Abstract
Objective
To develop and evaluate a novel, comprehensive prevention program for older adults designed to assess and improve adherence to preventive health care goals.
Method
In McKeesport, Pennsylvania, 389 men and women aged 65 and older were enrolled. We assessed adherence to 10 preventive health goals, provided education and counseling, and reevaluated after 12 months.
Results
At baseline, adherence varied. After 12 months, proportions of participants meeting goals were improved for several areas. Overall, improvements were seen for the proportion of participants meeting goals for low-density lipoprotein (LDL) cholesterol (+43%), blood pressure control in hypertensives (+17%), blood glucose control in diabetics (+50%), and colon cancer screening (+13%). Among those without prior vaccination, influenza vaccine increased by 25% and pneumonia vaccine by 20%.
Discussion
This comprehensive prevention program had short-term benefits for improving adherence to established prevention guidelines in older adults. This low-cost effective program could be disseminated nationwide.
Keywords: prevention, healthy aging, lifestyle interventions, cardiovascular disease, hypertension, diabetes, cancer screening, immunizations
Introduction
Prevention in older adults presents unique challenges. First, although the majority of older adults are nondisabled, as a group they are at high risk for several major disabling, chronic diseases (Hoffman, Rice, & Sung, 1996). Although nondisabled older adults may perceive themselves as being healthy and at low risk, they are actually at high risk for major illnesses and disability on the basis of their age alone. This nondisabled group includes populations with lower education and income who may not be aware of the opportunities for prevention.
Second, it is clear from clinical trials that more intensive therapy, often with medication, is needed to achieve significant risk reduction. Lifestyle modification is fundamentally important, yet it may not result in changes of adequate magnitude to substantially reduce risk. Although lifestyle modification was more effective than medication in older adults in the Diabetes Prevention Program (Diabetes Prevention Program Research Group, 2002), medications are more effective than lifestyle for controlling the cardiovascular risk factors of cholesterol (Shepherd et al., 2002), hypertension (Davis et al., 2002; SHEP Cooperative Research Group, 1991), and osteoporosis (Cummings et al., 1998). This need for medical therapy should be included with lifestyle prevention messages in an efficient and comprehensive manner. Because cardiovascular disease is a major cause of disability in the older population, intensive preventive therapy could potentially reduce disability and increase active life expectancy (Newman & Brach, 2001; Newman, Arnold, et al., 2003; Newman, Gottdiener, et al., 2001).
Third, older adults are at risk for multiple, simultaneous chronic conditions, and the number of conditions is strongly related to the degree of disability; thus an approach focusing on any single condition will probably be ineffective in reducing disability (Beswick et al., 2008; Karlamangla et al., 2007; Newman & Brach, 2001). Many community-based prevention programs focus on shortterm health educational programs that target single risk factors (Barrett & Mensing, 2004; Jones et al., 2008; Kushi et al., 2006; Veazie et al., 2005). These programs often provide general health information rather than specific interventions tailored to reducing overall risk. Finally, it is important for prevention programs to address the challenge of long-term adherence with medical therapies and continued adherence to screening schedules (Dunbar-Jacob et al., 2004; Schlenk, Dunbar-Jacob, & Engberg, 2004).
In partnership with a low-income, high-risk community, we designed a community-based program that addresses all of these factors. The program was developed to target conditions for older adults that contribute to a large proportion of preventable disability based on established effective therapies. The therapies and preventive strategies were based on published research and adapted for a community setting with input from professional and community advisory groups. In this report, we review the impetus for the program and an initial evaluation using well-defined benchmarks of adherence to these preventive interventions.
Method
Design
The prevention program was developed with input from local medical staff and community groups, delivered by health counselors from the community, hired and trained by the University of Pittsburgh's Prevention Research Center, and evaluated in 389 men and women aged 65 and above from McKeesport, Pennsylvania. The evaluation presented here was based on adherence to prevention goals before and after the core intervention. The protocol and consent forms were approved by the Institutional Review Board of the University of Pittsburgh.
The program was designed to target the most common chronic health conditions that contribute to preventable disability, their shared and unique risk factors, and the goals for their management. An initial evaluation of important conditions was conducted by reviewing the published literature regarding the major contributors to disability in older adults (Ettinger et al., 1994; Ferrucci et al., 1996; Hoffman et al., 1996). These papers demonstrate that multiple chronic diseases, including cardiovascular disease, stroke, arthritis, osteoporosis, depression, diabetes, cancer, pneumonia, and other infections, were the major contributors to disability in older adults. Additional surveys (National Health Interview Survey, 2008b) were reviewed to evaluate current levels of adherence to prevention guidelines for these conditions in the region. These findings were presented to local groups of health care workers and community agencies that deal with older adults to develop a consensus surrounding priority health conditions and goals for healthy aging and active life expectancy. Through these activities, significant support and enthusiasm was developed among the lay and medical communities for a comprehensive prevention program targeting older adults in the community.
