Abstract
Objectives. To assess longitudinal patterns of community health center (CHC) utilization and the effect of insurance discontinuity after Oregon’s 2008 Medicaid expansion (the Oregon Experiment).
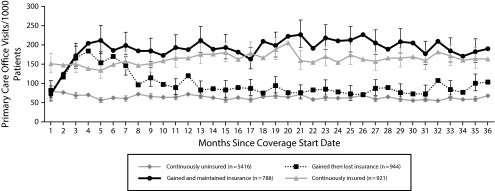
Methods. We conducted a retrospective cohort study with electronic health records and Medicaid data. We divided individuals who gained Medicaid in the Oregon Experiment into those who maintained (n = 788) or lost (n = 944) insurance coverage. We compared these groups with continuously insured (n = 921) and continuously uninsured (n = 5416) reference groups for community health center utilization rates over a 36-month period.
Results. Both newly insured groups increased utilization in the first 6 months. After 6 months, use among those who maintained coverage stabilized at a level consistent with the continuously insured, whereas it returned to baseline for those who lost coverage.
Conclusions. Individuals who maintained coverage through Oregon’s Medicaid expansion increased long-term utilization of CHCs, whereas those with unstable coverage did not.
Policy implications. This study predicts long-term increase in CHC utilization following Affordable Care Act Medicaid expansion and emphasizes the need for policies that support insurance retention.
The Affordable Care Act (ACA) provided Americans with new access to health insurance,1 and many policymakers predicted a subsequent increase in health care utilization.2–4 Early studies since the ACA’s implementation confirm this increase.5–7 However, important questions remain about where newly insured individuals will get care, how trends in utilization will evolve over time, and how discontinuity of insurance will have an impact on utilization.8,9 These important questions will guide allocation of resources and development of needed infrastructure and workforce to meet the primary care demands of a growing population of insured patients. Ensuring access to primary care for the newly insured is critical to optimizing public health and has proven challenging with previous Medicaid expansions.3,10 Because long-term data from the ACA are not yet available, previous insurance expansions must inform predictions of the ACA’s impact on long-term utilization of primary care.
Past studies of policy-driven expansions demonstrate how care-seeking behaviors change when a previously uninsured population receives coverage.11–14 In Massachusetts, a 2006 insurance expansion resulted in increased utilization among the newly insured,3,15,16 and community health centers (CHCs) saw utilization increase by 31%.17 After the 2008 Oregon Experiment Medicaid expansion, ambulatory care utilization increased18–20 and use of CHC services increased by 22% in the first year.21 Individuals who gained Medicaid coverage through the Oregon Experiment subsequently had 39% more CHC visits than those who did not gain coverage.22
We describe trends in CHC utilization for 36 months after Oregon’s 2008 Medicaid expansion to (1) investigate longitudinal utilization patterns, (2) observe the extent to which those gaining coverage experienced subsequent loss in coverage, and (3) better understand the extent to which a coverage loss affected utilization in subsequent years. Although we did not seek to estimate the causal effect of insurance coverage on primary care utilization as have others,22 this longitudinal investigation of insurance cohorts adds to previous studies reporting that even short coverage gaps can have significant effects on access to care and utilization.23–27
The use of new electronic health record (EHR) data sources enabled us to overcome some of the biases reported in past studies that used self-report (i.e., nonresponse bias, recall bias). Furthermore, unlike insurance claims data commonly used for tracking utilization rates, EHR data capture utilization among patients gaining and then losing insurance coverage and also allow for inclusion of an uninsured comparison group.
METHODS
In 2008, Oregon expanded Medicaid in a randomized natural experiment known as the Oregon Experiment. Approximately 90 000 low-income, uninsured adults added their names to a reservation list; approximately 30 000 names were randomly selected from this list to apply for coverage, and roughly 10 000 of these selected adults ultimately enrolled in Medicaid.28 The remaining individuals may have applied and been deemed ineligible, or may have opted not to apply. This created a natural experiment in which some individuals were randomly selected to apply for Medicaid and a subset of those individuals gained Medicaid coverage. Detailed information about the Oregon Experiment is available elsewhere.19,20,28,29 Though self-selection certainly influenced who ultimately enrolled, the scale of this expansion made an ideal setting to inform current policy.
