Abstract
A sound knowledge of anatomical variations that could be encountered during surgical procedures is helpful in avoiding surgical complications. The current article details anomalous morphology of inferior alveolar nerves encountered during routine dissection of the craniofacial region in the Gross Anatomy laboratory. We also report variations of the lingual nerves, associated with the inferior alveolar nerves. The variations were documented and a thorough review of literature was carried out. We focus on the variations themselves, and the clinical implications that these variations present. Thorough understanding of variant anatomy of the lingual and inferior alveolar nerves may determine the success of procedural anesthesia, the etiology of pathologic processes, and the avoidance of surgical misadventure.
Key Words: Inferior alveolar nerve, Lingual nerve, Dental anesthesia, Anatomical variation
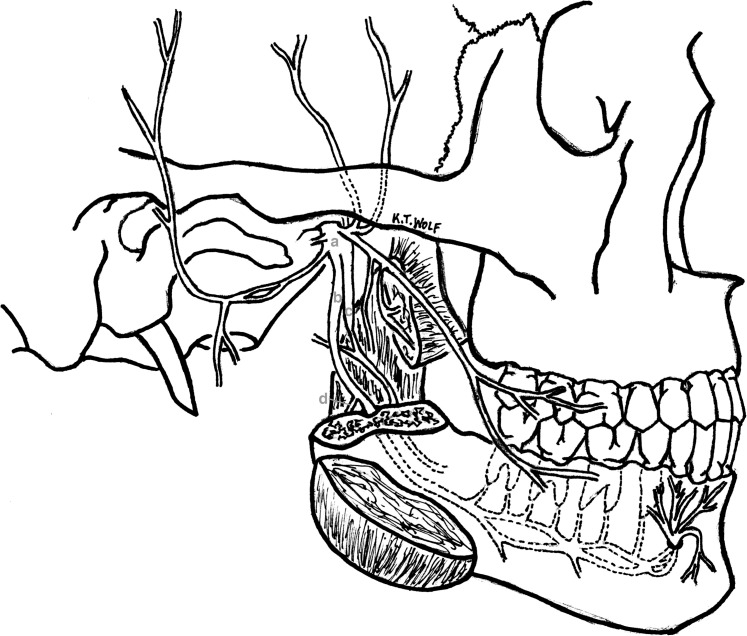
The inferior alveolar and lingual nerves, both sensory branches from the mandibular nerve (Cranial Nerve V3), are important nervous structures located within the infratemporal fossa (Figure 1, a). The inferior alveolar nerve (Figure 1, b) originates deep to the lateral pterygoid muscle and descends in the fossa, on the surface of the medial pterygoid muscle. Just prior to entering the mandible through the mandibular foramen, the mandibular nerve branches into an inferior alveolar nerve and a nerve to the mylohyoid (Figure 1, d). The inferior alveolar nerve enters the mandible through the mandibular foramen, while the nerve to the mylohyoid follows a more medial route, lying along the medial surface of the mandible to eventually innervate the mylohyoid muscle. Once it enters the mandible, the inferior alveolar nerve courses through the mandibular canal, running inferior to the roots of the mandibular teeth, and carries sensory information from the mandibular molars, second mandibular premolar, and the associated labial gingivae. The inferior alveolar nerve then divides into 2 terminal branches, the incisive and mental nerves. The incisive nerve continues within the mandibular canal, innervating the mandibular first premolar, canine, incisors, and associated gingivae, while the mental nerve exits the mandibular canal via the mental foramen to innervate the lower lip and chin.
Figure 1. .
Diagrammatic representation of the normal anatomy of the mandibular nerve in the infratemporal fossa. In the infratemporal fossa, the mandibular nerve (a) descends and gives off several branches. One of its branches, the inferior alveolar nerve (b), descends in the fossa, gives off the nerve to the mylohyoid (d), and enters the mandible through the mandibular foramen. Within the mandible, the nerve innervates the mandibular molars, second mandibular premolar and the associated labial gingivae, before dividing into 2 terminal branches, incisive and mental nerves. The lingual nerve (c) enters the oral cavity, carrying general sensation from soft tissue structures.
