Abstract
Background: Past research has found a relationship between the mental health of parental caregivers and their children with spinal cord injury (SCI), but little is known about how other aspects of caregiver health and functioning impact health-related quality of life (HRQOL) of youth.
Objective: The purpose of this study was to explore the importance of caregiver mental health, physical health, burden, and problem-solving skills in relation to children's physical and psychosocial HRQOL.
Methods: Forty youths with SCI ages 7 to 17 years completed the PedsQLTM; primary caregivers completed standardized measures of mental and physical health, burden, and problem solving. We evaluated 2 hierarchical linear regression models predicting children's physical and psychosocial HRQOL.
Results: The 40 youths were an average of 11.48 years (SD = 3.21), 62.5% were male, and 80% Caucasian. They had been injured an average of 6.90 years (SD = 3.92); 75% had paraplegia, and 61.5% had complete injuries. Most caregivers were mothers (85%), were married (60%), and had at least some college education (87.5%). Univariate analyses revealed that caregiver problem solving alone was related to children's physical HRQOL, and caregiver mental health, burden, and problem solving were related to children's psychosocial HRQOL. Regression analyses controlling for child age and injury level revealed effective caregiver problem solving (P < .01) was significantly related to greater child physical (Model R2 = 0.440) and psychosocial (Model R2 = 0.547) HRQOL.
Conclusions: Although relationships should be explored longitudinally with larger samples, results indicate caregiver problem solving may be a reasonable target for intervention to improve HRQOL among youth with SCI.
Keywords: caregivers, health-related quality of life, pediatrics, problem solving, psychosocial factors, spinal cord injuries
Literature relating to the health and well-being of youth with disabilities and chronic illness has made a strong case for attending to the needs of the caregiver.1 Central to this argument is the link between the functioning of caregivers and care recipients. This link has been investigated among parental caregivers of youth with spinal cord injuries (SCIs), spina bifida, cystic fibrosis, diabetes, cancer, and chronic pain, as parental characteristics including stress, mental health, coping, problem-solving skills, and marital satisfaction have been found to predict mental health, self-esteem, quality of life (QOL), adjustment to disability, and physical health outcomes in youth.2–8 While this research demonstrates the importance of caregivers to youth with complex health needs, little is known about what caregiver outcomes may be most important to address in an intervention. Further, little is known about what caregiver factors are most critical to QOL in children, which has been touted in SCI literature as the ultimate rehabilitation outcome.9,10 Evaluating the impact of caregiver characteristics together on child QOL would provide critical information regarding how to effectively intervene to assist families of youth with disabilities.
As mentioned, a number of caregiver characteristics have emerged as being important to outcomes in youth, including caregiver mental and physical health, problem solving, and stress or burden. Specific to mental health, the relationship between parental and child mental health has long been acknowledged among typically developing youth8 and has been demonstrated among youth with SCI. In particular, the current research team found bidirectional positive relationships between caregiver and child mental health among youth with SCI,4 and another group of pediatric SCI researchers found bidirectional positive relationships between mother and child posttraumatic stress disorder.5 These findings were echoed in a study involving youth with limb deficiencies that found that parental depression and anxiety and marital discord were related to child depression, anxiety, and self-esteem.3 Specific to problem solving, effective caregiver problem solving has been linked to better diabetes management among youth6 and ineffective caregiver problem solving has been linked to lower acceptance of disability and increased pressure ulcer diagnosis among adults with SCI.11 For pediatric SCI, although the current team found that negative coping strategies of youth reflected their caregivers' negative coping strategies,12 to date, caregiver problem solving has not been addressed among youth with SCI.
