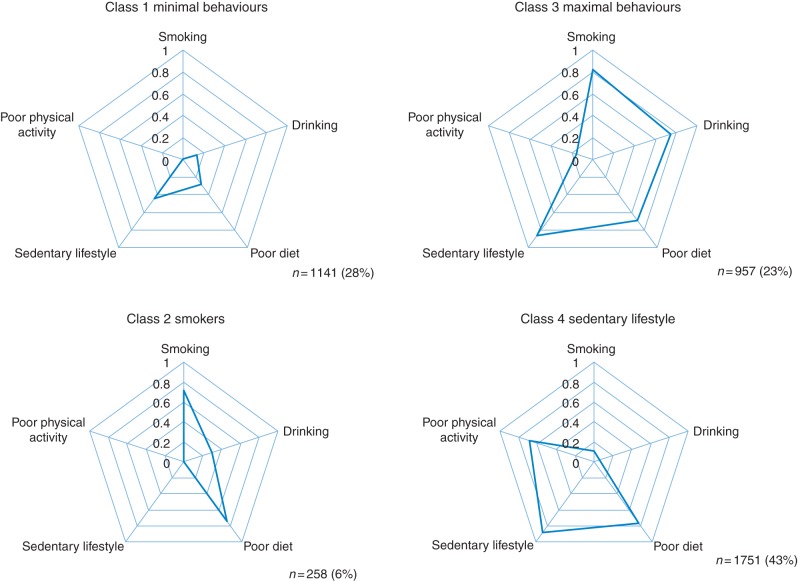
The latent class analysis revealed four latent classes. Figure 2 shows the profile of behaviours in each class. In Class 1, there were a minimal amount (<20%) of smoking, poor diet and sedentary behaviours (class label: ‘minimal behaviours’). In Class 2, the majority smoked, reported low fruit and vegetable consumption and about a third also reported high alcohol consumption (class label: ‘smokers’). In the third class, all behaviours except poor physical activity were exhibited by the majority (class label: ‘maximal behaviours’). Finally, in the largest class, Class 4, the majority reported high sedentary time, low fruit and vegetable consumption and low physical activity levels (class label: ‘sedentary lifestyle’). The classes were labelled according to these profiles.
Fig. 2.
Behavioural profile of different classes of individuals according to multiple behaviours.
The sociodemographic profiles of these classes are shown in Table 2. Table 2 also shows the relative risk of belonging in each class according to sociodemographic factors. Compared with the minimal behaviours class, respondents who were younger, male, white and unable to work were at greater risk of membership of the maximal behaviours class. Being white and unable to work was associated with greater risk of membership of the ‘smokers’ class.
Discussion
Main findings of this study
Our analyses suggest that there is clustering of risk behaviours in this survey sample in deprived London neighbourhoods. Daily smoking and moderate/high alcohol consumption were most strongly correlated and respondents reporting combinations of two, three or four risk behaviours were more likely to report further risk behaviours. Four classes of behaviours were identified using latent class analysis: ‘sedentary lifestyle’, ‘minimal risk behaviours’, ‘maximal risk behaviours’ and ‘smokers’. The largest class was the sedentary class, and those at highest risk of membership of this class were female and retired or unable to work. Compared with the minimal behaviours class, membership of the maximal risk behaviours class was associated with being younger, white, male and unable to work.
What is already known on this topic
Our findings suggest that only 8% of respondents to the survey had none of the five lifestyle risk behaviours examined here. This is slightly higher than the King's Fund analysis of Health Survey for England Data,5 which found 4% in 2003 and 6% in 2008. The King's Fund analyses focussed on clustering of four behaviours, whereas our analyses have additionally included analysis of sedentary time. Although our results and the national results from the King's Fund study are not directly comparable for this and other reasons, our findings are worth comparing and discussing further.
We find that rates of low reported physical activity are considerably lower than in the Health Survey for England data which the King's Fund used. The King's Fund found a complex relationship between risk behaviours and age, and speculated that this may be due to a combination of age and survivor effects. We report similar findings, with the odds of a higher number of risk behaviours highest in 35–44, 55–64 and over 65 year olds suggestive of life-course trajectories of risk. The King's Fund's national study did not assess ethnicity specifically. However, we find ethnicity is important, with Black, Asian and Mixed ethnicity associated with a lower number of risk behaviours. Much of this effect may be driven by their lower smoking and alcohol consumption rates reflecting differences in cultural attitudes to tobacco and alcohol.
