Abstract
Objective
To assess whether clinical characteristics and simple biomarkers of beta cell failure are associated with individual variation in glycemic response to GLP-1 receptor agonist therapy in patients with type 2 diabetes.
Research Design and Methods
We prospectively studied 620 participants with type 2 diabetes and HbA1c ≥58mmol/mol (7.5%) commencing GLP-1 receptor agonist therapy as part of their usual diabetes care and assessed response to therapy over 6 months. We assessed the association between baseline clinical measurements associated with beta cell failure and glycemic response (HbA1c change 0 to 6 months, primary outcome) with change in weight (0 to 6 months) as a secondary outcome using linear regression and ANOVA with adjustment for baseline HbA1c and co-treatment change.
Results
Reduced glycemic response to GLP-1R agonists was associated with longer duration diabetes, insulin co-treatment, lower fasting C-peptide, lower post meal urine C-peptide creatinine ratio and positive GAD or IA2 islet autoantibodies (p≤0.01 for all). Participants with positive autoantibodies or severe insulin deficiency (fasting C-peptide ≤0.25nmol/L) had markedly reduced glycemic response to GLP-1RA therapy (autoantibodies: mean HbA1c change -5.2 vs -15.2 mmol/mol (-0.5 vs -1.4%), p=0.005 C-peptide <0.25nmol/L: mean change -2.1 vs -15.3mmol/mol (-0.2 vs -1.4%), p=0.002). These markers were predominantly present in insulin treated participants and were not associated with weight change.
Conclusions
Clinical markers of low beta cell function are associated with reduced glycemic response to GLP-1R agonist therapy. C-peptide and islet autoantibodies represent potential biomarkers for the stratification of GLP-1R agonist therapy in insulin treated diabetes.
Introduction
The GLP-1 receptor agonists (GLP-1RA) are effective glucose lowering therapies commonly prescribed for patients with type 2 diabetes, typically as second or third line agents in combination with metformin and /or other oral therapy, or in combination with insulin (1–3). These treatments are associated with weight loss and have a low risk of hypoglycemia in comparison to older therapies (4). However in the absence of clear difference in effectiveness and long term outcome the choice of second and third line therapy in type 2 diabetes remains a subject of considerable debate (2; 5).
The glycemic response to GLP-1 receptor agonists is highly variable, with some individuals achieving very marked response but others achieving no improvement in HbA1c (3; 6; 7). While some of this variability will relate to lifestyle change, medication adherence and measurement imprecision it is likely that there will also be biological mechanisms contributing to this treatment response variation. Type 2 diabetes is a highly heterogeneous disease with likely different pathologies (8) and biomarker predictors of response to glucose lowering therapies have been identified (9). Identifying clinical features or biomarkers predictive of response may help target treatment to those most likely to benefit, this would be particularly beneficial for the incretin therapies given their relatively high cost and frequency of short term side effects (10).
A major mechanism of action of GLP-1R agonists is potentiation of beta cell insulin secretion (4). We hypothesised that patients with more marked beta cell failure will be unable to substantially increase insulin secretion in response to GLP-1R agonists and therefore will have reduced glycemic response.
We aimed to determine whether clinical characteristics and simple biomarkers associated with beta cell failure are associated with glycemic response to GLP-1R agonists in patients with a clinical diagnosis of Type 2 diabetes.
Methods
Study hypothesis and outcomes were pre-specified and registered with clinicaltrials.gov (https://clinicaltrials.gov/show/NCT01503112).
Study setting and participants
We prospectively studied 620 participants with a clinical diagnosis of type 2 diabetes, HbA1c ≥58mmol/mol (7.5%) and estimated glomerular filtration rate (eGFR) >30mls/min/1.73m2 commencing GLP-1RA therapy as part of their usual diabetes care and assessed response to therapy over 6 months. Participants were identified from National Health Service (NHS) primary and secondary care and recruited at 17 participating sites in England between April 2011 and October 2013. Ethical approval was granted by the South West National Research Ethics committee, all participants gave written informed consent.
Assessment
At baseline, prior to commencing treatment, we assessed HbA1c and clinical markers of beta cell failure (fasting C-peptide (11), post largest home meal urine C-peptide creatinine ratio (UCPCR) (12), GAD and IA2 autoantibodies (13), diabetes duration and insulin co-treatment (14)). At 3 month (10-14 weeks) and 6 months (22-26 weeks) after commencing GLP-1RA therapy we assessed HbA1c and adherence (self-reported over the 2 weeks prior to HbA1c measurement). Concurrent treatment was recorded at all visits.
The primary outcome measure was change in HbA1c in the first 6 months of GLP-1RA therapy. Change in weight (baseline to six months) was assessed as a secondary outcome.
To minimise confounding by adherence or treatment change we excluded a follow up visit from analysis where participants had stopped therapy ≥7 days prior to HbA1c assessment, had <75% self-reported adherence, commenced any additional glucose lowering therapies or stopped >1 concurrent oral hypoglycemic agent (OHA). Treatment response was based on the most recent eligible HbA1c, with 3 month result used if the 6 month result did not meet the above criteria. Analysis of weight change was restricted to those who met the above criteria at 6 months (n=443, weight at 3 months was not assessed).
Statistical Analysis
Continuous analysis
We assessed the relationship between baseline clinical markers of beta cell function and treatment response (HbA1c change post GLP-1RA therapy) using least squares linear regression with adjustment for baseline HbA1c and co-treatment change (discontinuation of OHA, % change in insulin dose). Results were not adjusted for OHA dose change due to lack of association with response (p=0.3).
To determine whether biomarkers added to knowledge of insulin treatment status this analysis was repeated in subgroups defined by presence or absence of insulin co-treatment, with the inclusion of Homeostasis Model Assessment estimates of beta cell function (HOMA2%B) in non-insulin treated participants. To determine independence of autoantibody status and fasting C-peptide this model was repeated with both C-peptide and autoantibody status as covariates. We assessed the relationship between clinical markers of beta cell function and weight loss post GLP-1RA therapy using the same model with weight change (6 months – baseline) as the outcome variable.