The lingual nerve, also a sensory branch of V3, descends in the infratemporal fossa between the tensor veli palatini and lateral pterygoid muscles to eventually enter the oral cavity, carrying general sensation from the anterior two thirds of the tongue, mucosa overlying the floor of the oral cavity, and lingual gingivae associated with the mandibular teeth (Figure 1, c). High in the infratemporal fossa, the lingual nerve is joined by the chorda tympani (branch of facial nerve, Cranial Nerve VII), and thus also carries taste from the anterior two thirds of the tongue, as well as parasympathetic innervation to all salivary glands below the oral fissure.1,2
BACKGROUND
The inferior alveolar nerve is known to present with anatomical variations prior to the nerve entering the mandibular canal, as well as along its course within the mandibular canal. Several cases of accessory mandibular foramina, with bifid inferior alveolar nerves located within the main mandibular canal or within accessory mandibular canals have been reported in literature. In 1967, Schejtman et al3,4 demonstrated the presence of accessory mandibular canals (retromolar canals) in a majority of dissected human cadavers (13 of 18 specimens). In 1971, Carter and Keen5 used dissected and dry mandible specimens to demonstrate the presence of numerous accessory foramina carrying neurovascular bundles to the muscles of mastication. Haveman and Tebo6 evaluated 150 dry mandibles and reported an average of 36 accessory foramina per mandible, and Serman's7 evaluation of 79 dry mandible specimens reported an 8.9% incidence of double mandibular foramina. Jeyaseelan and Sharma's8 study on 620 dry mandible specimens found a 4% incidence of accessory foramina, while Ossenberg9 reported a high incidence of accessory mandibular foramina in the retromolar region following an evaluation of 2500 dry mandible specimens. In addition to reports of accessory mandibular foramina and canals, Shiller and Wiswell,10 Sutton,11 and Chapnick12 have all reported the presence of accessory foramina located in the mandibular symphyseal region of dry skull specimens.
The first reported presence of bifid mandibular canals, as observed by radiographic evaluations, was made in 1973, Patterson and Funke,13 and Kiersch and Jordan.14 Later in 1977, Nortje et al15 described 3 unique presentations of supplemental mandibular canals following a retrospective study of panoramic radiographs from 3612 dental patients. Durst and Snow16 in 1980 reviewed 1024 panoramic radiographs and reported an incidence rate of 8.3% of multiple mandibular canals. Grover and Lorton's17 study in 1983 used 5000 radiographs and showed an incidence of 0.08% bifid mandibular canal occurrence. Langlais et al18 in 1985 evaluated 6000 panoramic radiographs taken over a period of 5 years, reported a 0.95% incidence of bifid mandibular canals, and went on to describe 4 main patterns of canals, while Zografos et al,19 evaluated 700 panoramic radiographs and reported an incidence of 0.4%. More recently, evaluations of panoramic radiographs by Devito and Tamburus,20 Sanchis et al,21 Vallarelli,22 Rossi et al,23 and Kuczynski et al24 reported incidences of 7.85%, 0.35%, 12.07%, 8.60%, and 1.98%, respectively, of bifid mandibular canals. Based on radiographic observations, Auluck et al25–27 reported a rare case of a trifid mandibular canal, in addition to bifid mandibular canals in 5 patients.
As reported incidences using dry skull specimens and radiographic evaluations have varied between 0.08% and 12.07%, investigators have used sectional imaging modalities, including computed tomography (CT) and cone beam CT, to provide high-resolution 3-dimensional images for evaluating variations of mandibular canals. Using CT techniques, Kaufman et al,28 Katakami et al,29 Naitoh et al,30–32 Kuribayashi et al,33 and Correr et al34 have all reported higher incidences of mandibular canal variations as compared with radiographic evaluations.
METHODS
During routine dissection of the infratemporal fossae of an 87-year-old female donor and a 92-year-old male donor, variations of the inferior alveolar nerves were encountered. The female donor had variations in the anatomy of both right and left inferior alveolar nerves, while the male donor had a variant left inferior alveolar nerve. The anatomical variations were dissected in detail and digital photographs taken. It was noted that the 2 reported variations were encountered following a total of 42 dissections of the temporal fossae completed over 3 years. A literature review was carried out to study the variations and understand the associated clinical implications.
