Abstract
Emergency coronary artery bypass grafting (CABG) is associated with increased in-hospital mortality rates and adverse events. This study retrospectively evaluated indications and outcomes in patients who underwent emergency CABG.
The Society of Thoracic Surgeons database for a single center (Jewish Hospital) was queried to identify patients undergoing isolated CABG. Univariate analysis was performed.
From January 2003 through December 2013, 5,940 patients underwent CABG; 212 presented with emergency status. A high proportion of female patients (28.2%) underwent emergency surgery. Emergency CABG patients experienced high rates of intra-aortic balloon pump support, bleeding, dialysis, in-hospital death, and prolonged length of stay. The proportion of emergency coronary artery bypass grafting declined during years 2008–2013 compared with 2003–2007 (2.2% vs. 4.5%, P < 0.001), but the incidence of angiographic accident (5.3% vs. 29.2%) increased as an indication.
Ongoing ischemia remains the most frequent indication for emergency CABG, yet the incidence of angiographic accident has greatly increased. In-hospital mortality rates and adverse events remain high. If we look specifically at emergency CABG cases arising from angiographic accident, we find that 14 (15%) of all 93 emergency CABG deaths occurred in that subset of patients. Efforts to improve outcomes should therefore be focused on this high-risk group.
Keywords: Coronary artery bypass/statistics & numerical data/trends, emergency, hospital mortality, myocardial reperfusion injury, myocardial revascularization/trends, percutaneous coronary intervention/trends, retrospective studies, treatment outcome
The prevalence of cardiovascular diseases continues to increase and is currently estimated at 34% in the United States.1 The most serious consequence of coronary artery disease is acute coronary syndrome (ACS), which can lead to long-term disability and death. Mortality rates from ACS for men and women older than 40 years of age are 18% and 23%, respectively, and account for nearly 1.5 million hospital admissions in the U.S. annually.1
Treatment for patients with ACS is coronary revascularization. Historically, this was achieved with coronary artery bypass grafting (CABG); however, the advent of percutaneous coronary intervention (PCI) over 30 years ago brought about an increase in PCI and a decrease in CABG during those decades by 5% per year.2 Today, more than 395,000 CABG procedures are performed annually in the United States.3 A small proportion of these procedures are performed in emergency situations, most often because of ongoing ischemia, angiographic accidents, multivessel disease, or anatomic unsuitability for PCI.4 Emergency CABG is associated with significantly higher adverse outcomes, including death, when compared with elective CABG.5–7 Although several investigators have studied emergency CABG outcomes,5,6,8–11 indications and outcomes of emergency CABG in recent years have not been fully reported; consequently, the ideal treatment strategy for patients who meet criteria for surgical revascularization is not clear. This study was performed to evaluate the indications and outcomes for patients who underwent emergency CABG at a single institution.
Patients and Methods
This study was conducted in accordance with Federal regulations, after University of Louisville Institutional Review Board approval. The Society of Thoracic Surgeons (STS) database for Jewish Hospital, Louisville, Kentucky, was queried for data from January 2003 through December 2013, to retrospectively identify patients who underwent isolated CABG. Patients who underwent unrelated procedures, such as carotid endarterectomy at the time of CABG, were excluded. Further demographic and clinical data were obtained from the STS database and hospital medical records.
All patients who underwent isolated CABG were classified into 2 groups, emergency and nonemergency, on the basis of the preoperative urgency for the surgery. Emergency status was assigned at the time of operation by the operating surgeon, in accordance with the STS database, to patients with refractory cardiac compromise not responsive to therapy—short of surgical intervention. Nonemergency status was given to all other patients who underwent isolated CABG.
Preoperative, operative, and short-term outcome variables were analyzed for both groups. The emergency group was further studied, to identify the indications that led to emergency surgery. On the basis of when the operation was performed, the emergency group was stratified by year and then classified into 2 periods of time: 2003–2007 and 2008–2013. Indications for emergency CABG include evolving myocardial infarction (MI), angiographic accident, shock, ongoing ischemia, and other. These terms are again defined in accordance with the STS database: for example, “angiographic accident” as an attempted PCI causing a coronary artery dissection that results in hemodynamic instability; “ongoing ischemia” as ischemia refractory to medical therapy, including intra-aortic balloon pump (IABP) therapy; and “shock” as ventricular dysfunction refractory to medical and IABP therapy.
