Supplemental Digital Content is available in the text
Key Words: certification, multilevel models, patient falls, patient safety, quality improvement
Abstract
Background
Researchers have studied inpatient falls in relation to aspects of nurse staffing, focusing primarily on staffing levels and proportion of nursing care hours provided by registered nurses (RNs). Less attention has been paid to other nursing characteristics, such as RN national nursing specialty certification.
Objective
The aim of the study was to examine the relationship over time between changes in RN national nursing specialty certification rates and changes in total patient fall rates at the patient care unit level.
Methods
We used longitudinal data with standardized variable definitions across sites from the National Database of Nursing Quality Indicators. The sample consisted of 7,583 units in 903 hospitals. Relationships over time were examined using multilevel (units nested in hospitals) latent growth curve modeling.
Results
The model indices indicated a good fit of the data to the model. At the unit level, there was a small statistically significant inverse relationship (r = −.08, p = .04) between RN national nursing specialty certification rates and total fall rates; increases in specialty certification rates over time tended to be associated with improvements in total fall rates over time.
Discussion
Our findings may be supportive of promoting national nursing specialty certification as a means of improving patient safety. Future study recommendations are (a) modeling organizational leadership, culture, and climate as mediating variables between national specialty certification rates and patient outcomes and (b) investigating the association of patient safety and specific national nursing specialty certifications which test plans include patient safety, quality improvement, and diffusion of innovation methods in their certifying examinations.
Because of their frequency, cost, and consequences, inpatient falls are an important indicator of patient safety (Brand & Sundararajan, 2010; Oliver, Killick, Even, & Willmott, 2008; Staggs, Mion, & Shorr, 2014; Wong et al., 2011). Researchers have studied falls in relation to various aspects of nurse staffing, focusing primarily on staffing levels and proportion of nursing care hours provided by registered nurses (RNs; e.g., Lake, Shang, Klaus, & Dunton, 2010; Staggs & Dunton, 2014). Less attention has been paid to experience and other nursing characteristics, such as RN national nursing specialty certification (Dunton, Gajewski, Klaus, & Pierson, 2007).
National nursing specialty certification is purported to improve quality of care and patient safety (Hickey et al., 2014; Institute of Medicine, 2010, 2015), so it is reasonable to expect that increasing national nursing specialty certification rates in acute care settings would contribute to a decrease in patient fall rates. However, varying levels of specificity about quality and patient safety exist in national nursing specialty certification test plans. For example, the Certified Medical-Surgical Registered Nurse (CMSRN) and the Medical-Surgical Nurse-Board Certified (RN-BC) test plans include content about minimizing adverse patient outcomes, reducing risk, and improving quality of care; falls are not listed specifically (American Nurses Credentialing Center, 2013a; Medical-Surgical Nursing Certification Board, 2014). Both the Certified Rehabilitation Registered Nurse (CRRN) and Gerontological Nurse-Board Certified (RN-BC) test plans are explicit about safety concerns, assessing safety risks, and safety interventions; falls are listed specifically (American Nurses Credentialing Center, 2013b; Association of Rehabilitation Nurses, 2014). Some national nursing certification programs, such as the CCRN (critical care) and the PCCN (progressive care), do not include content on patient safety or quality improvement as part of their test plans (American Association of Critical Care Nurses, 2014a, 2014b).
A few researchers have examined the link between specialty certification and patient falls in cross-sectional studies. Kendall-Gallagher and Blegen (2009) found that higher unit level RN certification rates—regardless of nurse education and experience—were associated with lower frequency of patient falls. Lange et al. (2009) found that units staffed with two or more geriatric-certified nurses had significantly lower fall rates than units with one or no geriatric-certified nurses. Similarly, Boltz, Capezuti, Wagner, Rosenberg, and Secic (2013) showed that units with higher RN certification rates in any specialty had lower fall rates, but geriatric certification rate by itself was not a significant predictor.
Recently, Boyle, Gajewski, and Miller (2012) examined changes over a 7-year period in acute care RN national nursing specialty certification rates and found that, in general, rates increased significantly over time, and Magnet designated hospitals had significantly higher rates than non-Magnet hospitals. Critical care, pediatric, and rehabilitation units had higher rates than medical, surgical, and step-down units. Units with the lowest national nursing specialty certification rates at the beginning of the 7-year period had the greatest increase in rates.
Bouldin et al. (2013) and He, Dunton, and Staggs (2012) studied time trends of inpatient fall rates. Bouldin et al. (2013) found a statistically significant decrease in both total falls and injurious falls over a 27-month time frame, with results varying by unit type. Total falls were highest in medical units. Similarly, He et al. (2012) found that fall rates decreased over a 6-year time frame (2004–2009), with results varying by unit type. The highest total fall rates were in rehabilitation units, and the lowest total fall rates were in critical care units.
Although national nursing specialty certification rates generally have increased over time whereas inpatient fall rates generally have decreased over time, researchers have not examined whether these national level trends are simply coincidence or reflect an actual association between increasing national nursing specialty certification rates and decreasing fall rates. Using longitudinal data with standardized variable definitions across sites from the National Database of Nursing Quality Indicators (NDNQI), we explored the issue by systematically examining the relationship over time between changes in RN national nursing specialty certification rates and changes in total fall rates at the patient care unit level.