Categorical analysis
We assessed differences in adjusted mean change in HbA1c, weight and insulin dose across subgroups defined by autoantibody and C-peptide status using univariate analysis of variance (ANOVA) with baseline HbA1c and treatment change as covariates. Fasting C-peptide subgroups were defined using previously reported thresholds for insulin requirement/type 1 diabetes (≤0.25nmol/L) and absence of ‘clinically significant’ endogenous insulin secretion (≤0.08nmol/L) (15).
Additional analysis
Differences in HbA1c change at 3 and 6 months follow up were assessed with the related samples T test, with analysis restricted to those on treatment at both visits with >75% adherence and no change in glucose lowering co-treatments. Differences in HbA1c reduction by GLP-1RA agent were assessed using univariate analysis of variance (ANOVA) with baseline HbA1c and treatment change as covariates.
Statistical analysis was performed using Stata Statistical Software: Release 13 (StataCorp, College Station, Texas, USA).
Laboratory analysis
HbA1c and fasting glucose were measured in recruitment centres’ local laboratories (all CPA accredited NHS blood science laboratories). HbA1c measurement was standardised to the IFCC reference method procedure, all repeated measurements within the same individual were analysed within the same laboratory. C-peptide (blood and urine), urine creatinine (for UCPCR) and GAD/IA2 autoantibodies were measured in the Blood Sciences Department at the Royal Devon and Exeter Hospital, Exeter, UK. C-peptide was measured using the E170 immuno-analyser from Roche Diagnostics (Manheim, Germany). GAD and IA2 were measured using commercial ELISA assays (RSR Ltd., Cardiff, UK) and a Dynex DSX automated ELISA system (Launch Diagnostics, Longfield, UK) and were considered positive if ≥ 97.5th centile of 500 adult control subjects (GAD >11 WHO units/ml, IA2>15 WHO units/ml), as previously reported (16).
Homeostasis model assessment estimates of beta cell function (HOMA2%B) and insulin sensitivity (HOMA2%S) were calculated in non-insulin treated participants from fasting glucose and C-peptide using the HOMA2 calculator available from http://www.dtu.ox.ac.uk/homacalculator/ and are reported in electronic supplementary materials.
Results
Participant characteristics and response to therapy
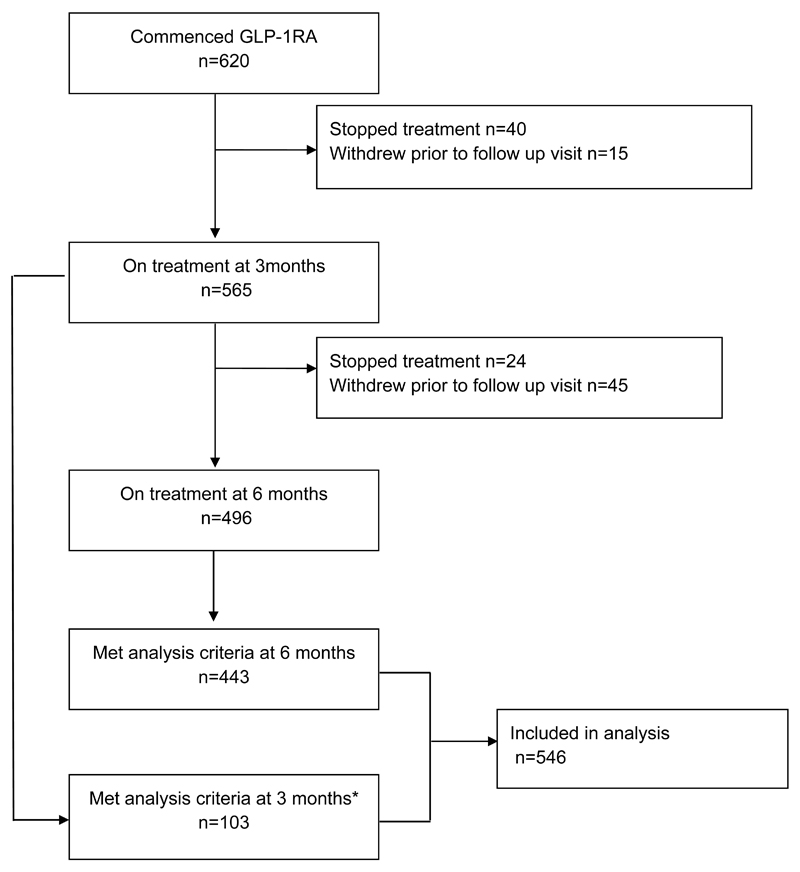
Participant characteristics are shown in Table 1, participant flow is detailed in Figure 1. Mean (SD) reduction in HbA1c and weight was 14.9 (17.2) mmol/mol (1.4 (1.6)%) and 4.5 (5.6) kg. 546 participants met criteria for inclusion in analysis (analysis on treatment HbA1c at 6 months n=443, 3 months n=103). HbA1c change at 3 and 6 months post treatment was not different (mean change -15.7 vs -15.1 mmol/mol respectively, p=0.2). 64% of participants were treated with Liraglutide, 27% Exenatide BD, 9% Exenatide OW.
Table 1. participant baseline characteristics.
N=546 except where otherwise specified, mean (SD) or %.
| Characteristic | Mean (SD) or % |
|---|---|
| HbA1c (mmol/mol) | 83 (17) |
| HbA1c % | 9.7 (1.6) |
| Fasting glucose (mmol/L) | 11.9 (3.7) |
| % male | 54% |
| % insulin treated | 38% |
| Age (years) | 56 (10.4) |
| Duration of diabetes (years) | 10.0 (6.6) |
| BMI (kg/m2) | 39.7 (7.5) |
| Fasting C-peptide (nmol/l) n=532 | 1.2 (0.6) |
| UCPCR (nmol/mmol) N=496 | 3.6 (3.1) |
| Islet autoantobody positive (GAD/IA2) N=520 | 3.7% (GAD only 3.1%, GAD and IA2 0.6%, IA2 only 0%) |
Figure 1.