Statistical Analysis
Univariate and descriptive statistical methods were used for analysis. The Student t and χ2 tests were used to compare preoperative, perioperative, and postoperative variables. A pie chart was computed to delineate, within the 2 periods of time, the indications for emergency surgery. Results are reported as number and percentage or mean ± SD. P values <0.05 are considered significant. All statistical analyses were performed with use of SPSS version 21 (IBM Corporation; Endicott, New York).
Results
During the 11-year time period (2003–2013), 5,940 patients underwent CABG. Of those, 212 (3.6%) were classified as emergency cases and 1,803 (30.4%) were classified as urgent. Patients with an urgent status were included in the nonemergency group. Table I shows the results for all comorbidities in the emergency and nonemergency groups. Table II shows all preoperative, operative, and postoperative variables.
TABLE I.
Demographic Characteristics of Patients Undergoing Nonemergency and Emergency Coronary Artery Bypass Grafting
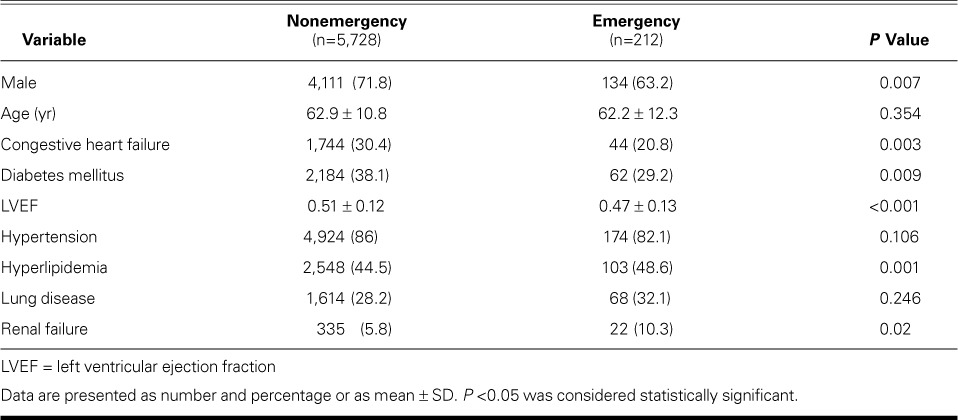
TABLE II.
Outcomes in Patients Undergoing Nonemergency versus Emergency Coronary Artery Bypass Grafting
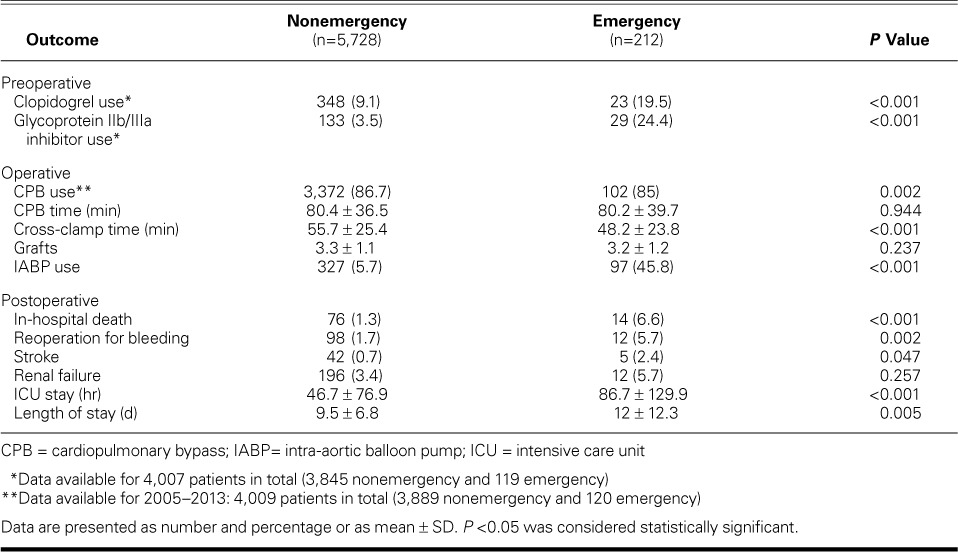
Postoperatively, emergency CABG patients had poor outcomes in terms of in-hospital death, reoperation for bleeding, and permanent deficit from a neurologic event. The incidence of renal failure, defined as an increase in serum creatinine by threefold (or >4 mg/dL), was high at 17.1% for the emergency group.
