Abstract
Cardiac myxoma is the most common cardiac tumor in patients of all ages; the majority are encountered as single left atrial tumors. Left ventricular myxomas are exceedingly rare, having been recorded in a small number of case reports involving children worldwide. We report a case of a left ventricular myxoma with left ventricular outflow tract obstruction in a previously healthy, asymptomatic adolescent black male. Transthoracic echocardiograms revealed a single, large (2.5 × 5-cm), lobulated, mobile mass within the left ventricular cavity that oscillated into the outflow tract, thereby causing moderate obstruction during systole. Advanced images delineated the location and tissue composition of the mass, characterizing it as a myxoma. Complete surgical excision of the mass was accomplished via aortotomy. Gross examination and histology confirmed the diagnosis of myxoma.
Keywords: Adolescent, cardiac magnetic resonance, cardiac tumors, heart murmurs/diagnosis, left ventricle/pediatric, magnetic resonance imaging/methods, male, myxoma/complications
Myxomas constitute about 50% of primary cardiac tumors in patients of all ages and are the 3rd most prevalent cardiac tumor among children. Cardiac myxomas are typically atrial in origin. Conversely, myxomas arising from the left ventricle (LV) and obstructing the LV outflow tract (LVOT) are rarely reported.1 Tumors of the LV are more frequently diagnosed because of signs and symptoms suggestive of cardiac pathologic conditions including syncope, thromboembolism, arrhythmias, congestive heart failure, and sudden death.1,2 We report a highly unusual case of an asymptomatic adolescent male with a common subtype of pediatric cardiac tumor in a rare location within the LV.
Case Report
A 12-year-old, asymptomatic black male without a significant medical history was referred to our cardiology department for a harsh murmur noted during a pre-participation sports physical examination. He had no spotty skin pigmentation or lentigines. His family history was negative for cardiac disease and thrombophilia. A transthoracic echocardiogram revealed a 2.5 × 5-cm single, lobulated, mobile, echogenic mass within the LV cavity (Fig. 1A), oscillating toward the LVOT and causing moderate obstruction (peak gradient, 35–40 mmHg; mean gradient, 21 mmHg). Magnetic resonance imaging (MRI) confirmed the findings of a heterogeneous, T2-enhancing mass within the LV cavity, with attachments to the ventricular septum (Fig. 1B). This confirmed our plan to perform surgical resection via aortotomy.
Fig. 1.
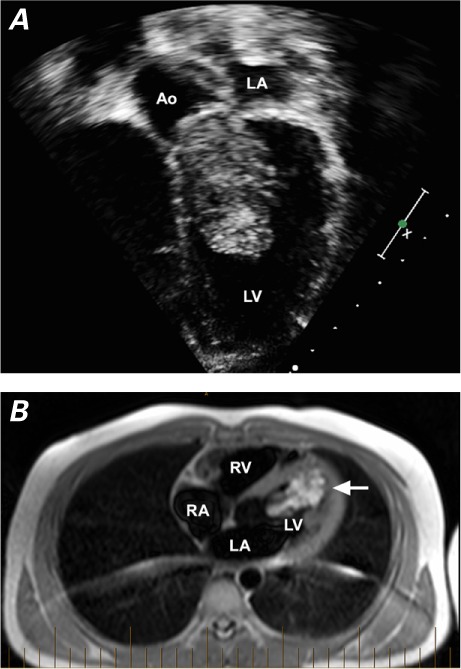
A) Two-dimensional transthoracic echocardiogram shows a 2.5 × 5-cm, lobulated echogenic mass within the left ventricular cavity, obstructing the left ventricular outflow tract. B) Cardiac magnetic resonance image shows the increased T2 signal of the mass (arrow) within the left ventricular cavity. Additional characteristics of the mass include an associated low T1 signal, irregular borders on steady-state free precession sequences, and heterogeneous enhancement on 5- and 10-minute delayed post-contrast imaging.
Ao = aorta; LA = left atrium; LV = left ventricle; RA = right atrium; RV = right ventricle
In the operating room, the LV was exposed via an aortotomy, and a large, multilobulated, gelatinous mass was found partially protruding from the LVOT. A broad-based stalk was attached to the lateral apical wall of the LV but spared the mitral valve apparatus. The mass was removed in a piecemeal fashion, thereby ensuring complete resection of the base (Fig. 2A). Once excision was complete, direct inspection revealed no residual tumor within the LV. A postoperative transesophageal echocardiogram verified no residual mass, no injury to the ventricular septum, to the LVOT, or to the aortic valve, and resolution of the LVOT gradient. The patient's recovery was uneventful, and he was discharged from the hospital on postoperative day 4. A final histologic review of the mass confirmed the diagnosis of a myxoma (Fig. 2B). At routine follow-up evaluation, the patient was doing well with no residual hemodynamic concerns or arrhythmia and no recurrence of the myxoma.
