Abbreviations
- SI
stimulus intensity
- SNAP
sensory nerve action potential
A 400‐kg 5‐year‐old Arabian gelding was presented for a 2‐ to 3‐year history of progressive uncontrollable violent headshaking that precluded any type of physical activity and compromised quality of life. Although there were no triggering events for the observed behavior, headshaking was exacerbated when a bridle was placed on the horse's head. One year before presentation, the horse underwent an extensive evaluation at another institution that included hematology and blood chemistry, testing for equine protozoal myelitis, skull radiographs, upper airway endoscopy (including guttural pouches), and magnetic resonance imaging of the head. Subtle asymmetry of the stylohyoid bone at its articulation was noted (left slightly thicker) on endoscopy. The rest of the diagnostic evaluation was within normal limits. Treatment with nonsteroidal anti‐inflammatory drugs, gabapentin, and diet modification failed to control the episodes. Additional laboratory testing, as well as oral and ophthalmologic examinations, was performed by the referring veterinarian and found normal. The horse was referred for further evaluation.
At presentation, the horse displayed violent continuous episodes of headshaking, which made the horse difficult to handle. Physical and neurologic examinations were normal except for the headshaking. These episodes were seen repeatedly while the horse was hospitalized, independent of time of day, light exposure, exercise, excitement, or confinement. The horse would frequently rub the right side of its face and eye. However, there were no obvious skin or ocular lesions. The horse would eat, but with interruptions attributable to headshaking. Some episodes associated with eating were triggered by hay touching the horse's muzzle. Therefore, soaked hay and pellets were offered. Laboratory testing showed mild neutrophilia (7,117/μL; reference range 2,600–6,800/μL) and 245 bands/μL with moderate toxicity, and normal plasma fibrinogen concentration; serum chemistry and blood gases analysis were within normal limits. Skull radiographs and upper airway endoscopy were not performed because computed tomography (CT) of the entire head was part of the diagnostic plan. A CT examination was done under general anesthesia and showed no abnormalities. Complete ophthalmologic and otoscopic examinations also were normal. Collection and evaluation of a spinal fluid sample were offered, but the owner declined.
Somatosensory evoked potentials of the trigeminal complex using the infraorbital nerve (branch of the maxillary nerve) were studied in this horse using an evoked potential system (Nicolet Viking IV1) as described by Aleman et al.1 In brief, with the horse in left lateral recumbency, a surface stimulus was applied to the dorsal gingival mucosa at the level of the right maxillary canine tooth.1 Three pairs of recording electrodes (Disposable EasyGrip monopolar electrode1) were placed along the sensory pathway of the trigeminal complex.1 Recording site 1 (R1: infraorbital nerve) was at the level of the infraorbital foramen; site 2 (R2: maxillary nerve) was at the level of the maxillary foramen; and site 3 (R3: spinal tract of trigeminal complex) was at the level of the spinal cord segment 1. A 4th recording site (R4: cortical somatosensory) utilized subdermal electrodes2 placed at the level of the frontoparietal cerebral cortex (Fig 1A). A ground electrode2 was placed between the stimulus site and first recording site. A surface temperature probe was positioned dorsal to the facial crest to monitor regional temperature while recording (local temperature was maintained at 35°C).
Figure 1.
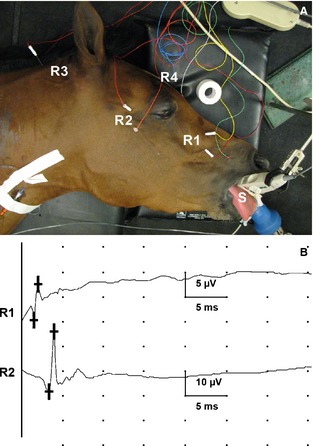
Sensory nerve conduction study. (A) Electrodes placement. S, stimulating probe at stimulus site at gingival mucosa of the maxillary canine; R1, recording site 1 (infraorbital nerve); R2, recording site 2 (maxillary nerve); R3, recording site 3 (spinal tract of trigeminal complex); R4, recording site 4 (cortical somatosensory). Surface temperature probe not shown here. (B) Sensory nerve action potentials at 5 mA stimulus intensity. R1, recording site 1; R2, recording site 2. Calibration bar at 5 ms per division, amplitude shown in μV for respective recording sites.