Conceptual Model
Figure 1 is a multilevel (units nested in hospitals), longitudinal (years 2004–2010) model showing hypothesized relationships between RN national specialty certification rates and total fall rates. Our model is informed by a modification of Donabedian’s (1988) framework in which the structure and processes of care influence the outcomes of care; we focus only on structure and outcomes in this study. Structure refers to setting attributes, including provider characteristics, in which patient care takes place. Patient outcomes are results of care and include patient safety measures. Our main study structure variable was changeover time in national nursing specialty certification rates, and our main study outcome variable was changeover time in total fall rates. We controlled for a range of unit structure characteristics (nursing care hours and percentage of nurses holding a Bachelor of Science in Nursing [BSN] or higher degree) and hospital structure characteristics (Magnet status, bed size, ownership, and metropolitan location).
FIGURE 1.
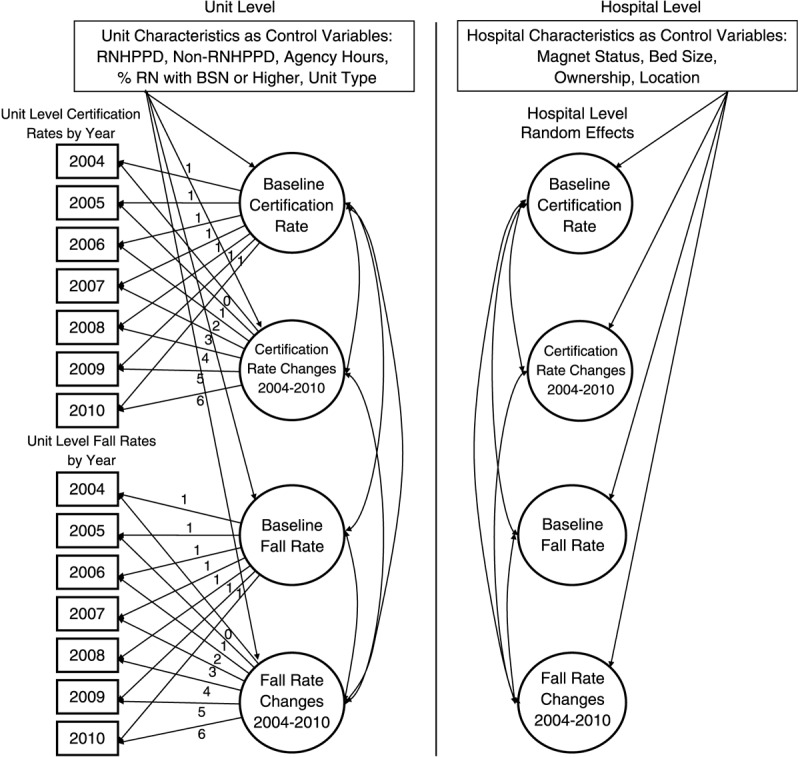
Theoretical model of RN national nursing specialty certification rates and patient total fall rates, showing hypothesized relationships. The figure depicts a multilevel latent growth curve model, which reflects variation in baseline rates and growth over time among units (unit level) and across hospitals (hospital level). Fixing loadings as shown allows linear change models to be estimated. RNHPPD = registered nurse hours per patient day; BSN = Bachelor of Science in Nursing.
Although we examined all relationships shown in Figure 1, our main study hypothesis was that, over time (2004–2010), units with greater increases in RN national nursing specialty certification rates would have greater decreases in total patient fall rates.
Methods
Our study was a secondary analysis of longitudinal data from the NDNQI. Two-level, multivariate, latent growth curve (or trend analysis) modeling was used to examine the relationships in the study conceptual model (Figure 1) and to our test hypothesis.
Sample
Patient care units were the main units of analysis—not the individual patient or nurse. The sample was limited to 7,583 units nested in 903 NDNQI hospitals that reported total patient fall rates and RN national specialty certification rates, as well as the control variables of nursing care hours (staffing levels) and RN education, for the years 2004 to 2010. All units were adult population-based and included critical care, step-down, medical, surgical, medical-surgical combined, and rehabilitation.
Measures
National Nursing Specialty Certification Rate National nursing specialty certification was reported by units to NDNQI once a year and was calculated as the percentage of unit RNs holding certification in a specialty area of nursing practice that was granted by a nationally accredited nursing certification program (Miller & Boyle, 2008). All certified nurses who spent 50% or more time in direct care were included in the rate calculation. Each certified RN was counted only once, regardless of how many certifications the RN held. Exclusions were (a) employer-based competencies, certifications, or other credentials; (b) courses such as Advanced Cardiac Life Support and Trauma Nurse Core Course; and (c) specialty certifications not direct care related. NDNQI national nursing specialty certification data collection began in 2002, but not until 2004 were there enough hospitals and units submitting data to provide an adequate sample size for longitudinal analysis.