Table III shows the causes of death for the 14 patients who underwent emergency CABG followed by in-hospital death. Most of these patients died from causes of cardiac origin: 7 patients had sustained ventricular failure, one had intractable ventricular fibrillation, and one had ventricular rupture approximately one week after emergency revascularization. Three patients died of multiorgan failure, and their families chose to withdraw care after a prolonged hospital course. Two patients developed sepsis after CABG, due to pneumonia in one and endocarditis in the other.
TABLE III.
Cause of Death in 14 Patients Undergoing Emergency Coronary Artery Bypass Grafting
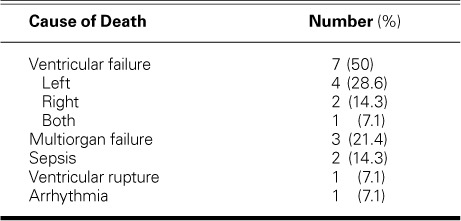
Figure 1 shows the number of CABG procedures performed at Jewish Hospital yearly, stratified by nonemergency and emergency status. Overall, the total number of cases decreased from 1,017 in 2003 to 319 in 2013. Of the total, the number of all emergency CABG cases decreased from 41 in 2003 to 11 in 2013. The proportion of emergency CABG cases declined during 2008–2013 (2.2%), in comparison with 2003–2007 (4.5%, P <0.001). Indications remained stable between time periods except for angiographic accident, which increased from 5.3% to 29.2%. These figures exclude cases with missing information (Fig. 2). If we look specifically at emergency CABG cases arising from angiographic accident, we find that 14 (15.4%) of all 93 emergency CABG deaths came from that subset of patients.
Fig. 1.
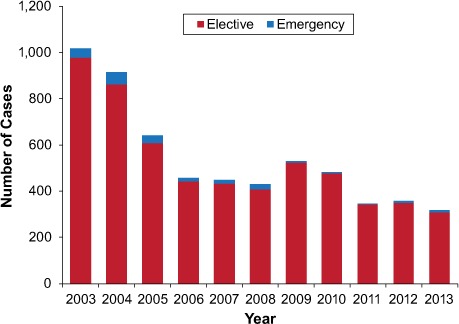
Graph shows the number of coronary artery bypass grafting procedures performed at our institution annually from 2003 through 2013, stratified by nonemergency and emergency status.
Fig. 2.
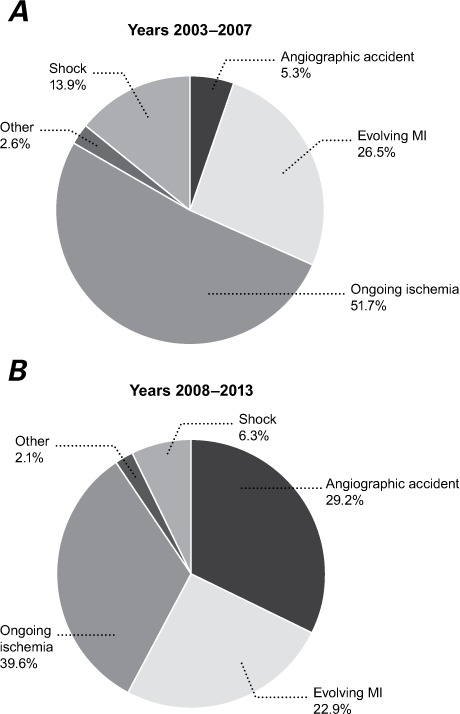
Pie charts show indications for emergency coronary artery bypass grafting stratified by time period 2003–2007 versus time period 2008–2013. A) In 2003–2007, angiographic accidents accounted for 5.3% of emergency operations. B) In 2008–2013, this percentage increased dramatically to 29.2%.