We found that in this population living in deprived parts of London, educational attainment does not explain risk behaviour clustering after adjusting for other sociodemographic factors. This contrasts with the national findings from the King's Fund study. It could be that the effect of education is being picked up in other variables, for instance in the employment or income variables. However, it could also be that education is less ‘protective’ in this population living in deprived neighbourhoods, from taking on multiple risk behaviours. Evidence from a review of large data sets on determinants’ risk behaviours18 suggests that large proportions of the variance by education in individual risk behaviours can be accounted for by differences in characteristics not examined in this study, including family background, social networks, knowledge and cognitive ability.
What this study adds
One of the starkest findings in this study is that people who report unable to work have more than three times higher odds of reporting a higher number of risk behaviours than those in full-time paid employment and more two and a half times the risk of belonging to the maximal behaviours class. Sixty-seven per cent of those unable to work, ill or disabled reported at least three risk behaviours. The latent class analyses also revealed that after adjusting for other sociodemographic factors, those who were not in employment were more likely to report a lifestyle characterized by high sedentary time, low levels of physical activity and low fruit and vegetable consumption. This raises politically sensitive questions of cause and effect, whether their lifestyles have led them into inability to work, or inability to work has led to poor lifestyles. Clearly, there is likely to be an element of both, and getting to the root cause will be important for designing appropriate solutions.
What is clear for local authorities as they take up their new roles for health improvement in London is that members of these behavioural risk classes are at very high risk of premature mortality due to lifestyle clustering and should be a priority for targeted action. Is there any sign of this yet? At a strategic level, we would hope to see this in Health and Wellbeing Board's strategies. The Local Government Association has recently developed a summary tool.19 Using this we searched for combinations of priorities focussing on alcohol and substance abuse, healthy living, obesity in adults, smoking, health inequalities and prevention and early intervention. All boroughs, except Brent and Richmond upon Thames, mentioned at least one of these as priorities, and four, Barking and Dagenham, Hillingdon, Kingston upon Thames and Merton, had four or more of these six areas as priorities. Yet, looking in depth at their strategies, the concept of how their populations experience behaviours as clusters—and the response—is either absent or inadequately expressed as part of the narrative of these core strategic plans.
This does not mean there are not pockets of relevant activity in these boroughs (for instance, Merton's LiveWell service20) or their local NHS, or indeed elsewhere, but it seems it is not part of mainstream strategy to take clustering of behaviours into account when deciding on how to set and implement prevention and public health plans locally. We agree with the King's Fund, that if we want to improve the health of London's poorest fastest, we need to understand and target behaviour change strategies and implement them in a way that populations actually experience them, rather than relying solely on blanket single behaviours approaches, one by one. There is little sign that this is happening yet. There could be a task for the new London Health Board,21 given its role to bring leadership to issues of pan-London significance. But, the London Health Board or others will need additional insight and evidence to shape their actions.
Further research is needed to identify other determinants of clustered behaviours. Theories of motivation and addiction suggest that certain psychological characteristics may explain underlying causes of behaviours.22 Furthermore, social ecological theories23 describing the interaction between these individual psychological characteristics and social and environmental cues to behaviour may be useful in guiding future research into determinants of clustered risk behaviours and interventions to target these clustered behaviours.
Limitations of this study
The cross-sectional design of this study prevents us from making inferences about the causal directions of the associations reported. For example, it is not clear whether clustered risk behaviours are adopted simultaneously or whether the adoption of one risk behaviour subsequently leads to the adoption of further risk behaviours. The high levels of physical activity reported in this sample are likely to result from problems with overestimation from the IPAQ-SF that have recently been reported in a systematic review of validation studies.24 The measure of physical activity in the Health Survey for England that the King's Fund used is a self-report recall measure similar to the IPAQ-SF. However, unlike the IPAQ-SF, there are not substantial concerns about the validity of physical activity measure used in the Health Survey for England.
It is also worth noting some strengths of the methods applied in this study. Previous studies examining clustering of risk behaviours25 have used approaches that have either analysed co-occurrence of risk behaviours or associations between co-occurring risk behaviours. We have used these approaches but have additionally examined underlying clustering of behaviours through analysis of latent class membership and looked at risk of class membership according to sociodemographic factors. This may be an additional helpful way to target activity.