CASE REPORT
Female Donor
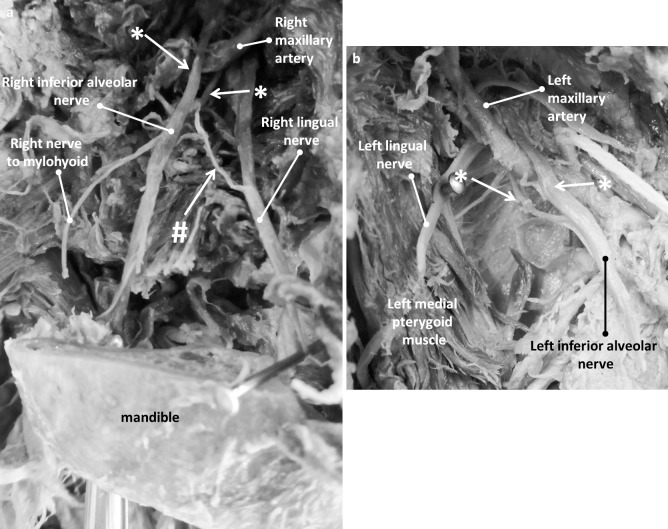
The female donor exhibited bilateral variations of the inferior alveolar nerve. The right lingual nerve traveled medially in the infratemporal fossa to enter the oral cavity, and the right inferior alveolar nerve entered the mandibular canal through the mandibular foramen in a lateral position. As expected, the nerve to mylohyoid was visualized branching from the inferior alveolar nerve (Figure 2a). Interestingly, the right inferior alveolar nerve exhibited a bifurcation around the right maxillary artery (Figure 2a, white asterisks and arrows). In addition, a nerve connecting the right lingual nerve and right inferior alveolar nerves was observed (Figure 2a, white hashtag and arrow). Dissection of the left infratemporal fossa of the same donor revealed a similar bifurcation of the left inferior alveolar nerve to surround the left maxillary artery (Figure 2b, white asterisks and arrows).
Figure 2. .
Photographs of dissected right and left infratemporal fossae. (a) The right infratemporal fossa shows the right lingual nerve traveling medially to enter the oral cavity and the right inferior alveolar nerve located laterally and entering the mandibular canal through the mandibular foramen. The nerve to mylohyoid is seen as a branch from the inferior alveolar nerve, as expected. White asterisks and arrows indicate the splitting of the inferior alveolar nerve around the maxillary artery. The white hashtag and arrow points to a nerve connecting the lingual and inferior alveolar nerves. (b) On the left side of the same donor body, dissection revealed a similar splitting of the left inferior alveolar nerve to surround the maxillary artery, indicated by white asterisks and arrows.
Male Donor
Dissection of the left infratemporal fossa showed the left inferior alveolar nerve entering the mandibular canal (Figure 3). The left lingual, inferior alveolar, and mylohyoid nerves showed expected anatomy. However, a distinct nerve connecting the left lingual and left inferior alveolar nerves was observed (Figure 3, white asterisk and arrow).
Figure 3. .
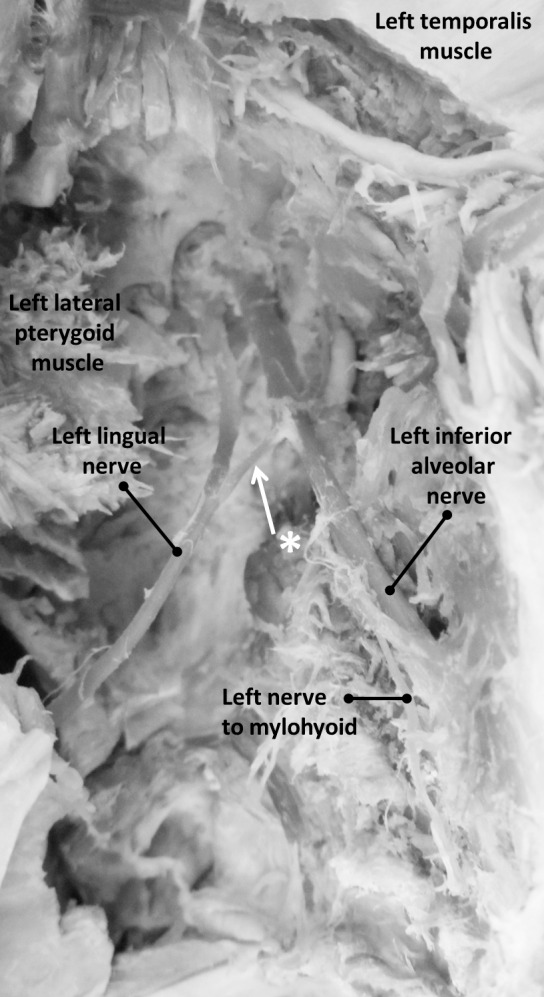
Photograph of dissected left infratemporal fossa. The left infratemporal fossa shows the mandible hemisected and turned over to expose the mandibular foramen with the left inferior alveolar nerve entering into the mandibular canal. The left lingual and inferior alveolar nerves show expected anatomy. A distinct nerve connects the lingual and inferior alveolar nerves, indicated by white asterisk and arrow.