Data Sources
We used EHR data from the OCHIN community health information network. OCHIN is a nonprofit organization that serves more than 300 CHCs across multiple states. Formerly known as the Oregon Community Health Information Network, the collaborative was renamed OCHIN as members from other states joined. OCHIN members share a single, linked, fully integrated EHR.
We obtained patient-level demographic, clinical, and utilization information from OCHIN’s EHR data. Aided by Link Plus software (version 2.0, Registry Plus, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Atlanta, GA), we probabilistically matched individuals on the Oregon Experiment reservation list to patients in the OCHIN database of EHRs by using demographic variables common to both data sets. We used Oregon’s Medicaid enrollment data to determine Medicaid coverage status during the study period.
Study Population
In the probabilistic matching process to link individuals on the Oregon Experiment reservation list to patients seen at OCHIN member clinics, we included all patients meeting the following criteria: aged 19 to 64 years and alive throughout the 36-month follow-up period; not pregnant throughout the study period; no record of health insurance other than that offered by the Oregon Experiment (i.e., Oregon Health Plan [OHP] Standard) during the 36-month study period; 1 or more office visits to an OCHIN primary care clinic in Oregon from 36 months before to 36 months after the person’s insurance start date (defined in the Study Period section); and meeting the pre- and postexpansion insurance coverage criteria described in the next paragraph. We excluded pregnant women and persons outside the 19- to 64-year age range as these factors affect eligibility for public coverage.
Within our study population, we compared 2 case groups and 2 comparison groups. “Cases” gained Medicaid through the Oregon Experiment. All cases were uninsured for at least 6 months, then were randomly selected to apply for coverage in the Oregon Experiment, and ultimately gained OHP Standard. Cases were then subdivided into 2 groups: (1) those who gained and maintained OHP Standard for 75% or more of their 36-month follow-up period (gained and maintained; n = 788), and (2) those who gained and then lost coverage, remaining covered for less than 75% of their 36-month follow-up period (gained and lost; n = 944).
The primary comparison group included patients who participated in the Oregon Experiment, but were not selected and had no insurance from 6 months before their start date through their entire 36-month follow-up period (continuously uninsured; n = 5416). The second comparison group had 100% OHP Standard coverage in the 6 months before the patient’s start date and 75% or more coverage for their 36-month follow-up period (continuously insured; n = 921). These individuals did not participate in the Oregon Experiment, but were included to represent contemporary utilization patterns among insured patients seen within the same clinic network.
Study Period
We assessed utilization beginning with insurance start date and ending 36 months after the start date for each member of the study population. In our study groups, all coverage start dates corresponded with the Oregon Experiment’s drawings held in March to October 2008. For the cases, start dates were assigned as the date of selection notification. Persons not selected to apply for coverage were randomly assigned a 2008 start date based on the distribution of start dates among those selected to apply (e.g., if 10% of those cases who gained insurance had an actual Medicaid start date of March 11, 2008, that start date was randomly assigned to 10% of persons in each comparison group).
For the 36-month study period, we measured monthly utilization rates of primary care services for each group. We defined primary care utilization as a completed office visit with a physician (MD or DO, including residents), nurse practitioner, or physician assistant at a public health or primary care clinic within the OCHIN network.
Covariates
We adjusted utilization rates for patient gender, age, race/ethnicity, chronic conditions, home CHC (to account for regional utilization differences), and household income as a percentage of the federal poverty level (FPL) averaged across the 36-month follow-up period. If patients did not have FPL data entered into the EHR during the 36-month follow-up period, we computed it from other records in the chart, if available.
We defined chronic conditions as previous diagnosis of 5 chronic conditions for which standard code sets are available as part of meaningful use criteria30 or the Healthcare Effectiveness Data and Information Set31: asthma, coronary artery disease, diabetes, dyslipidemia, and hypertension. We considered a patient to have a given condition if a qualifying diagnosis code appeared on the problem list or in 2 or more encounters before the patient’s start date.
