Abstract
Cyclosporine is an immunomodulatory drug used to treat an increasing spectrum of diseases in dogs. Cyclosporine is a calcineurin inhibitor, ultimately exerting its inhibitory effects on T‐lymphocytes by decreasing production of cytokines, such as interleukin‐2. Although, in the United States, oral cyclosporine is approved in dogs only for treatment of atopic dermatitis, there are many other indications for its use. Cyclosporine is available in 2 oral formulations: the original oil‐based formulation and the more commonly used ultramicronized emulsion that facilitates oral absorption. Ultramicronized cyclosporine is available as an approved animal product, and human proprietary and generic preparations are also available. Bioavailability of the different formulations in dogs is likely to vary among the preparations. Cyclosporine is associated with a large number of drug interactions that can also influence blood cyclosporine concentrations. Therapeutic drug monitoring (TDM) can be used to assist in attaining consistent plasma cyclosporine concentrations despite the effects of varying bioavailability and drug interactions. TDM can facilitate therapeutic success by guiding dose adjustments on an individualized basis, and is recommended in cases that do not respond to initial oral dosing, or during treatment of severe, life‐threatening diseases for which a trial‐and‐error approach to dose adjustment is too risky. Pharmacodynamic assays that evaluate individual patient immune responses to cyclosporine can be used to augment information provided by TDM.
Keywords: Cyclosporine, Pharmacodynamics, Pharmacokinetics, Therapeutic drug monitoring
Abbreviations
- CYP
cytochrome P450
- GME
granulomatous meningoencephalitis
- HPLC
high‐pressure liquid chromatography
- IBD
inflammatory bowel disease
- IFN‐γ
interferon‐gamma
- IL‐2
interleukin‐2
- IL‐4
interleukin‐4
- mRNA
messenger ribonucleic acid
- qRT‐PCR
quantitative reverse transcriptase polymerase chain reaction
- RIA
radioimmunoassay
- TDM
therapeutic drug monitoring
Cyclosporine is a potent immunosuppressive drug indicated for the treatment of autoimmune diseases and for organ transplantation. In dogs, cyclosporine is used to treat a spectrum of chronic inflammatory and immune‐mediated diseases. Cyclosporins (up to 9 different molecules, A–I) are cyclic polypeptide macrolides that were originally derived from the soil fungus Tolypocladium inflatum (Beauveria nivea), but are also produced by other fungal organisms. Cyclosporine A is the molecule developed for commercial use as an immunosuppressive agent.1, 2, 3 Discovered by Sandoz Laboratory in 1972, the use of cyclosporine as an immunosuppressive agent was first described in humans to prevent rejection of renal allografts.3, 4 Since that time, cyclosporine has become the cornerstone of immunosuppression for organ transplantation.4, 5 Cyclosporine was approved by the U.S. Food and Drug Administration (FDA) in 1983 for treatment and prevention of transplant rejection in human medicine.6 In veterinary medicine, Novartis Animal Health received FDA approval in 2003 for oral cyclosporine capsules (Atopica) for the treatment of canine atopy. However, by this time cyclosporine had already been used in an extralabel fashion for many years for renal transplantation in dogs and cats,7, 8, 9, 10 and for the treatment of a variety of inflammatory and immune‐mediated conditions.11, 12, 13, 14
Oral Cyclosporine Formulations
Cyclosporine is a large lipophilic molecule, which must be solubilized before intestinal absorption (Fig 1).15 Commercial cyclosporine is available as 2 very different types of oral formulations. Cyclosporine initially was approved for humans as a vegetable‐oil based preparation (Sandimmune), but variability in oral bioavailability caused marked intraindividual and interindividual variations in blood drug concentrations. A more recent formulation, an ultramicronized preparation approved in 1996 (Neoral), forms a microemulsion upon contact with aqueous fluids, resulting in more consistent and predictable absorption.16 Oral bioavailability of the microemulsion is improved by up to 50% compared with the oil‐based preparation.17, 18, 19 Because of the marked variability in bioavailability of the nonultramicronized Sandimmune preparation, it is not recommended for oral use in dogs. Only the veterinary version of the Neoral microemulsion preparation, Atopica, is approved for use in dogs and cats in the United States. Veterinarians continue to prescribe generic ultramicronized products for human use despite, in many countries, the availability of veterinary versions of the drug. However, only limited evidence exists that generic products for human use will be equally bioavailable in dogs, either as compared with one another, or with Atopica.
Figure 1.
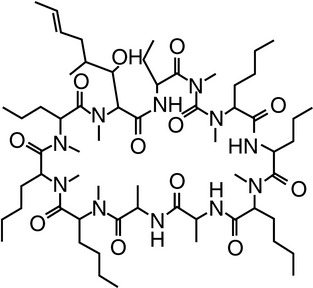
Chemical structure of cyclosporine.
Mechanism of Action
Cyclosporine's primary immunosuppressive mechanism of action is inhibition of T‐lymphocyte function. Antigen binding to CD3 receptors on the surface of T‐lymphocytes causes increased intracellular calcium and activation of calcineurin. Calcineurin is an intracellular protein phosphatase that activates gene transcription factors by dephosphorylation. Cyclosporine acts to inhibit calcineurin. Calcineurin inhibitors, including cyclosporine, act by binding to intracellular cyclophilins, which are proteins that facilitate protein folding. Cyclophilin A is the predominant cyclophilin found in T‐lymphocytes. Binding of cyclosporine to cyclophilin A creates a complex with high affinity for calcineurin. Activation of T‐lymphocytes results in activated calcineurin, which dephosphorylates inactive nuclear factor (NFAT). NFAT translocates into the nucleus, where it upregulates transcription of genes coding for several important cytokines. These include interleukin‐2 (IL‐2), interleukin‐4 (IL‐4), TNF‐α, and INF‐γ.6, 20, 21 Production of IL‐2, in particular, plays a key role in the activation and proliferation of T‐lymphocytes. By inhibition of calcineurin, cyclosporine specifically inhibits T‐cell function, and thus cell‐mediated immunity, but has little immediate impact on humoral immunity.22, 23, 24 Decreased IL‐2 expression in CD4+ Th1 cells associated with cyclosporine treatment leads to inhibition of proliferation and activation of both T‐helper and T‐cytotoxic lymphocytes, and blunting of the immune response (Fig 2).
Figure 2.
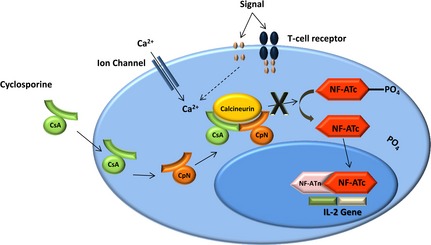
Cyclosporine mechanism of action.
Disposition of Cyclosporine
Absorption
After oral administration, cyclosporine is absorbed across the epithelium of the small intestine. Variability in the absorption of the oil‐based preparation is associated with variations in bile flow and gastrointestinal motility.25 The improved predictability of absorption of the microemulsion reflects its independence from these factors, although oral bioavailability still may vary from 23 to 45%.25, 26, 27
In dogs, food may impact the oral absorption of ultramicronized cyclosporine. A decrease in bioavailability and increase in pharmacokinetic variability were documented when ultramicronized cyclosporine was administered with food, leading to recommendations that the drug be administered 2 hours before or after feeding.27, 28 A later study in atopic dogs, however, did not demonstrate any impact of food on the clinical efficacy of ultramicronized cyclosporine.29
Cyclosporine is among the many drugs that are substrates for P‐glycoprotein, an efflux transporter pump located at portals of entry and sanctuaries. In intestinal epithelium, P‐glycoprotein is located in the brush border of the enterocytes, where it pumps a wide variety of xenobiotics out of the cell and back into the lumen. In people, intestinal P‐glycoprotein activity has been shown to influence intestinal absorption and metabolism of cyclosporine.30 A study in 3 normal and 3 P‐glycoprotein‐deficient dogs, in contrast, failed to identify a significant difference in cyclosporine pharmacokinetics when cyclosporine was administered both PO and IV. 31
In another study, cimetidine, an H2‐receptor antagonist, given concurrently with oral ultramicronized cyclosporine, caused a significant increase in time until maximal blood cyclosporine concentrations, an effect that may reflect either increased drug absorption or decreased clearance because of inhibition of cyclosporine metabolism.32 The overall maximum blood concentration of cyclosporine did not increase in dogs on cimetidine, suggesting that the reason was because of increased absorption.
Distribution
Cyclosporine has a high binding affinity for red blood cells and plasma lipoproteins.1 Because up to 50% of the drug in blood is located in red cells, whole blood is recommended for therapeutic drug monitoring (TDM). Once in the circulation, cyclosporine distributes widely, accumulating in the skin, liver, kidneys, and fat of dogs, resulting in a large volume of distribution.25 Tissue concentrations exceed concentrations in serum by a factor of 3 to 14.25 Variability in the volume of distribution contributes to variability in magnitude and time to peak blood concentration (C max) in dogs, with peak concentrations generally occurring approximately 2 hours after oral administration of ultramicronized cyclosporine.11, 28 Blood concentrations then rapidly decrease over the remainder of the dosing interval, reflecting a relatively rapid half‐life as the drug is cleared from plasma.
Metabolism
Extensive metabolism of cyclosporine by phase I microsomal (cytochrome P450 or CYP) enzymes mediates hydroxylation, N‐demethylation, or both, yielding many different metabolites.1, 33 Metabolism occurs in the liver, small intestine, and kidneys, with the liver being the major site of metabolism. The major cyclosporine metabolites produced by the liver in dogs include a 9 γ‐hydroxylated metabolite, a 4 N‐desmethylated metabolite, a 1‐β‐(8΄) hydroxylated metabolite, and a 1‐β‐1‐ε‐cyclized metabolite.33 In dogs, hepatic metabolism is extensive and occurs quickly, with 70 to 100% of the drug being metabolized within 30 minutes.25, 33, 34 In the liver, cytochrome P‐450 3A provides the key metabolic pathway. Metabolism in the small intestine is more variable and slower.33 Variation in the CYP 3A4 activity influences cyclosporine clearance in humans.
A number of drug interactions impacting cyclosporine involve the hepatic P‐450 enzyme system. Examples of drugs for human use and use in veterinary medicine that inhibit CYP450 3A4, leading to increased cyclosporine blood concentrations, as well as drugs known to decrease concentrations of cyclosporine by either induction of the enzymes involved in cyclosporine metabolism or increased excretion of cyclosporine, are listed in Table 1.
Table 1.
