Abstract
Objective: We conducted a pilot study to examine the feasibility of administering an individual, in-person version of Health Mechanics, an innovative self-management program designed to teach individuals with spinal cord injury (SCI) to maintain physical health and prevent secondary conditions.
Methods: After baseline assessments, 27 participants were randomized using a 2:1 block design to either the experimental intervention or a usual care group. Thirteen of the 19 participants in the intervention group completed the program. Follow-up assessments were completed at 3 and 6 months after baseline.
Results: Results suggest that the Health Mechanics intervention delivered in an in-person format was perceived as useful and relevant in addressing a diverse range of health issues with participants with a wide range of personal and impairment characteristics. However, attrition rates and barriers to recruitment suggested limitations in the acceptability of the format for this population.
Conclusion: Additional research is needed to identify the populations that would most benefit from the program and the most efficacious context for administration.
Keywords: health behavior, prevention, self-management, spinal cord injuries, treatment feasibility
Traumatic SCI affects an estimated 276,000 individuals in the United States, with approximately 12,500 new injuries annually.1 Although the prevalence is relatively low in comparison to other chronic conditions, the costs are high to individuals and society. Estimates suggest that acute care costs average $519,000 for individuals with paraplegia and over $1 million for those with tetraplegia, while lifetime medical costs average $1 million to $4.7 million.1 These costs are increased by preventable secondary conditions or complications. Urinary tract infections, spasticity, hypotension, depression, obesity, and chronic pain are frequent secondary conditions,2,3 whereas pressure ulcers, deep vein thrombosis, and pulmonary embolisms are less common but more costly.
Interventions with the potential to prevent these conditions, particularly when tailored to high-risk individuals, may prove very cost effective. In fact, many secondary conditions can be prevented or their effects minimized with appropriate management, including the performance of health maintenance behaviors and compensatory strategies.4,5 Physicians and other health care professionals can provide information, medication, and specific treatments, but health depends on the effective and consistent performance of behaviors by the person with SCI. Persons with SCI must be active participants in prevention, and effective interventions need to be based around techniques that have been shown to be effective in changing behaviors.
Theoretical Background and Intervention Development
A self-management approach was chosen as the focus of the Health Mechanics program because of its effectiveness in improving health status and health behaviors, increasing self-efficacy, improving adherence to medication regimens, decreasing pain, and lowering health care costs.5–10 Self-management provides a clear format for the acquisition and performance of skills and has produced encouraging results with other chronic disorders. In addition, self-management protocols have been effectively tailored to meet the needs and concerns of diverse populations.11,12
It is of particular importance that self-management programs attempt to provide individuals who have chronic conditions with the knowledge, skills, and self-efficacy necessary to take an active role in the management of their medical condition.5 Basic self-management skills include self-monitoring, medication adherence, environmental control, relaxation, and problem solving. In particular, problem solving has been identified as a key element with the potential to reduce secondary conditions.13–20
The Health Mechanics program for the self-management of SCI is a manualized program; its development was prompted by shortened hospitalizations and rehabilitative stays,1 a community-identified need for alternative approaches to health management,21 and a practical need for a structured program and materials likely to facilitate behavior change and health promotion (rather than educational materials describing SCI). In particular, it was critical that the program would be relevant to the concerns of individuals with SCI and inclusive of the wide range of issues and impairments that they face. The manual was written for providers to use in collaboration with individuals with SCI, though it might also be read and used independently by an individual with a good basic understanding of SCI and a high reading level. A copy of it can be found in the eAppendix.
The intervention was developed using a community participatory approach and the assistance of advisory boards including individuals with SCI and dysfunction (SCI/D) and health care professionals.22 After an extensive review of research literature, existing self-management programs, and rehabilitation structures, we investigated the way that individuals with SCI are provided with and acquire education and skills. A primary concern articulated by both individuals with SCI and health care providers was that approaches for teaching individuals to manage SCI have not been adapted to the reduced time and intensity of the rehabilitation process.
The models, theories, and programs that were considered in the development of the evidence-based self-management program Health Mechanics are reviewed elsewhere.23 Briefly summarized, though, self-management interventions are based on 4 theoretical constructs or techniques (either individually or combined): social cognitive theory, the stress coping model, the transtheoretical model, and cognitive-behavioral therapy.9 The Health Mechanics program was also influenced by self-regulation theory24 and the International Classification of Functioning, Disability and Health (ICF),25 as these theories and models are useful for understanding the role of environmental factors in health and health management – factors that are important to consider when working with individuals with physical disabilities because of their influence on functional ability.
The program contains 6 skill components – attitude, self-monitoring, problem solving, communication, organization, and stress management – that were created based on the above theories or adapted from an existing asthma self-management program developed by one of the project's consultants (Dr. Thomas Creer).26 The skills of attitude and organization were developed specifically for this program based on cognitive-behavioral therapy, the ICF, and the Model of Healthcare Disparities and Disability,27 while the approaches to self-monitoring, problem solving, communication, and stress management were based on reviews, deconstruction, and adaptations of how these skills are addressed in existing programs. Facilitators teach the skills and concepts outlined in the program but are trained to use their own judgment and expertise to assist participants in applying the skills to their life, situation, or concern.
The Health Mechanics program does not focus on providing education or information about SCI or secondary conditions associated with SCI. With the exception of a brief overview of the issues faced by individuals with SCI and the recommended behaviors for managing each, there is little information about SCI itself. This was a decision made by the developer (M. Meade) for several reasons: (a) because of the wealth of educational material already available for the management of SCI; (b) due to the recognition that different health care providers may recommend different types of behaviors; and (c) to allow for ongoing development and integration of best practices related to the health management of SCI. Instead, the focus of the Health Management program is the instruction or reinforcement of self-regulatory skills for individuals with SCI who manage their own health in order to help them apply those skills within the context of their current life situation.
