Abstract
We present a case of lipoma arborescens of the knee in a 17-year-old man, discuss its characteristic imaging findings, and review the relevant differential diagnoses.
Abbreviations: MRI, magnetic resonance imaging; PVNS, pigmented villonodular synovitis; STIR, short tau inversion recovery
Case Report
A 17-year-old male presented to the emergency department with a history of persistent knee swelling that had been troubling him on and off for the last few years. The week before admission his knee became acutely painful. He came to California from Mexico four months prior, and denied any history of trauma. He had no significant past medical history.
On exam, there was fullness in the suprapatellar region and his knee felt boggy. He had limited range of motion. There was no redness or warmth. His white count was normal and aspiration of the joint fluid showed no sign of infection. A lateral radiograph of the knee (Fig. 1) showed a prominent soft tissue density mass interspersed with fat density material in the suprapatellar region.
Figure 1.

Lipoma arborescens in a 17-year-old man. Lateral radiograph of the knee shows a large mass within the suprapatellar region with areas of soft tissue and fat density.
The patient went on to further evaluation with MRI. Sagittal T1 (Fig. 2) and sagittal proton density (Fig. 3) images showed a large joint effusion in the suprapatellar region. There was marked hypertrophy of the synovium by a proliferating frond-like mass. The underlying bones were normal and showed no erosions or degenerative changes. The synovial mass had the characteristics of fat on all sequences (Figure 4, Figure 5). There was no enhancement with contrast (Figure 6, Figure 7).
Figure 2.

Lipoma arborescens in a 17-year-old man. Sagittal T1 weighted MRI shows a large suprapatellar effusion with a frond-like synovial mass of fat intensity.
Figure 3.

Lipoma arborescens in a 17-year-old man. Sagittal proton density MRI shows the large high-signal effusion with synovial proliferation.
Figure 4.

Lipoma arborescens in a 17-year-old man. Sagittal STIR MRI shows the synovial mass to be the same low intensity as fat.
Figure 5.
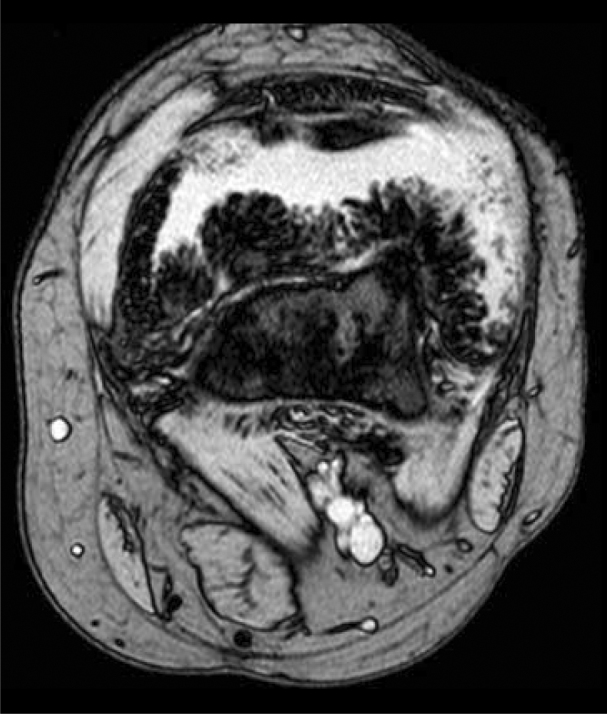
Lipoma arborescens in a 17-year-old man. Axial gradient echo MRI shows the characteristic frond-like pattern.
Figure 6.

Lipoma arborescens in a 17-year-old man. Coronal T1 fat-suppression MRI following gadolinium injection shows no enhancement of the synovial mass but enhancement of the effusion.
Figure 7.