Study Profile
Markers of low insulin secretion are associated with reduced glycaemic response to GLP-1R agonists
Markers of reduced insulin secretion were consistently associated with reduced glycaemic response to GLP-1RA therapy (Table 2). Less response was seen in those with lower C-peptide, lower UCPCR, positive GAD or IA2 islet autoantibodies, longer duration of diabetes and insulin co-treatment (p≤0.01 for all). A 1nmol/L decrease in fasting C-peptide was associated with a 3.2mmol/mol (0.3%) less HbA1c reduction post GLP-1RA therapy (Electronic Supplementary Materials Figure 1), the presence of insulin co-treatment or islet autoantibodies was associated with an 8.5 and 10.0mmol/mol (0.8 and 0.9%) reduction in glycaemic response respectively.
Table 2. The relationship between baseline markers of beta cell function and HbA1c change after GLP-1RA therapy.
Numbers in brackets represent 95% confidence interval. *A negative regression coefficient denotes a greater HbA1c reduction with a higher baseline value or presence of dichotomous state, **number of standard deviations difference in HbA1c change post GLP-1RA for a 1 standard deviation increase in baseline value ***regression coefficient/standard error
| Baseline Characteristic | Association with HbA1c change | |||
|---|---|---|---|---|
| Regression Coefficient (mmol/mol)* | Standardised regression coefficient ** | T statistic*** | Significance (p) | |
| Diabetes duration (years) | 0.27 (0.08, 0.46) | 0.10 (0.03, 0.18) | 2.7 | 0.006 |
| Insulin co-treatment | 8.5 (5.3, 11.7) | - | 5.2 | <0.001 |
| Fasting C-peptide (nmol/L) | -3.2 (-5.2, -1.2) | -0.12 (-0.19, -0.04) | -3.1 | 0.002 |
| UCPCR (nmol/mmol) | -0.56 (-1.0, -0.12) | -0.10 (-0.18, -0.02) | -2.5 | 0.01 |
| Autoantobody (GAD/IA2) positive | 10.0 (3.1 – 16.8) | - | 2.8 | 0.005 |
Baseline measurements associated with glycaemic response were not associated with change in weight (p>0.2 for all).
Participants with severe insulin deficiency had markedly reduced glycaemic response to GLP-1RA therapy
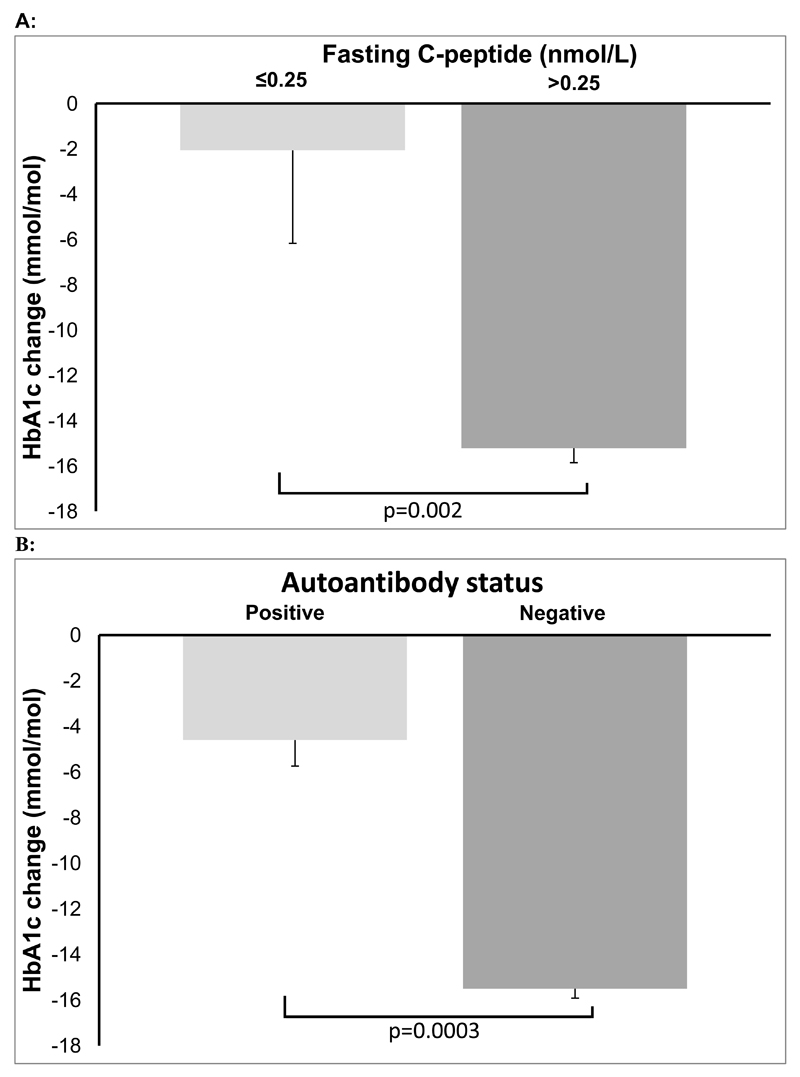
Participants with C-peptide under 0.25nmol/L (a previously reported threshold for insulin requirement and type 1 diabetes (15)) had markedly reduced glycaemic response (Figure 2A: mean (95% CI) adjusted HbA1c change −2.1 (−10.2, 6.0) vs −15.3 (−16.5, −14.0) mmol/mol (−0.2 vs −1.4%), p=0.002). Prevalence of C-peptide ≤0.25nmol/L was low, with this characteristic predominantly found in insulin treated participants (6.1% and 0.3% of insulin and non insulin treated participants respectively).
Figure 2.
HbA1c change post GLP-1RA therapy in those with and without A: severe insulin deficiency (C-peptide ≤0.25nmol/L, n=13/516) and B: positive GAD and/or IA2 antibodies (n=19/501). Bar represents mean change, error bars represent standard error.