Statistical Methods
We first assessed differences between the continuously uninsured group and the other insurance groups by using the χ2 test for categorical variables and the Kolmogorov–Smirnov test for continuous predictors. To model the longitudinal trajectory of each of the 4 insurance groups and compare the groups over time, we used an overall generalized estimating equation Poisson regression model with insurance group as the primary predictor to estimate adjusted monthly utilization rates and 95% confidence intervals for each insurance group over the 36-month follow-up period. This generalized estimating equation model included a term for the interaction between insurance group and time and implemented an empirical sandwich estimator and a first-order autoregressive correlation structure to account for correlation of observations within a participant over time.
This study was reviewed and approved by the Oregon Health and Science University institutional review board and was registered as an observational study (NCT02355132).32
RESULTS
There were significant differences in many demographic characteristics among each of the 4 study groups (Table 1). Compared with the continuously uninsured, those who gained insurance (both case groups) were more likely to be non-Hispanic White and to have income below the FPL (P < .05; Table 1). Those who gained and maintained insurance were more likely to be older, whereas those who gained and lost insurance were more likely to be male and to have fewer chronic health conditions (P < .05). Of the 2 comparison groups, the continuously insured group was the more likely to be female and to have more chronic health conditions (P < .05).
TABLE 1—
Demographic Characteristics of Study Groups as of Coverage Start Date (Total n = 8069): Oregon, 2008
| Gained Then Lost Insurance
(n = 944) |
Gained and Maintained Insurance
(n = 788) |
Continuously Insured
(n = 921) |
|||||
| Characteristic | Continuously Uninsured (n = 5416), No. (%) | No. (%) | P | No. (%) | P | No. (%) | P |
| Gender | .042a | .68 | < .001a | ||||
| Female | 2713 (50.1) | 439 (46.5) | 401 (50.9) | 546 (59.3) | |||
| Male | 2703 (49.9) | 505 (53.5) | 387 (49.1) | 375 (40.7) | |||
| Age at baseline, y | .29 | < .001a | < .001a | ||||
| 19–29 | 1415 (26.1) | 247 (26.2) | 113 (14.3) | 98 (10.6) | |||
| 30–39 | 1249 (23.1) | 224 (23.7) | 138 (17.5) | 174 (18.9) | |||
| 40–49 | 1500 (27.7) | 280 (29.7) | 274 (34.8) | 326 (35.4) | |||
| 50–59 | 1092 (20.2) | 174 (18.4) | 241 (30.6) | 281 (30.5) | |||
| 60–64 | 160 (3.0) | 19 (2.0) | 22 (2.8) | 42 (4.6) | |||
| Median (IQR) | 40 (20.0) | 40 (19.0) | .61 | 46 (14.5) | < .001b | 46 (14.0) | < .001b |
| Race/ethnicity | < .001a | < .001a | < .001a | ||||
| Hispanic | 865 (16.0) | 55 (5.8) | 43 (5.5) | 38 (4.1) | |||
| Non-Hispanic White | 3578 (66.1) | 705 (74.7) | 621 (78.8) | 692 (75.1) | |||
| Non-Hispanic other | 711 (13.1) | 109 (11.5) | 93 (11.8) | 155 (16.8) | |||
| Unknown | 262 (4.8) | 75 (7.9) | 31 (3.9) | 36 (3.9) | |||
| Household income | < .001a | < .001a | < .001a | ||||
| < 100% of FPL | 4051 (74.8) | 750 (79.4) | 694 (88.1) | 783 (85.0) | |||
| ≥ 100% of FPL | 1232 (22.7) | 159 (16.8) | 62 (7.9) | 91 (9.9) | |||
| Unknown | 133 (2.5) | 35 (3.7) | 32 (4.1) | 47 (5.1) | |||
| Median (IQR) % FPL | 55.2 (97.0) | 41 (82.5) | < .001b | 19.3 (62.0) | < .001b | 27.5 (69.0) | < .001b |
| Chronic conditionsc at baseline, no. | < .001a | .13 | < .001a | ||||
| 0 | 4334 (80.0) | 805 (85.3) | 653 (82.9) | 606 (65.8) | |||
| 1–2 | 939 (17.3) | 117 (12.4) | 114 (14.5) | 263 (28.6) | |||
| 3–5 | 143 (2.6) | 22 (2.3) | 21 (2.7) | 52 (5.6) | |||
Note. FPL = federal poverty level (as defined by US Department of Health and Human Services33); IQR = interquartile range.