Drug interactions with cyclosporine
| Drugs that may increase cyclosporine concentrations | |
| Acetazolamide | Flavonoids in grapefruit juice |
| Allopurinol | Fluconazole |
| Amiodarone | Fluoxetine |
| Azithromycin | Ketoconazole |
| Bromocriptine | Imapenem |
| Calcium channel blockers | Itraconazole |
| Carvedilol | Macrolide antibiotics (Erythromycin, clarithromycin) |
| Chloramphenicol | Methotrexate |
| Cimetidine | Metoclopramide |
| Ciprofloxacin/Enrofloxacin | Metronidazole |
| Cisapride | Omeprazole |
| Colchicine | Sertraline |
| Danazol | Tacrolimus |
| Digoxin | Tinidazole |
| Estrogens | |
| Drugs that may decrease blood concentrations of cyclosporine | |
| Azathioprine | Phenobarbital |
| Carbamazepine | Phenytoin |
| Clindamycin | Rifampin |
| Cyclosphosphamide | Sulfadiazine |
| Famotidine | Terbinafine |
| Nafcillin | Trimethoprim |
| Octreotide | |
| Drugs that may increase or decrease blood concentrations of cyclosporine | |
| Glucocorticoids | |
In dogs, several drugs have been given concurrently with cyclosporine to decrease the dosage needed to maintain adequate blood concentrations of cyclosporine. Two classes of drugs have been studied for this effect: the imidazole antifungal drugs ketoconazole and fluconazole, and H‐2 receptor‐blocking antihistaminergic drugs, such as cimetidine. 35 Of these, ketoconazole has received the most attention. Ketoconazole enables a decrease in oral cyclosporine dosages in dogs by as much as 75%, although individual responses are variable.36 Fluconazole also has been shown to enable reduction of oral cyclosporine dosages by between 30 and 50%.37, 38 Cimetidine is an inhibitor of several CYP enzymes and also is a substrate for P‐glycoprotein. Cimetidine significantly decreases cyclosporine clearance and prolongs elimination half‐life in rabbits,39 although similar effects could not be documented in rats, dogs, or humans.32, 40, 41 Interestingly, high‐dose powdered whole grapefruit has been shown to increase blood cyclosporine concentrations in dogs, possibly because grapefruit furanocoumarins inhibit intestinal P‐450 3A microsomal enzymes, thus increasing oral bioavailability.42
In addition to drug interactions, disease also may influence cyclosporine metabolism in dogs. Experimentally induced diabetes and pancreatectomy, for example, both increase cyclosporine clearance, whereas partial hepatectomy decreases drug clearance.43, 44, 45
Excretion
Most cyclosporine metabolites are excreted predominantly through the biliary system, with minimal renal excretion.1, 26, 46
Cyclosporine Generic Preparations
According to the FDA Orange Book (http://www.accessdata.fda.gov/scripts/cder/ob/default.cfm), over 20 generic cyclosporine preparations have been approved for use in humans in the United States. For FDA generic drug approval, generic drugs must demonstrate bioequivalence, with 90% confidence intervals for pivotal exposure parameters (area under the plasma drug concentration time curve [AUC] and maximum concentration in the dosing interval) falling within the range of 80–125% of the brand name (reference) product, which, for microemulsified cyclosporine, is Neoral.47 Instead of the equivalence code “A” typically granted to equivalent generic formulations, cyclosporine generic formulations are designated by the FDA as having a therapeutic equivalence code of “AB” (http://www.fda.gov/Drugs/DevelopmentApprovalProcess/ucm079068.htm#TherapeuticEquivalence-Related Terms), indicating that issues regarding bioequivalency to the reference compound existed, but sufficient evidence was presented to resolve these concerns, such that approval occurred as a “therapeutically equivalent” formulation in humans. Testing with generic preparations of cyclosporine has occurred primarily with young healthy human individuals.47 With a lack of comparative data relating pharmacokinetic parameters between the Neoral formulation and generic ultramicronized formulations in diseased patients requiring immunosuppressive treatment, recommendations to physicians are to use generic formulations of cyclosporine only in low‐risk human patients when additional testing can be performed to ensure attainment of desired blood concentrations.47 One study evaluating the pharmacokinetics of both Neoral and generic ultramicronized cyclosporine in human renal transplant recipients demonstrated that absorption of generic cyclosporine was significantly less than Neoral.48
No generic cyclosporine preparations have been approved for use in veterinary medicine. However, by virtue of the Animal Medicinal Drug Use Clarification Act (1984),1 US veterinarians are legally empowered to use any drug approved for use in any species in an extralabel fashion. The exception to this rule occurs, however, if an approved product exists for use in the species of interest. Accordingly, this calls into question the legitimacy of US veterinarians prescribing human generic cyclosporine solely because such preparations are less expensive. Concerns regarding the use of generic cyclosporine are justified in that, although therapeutic equivalence has been demonstrated in people, data from humans do not apply to dogs. Indeed, in the authors' experience, oral bioavailability of generic preparations for human use may vary by 3‐fold or more in dogs, depending on the manufacturer. Because pharmacies may change generic preparations, monitoring potentially should be implemented with each new prescription.
In addition to generic preparations, cyclosporine often is prescribed as a compounded preparation. Extreme caution is recommended with this approach. Marked variability in product quality and concentration has been demonstrated among cyclosporine preparations compounded for animals. Accordingly, prescription of compounded products is strongly discouraged, unless the needs of the patient simply cannot be met with current approved formulations.
Pharmacokinetics
Many investigators have reported the pharmacokinetics of cyclosporine in dogs (Table 2).11, 28, 31, 32, 38, 42, 43, 49, 50, 51, 52, 53, 54, 55, 56, 57 However, comparison among studies is difficult because of differences in dosage, routes of administration, preparations used, assays of quantitation, and other factors, such as fed versus fasting state. Some crucial points, however, can be obtained from evaluating these studies. The time to maximum drug concentrations after oral administration, regardless of the preparation, occurs within 1–2 hours, suggesting that 2 hours after administration is a reasonable time for monitoring peak drug concentration. Elimination half‐life is reported to be highly variable. For studies using oral cyclosporine, however, the terminal component of the drug concentration versus time curve may not necessarily reflect elimination, but may reflect prolonged absorption. Only studies using intravenous cyclosporine therefore can be used to confirm the duration of the elimination half‐life. Because formation of metabolites can impact the terminal curve, studies that include only the parent compound, such as high‐pressure liquid chromatography (HPLC) assays, are most informative. Based on these considerations, the elimination half‐life of cyclosporine in dogs appears to range from 7 to 10 hours. Use of assays that measure more than just the parent compound can markedly affect results. For example, in 1 study using fluorescence polarization immunoassay analysis, cyclosporine half‐life in plasma was recorded as 1.9 hours.52 Variability in half‐life has been reported in other studies, being >22 hours in several studies (after intravenous dosing in 1 study,43 and oral dosing in another50). In the Auburn TDM laboratory, cyclosporine elimination half‐life in dogs is markedly variable, ranging from 1 to 2 hours to over 150 hours, with longer half‐lives most commonly seen in patients receiving drugs known to prolong cyclosporine elimination.
Table 2.
Pharmacokinetic parameters of cyclosporine
| Species (n) | Dosage (mg/kg) | Route | Preparation | Sample | Method | CsA (ng/mL) | Parameter | T max (hour) | Half‐life (hour) | Duration | Status | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Collie dog (3) | 1 | IV | NS | Plasma | HPLC | 2,723 ± 229 | AUC (inf) | NS | 9.6 ± 3.2 | Single | ABCB1‐1Δ | Mealey et al31 |
| Collie dog (2) | 1 | IV | NS | Plasma | HPLC | 2,635 (1,980–3,290) | AUC (inf) | NS | 7.2 (6.9–7.5) | Single | ABCB1‐WT | |
| Beagle (5) | 5 | IV | NS | WB | FPIA | 3,721 ± 639 | C 0 | NS | 9.3 ± 2.3 | Single | DM | Alkharfy43 |
| 12,110 ± 1,882 | AUC (inf) | |||||||||||
| Beagle (5) | 5 | IV | NS | WB | FPIA | 3,681 ± 662 | C 0 | NS | 22.6 ± 2.3 | Single | H, N | |
| 25,181 ± 1,514 | AUC (inf) | |||||||||||
| Beagle (4) | 5 | PO | Neoral | WB | HPLC | 1,188 ± 349 | Peak | NS | NS | Single | H, N | Fukunaga and Orito49 |
| 3,829 ± 642 | AUC (inf) | |||||||||||
| Dog (8) | 5 | PO | Atopica | WB | HPLC‐MS‐MS | 1,075 ± 105 | Peak | 1.75 ± 0.12 | 12.2 ± 1.4 | Single | H, N | Radwanski et al42 |
| 6,700 ± 483 | AUC (inf) | |||||||||||
| Beagle (6) | 10–12.5 (100 mg) | PO | Neoral | WB | RP‐HPLC | 970 ± 176 | Peak | 1.8 ± 0.75 | 22.3 ± 10.5 | Single | H, N | Lai50 |
| 5,462 ± 991 | AUC (inf) | |||||||||||
| Collie dog (3) | 4 | PO (gavage) | NS | Plasma | HPLC | 992 ± 551 | Peak | 1.3 ± 0.29 | NS | Single | ABCB1‐1Δ | Mealey et al31 |
| 4,787 ± 1,359 | AUC (inf) | |||||||||||
| Collie dog (2) | 4 | PO (gavage) | NS | Plasma | HPLC | 895 (699–1,090) | Peak | 1.3 | NS | Single | ABCB1‐WT | |
| 4,420 (2,520–6,330) | AUC (inf) | (1.0–1.5) | ||||||||||
| Beagle (6) | 6.7–8.3 (100 mg) | PO | Neoral | WB | RIA | 1,241 ± 69 | Peak | 1.3 ± 0.4 | 7.2 ± 0.7 | Single | H, N | Yang57 |
| 8,683 ± 1,046 | AUC (inf) | |||||||||||
| Beagle (4) | 25 mg | PO | Neoral | WB | HPLC | 331 ± 57 | Peak | 0.88 ± 0.25 | NS | Single | H, N | Sander and Holm51 |
| 1,269 ± 256 | AUC (inf) | |||||||||||
| Beagle (4) | 10 | PO | Atopica | WB | FPIA | 1,437 ± 246 | Peak | 1.75 ± 0.5 | 5.4 ± 0.47 | Single | H, N | Katayama et al38 |
| 6,784 ± 246 | AUC (0–12) | |||||||||||
| Dog (8) | 5 | PO | Atopica | WB | FPIA | 699 ± 326 | Peak | 1.5 ± 0.5 | 5.6 ± 1.2 | Single | IBD, Severe | Allenspach et al11 |
| 34 ± 26 | C min (24 hours trough) | |||||||||||
| 4,770 ± 2,672 | AUC (0–24) | |||||||||||
| Dog (16) | 5 | PO | Atopica | WB | FPIA | 878 ± 131 | Peak | 1.6 ± 0.4 | 7.8 ± 1.1 | Single | H, N | |
| 50 ± 22 | C min (24 hours trough) | |||||||||||
| 6,729 ± 1,578 | AUC (0–24) | |||||||||||
| Dog (3) | 15 | PO | Neoral solution | Plasma | FPIA | 1,118 ± 124 | Peak | 1.5 | 1.94 ± 0.2 | Single | H, N | Amatori et al52 |
| 7,465 ± 926 | AUC (inf) | |||||||||||
| Beagle (8) | 5 | PO, FST capsule | Microemulsion | WB | FPIA | 1,059 ± 207 | Peak | 1.3 ± 0.5 | NS | Single | H, N | Steffan et al28 |
| 6,386 ± 2,079 | AUC (0–24) | |||||||||||
| PO, Fed capsule | Microemulsion | WB | FPIA | 845 ± 582 | Peak | 1.36 ± 2.9 | NS | Single | H, N | |||
| 5,453 ± 1,905 | AUC (0–24) | |||||||||||
| PO, FST solution | Microemulsion | WB | FPIA | 1,287 ± 180 | Peak | 1 | NS | Single | H, N | |||
| 7,533 ± 1,712 | AUC (0–24) | |||||||||||
| PO, Fed solution | Microemulsion | WB | FPIA | 949 ± 725 | Peak | 0.65 ± 0.26 | NS | Single | H, N | |||
| 5,396 ± 2,615 | AUC (0–24) | |||||||||||
| Beagle (20) | 5 | PO, FST capsule | Atopica | WB | HPLC | 577 ± 128 | Peak | 1.4 ± 0.3 | 9.4 ± 1.2 | Single | H, N | |
| 34 ± 12 | C min (24 hours predicted) | |||||||||||
| 3,997 ± 1,108 | AUC (inf) | |||||||||||
| Beagle (16) | 5 | PO, FST capsule | Atopica | WB | FPIA | 878 ± 131 | Peak | 1.6 ± 0.4 | 7.8 ± 1.1 | Single | H, N | |
| 50 ± 22 | C min (24 hours predicted) | |||||||||||
| 6,729 ± 1,587 | AUC (inf) | |||||||||||
| Beagle (6) | 6.7–8.3 (100 mg) | PO | Neoral solution | Plasma | RP‐HPLC | 1,707 ± 72 | Peak | 2.5 ± 0.55 | 6.82 ± 0.12 | Single | H, N | El‐Shabouri53 |
| 23,091 ± 1,204 | AUC (inf) | |||||||||||
| Dog (4) | 10 | PO | Sandimmune solution | WB | HPLC | 772 ± 71 | Peak | 1.25 ± 0.5 | NS | Single | H, N | Fischer et al54 |
| 4,250 ± 753 | AUC (inf) | |||||||||||
| Dog (4) | 10 | PO | Neoral solution | WB | HPLC | 977 ± 135 | Peak | 1.75 ± 0.5 | NS | Single | H, N | |
| 7,078 ± 1,777 | AUC (inf) | |||||||||||
| Beagle (10) | 5 | PO q24h | Neoral | WB | FPIA | 1,088 ± 167 | Peak | 1.3 ± 0.36 | NS | 3 doses | H, N | Daigle et al32 |
| Beagle (10) | 6.3–9.1 (100 mg) | PO | Neoral solution | WB | RIA | 1,689 (26% rel SD) | Peak | 1.9 | NS | Single | H, N | Ford et al55 |
| 12,790 (16% rel SD) | AUC (inf) | (37% rel SD) | ||||||||||
| German Shepherd (6) | 7.5 q12h | PO | Neoral | WB | EMIT | 578 ± 459 | Trough | NS | NS | 7 days | Anal Furunculosis | Griffiths et al56 |
| (205–1,370) |
AUC (ng*h/mL), area under the curve; C 0, initial blood drug concentration; C min, minimum concentration after dosing; HPLC, high‐performance (pressure) liquid chromatography; RP‐HPLC, reverse‐phase high‐performance (pressure) liquid chromatography ; HPLC‐MS‐MS, high‐performance (pressure) liquid chromatography tandem mass spectrometry; FPIA, fluorescence polarization immunoassay; EMIT, enzyme multiplied immunoassay technique; RIA, radioimmunoassay; rel SD, relative standard deviation; inf, infiniti; WB, whole blood; FST, fasted; H, N, healthy, normal; AD, atopic dermatitis; DM, diabetes mellitus; IBD, inflammatory bowel disease; ABCB1‐1Δ, P‐glycoprotein‐deficient dogs; ABCB1‐WT, normal P‐glycoprotein dogs; NS, not specified.