DISCUSSION
Variations of the Mandibular Nerve
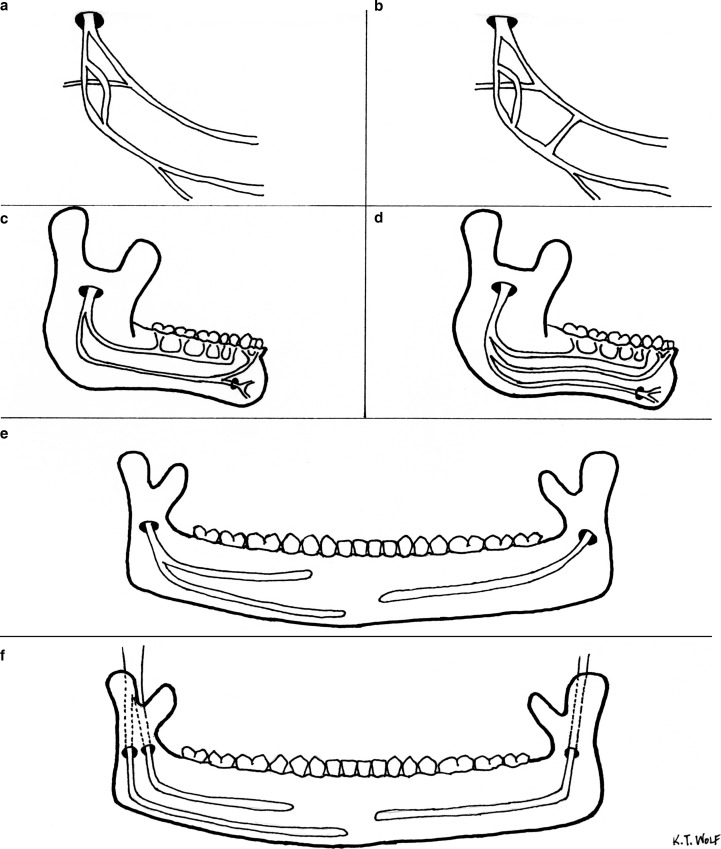
Branches of the mandibular nerve are known to exhibit variations within the infratemporal fossae, as they travel to enter the mandible. Specifically, the inferior alveolar nerve is known to bifurcate high in the infratemporal fossa and travel to the base of the coronoid process to then enter the mandible through accessory foramina in the retromolar region (Figure 4a).6,35–38 The presence of bifid inferior alveolar nerves may complicate dental anesthesia procedures because routine techniques for inferior alveolar nerve block, such as the Halstead method,39 may be insufficient to effectively block nerve conduction through both branches of the bifid nerve.40,41 The inferior alveolar nerve can enter the mandibular foramen as a single branch with variations within the mandible,42 and may also pose complications to obtaining profound anesthesia (Figure 4c, d, e).
Figure 4. .
Summary diagram indicating variant branching patterns of the inferior alveolar nerve. (a) The inferior alveolar nerve can split high in the infratemporal fossa and then reunite to enter the mandibular canal as a single nerve. (b) During its course in the infratemporal fossa, the inferior alveolar nerve may be connected via small nerve branches to the lingual nerve. (c) A single inferior alveolar nerve entering the mandibular canal may course through the mandible as 2 distinct branches. These branches may be located within a single mandibular canal, or within 2 independent mandibular canals. (d) A single inferior alveolar nerve entering the mandibular canal may course through the mandible as 3 distinct branches. (e) Variations of the inferior alveolar nerve within the mandible may be unilateral. (f) A unilateral presentation of the inferior alveolar nerve may include a bifid nerve entering the mandibular canal as 2 distinct nerves, and continuing to course through the mandible as independent nerves.
The inferior alveolar nerve may exist as 2 distinct branches, major and minor, within a single mandibular canal (Figure 4c, e). The major branch exits through the mental foramen to innervate the lower lip and chin, while the minor branch innervates the molars and premolars to then continue as the incisive nerve.
The inferior alveolar nerve may enter the mandibular foramen as a single branch and immediately trifurcate into 3 distinct branches within the mandible, with the first branch innervating the molars and premolars, the second branch innervating the canines and incisors, and a third branch continuing as the mental nerve after exiting the mandible through the mental foramen (Figure 4d).