A lower C-peptide threshold of ≤0.08nmol/L (absence of ‘clinically significant’ endogenous insulin (15)) identified fewer participants (3.4% of those insulin treated) with more marked lack of response to therapy (adjusted mean (95% CI) change +3.7 (−6.6, 14.0) vs −15.2 (−16.4, −14.0) mmol/mol (+0.3 vs −1.4%), p=0.0004).
The presence of raised GAD and/or IA2 islet autoantibodies is independently associated with reduced response to GLP-1RA therapy
Glycaemic response to GLP-1RA was also markedly lower in those who were GAD or IA2 antibody positive (adjusted mean (95% CI) HbA1c change -4.6 (−10.3, 1.1) vs −15.5 (−16.8, −14.2) mmol/mol (−0.4 vs −1.4%) , p=0.0003, Figure 2B). The relationship between autoantibody status and response was not fully explained by differences in fasting insulin secretion: after adjusting for fasting C-peptide autoantibodies were associated with an 8.1 mmol/mol (0.7%) reduction in glycaemic response to GLP-1A (p=0.02). 8.0% of insulin treated participants and 0.9% of non insulin treated participants were GAD or IA2 positive.
When analysis was restricted to autoantibody negative participants diabetes duration, insulin co-treatment and fasting C-peptide remained associated with glycaemic response (Electronic Supplementary Materials Table 1).
Biomarkers of beta cell failure remained associated with glycaemic response in patients receiving insulin treatment
Insulin treatment was strongly associated with other markers of beta cell failure, with longer diabetes duration, lower C-peptide based measures and higher proportion of positive autoantibodies seen in insulin treated patients (p<0.001 for all) (Electronic Supplementary Materials Table 2). In those treated with insulin, C-peptide based measures and autoantibodies remained predictive of glycaemic response (Electronic Supplementary Materials Table 3): a 1nmol/L decrease in fasting C-peptide was associated with a 4.3mmol/mol (0.4%) reduction in glycaemic response (p=0.01), positive autoantibodies an 8.1mmol/mol (0.7%) reduction in response (p=0.03). However these characteristics were not associated with response in non insulin treated participants (p for all >0.18, Electronic Supplementary Materials Table 4).
Insulin treated patients with low C-peptide or positive autoantibodies have reduced response to GLP-1RA therapy
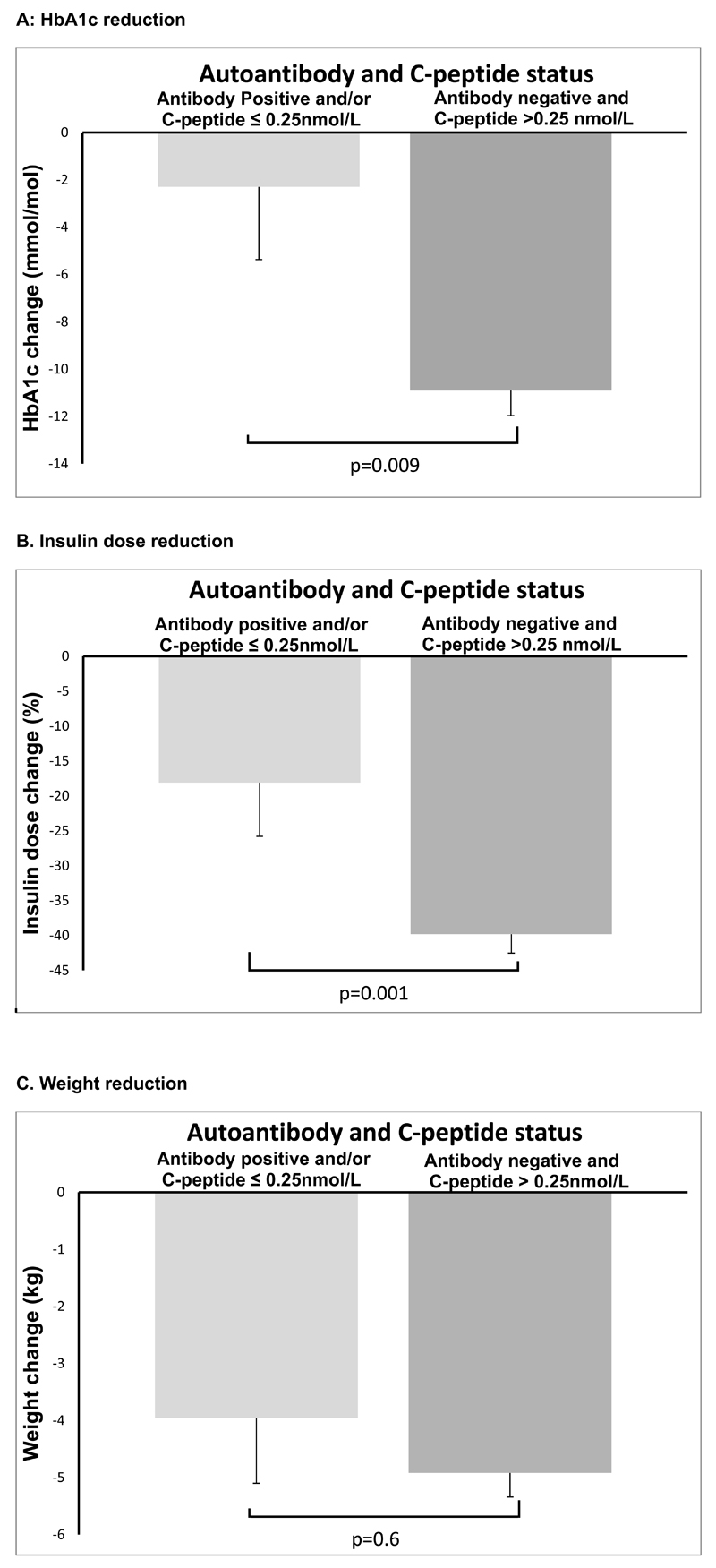
11% of insulin treated participants had either positive autoantibodies or low C-peptide (≤0.25nmol/L). These participants had mean change in HbA1c after GLP-1RA therapy of −2.3 (95% CI −8.4, 3.7) mmol/mol (−0.2%) compared to −10.9 (−12.9, -8.8) mmol/mol (−1.0%) in other insulin treated participants Figure 3. Antibody positive/low C-peptide participants also had less reduction in insulin dose (17% vs 40%, p=0.006), weight loss was similar (weight change at 6 months −4.2 vs −5.0kg, p=0.05), Figure 3. The clinical characteristics of insulin treated participants with and without low C-peptide and/or positive autoantibodies were similar: mean BMI 36.6 vs 39.7kg/m2 (p=0.07), age at diagnosis 42.2 vs 44.3 years (p=0.4), diabetes duration 14.5 vs 12.8 years (p=0.3), time to insulin 5.8 vs 5.9 years (p=0.9).