These concepts and general goals were further refined for the specific program. First, prevention goals were grouped into 10 simple and clear health targets that provided a consistent health message across multiple common medical conditions. The targeted conditions included coronary heart disease and stroke, breast and colon cancer, pneumonia and chronic lung disease, musculoskeletal health (osteoporosis and sarcopenia), and depression. Then, the corresponding risk factor prevention goals were defined and operationalized as follows: (a) blood pressure control (systolic blood pressure, <140 mmHg [Chobanian et al., 2003]), (b) cholesterol control (low-density lipoprotein [LDL] <130 mg/dl [Third Report of the National Cholesterol Education Program, 2002]), (c) glucose control (<110 dl/mg [Expert Committee on the Diagnosis and Classification of Diabetes Mellitus, 1997]), (d) smoking cessation, (e) flu immunization (past year) and pneumonia immunization (ever), (f) breast and colon cancer screening (U.S. Preventive Services Task Force, 2002a, 2002b), (g) osteoporosis screening (Kanis & Gluer, 2000; World Health Organization, 1994) and adequate muscle strength by function testing (five chair stands), (h) maintaining physical activity at least 2.5 hr per week (National Center for Chronic Disease Prevention and Health Promotion, 1996), (i) maintaining social contacts of at least once a week (Heitsmann & Kaplan, 1988), and (j) having few symptoms of depression (score <16 of 60 on a modified Center for Epidemiologic Studies Depression Scale [CES-D]; Orme, Reis, & Herz, 1986). These prevention goals were designated as the “10 Keys to Healthy Aging” (10 Keys). These guidelines have been updated as new guidelines have been published, such as the recommendation that high-risk older adults should have an LDL cholesterol of <100 mg/dl (Grundy et al., 2004).
Participants
The focus of the program was the community of McKeesport, Pennsylvania, which has a population of approximately 25,000, including more than 5,000 individuals aged 65 and older. The community represents an older, high-risk population adversely affected by the closing of the steel mills, with high levels of unemployment, low education, low socioeconomic status, and with substantial out-migration of younger individuals. Program eligibility criteria were designed to select a nondisabled population and included the following: aged 65 or older; not dependent on a cane or a walker; self-report of no difficulty walking one quarter of a mile and one flight of steps; no difficulty getting out of a bed or a chair, bathing, dressing, eating, or toileting; no cancer under active treatment excluding nonmelanoma skin cancer and maintenance adjuvant treatment such as tamoxifen; and no plans to move outside of western Pennsylvania in the next 2 years. We also required participation in Medicare Part A or B, a Medicare Health Maintenance Organization, or some other form of medical insurance so that services recommended could be accessed.
We initially recruited volunteers who were reached via media advertisements and community health promotion events. To increase participation, this was followed by a direct mail campaign using a recent voter registration list to a random sample of 10,388 community residents over age 65. For the direct mail campaign, a letter describing the study with a detachable return card was mailed to the resident's home. Residents could send back a card refusing further contact or asking for a telephone screening (n = 812). For those not returning this card, the letter informed them that a telephone follow-up would be conducted, with at least one and up to three telephone follow-up calls. For both the volunteer and the random sample groups, the initial telephone screening included assessment of health status and eligibility of the respondent and any age-eligible household members. These efforts resulted in a total of 417 participants enrolled in the program, including 93 household pairs. Of the 324 households, 94 were volunteers from advertising, 224 sent back cards following a mailing, and the remaining 6 were recruited by follow-up phone calls. There were 28 who dropped out without completing the follow-up assessment, leaving 389 participants in the evaluation. There was no significant difference in the number—12 (11.4%) versus16 (5.1%)—or in the characteristics of the dropouts in the volunteers (n = 93) versus those recruited from the random sample (n = 296), but nonsignificant trends suggested a greater proportion of men, smokers, and lower education groups in the random sample.
Measurements
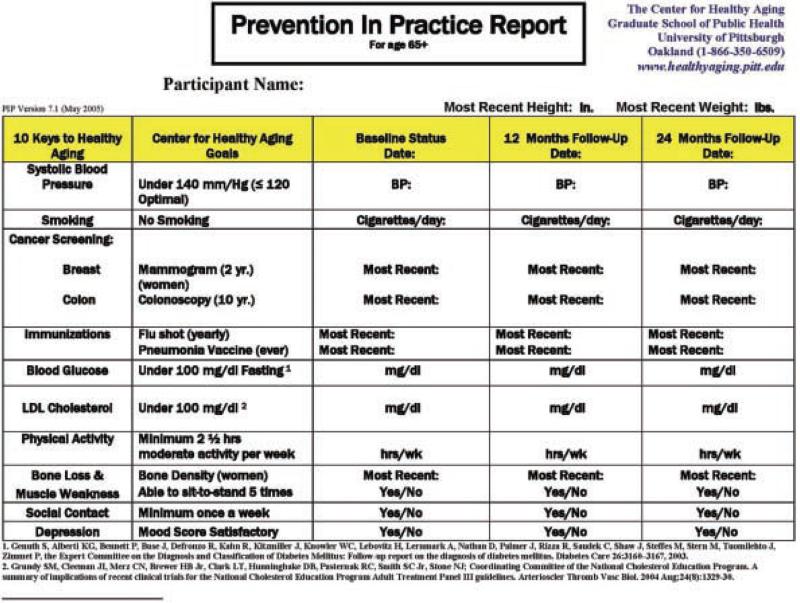
Participants were interviewed at home after informed consent was obtained and eligibility was confirmed. The clinical assessment at baseline assessed current health conditions along with current use of health preventive practices; history of high blood pressure, high cholesterol, or diabetes; smoking history; recent vaccines; and cancer screening history. Information on medication names, dosage, and adherence was collected and coded. Blood pressure was measured twice and averaged using a standard mercury sphygmomanometer. Weight and height were measured in light clothing without shoes. Current physical activity was assessed using the Modified Activity Questionnaire (Kriska, & Caspersen, 1997); physical function was assessed using standard questionnaires assessing activities of daily living (Fried et al., 1991; Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963) and mobility (Simonsick et al., 2001). Gait speed, standing balance, and chair stand time were assessed and summarized using the short physical performance battery (Guralnik, Ferrucci, Simonsick, Salive, & Wallace, 1995). Fasting serum glucose and total and LDL cholesterol were assessed by a local clinical laboratory. Depression symptoms were assessed using the CES-D questionnaire (Orme et al., 1986). Social contact was measured by the number of contacts a participant had per week (Heitsmann & Kaplan, 1988). An in-person, follow-up evaluation was conducted after 12 months, repeating the baseline assessments. This information was used to create an individualized summary of the initial level of adherence to prevention goals. This summary was named the Prevention in Practice Report. Figure 1 illustrates a current version of this report that illustrates more recent targets of glucose and cholesterol (Genuth et al., 2003; Grundy et al., 2004).