Variability in cyclosporine half‐life has therapeutic implications. The time to steady state, and thus time to evaluate therapeutic response, ranges from negligible (that is, no steady state exists) to over 18–25 days. Variability in half‐life also impacts the timing of sample collection, and may impact therapeutic response. With a half‐life of <2 hours, >90% of each dose is eliminated during a dosing interval, and concentrations will vary markedly with the timing of sample collection. In fact, trough concentrations are likely to be nondetectable. In contrast, when cyclosporine half‐life exceeds 12 hours, at least 50% of each dose will be retained, the drug will accumulate until steady‐state is reached, and less fluctuation will occur over a dosing interval. Because the drug may accumulate in some patients, peak blood concentrations also may vary. Other factors, however, also impact peak cyclosporine concentrations. Typically, peak blood concentrations are between 600 and 1,200 ng/mL after a standard 5 mg/kg microemulsified oral dose. Trough concentrations are less commonly reported, but 1 study in dogs with anal furunculosis reported a trough concentration range of 205–1,370 ng/mL after 1 week of cyclosporine treatment (Neoral) at a dosage of 7.5 mg/kg every 12 hours.56 Concentrations are highly susceptible to individual variability, and pharmacokinetic results should be interpreted in the context of the sample submitted (plasma or whole blood), assay used, and clinical response of the patient. Variability in the dose‐blood concentration relationship can be seen in Table 2. When C max or AUC are adjusted for dosage among the studies, the mean ± standard deviation of C max/dose is 179 ± 56 versus 863 ± 768 AUC/dose. The greater variability of the latter is likely to reflect variability in clearance as well as parameters that influence C max.
Adverse Effects
Although many adverse effects are associated with cyclosporine treatment in dogs, most are uncommon, with the exception of adverse gastrointestinal effects. In 1 large placebo‐controlled field study safety analysis58 in which dogs were given either placebo or ultramicronized cyclosporine at a mean dosage of 5 mg/kg/day (the approved atopy dosage), the most commonly observed adverse effects in the cyclosporine group were vomiting (31%), diarrhea (20%), persistent otitis externa (7%), urinary tract infections (4%), anorexia (3%), lethargy (2%), gingival hyperplasia (2%), and lymphadenopathy (2%), and the most common serum chemistry changes included increased serum creatinine concentration (8%), hyperglobulinemia (6%), hyperphosphatemia (5%), hyperproteinemia (3%), hypercholesterolemia (3%), hypoalbuminemia (2%), hypocalcemia (2%), and increased blood urea nitrogen concentration (2%), although only changes in creatinine, cholesterol, calcium, and blood urea nitrogen were statistically significant compared with baseline concentrations.
In other published studies, the most notable adverse effects of cyclosporine in dogs were gastrointestinal in nature, including diarrhea, vomiting, and anorexia.59 Adverse gastrointestinal effects occur across a range of dosages, with increased frequency of occurrence seen at higher dosages. Less commonly reported dermatologic adverse effects include hirsutism, coat shedding, gingival hyperplasia, gingival eruption cysts in neonatal dogs, cutaneous papillomatosis, hyperkeratosis of footpads, psoriasiform‐lichenoid–like dermatitis, hyperplastic verrucous lesions, and lymphoplasmatoid dermatitis.60, 61, 62 Clinicopathologic abnormalities seen in conjunction with cyclosporine treatment that were not reported in the previous safety analyses include lymphopenia, eosinopenia, anemia, and leukocytosis.59 Adverse effects common to most other immunosuppressive agents, but not reported with cyclosporine, include myelosuppression and neutropenia. Concurrent infections documented in patients receiving cyclosporine treatment include bacterial infections of the respiratory and urinary tracts, pyelonephritis, pyometra, purulent pericarditis, septic arthritis, toxoplasmosis, neosporosis, demodicosis, and pyoderma.63, 64, 65 Malignancies, including lymphoma, have occurred in conjunction with concurrent use of cyclosporine.26, 66 Other potential adverse reactions uncommonly reported in the literature include hepatotoxicity, defective hepatic protein synthesis, inhibition of insulin release, increase in insulin resistance, overt diabetes mellitus, lameness, lethargy, nephropathy, transient hypoalbuminemia, anaphylactic reaction, angioedema, tremors, emergence of neoplasia, and cystic nodules in the pericardium and diaphragm.16, 66, 67, 68, 69
At the FDA Center for Veterinary Medicine Adverse Event Reporting site (http://www.fda.gov/downloads/AnimalVeterinary/SafetyHealth/ProductSafetyInformation/UCM055404.pdf), the most common adverse events reported in dogs are vomiting (3,108), diarrhea (1,369), lethargy (1,142), anorexia (834), pruritus (790), and increased serum alkaline phosphatase (429) or alanine aminotransferase (311) activities. Gingival hyperplasia was reported in 260 animals (accessed May 2013). The FDA database provides no information regarding number of doses sold, nor does the collection of the information verify a cause‐effect relationship between dose and adverse event.
Precautions
The safety and efficacy of cyclosporine have not been evaluated in dogs <6 months of age or in dogs <4 pounds in weight, and the drug should therefore either not be used or be used cautiously in such patients. Cyclosporine is not for use in breeding, pregnant, or lactating dogs. Renal damage is a relatively common adverse effect in people during cyclosporine treatment. Nephrotoxicity has not been reported in dogs receiving therapeutic dosages of cyclosporine, but experimentally has been associated with very high blood drug concentrations (>3,000 ng/mL) over prolonged periods.16
Because of the dampening of the immune system associated with cyclosporine treatment, vaccine efficacy potentially may be impacted.70 Vaccine approval studies have documented adequate antibody titer responses in dogs receiving a killed rabies vaccine despite administration of 4 times the recommended cyclosporine atopy dosage. Although peer‐reviewed published research studies have documented vaccine efficacy in humans receiving cyclosporine,71, 72 no such studies are available in dogs, and clear recommendations therefore are not available. Some authors discourage the use of modified live vaccines in dogs receiving cyclosporine for fear of potential reactivation of the pathogen,70 and only killed vaccines are recommended by the drug manufacturer.
Therapeutic Drug Monitoring
Assays
The established complexities of cyclosporine disposition in normal animals, coupled with confounding factors associated with disease and differences in drug preparation, may contribute to markedly variable blood concentrations of cyclosporine both among patients and even within the same patient. Therapeutic management therefore may be facilitated by monitoring blood cyclosporine concentrations. Although traditionally considered a method for avoiding drug toxicity, TDM offers advantages beyond simple avoidance of toxic concentrations. TDM typically is considered to be most effective if a therapeutic range is available that describes a relationship between blood drug concentration and clinical response, but TDM can be equally effective in establishing the therapeutic range for an individual patient. Once a therapeutic range is established for a given patient, subsequent monitoring is designed to maintain blood drug concentrations within that range.15
Recommendations regarding target immunomodulatory blood concentrations for cyclosporine originally were based on experimental organ transplantation in dogs.10, 73 Initial recommendations centered on achieving a minimum target trough whole blood cyclosporine concentration of 500–600 ng/mL using a monoclonal radioimmunoassay (RIA), with blood collected just before the next oral dose.8, 16 Unfortunately, however, the process of adjusting drug doses based on monitoring cyclosporine blood concentrations is clinically complex, and not necessarily associated with the desired clinical outcome (Table 3).11, 12, 13, 14, 24, 29, 56, 58, 59, 63, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83
Table 3.