The inferior alveolar nerve may enter the mandibular foramen as 2 distinct nerves and continue as 2 distinct branches within the mandibular canal (Figure 4f).
Our dissections exposed the inferior alveolar nerve entering the mandibular canal as a single branch.Gross dissection of the hemisected mandible revealed that within the mandibular canal, the inferior alveolar nerve followed its predicted course; providing branches to innervate the molars and premolars and then bifurcating into the incisive and mental nerves inferior to the premolar roots.
Of note, the variations we report occurred high in the infratemporal fossa, where the inferior alveolar nerve seems to originate from the posterior division of the mandibular nerve (Cranial Nerve V3) as 2 distinct branches/roots. The 2 roots encircle the maxillary artery and rejoin, to then continue inferiorly as a single inferior alveolar nerve (Figure 4a). Roy et al,38 Khan et al,43 and Daimi et al44 have previously reported a similar branching pattern of the inferior alveolar nerve. In addition to the relationship between the inferior alveolar nerve and the maxillary artery that we report, Pai et al45 have reported a unique 3-rooted inferior alveolar nerve with the maxillary artery enclosed between 2 of the 3 roots. Additional reports have shown the maxillary artery being enclosed within the inferior alveolar nerve and the presence of a connecting nerve to the auriculotemporal nerve, or located between the inferior alveolar nerve and the lingual nerve.37,46 The presence of the maxillary artery enclosed between nervous structures can have several clinical implications. The associated nerves can be compressed by pulsations of the artery, resulting in symptoms such as pain and numbness. Nerve compression has often been implicated as one of the causes of conditions like Trigeminal neuralgia. In addition, the close proximity of the artery with branches of the mandibular nerve also poses an increased chance of arterial damage during anesthesia procedures, with risk of hematoma formation.
On both donor bodies dissected, we report the presence of a nervous connection between the inferior alveolar nerve and the lingual nerve (Figure 4b). Racz et al,47,48 Khaledpour,49 Bergman et al,50 and Sakamoto et al51 have previously reported connections between the inferior alveolar and lingual nerves, or other branches of the mandibular nerve.52 As indicated previously by Kim et al,53 we speculate that these accessory communications could provide auxiliary innervation to the mandibular teeth and associated soft tissues, and may be implicated in insufficient dental anesthesia owing to the potential for collateral transmission of nervous impulses.
Clinical Implications
In the dental office, lack of profound anesthesia following routine administration of local anesthetic agents is attributable to various causes, including but not limited to, local inflammatory conditions, insufficient anesthetic solution, inappropriate identification of anatomical landmarks, or presence of anatomical variations.54–56 The incidence of variations associated with the anatomy of the mandibular nerve and its branches necessitate that clinicians adopt alternate techniques of local anesthesia in order to achieve expected results. Alternate techniques to achieve anesthesia of the inferior alveolar nerve may include delivery of the anesthetic solution at a higher anatomical level in order to sufficiently anesthetize all branches of the mandibular nerve, including any additional inferior alveolar branches that may be present.57,58 Specific techniques that target the lingual nerve could also be used in situations where collateral anatomical connections between the inferior alveolar and lingual nerves are suspected. Preoperative imaging evaluation can provide evidence of such variations in the dental office, and the growing use of cone beam CT imaging for routine diagnostic purposes can increase the clinician's ability to identify and manage such variations in the population.59 In the more infrequent case where a vascular structure such as the maxillary artery is trapped between branches of the mandibular nerve, frequent and unexplained hematoma formation during anesthetic procedures may be indicative of vascular impingement.60 In such situations, diagnostic work-ups with magnetic resonance imaging or CT imaging may be required to accurately identify and manage the condition. If anatomical variations manifest as neuralgias, appropriate follow-up and referrals will be required to manage the patient's specific complaint.37,61
In conclusion, an understanding of anatomical variations is imperative, as without adopting alternate anesthesia techniques such variations may potentially thwart a clinician from achieving successful pain control. In addition, by performing thorough diagnostic and presurgical evaluations of the associated neurovasculature, clinicians will not only be better able to assess any anatomical variants present, but also be able to better influence outcomes of surgical procedures related to the infratemporal fossa or mandible.
Footnotes
Part of this manuscript was presented at the 2015 SIU-School of Dental Medicine Research Day.