Total Patient Fall Rate NDNQI (Simon, Klaus, Gajewski, & Dunton, 2013) defines a fall as an unplanned descent to the floor or other lower surface with or without an injury to the patient. The NDNQI total fall measure is National Quality Forum (NQF) endorsed as a national consensus measure and meets the rigorous NQF (2013) measurement criteria of importance, scientific acceptability (reliability and validity), usability, and feasibility. Reliability evidence of the total fall measure includes fall classification sensitivity of .90 and specificity of .88 (Simon et al., 2013) and an overall intraclass correlation (ICC[1,1]) of .85 (Garrard, Boyle, Simon, Dunton, & Gajewski, 2014), indicating substantial reliability of injury level assignment. Further detail about reliability and validity evidence for the NDNQI total fall measure is reported in Garrard et al. (2014) and Simon et al. (2013)
The total fall rate on each unit was calculated for each respective study year. To calculate the yearly fall rate, the total number of falls on a unit for the year was divided by the total number of patient days on that unit for the same period and then multiplied by 1,000.
Control Variables Unit structure characteristics included as control variables were percentage of unit RNs with a BSN or higher degree and the NDNQI nursing care hours variables RN hours per patient day (RNHPPD), non-RN hours per patient day (non-RNHPPD), and percentage of RN hours supplied by agency staff. The NDNQI nursing care hours variables are NQF endorsed. Reliability evidence of the nursing care hours measure includes ICCs for RNHPPD and non-RNHPPD of .96 and .72, respectively—indicating substantial reliability for RNHPPD and moderate reliability for non-RNHPPD (Choi, Boyle, & Dunton, 2014). Further detail about reliability and validity evidence for the nursing care hours measure can be found in Choi et al. (2014) and Klaus, Dunton, Gajewski, and Potter (2013).
Select hospital structure characteristics were included as control variables: the American Nurses Credentialing Center Magnet Recognition Program status (Magnet, not Magnet), hospital bed size (<100, 100–199, 200–299, 300–399, 400–499, ≥500), ownership (not-for-profit; for-profit; government, federal; government, nonfederal), and metropolitan location (≤50,000 population, >50,000 population).
Procedures
Approval for the study was obtained from the University of Kansas Medical Center’s Institutional Review Board. We then developed an analysis file, which was checked for errors and corrected as needed. File checking included manual checks of randomly selected hospitals to ensure the correct unit and hospital data were matched over the years 2004–2010 and investigating all outliers (e.g., unusually high fall rate) to determine if they were accurate or needed to be corrected (e.g., by contacting the hospital). NDNQI data quality procedures are described elsewhere (Boyle, Cramer, Potter, Gatua, & Stobinski, 2014).
Data Analysis
Descriptive statistics were generated using SAS version 9.2 to summarize hospital characteristics and unit characteristics at baseline (year 2004). RN national nursing specialty certification rates and total patient fall rates from 2004 to 2010 were plotted by unit type to show time trends.
Using Muthén and Muthén (1998/2009)) Mplus version 6.11, we fit multilevel (units nested in hospitals), latent growth curves using structural equation modeling. The model was estimated using maximum likelihood with robust standard errors to account for the outcome (patient falls) being a count variable. Unit level measures of total fall and national nursing specialty certification rates were used as indicators of the unit level latent variables (intercept and slope). The latent intercept (baseline 2004) variables for total fall rates and national nursing specialty certification rates were estimated by fixing the loadings for each variable (year of measure) to 1.0. The latent slope (rate of change over time) variables for both total fall rates and specialty certification rates were specified as linear by fixing the loading for 2004 to 0 and increasing the loading by one for each consecutive year. The hospital level latent variables reflect the random effects of hospital variation on unit level measures (see Figure 1). The Mplus code is available as Document, Supplemental Digital Content 1, http://links.lww.com/NRES/A148.
Conceptually, the time slopes indicate how rapidly national nursing specialty certification and total fall rates rose or declined over time—with larger positive (negative) slope values indicating greater increase (decrease) per year. This modeling framework allows for a change in total fall rates over time to be related to a change in national nursing specialty certification rates over time.
RNHPPD, non-RNHPPD, percentage of RN hours supplied by agency staff, and percentage of RNs with a BSN or higher were included as controls for the latent intercept and slope variables at the unit level. We also controlled for unit type because national nursing specialty certification rates and total fall rates vary by unit type. Magnet status, bed size, ownership, and metropolitan location were included as controls for the latent intercept and slope variables at the hospital level.
We assessed model fit using the comparative fit index (CFI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR), with the following criteria for acceptable fit: CFI > 0.90, RMSEA < 0.07, and SRMR < 0.05 (Hu & Bentler, 1999).
Results
Baseline Hospital and Unit Characteristics
The typical hospital in our sample (n = 903) was not-for-profit (85.2%) with less than 300 beds (71.4%) and located in a metropolitan area of greater than 50,000 population (97.0%). Magnet designation was held by almost one third of sample hospitals.