MI = myocardial infarction
Discussion
Our study presents one of the larger series of emergency CABG cases in the recent medical literature: more than 200 patients in the emergency CABG arm. According to Rastan and colleagues,6 these patients represent approximately 3% of all patients undergoing isolated CABG, yet they account for 20% of postoperative deaths overall. Although our study is consistent with the trend toward worsened outcomes in cases of emergency CABG, specific mortality (and other) postoperative outcomes are often mixed.
In a retrospective, single-center study of outcomes in 57 patients who underwent emergency CABG, Christiansen and Autschbach11 reported an in-hospital mortality rate of 12.2%, compared with our rate of 8.7%. Postoperative intensive-care-unit, mechanical-ventilation, and overall-hospital days were also considerably longer in their case-controlled study. This could be explained by our population's lower frequency of comorbid conditions. In a study examining immediate surgical coronary revascularization for acute MI, Khaladj and associates5 showed a 30-day mortality rate of 6%, slightly lower than ours. In a similar study, Sezai and co-authors12 reported an 11.4% mortality rate for patients after emergency CABG for acute MI. The lower mortality rate in the Khaladj and colleagues5 report (lower than the rate reported in this current study) is most likely the result of our including indications for emergency CABG in our study, which gives us an acutely sicker patient cohort. Refractory shock was present in 11% of patients in the Khaladj and colleagues5 study, whereas it was present in 20% of our emergency CABG population. Using STS variables to model operative risk, Shahian and colleagues13 reported a mortality rate of 8.1% when isolated CABG was classified as an emergency. Despite their variations, these studies indicate that mortality rates remain high after emergency CABG and are greatly dependent on comorbidities and indications for revascularization.
We also found that the proportion of women who underwent emergency CABG was high, at 36.8%. Women frequently present with an atypical clinical picture of ACS, often lacking chest pain14 and tending to lack ST-segment elevations on presentation. This can delay diagnosis and, as a consequence, can lead to clinical deterioration, necessitating operative intervention because of shock, worsening ischemia, or worsening MI.15 In addition, we found an increased use of glycoprotein IIb/IIIa inhibitors or clopidogrel in ACS patients who presented, respectively, with or without ST-segment-elevation MI (STEMI). Finally, as one would expect, postoperative sequelae were high for patients undergoing emergency CABG. Mortality rates nearly quadrupled in the emergency CABG group but did remain under 10%.
Emergency CABG is indicated for patients with left main coronary stenosis, 3-vessel disease, a history of failed PCI or an anatomy unsuitable for PCI, ongoing ischemia despite maximal nonsurgical therapy, angiographic accident, or cardiogenic shock with unsuitability for PCI.6 These patients are often supported with an IABP. Support with an IABP occurred in 45.7% of the emergency CABG patients in our study. Hemo and associates16 found an in-hospital mortality rate of 12.6% in a study examining long-term outcomes for patients undergoing CABG after preoperative support with an IABP. Although we identified ongoing ischemia as the most common indication for emergency CABG, we found that the proportion of angiographic accidents has increased in recent years. This runs contrary to an earlier study by Seshadri and colleagues,10 which found a decreased need for emergency CABG after angiographic accident, from 1.5% of PCIs in 1992 to 0.14% in 2000. However, the overall rate of PCI has declined over the last decade, because PCI now tends to be reserved for patients with more complex conditions.2 Whereas mortality rates after emergency CABG from all causes are reported to be between 7% and 12%,5,6,11,12 mortality rates in emergency CABG after attempted PCI are as high as 14%.17
These data are crucial in eventually improving outcomes for these patients. The steps to follow will include determining which patients should be considered for emergency CABG and what the optimal timing for surgical intervention should be. This question is central to current studies examining the European System for Cardiac Operative Risk Evaluation II (EuroSCORE II), which is a modification of the original EuroSCORE developed in 1999 to evaluate a patient's preoperative risk before undergoing a cardiac procedure.18 Although EuroSCORE II has been shown to accurately predict postoperative death, it has not been shown to reliably exclude patients from consideration for emergency CABG.19,20 Correct patient selection and the timing of surgery are essential to reduce sequelae and death from emergency CABG.