Figure 3.
Treatment response to GLP-1RA therapy in insulin treated participants by autoantibody and C-peptide status. Analysis adjusted for baseline HbA1c and co-treatment change. Bar represents mean change, error bars represent standard error. Antibody positive and/or low C-peptide n= 22, remaining participants n=176.
Discussion
This study demonstrates that markers of beta cell failure are associated with reduced glycaemic response to GLP-1R analogues. Insulin treated patients and those who have positive islet autoantibodies and/or low C-peptide have markedly reduced glycaemic response to this treatment. Participants with these markers of beta cell failure had reduced glycaemic response without additional weight loss, suggesting they will derive less overall benefit from GLP-1RA treatment.
Our finding that markers of beta cell failure are associated with reduced response to GLP-1RA therapy is consistent with previous studies. Research in smaller cohorts has suggested that those with lower blood C-peptide have less insulin secretion in response to GLP-1RA (17) and are less able to replace insulin with a GLP-1RA (18; 19), and that low home post meal urine C-peptide creatinine ratio is associated with reduced glycaemic response to liraglutide (20). Previous research demonstrating reduced response to GLP-1RA in those receiving insulin co-treatment or with longer diabetes duration is also consistent with our findings (3; 21). In contrast one study has demonstrated increased HbA1c reduction in insulin treated patients with longer duration of diabetes, a finding principally driven by increased response to placebo in the short duration comparator group (22).
To our knowledge this is the first study to assess the relationship between islet autoantibodies and response to GLP-1RA therapy. The independence of autoantibody and C-peptide testing in our study may suggest the mechanism, as well as the severity, of underlying beta cell failure is important to treatment response. Further studies with more robust assessment of stimulated insulin secretion would be needed to test this hypothesis.
The lack of glycaemic response seen in this cohort where beta cell failure is marked is consistent with potentiation of beta cell insulin secretion being the major mechanism of glucose lowering by GLP-1 receptor agonists. These agents have additional non beta cell dependant glucose lowering effects on gastric emptying and suppression of glucagon, however the relative contributions of these actions to glucose lowering remains unclear (23; 24). While acute administration of GLP-1 markedly reduces meal induced glucagon secretion, gastric emptying and postprandial glucose even in C-peptide negative type 1 diabetes (25), chronic treatment with GLP-1R agonists appears to have only a small effect on plasma glucagon (26–30) and may have little effect on gastric emptying (31; 32). This finding is consistent with poor glycaemic effect of on-going administration of GLP-1R agonists in Type 1 diabetes randomised controlled trials, where there appears to be a small reduction in insulin dose without improvement in glycaemia (33; 34).
Strengths and weaknesses
A strength of this study is that we have prospectively examined a large number of participants in a real world setting with detailed assessment at both baseline and follow up. Our finding that many different markers of reduced beta cell function are consistently associated with reduced GLP-1RA response suggests this is a robust finding.
Limitations of this study include that our major assessment of beta cell function is fasting blood or post home meal urine C-peptide. These are affected by concurrent glucose, insulin sensitivity and C-peptide clearance and therefore represent relatively crude indicators of underlying beta cell function (15). Physiological assessment of beta cell function would ideally involve measures after a standardised stimulus alongside correction for insulin sensitivity (35), however these measures would not be feasible for clinical practice. Beta cell function and insulin sensitivity are inversely related (36; 37). A role for beta cell failure (rather than insulin sensitivity) in reduced GLP-1RA glycaemic response is supported by the direction of association (better insulin sensitivity being an unlikely cause of reduced treatment response) and finding associations for factors predominantly associated with beta cell failure (autoantibodies (13), absolute insulin deficiency, insulin co-treatment and diabetes duration (14)). In addition characteristics associated with insulin resistance (BMI, triglycerides, HDL, sex hormone binding globulin (SHBG) and HOMA2%S (38; 39)) were not associated with glycaemic response in this cohort (p>0.6 for all, Electronic Supplementary Materials Table 5).
An additional potential limitation of fasting C-peptide measurement in a cohort including insulin treated patients is the potential suppression of fasting C-peptide if concurrent insulin results in low fasting glucose (40). However study participants had high fasting glucose at the time of C-peptide assessment, and difference between those treated with and without insulin was small (mean fasting glucose 11.2 and 12.4 mmol/L respectively).
Clinical Implications
The main clinical implications of this study are for use of GLP-1RA therapy in insulin treated patients. Our study confirms that overall less glycaemic response should be expected in those who are insulin treated. Where insulin treated patients are known to be antibody positive or have low C-peptide our results suggest these patients are unlikely to receive glycaemic benefit from GLP-1RA therapy. This would be consistent with existing guidelines which do not recommend GLP-1RA therapy for type 1 diabetes. When the antibody and C-peptide status is not known the cost of testing needs to be balanced against an empirical trial of therapy, further larger studies to confirm the effect size and prevalence of these features would be needed to determine whether a testing for this reason would be cost effective.
Our results show that a significant proportion of insulin treated patients receiving these treatments in the UK have islet autoantibodies and/or low C-peptide, despite having a clinical diagnosis of type 2 diabetes. These patients could not be identified by their clinical features. This may relate to the obese (and relatively young) nature of our cohort, as UK guidelines restrict these treatments to the obese (1). Differentiating type 1 and type 2 diabetes is particularly difficult in younger obese individuals. Both the clinical presentation and course of autoimmune diabetes can be very different from classical type 1 diabetes in the obese (41).