REFERENCES
- 1. Sicher H. The anatomy of mandibular anesthesia. J Am Dent Assoc. 1946; 33: 1541– 1557. [DOI] [PubMed] [Google Scholar]
- 2. Standring S. Gray's Anatomy . 40th ed. New York, NY: Elsevier; 2009. [Google Scholar]
- 3. Arias NH, Schejtman R, Devoto FC. Distribution of components of the retromolar mandibular canal in the buccinator muscle [in Spanish]. Rev Asoc Odontol Argent. 1967; 55: 502– 503. [PubMed] [Google Scholar]
- 4. Schejtman R, Devoto FC, Arias NH. The origin and distribution of the elements of the human mandibular retromolar canal. Arch Oral Biol. 1967; 12: 1261– 1268. [DOI] [PubMed] [Google Scholar]
- 5. Carter RB, Keen EN. The intramandibular course of the inferior alveolar nerve. J Anat. 1971; 108: 433– 440. [PMC free article] [PubMed] [Google Scholar]
- 6. Haveman CW, Tebo HG. Posterior accessory foramina of the human mandible. J Prosthet Dent. 1976; 35: 462– 468. [DOI] [PubMed] [Google Scholar]
- 7. Serman NJ. Differentiation of double mental foramina from extra bony coursing of the incisive branch of the mandibular nerve—an anatomic study. Refuat Hashinayim. 1987; 5: 20– 22. [PubMed] [Google Scholar]
- 8. Jeyaseelan N, Sharma JK. Morphological study of unnamed foramina in north Indian human mandibles and its possible role in neurovascular transmission. Int J Oral Surg. 1984; 13: 239– 242. [DOI] [PubMed] [Google Scholar]
- 9. Ossenberg NS. Retromolar foramen of the human mandible. Am J Phys Anthropol. 1987; 73: 119– 128. [DOI] [PubMed] [Google Scholar]
- 10. Shiller WR, Wiswell OB. Lingual foramina of the mandible. Anat Rec. 1954; 119: 387– 390. [DOI] [PubMed] [Google Scholar]
- 11. Sutton RN. The practical significance of mandibular accessory foramina. Aust Dent J. 1974; 19: 167– 173. [DOI] [PubMed] [Google Scholar]
- 12. Chapnick L. A foramen on the lingual of the mandible. J Can Dent Assoc. 1980; 46: 444– 445. [PubMed] [Google Scholar]
- 13. Patterson JE, Funke FW. Bifid inferior alveolar canal. Oral Surg Oral Med Oral Pathol. 1973; 36: 287– 288. [DOI] [PubMed] [Google Scholar]
- 14. Kiersch TA, Jordan JE. Duplication of the mandibular canal. Oral Surg Oral Med Oral Pathol. 1973; 35: 133– 134. [DOI] [PubMed] [Google Scholar]
- 15. Nortje CJ, Farman AG, Grotepass FW. Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg. 1977; 15: 55– 63. [DOI] [PubMed] [Google Scholar]
- 16. Durst JH, Snow JE. Multiple mandibular canals: oddities or fairly common anomalies? Oral Surg Oral Med Oral Pathol. 1980; 49: 272– 273. [DOI] [PubMed] [Google Scholar]
- 17. Grover PS, Lorton L. Bifid mandibular nerve as a possible cause of inadequate anesthesia in the mandible. J Oral Maxillofac Surg. 1983; 41: 177– 179. [DOI] [PubMed] [Google Scholar]
- 18. Langlais RP, Broadus R, Glass BJ. Bifid mandibular canals in panoramic radiographs. J Am Dent Assoc. 1985; 110: 923– 926. [DOI] [PubMed] [Google Scholar]
- 19. Zografos J, Kolokoudias M, Papadakis E. The types of the mandibular canal [in Greek, Modern]. Hell Period Stomat Gnathopathoprosopike Cheir. 1990; 5: 17– 20. [PubMed] [Google Scholar]
- 20. Devito KL, Tamburus JR. Anatomy of the mandibular canal: radiographic classification of variations. Rev Assoc Paul Cir Dent. 2001; 55: 261– 266. [Google Scholar]
- 21. Sanchis JM, Penarrocha M, Soler F. Bifid mandibular canal. J Oral Maxillofac Surg. 2003; 61: 422– 424. [DOI] [PubMed] [Google Scholar]
- 22. Vallarelli TP. Radiographic interpretation of the mandibular canal in panoramic radiographs. Rev Aca Tir Odo. 2007; 7: 432– 449. [Google Scholar]
- 23. Rossi PM, Brucker MR, Rockenbach MIB. Canais da mandibula bifurcados: anlise em radiografias panoramicas. Rev Cienc Med. 2009; 18: 99– 104. [Google Scholar]