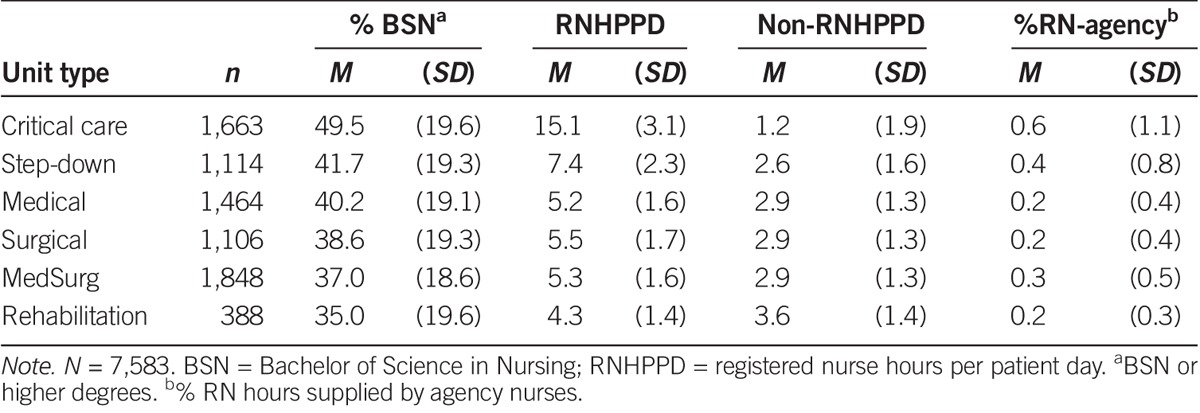
Among the 7,583 study units, there were 1,663 (21.9%) critical care, 1,114 (14.7%) step-down, 1,464 (19.3%) medical, 1,106 (14.6%) surgical, 1,848 (24.4%) medical-surgical combined, and 388 (5.1%) rehabilitation units. Table 1 displays the unit level control variable characteristics at baseline (2004) by unit type. Critical care units had higher mean RNHPPD, higher mean percentage of RN hours supplied by agency staff, and higher mean percentage of nurses with a BSN degree or greater than other unit types. Rehabilitation units had the lowest mean percentage of nursing hours supplied by agency.
TABLE 1.
Baseline Unit Level Characteristics by Unit Type
Longitudinal Description
RN National Nursing Specialty Certification Yearly RN national nursing specialty certification rates for each unit type are presented in Figure 2. The mean unit level specialty certification rates for critical care units (14.62% in 2004 to 19.34% in 2010) and rehabilitation units (13.92% in 2004 to 19.64% in 2010) were higher than mean rates for all other unit types, which were about 8–9.5% in 2004 and 10–13% in 2010. There was an overall increasing trend in mean national nursing specialty certification rates across all unit types.
FIGURE 2.
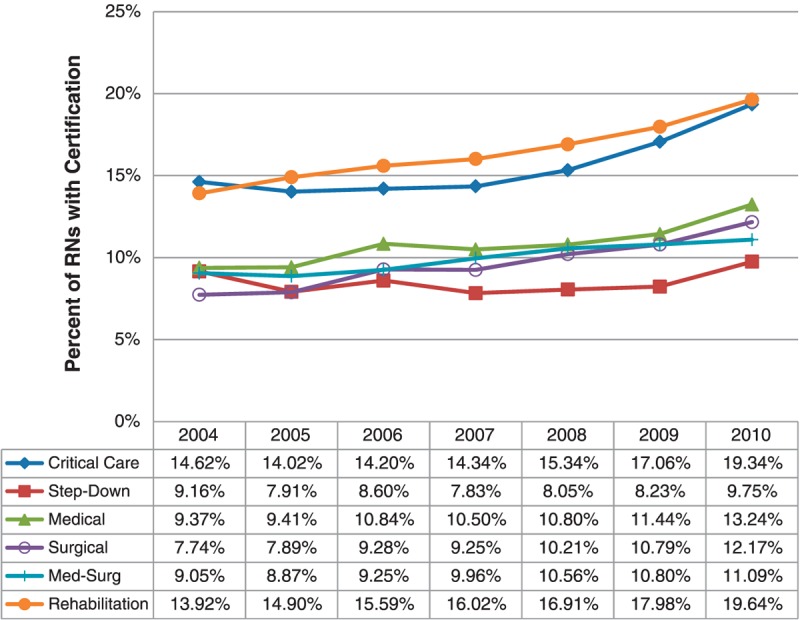
RN national specialty certification rate by unit type for 2004–2010.
Total Patient Fall Rates Figure 3 displays the yearly total fall rates for each unit type from 2004 to 2010. All unit types had a modest decrease in mean fall rates over time. Critical care units consistently had the lowest mean fall rates (1.58/1,000 patient days in 2004 to 1.29/1,000 patient days in 2010), and rehabilitation units consistently had the highest mean fall rates (6.97/1,000 patient days in 2004 to 6.60/1,000 patient days in 2010).
FIGURE 3.
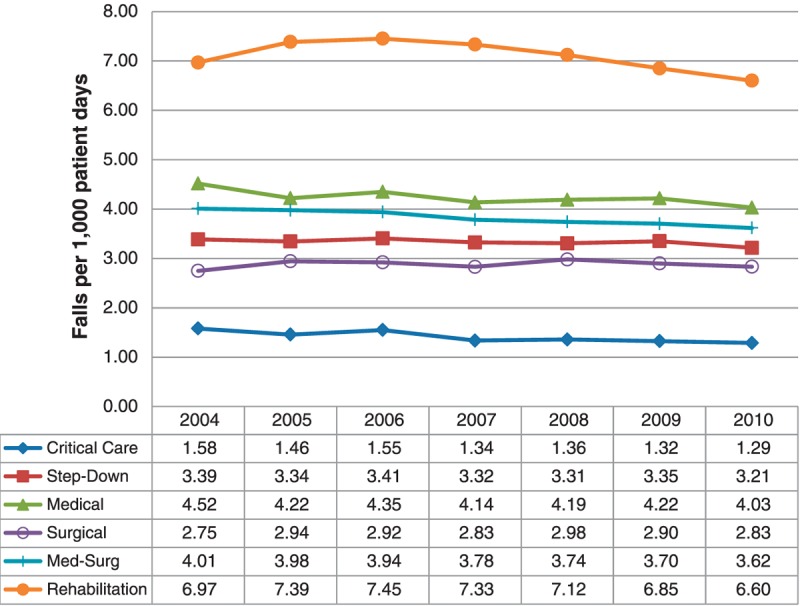
Total fall rate by unit type for 2004–2010.