Our study does not support the measurement of antibodies and C-peptide in non insulin treated patients, as prevalence of low C-peptide and positive autoantibodies was very low in this group and an association with response was not seen.
Unanswered questions and future research
Our findings of reduced response in those with positive autoantibodies and severe insulin deficiency need replication as they are driven by a marked difference in response in a relatively small number of participants. This would ideally be in the setting of a randomised trial targeting insulin treated patients who are more likely to have these characteristics. Further research is also needed to assess whether insulin treated patients with high antibody titres and/or absolute insulin deficiency have reduced response to all non insulin glucose lowering co-therapies. This is an important question given the increasing difficulties distinguishing type 1 and 2 diabetes as obesity becomes more prevalent and the lack of glycaemic effect of non-insulin treatments in type 1 diabetes randomised controlled trials to date (33; 34; 42–44), which may relate to loss of endogenous insulin secretion even where a treatment’s mechanism of action appears unrelated (45).
Supplementary Material
Summary.
In summary markers of reduced insulin secretion are associated with less glycaemic response to GLP-1R agonist therapy. C-peptide and autoantibodies represent potential biomarkers for the stratification of glucose lowering treatment in insulin treated diabetes.
Acknowledgements
We thank staff of the NIHR Exeter Clinical Research Facility and NIHR Diabetes Research Network for assistance with conducting the study. We thank Mandy Perry and technicians of the Blood Sciences Department, Royal Devon and Exeter Hospital for assistance with laboratory analysis. We thank the members of the PRIBA study group (Electronic Supplementary Materials) and all study participants.
Funding sources
The Predicting Response to Incretin Based Agents (PRIBA) study was funded by the National Institute of Health Research (NIHR) (UK) and supported by the NIHR Clinical Research Network. AGJ was funded by an NIHR Doctoral Research Fellowship and is an NIHR Clinical Lecturer. ATH is an NIHR Senior Investigator and a Wellcome Trust Senior Investigator. ATH, AVH, BAK and BMS are core staff members of the NIHR Exeter Clinical Research Facility. TJM is an NIHR CSO Clinical Scientist Fellow. The views given in this paper do not necessarily represent those of NIHR, the NHS or the Department of Health.
List of Abbreviations
- ANOVA
analysis of variance
- 95% CI
95% Confidence Interval
- HDL
High Density Lipoprotein
- HOMA2%B
Homeostasis Assessment Model 2 % beta cell function
- HOMA2%S
Homeostasis Assessment Model 2 % insulin sensitivity
- GAD
Glutamic Acid Decarboxylase islet autoantibody
- GLP-1RA
GLP-1 Receptor Agonist
- IA2
Islet Antigen 2
- NHS
National Health Service (UK)
- SHBG
Sex Hormone Binding Globulin
- UCPCR
Urine C-peptide Creatinine Ratio
Footnotes
ClinicalTrials.gov Identifier: NCT01503112
Conflicts of interest
The authors declare they have no conflicts of interest.
Author Contributions
AGJ, AVH, BAK, TJM and ATH researched the data, AGJ and BMS analysed the data, AGJ wrote the manuscript, TJM, BMS, AVH, CJH, BAK and ATH provided helpful discussion and reviewed/edited the manuscript. AGJ is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Diabetes Care
This is an author-created, un-copy-edited electronic version of an article accepted for publication in Diabetes Care. The American Diabetes Care Association (ADA), publisher of Diabetes Care, is not responsible for any errors or omissions in this version of the manuscript or any version derived from it by third parties. The definitive publisher-authenticated version will be available in a future issue of Diabetes Care in print and online at http://care.diabetesjournals.org,
References
- 1.National Institute of Clinical Excellence (UK) Guideline CG87 - Type 2 diabetes: the management of type 2 diabetes. 2009 [Google Scholar]
- 2.Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR. Management of Hyperglycemia in Type 2 Diabetes, 2015: A Patient-Centered Approach: Update to a Position Statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38:140–149. doi: 10.2337/dc14-2441. [DOI] [PubMed] [Google Scholar]
- 3.Thong KY, Jose B, Sukumar N, Cull ML, Mills AP, Sathyapalan T, Shafiq W, Rigby AS, Walton C, Ryder RE. Safety, efficacy and tolerability of exenatide in combination with insulin in the Association of British Clinical Diabetologists (ABCD) nationwide exenatide audit. Diabetes, Obesity & Metabolism. 2011;13:703–10. doi: 10.1111/j.1463-1326.2011.01393.x. [DOI] [PubMed] [Google Scholar]
- 4.Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368:1696–1705. doi: 10.1016/S0140-6736(06)69705-5. [DOI] [PubMed] [Google Scholar]
- 5.Hirsch IB, Molitch ME. Clinical decisions. Glycemic management in a patient with type 2 diabetes. The New England Journal of Medicine. 2013;369:1370–1372. doi: 10.1056/NEJMclde1311497. [DOI] [PubMed] [Google Scholar]
- 6.Diamant M, Van Gaal L, Stranks S, Northrup J, Cao D, Taylor K, Trautmann M. Once weekly exenatide compared with insulin glargine titrated to target in patients with type 2 diabetes (DURATION-3): an open-label randomised trial. Lancet. 2010;375:2234–2243. doi: 10.1016/S0140-6736(10)60406-0. [DOI] [PubMed] [Google Scholar]