The stimulus rate was set at 3 Hz with a stimulus duration of 0.2 ms. The sweep speed was set at 5 ms per division. Each recording was the average of 1,000 responses. Acquisition sensitivities were variable with settings at 200, 100, 10, and 10 μV/divsion for recording sites 1, 2, 3, and 4, respectively. Band widths for R1–R3 were 20 Hz to 3 KHz, and 20–250 Hz for R4. Recordings were made at each of the following stimulus intensities (SI ± 0.1 mA): 2.5, 5, 10, 15, and 20 mA.1 Two sets of recordings were performed at each SI to test the reproducibility of the data. As a negative control, the study was also done with the SI set at 0 mA. Presence or absence of sensory nerve action potentials (SNAPs) was recorded, and the conduction velocity (m/s) was calculated for recording sites 1 and 2.1 The distance between recording sites was measured with a flexible measuring tape and used for the calculation of conduction velocity. For regions 3 and 4, the recordings were reported as present when seen because accurate estimation of distance can be difficult because of depth.1
Sensory nerve action potentials were triggered and recorded at SI of 5 (Fig 1B), 10, 15, and 20 mA. A muzzle twitch was observed associated with every stimulus applied. No SNAPs were triggered at stimulation intensities of 0 and 2.5 mA. The threshold for the induction of SNAP was low (SI, 5 mA) and consistent with other horses with idiopathic headshaking.1 Conduction velocity was within the range reported for control horses at higher stimulus intensities.1 At 20 mA SI, the conduction velocity at R1 was 65 m/s (reference range 64–85 m/s) and R2 was 97.2 m/s (reference range 74–109 m/s).1 Infusion of 20 mL of lidocaine hydrochloride in the region of the maxillary foramen was done and the sensory conduction study was repeated at a SI of 5 mA. The study showed failure to block sensory conduction with this infusion. To decrease the time of anesthesia and possible complications, only the right side was evaluated. The horse had a difficult recovery from anesthesia because of headshaking. The horse was also noted to cough a few times while recovering from anesthesia.
Because of the constant and violent nature of its headshaking, the horse was given detomidine hydrochloride (0.25 mg/kg IV), phenobarbital (6 mg/kg IV in saline over 30 minutes), and flunixin meglumine (1 mg/kg IV) while in the anesthesia recovery stall. Once the horse was returned to its stall, cyproheptadine hydrochloride was begun at a dosage of 0.31 mg/kg PO q12h and the horse was continued on flunixin meglumine at a dosage of 1 mg/kg IV q12h. The horse continued to display headshaking over the next 12 hours, but the frequency decreased from constantly to several minutes without episodes per hour. A thoracic ultrasound examination identified mild comet tails in both cranioventral lung fields (more pronounced on the right side), and the horse was started on ceftiofur at 2.2 mg/kg IV q12h and gentamicin at 6.6 mg/kg IV q24h. After 24 hours from the initiation of cyproheptadine, the frequency of headshaking substantially decreased to sporadic episodes during the day and the horse could eat hay and pellets without interruption. After 4 days of consistent improvement, the horse was safe to take for walks without headshaking. The pneumonia also improved and was switched to trimethoprim sulfamethoxazole at a dosage of 30 mg/kg PO q12h.
One day before the scheduled discharge of this horse, another horse in the barn developed a fever. As part of an infectious disease protocol, all horses in the barn had nasal swabs performed to investigate for respiratory pathogens. Nasal swabbing triggered frequent violent headshaking in this horse, which lasted approximately 12 hours. A few hours after the next dose of cyproheptadine, the horse's episodes diminished substantially. The horse was discharged on cyproheptadine 16 days after arrival. A few weeks after discharge, the horse would occasionally shake its head, but the frequency and severity were considered mild and the horse resumed training.
Idiopathic headshaking is a spontaneously occurring disorder of mature horses that can potentially compromise performance, quality of life, and might present safety concerns as was the case in the horse of this report.2 Although the disorder is seen primarily in geldings of Thoroughbred, Warmblood, and Quarter horse breeds, other breeds also can be affected as demonstrated by this Arabian gelding.3, 4 Shaking, tossing, or jerking movements of the head, rubbing of the muzzle and eyes, snorting, sneezing, striking at the face, and an anxious facial expression all are reported clinical manifestations in horses with idiopathic headshaking.3, 4, 5 Reported causes for headshaking include oral, dental, ocular, upper airway, ear lesions or some combination of these, temporomandibular joint disease, temporohyoid osteoarthropathy, skull fractures, neoplasia, behavioral disorders, and reaction to the placement of riding equipment (eg, bridle).5, 6, 7, 8, 9, 10, 11, 12, 13
Clinical diagnosis is based on the presence of clinical manifestations and elimination of other disorders.3, 4, 14, 15, 16 Infraorbital nerve blocks also have been used to support the diagnosis of idiopathic headshaking in horses.15, 17, 18 The infraorbital nerve, a branch of the maxillary nerve, provides sensory innervation to the rostral maxillary teeth, upper lip, part of maxillary sinus, and nose.19 Pain in any of these areas should be blocked with infraorbital or maxillary nerve desensitization techniques. Therefore, response to an infraorbital nerve block does not entirely define idiopathic headshaking, because a tooth ache will be blocked, for example.19 This may be further supported by the fact that people suffering from idiopathic trigeminal neuralgia have been misdiagnosed with dental disease and had extensive dental work to alleviate pain.20 Therefore, a more accurate and objective diagnostic modality is needed.1 Furthermore, a nerve block in the area of the maxillary nerve failed to block sensory nerve conduction in this gelding.
