Abstract
The ingestion of ethylene glycol results in toxicity with characteristic chemical, pathological, and imaging findings. In the case presented, magnetic resonance imaging demonstrated bilateral symmetric hyperintensity within the basal ganglia, thalami, and brainstem. Ethylene glycol toxicity also resulted in restricted diffusion within the white matter tracts of the corona radiata, a finding not previously described in the literature. In the acute clinical setting, ethylene glycol toxicity is an important differential consideration of the pathologies involving the deep grey matter nuclei.
Abbreviations: ADC, apparent diffusion coefficient; CT, computed tomography; DWI, diffusion-weighted images; FLAIR, fluid attenuation inversion recovery; MRI, magnetic resonance imaging; T2WI, T2-weighted images
Introduction
The ingestion of ethylene glycol, an organic solvent used in common household products such as automotive antifreeze and paints, results in toxicity with characteristic chemical, pathological, and imaging findings.
Case Report
A 20-year-old male presented to the emergency department following increasing lethargy and emesis over a twelve hour period. At presentation, the patient's Glasgow coma scale score was 6. Arterial blood gas demonstrated a pH of 6.96, pCO2 25 mm Hg, pO2 225 mm Hg and HCO3 5 mmol/L. The serum osmolality was 337 mmol/L and the osmolality gap was markedly elevated at 32 mmol/L. Microscopic examination of the urine demonstrated cigar and envelope shaped crystals characteristic of calcium oxalate crystals (Figure 1). Based on the clinical picture, laboratory findings and microscopic examination of the urine, the diagnosis of ethylene glycol toxicity was confirmed.
Figure 1.
Urine microscopy demonstrates “cigar” and “envelope” crystals, a pattern characteristic of calcium oxalate monohydrate and calcium oxalate dihydrate crystals respectively.
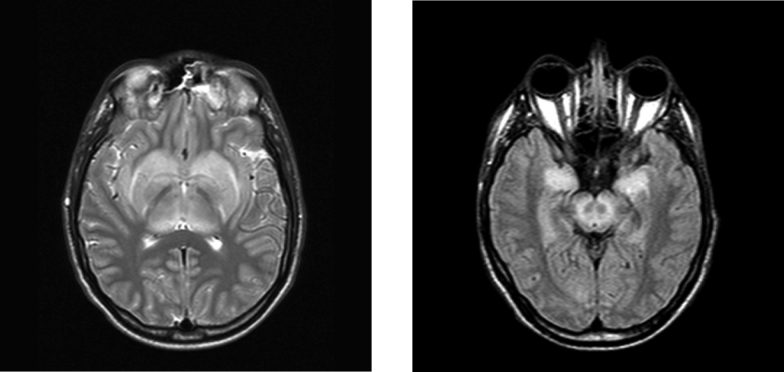
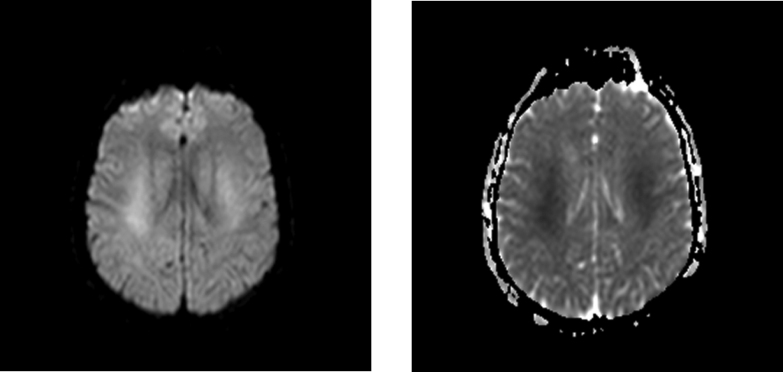
The patient was transferred to the intensive care unit for mechanical respiratory support, fluid management, and hemodialysis. Arterial blood gases were monitored from initial presentation through normalization. pO2 levels ranged from 225 mm Hg (elevated due to supplemental oxygen administration as part of resuscitation) to 84 mm Hg (normal at 36 hours into management). No hypoxic or anoxic periods were demonstrated during hospitalization. Due to clinical concern for seizure activity, head computed tomography (CT) was performed which showed diffuse hypodensity within the bilateral basal ganglia and thalami with loss of differentiation with the subjacent white matter, compatible with edema (Figure 2). For further evaluation, magnetic resonance imaging (MRI) was performed (day one of hospitalization) which demonstrated increased signal intensity on T2 and fluid attenuation inversion recovery (FLAIR) sequences within the basal ganglia, thalami, amygdala, hippocampus, and brainstem bilaterally (Figure 3). There was restricted diffusion within the white matter tracks of the corona radiata bilaterally (Figure 4) on diffusion weighted (DWI) and apparent diffusion coefficient (ADC) imaging. On completion of the medical treatment seven days later, the patient's minimental status exam was normal with a score of 27. As the patient's symptoms had resolved, no further imaging was clinically indicated.