- 7.Bergenstal RM, Wysham C, Macconell L, Malloy J, Walsh B, Yan P, Wilhelm K, Malone J, Porter LE, Group D-S. Efficacy and safety of exenatide once weekly versus sitagliptin or pioglitazone as an adjunct to metformin for treatment of type 2 diabetes (DURATION-2): a randomised trial. Lancet. 2010;376:431–439. doi: 10.1016/S0140-6736(10)60590-9. [DOI] [PubMed] [Google Scholar]
- 8.Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.t Hart LM, Fritsche A, Nijpels G, van Leeuwen N, Donnelly LA, Dekker JM, Alssema M, Fadista J, Carlotti F, Gjesing AP, Palmer CN, et al. The CTRB1/2 locus affects diabetes susceptibility and treatment via the incretin pathway. Diabetes. 2013;62:3275–3281. doi: 10.2337/db13-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nauck MA. A critical analysis of the clinical use of incretin-based therapies: The benefits by far outweigh the potential risks. Diabetes care. 2013;36:2126–2132. doi: 10.2337/dc12-2504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Besser RE, Jones AG, McDonald TJ, Shields BM, Knight BA, Hattersley AT. The impact of insulin administration during the mixed meal tolerance test. Diabetic Medicine. 2012;29:1279–1284. doi: 10.1111/j.1464-5491.2012.03649.x. [DOI] [PubMed] [Google Scholar]
- 12.Jones AG, Besser RE, McDonald TJ, Shields BM, Hope SV, Bowman P, Oram RA, Knight BA, Hattersley AT. Urine C-peptide creatinine ratio is an alternative to stimulated serum C-peptide measurement in late-onset, insulin-treated diabetes. Diabetic Medicine. 2011;28:1034–1038. doi: 10.1111/j.1464-5491.2011.03272.x. [DOI] [PubMed] [Google Scholar]
- 13.Borg H, Gottsater A, Fernlund P, Sundkvist G. A 12-year prospective study of the relationship between islet antibodies and beta-cell function at and after the diagnosis in patients with adult-onset diabetes. Diabetes. 2002;51:1754–1762. doi: 10.2337/diabetes.51.6.1754. [DOI] [PubMed] [Google Scholar]
- 14.Fonseca VA. Defining and characterizing the progression of type 2 diabetes. Diabetes Care. 2009;32(Suppl 2):S151–156. doi: 10.2337/dc09-S301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones AG, Hattersley AT. The clinical utility of C-peptide measurement in the care of patients with diabetes. Diabetic Medicine. 2013;30:803–817. doi: 10.1111/dme.12159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McDonald TJ, Colclough K, Brown R, Shields B, Shepherd M, Bingley P, Williams A, Hattersley AT, Ellard S. Islet autoantibodies can discriminate maturity-onset diabetes of the young (MODY) from Type 1 diabetes. Diabetic Medicine. 2011;28:1028–1033. doi: 10.1111/j.1464-5491.2011.03287.x. [DOI] [PubMed] [Google Scholar]
- 17.Takabe M, Matsuda T, Hirota Y, Hashimoto N, Nakamura T, Sakaguchi K, Ogawa W, Seino S. C-peptide response to glucagon challenge is correlated with improvement of early insulin secretion by liraglutide treatment. Diabetes Research and Clinical Practice. 2012;98:e32–35. doi: 10.1016/j.diabres.2012.09.036. [DOI] [PubMed] [Google Scholar]
- 18.Davis SN, Johns D, Maggs D, Xu H, Northrup JH, Brodows RG. Exploring the substitution of exenatide for insulin in patients with type 2 diabetes treated with insulin in combination with oral antidiabetes agents. Diabetes Care. 2007;30:2767–2772. doi: 10.2337/dc06-2532. [DOI] [PubMed] [Google Scholar]
- 19.Iwao T, Sakai K, Sata M. Postprandial serum C-peptide is a useful parameter in the prediction of successful switching to liraglutide monotherapy from complex insulin therapy in Japanese patients with type 2 diabetes. J Diabetes Complications. 2013;27:87–91. doi: 10.1016/j.jdiacomp.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 20.Thong KY, McDonald TJ, Hattersley AT, Blann AD, Ramtoola S, Duncan C, Carr S, Adamson K, Nayak AU, Khurana R, Hunter SJ, et al. The association between postprandial urinary C-peptide creatinine ratio and the treatment response to liraglutide: a multi-centre observational study. Diabetic Medicine. 2013;31:403–411. doi: 10.1111/dme.12367. [DOI] [PubMed] [Google Scholar]
- 21.Penformis A GP, Martinez S, Madani S, Charpentier G, Eschwege E, Gautier J-F. Diabetes duration and background diabetes therapies in predicting liraglutide treatment response: data from post-marketing EVIDENCE study. Diabetologia. 2013;56(Supplement 1) [Google Scholar]
- 22.Rosenstock J, Shenouda SK, Bergenstal RM, Buse JB, Glass LC, Heilmann CR, Kwan AY, MacConell LA, Hoogwerf BJ. Baseline factors associated with glycemic control and weight loss when exenatide twice daily is added to optimized insulin glargine in patients with type 2 diabetes. Diabetes Care. 2012;35:955–958. doi: 10.2337/dc11-1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Christensen M, Bagger JI, Vilsboll T, Knop FK. The alpha-cell as target for type 2 diabetes therapy. The review of diabetic studies: RDS. 2011;8:369–381. doi: 10.1900/RDS.2011.8.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.D'Alessio DA. Taking aim at islet hormones with GLP-1: is insulin or glucagon the better target? Diabetes. 2010;59:1572–1574. doi: 10.2337/db10-0299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kielgast U, Holst JJ, Madsbad S. Antidiabetic actions of endogenous and exogenous GLP-1 in type 1 diabetic patients with and without residual beta-cell function. Diabetes. 2011;60:1599–1607. doi: 10.2337/db10-1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rother KI, Spain LM, Wesley RA, Digon BJ, 3rd, Baron A, Chen K, Nelson P, Dosch HM, Palmer JP, Brooks-Worrell B, Ring M, et al. Effects of exenatide alone and in combination with daclizumab on beta-cell function in long-standing type 1 diabetes. Diabetes Care. 2009;32:2251–2257. doi: 10.2337/dc09-0773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gastaldelli A, Balas B, Ratner R, Rosenstock J, Charbonnel B, Bolli GB, Boldrin M, Balena R. A direct comparison of long- and short-acting GLP-1 receptor agonists (taspoglutide once weekly and exenatide twice daily) on postprandial metabolism after 24 weeks of treatment. Diabetes, Obesity & Metabolism. 2014;16:170–178. doi: 10.1111/dom.12192. [DOI] [PubMed] [Google Scholar]