Figure 1.
Prevention in Practice (PIP) Report—10 Keys to Healthy Aging Program, Center for Healthy Aging, McKeesport, PA, 2004 Adapted from Genuth et al. (2003) and Grundy et al. (2004).
Program Intervention
After the initial evaluation, each participant in the program met individually with a health counselor from the University of Pittsburgh's Prevention Research Center. This interaction lasted approximately 15 to 30 min with the purpose of reviewing his or her Prevention in Practice Report and to identify the keys that required action. Because many participants required simultaneous risk reduction efforts and to engage the participant in establishing his or her own prevention goals, the counselor assisted the participant with prioritizing key health areas that required action. Potential strategies discussed included both lifestyle and medical intervention for maximum risk reduction. Strategies to promote behavior change, including knowledge acquisition, skills development, social support, and self-monitoring, were used to develop an action plan. Subsequently, action plans were discussed and modified as necessary by the health counselor and participant via telephone follow-ups or in-person visits conducted every 3 months to promote long-term adherence.
The time for the baseline evaluation specific to the 10 keys was about 30 min at baseline and 15 to 30 min at each follow-up for a total of about 1.5 evaluation hours per person. The intervention time was about 30 to 45 min at baseline and 15 to 30 min at each of four quarterly follow-ups for a total of about 2 hr intervention time or about 3.5 hr per participant over the course of a year. As one of the primary strategies to improve adherence, participants were encouraged to take the Prevention in Practice Report to their physician and solicit his/her support in addressing these goals.
Monthly calls were made to participants with systolic blood pressure greater than 160 mmHg (Chobanian et al., 2003) and blood glucose >130 (Expert Committee on the Diagnosis and Classification of Diabetes Mellitus, 1997), to those with a positive depression screening score (American Geriatrics Society & American Association for Geriatric Psychiatry, 2003), to those with no current physical activity (Nelson et al., 2007), or who were currently smoking. These calls ensured that they had sought medical care. Participants with no regular primary care physician were encouraged to make an appointment with a physician from a list provided by the local medical society and hospital. Participants with difficulty obtaining or adhering to prescribed medications were provided with additional information on prescription medication benefits and strategies for better adherence. These calls were continued on a monthly basis until these medical issues were resolved and subsequently then continued at least every 3 months for the remainder of the year.
The intervention program was conducted by health counselors recruited from the community with at least a bachelor-level training in health education, nutrition, or exercise science with standardized training in research assessment methods and behavior change techniques (Botelho & Skinner, 1995). Additional health counselor training in behavior change methodology was provided by our own faculty.
Data Analysis
Data were compared using means and t tests for continuous variables or proportions and chi-squared tests for categorical variables. Mean differences and mean changes were evaluated before and after intervention, using overall values for baseline, follow-up, and change. Only participants with data at both time points are included in the analyses. All analyses were conducted using SAS version 9.1 (Cary, NC).
Results
The 389 participants who completed the outcome evaluation were characterized as to their demographic characteristics and baseline health status (Table 1). The mean age was 74 years; 60% were women. The majority were married with at least a high school education or higher. The prevalence of major chronic disease was substantial, with about half reporting hypertension, a quarter having coronary artery disease, and 12% having diabetes.
Table 1.
Baseline Characteristics of the Demonstration Project Participants (Center for Healthy Aging, McKeesport, PA, 2004)
| Characteristic | M (SD), range |
|---|---|
| Age (y) | 73.9 (5.4), 65-91 |
| Gender | n (%) |
| Men | 158 (40,6) |
| Women | 231 (59.38) |
| Race | |
| White | 369 (94.9) |
| Black | 20 (5.1) |
| Educational attainment | |
| Less than high school | 31 (8.2) |
| High school | 184 (48.5) |
| Greater than high school | 164 (43,3) |
| Marital status | |
| Single | 21 (5.4) |
| Married | 233 (59.9) |
| Separated | 5 (1.3) |
| Divorced | 14 (3.6) |
| Widowed | 116 (29.8) |
| Self-reported health status | |
| Excellent | 49 (12.6) |
| Very good | 143 (36.7) |
| Good | 159 (40.9) |
| Fair | 38 (9.8) |
| Poor | 0 (0.0) |
| Smoking status | |
| Current smoker | 18 (4.6) |
| Past smoker | 177 (47.7) |
| Hypertension | 194 (49.9) |
| Coronary heart diseasea | 88 (22,6) |
| Stroke | 28 (7.2) |
| Diabetes | 45 (11.6) |
| Blood pressure | M (SD), range |
| Systolic (mmHg) | 130.5 (16.2), 90.5-207.0 |
| Diastolic (mmHg) | 71.5 (10.1), 40.0-96.0 |
| Fasting blood glucose (mg/dL) | 97.6 (22.6). 66.0-236.0 |
| LDL cholesterol (mg/dL) | 116.3 (34.3), 40.0-243.0 |
| Body mass index (kg/m1) | 28.3 (4.7), 17.5-45.7 |
LDL = low-density lipoprotein.