Caregiver burden has been defined by Zarit and colleagues13 as the degree to which caregivers perceive that caregiving has had an adverse effect on their emotional, social, financial, physical, and spiritual functioning. Caregiver health often deteriorates as caregivers continue to provide care; many attribute their burden to a lack of time and control and decreased psychosocial energy.14 Worsening caregiver health and lack of resources for caregivers have been found to negatively impact child outcomes, including repeated hospitalization among youth with chronic illnesses including seizures, cystic fibrosis, epilepsy, and asthma15 and increased out-of-home placement for youth with severe intellectual, physical, and sensory disabilities.16 To date, neither caregiver burden nor caregiver health have been examined among youth with SCI.
Finally, a number of child outcomes have been examined in relation to the functioning of their caregivers. For the current study, we sought to include an outcome that would best represent the youth's functioning across a number of important domains. QOL has emerged as a critical endpoint in the SCI literature.10 Among youth with disabilities, investigations have typically centered on health-related quality of life (HRQOL), a subset of QOL which evaluates children's views of the impact of their disability and accompanying treatment on a number of aspects of their lives, including physical, mental, social, and academic domains.9 HRQOL was therefore selected for the current study as it allows for a comprehensive look at children's self-reported functioning.
Existing literature provides an important start to understanding the needs of families of youth with disabilities and chronic illness. However, there remains a dearth of knowledge specific to families of youth with permanent, acquired physical disabilities like SCI. Although youth with SCI share many common characteristics with youth with other chronic health conditions, youth with SCI often sustain their permanent disabilities in a traumatic way, which may have a particularly negative effect on their caregivers. Further, there are a variety of parental factors that have been found to impact youth with chronic illness; understanding which of these factors is most critical to youth HRQOL can help in the prioritization of intervention efforts. The purpose of the current study was therefore to evaluate the importance of caregiver mental health, physical health, burden, and problem-solving skills in relation to the physical and psychosocial HRQOL of youth with SCI. Based on past research, we hypothesized that caregiver physical health, problem solving, and burden would be positively related to child physical HRQOL, and caregiver mental health, physical health, problem solving, and burden would be positively related to child psychosocial HRQOL.
Methods
Participants
The current study analyzed baseline data from an in-person intervention for primary caregivers of youth with SCI (ie, typically parents). This intervention took place within one pediatric specialty hospital; the hospital was located in the United States but was part of a health care system that spanned North America. Recruitment efforts included outreach mailings and phone calls to families within this system and outreach to other community organizations serving youth and families with disabilities. Eligible families were those whose children with SCI were 7 to 17 years old and had been injured at least 1 year. A total of 250 families were contacted about the study, 53 were consented, and 41 participated in the intervention.
Instruments
Youth with SCI
PediatricQualityofLifeInventory (PedsQLTM). Youth completed the child self-report PedsQLTM (4.0 Generic Core Scales), which includes 2 overarching scales: Physical (8 items) and Psychosocial (15 items) Health. The PedsQLTM was developed by Dr. James W. Varni and is a reliable and valid measure of HRQOL for children from 5 to 18 years old.9 The Psychosocial Health Scale in particular comprises emotional, social, and school functioning subscales, which are averaged to create the psychosocial scale score. Internal consistency reliability was demonstrated for both scales with the current sample (α = 0.761 for Physical Health; α= 0.862 for Psychosocial Health).
Primary caregivers
Caregivers completed standardized measures of mental and physical health, burden, and problem solving.
Hospital Anxiety and Depression Scale (HADS). The HADS is a reliable and valid self-report screening tool for anxiety and depression in adults.17 It consists of 14 items total, 7 each for anxiety and depression. Each item is rated on a 4-point scale ranging from 0 (not at all) to 3 (very often), based on the frequency of symptoms over the preceding week. Internal consistency reliability was demonstrated with the current sample (α = 0.836).
The Pennebaker Inventory of Limbic Languidness (PILL). The PILL is a 54-question self-report tool that measures frequency of occurrence of a group of common physical symptoms and sensations.18 Subjects indicate the frequency with which they experience each symptom on a 5-point scale, from “have never or almost never experienced the symptom” to “more than once every week.” Scores are summed, with higher scores indicating greater symptomatology. Internal consistency reliability was demonstrated with the current sample (α = 0.961).