Studies in dogs in which efficacy was established for select diseases
| Investigation | Disease Investigated | Number of Dogs | Cyclosporine Preparation | Cyclosporine Dosage | Cyclosporine Concentrations | Method of Measurement | Treatment Duration | Efficacy | Reference |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Atopy | 130 (Phase 1) | Atopica | 5 mg/kg q24h | N/A | N/A | 4 weeks | 45% had a reduction in CADESI score by >50% of baseline | Steffan et al58 |
| 186 (Phase 2) | 16 weeks | 68% had a reduction in CADESI score by >50% of baseline | |||||||
| 2 | Atopy | 117 | Atopica | 5 mg/kg q24h | N/A | N/A | 4 months | 76% responded with excellent or good response to treatment | Steffan et al74 |
| 3 | Atopy | 30 | Neoral | 2.5 mg/kg q24h | N/A | N/A | 6 weeks | 47% had a reduction in CADESI score by >50% of baseline | Olivry et al59 |
| 31 | 5 mg/kg q24h | 6 weeks | 71% had a reduction in CADESI score by >50% of baseline | ||||||
| 4 | Atopy | 14 | Neoral | 5 mg/kg q24h | N/A | N/A | 2 weeks | 93% had a marked reduction in total clinical score as compared with baseline | Fontaine and Olivry75 |
| 5 | Atopy | 15 | Neoral | 5 mg/kg q24h | N/A | N/A | 6 weeks | 69% had a reduction in CADESI score by >50% of baseline | Olivry et al59 |
| 6 | Atopy | 51 | Neoral | 5 mg/kg q24h | N/A | N/A | 6–30 months' follow‐up | 78% obtained well‐controlled clinical signs | Radowicz and Power63 |
| 7 | Atopy | 25 | Atopica | 5 mg/kg q24h | N/A | N/A | 6 months | 100% had a reduction in CADESI score of at least by >50% of baseline | Thelen et al29 |
| 8 | Canine Pemphigus foliaceus | 5 | Neoral | 5–10 mg/kg q24h | N/A | N/A | 3 months | 0% had a significant improvement in clinical signs | Olivry et al12 |
| 9 | Sebaceous adenitis | 12 | Neoral | 5 mg/kg q24h | N/A | N/A | 12 months | 83% demonstrated a significant reduction in clinical scores | Linek et al77 |
| 10 | Perianal fistula | 10 | Sandimmune | 7.5–10 mg/kg q12h | Adjusted to maintain trough of 400–600 ng/mL | Monoclonal RIA | 20 weeks | 100% of dogs showed resolution of fistulas | Mathews and Sukhiani13 |
| 11 | Perianal fistula | 10 | Sandimmune | 5 mg/kg q12h | Adjusted to maintain trough of 400–600 ng/mL | Monoclonal RIA | 16 weeks | 100% of dogs showed complete resolution of fistulas or substantial reduction in size | Mathews and Sukhiani13 |
| 12 | Perianal fistula | 6 | Neoral | 7.5 mg/kg q12h |
Adjusted to maintain trough of 400–600 ng/mL Initial trough ranged from 205 to 1,370 ng/mL after 7 days |
Emit assay | 10–20 weeks | 100% of dogs demonstrated marked improvement | Griffiths et al56 |
| 13 | Perianal fistula | 16 | Neoral | Cyclosporine 1 mg/kg q12h plus ketoconazole (10 mg/kg q24h) | Adjusted to maintain trough >200 ng/mL | HPLC | 16 weeks | 100% of dogs showed marked improvement of lesions within 14 days of treatment | Mouatt78 |
| 14 | Perianal fistula | 12 | Neoral | Cyclosporine 2.5 mg/kg q12h or 4 mg/kg q24h plus ketoconazole (8 mg/kg q24h) |
Adjusted to maintain trough of 400–600 ng/mL Initial trough ranged from 130 to 1,398 ng/mL after 5 days |
HPLC | 4–39 weeks | 100% of dogs showed resolution of clinical signs by 9 weeks of treatment | Patricelli et al24 |
| 15 | Perianal fistula | 3 | Neoral | Cyclosporine (0.5 mg/kg q12h) + Ketoconazole (7.5 mg/kg q12h) | Adjusted to maintain trough of 400–600 ng/mL | RIA | 3–10 weeks | 100% of visible lesions completely resolved | O'Neill et al79 |
| 6 | Cyclosporine (0.75 mg/kg q12h) + Ketoconazole (7.5 mg/kg q12h) | ||||||||
| 6 | Cyclosporine (1 mg/kg q12h) + Ketoconazole (7.5 mg/kg q12h) | ||||||||
| 4 | Cyclosporine (2 mg/kg q12h) + Ketoconazole (7.5 mg/kg q12h) | ||||||||
| 16 | Perianal fistula | 10 | Neoral | 2 mg/kg q24h | Mean trough after 4 weeks 39 ng/mL (25–77) | RIA | 8 weeks | 10% of dogs experienced resolution of external lesions | House et al80 |
| 10 | 5 mg/kg q24h | Mean trough after 4 weeks 122 ng/mL (47‐237) | 60% of dogs experienced resolution of external lesions | ||||||
| 17 | Perianal fistula | 26 | Neoral | 4 mg/kg q12h | N/A | N/A | 4–24 weeks | 96% of dogs experienced complete resolution or improvement | Hardie et al81 |
| 18 | Perianal fistula | 6 | Neoral | Cyclosporine (1.5 mg/kg q24h) | Concentrations iin all dogs ranged from 0 to 330 ng/mL | Emit assay | 13 weeks | 50% demonstrated improvement with resolution of CS | Doust et al82 |
| 6 | Cyclosporine (3 mg/kg q24h) | 66% demonstrated improvement with resolution of CS | |||||||
| 6 | Cyclosporine (5 mg/kg q24h) | 66% demonstrated improvement with resolution of CS | |||||||
| 6 | Cyclosporine (7.5 mg/kg q24h) | 100% demonstrated improvement with resolution of CS | |||||||
| 19 | Granulomatous Meningoencephalitis | 3 | Atopica | Initial cyclosporine dosage of 10 mg/kg q24h | N/A | N/A | 6 weeks | Complete resolution of clinical signs in all 3 dogs | Gnirs14 |
| 20 | Granulomatous Meningoencephalitis | 3 | Not revealed in the study | Initial cyclosporine dosage of 3 mg/kg q12h, adjusted upward in all dogs | Dog 1 at 6 mg/kg q12h dosage: trough of 235 ng/mL | N/A | Up to 12 months | Considered effective in 2 of 3 dogs | Adamo and O'Brien83 |
| Dog 2 at 3 mg/kg q12h dosage: trough f 82 ng/mL | |||||||||
| Dog 3 at 3 mg/kg q12h dosage: otrough of 117 ng/mL | |||||||||
| 21 | Inflammatory Bowel Disease | 14 | Atopica | 5 mg/kg q24h | Mean trough concentration 34 ± 26 ng/mL | FPIA | 10 weeks | 79% demonstrated a significant reduction in clinical score | Allenspach et al11 |
| Mean peak concentration 699 ± 326 ng/mL |
CADESI, canine atopic dermatitis extent and severity index; RIA, radioimmunoassay; HPLC, high‐performance (pressure) liquid chromatography; CS, clinical signs; FPIA, flourescence polarized immunoassay.
The method used to measure cyclosporine blood concentrations must be considered when interpreting results. Past methods for measuring cyclosporine blood concentrations included HPLC and assays dependent on antibodies to the drug, including fluorescence polarization immunoassay and antibody (both monoclonal and polyclonal) RIA methods. Currently available methods include HPLC as well as a specific monoclonal RIA. HPLC has the advantage that the parent drug can be discriminated from metabolites, although most methods detect only the parent compound. RIA, in contrast, measures metabolites as well as the parent drug, and blood cyclosporine concentrations therefore will be higher by a factor of 1.5–1.7 compared to the same sample analyzed using HPLC.28 Although HPLC is considered the gold standard for measuring cyclosporine blood concentrations, HPLC is labor‐intensive and not routinely offered for patient monitoring. Furthermore, with HPLC, the method of separating, detecting, and quantitating the drug (ie, mass spectrophotometry versus other methods) can influence concentrations. Fluorescence polarization immunoassay and RIA have been the methods most often employed in clinical situations, with the laboratory performing the assay typically providing recommendations regarding ideal target blood drug concentrations. Some laboratories have adjusted target blood concentrations upward to reflect the fact that fluorescence polarization immunoassay and RIA results will be approximately double HPLC assay results. Other laboratories have not made this adjustment, with the rationale that the cyclosporine metabolites measured by the fluorescence polarization immunoassay and RIA assays may arguably be pharmacologically active and contribute to the overall immunosuppressive effects. However, if the goal of monitoring is to establish the individual patient's therapeutic range, variability in drug concentrations based on differences in methods is not important, provided the same method is used each time for the patient.
Sample type also influences interpretation of cyclosporine concentration. Plasma concentrations will be lower than whole blood concentrations attributable to the concentration of cyclosporine in erythrocytes and leukocytes. Although either whole blood or plasma cyclosporine concentrations can be measured, most laboratories recommend measuring whole‐blood concentrations, and some assays are validated only for whole blood.
The timing of sample collection also affects results. The short half‐life of cyclosporine precludes predicting concentrations throughout a dosing interval based on a single sample. Peak concentrations are often 2‐ to 8‐fold higher than trough concentrations in normal animals. Much study has been applied to determining the most appropriate sample collection time for TDM in patients receiving cyclosporine. In human medicine, trough blood concentrations were the initial basis for adjustment of drug dosages. However, many studies in people have since suggested that AUC or 2‐hour peak drug concentrations are preferred. Although nephrotoxicity and hepatotoxicity can be predicted based on trough cyclosporine concentrations, trough concentrations have been shown to inadequately predict immunosuppression in human transplant patients.5 Dose adjustment based on the AUC over hours 0–12 in the dosing interval provides a much more reliable indicator of clinical immunosuppression in people, but the need to collect many blood samples adds to expense as well as patient discomfort and inconvenience. Because absorption of ultramicronized cyclosporine is virtually complete during the first 4 hours after dosing, the AUC for hours 0–4 was investigated as a simpler alternative to the AUC for hours 0–12. A close correlation was shown between the 2 methods, with fewer samples needed to calculate the AUC for 0–4 hours. Additional work in human medicine identified that the peak cyclosporine concentration, or the concentration in blood 2 hours postdosing, closely approximated patient outcome and 0–4 hours AUC results, and confirmed that trough concentrations correlated poorly with AUC calculations. With measurement of peak cyclosporine concentrations requiring only a single sample, adjusting drug dosages to attain target peak drug concentrations has become the single best blood concentration measurement for use during human organ transplantation. These findings apply to ultramicronized cyclosporine such as Neoral, as a 2‐hour blood sample reflects peak concentrations in virtually all patients. In contrast, these findings cannot be applied to the Sandimmune formulation, because the peak blood concentration varies between 2 and 6 hours.
In veterinary medicine, measurement of trough cyclosporine concentrations prevailed for many years based on initial work carried out in renal transplant studies in dogs. For twice‐daily cyclosporine dosing, trough samples are taken 12 hours postdosing, whereas, for once‐daily dosing, trough samples are taken 24 hours after dosing. More recent recommendations from laboratories offering TDM in dogs typically have involved measurement of both peak and trough cyclosporine blood concentrations, although target peak concentrations have not been well established. Individual laboratory recommendations depend on the target ranges determined by each laboratory as well as the assay used to measure cyclosporine concentrations. At the Auburn University TDM laboratory, for example, typical recommended therapeutic ranges for cyclosporine concentrations based on a monoclonal immunoassay are for renal transplantation, a trough concentration of 750 ng/mL for the first 3 months and then 350–400 ng/mL; for chronic inflammatory diseases, such as inflammatory bowel disease, a trough concentration of 250 ng/mL; and, for anal furunculosis, a trough concentration of 100–600 ng/mL (Boothe, unpublished observations, 2012). For canine atopic dermatitis, Steffen et al failed to find a significant difference among atopic scores at different cyclosporine concentrations, indicating a lack of relationship between drug concentration and response, and suggesting that there was no need for drug monitoring in dogs with atopy.28 However, as with other previous and comparable cyclosporine studies that failed to find significant differences using relatively small animal numbers, the risk of a type II error (failure to find a significant difference when one truly exists) was not evaluated. TDM is probably best approached as a method for determining individual patient responses rather than sample population responses and, given the complexity of cyclosporine pharmacokinetics, dose adjustments in individual patients should be made in consultation with the laboratory providing TDM.
Pharmacodynamic Assays
Pharmacokinetic measurements can provide evidence that cyclosporine blood concentrations are within the estimated target therapeutic range recommended by reference laboratories. This therapeutic range is established to capture the majority of patients expected to respond for a given condition. For some patients, this estimation may accurately predict immunosuppression, whereas, for others, clinical efficacy may not occur despite achievement of blood cyclosporine concentrations in the target therapeutic range. This variability in response to comparable blood concentrations may be attributed to differences in individual patient pharmacologic responses to cyclosporine, specifically within target cells, such as T‐lymphocytes. Wide variability in the relationship between clinical efficacy and therapeutic drug concentrations also is seen in human patients.84 For this reason, several pharmacodynamic assays have been developed in human medicine in an attempt to better estimate the dosage of cyclosporine needed to maintain immunosuppression and prevent organ rejection in individual transplant patients while minimizing the expense and adverse effects associated with excessive drug dosages.
Pharmacodynamic assays investigate a drug's effect on target cells. Several pharmacodynamic biomarkers of the immunosuppressive effects of cyclosporine have been studied in human medicine, including lymphocyte proliferation, enzyme (calcineurin) activity, lymphocyte surface antigen expression, and intracellular cytokine quantitation.85 Through pharmacodynamic monitoring, studies in humans have shown individually distinct degrees of calcineurin inhibitor sensitivity in patients. Selected immunologic biomarkers of immunosuppression have been validated in human medicine, suggesting their suitability for pharmacodynamic monitoring in clinical trials of human patients.86 Pharmacodynamic monitoring shows great promise for optimizing cyclosporine treatment and delivering individualized treatment.