One of the novel components of this self-management program is that it considers the assumptions and behaviors of health care providers and encourages participants to adapt their actions, interactions, and responses accordingly. The program encourages participant-patients to ascertain the degree to which health care providers have matching (or at least complementary) expectations of the patients' role in managing their chronic impairment and the prevention of common acute conditions. Ideally, health care providers should be familiar with the concept of self-management as well as the key issues and concerns associated with SCI/D. In addition, the program encourages participant-patients to identify or discuss the provider's comfort with their self-management of common conditions such as urinary tract infections and pain and ask for information to facilitate accurate monitoring of health status and preferred self-advocacy approaches in order to prevent punitive reactions (eg, being viewed as “demanding” or “drug-seeking”).21,28
The Health Mechanics program was revised and refined based on focus group feedback from individuals with SCI/D and health care professionals in 2 regions of the United States.29
This research was a pilot study that used a randomized controlled experimental design to evaluate the feasibility of administering Health Mechanics22,29 in an individual, in-person format to improve self-regulatory skills and health of individuals with SCI. More specifically, study objectives were to (a) evaluate the feasibility of administering the self-management program to individuals with traumatic SCI as an individualized, in-person intervention and (b) determine the relevance of the intervention in addressing the needs of diverse samples of individuals with SCI with a variety of secondary conditions.
Methods
Sampling and procedure
This study was conducted between October 2011 and June 2013; it was stopped prior to the enrollment of 30 participants because of limitations in staff time and funding. The target population for this study was community-living individuals with traumatic SCI who were at least 6 months post injury and were experiencing secondary medical conditions. Participants were recruited through organizational newsletters of a state chapter of the Paralyzed Veterans of America, the SCI registry at a Midwestern medical center that serves as an SCI Model Systems Center, a state chapter of the National Spinal Injury Association, and an urban advocacy organization for individuals with mobility impairments. Potential participants were eligible for inclusion if they were between 18 and 80 years old; had a diagnosis of traumatic SCI with significant functional impairment; reported mild to moderate secondary conditions related to SCI with associated reports of emotional distress; lived in the community (ie, their own home or apartment); had reliable transportation to assessment and intervention visits; and were English speaking.
Trained research personnel screened individuals for eligibility and administered baseline assessments. After initial telephone screening to determine basic eligibility for participation, individuals were scheduled for an in-person meeting with the research assistant. At that visit, informed consent procedures were followed and the necessary documents completed. The research assistant read all assessment measures to participants and asked for their responses; thus, administration of measures was standardized since many individuals with tetraplegia find it difficult to complete written questionnaires independently.
Following completion of the baseline assessments, participants were randomly assigned using a 2:1 block design to either the experimental intervention or a usual care group; this design was selected because of the greater demands and potential for nonadherence and drop-out in the experimental group. Follow-up assessments, with the exception of a process evaluation, occurred (also in person) at 3 and 6 months post baseline. The process evaluation was conducted either over the phone, in person, or through e-mail at between 6 and 9 months post baseline. Participants were compensated for their completion of the assessment measures; no additional funds were provided for experimental participants to reimburse them for their travel or the additional time that they spent in the study.
The usual care group completed all outcome assessments and had contact with the study team through monthly e-mails or telephone calls between outcome assessments to facilitate retention. At the end of the study, participants in this group received a copy of Health Mechanics.
Experimental intervention
The experimental intervention utilized the Health Mechanics manualized program.22,29 At the beginning of each skill module, a series of screening questions are provided. These questions allow individuals with SCI/D and facilitators to consider the degree to which a particular skill has been learned and applied. If individuals' responses indicate a good understanding of the concept, less time or attention may be needed for that section. If their answers show a limited awareness of the skills or demonstrate poor integration into daily activities, facilitators can spend more time on the explanations and examples. Exercises are included and handouts for individuals with SCI are provided at the end of the manual.
For this study, the experimental intervention was administered to individuals by a trained behavioral health specialist in person at an outpatient clinic setting. During the course of this study, 3 individuals were hired, trained, and began administering the intervention with at least one participant; however, 2 of them were found to not have the degree of flexibility and clinical skills required to deliver it reliably. The individual with the requisite skills had a master's degree in counseling and experience in working with children and adolescents but no previous experience in the rehabilitation setting or with individuals with SCI; rather, he was required to learn about living with SCI as part of his training.
Based on recommendations from the National Institutes of Health (NIH) Behavior Change Consortium,30,31 facilitators were required to read the Health Mechanics program and discuss their understanding of it with the program developer (Meade); they were then required to facilitate sessions with a practice participant, which were taped and reviewed by the developer and an outside consultant (a PsyD psychologist). Finally, results were reviewed and discussed and additional training provided when needed. All intervention sessions were recorded to allow for ongoing review and evaluation of treatment fidelity using checklists and logs completed by the facilitators and the principal investigator.
Participants who completed the intervention attended between 3 and 10 sessions. Each session lasted approximately 45 minutes, during which time facilitators taught the skills and concepts outlined in the program and assisted participants in applying skills to their life, situation, or concern. The amount of time spent on each skill depended upon the facilitator's perceptions of the participant's understanding of a skill and individual needs; some participants needed 2 or 3 sessions to cover a single skill while other participants could review 2 skills in one 45-minute session. At the initial session, participants identified the primary issue they wanted to address; this became the focal point the facilitator used throughout the program.
Assessments and measures
To the extent available, standardized assessments of health and self-regulatory skills were utilized. We adapted a knowledge measure from a much more limited measure from Thietje and colleagues.32
Demographic and injury-related information
At the baseline assessment, participants were asked to provide information about demographic and injury-related characteristics. Demographic information included gender, current age, race/ethnicity, marital status, education, employment status, and residence (including location and person with whom they were living). Injury-related information included age at injury, time since injury, level and severity of injury, cause of injury, and concurrent injuries (including traumatic brain injury [TBI]).