Defined as a reported diagnosis of myocardial infarction (MI), angina, Coronary Artery Bypass Graft (CABG), cardiac stent, or angioplasty.
At baseline, the overall percentage of individuals with adherence to the 10 Keys recommendations was fairly high (Table 2). More than 90% were socially active and nonsmokers. More than 80% had normal fasting blood glucose and normal (low) depression scores. Rates of breast cancer screening and annual flu vaccination exceeded 75%. Cardiovascular risk factors were less well controlled, with less than half having recommended levels of LDL cholesterol, 72% with acceptable systolic blood pressure, and 60% meeting physical activity recommendations. Among participants with diabetes, 24% had blood glucose <110 mg/dl, and among those with hypertension, 59% had systolic blood pressure <140 mmHg. Only 59% of women reported having been screened for osteoporosis, and 69% reported a previous pneumonia immunization.
Table 2.
Percentage of Participants Achieving 10 Keys at Baseline, 12-Month Fol low-Up, and Change (Center for Healthy Aging, McKeesport, PA, 2004)
|
N = 389 |
|||||
|---|---|---|---|---|---|
| Key and goals | Total N | Baseline, n (%) | Follow-up, n (%) | Relative improvement | Absolute difference |
| Control systolic blood pressure to less than 1-40 mmHg | |||||
| All participants | 388 | 281 (72%) | 303 (73%) | +8%* | |
| Subgroup with hypertension at baseline | 262 | 155 (59%) | 182 (69%) | +17%** | |
| Stop smoking | 389 | 371 (95%) | 371 (95%) | <l% | |
| Participate in cancer screenings | |||||
| Mammogram | 225 | 183 (31%) | 181 (80%) | –1% | |
| Colonoscopy | 364 | 190 (52%) | 215 (59%) | +13% | |
| Get regular immunizations | |||||
| Influenza vaccine | 385 | 314 (32%) | 296 (77%) | –6%* | |
| Subgroup with no influenza vaccine at baseline | 71 | 0 (0%) | 18 (25%) | +25% | |
| Pneumonia vaccine | 371 | 256 (69%) | 279 (75%) | +8%*** | |
| Subgroup with no pneumonia vaccine at baseline | 115 | 0 (0%) | 23 (20%) | +20% | |
| Regulate diabetes: Blood glucose to less than 110 mg/dl | |||||
| All participants | 371 | 319 (36%) | 316 (85%) | –1% | |
| Subgroup with diabetes at baseline | 51 | 12 (24%) | 18 (35%) | +50% | |
| Lower LDL cholesterol to less than 100 mg/dl | |||||
| All participants | 371 | 118 (32%) | 169 (46%) | +43%*** | |
| Subgroup with history of coronary heart disease | 97 | 47 (48%) | 67 (69%) | +43%*** | |
| Subgroup with baseline LDL cholesterol > 130 mg/dl | 124 | 0 (0%) | 24 (19%) | +19% | |
| Be physically active at least 2.5 hr per week | 389 | 247 (63%) | 267 (69%) | +7% | |
| Prevent bone loss and muscle weakness | |||||
| Bone density screen | 383 | 227 (59%) | 236 (62%) | +4%*** | |
| Able to rise from chair | 383 | 383 (98%) | 365 (94%) | –5%*** | |
| Maintain social contact at least once per week | 389 | 387 (99%) | 387 (99%) | <l% | |
| Combat depression | |||||
| No depression on screening | 389 | 345 (39%) | 354 (91%) | +3% | |
LDL = low-density lipoprotein.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Overall, improvement in adherence to the 10 Keys was seen for several important goals (Table 2). Improvement was greatest for lipid lowering with a relative improvement of 43% in the whole group. This degree of improvement was also seen in the subgroup of participants with a history of coronary heart disease or a history of LDL cholesterol >130 mg/dl at baseline. Participants with hypertension had a statistically significant 17% improvement in the proportion achieving blood pressure control, and those with diabetes had a nonsignificant 50% improvement in achieving blood glucose control. For cancer screening, we were able to increase the use of colonoscopy by 13%, but this was not statistically significant. Breast cancer screening rates were high and not significantly changed at 1 year of follow-up.
An 8% improvement in pneumonia immunization was also achieved, whereas overall influenza vaccine rate was a little lower. This was due in part to a delay in the provision of influenza vaccination in the subsequent year. Improvement in vaccination rates was more dramatic when looking at the subgroups who did not report influenza vaccine in the past year or who never had a pneumonia vaccine, where we were able to achieve prevention goals in 18/71 individuals for influenza (25% increase) and 23/115 new individuals who received a pneumonia vaccine (20% increase). Improvements were not noted for bone density screening or for muscle strength, defined as the ability to rise from a chair five times. Ability to perform the chair stand task actually decreased over 12 months, consistent with the tendency for older adults to lose function over time.