Proportions significantly different from continuously uninsured based on χ2 test.
Distribution significantly different from continuously uninsured based on Kolmogorov–Smirnov test.
Chronic conditions included asthma, coronary artery disease, diabetes, dyslipidemia, and hypertension.
At baseline, patients who gained Medicaid coverage exhibited rates of primary care utilization similar to the continuously uninsured and significantly lower than the continuously insured (Figure 1). Over the following 3 months, utilization among patients who gained coverage increased sharply; 4 months into the study period, the 2 case groups matched or exceeded rates among continuously insured patients. After 6 months, rates of utilization for the 2 case groups diverged, and by month 8, the “gained and lost” case group used care at a rate similar to the continuously uninsured, whereas the “gained and maintained” group continued to use care at a similar rate to the continuously insured group.
FIGURE 1—
Comparison of Monthly Primary Care Utilization Rates in the 3 Years After the Oregon Experiment, by Insurance Group, 2008–2011
Note. Rates averaged over each 1-month interval and adjusted for patient gender, age, race/ethnicity, chronic conditions, health center, and household income. Vertical bars denote 95% confidence intervals of monthly utilization rate.
DISCUSSION
Those who gained insurance through Oregon’s Medicaid expansion and maintained coverage during the 36-month study period showed similar long-term utilization patterns to the continuously insured. Those who gained insurance through the expansion and subsequently lost coverage or churned on and off coverage increased utilization initially, but after the first year showed utilization similar to that of the continuously uninsured. Though long-term retention of patients in any health system depends on delivery of safe, timely, and satisfactory care, these findings suggest that the ACA will lead to a sustained increase in demand for primary care services at CHCs and highlight the powerful effect of insurance discontinuity on health care use. Our findings refute the suggestion that CHC utilization may decrease if patients seek care elsewhere after gaining Medicaid.34–36 On the contrary, the evidence supports the recent federal decision to expand funding to CHCs.37
This study confirms previous reports of increased utilization after the Oregon Experiment18–22 and also contributes to the literature in meaningful new ways. First, the use of EHR data strengthens the assessment of health care utilization by avoiding the potential biases of self-reported data, and enabling longitudinal collection of information not dependent on insurance continuity, as with insurance claims data. Second, we estimate longitudinal patterns of utilization, which are immediately relevant to informing predictions about long-term use after ACA insurance expansions. Finally, by following 2 distinct groups that gained coverage—those who maintained and those who lost—we identify significant differences in longitudinal use depending on Medicaid retention. The divergence in utilization between these 2 groups at 6 months likely represents the portion of individuals who lost coverage after their initial 6-month coverage period expired. This highlights the challenges associated with reapplication for coverage and supports policies that allow longer coverage periods.38
Our findings have important public health implications. Many studies show that utilization of primary care is associated with improved receipt of preventive services,39–43 effective management of chronic conditions,44,45 reduced use of expensive emergency and hospital services,46,47 and improved health outcomes.48 In Massachusetts and Oregon, primary care access barriers were implicated in increased use of emergency departments after insurance expansion.19 Thus, policies and structures to promote insurance enrollment and retention, and access to primary care, will be vital to supporting the health of Americans. As we face projected primary care workforce deficits, accurate estimates of demand will help guide upstream decisions regarding training and development.49
Limitations
Although our population is similar to that targeted by the ACA, there are important differences between the Oregon Experiment and the ACA. Participation in the Oregon Experiment was voluntary whereas the ACA made insurance mandatory; furthermore, our findings may not be generalizable beyond Oregon. Though the ACA is now implemented, there are not yet sufficient data to study the long-term changes in utilization, so it is important to look to analogous policies and populations such as those in the Oregon Experiment. There is also potential that the 4 cohorts significantly differ in other important unobserved confounders for which we were not able to adjust, and thus could bias the study findings. Finally, among those who gained and lost insurance, we did not measure when and for what duration insurance was lost, nor the reason insurance was lost. These factors may lead to heterogeneity of this group.