Latent Growth Curve Modeling
The overall model indices indicated a good fit of the data to the model: CFI = .94; RMSEA = 0.02; SRMR (unit) = 0.03; SRMR (hospital) = 0.05. Figure 4 shows the significant (p ≤ .05) relationships in our study model. Standardized model results are presented below. Relationships between the main study variables of RN national nursing specialty certification rates (intercept and slope) and total patient fall rates (intercept and slope) are presented as correlational (r) relationships. Standardized regression weights (b*) are used to present the effects of the control variables on the main study variables.
FIGURE 4.
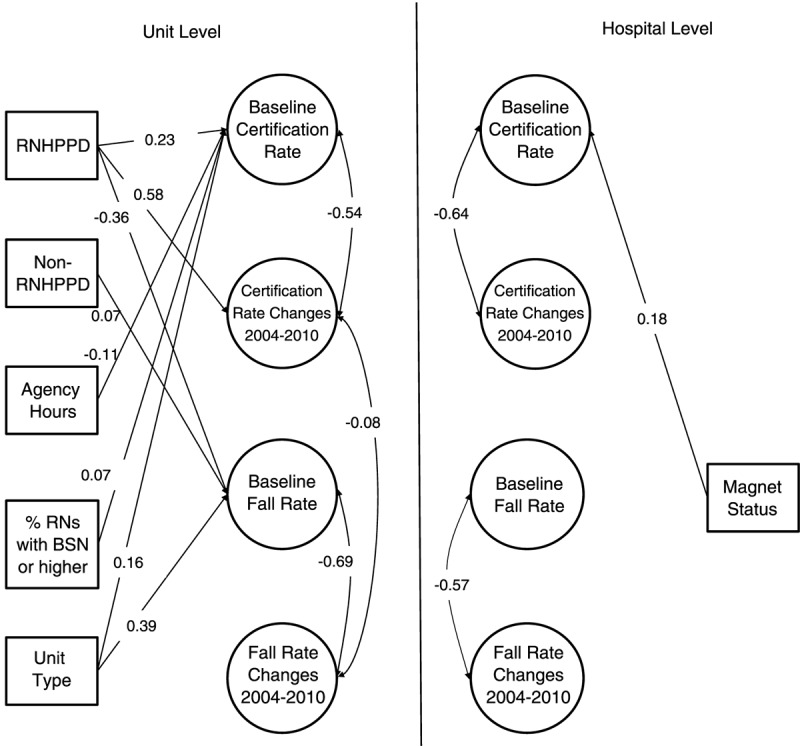
Significant parameter estimates in the multilevel latent growth curve model. Model fit statistics: χ2 = 1303.78, p < .01; RMSEA = 0.02; SRMR (unit) = 0.03; SRMR (hospital) = 0.05. Standardized model results are presented. Double-headed arrows show the significant correlational (r) relationships between the main study variables of RN national nursing specialty certification rates (intercept and slope) and total patient fall rates (intercept and slope). Single-headed arrows show standardized regression weights (b*) of the significant effects of the control variables on the main study variables. BSN = Bachelor of Science in Nursing; RMSEA = root mean squared error of approximation; RNHPPD = registered nurse hours per patient day; SRMR = standardized root mean residual.
At the unit level, the relationship between the 2004 national nursing specialty certification rates and the 2004 total patient fall rates was not significant (r = .02, p = .40). There was a small, statistically significant inverse relationship (r = −.08, p = .04) between the slope of national nursing specialty certification rates and the slope of total fall rates; meaning that on units where national nursing specialty certification rates increased over time, unit total fall rates tended to improve over time (decrease or increase at a slower rate—if fall rates on the respective unit were increasing).
Not surprisingly, we found that units (r = −.54, p < .01) and hospitals (r = −.64, p < .01) with higher national nursing specialty certification rates in 2004 tended to experience less increase (or greater decrease) in specialty certification rates over time, whereas units and hospitals with more room for improvement (in 2004) tended to see greater increases going forward. Also, units (r = −.69, p < .01) and hospitals (r = −.57, p < .01) with lower total fall rates (in 2004) experienced less decrease (or increases) in fall rates over time, whereas units and hospitals with higher total fall rates (in 2004) tended to see greater decreases over time. No other significant relationships were found.