- 28.Berg JK, Shenouda SK, Heilmann CR, Gray AL, Holcombe JH. Effects of exenatide twice daily versus sitagliptin on 24-h glucose, glucoregulatory and hormonal measures: a randomized, double-blind, crossover study. Diabetes, Obesity & Metabolism. 2011;13:982–989. doi: 10.1111/j.1463-1326.2011.01428.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rosenstock J, Reusch J, Bush M, Yang F, Stewart M, Albiglutide Study G Potential of albiglutide, a long-acting GLP-1 receptor agonist, in type 2 diabetes: a randomized controlled trial exploring weekly, biweekly, and monthly dosing. Diabetes Care. 2009;32:1880–1886. doi: 10.2337/dc09-0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zinman B, Gerich J, Buse JB, Lewin A, Schwartz S, Raskin P, Hale PM, Zdravkovic M, Blonde L, Investigators L-S. Efficacy and safety of the human glucagon-like peptide-1 analog liraglutide in combination with metformin and thiazolidinedione in patients with type 2 diabetes (LEAD-4 Met+TZD) Diabetes Care. 2009;32:1224–1230. doi: 10.2337/dc08-2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nauck MA, Kemmeries G, Holst JJ, Meier JJ. Rapid tachyphylaxis of the glucagon-like peptide 1-induced deceleration of gastric emptying in humans. Diabetes. 2011;60:1561–1565. doi: 10.2337/db10-0474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kapitza C, Zdravkovic M, Hindsberger C, Flint A. The effect of the once-daily human glucagon-like peptide 1 analog liraglutide on the pharmacokinetics of acetaminophen. Advances in Therapy. 2011;28:650–660. doi: 10.1007/s12325-011-0044-y. [DOI] [PubMed] [Google Scholar]
- 33.Kielgast U, Krarup T, Holst JJ, Madsbad S. Four weeks of treatment with liraglutide reduces insulin dose without loss of glycemic control in type 1 diabetic patients with and without residual beta-cell function. Diabetes Care. 2011;34:1463–1468. doi: 10.2337/dc11-0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sarkar G, Alattar M, Brown RJ, Quon MJ, Harlan DM, Rother KI. Exenatide Treatment for 6 Months Improves Insulin Sensitivity in Adults with Type 1 Diabetes Mellitus. Diabetes care. 2014;37:666–670. doi: 10.2337/dc13-1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kahn SE, Carr DB, Faulenbach MV, Utzschneider KM. An examination of beta-cell function measures and their potential use for estimating beta-cell mass. Diabetes, Obesity & Metabolism. 2008;10(Suppl 4):63–76. doi: 10.1111/j.1463-1326.2008.00945.x. [DOI] [PubMed] [Google Scholar]
- 36.Kahn SE. The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of Type 2 diabetes. Diabetologia. 2003;46:3–19. doi: 10.1007/s00125-002-1009-0. [DOI] [PubMed] [Google Scholar]
- 37.Kahn SE, Prigeon RL, McCulloch DK, Boyko EJ, Bergman RN, Schwartz MW, Neifing JL, Ward WK, Beard JC, Palmer JP, et al. Quantification of the relationship between insulin sensitivity and beta-cell function in human subjects. Evidence for a hyperbolic function. Diabetes. 1993;42:1663–1672. doi: 10.2337/diab.42.11.1663. [DOI] [PubMed] [Google Scholar]
- 38.H Y-J. Insulin Resistance in Type 2 Diabetes. In: Holt RGCC, Flyvbjerg A, Goldstein BJ, editors. Textook of Diabetes. 4th. Wiley-Blackwell; 2010. [Google Scholar]
- 39.Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes care. 2004;27:1487–1495. doi: 10.2337/diacare.27.6.1487. [DOI] [PubMed] [Google Scholar]
- 40.Albareda M, Rigla M, Rodriguez-Espinosa J, Caballero A, Chico A, Cabezas R, Carreras G, Perez A. Influence of exogenous insulin on C-peptide levels in subjects with type 2 diabetes. Diabetes Research and Clinical Practice. 2005;68:202–206. doi: 10.1016/j.diabres.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 41.Gale EA. Latent autoimmune diabetes in adults: a guide for the perplexed. Diabetologia. 2005;48:2195–2199. doi: 10.1007/s00125-005-1954-5. [DOI] [PubMed] [Google Scholar]
- 42.Vella S, Buetow L, Royle P, Livingstone S, Colhoun HM, Petrie JR. The use of metformin in type 1 diabetes: a systematic review of efficacy. Diabetologia. 2010;53:809–820. doi: 10.1007/s00125-009-1636-9. [DOI] [PubMed] [Google Scholar]
- 43.Garg SK, Moser EG, Bode BW, Klaff LJ, Hiatt WR, Beatson C, Snell-Bergeon JK. Effect of sitagliptin on post-prandial glucagon and GLP-1 levels in patients with type 1 diabetes: investigator-initiated, double-blind, randomized, placebo-controlled trial. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2013;19:19–28. doi: 10.4158/EP12100.OR. [DOI] [PubMed] [Google Scholar]
- 44.Ellis SL, Moser EG, Snell-Bergeon JK, Rodionova AS, Hazenfield RM, Garg SK. Effect of sitagliptin on glucose control in adult patients with Type 1 diabetes: a pilot, double-blind, randomized, crossover trial. Diabetic Medicine. 2011;28:1176–1181. doi: 10.1111/j.1464-5491.2011.03331.x. [DOI] [PubMed] [Google Scholar]
- 45.Riddle MC. Combined therapy with insulin plus oral agents: is there any advantage? An argument in favor. Diabetes Care. 2008;31(Suppl 2):S125–130. doi: 10.2337/dc08-s231. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.