Use of EHR data is a significant strength of this study; however, it resulted in scope limited to patients at CHCs within the OCHIN network. If patients received care outside the OCHIN network, this use was not captured. Because we included only patients within the OCHIN network, our results are not generalizable to all individuals who gained health insurance through the Oregon Experiment. Though determining if and where newly enrolled individuals seek health care was beyond the scope of this study, this is an important question for future research to inform allocation of resources and optimization of health care delivery systems. Although some equate primary care utilization with improved health, this study did not assess whether the CHC services received after the Oregon Experiment resulted in better health outcomes, though the EHR may offer powerful tools with which to examine these questions in the future.
Conclusions
Our findings suggest that utilization of primary care services at CHCs will increase in the wake of ACA-supported Medicaid expansion. Discontinuity of insurance may pose a significant barrier to accessing essential primary care services, particularly after initial coverage periods expire. As clinics, educators, and policymakers begin making projections for future clinical and workforce demands, our study supports continued investment in primary care and CHCs to meet the health care needs of vulnerable patients in the United States.
ACKNOWLEDGMENTS
The project was supported in part by funding from the National Institutes of Health, National Heart, Lung, and Blood Institute, 1R01HL107647-01.
The authors appreciate project guidance and article review from John Heintzman, MD, MPH, Rachel Gold, PhD, Jean O’Malley, MPH, and Megan Hoopes, MPH.
HUMAN PARTICIPANT PROTECTION
The institutional review board at Oregon Health and Science University approved this project.
Footnotes
See also Galea and Vaughan, p. 592.
REFERENCES
- 1. The Medicaid program at a glance. Henry J. Kaiser Family Foundation. 2013. Available at: https://kaiserfamilyfoundation.files.wordpress.com/2013/03/7235-061.pdf. Accessed August 1, 2015.
- 2.Abraham JM, Karaca-Mandic P, Simon K. How has the Affordable Care Act’s medical loss ratio regulation affected insurer behavior? Med Care. 2014;52(4):370–377. doi: 10.1097/MLR.0000000000000091. [DOI] [PubMed] [Google Scholar]
- 3.Ku L, Jones K, Shin P, Bruen B, Hayes K. The states’ next challenge—securing primary care for expanded Medicaid populations. N Engl J Med. 2011;364(6):493–495. doi: 10.1056/NEJMp1011623. [DOI] [PubMed] [Google Scholar]
- 4.Schoen C, Hayes SL, Radely DC, Collins SR. Access to primary and preventive health care across states prior to the coverage expansions of the Affordable Care Act. Issue Brief (Commonw Fund) 2014;17:1–14. [PubMed] [Google Scholar]
- 5.Hempstead K. Princeton, NJ: Robert Wood Johnson Foundation; 2014. Early trends in health care utilization in the commercial market. [Google Scholar]
- 6.Wachino V, Artiga S, Rudowitz R. How is the ACA affecting Medicaid enrollment? Henry J. Kaiser Family Foundation; 2014. Available at: http://kff.org/medicaid/issue-brief/how-is-the-aca-impacting-medicaid-enrollment. Accessed August 1, 2015.
- 7.Angier H, Hoopes M, Gold R et al. An early look at rates of uninsured safety net clinic visits after the Affordable Care Act. Ann Fam Med. 2015;13(1):10–16. doi: 10.1370/afm.1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Richards MR, Saloner B, Kenney GM, Rhodes K, Polsky D. Access points for the underserved: primary care appointment availability at federally qualified health centers in 10 states. Med Care. 2014;52(9):818–825. doi: 10.1097/MLR.0000000000000184. [DOI] [PubMed] [Google Scholar]
- 9.Marbury D. Unanswered questions remain for providers as ACA enrollment ends. Med Econ. 2014;91(8):65. [PubMed] [Google Scholar]
- 10.Stuber J, Bradley E. Barriers to Medicaid enrollment: who is at risk? Am J Public Health. 2005;95(2):292–298. doi: 10.2105/AJPH.2002.006254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buchmueller TC, Grumbach K, Kronick R, Kahn JG. The effect of health insurance on medical care utilization and implications for insurance expansion: a review of the literature. Med Care Res Rev. 2005;62(1):3–30. doi: 10.1177/1077558704271718. [DOI] [PubMed] [Google Scholar]
