Abstract
Background: The management of neurogenic bowel and bladder by individuals with spinal cord injury (SCI) often requires a complicated set of behaviors to optimize functioning and reduce complications. However, limited research is available to support the many recommendations that are made.
Objective: To describe the occurrence of behaviors associated with the management of neurogenic bowel and bladder among individuals with chronic SCI and to explore whether relationships exist between the performance of those behaviors and outcomes related to health and quality of life.
Methods: A survey was developed based on clinical guidelines to collect self-report information about the performance of specific behaviors associated with the management of neurogenic bowel and bladder by individuals with SCI. It was administered to 246 individuals with chronic SCI living in the community as part of a larger ongoing study.
Results: Results suggest that the methods that those with SCI use to manage neurogenic bowel and bladder are multifaceted. Many methods are performed with significant consistency, but significant variations exist for some and are often associated with neurological status, methods of evacuation, and quality of life.
Conclusion: Many people with SCI of long duration are not sure of the sources of recommendations for some of the management activities that they or their personal care assistants conduct. It is prudent for clinicians working with these people to review their recommendations periodically to ensure that they are current and understood.
Keywords: health behaviors, neurogenic bladder, neurogenic bowel
The vast majority of those with spinal cord injury (SCI) have associated bladder and bowel dysfunction that negatively impacts quality of life (QOL).1 While some progress has been made in bladder management and prevention of medical complications, bowel management and complications after SCI have been understudied such that many recommendations in US guidelines2 are based on expert opinion rather than research. Furthermore, very few studies have focused on behavioral factors associated with bladder and bowel dysfunction and management.
Bladder dysfunction refers to problems with voiding urine and abnormalities in bladder function.3 For individuals with a neurogenic bladder, voiding is often the result of conscious planning and use of external supplies. Neurogenic bowel dysfunction is usually characterized by lower gastrointestinal symptoms, such as loss of voluntary control over bowel movements, difficulty with evacuation, and loss of stool. It is a major physical and psychosocial problem for individuals with SCI, as changes in bowel motility and sphincter control, coupled with impaired mobility and hand dexterity, make bowel management a time-consuming, major life-limiting problem. Unlike bladder management, there are no clearly distinct bowel management methods, with the exception of colostomies, ileostomies, and antegrade continence enema/Malone antegrade continence enema (ACE/MACE) procedures. Instead, bowel management methods consist of a combination of prescribed treatments, such as a high-fiber diet, adequate hydration, oral or rectal medications, along with digital rectal stimulation, manual evacuation, suppositories, flushing, and enemas or mini-enemas, depending on each person's health needs and characteristics.
There is very limited clinical information on bowel management to aid clinicians caring for people with SCI and neurogenic bowel.4 The current US guidelines for neurogenic bowel management are outdated and require a stronger evidence base. Especially lacking from the guidelines2 are key behavioral and psychosocial factors, which can influence the acceptability of and adherence to treatment regimens. Adherence to recommendations that are tailored to patients' lifestyles can be crucial to preventing complications.5 Educating individuals with SCI, their families, and caregivers about approaches to prevent bladder and bowel complications is critical to living well with SCI.
The specific questions related to the behavioral management of neurogenic bowel and bladder that were explored in this study were:
(1) What behaviors do individuals with SCI perform to manage their bowels and bladder?
(2) Are there response patterns that are related to either demographic or injury-related characteristics?
(3) Does an association exist between the consistency of performance of specific behaviors and secondary conditions, relationships with a care providers, and QOL?
(4) Can a subset of items be identified for use in the future that may be valuable in encouraging specific behaviors or management patterns?
Methods
This study was reviewed and received approval from the institutional review board at a large academic medical center in the Midwest. Procedures followed the approved protocol in accordance with ethical standards. Subjects were recruited in SCI clinics, following completion of interviews for another study of people with SCI, and via flyers that were left in Urology and Physical Medicine and Rehabilitation (PM&R) clinics and were posted on a PM&R research program's website. We recruited 246 adults who had lived with SCI for at least 5 years. Additional inclusion criteria were having neurogenic bowel and/or bladder, English-speaking, and ASIA Impairment Scale6 grades of A to D inclusive.
Procedure
Trained interviewers conducted phone and in-person interviews. The assessments used in this study occurred over 2 years and 3 months and were imbedded in the data collection for a larger study that took between 1 and 2 hours.
Development of a questionnaire
The survey assessing health behaviors for this study – hereafter referred to as the Bladder and Bowel Behavioral Management Questionnaire (B3MQ) – was developed to assess the extent to which individuals with SCI conduct behaviors associated with the management of neurogenic bowel and bladder and the prevention of secondary conditions. Items for the B3MQ were developed based on clinical guidelines and recommendations for management of neurogenic bowel and bladder provided in Yes, You Can! A Guide to Self-Care for Persons with Spinal Cord Injury7 and the Consortium for Spinal Cord Medicine,2,3 as well as through input provided by physiatrists, urologists, and psychologists experienced with individuals with SCI. All items were reviewed and refined by a team of expert clinicians.