Health
Health was assessed at baseline and at the 3- and 6-month follow-ups using the Spinal Cord Injury Secondary Conditions Scale (SCI-SCS) and the Patient Health Questionnaire (PHQ-9). The SCI-SCS is a 16-item scale based on the Seekins Secondary Conditions Scale,33 and it has 2 subscales based on frequency of secondary conditions and distress associated with those conditions. Higher scores indicate greater overall problems with secondary conditions. The PHQ-934 is a measure of self-reported depressive symptoms.
Self-regulatory skills
Self-regulatory skills, including problem-solving skills, self-efficacy, and knowledge, were assessed at baseline and at the 3- and 6-month follow-ups. Self-assessed problem-solving ability was measured using the total score of the Social Problem-Solving Inventory – Revised: Short (SPSI-R:S).35 Perceived self-efficacy for managing SCI was assessed using the Disability Management Self-Efficacy Scale (DMSES).36 Finally, we used an adapted measure of knowledge about managing SCI and preventing secondary conditions.32
Process evaluation
A process evaluation was created for the study to collect systematic feedback from participants about various components of the study, including assessment procedures, staff, and the intervention. Study personnel attempted to contact participants by phone to gather this information after the 6-month assessment was complete; if no contact was made, a survey of the items was mailed to them.
Statistical analyses
Descriptive and inferential statistics (including chi-square and t test) were conducted using IBM SPSS version 22 (IBM, Inc., Armonk, NY). Because of the small sample size, a significance value of p ≤.10 (2-sided) was used to determine possible statistical differences between groups.
Results
Figure 1 provides a CONSORT diagram of the flow of participants through the study. As noted, of the 68 individuals who were screened to participate in the study, 60% were not included in the study. The primary reasons for exclusion were transportation issues and distance to the assessments and the amount of time required for participation. Twenty-seven individuals were enrolled, completed baseline assessments, and were randomized (19 to the experimental intervention and 8 to the usual care control groups).
Figure 1.
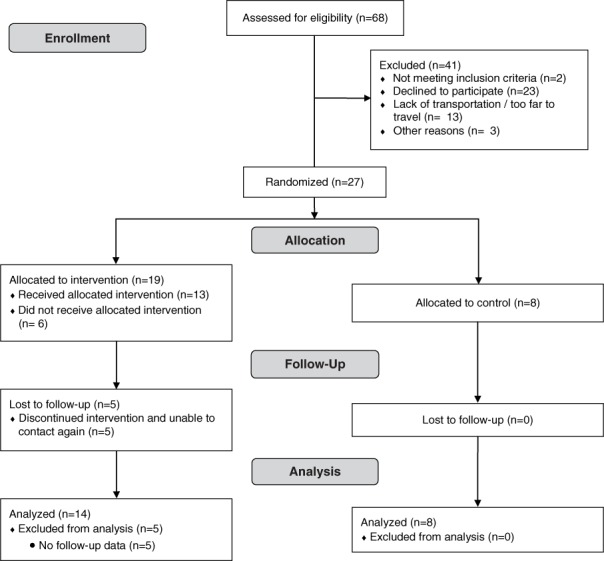
CONSORT flow diagram of participants through the study.
Baseline characteristics of groups
Twenty-seven individuals with chronic SCI who reported experiencing secondary conditions were recruited from the community. All participants were non-Hispanic White and most were male (85.2%). Average age at the time of participation in the study was 44.59 years old (SD = 12.4), and the average time since injury was 15.91 years (SD = 12.5). Participants displayed a wide range of levels of impairment and severity of injury and secondary conditions. Table 1 provides information on the baseline demographic and injury-related characteristics of