- 12.Decker SL, Doshi JA, Knaup AE, Polsky D. Health service use among the previously uninsured: is subsidized health insurance enough? Health Econ. 2012;21(10):1155–1168. doi: 10.1002/hec.1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Polsky D. How the newly insured use health services: a lesson for the U.S. from Medicare. LDI Issue Brief. 2011;17(4):1–4. [PubMed] [Google Scholar]
- 14.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Use of health services by previously uninsured Medicare beneficiaries. N Engl J Med. 2007;357(2):143–153. doi: 10.1056/NEJMsa067712. [DOI] [PubMed] [Google Scholar]
- 15.Miller S. The effect of the Massachusetts reform on health care utilization. Inquiry. 2012–2013;49(4):317–326. doi: 10.5034/inquiryjrnl_49.04.05. [DOI] [PubMed] [Google Scholar]
- 16.Long SK, Masi PB. Access and affordability: an update on health reform in Massachusetts, fall 2008. Health Aff (Millwood) 2009;28(4):w578–w587. doi: 10.1377/hlthaff.28.4.w578. [DOI] [PubMed] [Google Scholar]
- 17.Ku L, Jones E, Shin P, Byrne FR, Long SK. Safety-net providers after health care reform: lessons from Massachusetts. Arch Intern Med. 2011;171(15):1379–1384. doi: 10.1001/archinternmed.2011.317. [DOI] [PubMed] [Google Scholar]
- 18.Baicker K, Finkelstein A. The effects of Medicaid coverage—learning from the Oregon experiment. N Engl J Med. 2011;365(8):683–685. doi: 10.1056/NEJMp1108222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baicker K, Taubman SL, Allen HL et al. The Oregon experiment—effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Finkelstein A, Taubman S, Wright B et al. The Oregon health insurance experiment: evidence from the first year. Q J Econ. 2012;127(3):1057–1106. doi: 10.1093/qje/qjs020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gold R, Bailey SR, O’Malley JP et al. Estimating demand for care after a Medicaid expansion: lessons from Oregon. J Ambul Care Manage. 2014;37(4):282–292. doi: 10.1097/JAC.0000000000000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeVoe JE, Marino M, Gold R et al. Community health center use after Oregon’s randomized Medicaid experiment. Ann Fam Med. 2015;13(4):312–320. doi: 10.1370/afm.1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DeVoe JE, Graham A, Krois L, Smith J, Fairbrother GL. “Mind the gap” in children’s health insurance coverage: does the length of a child’s coverage gap matter? Ambul Pediatr. 2008;8(2):129–134. doi: 10.1016/j.ambp.2007.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bindman AB, Chattopadhyay A, Auerback GM. Medicaid re-enrollment policies and children’s risk of hospitalizations for ambulatory care sensitive conditions. Med Care. 2008;46(10):1049–1054. doi: 10.1097/MLR.0b013e318185ce24. [DOI] [PubMed] [Google Scholar]
- 25.Carlson MJ, DeVoe J, Wright BJ. Short-term impacts of coverage loss in a Medicaid population: early results from a prospective cohort study of the Oregon health plan. Ann Fam Med. 2006;4(5):391–398. doi: 10.1370/afm.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eisert SL, Durfee MJ, Welsh A, Moore SL, Mehler PS, Gabow PA. Changes in insurance status and access to care in an integrated safety net healthcare system. J Community Health. 2009;34(2):122–128. doi: 10.1007/s10900-008-9136-2. [DOI] [PubMed] [Google Scholar]
- 27.DeVoe JE, Baez A, Angier H, Krois L, Edlund C, Carney PA. Insurance + access not equal to health care: typology of barriers to health care access for low-income families. Ann Fam Med. 2007;5(6):511–518. doi: 10.1370/afm.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.OHP standard reservation list, final report. Salem, OR: Oregon Division of Medical Assistance Programs; 2008. [Google Scholar]
- 29.Allen H, Baicker K, Finkelstein A, Taubman S, Wright BJ Oregon Health Study Group. What the Oregon Health Study can tell us about expanding Medicaid. Health Aff (Millwood) 2010;29(8):1498–1506. doi: 10.1377/hlthaff.2010.0191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Center for Medicaid and Medicare Services. 2011–2012 eligible professional clinical quality measures (CQMs) Available at: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/CQM_EPs_2012_02_02.pdf. Accessed December 5, 2014.