- 24. Kuczynski A, Kucharski W, Franco A, Westphalen FH, de Lima AA, Fernandes A. Prevalence of bifid mandibular canals in panoramic radiographs: a maxillofacial surgical scope. Surg Radiol Anat. 2014; 36: 847– 850. [DOI] [PubMed] [Google Scholar]
- 25. Auluck A, Pai KM. Trifid mandibular nerve canal. Dentomaxillofac Radiol. 2005; 34: 259. [DOI] [PubMed] [Google Scholar]
- 26. Auluck A, Pai KM, Mupparapu M. Multiple mandibular nerve canals: radiographic observations and clinical relevance. Report of 6 cases. Quintessence Int. 2007; 38: 781– 787. [PubMed] [Google Scholar]
- 27. Auluck A, Pai KM, Shetty C. Pseudo bifid mandibular canal. Dentomaxillofac Radiol. 2005; 34: 387– 388. [DOI] [PubMed] [Google Scholar]
- 28. Kaufman E, Serman NJ, Wang PD. Bilateral mandibular accessory foramina and canals: a case report and review of the literature. Dentomaxillofac Radiol. 2000; 29: 170– 175. [DOI] [PubMed] [Google Scholar]
- 29. Katakami K, Mishima A, Kuribayashi A, Shimoda S, Hamada Y, Kobayashi K. Anatomical characteristics of the mandibular lingual foramina observed on limited cone-beam CT images. Clin Oral Implants Res. 2009; 20: 386– 390. [DOI] [PubMed] [Google Scholar]
- 30. Naitoh M, Hiraiwa Y, Aimiya H, Ariji E. Observation of bifid mandibular canal using cone-beam computerized tomography. Int J Oral Maxillofac Implants. 2009; 24: 155– 159. [PubMed] [Google Scholar]
- 31. Naitoh M, Hiraiwa Y, Aimiya H, Gotoh K, Ariji E. Accessory mental foramen assessment using cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107: 289– 294. [DOI] [PubMed] [Google Scholar]
- 32. Naitoh M, Nakahara K, Hiraiwa Y, Aimiya H, Gotoh K, Ariji E. Observation of buccal foramen in mandibular body using cone-beam computed tomography. Okajimas Folia Anat Jpn. 2009; 86: 25– 29. [DOI] [PubMed] [Google Scholar]
- 33. Kuribayashi A, Watanabe H, Imaizumi A, Tantanapornkul W, Katakami K, Kurabayashi T. Bifid mandibular canals: cone beam computed tomography evaluation. Dentomaxillofac Radiol. 2010; 39: 235– 239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Correr GM, Iwanko D, Leonardi DP, Ulbrich LM, Araujo MR, Deliberador TM. Classification of bifid mandibular canals using cone beam computed tomography. Braz Oral Res. 2013; 27: 510– 516. [DOI] [PubMed] [Google Scholar]
- 35. Sawyer DR, Kiely ML. Retromolar foramen: a mandibular variant important to dentistry. Ann Dent. 1991; 50: 16– 18. [PubMed] [Google Scholar]
- 36. Pyle MA, Jasinevicius TR, Lalumandier JA, Kohrs KJ, Sawyer DR. Prevalence and implications of accessory retromolar foramina in clinical dentistry. Gen Dent. 1999; 47: 500– 503; quiz 04–05. [PubMed] [Google Scholar]
- 37. Anil A, Peker T, Turgut HB, Gulekon IN, Liman F. Variations in the anatomy of the inferior alveolar nerve. Br J Oral Maxillofac Surg. 2003; 41: 236– 239. [DOI] [PubMed] [Google Scholar]
- 38. Roy TS, Sarkar AK, Panicker HK. Variation in the origin of the inferior alveolar nerve. Clin Anat. 2002; 15: 143– 147. [DOI] [PubMed] [Google Scholar]
- 39. Malamed SF. Handbook of Local Anesthesia. 6th ed. St Louis, Mo: Mosby; 2014. [Google Scholar]
- 40. DeSantis JL, Liebow C. Four common mandibular nerve anomalies that lead to local anesthesia failures. J Am Dent Assoc. 1996; 127: 1081– 1086. [DOI] [PubMed] [Google Scholar]
- 41. Lew K, Townsen G. Failure to obtain adequate anaesthesia associated with a bifid mandibular canal: a case report. Aust Dent J. 2006; 51: 86– 90. [DOI] [PubMed] [Google Scholar]