participants. Nonparametric statistics were used to determine whether there were differences between groups. As noted in Table 1, at the baseline assessment, chi-square analyses showed few differences between experimental (n = 19) and control (n = 8) groups for most comparisons of demographic and injury-related information. The 2 demographic differences between groups were associated with time since injury (with participants assigned to the experimental intervention having lived for a longer time with their SCIs) and marital status (with experimental participants more likely to be divorced).
Table 1.
Demographic characteristics of sample (N = 27) at baseline
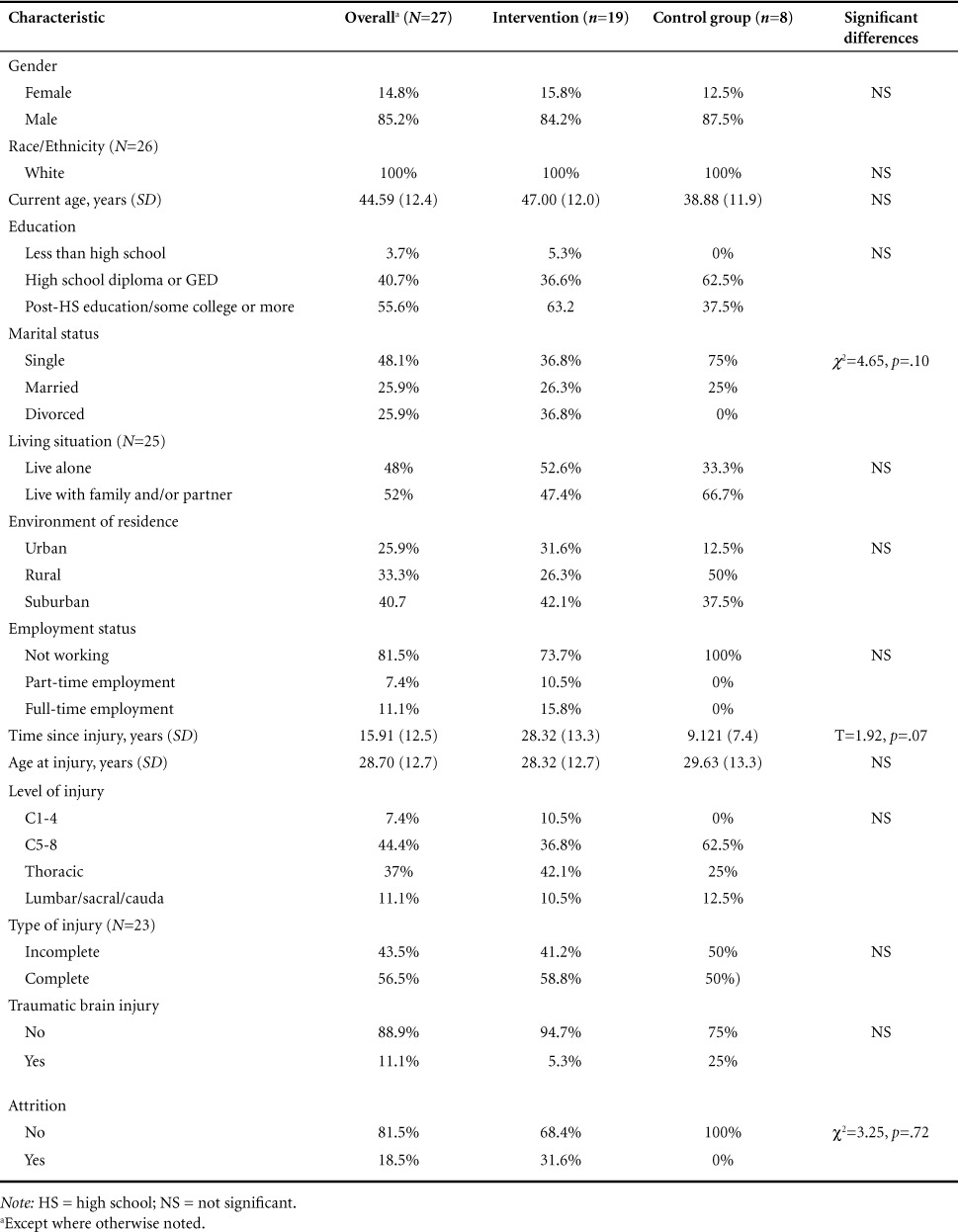
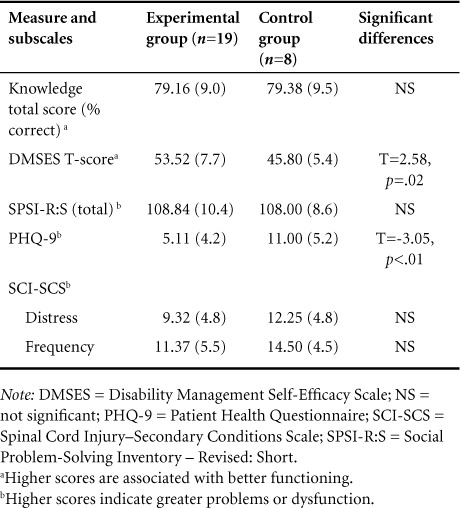
Participants' scores on psychosocial measures are shown in Table 2. Baseline differences were found to exist between the control and experimental groups. Individuals in the experimental intervention showed higher levels of self-efficacy (DMSES; t = 2.58, p = .02) and fewer depressive symptoms (t = −3.05, p < .01). No significant differences can be seen between groups at the baseline assessment on measures of SCI knowledge or secondary conditions or on the total score on the SPSI-R:S.
Table 2.
Baseline assessment scores on measures of health and self-regulation (means and standard deviations)
Feasibility
As noted in Figure 1, 68 individuals with SCI were screened for participation in the study. Of those, 2 did not meet inclusion criteria; 36 were eligible but decided not participate in the study, either because of the time associated with the intervention or travel- and transportation-related issues. Twenty-seven individuals with chronic SCI were recruited into the study, underwent baseline assessments, and were randomized into either the experimental intervention (n = 19) or the usual care control group (n = 8). Of the 19 individuals randomized to the experimental intervention, 5 withdrew from the study and 1 was mistakenly discontinued by research study staff, although he continued to participate in assessments. In contrast, all of the participants in the control group (n = 8) completed the study. This difference was significant (χ2 = 3.25, df = 1, p = .07). No differences were noted in attrition associated with any demographic or injury characteristic. However, a difference in attrition was noted based on PHQ-9 scores (t = 2.49, p = .02); individuals who showed fewer depressive symptoms were more likely to drop out of the study.
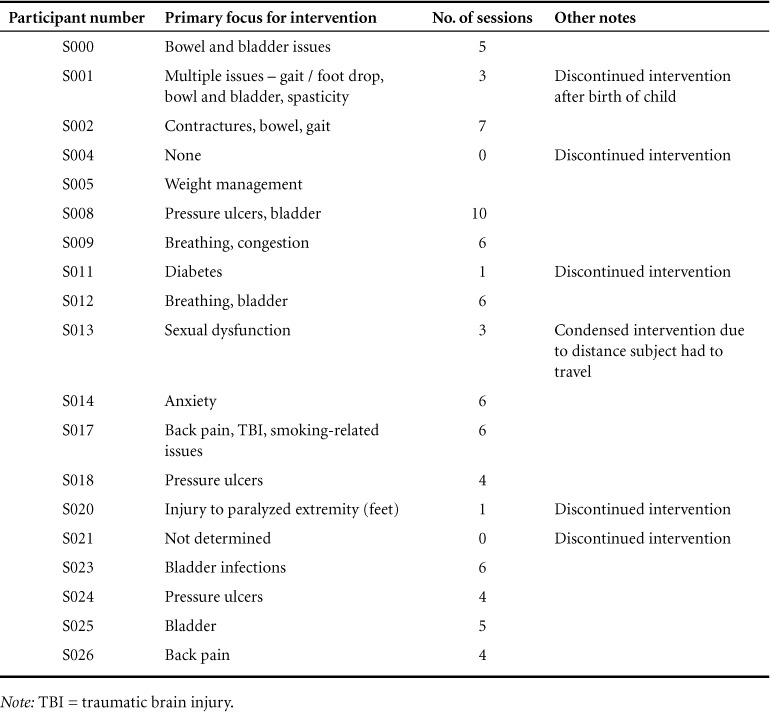
The range of issues addressed by the intervention is shown in Table 3, which lists the primary focus of the intervention for participants in the experimental group and the number of sessions that each completed. Individuals who completed the intervention addressed a range of issues, including bowel and bladder management, pressure ulcers, and sexual dysfunction. Among the 13 individuals who completed the program, the median and mode number of sessions were 6.