The Revised Caregiver Burden Interview, short form. The Zarit Burden Interview is a self-report measure of the impact of caregiving.19 The short version contains 12 items endorsed on a 5-point scale with response options ranging from 0 (never) to 4 (nearly always) and was found to demonstrate reliability and validity and to be comparable to the original full-length version.20 Internal consistency reliability was demonstrated with the current sample (α = 0.903).
The Social Problem Solving Inventory, revised, short form (SPSI-R:S). The SPSI-R:S is a self-report measure of problem-solving styles and solution generation, consisting of 25 items with 5 component scales.21 Two of these scales measure problem-solving orientation, including Positive (ie, seeing problems as solvable challenges; α = 0.795) and Negative (ie, seeing problems as insurmountable threats; α=0.837). The other 3 scales measure problem-solving style, including Rational (ie, systematically applying effective problem-solving techniques; α = 0.736), Impulsivity/Carelessness (ie, applying narrow, hurried, incomplete solutions; α = 0.833), and Avoidance (ie, avoiding problems rather than confronting them; α = 0.774). Each item is endorsed on a 5-point scale with response options ranging from 0 (not at all true of me) to 4 (extremely true of me). The measure also yields a total problem-solving score, with higher scores indicating more effective problem solving. Unless otherwise indicated, this total score was used in all analyses. This short form has been found to be reliable and valid in past research21; as reported above, all 5 scales demonstrated internal consistency reliability with the current sample.
Procedures
Caregivers were contacted from a master list of active SCI patients within one health care system and through outreach to key community organizations. Once they agreed to participate, caregivers and their children were consented/assented by project staff. Caregivers and children completed measures within 2 weeks of caregivers participating in an in-person intervention.
Data analysis
Pearson correlation coefficients assessed relationships between demographic characteristics (child sex, age, injury level, injury duration) and caregiver factors (mental health, problem solving, burden, and physical health) and child physical and psychosocial HRQOL. Factors with significant univariate relationships with the HRQOL scales were included in subsequent regression analyses as independent predictors. Specific to the demographic variables, child's age and injury level were the only 2 to demonstrate any significant relationship with either HRQOL subscale, so these variables were retained for all analyses.