Few pharmacodynamic studies assessing the immunologic effects of cyclosporine are found in the veterinary literature. One study demonstrated suppression of lymphocyte proliferation by flow cytometry after use of topical cyclosporine for treatment of canine keratoconjunctivitis sicca,87 but the findings were later refuted by another study that documented minimal cyclosporine blood concentrations and no effects on mitogen stimulation of peripheral blood lymphocytes after treatment with topical cyclosporine.88 A separate study did, however, confirm local suppression of inflammatory markers in the conjunctival epithelium after treatment with topical cyclosporine.89 In more recent veterinary studies utilizing cytokine analysis, quantitative reverse transcriptase polymerase chain reaction (qRT‐PCR) assays have been used to measure canine cellular messenger ribonucleic acid (mRNA) expression. One study investigated the effects of cyclosporine on activated canine mononuclear cells in vitro, and demonstrated a concentration‐dependent decrease in IL‐2, IL‐4, and IFN‐γ mRNA expression by qRT‐PCR.90 Another study evaluated cellular cytokine mRNA expression within lesional biopsies from dogs with anal furunculosis treated with oral cyclosporine, and demonstrated a significant reduction in IL‐2 mRNA expression and a lesser decrease in IFN‐γ expression with cyclosporine treatment.91
Recent pharmacodynamic studies in our laboratory have investigated ultramicronized cyclosporine (Atopica) in normal dogs. An initial in vitro investigation demonstrated cyclosporine‐mediated suppression of T‐lymphocyte activation–related molecules and cytokines in normal dogs. 92 Peripheral blood mononuclear cells were isolated and activated, with half of the cells incubated while exposed to cyclosporine, and the other half not exposed to the drug. Cells then were analyzed using flow cytometry, with T‐cell expression of the intracellular cytokines IL‐2, IL‐4, and IFN‐γ evaluated after drug exposure. All cytokines demonstrated a time‐dependent suppression profile. The T‐cell surface molecules CD25 and CD95, which have roles in T‐cell activation and development, were evaluated after drug exposure, and there was also significant suppression of expression of both biomarkers in the presence of cyclosporine. In a subsequent in vivo study, activated T‐cell expression of IL‐2, IL‐4, and IFN‐γ was investigated by flow cytometry when dogs were treated with 2 different oral cyclosporine dosages.93 The dogs first were given a high dosage of cyclosporine (10 mg/kg PO q12h), with doses adjusted upward as needed to attain a target trough drug concentration >600 ng/mL as measured via HPLC, a dosing protocol known to be sufficiently immunosuppressive for organ transplantation in dogs. With high‐dose cyclosporine, activated T‐cell expression of IL‐2 and IFN‐γ was significantly suppressed, but IL‐4 was not similarly affected. The dogs then were given the FDA‐approved dosage of cyclosporine used to treat canine atopy (5 mg/kg PO q24h), a dosage that has been considered to be low enough to avoid predisposing to immunosuppression‐associated infection.27 Even with this low dosage of cyclosporine, however, T‐cell expression of IFN‐γ was still significantly suppressed. Mean T‐cell expression of IL‐2 also was decreased and, although the degree of suppression in the group of dogs as a whole was not statistically significant, expression of IL‐2 in several individual dogs was markedly decreased.
Specific Disease Considerations
Atopic Dermatitis
Atopic dermatitis is a common pruritic dermatologic problem afflicting dogs, and is associated with IgE antibodies targeting environmental allergens.94 In the United States, Atopica is FDA‐approved for the treatment of atopy and, in fact, atopy is the only condition in dogs for which the systemic use of cyclosporine has been approved by the FDA. Many studies have focused on the sole use of cyclosporine for treatment of canine atopy. In an initial pilot study, 14 atopic dogs were treated with ultramicronized cyclosporine at a dosage of 5 mg/kg PO q24h for 2 weeks, and only 1 dog failed to respond to treatment.75 In a subsequent larger scale randomized controlled trial, atopic dogs were treated with placebo or ultramicronized cyclosporine at either 2.5 or 5 mg/kg PO q24h for 6 weeks, and the dogs given the higher dosage of cyclosporine were shown to have the most marked reductions in skin lesions and pruritus scores.59 Similar results have been seen in other studies investigating cyclosporine's utility in the treatment of atopic dermatitis.28, 74, 76, 95 Most studies in atopic dogs have been performed using the proprietary forms of ultramicronized cyclosporine, Atopica or Neoral. A recent study investigating the ability of a generic ultramicronized cyclosporine preparation for human use to treat canine atopy, however, demonstrated that the generic product also was effective in decreasing the severity of clinical signs. Thirteen atopic dogs received generic cyclosporine (Equoral) at a dosage of 5 mg/kg PO q24h, and outcome was compared to outcome in 7 atopic dogs treated with prednisone. Both groups showed significant reduction in clinical signs, and there was no difference between the treatment groups.96 Interestingly, response to cyclosporine treatment does not appear to be related to blood drug concentrations, perhaps because the drug is known to accumulate in the skin. In 1 study in atopic dogs, trough blood cyclosporine concentrations were measured in 97 patients receiving the FDA‐approved dosage of approximately 5 mg/kg of cyclosporine (Atopica) PO q24h.28 Although reduction in lesion scores approximated that of previous studies, no significant correlation was found between clinical improvement and blood drug concentrations. TDM of cyclosporine in dogs being treated for atopy therefore is not typically recommended initially in the course of treatment, but still may be useful in dogs that fail to respond to standard treatment with cyclosporine.
Sebaceous Adenitis
Sebaceous adenitis is an uncommon skin disease of dogs characterized by early perifollicular infiltration with inflammatory cells and later inflammation around sebaceous glands. Cyclosporine was specifically investigated in 1 study for its efficacy in treating sebaceous adenitis.77 Twelve dogs diagnosed with sebaceous adenitis were treated with ultramicronized cyclosporine at a dosage of 5 mg/kg PO q24h for 12 months, with re‐evaluations performed every 4 months. Mean clinical score was significantly decreased at all re‐evaluation points compared with pre treatment assessment, and posttreatment biopsy results identified a significant decrease in inflammation compared with initial biopsies.
Pemphigus Foliaceus
Pemphigus foliaceus is a relatively common canine autoimmune skin disease characterized by scaling, crusts, pustules, alopecia, and erosions, which may remain localized or become generalized.97 In a pilot study evaluating cyclosporine as sole treatment for treatment of pemphigus foliaceus, 5 affected dogs were given ultramicronized cyclosporine at a dosage of 5 mg/kg PO q24h for up to 3 months.12 Complete remission of pemphigus foliaceus was not attained in any dog, and 4 of 5 dogs had to be withdrawn from the study because of worsening signs and lack of response to cyclosporine monotherapy.
Anal Furunculosis
Anal furunculosis (or perianal fistula) is a chronic inflammatory and ulcerative disease in dogs causing focal to multifocal ulcerative tracts within perianal, anal, or perirectal tissues.46 Oral cyclosporine has been shown in several studies to be effective in the treatment of anal furunculosis.46 Oral cyclosporine typically is administered at a dosage between 4 and 8 mg/kg PO q24h or q12h.46 In an initial randomized controlled trial evaluating cyclosporine for treatment of anal furunculosis, 10 dogs received cyclosporine (Sandimmune) at a dosage of 5 mg/kg PO q12h while another 10 dogs received placebo.13 After 4 weeks of treatment, all dogs treated with cyclosporine had shown improvement, whereas no dogs treated with placebo had improved. All affected dogs then received cyclosporine treatment longer term. After 16 weeks of treatment with cyclosporine, 85% of treated dogs showed complete resolution of disease, with the remaining dogs showing detectable improvement. Disease recurrence occurred in 41% of dogs after treatment was discontinued. Other studies have shown similar results, with a majority of dogs treated with ultramicronized cyclosporine demonstrating either complete resolution of disease or at least substantial improvement.24, 56, 79, 82 Because a strong correlation between cyclosporine blood concentrations and clinical efficacy has not been recognized in dogs being treated for anal furunculosis,24, 56, 79, 82 measurement of blood cyclosporine concentrations is not recommended during initial treatment.46 Instead, treatment should be titrated based on resolution of clinical signs, with TDM reserved for those patients that fail to respond to standard treatment.46
Cyclosporine also has been combined with ketoconazole to achieve control of anal furunculosis, with substantial reductions in the cost of cyclosporine treatment. One study combined once‐daily ketoconazole (5.1–11 mg/kg) with once (2.5–5.5 mg/kg)‐ or twice (1.9–3.5 mg/kg)‐daily ultramicronized cyclosporine, and found resolution of clinical signs in all dogs within 9 weeks, with a cost savings of 36–71% over cyclosporine monotherapy. This study targeted trough blood concentrations of 400–600 ng/mL using HPLC.24 A similar study found remission in 93% of dogs treated for 16 weeks with ultramicronized cyclosporine (1 mg/kg PO q12h, initial dose) and ketoconazole (10 mg/kg PO q24h), with a target trough concentration of 200 ng/mL as measured by HPLC.78 A third study assessing varying ultramicronized cyclosporine dosages (0.5, 0.75, 1, and 2 mg/kg PO q12h) with ketoconazole (5.3–8.9 mg/kg PO q12h) and adjusting dosage to achieve trough concentrations of at least 400–600 ng/mL by RIA reported resolution of clinical signs in 3–10 weeks for all dogs.79 TDM is recommended when combining cyclosporine with ketoconazole to ensure that therapeutic concentrations are being attained, and to detect potentially toxic drug concentrations. The Auburn TDM laboratory has documented a change in cyclosporine half‐life from <10 to >150 hours in a dog treated simultaneously with ketoconazole and cyclosporine. On the other hand, elimination half‐lives of <15 hours also have been documented in dogs receiving both drugs, indicating marked variability in response to the effects of ketoconazole. Using ketoconazole and cyclosporine concurrently is an effective method for treating anal furunculosis in large dogs, and should be considered when cost is an issue. When using this approach, appropriate monitoring for ketoconazole hepatotoxicity should be performed. The use of cyclosporine in veterinary dermatology recently was reviewed by Kovalik et al, with an emphasis on the treatment of dermatologic conditions in dogs.98
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) is recognized as one of the most common causes of chronic gastrointestinal disease in dogs, with clinical signs typically including vomiting, diarrhea, and weight loss.99 Cyclosporine was shown to be effective as a sole drug treatment in some dogs with IBD. In a study of 14 dogs diagnosed with IBD that were refractory to glucocorticoid treatment, response to oral cyclosporine monotherapy was investigated.11 All dogs were treated with ultramicronized cyclosporine at a dosage of 5 mg/kg PO q24h for 10 weeks. Clinical signs and extent of infiltration of inflammatory cells into duodenal tissues were evaluated over the treatment period. Improvement in clinical signs was observed in 12 of 14 dogs, and significant decreases in T‐cell infiltration within duodenal biopsy specimens was appreciated when comparing posttreatment biopsies with pretreatment biopsies. A correlation between cyclosporine blood concentrations and resolution of clinical signs was not identified. Routine monitoring of cyclosporine concentrations in dogs being treated for IBD therefore is not recommended, except in those patients that fail to respond to standard treatment.
Myasthenia Gravis
Myasthenia gravis is a neuromuscular disorder characterized by inefficient synaptic transmission secondary to acetylcholine receptor dysfunction on the postsynaptic muscle membrane. Acquired myasthenia gravis is an immune‐mediated process characterized by antibody production targeting the nicotinic acetylcholine receptors found within skeletal muscle neuromuscular junctions. Initial treatment of myasthenia gravis often involves anticholinesterase medications. If a positive response is not observed, immunosuppressive medications are considered as additional treatment options. One case report described the use of cyclosporine in 2 dogs diagnosed with acquired myasthenia gravis that initially did not respond to pyridostigmine bromide and glucocorticoid treatment.100 Ultramicronized cyclosporine at a dosage of 4 mg/kg PO q12h was initiated in both dogs, and both demonstrated improvement in clinical signs after treatment with cyclosporine.
Meningoencephalomyelitis of Unknown Etiology
Meningoencephalomyelitis of unknown etiology refers to an inflammatory condition that affects the central nervous system of dogs without a documented cause.101 Diseases characterized as meningoencephalomyelitis of unknown etiology include granulomatous meningoencephalitis (GME), necrotizing meningoencephalitis, and necrotizing leukoencephalitis.101, 102, 103 Treatment for these diseases includes aggressive immunosuppression, with cyclosporine being 1 drug used for this purpose. In an initial study evaluating treatment of GME in 3 dogs with cyclosporine, all dogs achieved complete resolution of clinical signs.14 Ultramicronized cyclosporine was administered as sole treatment at an initial dosage of 10 mg/kg PO q24h after a variable period of glucocorticoid administration.14, 83 In a larger study evaluating 10 dogs diagnosed with meningoencephalomyelitis of unknown etiology, all dogs were treated with cyclosporine alone or in combination with steroids, ketoconazole, or both. The cyclosporine dosage was adjusted to maintain a trough blood concentration range of 200–400 ng/mL by HPLC.104 All dogs had either a partial or complete initial response to treatment. In all dogs, marked improvement in inflammation was demonstrated by serial cerebrospinal fluid analyses.