There were a few individuals whose evaluation revealed values of risk factors that warranted more frequent contact (Table 3). Fourteen (3.6%) individuals had systolic blood pressure >160 mmHg, and 26 (6.7%) had uncontrolled blood glucose (fasting glucose >130), whereas 44 (11.3%) had levels of depressive symptoms that warranted referral to their physician (CES-D score ≤16). A few reported no physical activity (36, 10.1%) or current smoking (18, 4.6%). As planned in the design of the program, these individuals were contacted monthly until these issues were resolved. A majority of individuals improved and a substantial minority reached targeted 10 key goals. Once improved, they were contacted every 3 months along with the other participants to maintain engagement and motivation toward healthy aging goals.
Table 3.
Subgroup Targeted for More Intensive Follow-Up With Monthly Telephone Call: 12 Month Outcomes
| 12 month results |
|||
|---|---|---|---|
| Any improvementa |
Improved to 10 Key goal |
||
| Indication for monthly telephone call | N (%) | n (%) | n (%) |
| Systolic blood pressure > 160 mmHg | 14 (3.6) | 11 (79.6) | 4 (28.6) |
| Fasting blood sugar > 130 mg/dl | 26 (6.7) | 15 (57.7) | 7 (25.0) |
| No physical activity | 39 (10.1) | 19 (48.7) | 10 (25.6) |
| Current smoker | 18 (4.6) | 1 (5.6) | 1 (5.6) |
| Depression (CES-D ≥ 16) | 44 (11.3) | 29 (65.9) | 29 (65.9) |
CES-D = Center for Epidemiologic Studies-Depress ion Scale.
Improvement was defined as no longer exceeding a level indicating need for monthly follow-up in the subgroup with an indication.
Discussion
This project showed that well-functioning older adults in the community were not meeting several important prevention goals, especially in the area of cardiovascular risk factor control. Areas of greatest improvement included control of cardiovascular risk factors and increased use of the pneumonia vaccine. We were successful in improving the proportion meeting recommended goals for LDL cholesterol and for hypertension control. Cancer screening rates varied by cancer type. We were most successful with increasing the use of colonoscopy for colon cancer screening.
It is important to recognize that these improvements were achieved in spite of fairly good adherence to preventive health practice in the program participants at the baseline. For example, influenza vaccine rates were 82% compared to 65% in the 2003-2004 National Health Interview Survey (2008a). Similarly, 69% of our group had reported a pneumonia vaccine compared to 56% nationally. Rates of smoking were only 5%, much lower than the 9% prevalence in Pennsylvania for the 65+ population (Behavioral Risk Factor Surveillance System, 2008a). Though the population recruited had a higher socioeconomic status than the community at large, substantial needs were recognized and improvements achieved.
Levels of physical activity were slightly improved but remained suboptimal, consistent with recent reports (Behavioral Risk Factor Surveillance System, 2008b). Goals were not improved in several areas, and in fact, there were documented declines in physical performance over the 12 months, with fewer maintaining the ability to complete the challenge task of rising from a chair repeatedly. The decline in function may reflect the fact that the usual progression of function in the population above age 65 is one of decline. Prevention of this decline will likely require interventions that are more aggressive than were offered in our program. Although we were not able to provide more intensive interventions with the resources available for this project, other studies have shown short-term benefit from more intensive programs (Rejeski et al., 2005), but no program has been tested for a sustained period of time. More intensive intervention and greater attention to adherence are likely to be necessary to improve physical activity adherence to sufficiently impact disability prevention in the long term (Rejeski et al., 2005).
Though this was a nondisabled population, the prevalence of major chronic diseases was in line with national surveys (National Health Interview Survey, 2008b) for this age group, emphasizing the need for aggressive risk factor management in well-functioning older adults. We identified a few individuals with risk factors levels that were far worse than recommended goals and were able to move them closer to goals. Greater success in controlling LDL cholesterol to recommended levels would require more emphasis on lipid-lowering medication. In addition, more attention to the harmful consequences of poorly controlled blood pressure might motivate the public and the medical community to push for tighter blood pressure control. Sodium reduction, although an effective strategy to lower blood pressure, will be very difficult to achieve because of the high sodium content of prepared foods. Policy makers would need to impose regulations on the food industry to produce healthy lower sodium foods at competitive prices. This trend is currently gaining momentum in Europe (Asaria, Chisholm, Mathers, Ezzati, & Beaglehole, 2007).
Many participants did not have knowledge of their risk factor status, know what their prevention goals should be, or understand the importance of maintaining lower levels of risk factors for long-term health. Sometimes the participants commented that they had been told their risk factors levels were good for their age, in other words, discounting the potential to do better and giving a false sense of security. Our findings suggest that people need and can benefit from much better health education regarding prevention and more information regarding their personal health risk. The Prevention in Practice Report, which combines both personal risk as well as recommended goals, may provide a useful tool to educate and empower older individuals to reach personal goals and to potentially help others in the community to do so as well. Counseling, assessment, and close follow-up of participants by health educators were effective in improving adherence to these study guidelines. The program involved approximately 3-4 total evaluation and intervention contact hours per participant. This may be a cost-effective approach for stimulating preventive health services in the community as long as adequate quality medical services are available to provide the recommended pharmacologic treatment and testing. The Area Agency on Aging, managed care organizations, Medicare programs, and voluntary agencies such as the American Association of Retired People are attempting to integrate more preventive services into their programs. Integration of the 10 Keys approach into these programs is probably an important step toward that goal.