We evaluated 2 hierarchical linear regression models, one predicting children's physical HRQOL and the other predicting psychosocial HRQOL. Hierarchical linear regression analyses were used to assess whether caregiver outcomes contributed significantly to child HRQOL, above and beyond child age and injury level. Data were screened and the assumptions of normality, linearity, and homoscedasticity were met, and there were no multivariate outliers.22 Due to the relatively small sample size, this project is considered exploratory and we have reported Cohen's f 2 to assess the effect size for each significant predictor in the regression equations, with 0.02 considered to be a small effect, 0.15 a medium effect, and 0.35 a large effect.23
Results
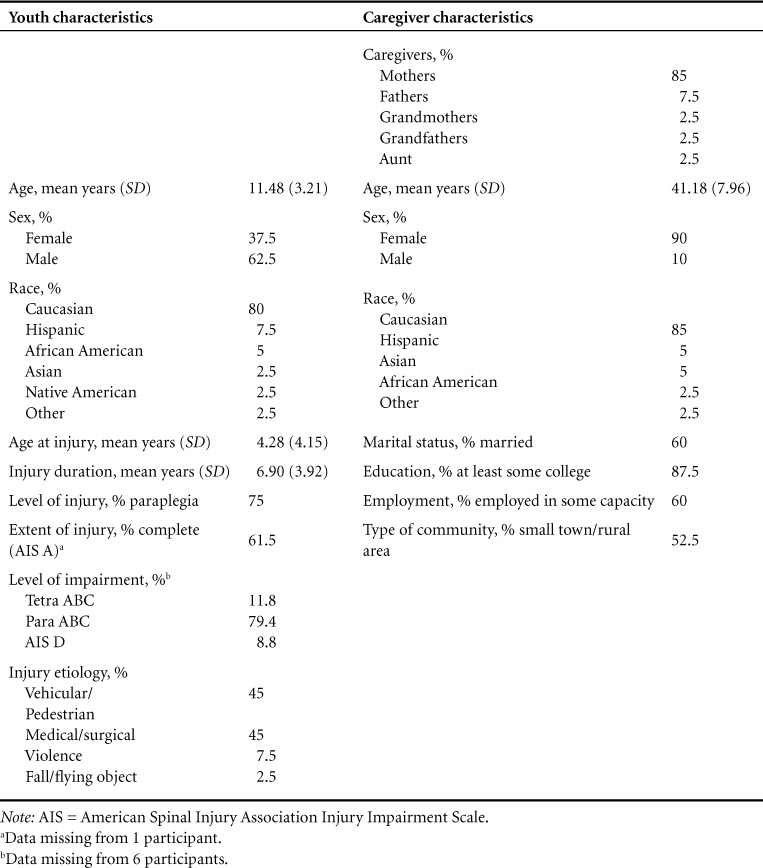
Of the 41 families who were eligible for inclusion in this study, one family experienced significant missing data so was excluded from the current analyses. The 40 included youths were an average of 11.48 years (SD = 3.21), 62.5% were male, and 80% Caucasian. They had been injured an average of 6.90 years (SD = 3.92); 75% had paraplegia and 61.5% had complete injuries. Most caregivers were mothers (85%), married (60%), and had at least some college education (87.5%) (Table 1). The majority of families were from one pediatric specialty hospital system in North America (95%), but participants were geographically diverse, as they lived in a total of 21 states as well as 2 provinces in Canada.
Table 1.
Participant characteristics (N = 40)
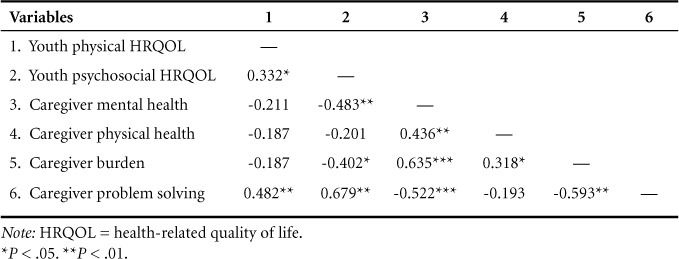
Univariate analyses revealed caregiver problem solving alone was related to child physical HRQOL, and caregiver mental health, burden, and problem solving were related to child psychosocial HRQOL (Table 2). Caregiver physical health was not significantly related to either physical or psychosocial HRQOL.
Table 2.
Correlations between caregiver outcomes and child HRQOL (N = 40)
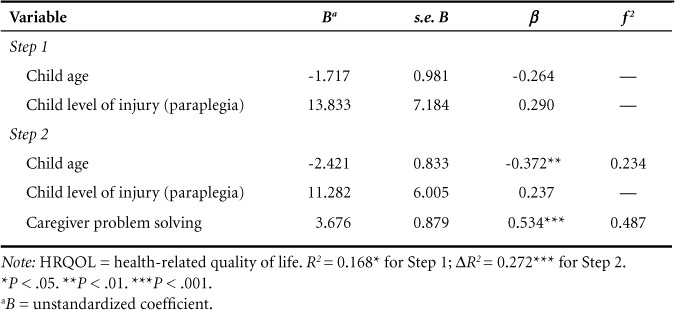
Specific to physical HRQOL, regression analyses controlling for child age and injury level revealed effective caregiver problem solving (P < .001) was significantly related to greater child physical HRQOL (Model R2 = 0.440) (Table 3). Cohen's f 2 indicated a large effect size for problem solving (0.487) in terms of physical HRQOL. Age also emerged as significant in the final model (P < .01), as younger youth reported greater child physical HRQOL.