Fig. 2.

A) Photograph shows the segments of a large multilobulated mass removed piecemeal via sharp dissection. B) Photomicrograph shows stellate-shaped cells loosely dispersed within a basophilic-staining mucoid ground substance consistent with myxoma (H & E, orig. ×400).
Discussion
Most myxomas of ventricular origin present with signs and symptoms associated with such cardiac pathologic conditions as syncope, thromboembolism, arrhythmias, congestive heart failure, and sudden death.1,2 Conversely, our patient was asymptomatic and had been referred for routine evaluation of an incidental cardiac murmur. Upon further investigation with echocardiography, the patient was found to have a large tumor in the LV, partially obstructing the LVOT.
Cardiac MRI offers a noninvasive alternative for comprehensive cardiac evaluation and provides several advantages, such as temporal resolution superior to that of echocardiography and soft-tissue contrast resolution superior to that of computed tomography.3–5 In this patient, the finding of a pedunculated mobile mass—with irregular borders on steady-state free precession images, hyperintensity on T2-weighted sequences, and delayed heterogeneous post-contrast enhancement on MRI—was consistent with the diagnosis of benign myxoma before definitive surgical removal and histologic analysis. This was important clinically, because differentiating the mass from other cardiac tumors could have had profound implications on treatment. For example, hemangiomas, thromboses, or lymphoma would present additional risks for surgery, as well as prompt additional interventions such as anticoagulation or chemotherapy. Furthermore, the advanced imaging was used to guide surgical planning for complete resection of the mass via aortotomy, thereby giving the patient an improved risk profile by obviating the need for ventriculotomy.
Acknowledgments
The authors thank Drs. Vivekanand Singh and Eugenio Taboada for providing the histologic slides and analysis for this case report.
Footnotes
From: Divisions of Cardiology (Drs. Chlebowski, O'Brien, and Wagner) and Clinical Pharmacology, Medical Toxicology and Therapeutic Innovation (Dr. Wagner), Children's Mercy Hospital, Kansas City, Missouri 64108; Departments of Pediatrics (Drs. Chlebowski and Wagner) and Surgery (Dr. O'Brien), University of Missouri-Kansas City School of Medicine, Kansas City, Missouri 64108; and Division of Cardiovascular Surgery, University of Kansas Medical Center and Department of Surgery University of Kansas School of Medicine (Dr. Hertzenberg), Kansas City, Kansas 66160
References
- 1.Miyake CY, Del Nido PJ, Alexander ME, Cecchin F, Berul CI, Triedman JK et al. Cardiac tumors and associated arrhythmias in pediatric patients, with observations on surgical therapy for ventricular tachycardia. J Am Coll Cardiol. 2011;58(18):1903–9. doi: 10.1016/j.jacc.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Kure K, Lingamfelter D, Taboada E. Large multifocal cardiac myxoma causing the sudden unexpected death of a 2-month-old infant--a rapidly growing, acquired lesion versus a congenital process? A case report. Am J Forensic Med Pathol. 2011;32(2):166–8. doi: 10.1097/PAF.0b013e318219c84c. [DOI] [PubMed] [Google Scholar]
- 3.Ghadimi Mahani M, Lu JC, Rigsby CK, Krishnamurthy R, Dorfman AL, Agarwal PP. MRI of pediatric cardiac masses. AJR Am J Roentgenol. 2014;202(5):971–81. doi: 10.2214/AJR.13.10680. [DOI] [PubMed] [Google Scholar]
- 4.Beroukhim RS, Prakash A, Buechel ER, Cava JR, Dorfman AL, Festa P et al. Characterization of cardiac tumors in children by cardiovascular magnetic resonance imaging: a multi-center experience. J Am Coll Cardiol. 2011;58(10):1044–54. doi: 10.1016/j.jacc.2011.05.027. [DOI] [PubMed] [Google Scholar]
- 5.Motwani M, Kidambi A, Herzog BA, Uddin A, Greenwood JP, Plein S. MR imaging of cardiac tumors and masses: a review of methods and clinical applications. Radiology. 2013;268(1):26–43. doi: 10.1148/radiol.13121239. [DOI] [PubMed] [Google Scholar]