Table 3.
Primary focus and number of sessions for participants in the intervention group (N=19)
Implementation of experimental intervention
After the study was completed, feedback was collected from the facilitator about his experience in implementing the Health Mechanics program as an individual, in-person intervention.
Scheduling sessions
Upcoming sessions were always scheduled at the end of the session that was just completed; this helped minimize issues with phone contact. Some individuals were given the option of going over more than one skill lesson per session. This was done to reduce travel for the participant. This was also only offered to individuals who demonstrated general comprehension of the skills. The attendance rate of individuals was high and rescheduling of sessions was not cumbersome.
Selecting an issue
The focus of the sessions was generated by the participant. It had to be a condition secondary to SCI, and it had to be something that the participant wanted to work on.
Administration of the intervention
The facilitator thought that conducting the intervention using an in-person, face-to-face format was beneficial as it allowed him to more accurately gauge comprehension of the material; this was particularly important when reviewing the content of the session. He also felt that being able to read facial expressions and body language provided opportunities to identify issues that were not verbally expressed and to provide further explanation of the concepts that might have be missed. The facilitator felt that he was able to go more in depth or approach a topic in a different manner to aid the learning process. One individual could recite from memory some parts of the modules. The facilitator asked more questions to ascertain the individual's actual comprehension of the topic. This awareness and flexibility are essential for facilitating this intervention.
All participants – even those who did not continue past the first session – were perceived as being engaged in the sessions and participating fully; that is, they exhibited verbal and nonverbal signals that they were interested in the topic.
The facilitator noted that literacy level and cognitive functioning needed to be accounted for when enrolling subjects. The process of this particular intervention requires that the participant has some introspection ability. One participant had low levels of literacy and showed evidence of cognitive inflexibility. Although the Health Mechanics program as designed is capable of overcoming lower literacy levels by implementing more guidance from the facilitator and allowing the homework to be completed in session as opposed to between sessions, a redesign of the program may be required to overcome executive function deficits, especially inflexibility of thinking and self-awareness. It was noted, though, that it was not particularly problematic to engage the individuals with TBIs in the program, as long as they were aware of their impairments.
Finally, with regard to the homework that was assigned at the end of each skill section, the facilitator noted that while no participant verbally refused to do the homework, there were times that the homework was not completed prior to the session. In these cases, the facilitator worked with the participant to complete it. There was no resistance with completing the homework in session.
Subjective evaluation of experimental intervention
Process evaluations were collected from 8 individuals who completed the experimental intervention. Responses are summarized below based on the structured questions in the assessment.
Training of facilitator
When asked about the training of the facilitator, 7 of the 8 agreed that he was well trained. One individual thought that he initially lacked knowledge about SCI and the impact it has on the lives of individuals with SCI but said that the facilitator's understanding improved as the intervention went forward.
Length of intervention
When asked about the time required for the intervention, participants seemed to feel that both the number of skills and the length of the sessions were appropriate, though some recognized that these might vary based on individualized needs.
Thoughts about the intervention
In general, participants reported feeling positive about the intervention. Specific comments included:
[It] went well, refreshed on stuff, allowed [me] to refocus on issues previously learned.
[The program] offered a lot of variety and approaches in dealing with issues in problem-solving.
“Do you think the intervention taught you useful skills? Have you applied these skills to managing your health?” While one individual felt that they did not learn anything, the other 7 noted learning and applying at least one of the skills. Specific comments included:
[I] applied them. [They] made sense ten years later in context.
Almost everything was something [I] had exposure to. Going through process was useful.
[It] helped reinforce health management skills—a lot of stuff about skin and bowel program.
“Overall, do you think you benefitted from participating in the intervention? If yes, in what way? If no, why not?” All of the respondents reported that they benefitted from participating. Comments about the benefits included:
The intervention made [me] reflect a little more about what was going on.
It absolutely increased [my] knowledge base.
It directed [me] into a structured approach to problem-solving.
“How helpful do you think this project / intervention was?” Responses ranged from “not really relevant to me” (n = 1), to “somewhat useful” (n = 4) and “very helpful” (n = 3). One individual qualified their response of “very helpful” with a note that they “have been in the [wheel]chair a long time and so there was much I did not need.” One participant noted he felt that the program would benefit from putting individuals with SCI in contact with peers.
“Who do you think could benefit most from the intervention?” Although the participants reported that the program was beneficial to them, they appeared to think that it would be most beneficial for individuals who were earlier in their experience in living with SCI (generally for those 2 years or less). That said, one individual expressed concern that those who were younger or earlier post injury would take the training less seriously. Others who were identified as potentially benefitting from the intervention were “anyone in danger or at risk for not doing things” and individuals with specific problems to address. Finally, one of the participants felt that many individuals beyond those with SCI would benefit from the intervention, including caregivers and health care providers, insomuch as the program focused on empowering patients.
Factors influencing participation
When asked how various environmental factors influenced participation in the assessments, participants who completed the process evaluation noted that their ability travel to the sessions was impacted by weather (n = 1); transportation, including the price of gas (n = 3); and personal-care attendants (n = 1). When queried about whether they thought the program could be effectively administered using the phone or other telehealth devices, several said yes, at least as a supplemental approach, whereas others noted that they did not think that just a phone-based intervention would have been as helpful.