Transplantation
Cyclosporine traditionally has been considered the cornerstone of immunosuppressive treatment for the prevention of organ rejection in canine transplantation medicine, although transplant procedures in dogs are not currently readily available.37, 105 In canine transplantation, cyclosporine was administered twice daily, with blood concentrations measured and dosages adjusted as needed to meet target concentrations. Cyclosporine treatment then was continued throughout the lifetime of the recipient. In 1 recent study, 15 dogs underwent allogeneic renal transplantation and were given immunosuppressive treatment consisting of ultramicronized cyclosporine (Neoral; 10 mg/kg PO q12h), azathioprine (2–3 mg/kg PO q48h), and prednisolone (0.5 mg/kg PO q12h initially and then tapered).105 Cyclosporine dosages were adjusted based on whole blood trough concentrations to maintain a target concentration of 400–500 ng/mL as measured by HPLC for the first 6 months after surgery, and then between 350 and 450 ng/mL thereafter. Nine dogs died within 1 month of surgery, 3 dogs survived between 6 and 25 months, and 3 dogs were alive at the time of publication and had survived between 22 and 48 months postsurgery. Although triple‐drug immunosuppressive treatment prevented acute organ rejection in some dogs, there was a high frequency of drug‐related infection, and the authors felt that the dogs were overly immunosuppressed. The authors also stated that there was a “clear need for a pharmacodynamic assay that might achieve a balance between development of allograft rejection and infection,” as is the case in human transplantation medicine. Other older studies investigating cyclosporine treatment alone or in combination with other medications during organ transplantation in dogs have shown similar results, in that prevention of acute organ rejection is achieved in some dogs, but with a high prevalence of infection developing during treatment.9, 10, 106, 107, 108, 109
Other Diseases Associated with Cyclosporine Usage
Clinicians have considered using cyclosporine as part of the treatment for a wide variety of diseases that have the potential for responding to immunosuppressive treatment. Unfortunately, for most diseases, an insufficient number of cases have been published to allow objective assessment of the response to cyclosporine treatment. Diseases described in the literature for which oral cyclosporine has been used as a component of treatment include immune‐mediated hemolytic anemia, immune‐mediated thrombocytopenia, and immune‐mediated polyarthritis.110, 111, 112, 113, 114
Overview of Clinical Use of Cyclosporine
Recent pharmacodynamic research evaluating T‐cell responses to cyclosporine in dogs has confirmed that responses in dogs are comparable to the response profile that is well recognized in people. Individual responses to cyclosporine are extremely variable from dog to dog, both in dogs receiving the same standard oral dosage and in dogs receiving oral dosages adjusted to attain comparable blood concentrations of cyclosporine. Given that a high degree of variability in individual responsiveness to cyclosporine has been established in dogs, cyclosporine dosing protocols should be tailored to allow for this patient‐to‐patient variability. In our opinion, recommended dosing protocols in dogs with chronic, nonlife‐threatening inflammatory skin and gastrointestinal diseases should be quite different from protocols used in dogs with more acute and life‐threatening immune‐mediated diseases.
In chronic inflammatory diseases that are not immediately life‐threatening (eg, atopic dermatitis, anal furunculosis, mild IBD), cyclosporine often is effective at a standard, relatively low starting dosage. Although most clinical studies of these diseases have used the proprietary forms of ultramicronized cyclosporine, limited evidence indicates that generic preparations for human use may be equally effective, at least for the treatment of atopy. Generic preparations for human use probably should be considered only in nonlife‐threatening diseases in which sufficient time to titrate to effect is available. Cyclosporine treatment typically is delivered long‐term, with drug dosages adjusted upward if needed to effect, based predominantly on clinical signs. Most commonly, however, starting doses do not need to be increased and, in the long‐term, the cyclosporine dosage typically is tapered to the lowest effective dosage needed to maintain disease remission. Cyclosporine blood concentrations are usually not necessary in these circumstances, and remission of disease is the main criterion used to decide whether adequate cyclosporine treatment is being delivered. In fact, for many of these conditions, cyclosporine blood concentrations have been shown to have minimal correlation with disease remission, perhaps because the drug is selectively concentrated in tissues, such as the skin. TDM should be reserved for patients who fail to respond to standard treatment. Recent pharmacodynamic studies have shown that, even at standard low FDA‐approved dosages, some dogs can still develop clinically relevant suppression of certain T‐lymphocyte biomarkers of immunosuppression despite very low trough cyclosporine concentrations.93 Specifically, IFN‐γ expression can be substantially suppressed after treatment with low cyclosporine dosages, as compared with pretreatment levels of expression. This could explain the phenomenon anecdotally reported by some clinicians that individual dogs treated for atopic dermatitis can develop severe secondary infections (personal communication, Dr Amy Grooters, Louisiana State University, and Dr Juli Gunter, Mississippi State University), although the cyclosporine dosage originally chosen was not thought to cause clinically relevant immunosuppression. Therefore, even in dogs on low cyclosporine dosages, clinicians should remain vigilant for potential signs of systemic infection.
In dogs suffering from more acute and life‐threatening diseases, such as severe immune‐mediated hemolytic anemia and immune‐mediated thrombocytopenia, however, cyclosporine treatment must be targeted to attain effective immunosuppression as rapidly as possible. These animals are somewhat comparable to patients that have recently undergone organ transplantation, in that any delay in attaining effective immunosuppression can lead to a disastrous outcome. In these patients, starting cyclosporine at a low dosage and adjusting the dosage upward to effect is not recommended. Attaining effective oral doses as rapidly and accurately as possible is essential for ensuring adequate immunosuppression while avoiding overdosage with associated adverse effects and expense. Measurement of blood cyclosporine concentrations is the best method currently available to assess adequacy of treatment, and is strongly recommended in patients with life‐threatening immune‐mediated diseases.
Recent pharmacodynamic studies have shown that attainment of a trough blood cyclosporine concentration of 600 ng/mL (as measured by HPLC) reliably causes substantial immune system suppression in most dogs. However, because individual dogs exhibit impaired T‐cell function at much lower blood concentrations, this target blood concentration may reflect an unnecessarily high dosage for some dogs. Although, based on the human model, measurement of peak cyclosporine concentrations probably would enable far more accurate adjustment of treatment than would measurement of trough concentrations, to date, ideal target peak concentrations in dogs have not been well established. Continued assessment of peak cyclosporine blood concentrations is recommended (in addition to traditionally measured trough concentrations) to identify target ranges for various conditions in veterinary medicine. In human medicine, patients receiving cyclosporine often have pharmacodynamic evaluation of T‐cell function performed, in conjunction with the measurement of blood cyclosporine concentrations, to enable individualized adjustment of treatment for the patient. In veterinary medicine, it is likely that both measurement of blood drug concentrations and evaluation of T‐cell function also will be needed before we can truly deliver individualized medicine and appropriately adjust treatment for dogs with serious diseases being treated with cyclosporine at immunosuppressive dosages.
The most common adverse effects associated with initial cyclosporine usage, especially at higher dosages, are gastrointestinal in nature, including vomiting, diarrhea, and inappetence. In a dog with a life‐threatening disease and adverse gastrointestinal effects that needs ongoing cyclosporine treatment, options include administering the medication frozen (which appears to decrease nausea in some dogs) with food or both, or decreasing drug dosage. However, if cyclosporine is administered frozen or with food, it may alter drug absorption and change the amount of drug reaching the systemic circulation, thereby potentially jeopardizing the efficacy of treatment. Decreasing the cyclosporine dosage raises the same concern. Adjusting drug dosages or administration protocols to attain precisely targeted peak blood concentrations or indices of T‐cell suppression would enable clinicians to minimize adverse effects by precisely administering only enough drug to cause the desired extent of immunosuppression in the individual patient.
Cyclosporine is an expensive drug, particularly at higher immunosuppressive dosages, and clinicians therefore are tempted to explore cheaper forms of the drug. In human medicine, there are many approved generic microemulsion preparations similar to the Neoral formulation, and these generic preparations have been shown to have therapeutic equivalency in people. Studies investigating the pharmacokinetic properties of these generic preparations in dogs have not been performed and, for many diseases of dogs, it is not safe to assume that a generic formulation is therapeutically equivalent to the approved product for dogs (Atopica). In our experience, there appears to be marked variability in individual dogs in the oral bioavailability of these generic products. Use of generic products can therefore place our patients at risk of either therapeutic failure or toxicity. In our opinion, the preferred cyclosporine formulation for use in dogs remains the FDA‐approved veterinary product, for which extensive testing in the appropriate species has been conducted, although generic formulations may be a viable option in countries where the proprietary product is not available. Finally, the authors recommend that compounded cyclosporine not be prescribed unless no alternative preparations exist that meet the needs of the patient.
Conclusions
Cyclosporine is a powerful immunosuppressive agent used to treat a variety of diseases in dogs. Drug absorption and clinical efficacy can vary markedly among patients. In mild diseases that are not life‐threatening (eg, atopy), cyclosporine usually is administered at recommended dosages with dose adjustments based on individual patient response to treatment. In more life‐threatening immune‐mediated diseases, cyclosporine often is administered at higher dosages, with TDM used to ensure that adequate blood concentrations have been achieved. Trough blood drug concentrations traditionally have been used for veterinary drug monitoring, but peak concentrations may be preferable. Even with meticulous TDM, some dogs may not respond to treatment despite attainment of target blood cyclosporine concentrations. Pharmacodynamic monitoring is being investigated as an adjunctive strategy to further assess the immune system in dogs receiving cyclosporine. TDM in combination with pharmacodynamic assessment may offer a better overall evaluation of the immune response to cyclosporine treatment, providing clinically useful information for dose adjustments and allowing for better delivery of individualized medicine.
Acknowledgment
Conflict of Interest Declaration: Authors disclose no conflict of interest.