Table 3.
Summary of hierarchical linear regression analyses predicting child physical HRQOL (N = 40)
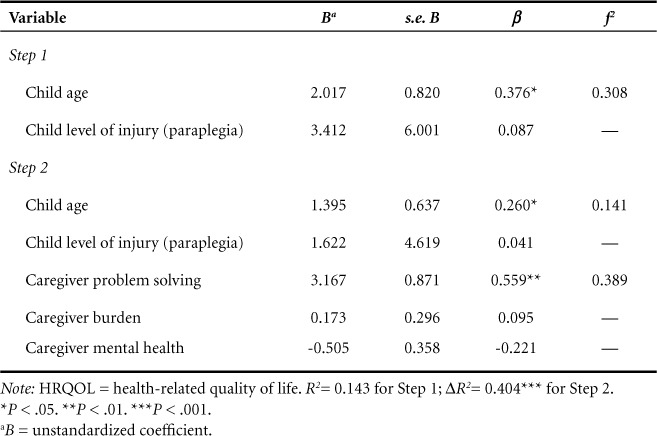
Specific to psychosocial HRQOL, regression analyses controlling for child age and injury level revealed effective caregiver problem solving (P < .01) was significantly related to greater psychosocial HRQOL (Model R2 = 0.544) (Table 4). Cohen's f 2 indicated a large effect size for problem solving (0.389) in terms of psychosocial HRQOL. Similar to physical HRQOL, age also remained a significant predictor in the final model (P < .05), but here older youth reported greater psychological HRQOL.
Table 4.
Summary of hierarchical linear regression analyses predicting child psychosocial HRQOL (N = 40)
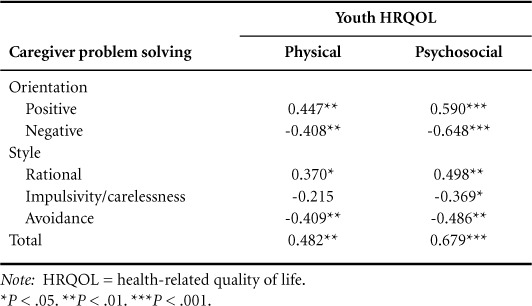
Finally, given the importance of problem solving, we examined what aspects of problem solving were related to HRQOL (Table 5). We found problem-solving orientation to be related to both physical and psychosocial HRQOL, as having a caregiver who demonstrated a positive problem-solving orientation was related to greater child HRQOL and a caregiver demonstrating a negative problem-solving orientation was related to decreased child HRQOL. Univariate analyses also indicated relationships between caregiver problem-solving style and youth HRQOL, as having a caregiver who demonstrated rational problem solving was related to greater child HRQOL and having a caregiver who demonstrated avoidance problem solving was related to decreased child HRQOL. Finally, caregivers demonstrating impulsivity/carelessness was related to kids having lower psychosocial HRQOL.
Table 5.
Correlations between caregiver problem solving and physical and psychosocial HRQOL (N = 40)
Discussion
The purpose of this article was to examine the relationship between a variety of caregiver factors and the HRQOL of youth with SCI. In particular, we explored relationships between caregiver burden, mental health, physical health, and problem solving and youth physical and psychosocial HRQOL. When examining these caregiver factors together, problem solving emerged as the caregiver characteristic most related to youth HRQOL. These results suggest that caregiver problem solving may be a reasonable target for intervention to improve HRQOL among youth with SCI.