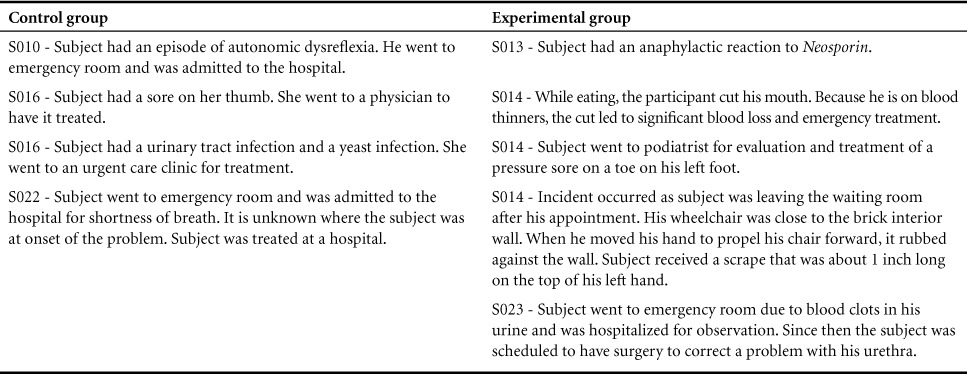
Adverse and unexpected events
Adverse and unexpected events (AE/UEs) occurred to individuals in both the control and the experimental groups; many of these were consistent with the types of injuries and conditions (such as urinary tract infections and pressure sores) for which individuals with SCI are at increased risk. The number and severity of AE/UEs appeared generally equal between the 2 groups, and none appeared to be associated with participation in the study. Table 4 provides information about the AE/UEs in the study.
Table 4.
Adverse and unexpected events
Discussion
Results suggest that the Health Mechanics program, when conducted as an individually administered, in-person intervention, could be used to address a wide range of behavioral and health targets. It was evaluated as relevant and useful by participants and was not associated with any specific adverse events. Many of the participants in the intervention group suggested that the self-management program would be most beneficial to persons with newer injuries, but most still reported that they received benefit from participating.
The study and the experimental intervention were successful in engaging a diverse group of individuals. Participants ranged from 6 months to 38 years post injury; the study included individuals with high-level tetraplegia as well as those with incomplete SCI who were able to ambulate. In addition, males and females appeared equally as likely to both enroll in and drop out from this study. The one exception with regard to diversity of the sample, however, was the lack of enrollment of individuals with SCI from racial and ethnic minority backgrounds. At this time, it is unclear whether this due to the location of the outpatient clinic, the pool of participants, the format of the program, or some other factor.
The range of health targets that were addressed through the self-management program is worth noting. The skill development format appeared relevant to addressing a wide range of physical and psychological issues; this differentiates the program from existing psychoeducational approaches and programs that focus on a more limited range of issues.37–43
Ultimately though, the relatively high number of individuals who were unable or declined to participate because of transportation issues or other reasons, as well as the rate of attrition from the experimental intervention, brings up the question of the feasibility of the program. This program has been clinically utilized to provide the format and structure for an inpatient group by the lead author (Meade) with at least a subjective assessment of engagement and success, but its application in an outpatient setting was less clear. At the very least, the requirement of traveling to the outpatient clinic reduced the number of individuals who were willing to participate in the study and possibly biased the sample by self-selecting individuals who were serious about making changes in their lives; this may contrast with briefer interventions, such as motivational interviewing, which are more integrated into existing care processes and may be easier for participants to engage with.44
Also of concern is the facilitator's question about the usefulness of Health Mechanics, in its current format, to address the needs of individuals with a lack of awareness and cognitive inflexibility. This is important considering that the concomitance of SCI and TBI is as high as 60%.45 Future iterations of the program, as well as other health management programs for this population, will need to consider how to better define the selection of participants or tailor recommendations and approaches to the needs of individuals with cognitive deficits.
Despite its limitations, the Health Mechanics program appears to warrant additional research with a larger, more well-defined population given its flexibility to address a broad range of issues, the positive feedback from participants, and the lack of serious adverse events. Future studies, though, should examine and better define the characteristics of participants who would be thought to benefit from an intervention focused on skill development. In particular, the Health Mechanics program administered within a health care setting may be a useful complement to existing health management approaches, including the education and groups often offered during inpatient rehabilitation,37 patient-provider interactions in outpatient clinics, and support groups.38–41
Limitations
This study has limitations that must be acknowledged and addressed in future research. Designing the intervention to be administered in person in an outpatient clinic setting definitely limited the number of individuals with SCI who were able to participate. Transportation and travel is often a significant barrier for individuals with SCI – either because of the time or cost involved or the need to engage others (whether paid or unpaid caregivers) to assist with arrangements.
Similarly, the time required to participate in the intervention definitely influenced recruitment and likely influenced attrition. Even though the number of sessions and demands of the intervention were comparable or less than seen in other self-management programs,38,46 the burden and effort required to attend and participate in these sessions for individuals with SCI partially explained the fact that only the experimental group experienced attrition.
Because of the small sample size of this pilot study, we have limited our analysis and discussion to issues directly associated with the feasibility and subjective evaluation of the program. An article is currently being developed that examines the changes that may or may not have occurred with the intervention group in order to try and distinguish who the intervention may and may not be appropriate for.
Although participants were randomized, there were baseline differences between the control and experimental groups. Participants in the intervention group had lived longer with their SCIs and were generally healthier and more confident.
Finally, this study used a usual care control group as opposed to placebo/attention control group that was subject to equal demands and burden; this may have impacted the outcome. The design would have been stronger if the “usual care group” had served as an “attention control,” matching the number of in-person meetings without a treatment focus.
Implications
The Health Mechanics program provides a flexible self-management intervention that can be utilized to address any number of conditions or issues with individuals who vary significantly with regard to severity of impairment and functional ability. Implementation of the program – particularly with motivated, high-risk individuals – may reduce secondary conditions and associated health care costs. Future studies are warranted to explore the effectiveness of offering the program in various formats (eg, individual in-person vs group in-person vs individual telehealth) and to determine the characteristics of the population who may most benefit from this approach.