Footnote
Code of Federal Regulations that delineate the Animal Medicinal Drug Use Act (CFR 21)
References
- 1. Tedesco D, Haragsim L. Cyclosporine: A review. J Transplant 2012;2012:230386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kahan BD. Therapeutic drug monitoring of cyclosporine: 20 years of progress. Transplant Proc 2004;36:378S–391S. [DOI] [PubMed] [Google Scholar]
- 3. Calne R. Cyclosporine as a milestone in immunosuppression. Transplant Proc 2004;36:13S–15S. [DOI] [PubMed] [Google Scholar]
- 4. Graeb C, Arbogast H, Guba M, et al. Cyclosporine: 20 years of experience at the University of Munich. Transplant Proc 2004;36:125S–129S. [DOI] [PubMed] [Google Scholar]
- 5. Citterio F. Evolution of the therapeutic drug monitoring of cyclosporine. Transplant Proc 2004;36:420S–425S. [DOI] [PubMed] [Google Scholar]
- 6. Kapturczak MH, Meier‐Kriesche HU, Kaplan B. Pharmacology of calcineurin antagonists. Transplant Proc 2004;36:25S–32S. [DOI] [PubMed] [Google Scholar]
- 7. Kadar E, Sykes JE, Kass PH, et al. Evaluation of the prevalence of infections in cats after renal transplantation: 169 cases (1987–2003). J Am Vet Med Assoc 2005;227:948–953. [DOI] [PubMed] [Google Scholar]
- 8. Mathews KA, Holmberg DL. Kidney transplantation in dogs with naturally occurring end‐stage renal disease. J Am Anim Hosp Assoc 2000;36:475. [DOI] [PubMed] [Google Scholar]
- 9. Kyles AE, Gregory CR, Griffey SM, et al. An evaluation of combined immunosuppression with MNA 715 and microemulsified cyclosporine on renal allograft rejection in mismatched mongrel dogs. Vet Surg 2002;31:358–366. [DOI] [PubMed] [Google Scholar]
- 10. Bernsteen L, Gregory CR, Kyles AE, et al. Microemulsified cyclosporine‐based immunosuppression for the prevention of acute renal allograft rejection in unrelated dogs: Preliminary experimental study. Vet Surg 2003;32:213–219. [DOI] [PubMed] [Google Scholar]
- 11. Allenspach K, Rufenacht S, Sauter S, et al. Pharmacokinetics and clinical efficacy of cyclosporine treatment of dogs with steroid‐refractory inflammatory bowel disease. J Vet Intern Med 2006;20:239–244. [DOI] [PubMed] [Google Scholar]
- 12. Olivry T, Rivierre C, Murphy KM. Efficacy of cyclosporine for treatment induction of canine pemphigus foliaceus. Vet Rec 2003;152:53–54. [DOI] [PubMed] [Google Scholar]
- 13. Mathews KA, Sukhiani HR. Randomized controlled trial of cyclosporine for treatment of perianal fistulas in dogs. J Am Vet Med Assoc 1997;211:1249–1253. [PubMed] [Google Scholar]
- 14. Gnirs K. Ciclosporin treatment of suspected granulomatous meningoencephalomyelitis in three dogs. J Small Anim Pract 2006;47:201–206. [DOI] [PubMed] [Google Scholar]
- 15. Boothe DM. Therapeutic drug monitoring In: Boothe DM, ed. Small Animal Clinical Pharmacology and Therapeutics. St. Louis, MO: Elsevier; 2012:112–127. [Google Scholar]
- 16. Gregory C. Current veterinary therapy XIV In: Bonagura JD, ed. Immunosuppressive Agents. St. Louis, MO: Saunders Elsevier; 2009:2. [Google Scholar]
- 17. Kovarik JM, Mueller EA, van Bree JB, et al. Reduced inter‐ and intraindividual variability in cyclosporine pharmacokinetics from a microemulsion formulation. J Pharm Sci 1994;83:444–446. [DOI] [PubMed] [Google Scholar]
- 18. Mueller EA, Kovarik JM, van Bree JB, et al. Improved dose linearity of cyclosporine pharmacokinetics from a microemulsion formulation. Pharm Res 1994;11:301–304. [DOI] [PubMed] [Google Scholar]
- 19. Jorga A, Holt DW, Johnston A. Therapeutic drug monitoring of cyclosporine. Transplant Proc 2004;36:396S–403S. [DOI] [PubMed] [Google Scholar]
- 20. Rao A, Luo C, Hogan PG. Transcription factors of the NFAT family: Regulation and function. Annu Rev Immunol 1997;15:707–747. [DOI] [PubMed] [Google Scholar]
- 21. Rovira P, Mascarell L, Truffa‐Bachi P. The impact of immunosuppressive drugs on the analysis of T cell activation. Curr Med Chem 2000;7:673–692. [DOI] [PubMed] [Google Scholar]
- 22. Murphy K, Travers P, Walport M. Janeway's Immunobiology, 7th ed New York, NY: Garland Science; 2008. [Google Scholar]
- 23. Robson D. Review of the properties and mechanisms of action of cyclosporine with an emphasis on dermatological therapy in dogs, cats and people. Vet Rec 2003;152:768–772. [DOI] [PubMed] [Google Scholar]
- 24. Patricelli AJ, Hardie RJ, McAnulty JE. Cyclosporine and ketoconazole for the treatment of perianal fistulas in dogs. J Am Vet Med Assoc 2002;220:1009–1016. [DOI] [PubMed] [Google Scholar]
- 25. Robson D. Review of the pharmacokinetics, interactions and adverse reactions of cyclosporine in people, dogs and cats. Vet Rec 2003;152:739–748. [DOI] [PubMed] [Google Scholar]
- 26. Plumb DC. Plumb's Veterinary Drug Handbook, 6th ed Ames, IA: PharmaVet Inc.; 2008:5. [Google Scholar]
- 27. Guaguere E, Steffan J, Olivry T. Cyclosporin A: A new drug in the field of canine dermatology. Vet Dermatol 2004;15:61–74. [DOI] [PubMed] [Google Scholar]
- 28. Steffan J, Strehlau G, Maurer M, et al. Cyclosporin A pharmacokinetics and efficacy in the treatment of atopic dermatitis in dogs. J Vet Pharmacol Ther 2004;27:231–238. [DOI] [PubMed] [Google Scholar]
- 29. Thelen A, Mueller RS, Linek M, et al. Influence of food intake on the clinical response to cyclosporin A in canine atopic dermatitis. Vet Rec 2006;159:854–856. [PubMed] [Google Scholar]
- 30. Lown KS, Mayo RR, Leichtman AB, et al. Role of intestinal P‐glycoprotein (mdr1) in interpatient variation in the oral bioavailability of cyclosporine. Clin Pharmacol Ther 1997;62:248–260. [DOI] [PubMed] [Google Scholar]
- 31. Mealey KL, Waiting D, Raunig DL, et al. Oral bioavailability of P‐glycoprotein substrate drugs do not differ between ABCB1‐1Delta and ABCB1 wild type dogs. J Vet Pharmacol Ther 2010;33:453–460. [DOI] [PubMed] [Google Scholar]
- 32. Daigle JC, Hosgood G, Foil CS, et al. Effect of cimetidine on pharmacokinetics of orally administered cyclosporine in healthy dogs. Am J Vet Res 2001;62:1046–1050. [DOI] [PubMed] [Google Scholar]
- 33. Whalen RD, Tata PN, Burckart GJ, et al. Species differences in the hepatic and intestinal metabolism of cyclosporine. Xenobiotica 1999;29:3–9. [DOI] [PubMed] [Google Scholar]
- 34. Vickers AE, Fischer V, Connors S, et al. Cyclosporin A metabolism in human liver, kidney, and intestine slices. Comparison to rat and dog slices and human cell lines. Drug Metab Dispos 1992;20:802–809. [PubMed] [Google Scholar]
- 35. D'Mello A, Venkataramanan R, Satake M, et al. Pharmacokinetics of the cyclosporine‐ketoconazole interaction in dogs. Res Commun Chem Pathol Pharmacol 1989;64:441–454. [PMC free article] [PubMed] [Google Scholar]
- 36. Dahlinger J, Gregory C, Bea J. Effect of ketoconazole on cyclosporine dose in healthy dogs. Vet Surg 1998;27:64–68. [DOI] [PubMed] [Google Scholar]
- 37. Katayama M, Igarashi H, Fukai K, et al. Fluconazole decreases cyclosporine dosage in renal transplanted dogs. Res Vet Sci 2010;89:124–125. [DOI] [PubMed] [Google Scholar]
- 38. Katayama M, Igarashi H, Tani K, et al. Effect of multiple oral dosing of fluconazole on the pharmacokinetics of cyclosporine in healthy beagles. J Vet Med Sci 2008;70:85–88. [DOI] [PubMed] [Google Scholar]
- 39. D'Souza MJ, Pollock SH, Solomon HM. Cyclosporine‐cimetidine interaction. Drug Metab Dispos 1988;16:57–59. [PubMed] [Google Scholar]
- 40. Bar‐Meir S, Bardan E, Ronen I, et al. Cimetidine and omeprazole do not affect cyclosporine disposition by the rat liver. Eur J Drug Metab Pharmacokinet 1993;18:355–358. [DOI] [PubMed] [Google Scholar]
- 41. Shaefer MS, Rossi SJ, McGuire TR, et al. Evaluation of the pharmacokinetic interaction between cimetidine or famotidine and cyclosporine in healthy men. Ann Pharmacother 1995;29:1088–1091. [DOI] [PubMed] [Google Scholar]
- 42. Radwanski NE, Cerundolo R, Shofer FS, et al. Effects of powdered whole grapefruit and metoclopramide on the pharmacokinetics of cyclosporine in dogs. Am J Vet Res 2012;72:687–693. [DOI] [PubMed] [Google Scholar]
- 43. Alkharfy KM. Influence of overt diabetes mellitus on cyclosporine pharmacokinetics in a canine model. Exp Diabetes Res 2009;2009:363787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. White JV, Ravis WR, Nachreiner R, et al. Cyclosporine pharmacokinetics in normal and pancreatectomized dogs. Transplantation 1986;42:390–395. [DOI] [PubMed] [Google Scholar]
- 45. Takaya S, Iwatsuki S, Noguchi T, et al. The influence of liver dysfunction on cyclosporine pharmacokinetics—A comparison between 70 per cent hepatectomy and complete bile duct ligation in dogs. Jpn J Surg 1989;19:49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Patterson AP, Campbell KL. Managing anal furunculosis in dogs. Compendium 2005;27:339–355. [Google Scholar]
- 47. Singh AK. Narsipur SS. Cyclosporine A: Commentary on brand versus generic formulation exchange. J Transplant 2011;2011:480642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hibberd AD, Trevillian PR, Roger SD, et al. Assessment of the bioequivalence of a generic cyclosporine A by a randomized controlled trial in stable renal recipients. Transplantation 2006;81:711–717. [DOI] [PubMed] [Google Scholar]
- 49. Fukunaga K, Orito K. Time‐course effects of St John's wort on the pharmacokinetics of cyclosporine in dogs: Interactions between herbal extracts and drugs. J Vet Pharmacol Ther 2011;35:446–451. [DOI] [PubMed] [Google Scholar]
- 50. Lai J, Lu Y, Yin Z, et al. Pharmacokinetics and enhanced oral bioavailability in Beagle dogs of cyclosporine A encapsulated in glyceryl monooleate/poloxamer 407 cubic nanoparticles. Int J Nanomedicine 2010;5:13–23. [PMC free article] [PubMed] [Google Scholar]
- 51. Sander C, Holm P. Porous magnesium aluminometasilicate tablets as carrier of a cyclosporine self‐emulsifying formulation. AAPS PharmSciTech 2009;10:1388–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Amatori FM, Meucci V, Giusiani M, et al. Effect of grapefruit juice on the pharmacokinetics of cyclosporine in dogs. Vet Rec 2004;154:180–181. [DOI] [PubMed] [Google Scholar]
- 53. El‐Shabouri MH. Positively charged nanoparticles for improving the oral bioavailability of cyclosporin‐A. Int J Pharm 2002;249:101–108. [DOI] [PubMed] [Google Scholar]
- 54. Fischer JR, Harkin KR, Freeman LC. Concurrent administration of water‐soluble vitamin E can increase the oral bioavailability of cyclosporine A in healthy dogs. Vet Ther 2002;3:465–473. [PubMed] [Google Scholar]
- 55. Ford J, Woolfe J, Florence AT. Nanospheres of cyclosporin A: Poor oral absorption in dogs. Int J Pharm 1999;183:3–6. [DOI] [PubMed] [Google Scholar]
- 56. Griffiths LG, Sullivan M, Borland WW. Cyclosporin as the sole treatment for anal furunculosis: Preliminary results. J Small Anim Pract 1999;40:569–572. [DOI] [PubMed] [Google Scholar]
- 57. Yang SG. Biowaiver extension potential and IVIVC for BCS Class II drugs by formulation design: Case study for cyclosporine self‐microemulsifying formulation. Arch Pharm Res 2010;33:1835–1842. [DOI] [PubMed] [Google Scholar]
- 58. Steffan J, Parks C, Seewald W. Clinical trial evaluating the efficacy and safety of cyclosporine in dogs with atopic dermatitis. J Am Vet Med Assoc 2005;226:1855–1863. [DOI] [PubMed] [Google Scholar]
- 59. Olivry T, Steffan J, Fisch RD, et al. Randomized controlled trial of the efficacy of cyclosporine in the treatment of atopic dermatitis in dogs. J Am Vet Med Assoc 2002;221:370–377. [DOI] [PubMed] [Google Scholar]