Analyses provided partial support for our hypotheses. Although physical HRQOL was not related to caregiver physical health or perceived burden, it was related to caregiver problem solving. This echoes past research among youth with diabetes finding that effective diabetes-specific problem solving by caregivers was related to better diabetes management.6 Even though physical HRQOL is not identical to physical health outcomes, physical HRQOL is an indicator of how health status impacts youth physical functioning. Specific to SCI, caregiver problem solving has also been related to the presence of pressure sores at 1 year post discharge among adults with SCI.11 Across these studies, it is likely that more effective problem solving among caregivers leads to more efficient management of youth's health issues, leading to a lower incidence of secondary conditions and greater physical HRQOL.
Specific to psychosocial HRQOL, the significant relationship between caregiver problem solving and psychosocial functioning mirrors findings from Elliott and colleagues, who found that among adults with SCI, caregiver problem solving at the time of their family member's initial inpatient admission predicted their family member's acceptance of disability at time of discharge.11 Univariate analyses were more in line with our original hypothesis, as significant relationships emerged between psychosocial HRQOL and 3 caregiver factors, including mental health, burden, and problem solving. Once considering all these factors together, however, caregiver mental health and burden dropped out, indicating that caregiver problem solving had the strongest relationship with psychosocial HRQOL.
Caregiver physical health was not significantly associated with youth HRQOL. Although we suspect that the physical health of caregivers would impact care recipients in some way, this null finding may be due to the measure of caregiver physical health that we incorporated, as the PILL assesses the frequency of occurrence of several common physical symptoms.18 It is possible that using a measure of perceived overall caregiver physical health would be more likely to demonstrate relationships with child HRQOL. Or, perhaps youth HRQOL is not the optimal child outcome to use in assessing this relationship. Alternatively, it is also possible that youth may not be aware of their caregivers' health status, particularly if caregivers shield them from this information in a protective manner. To our knowledge, this was the first study to examine caregiver physical health in pediatric SCI. Future research should continue exploring how caregiver physical health may impact the care that caregivers are able to provide in order to better understand the supports that caregivers may need as they care for their children.
Clinical implications
Results provide support for developing interventions to improve youth HRQOL by addressing caregiver problem solving. These findings are encouraging, as past problem-solving interventions have yielded successful results.24–27 For example, Sahler and colleagues24 observed positive effects for problem-solving training among mothers of youth recently diagnosed with cancer, including improved problem-solving skills and mood. Palermo et al25 found that problem-solving training for parent caregivers of youth with chronic pain demonstrated preliminary positive results on parents and youth. Elliott26 implemented a brief individualized problem-solving intervention with caregivers of adults with SCI and found caregivers in the intervention group to experience a decrease in dysfunctional problem solving. This research offers a start to clinicians and researchers working with youth with SCI and their families.
In terms of clinical practice, best practices in pediatric rehabilitation emphasize the involvement of caregivers28; modeling and directly teaching successful problem-solving skills should be incorporated throughout the various rehabilitation disciplines. This is true not only among families of patients with new injuries but also for youth with “older” injuries, as children will experience new physical and psychosocial challenges and gain additional personal resources with each new developmental phase.29 Each of these stages therefore offers new opportunities for collaboration and modeling for caregivers in terms of how to handle stressful situations that may arise.
Primary caregivers are arguably the most influential models in the lives of their children and embody their children's most immediate context.30 Caregivers can be the strongest resource and advocate for their children; as rehabilitation professionals we should make it a goal to strengthen their capacity. Although not readily explored in the research literature, stress is a normative response for parents after their child sustains (and then lives with) a serious, permanent disability. Our role as pediatric providers should therefore involve establishing and strengthening parents' skills (like problem solving) to encourage positive outcomes for youth and their families. Improving caregiver problem solving should improve caregivers' ability to manage their children's needs, thereby relieving their burden and positively impacting health and HRQOL for their children and themselves.