We previously described a novel technique to evaluate the function of the maxillary nerve in an objective manner, specifically by testing sensory nerve conduction and recorded evoked potentials from the trigeminal complex.1 Our nerve conduction studies showed that horses with idiopathic headshaking have a statistically significant lower threshold (stimulus intensity ≤5 mA) to trigger SNAP than healthy horses (≥10 mA).1 However, once SNAPs were triggered, no statistically significant differences in nerve conduction velocities were observed between control horses and horses with idiopathic headshaking.1 Similarly, the horse of this report had a low stimulus threshold (5 mA), but when the conduction velocity at higher SI was compared with previously reported controls or horses with idiopathic headshaking, there were no differences.1
This is the first report (ie, nonterminal study) in which this novel technique has been applied to support a clinical diagnosis of idiopathic headshaking.1 A limitation of the study was that testing was not performed bilaterally, particularly because this horse had asymmetrical signs (the right side was apparently more affected than the left). Asymmetry of signs was not noted in the previous nerve conduction study.1 An important observation was that after the infiltration of 20 mL of lidocaine hydrochloride around the maxillary nerve branch (a block routinely done for dental procedures), sensory nerve conduction was still observed. This raises concerns about the efficacy of nerve blocks at this location in horses. However, it is unknown if this finding would only apply to horses with idiopathic headshaking that apparently have lower thresholds for SNAP (nociception) than control horses and merits further investigation. This observed low threshold of triggered SNAP is appreciated clinically because apparently inocuous environmental stimuli are capable of inducing headshaking.4 An example of the hypersensitivity of this nerve was the reinitiation of violent headshaking after a nasal swab was collected from this horse.
There have been reports of various physical, medical, and surgical treatments for this condition in horses.3, 15, 17, 18, 21, 22, 23, 24 Cyproheptadine is an antihistamine with anticholinergic, antiserotonergic, and local anesthetic properties. Cyproheptadine was used in this horse and marked improvement was noted. This treatment was selected based on a favorable response to cyproheptadine in 70% (43 of 61) of affected horses reported in an owner survey.3 However, its mechanism of action for this particular disorder in horses is unknown.
Although this case and the previously reported study provide evidence of the involvement of the sensory trigeminal complex (maxillary branch), a specific cause for idiopathic headshaking was not identified.1 Based on this and other studies, a definitive cause for this disorder remains unknown, and structural abnormalities have not been fully investigated.1, 3, 14, 15, 25, 26 In addition, the involvement of other branches of the trigeminal complex warrants investigation. Infraorbital nerve blocks might not be definitive for the diagnosis of idiopathic headshaking and a more reliable and objective test is needed. In conclusion, sensory nerve conduction and evoked potentials studies of the maxillary nerve provide further support for the diagnosis of idiopathic headshaking in the clinical setting.
Acknowledgments
The authors thank John Doval for technical assistance. Financial support provided by anonymous private donors to the Equine and Comparative Neurology Research Group at UCD.
Conflict of Interest Declaration: Authors disclose no conflict of interest.