Unfortunately, in recent years, longitudinal epidemiological studies such as the Cardiovascular Health Study (Psaty et al., 1992, 1993) and the Health, Aging, and Body Composition Study (Franse et al., 2001; Resnick, Shorr, Kuller, Franse, & Harris, 2001) have documented both the very high prevalence of undiagnosed disease (Chaves, Kuller, O'Leary, Manolio, & Newman, 2004) among older individuals and also the strong association between undiagnosed subclinical disease and subsequent morbidity and disability (Newman, Arnold, et al., 2003). Prevention of the conversion of undiagnosed subclinical to clinical disease and disability must be a very high priority to enhance active life expectancy and to potentially moderate rising health care costs for older individuals. These prevention programs, as noted, must be both broad based and intensive using both pharmacological and nonpharmacological approaches and include support to reinforce optimal adherence.
Many older individuals and some physicians still do not believe that preventive programs should be a priority. Ongoing efforts are needed, including continuing to market the concepts of prevention to both the medical and lay communities in collaboration with community organizations and health departments. However, it is obvious that it will take a considerable amount of effort to change the paradigm of medical care to emphasize prevention and active life expectancy, especially in low-income, high-risk populations.
The comprehensive nature of this program and its foundation in wellestablished clinical practice guidelines are strengths. Although the participation from the community at large was low, our aggressive efforts to contact and recruit every person in the sampling frame by mail and then telephone is likely to have resulted in a more representative group than would have been identified by enrolling participants from senior centers or other existing programs. As noted above, this group had lower rates of smoking and higher rates of immunization compared to national surveys, suggesting that other approaches need to be developed to further engage those at highest risk into these programs. The pre–post design of the evaluation is a limitation but provides evidence of benefit. The resources for dietary and activity interventions were limited and are not emphasized here but were applied to a random subset of the cohort and will be reported separately. This was a community program evaluation and not a randomized clinical trial; thus we cannot determine whether changes might be due to secular trends. Finally, the follow-up reported here was for only the first 12 months. Longer term follow-up may show continued improvement.
Conclusion
Comprehensive preventive health programs for older individuals in the community can lead to improvements in diverse indicators of preventive health. Ongoing monitoring and follow-up efforts are needed to maximize adherence. Prevention programs for older individuals must be based on results of prior scientific studies of efficacy of the intervention to reduce morbidity, disability, and mortality. Single disease prevention programs or single modality interventions can be replaced by comprehensive programs such as this one that incorporate screening, immunizations, and incorporate both behavioral and pharmacological approaches that recognize the importance of long-term adherence to reduce risk. Efforts to reach more individuals at high risk should remain a top priority. The primary goal of prevention should be to maximize quality of life and active life expectancy. Empowering older individuals to know their own risk factor status and to understand the importance of screening, immunization, and lifestyle and medication should maximize the quality of their health. The translation of the 10 Keys—a low cost but effective approach—to other community settings could successfully impact health quality.
Acknowledgments
Funding The authors received no financial support for the research and/or authorship of this article.
The University of Pittsburgh's Center for Healthy Aging is a member of the Prevention Research Centers Program, supported by the Centers for Disease Control and Prevention cooperative agreement number 1 U48 DP000025.
Footnotes
Declaration of Conflicting Interests The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
References
- American Geriatrics Society & American Association for Geriatric Psychiatry The American Geriatrics Society and American Association for Geriatric Psychiatry recommendations for policies in support of quality mental health care in U.S. nursing homes. Journal of the American Geriatrics Society. 2003;51:1299–1304. doi: 10.1046/j.1532-5415.2003.51416.x. [DOI] [PubMed] [Google Scholar]
- American Geriatrics Society & American Association for Geriatric Psychiatry The American Geriatrics Society and American Association for Geriatric Psychiatry recommendations for policies in support of quality mental health care in U.S. nursing homes. Journal of the American Geriatrics Society. 2003;51:1299–1304. doi: 10.1046/j.1532-5415.2003.51416.x. [DOI] [PubMed] [Google Scholar]
- Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: Health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007;370:2044–2053. doi: 10.1016/S0140-6736(07)61698-5. [DOI] [PubMed] [Google Scholar]
- Barrett EJ, Mensing C. The American Diabetes Association, the American Cancer Society, and the American Heart Association: A triumvirate of hope for the nation's health. Diabetes Care. 2004;27:1789–1790. doi: 10.2337/diacare.27.7.1789. [DOI] [PubMed] [Google Scholar]
- Behavioral Risk Factor Surveillance System [January 31, 2008];Cigarette smoking by state, 1993-2006. National Center for Health Statistics, Trends in Health and Aging. 2008a from http://www.cdc.gov/nchs/agingact.htm.
- Behavioral Risk Factor Surveillance System [January 31, 2008];Physical activity by state, 1994-2006. National Center for Health Statistics, Trends in Health and Aging. 2008b from http://www.cdc.gov/nchs/agingact.htm.