Figure 2.
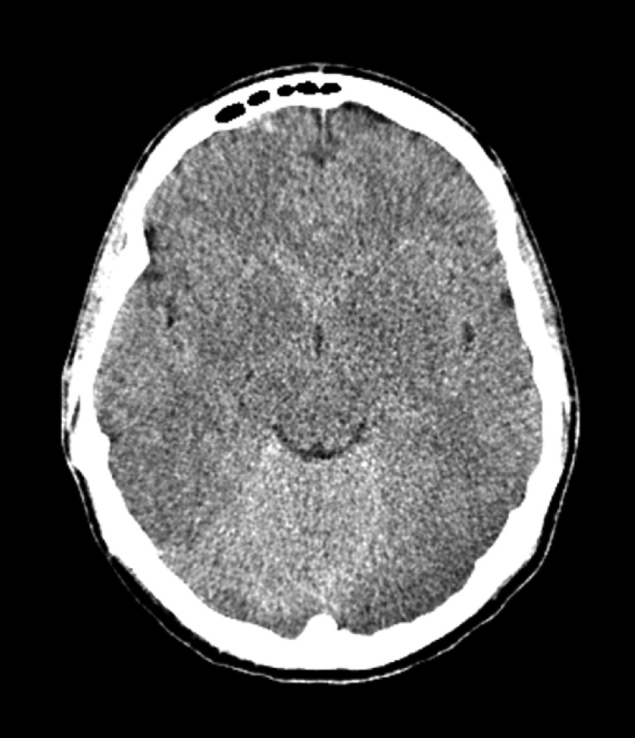
Unenhanced head CT shows diffuse hypodensity in the deep gray matter nuclei with loss of differentiation of the deep gray matter nuclei and subjacent white matter compatible with edema.
Figure 3.
Axial T2WI (A) and FLAIR (B) images demonstrate symmetrical increased signal intensity within the basal ganglia, thalami, amygdala, hippocampus, and brainstem bilaterally.
Figure 4.
Axial DWI (A) and ADC (B) images at the level of corona radiata demonstrates restricted diffusion bilaterally.
Discussion
Ethylene glycol is a common organic solvent, which is found in antifreeze as well as numerous other household products (paints, lacquers and polishes). Small quantity ingestions, either accidental or intentional, can produce toxicity, which is characterized by a severe anion gap metabolic acidosis, osmolar gap, and calcium oxalate crystals in the urine.
Chemistry
Ethylene glycol is metabolized in the liver through a series of enzymes. The intermediate metabolites of the pathway (in order) are: glycoaldehyde, glycolic acid, and glyoxylic acid. Ultimately, glyoxylic acid is converted to oxalic acid, which precipitates in the presence of calcium as calcium oxalate crystals. The most clinically significant metabolite in the pathway is glycolic acid which is primarily responsible for the metabolic acidosis [1, 2]. This pathway assists in explaining our patient's laboratory and urine microscopy findings.
Pathogenesis
Ethylene glycol toxicity can affect multiple organs systems but predominatly involves the central nervous, cardiopulmonary and renal systems. Multiorgan damage is mainly due to the various toxic metabolites which have numerous deleterious effects at the cellular level including on the electron transfer chain, oxidative phosphorylation, cellular respiration, glucose metabolism, and DNA replication [1]. The deep grey matter nuclei of the basal ganglia being metabolically more active than the remaining brain parenchyma are affected first by these metabolites, as well as by the associated hypoxia and acidosis. Additionally, human autopsy studies have demonstrated calcium oxalate crystal deposition within the walls of the cerebral blood vessels and accompanying perivascular edema and inflammation [3, 4]. The deposition of calcium oxalate crystals within the vasculature likely add up to produce further edema and damage to the deep grey matter nuclei and adjacent white matter.