The basic questionnaire consists of 40 items that can be supplemented by 2 additional multipart items in order to gather information about identified health care and methods of bladder and bowel emptying. Self-report responses reflect the frequency of performance of method-specific and universal behaviors for both bowel and bladder management. Most items refer to the frequency of behaviors during the last 4 weeks on a 5-point Likert-type scale: never (0%), rarely (1%–20% of the time), sometimes (21%–69% of the time), often (70%–99% of the time), and always (100% of the time), as well as not applicable (NA).
Questionnaire piloting and revision
The measure was piloted with 7 individuals by 2 interviewers during July and August of 2012; information was collected about the experience of both participants and interviewers. Trained interviewers took approximately 15 minutes to administer the B3MQ over the phone as a structured interview. A primary issue that arose was that pilot participants could not specify the bowel and bladder management regimens that were prescribed to them or to identify the health care provider who provided those instructions/recommendations. There were other issues regarding question wording and response choices.
The revised B3MQ was easier to understand and instructions and items were revised based on interviewer feedback. The most significant change was in the context of the questions; rather than asking participants if behaviors were “performed as recommended,” interviewers asked only if behaviors were “performed.” The former approach assumed that clear recommendations were given by appropriate clinicians and recalled by participants, but participants did not always know the source of recommendations, which often was personal reading or advice from nonclinicians.
Other measures
Data were collected on demographics (gender, age, race/ethnicity, education, vocational status, marital status, primary living situation) and injury characteristics (years since injury, neurological status, level of injury). Bladder- and bowel-related status and QOL were assessed with the following instruments:
(a) Selected items from the Bowel and Bladder Treatment Index8 (BBTI), which addresses methods of bowel and bladder management, satisfaction with these methods, complications, and QOL.
(b) The SF-Qualiveen,9 an 8-item questionnaire that assesses the interference of urinary problems with QOL, with 2 items addressing each of the following areas: feeling bothered by limitations, frequency of limitations, fears, and feelings. Item scores range from 0 to 4, with lower scores indicating less interference. The total score is the mean of the subscale's scores.
(c) Spinal cord injury multidimensional Qualit y of Life (SCI-QOL), 10 a computerized adaptive test that produces T-scores. SCI-QOL scales for bladder complications, distress due to bladder management, distress due to bowel management, and ability to participate in social roles and activities were used. Higher T-scores reflect higher levels of the concepts measured (eg, if distress due to bowel management is measured, higher scores indicate greater distress; if ability to participate is measured, higher scores represent greater ability).
(d) Life Satisfaction Index, Form Z (LSI-Z)11 is a 13-item measure of life satisfaction. Scores range from 0 to 26, with higher scores reflecting greater life satisfaction.
Data analyses
Descriptive statistics, including frequency, percentages, means, and standard deviations (SD), were computed for relevant variables using IBM SPSS, version 22 (IBM, Inc., Armonk, NY). The quality and quantity of data available specified the type of analyses performed. Because of the small number of participants in each response category, when possible, categories of responses were combined to facilitate statistical analysis. When not limited by the small sample or cell sizes, differential statistics were calculated, including chi-square tests and tests of means (t tests, analysis of variance [ANOVA], and Kruskal-Wallis H tests). Because the current study is exploratory in nature, corrections for the conduct of multiple tests were not made. The significance level was set at p ≤ .05.
Results
Sample characteristics
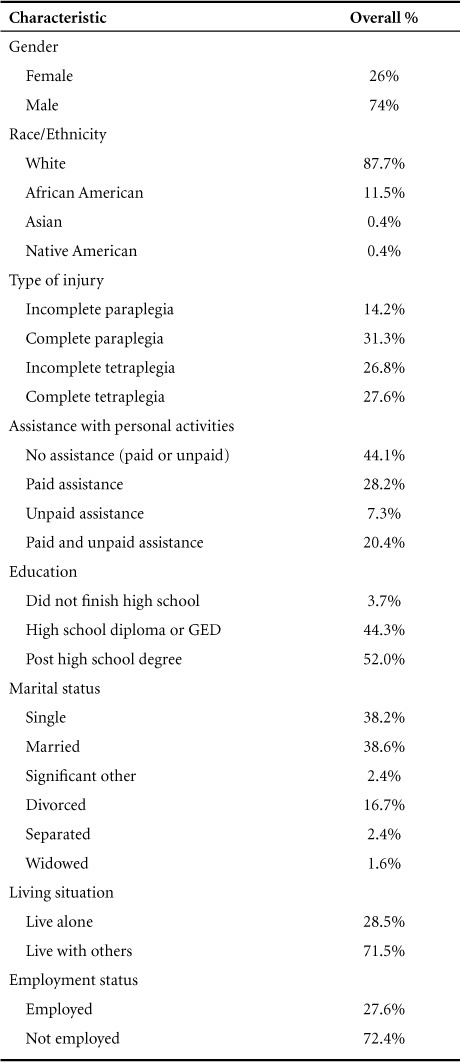
The sample for the current study included 246 people with SCI (mean age = 49.73 years, SD = 12.8), all of whom were at least 5 years post injury (mean = 18.73 years, SD = 10.2) and experienced neurogenic bowel or bladder (or both). As can be seen in Table 1, participants were primarily male, White, unemployed, and had completed high school. They varied with regard to neurological status. More than half of the participants reported receiving some type of assistance with personal activities.