Higher unit RNHPPD (b* = 0.23, p = .001), a higher percentage of unit RNs with a BSN or higher (b* = 0.16, p =.02), and a lower percentage of nursing hours supplied by agency nurses (b* = −0.11, p < .001) were associated significantly with higher unit national specialty certification rates at baseline. Only higher RNHPPD (b* = 0.06, p = .04) was associated with improvements over time in national specialty certification rates. Lower baseline total fall rates were significantly associated with higher RNHPPD (b* = −0.36, p < .001) and lower non-RNHPPD (b* = 0.07, p < .001). Having Magnet designation was associated with higher baseline specialty certification rates (b* = 0.18, p < .001); there were no other significant associations.
Discussion
We found a small, statistically significant inverse association between unit level changes in RN national nursing specialty certification rates and unit level changes in total fall rates during 2004–2010. Our findings may be suggestive that larger increases in national nursing specialty certification rates over time tend to be associated with improvements in total fall rates over time. Because our modeling was not causal, we do not know if the association was direct or whether improving national nursing specialty certification rates and total fall rates were both part of a larger effort to improve quality and patient safety in the units and hospitals. However, when considering our findings alongside those of Kendall-Gallagher and Blegen (2009), Lange et al. (2009), and Boltz et al. (2013), it seems likely that we can add national nursing specialty certification to the list of nursing characteristics associated with lower unit level total fall rates.
We also found that higher RNHPPD was associated with improvements in total fall rates over time. Although research on the associations of RNHPPD and percentage of nursing hours supplied by RNs with falls has not led to clear, definitive conclusions (in part because findings can differ by unit type [e.g., Lake et al., 2010; Staggs & Dunton, 2014]), quality of nurse staffing is clearly important in relation to falls. Higher levels of non-RNHPPD have been associated with higher fall rates in two studies (Lake et al., 2010) and higher mean RN tenure on the unit with lower falls in one study (Dunton et al., 2007).
The mechanism by which national nursing specialty certification rates may affect fall rates deserves some comment. It is unknown whether specific fall prevention methods included in national nursing specialty certification test plans (where such methods are included at all) are responsible for lower fall rates on units with a higher percentage of specialty certified nurses. Despite inpatient falls being a long time national patient safety issue (Institute of Medicine, 1999) and the Agency for Healthcare Research and Quality (2013) producing a fall prevention toolkit, three recent systematic reviews (Cameron et al., 2012; Coussement et al., 2008; Hempel et al., 2013) concluded that, despite the existence of promising approaches to fall prevention, there is “no conclusive evidence that hospital fall prevention programs can reduce the number of falls or fallers” (Coussement et al., 2008, p. 29).
A more plausible explanation for an association between national nursing specialty certification rates and falls is that specialty certified nurses have acquired greater awareness and more general knowledge of patient safety and quality of care, and this results in better patient outcomes overall. For example, a national nursing specialty certified nurse may provide consultation to noncertified nurses regarding patient care, so that patients not directly treated by specialty certified nurses may still benefit from their expertise (Institute of Medicine, 2015, p. 21). Future research linking higher national nursing specialty certification rates with lower rates of adverse outcomes would support this hypothesis. If true, one implication of the hypothesis is that general content on safety and quality (e.g., assessing for risk, tracking and benchmarking safety outcomes, conducting quality improvement studies, diffusion of innovations) is an important part of national nursing specialty certification test plans in its own right—even in the absence of effective, evidence-based methods for preventing a specific adverse outcome.
Needleman (Institute of Medicine, 2015, p. 19) recently proposed an expanded conceptual model for credentialing research in nursing that includes investigation of the “invisible architecture” as a mediating variable between national nursing specialty certified nurses and patient outcomes. The invisible architecture includes factors such as organizational leadership, culture, and climate. Specialty certified nurses expect higher levels of autonomy and decision-making (Boyle et al., 2014), yet they may not be afforded the opportunity for autonomous practice in acute care settings because the invisible architecture is unfavorable to more autonomy. Therefore, a plausible explanation of our finding of a small—as opposed to a moderate or strong—inverse association between unit level changes over time in RN national nursing specialty certification rates and unit level changes over time in total fall rates may be an unfavorable invisible infrastructure. Future research guided by the Expanded Conceptual Model is needed.
Our NDNQI data set did not include specific national specialty certifications held by RNs on study units. In future research, linking patient safety and quality to specific national nursing specialty certifications which test plans include general patient safety content about risk assessment, prevention protocols, monitoring unit level patient safety data, quality improvement methods, and diffusion of innovation methods in their certifying examinations may provide more fruitful results.
Limitations
NDNQI hospitals electively pay to join the database and are a select sample. Nearly all Magnet facilities participate in NDNQI, and they tend to be larger facilities. NDNQI is underrepresentative of small facilities. Although about half of U.S. hospitals are under 100 beds, only one quarter of NDNQI facilities are of that size. Therefore, the results are not representative of all units in U.S. hospitals. Only critical care, step-down, medical, surgical, medical-surgical combined, and rehabilitation units were included in our study. Results may not be generalizable to other unit types.
Conclusions
Our study is unique in examining time trend (2004–2010) associations between unit level RN national nursing specialty certification rates and total patient fall rates. We found a small, statistically significant relationship that may suggest that increases in RN national nursing specialty certification rates are associated with improvements in total fall rates in acute care settings. Our finding—along with the findings of Kendall-Gallagher and Blegen (2009), Lange et al. (2009), and Boltz et al. (2013)—are encouraging and supportive of promoting RN nursing national specialty certification as a means of improving patient safety.