Supplementary data
Funding
This work was supported by the Wellcome Trust [083679/Z/07/Z].
Supplementary Material
Acknowledgements
We are very grateful for the contributions of numerous fieldworkers to the collection of the household survey data. We thank members of the Well London evaluation team for their contributions to the data collection and preparation processes.
References
- 1.Khaw K-T, Wareham N, Bingham S et al. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med 2008;5(1):e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knoops KT, de Groot LC, Kromhout D et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA 2004;292(12):1433–9. [DOI] [PubMed] [Google Scholar]
- 3.Ford ES, Bergmann MM, Boeing H et al. Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Prev Med 2012;55(1):23–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Dam RM, Li T, Spiegelman D et al. Combined impact of lifestyle factors on mortality: prospective cohort study in US women. BMJ 2008;337(7672):a1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buck D, Frosini F. Clustering of Unhealthy Behaviours Over Time. Implications for Policy and Practise. London, UK: The King's Fund, 2012. [Google Scholar]
- 6.Lakshman R, McConville A, How S et al. Association between area-level socioeconomic deprivation and a cluster of behavioural risk factors: cross-sectional, population-based study. J Public Health 2011;33(2):234–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Department of Health. Healthy Lives, Healthy People: our strategy for public health in England. Norwich, UK: The Stationery Office, 2010. [Google Scholar]
- 8.Wall M, Hayes R, Moore D et al. Evaluation of community level interventions to address social and structural determinants of health: a cluster randomised controlled trial. BMC Public Health 2009;9(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Phillips G, Renton A, Moore DG et al. The Well London program - a cluster randomized trial of community engagement for improving health behaviors and mental wellbeing: baseline survey results. Trials 2012;13(1):105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Phillips G, Bottomley C, Schmidt E et al. Well London Phase - 1: results among adults of a cluster-randomised trial of a community engagement approach to improving health behaviours and mental well-being in deprived inner-city neighbourhoods. J Epidemiol Community Health 2014;68(7):606–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NHS Information Centre. Health Survey for England 2008: statistics on obesity, physical activity and diet. London, UK: NHS Information Centre, 2008. [Google Scholar]
- 12.Clark C, Haines MM, Head J et al. Psychological symptoms and physical health and health behaviours in adolescents: a prospective 2-year study in East London. Addiction 2007;102(1):126–35. [DOI] [PubMed] [Google Scholar]
- 13.Department of Health. 5 a day 2014. http://www.nhs.uk/Livewell/5ADAY/Pages/5ADAYhome.aspx (14 March 2014, date last accessed).
- 14.Craig CL, Marshall AL, Sjöström M et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35(8):1381. [DOI] [PubMed] [Google Scholar]
- 15.Department of Health. Start Active, Stay Active: a report on physical activity for health from the four home countries’ Chief Medical Officers. London, UK: Department of Health, 2011. [Google Scholar]
- 16.Donaldson L. Physical activity health improvement and prevention: at least 5 a week – a report from the Chief Medical Officer. Norwich, UK: HM Stationery Office, 2004. [Google Scholar]
- 17.Biddle S, Cavil N, Eklund U et al. Sedentary Behaviour and Obesity: Review of the Current Scientific Evidence. London, UK: Deparment of Health, 2010. [Google Scholar]
- 18.Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. J Health Econ 2010;29(1):1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Local Government Association. Health and Wellbeing Board prioirities across England. Local Government Association, 2014. http://www.local.gov.uk/health-and-wellbeing-boards/-/journal_content/56/10180/6111055/ARTICLE (15 June 2014, date last accessed). [Google Scholar]
- 20.LiveWell Merton, 2014. https://www.live-well.org.uk/merton (15 June 2014, date last accessed).
- 21.London Health Board. What is the London Health Board? http://www.londonhealthboard.org.uk/about/default.htm (15 June 2014, date last accessed).
- 22.Walters ST, Rotgers F. Treating Substance Abuse: Theory and Technique. New York: Guilford Press, 2011. [Google Scholar]
- 23.Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer B, Viswanath K (eds). Health Behaviour and Health Education: Theory, Research and Practice. Jossy-Bass, 2007. [Google Scholar]
- 24.Lee PH, Macfarlane DJ, Lam T et al. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act 2011;8(1):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McAloney K, Graham H, Law C et al. A scoping review of statistical approaches to the analysis of multiple health-related behaviours. Prev Med 2013;56(6):365–71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.