Our study is limited by its collection of data at a single institution. We also chose to exclude patients who underwent additional procedures concurrently with emergency CABG. Further examination of this population could yield better prognostic data about patients who need emergency cardiac surgery because of ACS and STEMI and could yield ways to improve overall outcomes. Finally, the number of patients who underwent emergency CABG is small in comparison with the number who underwent nonemergency CABG, and there were some baseline differences that could lend bias to the comparison. The tables are shown as a reference.
Although emergency CABG accounts for only a small portion of all patients who undergo surgical coronary revascularization, these patients have a disproportionately high rate of postoperative sequelae and death. This report shows that efforts to improve outcomes in CABG should therefore be focused on this high-risk group.
Footnotes
From: Department of Cardiovascular and Thoracic Surgery, University of Louisville, Louisville, Kentucky 40202
Dr. Williams is now at Philadelphia Heart Institute, University of Pennsylvania, Philadelphia, Pennsylvania.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Riley RF, Don CW, Powell W, Maynard C, Dean LS. Trends in coronary revascularization in the United States from 2001 to 2009: recent declines in percutaneous coronary intervention volumes. Circ Cardiovasc Qual Outcomes. 2011;4(2):193–7. doi: 10.1161/CIRCOUTCOMES.110.958744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Hospital Discharge Summary: 2010 table. CDC/National Center for Health Statistics [Internet] Available from: http://www.cdc.gov/nchs/fastats/inpatient-surgery.htm [2015 April 29; cited 2016 Mar 30]
- 4.American College of Emergency Physicians; Society of Cardiovascular Angiography and Interventions. O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78–140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 5.Khaladj N, Bobylev D, Peterss S, Guenther S, Pichlmaier M, Bagaev E et al. Immediate surgical coronary revascularisation in patients presenting with acute myocardial infarction. J Cardiothorac Surg. 2013;8:167. doi: 10.1186/1749-8090-8-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rastan AJ, Eckenstein JI, Hentschel B, Funkat AK, Gummert JF, Doll N et al. Emergency coronary artery bypass graft surgery for acute coronary syndrome: beating heart versus conventional cardioplegic cardiac arrest strategies. Circulation. 2006;114(1 Suppl):I477–85. doi: 10.1161/CIRCULATIONAHA.105.001545. [DOI] [PubMed] [Google Scholar]
- 7.Hagl C, Khaladj N, Peterss S, Martens A, Kutschka I, Goerler H et al. Acute treatment of ST-segment-elevation myocardial infarction: is there a role for the cardiac surgeon? Ann Thorac Surg. 2009;88(6):1786–92. doi: 10.1016/j.athoracsur.2009.07.050. [DOI] [PubMed] [Google Scholar]
- 8.Emmert MY, Salzberg SP, Seifert B, Schurr UP, Hoerstrup SP, Reuthebuch O, Genoni M. Routine off-pump coronary artery bypass grafting is safe and feasible in high-risk patients with left main disease. Ann Thorac Surg. 2010;89(4):1125–30. doi: 10.1016/j.athoracsur.2009.12.059. [DOI] [PubMed] [Google Scholar]