Table 1.
Demographic characteristics of sample (N = 246)
Interactions with health care providers
The B3MQ contained several questions related to the extent that respondents worked with health care providers to manage their neurogenic bowel and bladder. In response to the question “Do you have a clinician who you work with on bladder-related issues?”, 71.8% of respondents responded “yes.” Of the 167 individuals who provided information about the type of clinician, 78.4% worked with a urologist, 10.8% worked with a physiatrist, 4.8% worked with a provider from internal medicine, and the remainder worked with various types of clinicians.
If they responded that they had a provider with whom they worked on bladder-related issues, a follow-up question was asked: “How often do you communicate with this healthcare provider when having bladder-related problems?” Of the 113 individuals who responded to this question, 5.3% reported “never,” 8% “rarely,” 16.8% “sometimes,” 20.4% “often,” and 49.6% “always.”
Only 50.1% of participants reported having a clinician with whom they worked on bowel-related issues. Among these, 62.7% indicated that this was a physiatrist. Other providers were from internal medicine (11%), family medicine (11%), gastroenterology (5.1%), and other disciplines (12.7%). Five individuals did not know the background of these clinicians.
In response to the follow-up question: “How often do you communicate with your health care provider when having bowel-related problems (such as constipation, bleeding, excessive pain, bloating)?”, there were 76 responses, with 13.2% reporting “never,” 15.8% “rarely,” 26.3% “occasionally,” 11.8% “often,” and 32.9% reporting “always.”
Frequency of behaviors
As previously noted, the majority of the questions on the B3MQ refer to the frequency of performance of behaviors during the previous 4 weeks. Tables 2, 3, and 4 provide a detailed breakdown of the responses to each of these items.
Table 2.
Percent reported adherence with bladder and bowel method-specific management
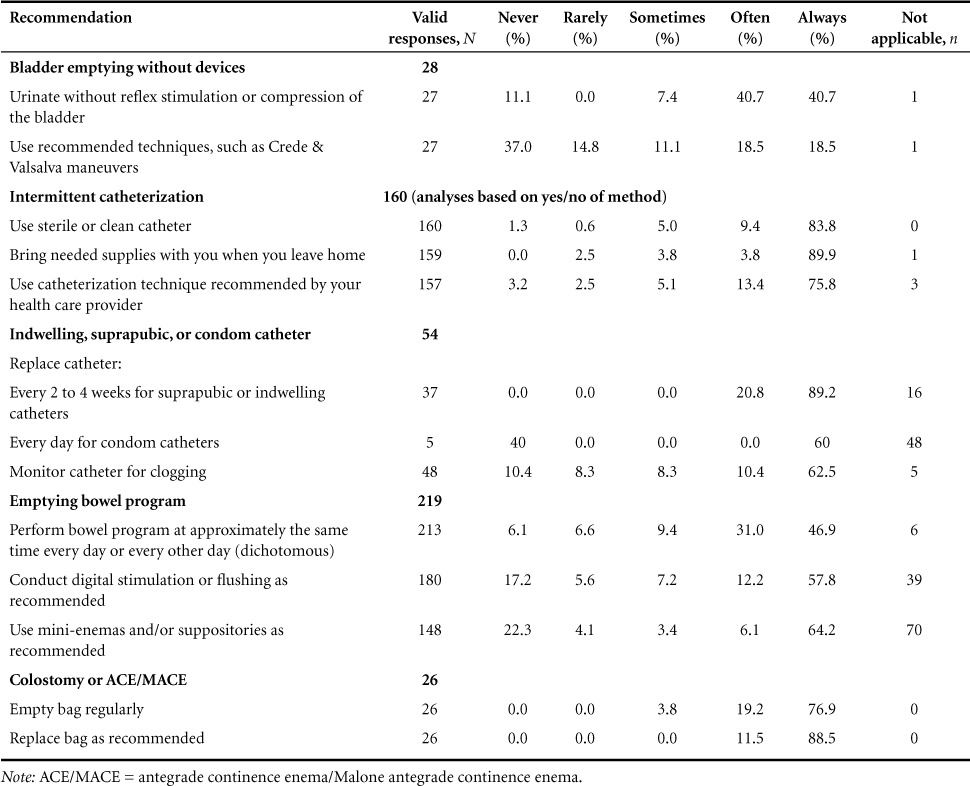
Table 3.