- 42. Rodella LF, Buffoli B, Labanca M, Rezzani R. A review of the mandibular and maxillary nerve supplies and their clinical relevance. Arch Oral Biol. 2012; 57: 323– 334. [DOI] [PubMed] [Google Scholar]
- 43. Khan MM, Darwish HH, Zaher WA. Perforation of the inferior alveolar nerve by the maxillary artery: an anatomical study. Br J Oral Maxillofac Surg. 2010; 48: 645– 647. [DOI] [PubMed] [Google Scholar]
- 44. Daimi SR, Siddiqui AU, Vyas VR, Sheikh S. Unique presentation of maxillary artery, lingual nerve, and inferior alveolar nerve complex. Int J Appl Basic Med Res. 2011; 1: 125– 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Pai MM, Swamy RS, Prabhu LV. A variation in the morphology of the inferior alveolar nerve with potential clinical significance. Biomed Int. 2010; 1: 93– 95. [Google Scholar]
- 46. Gulekon N, Anil A, Poyraz A, Peker T, Turgut HB, Karakose M. Variations in the anatomy of the auriculotemporal nerve. Clin Anat. 2005; 18: 15– 22. [DOI] [PubMed] [Google Scholar]
- 47. Racz L, Maros T. The anatomic variants of the lingual nerve in human (author's translation) [in German]. Anat Anz. 1981; 149: 64– 71. [PubMed] [Google Scholar]
- 48. Racz L, Maros T, Seres-Sturm L. Anatomical variations of the nervus alveolaris inferior and their importance for the practice (author's translation) [in German]. Anat Anz. 1981; 149: 329– 332. [PubMed] [Google Scholar]
- 49. Khaledpour C. An anatomic variant of the inferior alveolar nerve in man [in German]. Anat Anz. 1984; 156: 403– 406. [PubMed] [Google Scholar]
- 50. Bergman RA, Thompson SA, Afifi AK. Catalog of Human Variation . Baltimore, Md: Urban and Schwarzenberg; 1983. [Google Scholar]
- 51. Sakamoto Y, Akita K. Spatial relationships between masticatory muscles and their innervating nerves in man with special reference to the medial pterygoid muscle and its accessory muscle bundle. Surg Radiol Anat. 2004; 26: 122– 127. [DOI] [PubMed] [Google Scholar]
- 52. Fazan VPS, Rodrigues Filho OA, Matamala F. Communication between the mylohyoid and lingual nerves: clinical implications. Int J Morphol. 2007; 25: 561– 564. [Google Scholar]
- 53. Kim SY, Hu KS, Chung IH, Lee EW, Kim HJ. Topographic anatomy of the lingual nerve and variations in communication pattern of the mandibular nerve branches. Surg Radiol Anat. 2004; 26: 128– 135. [DOI] [PubMed] [Google Scholar]
- 54. Fleury AA. Local anesthesia failure in endodontic therapy: the acute inflammation factor. Compendium. 1990; 11:210, 12, 14 passim. [PubMed] [Google Scholar]
- 55. Wong MK, Jacobsen PL. Reasons for local anesthesia failures. J Am Dent Assoc. 1992; 123: 69– 73. [DOI] [PubMed] [Google Scholar]
- 56. Vreeland DL, Reader A, Beck M, Meyers W, Weaver J. An evaluation of volumes and concentrations of lidocaine in human inferior alveolar nerve block. J Endod. 1989; 15: 6– 12. [DOI] [PubMed] [Google Scholar]
- 57. Meechan JG. How to overcome failed local anaesthesia. Br Dent J. 1999; 186: 15– 20. [DOI] [PubMed] [Google Scholar]
- 58. Blanton PL, Jeske AH. Dental local anesthetics: alternative delivery methods. J Am Dent Assoc. 2003; 134: 228– 234. [DOI] [PubMed] [Google Scholar]
- 59. Afsar A, Haas DA, Rossouw PE, Wood RE. Radiographic localization of mandibular anesthesia landmarks. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998; 86: 234– 241. [DOI] [PubMed] [Google Scholar]
- 60. Blanton PL, Jeske AH. Avoiding complications in local anesthesia induction: anatomical considerations. J Am Dent Assoc. 2003; 134: 888– 893. [DOI] [PubMed] [Google Scholar]
- 61. Krmpotic-Nemanic J, Vinter I, Hat J, Jalsovec D. Mandibular neuralgia due to anatomical variations. Eur Arch Otorhinolaryngol. 1999; 256: 205– 208. [DOI] [PubMed] [Google Scholar]