Figure.
No caption available.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.nursingresearchonline.com).
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 3.0 License, where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially.
The authors acknowledge that funding was provided by the AACN Certification Corporation and American Association of Critical-Care Nurses; American Board of Nursing Specialties; American Board of Certification for Gastroenterology Nurses; American Board of Neuroscience Nursing; American Board for Occupational Health Nurses; American Board of Perianesthesia Nursing Certification; American Organization of Nurse Executives-Credentialing Center; Applied Measurement Professionals; Board of Certification for Emergency Nursing; Canadian Nurses Association Certification Program; Castle Worldwide; Center for Nursing Education and Testing; Citizen Advocacy Center; Competency & Credentialing Institute; Infusion Nurses Certification Corporation; Medical-Surgical Nursing Certification Board; National Alliance of Wound Care Certification Board; National Board for Certification of Hospice and Palliative Nurses; National Board of Certification and Recertification of Nurse Anesthetists; National Board for Certification of School Nurses; National Certification Board for Diabetes Educators; Nephrology Nursing Certification Commission; Oncology Nursing Certification Corporation; Orthopaedic Nurses Certification Board; Pediatric Nursing Certification Board; Professional Examination Service; Rehabilitation Nursing Certification Board; and the Wound, Ostomy, and Continence Nursing Certification Board.
The authors declare no conflicts of interest. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the funders.
REFERENCES
- Agency for Healthcare Research and Quality ( 2013). Preventing falls in hospitals: A toolkit for improving quality of care. Retrieved from www.ahrq.gov/professionals/systems/hospital/fallpxtoolkit/index.html
- American Association of Critical Care Nurses ( 2014a). CCRN exam handbook. Retrieved from www.aacn.org/wd/certifications/docs/ccrn-exam-handbook.pdf
- American Association of Critical Care Nurses ( 2014b). PCCN exam handbook. Retrieved from www.aacn.org/wd/certifications/docs/pccn-exam-handbook.pdf
- American Nurses Credentialing Center ( 2013a). Medical-surgical nursing board certification examination (test content outline). Retrieved from www.nursecredentialing.org/MedSurg-TCO2014
- American Nurses Credentialing Center ( 2013b). Gerontological nursing board certification examination (test content outline). Retrieved from www.nursecredentialing.org/GeroNurse-TCO2015
- Association of Rehabilitation Nurses ( 2014). CRRN examination content outline. Retrieved from www.rehabnurse.org/uploads/files/outline12.pdf
- Boltz M., Capezuti E., Wagner L., Rosenberg M. C., Secic M. ( 2013). Patient safety in medical-surgical units: Can nurse certification make a difference? Medsurg Nursing, 22, 26– 32, 37. [PubMed] [Google Scholar]
- Bouldin E. L., Andresen E. M., Dunton N. E., Simon M., Waters T. M., Liu M., Shorr R. I. ( 2013). Falls among adult patients hospitalized in the United States: Prevalence and trends. Journal of Patient Safety, 9, 13– 17. doi:10.1097/PTS.0b013e3182699b64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle D. K., Cramer E., Potter C., Gatua M. W., Stobinski J. X. ( 2014). The relationship between direct-care RN specialty certification and surgical patient outcomes. AORN Journal, 100, 511– 528. doi:10.1016/j.aorn.2014.04.018 [DOI] [PubMed] [Google Scholar]
- Boyle D. K., Gajewski B. J., Miller P. A. ( 2012). A longitudinal analysis of nursing specialty certification by Magnet® status and patient unit type. The Journal of Nursing Administration, 42, 567– 573. doi:10.1097/NNA.0b013e318274b581 [DOI] [PubMed] [Google Scholar]
- Brand C. A., Sundararajan V. ( 2010). A 10-year cohort study of the burden and risk of in-hospital falls and fractures using routinely collected hospital data. Quality & Safety in Health Care, 19 e51 doi:10.1136/qshc.2009.038273 [DOI] [PubMed] [Google Scholar]
- Cameron I. D., Gillespie L. D., Robertson M. C., Murray G. R., Hill K. D., Cumming R. G., Kerse N. ( 2012). Interventions for preventing falls in older people in care facilities and hospitals. The Cochrane Database of Systematic Reviews, 12, CD005465 doi:10.1002/14651858.CD005465.pub3 [DOI] [PubMed] [Google Scholar]
- Choi J., Boyle D. K., Dunton N. ( 2014). A standardized measure: NDNQI nursing care hours indicator. Western Journal of Nursing Research, 36, 105– 116. doi:10.1177/0193945913501723 [DOI] [PubMed] [Google Scholar]
- Coussement J., De Paepe L., Schwendimann R., Denhaerynch K., Dejaeger E., Milisen K. ( 2008). Interventions for preventing falls in acute- and chronic-care hospitals: A systematic review and meta-analysis. Journal of the American Geriatrics Society, 56, 29– 36. doi:10.1111/j.1532-5415.2007.01508.x [DOI] [PubMed] [Google Scholar]
- Donabedian A. ( 1988). The quality of care: How can it be assessed? JAMA, 260, 1743– 1748. doi:10.1001/jama.1988.03410120089033 [DOI] [PubMed] [Google Scholar]