- 9.Roy P, de Labriolle A, Hanna N, Bonello L, Okabe T, Pinto Slottow TL et al. Requirement for emergent coronary artery bypass surgery following percutaneous coronary intervention in the stent era. Am J Cardiol. 2009;103(7):950–3. doi: 10.1016/j.amjcard.2008.12.025. [DOI] [PubMed] [Google Scholar]
- 10.Seshadri N, Whitlow PL, Acharya N, Houghtaling P, Blackstone EH, Ellis SG. Emergency coronary artery bypass surgery in the contemporary percutaneous coronary intervention era. Circulation. 2002;106(18):2346–50. doi: 10.1161/01.cir.0000036595.92742.69. [DOI] [PubMed] [Google Scholar]
- 11.Christiansen S, Autschbach R. Results and treatment strategy for patients undergoing emergent coronary artery bypass grafting. Ann Thorac Cardiovasc Surg. 2010;16(3):168–73. [PubMed] [Google Scholar]
- 12.Sezai A, Hata M, Yoshitake I, Kimura H, Takahashi K, Hata H, Shiono M. Results of emergency coronary artery bypass grafting for acute myocardial infarction: importance of intraoperative and postoperative cardiac medical therapy. Ann Thorac Cardiovasc Surg. 2012;18(4):338–46. doi: 10.5761/atcs.oa.11.01821. [DOI] [PubMed] [Google Scholar]
- 13.Shahian DM, O'Brien SM, Filardo G, Ferraris VA, Haan CK, Rich JB et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 1--coronary artery bypass grafting surgery. Ann Thorac Surg. 2009;88(1 Suppl):S2–22. doi: 10.1016/j.athoracsur.2009.05.053. [DOI] [PubMed] [Google Scholar]
- 14.Canto JG, Goldberg RJ, Hand MM, Bonow RO, Sopko G, Pepine CJ, Long T. Symptom presentation of women with acute coronary syndromes: myth vs reality. Arch Intern Med. 2007;167(22):2405–13. doi: 10.1001/archinte.167.22.2405. [DOI] [PubMed] [Google Scholar]
- 15.Sezai A, Minami K, Hata M, Yoshitake I, Wakui S, Takasaka A et al. Long-term results (three-year) of emergency coronary artery bypass grafting for patients with unstable angina pectoris. Am J Cardiol. 2010;106(4):511–6. doi: 10.1016/j.amjcard.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 16.Hemo E, Medalion B, Mohr R, Paz Y, Kramer A, Uretzky G et al. Long-term outcomes of coronary artery bypass grafting patients supported preoperatively with an intra-aortic balloon pump. J Thorac Cardiovasc Surg. 2014;148(5):1869–75. doi: 10.1016/j.jtcvs.2013.12.063. [DOI] [PubMed] [Google Scholar]
- 17.Yang EH, Gumina RJ, Lennon RJ, Holmes DR, Jr, Rihal CS, Singh M. Emergency coronary artery bypass surgery for percutaneous coronary interventions: changes in the incidence, clinical characteristics, and indications from 1979 to 2003. J Am Coll Cardiol. 2005;46(11):2004–9. doi: 10.1016/j.jacc.2005.06.083. [DOI] [PubMed] [Google Scholar]
- 18.Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE) Eur J Cardiothorac Surg. 1999;16(1):9–13. doi: 10.1016/s1010-7940(99)00134-7. [DOI] [PubMed] [Google Scholar]
- 19.Biancari F, Vasques F, Mikkola R, Martin M, Lahtinen J, Heikkinen J. Validation of EuroSCORE II in patients undergoing coronary artery bypass surgery. Ann Thorac Surg. 2012;93(6):1930–5. doi: 10.1016/j.athoracsur.2012.02.064. [DOI] [PubMed] [Google Scholar]
- 20.Paparella D, Guida P, Di Eusanio G, Caparrotti S, Gregorini R, Cassese M et al. Risk stratification for in-hospital mortality after cardiac surgery: external validation of EuroSCORE II in a prospective regional registry. Eur J Cardiothorac Surg. 2014;46(5):840–8. doi: 10.1093/ejcts/ezt657. [DOI] [PubMed] [Google Scholar]