Lipoma arborescens in a 17-year-old man. Sagittal T1 fat-suppression MRI following gadolinium injection shows no enhancement of the synovial mass but enhancement of the effusion.
Based on the history and distinctive imaging characteristics on MRI, the diagnosis of lipoma arborescens was made.
Discussion
Lipoma arborescens is a rare benign lesion, which arises in the synovium and is characterized by villous proliferation of fat cells [1]. The proliferating cells appear organic and often resemble a tree thus its name, arborescens, from the Latin arbor for tree. The cause is uncertain, though one hypothesis is that the synovial hyper-proliferation is in response to traumatic or inflammatory stimuli [1, 4]. While lipoma arborescens is often associated with trauma, osteoarthritis or rheumatoid arthritis, there have been cases which arose without any underlying condition [2, 3, 7].
Patients usually present with a history of a painless, slowly developing swollen knee [1, 4]. There is often a history of recurrent effusions [3, 4, 7]. The mean age of presentation is 43 years [5]. The most commonly affected joint is the knee, though there are cases reported in the shoulder, hip, elbow, ankle and wrist [6]. While usually unilateral, bilateral cases of lipoma arborescens have been reported [4, 8].
Lipoma arborescens has enough characteristic features on MRI to distinguish it from other conditions [1]. In a study which looked at 32 cases of lipoma arborescens, all were found to have an associated joint effusion. Other common findings were degenerative changes in the knee and meniscal tears. A smaller percentage (38%) were associated with a Baker's cyst [4]. Conventional radiographs of the knee often reveal nothing more than a soft tissue density, though it may also contain areas of radiolucency suggestive of fat. There may be underlying degenerative changes in the joint. These findings are not specific of lipoma arborescens, and it is only with MRI that we can confidentially make the diagnosis [1, 3]. On MRI lipoma arborescens is a villous proliferation, often with a frond-like configuration, which arises from within the synovial cavity. Because of its fatty characteristics and typical pattern of proliferation, lipoma arborescens has a very distinct appearance on MRI. The mass is of uniform high signal intensity on both T1 and T2 weighted images, the same as subcutaneous fat. On STIR or fat-saturated sequences the synovial proliferation will be of low signal intensity [1, 2, 3, 4, 6]. Morphologically, lipoma arborescens mostly presents as a diffuse villous proliferation, but there have been reports of lipoma arborescens appearing as a more focal pseudo mass [4]. Gadolinium enhanced images show no enhancement of the synovial proliferation, though there may be enhancement of the surrounding synovial fluid [9]. Ultrasound imaging may show the telltale frond-like projections from the mass surrounded by a joint effusion, which undulate in real time [1].
Gross specimens show replacement of synovial tissue with adipose tissue in its characteristic frond-like pattern [1]. Microscopically there are mature adipocytes with hypertrophic villi in the subsynovial tissue [4]. Synovectomy is the treatment of choice and recurrence is rare [1].
Other conditions, which may present in a similar fashion but are easily distinguishable, are: pigmented villonodular synovitis (PVNS), synovial osteochondromatosis, synovial hemangioma, rheumatoid arthritis and an intraarticular lipoma [3, 4]. PVNS should show a lobulated mass with lower signal intensity on T1 and T2 weighted sequences from the associated hemosiderin. There may be a surrounding bright effusion as well as areas of fat with the lesion [1, 10]. Synovial osteochondromatosis may have an effusion and adjacent erosions. The intraarticular bodies vary in signal intensity depending on the amount of cartilage and bone they contain [1, 4]. Synovial hemangiomas show a lobulated intraarticular mass with intermediate signal intensity on T1 weighted images [1]. On T2 weighted and fat-saturated imaging the lesion is often brighter than subcutaneous fat and often has areas of dark intensity thought to represent fibrous septa. The lesion should enhance with gadolinium [6]. Rheumatoid arthritis shows a proliferative pannus that is of intermediate to low signal intensity on T1 and T2 weighted sequences. There may be erosions and joint space narrowing [1] as well as intraarticular loose or rice bodies. A lipoma of the tendon sheath or an intraarticular lipoma is rare and may present as a focal area of fat without villous synovial proliferation [3].
Footnotes
Published: April 29, 2008
References
- 1.Sheldon PJ, Forrester DM, Learch TJ. Imaging of Intraarticular Masses. Radiographics. 2005; Jan-Feb;25(1):105–119. doi: 10.1148/rg.251045050. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Ryu KN, Jaovishida S, Schweitzer M, Motta AO, Resnick D. MR Imaging of Lipoma Arborescens of the Knee Joint. Am J Roentgenol. 1996; Nov;167(5):1229–1232. doi: 10.2214/ajr.167.5.8911186. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Murphey MD, Carroll JF, Flemming DJ, Pope TL, Gannon FH, Kransdorf MJ. Benign Musculoskeletal Lipomatous Lesions. Radiographics. 2004 Sep-Oct;24(5):1433–1466. doi: 10.1148/rg.245045120. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Vilanova JC, Barceló J, Villalón M, Aldomà J, Delgado E, Zapater I. MR Imaging of Lipoma Arborescens and the Associated Lesions. Skeletal Radiol. 2003 Sep;32(9):504–509. doi: 10.1007/s00256-003-0654-9. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Kloen P, Keel SB, Chandler HP, Geiger RH, Zarins B, Rosengerg AE. Lipoma Arborescens of the Knee. J Bone Joint Surg (Br) 1998 Mar;80(2):298–301. doi: 10.1302/0301-620x.80b2.8244. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Greenspan A. Orthopedic Imaging: A Practical Approach. 4th ed. Lippincott Williams & Williams; 2004. pp. 766–768. [Google Scholar]
- 7.Bancroft LW, Kransdorf MJ, Peterson JJ, O'Connor MI. Benign Fatty Tumors: Classification, Clinical Course, Imaging Appearance, and Treatment. Skeletal Radiol. 2006 Oct;35(10):719–733. doi: 10.1007/s00256-006-0189-y. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Bejia I, Younes M, Moussa A, Said M, Touzi M, Bergaoui N. Lipoma Arborescens Affecting Multiple Joints. Skeletal Radiol. 2005 Sep;34(9):536–538. doi: 10.1007/s00256-005-0900-4. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Chaljub G, Johnson PR. In vivo MRI characteristics of lipoma arborescens utilizing fat suppression and contrast administration. J Comput Assist Tomogr. 1996 Jan-Feb;20(1):85–87. doi: 10.1097/00004728-199601000-00016. [PubMed] [DOI] [PubMed] [Google Scholar]