- 60. Seibel W, Yahia NA, McCleary LB, et al. Cyclosporine‐induced gingival overgrowth in Beagle dogs. J Oral Pathol Med 1989;18:240–245. [DOI] [PubMed] [Google Scholar]
- 61. Werner AH. Psoriasiform‐lichenoid‐like dermatosis in three dogs treated with microemulsified cyclosporine A. J Am Vet Med Assoc 1986;2003:1013–1016. [DOI] [PubMed] [Google Scholar]
- 62. Favrot C, Olivry T, Werner AH, et al. Evaluation of papillomaviruses associated with cyclosporine‐induced hyperplastic verrucous lesions in dogs. Am J Vet Res 2005;66:1764–1769. [DOI] [PubMed] [Google Scholar]
- 63. Radowicz SN, Power HT. Long‐term use of cyclosporine in the treatment of canine atopic dermatitis. Vet Dermatol 2005;16:81–86. [DOI] [PubMed] [Google Scholar]
- 64. Mohri T, Takashima K, Yamane T, et al. Purulent pericarditis in a dog administered immune‐suppressing drugs. J Vet Med Sci 2009;71:669–672. [DOI] [PubMed] [Google Scholar]
- 65. Galgut BI, Janardhan KS, Grondin TM, et al. Detection of Neospora caninum tachyzoites in cerebrospinal fluid of a dog following prednisone and cyclosporine therapy. Vet Clin Pathol 2010;39:386–390. [DOI] [PubMed] [Google Scholar]
- 66. Blackwood L, German AJ, Stell AJ, et al. Multicentric lymphoma in a dog after cyclosporine therapy. J Small Anim Pract 2004;45:259–262. [DOI] [PubMed] [Google Scholar]
- 67. Callan MB, Preziosi D, Mauldin E. Multiple papillomavirus‐associated epidermal hamartomas and squamous cell carcinomas in situ in a dog following chronic treatment with prednisone and cyclosporine. Vet Dermatol 2005;16:338–345. [DOI] [PubMed] [Google Scholar]
- 68. Wahlstrom HE, Lavelle‐Jones M, Endres D, et al. Inhibition of insulin release by cyclosporine and production of peripheral insulin resistance in the dog. Transplantation 1990;49:600–604. [DOI] [PubMed] [Google Scholar]
- 69. Wahlstrom HE, Akimoto R, Endres D, et al. Recovery and hypersecretion of insulin and reversal of insulin resistance after withdrawal of short‐term cyclosporine treatment. Transplantation 1992;53:1190–1195. [DOI] [PubMed] [Google Scholar]
- 70. Thacker EL. Immunomodulators, immunostimulants, and immunotherapies in small animal veterinary medicine. Vet Clin North Am Small Anim Pract 2010;40:473–483. [DOI] [PubMed] [Google Scholar]
- 71. Rodriguez‐Romo R, Morales‐Buenrostro LE, Lecuona L, et al. Immune response after rabies vaccine in a kidney transplant recipient. Transpl Infect Dis 2011;13:492–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Cramer CH 2nd, Shieck V, Thomas SE, et al. Immune response to rabies vaccination in pediatric transplant patients. Pediatr Transplant 2008;12:874–877. [DOI] [PubMed] [Google Scholar]
- 73. Mathews KA, Holmberg DL, Johnston K, et al. Renal allograft survival in outbred mongrel dogs using rabbit anti‐dog thymocyte serum in combination with immunosuppressive drug therapy with or without donor bone marrow. Vet Surg 1994;23:347–357. [DOI] [PubMed] [Google Scholar]
- 74. Steffan J, Alexander D, Brovedani F, et al. Comparison of cyclosporine A with methylprednisolone for treatment of canine atopic dermatitis: A parallel, blinded, randomized controlled trial. Vet Dermatol 2003;14:11–22. [DOI] [PubMed] [Google Scholar]
- 75. Fontaine J, Olivry T. Treatment of canine atopic dermatitis with cyclosporine: A pilot clinical study. Vet Rec 2001;148:662–663. [DOI] [PubMed] [Google Scholar]
- 76. Olivry T, Rivierre C, Jackson HA, et al. Cyclosporine decreases skin lesions and pruritus in dogs with atopic dermatitis: A blinded randomized prednisolone‐controlled trial. Vet Dermatol 2002;13:77–87. [DOI] [PubMed] [Google Scholar]
- 77. Linek M, Boss C, Haemmerling R, et al. Effects of cyclosporine A on clinical and histologic abnormalities in dogs with sebaceous adenitis. J Am Vet Med Assoc 2005;226:59–64. [DOI] [PubMed] [Google Scholar]
- 78. Mouatt JG. Cyclosporin and ketoconazole interaction for treatment of perianal fistulas in the dog. Aust Vet J 2002;80:207–211. [DOI] [PubMed] [Google Scholar]
- 79. O'Neill T, Edwards GA, Holloway S. Efficacy of combined cyclosporine A and ketoconazole treatment of anal furunculosis. J Small Anim Pract 2004;45:238–243. [DOI] [PubMed] [Google Scholar]
- 80. House AK, Guitian J, Gregory SP, et al. Evaluation of the effect of two dose rates of cyclosporine on the severity of perianal fistulae lesions and associated clinical signs in dogs. Vet Surg 2006;35:543–549. [DOI] [PubMed] [Google Scholar]
- 81. Hardie RJ, Gregory SP, Tomlin J, et al. Cyclosporine treatment of anal furunculosis in 26 dogs. J Small Anim Pract 2005;46:3–9. [DOI] [PubMed] [Google Scholar]
- 82. Doust R, Griffiths LG, Sullivan M. Evaluation of once daily treatment with cyclosporine for anal furunculosis in dogs. Vet Rec 2003;152:225–229. [DOI] [PubMed] [Google Scholar]
- 83. Adamo FP, O'Brien RT. Use of cyclosporine to treat granulomatous meningoencephalitis in three dogs. J Am Vet Med Assoc 2004;225:1196. [DOI] [PubMed] [Google Scholar]
- 84. Stein CM, Murray JJ, Wood AJ. Inhibition of stimulated interleukin‐2 production in whole blood: A practical measure of cyclosporine effect. Clin Chem 1999;45:1477–1484. [PubMed] [Google Scholar]
- 85. Oellerich M, Barten MJ, Armstrong VW. Biomarkers: The link between therapeutic drug monitoring and pharmacodynamics. Ther Drug Monit 2006;28:35–38. [DOI] [PubMed] [Google Scholar]
- 86. Bohler T, Nolting J, Kamar N, et al. Validation of immunological biomarkers for the pharmacodynamic monitoring of immunosuppressive drugs in humans. Ther Drug Monit 2007;29:77–86. [DOI] [PubMed] [Google Scholar]
- 87. Gilger BC, Andrews J, Wilkie DA, et al. Cellular immunity in dogs with keratoconjunctivitis sicca before and after treatment with topical 2% cyclosporine. Vet Immunol Immunopathol 1995;49:199–208. [DOI] [PubMed] [Google Scholar]
- 88. Williams DL. Lack of effects on lymphocyte function from chronic topical ocular cyclosporine medication: A prospective study. Vet Ophthalmol 2010;13:315–320. [DOI] [PubMed] [Google Scholar]
- 89. Brignole F, Pisella PJ, De Saint Jean M, et al. Flow cytometric analysis of inflammatory markers in KCS: 6‐month treatment with topical cyclosporin A. Invest Ophthalmol Vis Sci 2001;42:90–95. [PubMed] [Google Scholar]
- 90. Kobayashi T, Momoi Y, Iwasaki T. Cyclosporine A inhibits the mRNA expressions of IL‐2, IL‐4 and IFN‐gamma, but not TNF‐alpha, in canine mononuclear cells. J Vet Med Sci 2007;69:887–892. [DOI] [PubMed] [Google Scholar]
- 91. Tivers MS, Catchpole B, Gregory SP, et al. Interleukin‐2 and interferon‐gamma mRNA expression in canine anal furunculosis lesions and the effect of ciclosporin therapy. Vet Immunol Immunopathol 2008;125:31–36. [DOI] [PubMed] [Google Scholar]
- 92. Fellman CL, Stokes JV, Archer TM, et al. Cyclosporine A affects the in vitro expression of T cell activation‐related molecules and cytokines in dogs. Vet Immunol Immunopathol 2011;140:175–180. [DOI] [PubMed] [Google Scholar]
- 93. Archer TM, Fellman CL, Stokes JV, et al. Pharmacodynamic monitoring of canine T‐cell cytokine responses to oral cyclosporine. J Vet Intern Med 2011;25:1391–1397. [DOI] [PubMed] [Google Scholar]
- 94. Olivry T, DeBoer DJ, Favrot C, et al. Treatment of canine atopic dermatitis: 2010 clinical practice guidelines from the International Task Force on Canine Atopic Dermatitis. Vet Dermatol 2010;21:233–248. [DOI] [PubMed] [Google Scholar]
- 95. Steffan J, Favrot C, Mueller R. A systematic review and meta‐analysis of the efficacy and safety of cyclosporin for the treatment of atopic dermatitis in dogs. Vet Dermatol 2006;17:3–16. [DOI] [PubMed] [Google Scholar]
- 96. Kovalik M, Taszkun I, Pomorski Z, et al. Evaluation of a human generic formulation of ciclosporin in the treatment of canine atopic dermatitis with in vitro assessment of the functional capacity of phagocytic cells. Vet Rec 2011;168:537. [DOI] [PubMed] [Google Scholar]
- 97. Gomez SM, Morris DO, Rosenbaum MR, et al. Outcome and complications associated with treatment of pemphigus foliaceus in dogs: 43 cases (1994–2000). J Am Vet Med Assoc 2004;224:1312–1316. [DOI] [PubMed] [Google Scholar]
- 98. Kovalik M, Thoday KL, van den Broek AH. The use of ciclosporin A in veterinary dermatology. Vet J 2012;193:317–325. [DOI] [PubMed] [Google Scholar]
- 99. Fogle JE, Bissett SA. Mucosal immunity and chronic idiopathic enteropathies in dogs. Compend Contin Educ Vet 2007;29:290–302; quiz 306. [PubMed] [Google Scholar]
- 100. Bexfield NH, Watson PJ, Herrtage ME. Management of myasthenia gravis using cyclosporine in 2 dogs. J Vet Intern Med 2006;20:1487–1490. [DOI] [PubMed] [Google Scholar]
- 101. Adamo PF, Adams WM, Steinberg H. Granulomatous meningoencephalomyelitis in dogs. Compend Contin Educ Vet 2007;29:678–690. [PubMed] [Google Scholar]
- 102. Higginbotham MJ, Kent M, Glass EN. Noninfectious inflammatory central nervous system diseases in dogs. Compend Contin Educ Vet 2007;29:488–497; quiz 497, 501. [PubMed] [Google Scholar]
- 103. Talarico LR, Schatzberg SJ. Idiopathic granulomatous and necrotising inflammatory disorders of the canine central nervous system: A review and future perspectives. J Small Anim Pract 2009;51:138–149. [DOI] [PubMed] [Google Scholar]
- 104. Adamo PF, Rylander H, Adams WM. Ciclosporin use in multi‐drug therapy for meningoencephalomyelitis of unknown aetiology in dogs. J Small Anim Pract 2007;48:486–496. [DOI] [PubMed] [Google Scholar]
- 105. Gregory CR, Kyles AE, Bernsteen L, et al. Results of clinical renal transplantation in 15 dogs using triple drug immunosuppressive therapy. Vet Surg 2006;35:105–112. [DOI] [PubMed] [Google Scholar]
- 106. Collier DS, Calne RY, De Curtins M, et al. Alternate‐day cyclosporine A and azathioprine in experimental dog renal allografts. Transplant Proc 1987;19:1279–1280. [PubMed] [Google Scholar]
- 107. Ochiai T, Sakamoto K, Gunji Y, et al. Effects of combination treatment with FK506 and cyclosporine on survival time and vascular changes in renal‐allograft‐recipient dogs. Transplantation 1989;48:193–197. [DOI] [PubMed] [Google Scholar]
- 108. Kyles AE, Gregory CR, Griffey SM, et al. Immunosuppression with a combination of the leflunomide analog, FK778, and microemulsified cyclosporine for renal transplantation in mongrel dogs. Transplantation 2003;75:1128–1133. [DOI] [PubMed] [Google Scholar]
- 109. Finco DR, Rawlings CA, Crowell WA, et al. Efficacy of azathioprine versus cyclosporine on kidney graft survival in transfused and nontransfused unmatched mongrel dogs. J Vet Intern Med 1987;1:61–66. [DOI] [PubMed] [Google Scholar]
- 110. Grundy SA, Barton C. Influence of drug treatment on survival of dogs with immune‐mediated hemolytic anemia: 88 cases (1989–1999). J Am Vet Med Assoc 2001;218:543–546. [DOI] [PubMed] [Google Scholar]
- 111. O'Marra SK, Delaforcade AM, Shaw SP. Treatment and predictors of outcome in dogs with immune‐mediated thrombocytopenia. J Am Vet Med Assoc 2011;238:346–352. [DOI] [PubMed] [Google Scholar]
- 112. Miller MD, Lunn KF. Diagnostic use of cytologic examination of bone marrow from dogs with thrombocytopenia: 58 cases (1994–2004). J Am Vet Med Assoc 2007;231:1540–1544. [DOI] [PubMed] [Google Scholar]
- 113. Putsche JC, Kohn B. Primary immune‐mediated thrombocytopenia in 30 dogs (1997–2003). J Am Anim Hosp Assoc 2008;44:250–257. [DOI] [PubMed] [Google Scholar]
- 114. Clements DN, Gear RN, Tattersall J, et al. Type I immune‐mediated polyarthritis in dogs: 39 cases (1997–2002). J Am Vet Med Assoc 2004;224:1323–1327. [DOI] [PubMed] [Google Scholar]