Footnotes
Nicolet Biomedical Inc., Madison, WI
Subdermal E‐2 Grass electrode; Astro‐Med Inc., West Warwick, RI
References
- 1. Aleman M, Williams DC, Brosnan RJ, et al. Sensory nerve conduction and somatosensory evoked potentials of the trigeminal nerve in horses with idiopathic headshaking. J Vet Intern Med 2013. 10.1111/jvim.12191:1‐10. [DOI] [PubMed] [Google Scholar]
- 2. Taylor KD, Mills DS. Headshaking syndrome In: Robinson NE, Sprayberry KA, eds. Current Therapy in Equine Medicine, 6th ed St. Louis, MO: Saunders Elsevier; 2009:103–107. [Google Scholar]
- 3. Madigan JE, Bell SA. Owner survey of headshaking in horses. J Am Vet Med Assoc 2001;219:334–337. [DOI] [PubMed] [Google Scholar]
- 4. Madigan JE, Bell SA. Characterisation of headshaking syndrome—31 cases. Equine Vet J Suppl 1998;27:28–29. [DOI] [PubMed] [Google Scholar]
- 5. Millls DS, Cook S, Taylor K, et al. Analysis of the variations in clinical signs shown by 254 cases of equine headshaking. Vet Rec 2002;150:236–240. [DOI] [PubMed] [Google Scholar]
- 6. Berger JM, Bell SA, Holmberg BJ, et al. Successful treatment of head shaking by use of infrared diode laser deflation and coagulation of corpora nigra cysts and behavioral modification in a horse. J Am Vet Med Assoc 2008;233:1610–1612. [DOI] [PubMed] [Google Scholar]
- 7. Blythe LL, Watrous BJ, Pearson EG. Otitis media/interna in the horse—A cause of head shaking and skull fractures. Am Assoc Equine Pract 1990;36:517–528. [Google Scholar]
- 8. Kold SE, Ostblom LC, Philipsen HP. Headshaking caused by a maxillary osteoma in a horse. Equine Vet J 1982;14:167–169. [DOI] [PubMed] [Google Scholar]
- 9. Mair TS. Headshaking associated with Trombicula autumnalis larval infestation in two horses. Equine Vet J 1994;26:244–245. [DOI] [PubMed] [Google Scholar]
- 10. McGorum BC, Dixon PM. Vasomotor rhinitis with headshaking in a pony. Equine Vet J 1990;22:220–222. [DOI] [PubMed] [Google Scholar]
- 11. Mills D, Geering R. Equine headshaking survey. Vet Rec 1997;141:504. [PubMed] [Google Scholar]
- 12. Moore LA, Johnson PJ, Messer NT, et al. Management of headshaking in three horses by treatment for protozoal myeloencephalitis. Vet Rec 1997;141:264–267. [DOI] [PubMed] [Google Scholar]
- 13. Voigt A, Saulez MN, Donnellan CM. Nuchal crest avulsion fracture in 2 horses: A cause of headshaking. J S Afr Vet Assoc 2009;80:111–113. [DOI] [PubMed] [Google Scholar]
- 14. Roberts V. Idiopathic headshaking in horses: Understanding the pathophysiology. Vet Rec 2011;168:17–18. [DOI] [PubMed] [Google Scholar]
- 15. Newton SA, Knottenbelt DC, Eldridge PR. Headshaking in horses: Possible aetiophathogenesis suggested by the results of diagnostic tests and several treatment regimes used in 20 cases. Equine Vet J 2000;32:208–216. [DOI] [PubMed] [Google Scholar]
- 16. Madigan JE, Kortz G, Murphy C, et al. Photic headshaking in the horse: 7 cases. Equine Vet J 1995;27:306–311. [DOI] [PubMed] [Google Scholar]
- 17. Mair TS. Assessment of bilateral infra‐orbital nerve blockade and bilateral infra‐orbital neurectomy in the investigation and treatment of idiopathic headshaking. Equine Vet J 1999;31:262–264. [DOI] [PubMed] [Google Scholar]
- 18. Roberts VLH, Perkins JD, Skarlina E, et al. Caudal anaesthesia of the infraorbital nerve for diagnosis of idiopathic headshaking and caudal compression of the infraorbital nerve for its treatment, in 58 horses. Equine Vet J 2013;45:107–110. [DOI] [PubMed] [Google Scholar]
- 19. Budras KD, Sack WO, Rock S, et al. Anatomy of the Horse, 5th ed Hannover: Schlutersche; 2009. [Google Scholar]
- 20. de Siqueira SR, Nobrega JC, Valle LB, et al. Idiopathic trigeminal neuralgia: Clinical aspects and dental procedures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;98:311–315. [DOI] [PubMed] [Google Scholar]
- 21. Mair TS, Howarth S, Lane JG. Evaluation of some prophylactic therapies for the idiopathic headshaker syndrome. Equine Vet J Suppl 1992;11:10–12. [DOI] [PubMed] [Google Scholar]
- 22. Mills DS, Cook S, Jones B. Reported response to treatment among 245 cases of equine headshaking. Vet Rec 2002;150:311–313. [DOI] [PubMed] [Google Scholar]
- 23. Mills DS, Taylor K. Field study of the efficacy of three types of nose net for the treatment of headshaking in horses. Vet Rec 2003;152:41–44. [DOI] [PubMed] [Google Scholar]
- 24. Roberts VL, McKane SA, Williams A, et al. Caudal compression of the infraorbital nerve: A novel surgical technique for treatment of idiopathic headshaking and assessment of its efficacy in 24 horses. Equine Vet J 2009;41:165–170. [DOI] [PubMed] [Google Scholar]
- 25. Pickles KJ, Berger J, Davies R, et al. Use of a gonadotrophin‐releasing hormone vaccine in headshaking horses. Vet Rec 2011;168:19. [DOI] [PubMed] [Google Scholar]
- 26. Aleman M, Pickles KJ, Simonek G, et al. Latent equine herpesvirus‐1 in trigeminal ganglia and equine idiopathic headshaking. J Vet Intern Med 2011;26:192–194. [DOI] [PubMed] [Google Scholar]