Acknowledgments
The authors declare that they have no conflicts of interest to report. All procedures performed with human participants were in accordance with the ethical standards of the Institutional Research Committee and with the 1964 Helsinki Declaration and its later amendments. Informed consent was obtained from all individual participants in the study.
A copy of the Health Mechanics program and the full protocol for this trial can be obtained from the primary author (M. Meade).
The Health Mechanics program was created by Dr. Michelle Meade at the University of Michigan in collaboration with consultants, individuals with spinal cord injury and disease, and health care providers. The authors would like to thank the members of both the professional and consumer advisory committees whose insight and input informed the development of the Health Mechanics program. In addition, they would like to recognize the contributions, advice, and guidance of Thomas L. Creer, PhD, who served as consultant and mentor for this project prior to passing away in 2011. Support for the development of the Health Mechanics program was provided by grant #576 from the Paralyzed Veterans of America (PVA) Education Foundation.
The authors would also like to thank the consultants and advisory board members who informed the development and assisted with the implementation of this study, including Catherine Wilson, PsyD, Tim Elliot, PhD, Anthony Chiodo, PhD, Dawn Edhe, PhD, and Susan Murphy, PhD. Support for this study was provided by grant #2751 from the Paralyzed Veterans of America (PVA) Research Foundation.
Thank you also to Joanna Jennie, who assisted in the preparation of the manuscript.
Footnotes
Supplementary material: The online version of this article contains the eAppendix (1.4MB, pdf) .
REFERENCES
- 1.National Spinal Cord Injury Statistical Center. Birmingham, AL: University of Alabama at Birmingham; 2015. Facts and figures at a glance. https://www.nscisc.uab.edu/Public/Facts%202015%20Aug.pdf. Accessed November 29, 2015. [Google Scholar]
- 2.Anson CA, Shepherd C. Incidence of secondary complications in spinal cord injury. IJRR. 1996;19(1):55–66. doi: 10.1097/00004356-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 3.McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ. Long-term medical complications after traumatic spinal cord injury: A regional model systems analysis. Arch Phys Med Rehabil. 1999;80(11):1402–1410. doi: 10.1016/s0003-9993(99)90251-4. [DOI] [PubMed] [Google Scholar]
- 4.Holman H, Lorig K. Patient self-management: A key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 2004;119(3):239–243. doi: 10.1016/j.phr.2004.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lorig K. Self-management education: More than a nice extra. Med Care. 2003;41(6):699–701. doi: 10.1097/01.MLR.0000072811.54551.38. [DOI] [PubMed] [Google Scholar]
- 6.Bodenheimer T, Lorig K, Holman J, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 7.Lorig KR, Holman HR. Self-management education: History, definition, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 8.Lorig KR, Sobel DS, Stewart AL et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Med Care. 1999;37(1):5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004;364(9444):1523–1537. doi: 10.1016/S0140-6736(04)17277-2. [DOI] [PubMed] [Google Scholar]
- 10.Steed L, Cooke D, Newman S. A systematic review of psychosocial outcomes following education, self-management and psychological interventions in diabetes mellitus. Patient Educ Couns. 2003;51(1):5–15. doi: 10.1016/s0738-3991(02)00213-6. [DOI] [PubMed] [Google Scholar]
- 11.Rosal MC, Olendzki B, Reed GW, Gumieniak O, Scavron J, Ockene I. Diabetes self-management among low-income Spanish-speaking patients: A pilot study. Ann Behav Med. 2005;29(3):225–235. doi: 10.1207/s15324796abm2903_9. [DOI] [PubMed] [Google Scholar]
- 12.Vincent D, Clark L, Zimmer LM, Sanchez J. Using focus groups to develop a culturally competent diabetes self-management program for Mexican Americans. Diabetes Educ. 2006;32(1):89–97. doi: 10.1177/0145721705284372. [DOI] [PubMed] [Google Scholar]
- 13.Brownlee AT. Applied research as a problem-solving tool: Strengthening the interface between health management and research. J Health Admin Educ. 1986;4(1):31–44. [PubMed] [Google Scholar]
- 14.Dohoo IR. Problem solving in dairy health management. Can Vet J. 1985;26(1):20–23. [PMC free article] [PubMed] [Google Scholar]
- 15.Dreer LE, Elliott TR, Tucker E. Social problem-solving abilities and health behaviors among persons with recent-onset spinal cord injury. J Clin Psychol Med Settings. 2004;11(1):7–13. doi: 10.1023/B:JOCS.0000016265.62022.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elliott TR, Berry JW. Brief problem-solving training for family caregivers of persons with recent-onset spinal cord injuries: A randomized controlled trial. J Clin Psych. 2009;65(4):406–422. doi: 10.1002/jclp.20527. [DOI] [PubMed] [Google Scholar]
- 17.Elliott TR, Godshall FJ, Herrick SM, Witty TE, Spruell M. Problem-solving appraisal and psychological adjustment following spinal cord injury. Cogn Ther Res. 1991;15(5):387–398. doi: 10.1016/0005-7967(91)90133-n. [DOI] [PubMed] [Google Scholar]
- 18.Elliott TR, Brossart D, Berry JW, Fine PR. Problem-solving training via videoconferencing for family caregivers of persons with spinal cord injuries: A randomized controlled trial. Behav Res Ther. 2008;46(11):1220–1229. doi: 10.1016/j.brat.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 19.Herrick S, Elliott TR, Crow F. Self-appraised problem-solving skills and the prediction of secondary complications among persons with spinal cord injuries. J Clin Psychol Med Settings. 1994;1(3):269–283. doi: 10.1007/BF01989628. [DOI] [PubMed] [Google Scholar]
- 20.Hill-Briggs F, Echemendia RJ. Association of metabolic control with problem-solving skills. Diabetes Care. 2001;24(5):959. doi: 10.2337/diacare.24.5.959. [DOI] [PubMed] [Google Scholar]
- 21.Meade M, Jackson MN, Barrett K, Ellenbogen P. Needs assessment of Virginians with spinal cord injury: Final report – findings and recommendations. Spring 2006. http://www.pmr.vcu.edu/programs/sci/pdf/ExecutiveSummary.pdf. Accessed February 15, 2016.