Limitations
There are several limitations to this research. First, our sample size was relatively small, and although geographically diverse, caregivers were highly educated and were primarily limited to one pediatric health care system. Further, to be included in the current study, participants needed to be willing and able to travel to Chicago for a 2-day (all expenses paid) in-person intervention. Future research should examine these hypotheses among larger samples in order to better represent the population of families living with pediatric SCI. Second, this research was cross-sectional; longitudinal research is needed to truly identify predictive relationships. Finally, because no version of the PedsQLTM exists for youth with mobility impairments, 2 questions on the Physical Health Scale refer to walking, so were irrelevant for many of the youth who use wheelchairs in the current study. Future research should strive to identify a more appropriate measure of HRQOL for youth with SCI.
Conclusion
Among this sample of caregivers of youth with SCI, caregiver problem solving contributed significantly to child physical and psychosocial HRQOL. While further research should explore relationships among larger samples, results indicate caregiver problem solving is a reasonable target for intervention to improve HRQOL among youth with SCI.
Acknowledgments
This research was funded by a grant from the Craig H. Neilsen Foundation. The authors wish to thank the caregivers and their children with SCI who participated in this research.
The authors report no conflicts of interest.
REFERENCES
- 1.Elliott TR, Shewchuk RM. Recognizing the family caregiver: Integral and formal members of the rehabilitation process. J Vocat Rehabil. 1998;10:123–132. [Google Scholar]
- 2.Friedman D, Holmbeck GN, Jandasek B, Zukerman J, Abad M. Parent functioning in families of preadolescents with spina bifida: Longitudinal implications for child adjustment. J Fam Psychol. 2004;18(4):609–619. doi: 10.1037/0893-3200.18.4.609. [DOI] [PubMed] [Google Scholar]
- 3.Varni JW, Setoguchi Y. Effects of parental adjustment on the adaptation of children with congenital or acquired limb deficiencies. J Dev Behav Pediatr. 1993;14(1):13–20. [PubMed] [Google Scholar]
- 4.Kelly EH, Anderson CJ, Garma S et al. Relationships between the psychological characteristics of youth with spinal cord injury and their primary caregivers. Spinal Cord. 2011;49:200–205. doi: 10.1038/sc.2010.78. [DOI] [PubMed] [Google Scholar]
- 5.Boyer BA, Knolls ML, Kafkalas CM, Tollen LG, Swartz M. Prevalence and relationships of posttraumatic stress in families experiencing pediatric spinal cord injury. Rehabil Psychol. 2000;45(4):339–355. [Google Scholar]
- 6.Wysocki T, Iannotti R, Weissberg-Benchecll J et al. Diabetes problem solving by youths with type 1 diabetes and their caregivers: Measurement, validation, and longitudinal associations with glycemic control. J Pediatr Psychol. 2008;33(8):875–884. doi: 10.1093/jpepsy/jsn024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cousino MK, Hazen RA. Parenting stress among caregivers of children with chronic illness: A systematic review. J Pediatr Psychol. 2013;38(8):809–828. doi: 10.1093/jpepsy/jst049. [DOI] [PubMed] [Google Scholar]
- 8.Billings AG, Moos RH. Comparisons of children of depressed and nondepressed parents: A social-environmental perspective. J Abnorm Child Psychol. 1983;11(4):463–486. doi: 10.1007/BF00917076. [DOI] [PubMed] [Google Scholar]
- 9.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39(8):800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Whiteneck GG. Measuring what matters: Key rehabilitation outcomes. Arch Phys Med Rehabil. 1994;75:1073–1076. doi: 10.1016/0003-9993(94)90080-9. [DOI] [PubMed] [Google Scholar]