- Beswick AD, Rees K, Dieppe P, Ayis S, Gooberman-Hill R, Horwood J. Complex interventions to improve physical function and maintain independent living in elderly people: A systematic review and meta-analysis. Lancet. 2008;371:725–735. doi: 10.1016/S0140-6736(08)60342-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botelho RJ, Skinner H. Motivating change in health behavior. Implications for health promotion and disease prevention. Primary Care. 1995;22:565–589. [PubMed] [Google Scholar]
- Chaves PH, Kuller LH, O'Leary DH, Manolio TA, Newman AB. Cardiovascular Health Study. Subclinical cardiovascular disease in older adults: Insights from the Cardiovascular Health Study. American Journal of Geriatric Cardiology. 2004;13:137–151. doi: 10.1111/j.1076-7460.2004.02120.x. [DOI] [PubMed] [Google Scholar]
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- Cummings SR, Black DM, Thompson DE, Applegate WB, Barret-Connor E, Musliner TA, et al. Effects of alendronate on risk of fracture in women with low bone density but without vertebral fractures: Results from the Fracture Intervention Trial. Journal of the American Medical Association. 1998;280:2077–2082. doi: 10.1001/jama.280.24.2077. [DOI] [PubMed] [Google Scholar]
- Davis BR, Cutler JA, Furberg CD, Wright JT, Jr., Farber MA, Felicetta JV, et al. Relationship of antihypertensive treatment regimens and change in blood pressure to risk for heart failure in hypertensive patients randomly assigned to doxazosin or chlorthalidone: Further analyses from the antihypertensive and lipidlowering treatment to prevent heart attack trial. Annals of Internal Medicine. 2002;137:313–320. doi: 10.7326/0003-4819-137-5_part_1-200209030-00006. [DOI] [PubMed] [Google Scholar]
- Diabetes Prevention Program Research Group Reduction in the incidence of Type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunbar-Jacob J, Holmes JL, Sereika S, Kwoh CK, Burke LE, Starz TW, et al. Factors associated with attrition of African Americans during the recruitment phase of a clinical trial examining adherence among individual with rheumatoid arthritis. Arthritis Rheumatism. 2004;51:422–428. doi: 10.1002/art.20411. [DOI] [PubMed] [Google Scholar]
- Ettinger WH, Jr., Fried LP, Harris T, Shemanski L, Schulz R, Robbins J, et al. Self-reported causes of physical disability in older people: The Cardiovascular Health Study. Journal of the American Geriatrics Society. 1994;42:1035–1044. doi: 10.1111/j.1532-5415.1994.tb06206.x. [DOI] [PubMed] [Google Scholar]
- Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997;20:1183–1197. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- Ferrucci L, Guralnik JM, Simonsick E, Salive ME, Corti C, Langlois J. Progressive versus catastrophic disability: A longitudinal view of the disablement process. Journals of Gerontology, Series A: Biological Sciences and Medical Sciences. 1996;51A:M123–M130. doi: 10.1093/gerona/51a.3.m123. [DOI] [PubMed] [Google Scholar]
- Franse LV, Dibari M, Shorr RI, Resnick HE, van Eijk JTM, Bauer DC, et al. Type 2 diabetes in older well functioning people: Who is undiagnosed? Data from the Health, Aging and Body Composition Study. Diabetes Care. 2001;24:2065–2070. doi: 10.2337/diacare.24.12.2065. [DOI] [PubMed] [Google Scholar]
- Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, et al. The Cardiovascular Health Study: Design and rationale. Annals of Epidemiology. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- Genuth S, Alberti KG, Bennett P, Buse J, Defronzo R, Kahn R, et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26:3160–3167. doi: 10.2337/diacare.26.11.3160. [DOI] [PubMed] [Google Scholar]
- Grundy SM, Cleeman JI, Merz CN, Brewer HB, Jr., Clark LT, Hunninghake DB. A summary of implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Arteriosclerosis, Thrombosis, and Vascular Biology. 2004;24:1329–1330. doi: 10.1161/01.ATV.0000139012.45265.e0. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. New England Journal of Medicine. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heitsmann CA, Kaplan RM. Assessment of methods for measuring social support. Health Psychology. 1988;7:75–109. doi: 10.1037//0278-6133.7.1.75. [DOI] [PubMed] [Google Scholar]
- Hoffman C, Rice D, Sung HY. Persons with chronic conditions. Their prevalence and costs. Journal of the American Medical Association. 1996;276:1473–1479. [PubMed] [Google Scholar]
- Jones DW, Peterson ED, Bonow RO, Masoudi FA, Fonarow GC, Smith SC, Jr., et al. Translating research into practice for healthcare providers, the American Heart Association's strategy for building healthier lives, free of cardiovascular diseases and strokes. Circulation. 2008;118:687–696. doi: 10.1161/CIRCULATIONAHA.108.189934. [DOI] [PubMed] [Google Scholar]
- Kanis JA, Gluer CC. An update on the diagnosis and assessment of osteoporosis with densitometry. Osteoporosis International. 2000;11:192–202. doi: 10.1007/s001980050281. [DOI] [PubMed] [Google Scholar]
- Karlamangla A, Tinetti M, Guralnik J, Studenski S, Wetle T, Reuben D. Comorbidity in older adults: Nosology of impairment, diseases, and conditions. Journals of Gerontology, Series A: Biological Sciences and Medical Sciences. 2007;62A:296–300. doi: 10.1093/gerona/62.3.296. [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. Journal of the American Medical Association. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Kriska AM, Caspersen CJ. Introduction to the collection of physical activity questionnaires. In A Collection of Physical Activity Questionnaires for Health-Related Research. Medicine and Science in Sports and Exercise. 1997;29:S5–S9. S73–S78. [PubMed] [Google Scholar]
- Kushi LH, Byers T, Doyle C, Bandera EV, McCullough M, McTiernan A, et al. American Cancer Society Guidelines on Nutrition and Physical Activity for cancer prevention: Reducing the risk of cancer with healthy food choices and physical activity. CA: A Cancer Journal for Clinicians. 2006;56:254–281. doi: 10.3322/canjclin.56.5.254. [DOI] [PubMed] [Google Scholar]
- National Center for Chronic Disease Prevention and Health Promotion Notice to readers publication of surgeon general's report on physical activity and health. MMWR Morbidity and Mortality Weekly Report. 1996;45:591–592. [Google Scholar]
- National Health Interview Survey [January 31, 2008];Influenza, and pneumonia vaccinations by age, sex, and race/ethnicity: United States, 1993-1995, 1997-2006. National Center for Health Statistics, Trends in Health and Aging. 2008a from http://www.cdc.gov/nchs/agingact.htm.