- 22.Meade MA. Health Mechanics: Tools for the Self-Management of Spinal Cord Injury and Disease. Ann Arbor, MI: University of Michigan; 2009. [Google Scholar]
- 23.Meade MA, Cronin LA. The expert patient and the self-management of chronic conditions and disabilities. In: Kennedy P., editor. The Oxford Handbook of Rehabilitation Psychology. New York: Oxford University Press; 2012. pp. 492–510. [Google Scholar]
- 24.Clark NM, Gong M, Kaciroti N. A model of self-regulation for control of chronic disease. Health Educ Behav. 2001;28(6):769–782. doi: 10.1177/109019810102800608. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization. Geneva: Author; 2001. The International Classification of Functioning, Disability and Health (ICF) http://www.who.int/classifications/icf/en/. Accessed November 29, 2015. [Google Scholar]
- 26.Creer TL, Kotses H, Reynolds RV. A Handbook for Asthma Self-Management: A Patient's Guide to Living with Asthma. Athens, OH: Ohio University Press; 1991. [Google Scholar]
- 27.Meade MA, Mahmoudi E, Lee SY. The intersection of disability and healthcare disparities: A conceptual framework. Disabil Rehabil. 2015;37(7):632–641. doi: 10.3109/09638288.2014.938176. [DOI] [PubMed] [Google Scholar]
- 28.Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, Ford DE. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282(6):583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 29.Meade MA. Final report on grant #576. Ann Arbor, MI: Paralyzed Veterans of America Education Foundation; 2009. [Google Scholar]
- 30.Bellg AJ, Borrelli B, Resnick B et al. Enhancing treatment fidelity in health behavior change studies: Best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443–451. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- 31.Spillane V, Byrne MC, Byrne M, Leathem CS, O'Malley M, Cupples ME. Monitoring treatment fidelity in a randomized controlled trial of a complex intervention. J Adv Nurs. 2007;60(3):343–352. doi: 10.1111/j.1365-2648.2007.04386.x. [DOI] [PubMed] [Google Scholar]
- 32.Thietje R, Giese R, Pouw M et al. How does knowledge about spinal cord injury-related complications develop in subjects with spinal cord injury? A descriptive analysis in 214 patients. Spinal Cord. 2011;49(1):43–48. doi: 10.1038/sc.2010.96. [DOI] [PubMed] [Google Scholar]
- 33.Kalpakjian CZ, Scelza WM, Forchheimer MB, Toussaint LL. Preliminary reliability and validity of a spinal cord injury secondary conditions scale. J Spinal Cord Med, 2007;30(2):131–139. doi: 10.1080/10790268.2007.11753924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.D'Zurilla TJ, Nazu AM, Maydeu-Olivares A. Social Problem-Solving Inventory – Revised. North Tonawanda, NY: Multi-Health Systems (MHS), Inc.; 2002. [Google Scholar]
- 36.University of Washington Center on Outcomes Research in Rehabilitation (UWCORR) Disability Management Self Efficacy Scale (DMSES; spinal cord injury version) Seattle, WA: University of Washington Department of Rehabilitation Medicine; date unknown. [Google Scholar]
- 37.Wolfe DL, Potter PJ, Sequeira KAJ. Overcoming challenges: The role of educating individuals with SCI to reduce secondary conditions. Top Spinal Cord Inj Rehabil. 2004;10(1):41–50. [Google Scholar]
- 38.Oregon Office on Disability and Health. Healthy living program. http://cdrc.ohsu.edu/oodh/healthpromotion/index.html. Accessed February 1, 2007.
- 39.Chen Y, Henson S, Jackson AB, Richards JS. Obesity intervention in persons with spinal cord injury. Spinal Cord. 2006;44(2):82–91. doi: 10.1038/sj.sc.3101818. [DOI] [PubMed] [Google Scholar]
- 40.Froehlich-Grobe K, White G. Promoting physical activity among women with mobility impairments: A randomized controlled trial to assess a home- and community-based intervention. Arch Phys Med Rehabil. 2004;85(4):640–648. doi: 10.1016/j.apmr.2003.07.012. [DOI] [PubMed] [Google Scholar]
- 41.Zemper ED, Tate DG, Roller S et al. Assessment of a holistic wellness program for persons with spinal cord injury. Am J Phys Med Rehabil. 2003;82(12):957–968. doi: 10.1097/01.PHM.0000098504.78524.E2. quiz 969-71. [DOI] [PubMed] [Google Scholar]
- 42.King C, Kennedy P. Coping effectiveness training for people with spinal cord injury: Preliminary results of a controlled trial. Br J Clin Psychol. 1999;38(1):5–14. doi: 10.1348/014466599162629. [DOI] [PubMed] [Google Scholar]
- 43.Kennedy P, Duff J, Evans M, Beedie A. Coping effectiveness training reduces depression and anxiety following traumatic spinal cord injuries. Br J Clin Psychol. 2003;42(1):41–52. doi: 10.1348/014466503762842002. [DOI] [PubMed] [Google Scholar]
- 44.Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: A systematic review. Addiction. 2001;96(12):1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- 45.Macciocchi S, Seel RT, Thompson N, Byams R, Bowman B. Spinal cord injury and co-occurring traumatic brain injury: Assessment and incidence. Arch Phys Med Rehabil. 2008;89(7):1350–1357. doi: 10.1016/j.apmr.2007.11.055. [DOI] [PubMed] [Google Scholar]
- 46.Packer TL, Boldy D, Ghahari S, Melling L, Parsons R, Osborne RH. Self-management programs conducted within a practice setting: Who participates, who benefits and what can be learned? Patient Educ Counsel. 2012;87(1):93–100. doi: 10.1016/j.pec.2011.09.007. [DOI] [PubMed] [Google Scholar]