- 11.Elliott TR, Shewchuk RM, Richards JS. Caregiver social problem-solving abilities and family member adjustment to recent-onset physical disability. Rehabil Psychol. 1999;44(1):104–123. [Google Scholar]
- 12.Dasch KB, Russell HF, Kelly EH et al. Coping in caregivers of youth with spinal cord injury. J Clin Psychol Med Settings. 2011;18:361–371. doi: 10.1007/s10880-011-9258-z. [DOI] [PubMed] [Google Scholar]
- 13.Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: A longitudinal study. Gerontologist. 1986;26(3):260–266. doi: 10.1093/geront/26.3.260. [DOI] [PubMed] [Google Scholar]
- 14.Murphy NA, Christian B, Caplin DA, Young PC. The health of caregivers for children with disabilities: Caregiver perspectives. Child Care Health Dev. 2006;33(2):180–187. doi: 10.1111/j.1365-2214.2006.00644.x. [DOI] [PubMed] [Google Scholar]
- 15.Kelly AF, Hewson PH. Factors associated with recurrent hospitalization in chronically ill children and adolescents. J Paediatr Child Health. 2000;36:13–18. doi: 10.1046/j.1440-1754.2000.00435.x. [DOI] [PubMed] [Google Scholar]
- 16.Llewellyn G, Dunn P, Fante M, Turnbull L, Grace R. Family factors influencing out-of-home placement decisions. J Intellect Disabil Res. 1999;43(3):219–233. doi: 10.1046/j.1365-2788.1999.00189.x. [DOI] [PubMed] [Google Scholar]
- 17.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 18.Pennebaker JW. The Pennebaker Inventory of Limbic Languidness (the PILL) In: Pennebaker JW, editor. The Psychology of Physical Symptoms. New York: Springer-Verlag; 1982. [Google Scholar]
- 19.Zarit SH, Reever KE, Back-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- 20.Bédard M, Molloy DW, Squire L et al. The Zarit Burden Interview: A new short version and screening version. Gerontologist. 2001;41(5):652–657. doi: 10.1093/geront/41.5.652. [DOI] [PubMed] [Google Scholar]
- 21.D'Zurilla TJ, Nezu AM, Maydeu-Olivares A. Social Problem-Solving Inventory-Revised (SPSI-R): Technical Manual. North Tonawanda, NY: Multi-Health Systems, Inc.; 2002. [Google Scholar]
- 22.Tabachnick BG, Fidell LS. Using Multivariate Statistics. New York: Harper Collins College Publishers; 1996. [Google Scholar]
- 23.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 24.Sahler OJ, Fairclough DL, Phipps S et al. Using problem-solving skills training to reduce negative affectivity in mothers of children with newly diagnosed cancer: Report of a multisite randomized trial. J Consult Clin Psychol. 2005;73(2):272–283. doi: 10.1037/0022-006X.73.2.272. [DOI] [PubMed] [Google Scholar]
- 25.Palermo TM, Law EF, Essner B, Jessen-Fiddick T, Eccleston C. Adaptation of problem-solving skills training (PSST) for parent caregivers of youth with chronic pain. Clin Pract Pediatr Psychol. 2014;(3):212–223. doi: 10.1037/cpp0000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elliott TR, Berry JW. Brief problem-solving training for family caregivers of persons with recent-onset spinal cord injuries: A randomized controlled trial. J Clin Psychol. 2009;65(4):406–422. doi: 10.1002/jclp.20527. [DOI] [PubMed] [Google Scholar]
- 27.Wade SL, Walz NC, Carey J et al. A randomized trial of teen online problem solving: Efficacy in improving caregiver outcomes after brain injury. Health Psychol. 2012;31(6):767–776. doi: 10.1037/a0028440. [DOI] [PubMed] [Google Scholar]
- 28.Lucas LR. Psychosocial aspects of pediatric rehabilitation. In: Alexander MA, Matthews DJ, editors. Pediatric Rehabilitation: Principles and Practice. New York: Demos Medical Publishing; 2010. [Google Scholar]
- 29.Chavelier Z, Kelly EH, Jones K. An overview of psychosocial adjustment after pediatric spinal cord injury. In: Mulcahey MJ, Betz R, Vogel LC, Zebracki K, editors. Child with a Spinal Cord Injury. 2nd ed. London: MacKeith Press; 2014. [Google Scholar]
- 30.Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]