Imaging
CT in the acute stages of ethylene glycol toxicity reveals edema without signficant mass effect with an affinity for the basal ganglia. Edema may also involve the temporal basal regions and brainstem [5, 6]. Although the CT scan findings of ethylene glycol toxicity have been documented, there are only a few prior case reports with MR images published in the setting of ethylene glycol intoxication. Morgan et al. reported bilateral putaminal necrosis by MRI [6]. Caparros-Lefebvre et al. demonstrated bipallidal hemorrhage in the setting of ethylene glycol ingestion [7]. Lewis et al. demonstrated delayed sequelae of ethylene glycol toxicity with bilateral enhancement of the fifth cranial nerves and communicating hydrocephalus in the setting of cranial nerve dysfunction [8]. Our patient's case demonstrates bilateral symmetrical hyperintensity within the basal ganglia, thalami, amygdala, hippocampus, and brainstem on MRI. Our patient's case also demonstrates restricted diffusion within the white matter tracts of the corona radiata bilaterally, consistent with cytotoxic edema. This feature has not been previously described in the setting of ethylene glycol ingestion.
Bilateral symmetrical hyperintensity on MRI in the deep gray matter nuclei is challenging for the radiologist. Various acute toxic conditions and chronic metabolic diseases can produce signal abnormalities. Acute causes include hypoxia, carbon monoxide inhalation, or ingestion of toxic materials (methanol, ethylene glycol, or cyanide). Rarely infection and deep venous thrombosis can cause an acute abnormality especially in pediatric patients. Chronic conditions, particularly inborn errors in metabolism such as Leigh's disease or Wilson's disease, can give similar MRI findings however these can be differentiated from acute etiologies on clinical grounds.
The authors believe that the best way to formulate an appropriate differential diagnosis in patients with involvement of bilateral deep gray matter nuclei is by detailed history combined with identifying the primary site of involvement. Magnetic resonance imaging is particularly valuable in this regard. Though there are multiple acute conditions that can involve the deep gray matter nuclei, more commonly seen are carbon monoxide poisoning, acute hypoxia, methanol and ethylene glycol poisoning. Carbon monoxide poisoning has an affinity for the globus pallidus while acute hypoxia often involves the putamen, globus pallidus and caudate head. Methanol demonstrates an affinity for putamen which besides bright signal intensity on T2WI may also demonstrate hemorrhage and necrosis [9, 10]. Our patient's case demonstrates that bilateral symmetrical hyperintensity within the basal ganglia, thalami and brainstem is a pattern associated with ethylene glycol toxicity. Restricted diffusion within the white matter tracts of the corona radiata can also be associated with ethylene glycol toxicity. In the acute clinical setting, ethylene glycol toxicity is an important differential consideration of the pathologies involving the bilateral deep grey matter nuclei.
Footnotes
Published: January 29, 2008
References
- 1.Davis DP, Bramwell KJ, Hamilton RS, Williams SR. Ethylene glycol poisoning: case report of a record-high level and a review. J Emerg Med. 1997;15(5):653–667. doi: 10.1016/s0736-4679(97)00145-5. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Gabow PA, Clay K, Sullivan JB, Lepoff R. Organic acids in ethylene glycol intoxication. Ann Intern Med. 1986;105(1):16–20. doi: 10.7326/0003-4819-105-1-16. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Leth PM, Gregersen M. Ethylene glycol poisoning. Forensic Sci Int. 2005;155(2-3):179–184. doi: 10.1016/j.forsciint.2004.11.012. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Froberg K, Dorion RP, McMartin KE. The role of calcium oxalate crystal deposition in cerebral vessels during ethylene glycol poisoning. Clin Toxicol. 2006;44(3):315–318. doi: 10.1080/15563650600588460. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Maier W. Cerebral computed tomography of ethylene glycol intoxication. Neuroradiology. 1983;24(3):175–177. doi: 10.1007/BF00347839. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Morgan BW, Ford MD, Follmer R. Ethylene glycol ingestion resulting in brainstem and midbrain dysfunction. Clin Toxicol. 2000;38(4):445–451. doi: 10.1081/clt-100100956. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Caparros-Lefebvre D, Policard J, Sengler C, Benabdallah E, Colombani S, Rigal M. Bipallidal haemorrhage after ethylene glycol intoxication. Neuroradiology. 2005;47(2):105–107. doi: 10.1007/s00234-005-1347-y. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Lewis LD, Smith BW, Mamourian AC. Delayed sequelae after acute overdoses or poisonings: cranial neuropathy related to ethylene glycol ingestion. Clin Pharmacol Ther. 1997;61(6):692–699. doi: 10.1016/S0009-9236(97)90105-3. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Hantson P, Duprez T, Mahieu P. Neurotoxicity to the basal ganglia shown by magnetic resonance imaging following poisoning by methanol and other substances. Clin Toxicol. 1997;35(2):151–161. doi: 10.3109/15563659709001186. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.Gaul HP, Wallace CJ, Auer RN, Fong TC. MR Findings in methanol intoxication. AJNR Am J Neuroradiol. 1995;16(9):1783–1786. [PubMed] [PMC free article] [PubMed] [Google Scholar]