- Dunton N., Gajewski B., Klaus S., Pierson B. ( 2007). The relationship of nursing workforce characteristics to patient outcomes. OJIN: The Online Journal of Issues in Nursing, 12, 1– 11. doi:10.3912/OJIN.Vol12No03Man0321848348 [Google Scholar]
- Garrard L., Boyle D. K., Simon M., Dunton N., Gajewski B. ( 2014). Reliability and validity of the NDNQI® injury falls measure. Western Journal of Nursing Research Advance online publication. doi:10.1177/0193945914542851 [DOI] [PubMed] [Google Scholar]
- He J., Dunton N., Staggs V. ( 2012). Unit-level time trends in inpatient fall rates of US hospitals. Medical Care, 50, 801– 807. doi:10.1097/MLR.0b013e31825a8b88 [DOI] [PubMed] [Google Scholar]
- Hempel S., Newberry S., Wang Z., Booth M., Shanman R., Johnsen B., Ganz D. A. ( 2013). Hospital fall prevention: A systematic review of implementation, components, adherence, and effectiveness. Journal of the American Geriatrics Society, 61, 483– 494. doi:10.1111/jgs.12169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickey J. V., Unruh L. Y., Newhouse R. P., Koithan M., Johantgen M., Hughes R. G., Lundmark V. A. ( 2014). Credentialing: The need for a national research agenda. Nursing Outlook, 62, 119– 127. doi:10.1016/j.outlook.2013.10.011 [DOI] [PubMed] [Google Scholar]
- Hu L., Bentler P. M. ( 1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1– 55. doi: 10.1080/10705519909540118 [Google Scholar]
- Institute of Medicine ( 1999). To err is human: Building a safer health system. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Institute of Medicine ( 2010). The future of nursing: Leading change, advancing health. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Institute of Medicine ( 2015). Future directions of credentialing research in nursing: Workshop summary. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Kendall-Gallagher D., Blegen M. A. ( 2009). Competence and certification of registered nurses and safety of patients in intensive care units. American Journal of Critical Care, 18, 106– 113. doi:10.4037/ajcc2009487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaus S. F., Dunton N., Gajewski B., Potter C. ( 2013). Reliability of the nursing care hour measure: A descriptive study. International Journal of Nursing Studies, 50, 924– 932. doi:10.1016/j.ijnurstu.2012.07.012 [DOI] [PubMed] [Google Scholar]
- Lake E. T., Shang J., Klaus S., Dunton N. E. ( 2010). Patient falls: Association with hospital Magnet status and nursing unit staffing. Research in Nursing & Health, 33, 413– 425. doi:10.1002/nur.20399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange J., Wallace M., Gerard S., Lovanio K., Fausty N., Rychlewicz S. ( 2009). Effect of an acute care geriatric educational program on fall rates and nurse work satisfaction. Journal of Continuing Education in Nursing, 40, 371– 379. doi:10.3928/00220124-20090723-03 [DOI] [PubMed] [Google Scholar]
- Medical-Surgical Nursing Certification Board ( 2014). Exam blueprint. Retrieved from https://msncb.org/exam-blueprint [Google Scholar]
- Miller P. A., Boyle D. K. ( 2008). Nursing specialty certification: A measure of expertise. Nursing Management, 39, 10– 16. doi:10.1097/01.NUMA.0000338302.02631.5b [DOI] [PubMed] [Google Scholar]
- Muthén L. K., Muthén B. O. ( 1998/2009). Mplus user’s guide (5th ed.). Los Angeles, CA: Author. [Google Scholar]
- National Quality Forum ( 2013). Measure evaluation criteria. Washington, DC: Author; Retrieved from www.qualityforum.org/docs/measure_evaluation_criteria.aspx [Google Scholar]
- Oliver D., Killick S., Even T., Willmott M. ( 2008). Do falls and falls–injuries in hospital indicate negligent care—and how big is the risk? A retrospective analysis of the NHS Litigation Authority Database of clinical negligence claims, resulting from falls in hospitals in England 1995 to 2006. Quality & Safety in Health Care, 17, 431– 436. doi:10.1136/qshc.2007.024703 [DOI] [PubMed] [Google Scholar]
- Simon M., Klaus S., Gajewski B. J., Dunton N. ( 2013). Agreement of fall classifications among staff in U.S. hospitals. Nursing Research, 62, 74– 81. doi:10.1097/NNR.0b013e31827bf8c9 [DOI] [PubMed] [Google Scholar]
- Staggs V. S., Dunton N. ( 2014). Associations between rates of unassisted inpatient falls and levels of registered and non-registered nurse staffing. International Journal of Quality in Health Care, 26, 87– 92. doi:10.1093/intqhc/mzt080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staggs V. S., Mion L. C., Shorr R. I. ( 2014). Assisted and unassisted falls: Different events, different outcomes, different implications for quality of hospital care. Joint Commission Journal on Quality and Patient Safety, 40, 358– 364. doi: 10.1093/intqhc/mzt080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong C. A., Recktenwald A. J., Jones M. L., Waterman B. M., Bollini M. L., Dunagan W. C. ( 2011). The cost of serious fall-related injuries at three Midwestern hospitals. Joint Commission Journal on Quality and Patient Safety, 37, 81– 87. [DOI] [PubMed] [Google Scholar]