- National Health Interview Survey [January 31, 2008];Prevalence of selected chronic conditions by age, sex, and race/ethnicity: United States, 1997-2006. National Center for Health Statistics, Trends in Health and Aging. 2008b from http://www.cdc.gov/nchs/agingact.htm.
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- Newman AB, Brach JS. The gender gap in longevity and disability in older persons. Epidemiologic Reviews. 2001;23:343–350. doi: 10.1093/oxfordjournals.epirev.a000810. [DOI] [PubMed] [Google Scholar]
- Newman AB, Arnold AM, Naydeck BL, Fried LP, Burke GL, Enright P, et al. “Successful aging”: Impact of subclinical cardiovascular disease. Archives of Internal Medicine. 2003;163:2315–2322. doi: 10.1001/archinte.163.19.2315. [DOI] [PubMed] [Google Scholar]
- Newman AB, Gottdiener JS, McBurnie MA, Hirsch CH, Kop WJ, Tracy R, et al. Associations of subclinical cardiovascular disease with frailty. Journals of Gerontology, Series A: Biological Sciences and Medical Sciences. 2001;56A:M158–M166. doi: 10.1093/gerona/56.3.m158. [DOI] [PubMed] [Google Scholar]
- Orme J, Reis J, Herz E. Factorial and indiscriminate validity of the center for epidemiological studies depression (CES-D) scale. Journal of Clinical Psychology. 1986;42:28–33. doi: 10.1002/1097-4679(198601)42:1<28::aid-jclp2270420104>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- Psaty BM, Furbergm CD, Kullerm LH, Borhani NO, Rautaharjum PM, O'Learym DH, et al. Isolated systolic hypertension and subclinical cardiovascular disease in the elderly. Journal of the American Medical Association. 1992;288:1287–1291. [PubMed] [Google Scholar]
- Psaty BM, Savage PJ, Tell GS, Polak JF, Hirsch CH, Gardin JM, et al. Temporal patterns if antihypertensive medication use among elderly patients: The Cardiovascular Health Study. Journal of the American Medical Association. 1993;270:1837–1841. [PubMed] [Google Scholar]
- Rejeski WJ, Fielding RA, Blair SN, Guralnik JM, Gill TM, Hadley EC, et al. The Lifestyle Interventions and Independence for Elders (LIFE) Pilot Study: Design and methods. Contemporary Clinical Trials. 2005;26:141–154. doi: 10.1016/j.cct.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Resnick HE, Shorr RI, Kuller L, Franse L, Harris TB. Prevalence and clinical implications of American Diabetes Association–defined diabetes and other categories of glucose dysregulation in older adults: The Health, Aging and Body Composition Study. Journal of Clinical Epidemiology. 2001;54:869–876. doi: 10.1016/s0895-4356(01)00359-6. [DOI] [PubMed] [Google Scholar]
- Schlenk EA, Dunbar-Jacob J, Engberg S. Medication non-adherence among older adults: A review of strategies and interventions for improvement. Journal of Gerontological Nursing. 2004;30:33–43. doi: 10.3928/0098-9134-20040701-08. [DOI] [PubMed] [Google Scholar]
- SHEP Cooperative Research Group Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the systolic hypertension in the elderly program (SHEP). Journal of the American Medical Association. 1991;265:3255–3264. [PubMed] [Google Scholar]
- Shepherd J, Blauw GJ, Murphy MB, Bollen ELEM, Buckley BM, Cobbe SM, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): A randomized controlled trial. Lancet. 2002;360:1623–1630. doi: 10.1016/s0140-6736(02)11600-x. [DOI] [PubMed] [Google Scholar]
- Simonsick EM, Newman AB, Nevitt MC, Kritchevsky SB, Ferrucci L, Guralnik JM, et al. Measuring higher level physical function in wellfunctioning older adults: Expanding familiar approaches in the Health ABC Study. Journals of Gerontology, Series A: Biological Sciences and Medical Sciences. 2001;56A:M644–M649. doi: 10.1093/gerona/56.10.m644. [DOI] [PubMed] [Google Scholar]
- Third report of the National Cholesterol Education Program (NCEP) Expert panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force . Screening for breast cancer: Recommendations and rationale. Agency for Healthcare Research and Quality; Rockville, MD: 2002a. [Google Scholar]
- U.S. Preventive Services Task Force Screening for colorectal cancer: Recommendations and rationale. Annals of Internal Medicine. 2002b;137:129–131. doi: 10.7326/0003-4819-137-2-200207160-00003. [DOI] [PubMed] [Google Scholar]
- Veazie MA, Galloway JM, Matson-Koffman D, LaBarthe DR, Brownstein JN, Emr M. Taking the initiative: Implementing the American Heart Association Guide for improving cardiovascular health at the community level: Healthy People 2010 Heart Disease and Stroke Partnership Community Guideline Implementation and Best Practices Workgroup. Circulation. 2005;112:2538–2554. doi: 10.1161/CIRCULATIONAHA.105.169179. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Assessment of fracture risk and its application to screening for postmenopausal osteoporosis (Technical Report Series 843) Author; Geneva: 1994. [PubMed] [Google Scholar]