- 31.HEDIS. Washington, DC: National Committee for Quality Assurance; 2013. 2013: technical specifications for physician measurement. [Google Scholar]
- 32.Devoe JE. Assessing a Medicaid randomized insurance experiment within community clinics. Available at: https://clinicaltrials.gov/ict2/show/NCT02355132. Accessed February 1, 2015.
- 33.Office of the Secretary. Health and Human Resources. Annual update of the HHS poverty guidelines. 2013. Available at: https://federalregister.gov/a/2013-01422. Accessed December 1, 2014.
- 34.Katz MH. Health insurance is not health care. JAMA Intern Med. 2014;174(6):859–860. doi: 10.1001/jamainternmed.2014.598. [DOI] [PubMed] [Google Scholar]
- 35.Kulesher RR. Health reform’s impact on federally qualified community health centers: the unintended consequence of increased Medicaid enrollment on the primary care medical home. Health Care Manag (Frederick) 2013;32(2):99–106. doi: 10.1097/HCM.0b013e31828ef5d5. [DOI] [PubMed] [Google Scholar]
- 36.Andrulis DP, Siddiqui NJ. Health reform holds both risks and rewards for safety-net providers and racially and ethnically diverse patients. Health Aff (Millwood) 2011;30(10):1830–1836. doi: 10.1377/hlthaff.2011.0661. [DOI] [PubMed] [Google Scholar]
- 37.The Obama administration and community health centers. Washington, DC: The White House; 2012. [Google Scholar]
- 38.Baltimore, MD: The Department of Health and Human Services, Centers for Medicare and Medicaid Services; 2013. Facilitating Medicaid and CHIP enrollment and renewal in 2014. [Google Scholar]
- 39.DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003;93(5):786–791. doi: 10.2105/ajph.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xu KT. Usual source of care in preventive service use: a regular doctor versus a regular site. Health Serv Res. 2002;37(6):1509–1529. doi: 10.1111/1475-6773.10524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim MY, Kim J, Choi I, Hwang I, Kim S. Effects of having usual source of care on preventive services and chronic disease control: a systematic review. Korean J Fam Med. 2012;33(6):336–345. doi: 10.4082/kjfm.2012.33.6.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heintzman J, Marino M, Hoopes M et al. Using electronic health record data to evaluate preventive service utilization among uninsured safety net patients. Prev Med. 2014;67:306–310. doi: 10.1016/j.ypmed.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Davidoff A, Kenney G, Dubay L. Effects of the state children’s health insurance program expansions on children with chronic health conditions. Pediatrics. 2005;116(1):e34–e42. doi: 10.1542/peds.2004-2297. [DOI] [PubMed] [Google Scholar]
- 44.Cowburn S, Carlson M, Lapidus J, Heintzman J, Bailey S, DeVoe JDP. Insurance continuity and human papillomavirus vaccine uptake in Oregon and California federally qualified health centers. Am J Public Health. 2014;104(9):e71–e79. doi: 10.2105/AJPH.2014.302007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Skinner EH, Foster M, Mitchell G et al. Effect of health insurance on the utilization of allied health services by people with chronic disease: a systematic review and meta-analysis. Aust J Prim Health. 2014;20(1):9–19. doi: 10.1071/PY13092. [DOI] [PubMed] [Google Scholar]
- 46.Hadley J, Cunningham P. Availability of safety net providers and access to care of uninsured persons. Health Serv Res. 2004;39(5):1527–1546. doi: 10.1111/j.1475-6773.2004.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hadley J. Insurance coverage, medical care use, and short-term health changes following an unintentional injury or the onset of a chronic condition. JAMA. 2007;297(10):1073–1084. doi: 10.1001/jama.297.10.1073. [DOI] [PubMed] [Google Scholar]
- 48.Starfield B, Shi L. The medical home, access to care, and insurance: a review of evidence. Pediatrics. 2004;113(5, suppl):1493–1498. [PubMed] [Google Scholar]
- 49.Petterson SM, Liaw WR, Phillips R et al. Projecting US primary care physician workforce needs: 2010–2025. Ann Fam Med. 2012;10(6):503–509. doi: 10.1370/afm.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]