Frequency of performance of bladder management methods during the last 4 weeks
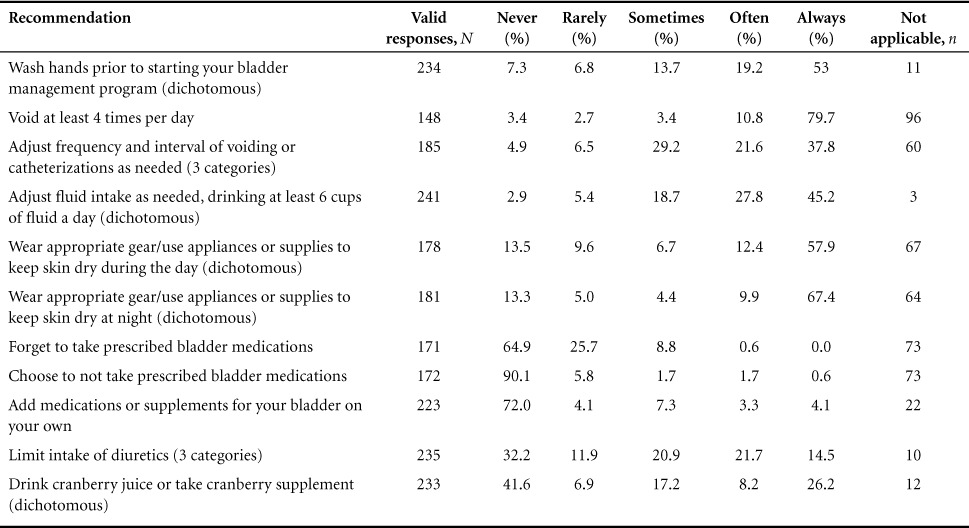
Table 4.
Frequency of performance of bowel management methods in the last 4 weeks (N = 246 respondents)

Method-specific management behaviors for both bladder and bowel are shown in Table 2. There was relatively little variation in responses about method-specific behaviors for the management of neurogenic bowel and bladder. Among the 28 individuals who empty their bladder without devices, more than 81% reported urinating without reflex stimulation or compression of the bladder “often or always.” Among those who used intermittent catheterization, the majority said that they always used sterile or clean catheters (83.8%), brought needed supplies when they left home (89.9%), and used the catheterization technique recommended by their health care provider (75.8%).
More variation was found related to bowel programs; most participants reported that they either “always” or “often” did each of the following: performed bowel program at the same time (77.9%), conducted digital stimulation or flushing (70%), and used mini-enemas and/or suppositories (70.3%).
Bladder management
Table 3 provides the responses to B3MQ items related to bladder management. When asked “Are there other activities that you regularly do for bladder management that were recommended by your health care provider?”, 90.6% of the sample answered “no.” The respondents who reported that they performed additional recommended bladder management behaviors listed a total of 23 different recommendations, including massaging the bladder for complete drainage, using a Foley catheter at night, avoiding sugary drinks, using a lubricant when cathing, flushing the catheter with vinegar and water, and having a urogram and cystoscopy annually.
There were 11.8% of participants who reported that they conducted behaviors for bladder management that were not recommended by a health care provider. Twenty-eight different behaviors were reported, including boiling catheters and then freezing them, taking D-Mannose daily for urinary tract infections (UTIs), taking lime oil monthly for UTIs, doing wheelchair pressure relief at end of catheterization, and drinking coffee.
In response to the open-ended question about frequency of drinking cranberry juice or taking a cranberry supplement, answers were clustered into 4 response categories: never, less than weekly, less than daily, and at least once per day. Differences in cranberry usage were found only as a function of neurological status (χ2 = 18.83; p = .027), with participants with more severe neurological impairments using cranberry more frequently.
Bowel management
Table 4 shows the responses to items related to bowel management. Most participants reported consuming enough fiber (73%) and drinking at least 6 cups of fluid a day “often” or “always” (81%), but other items in this category showed more variability. In particular, items associated with varying diet and medications (including laxatives) based on stool consistency were much more evenly reported across the response categories.
As part of the follow-up questions to items in the bowel management section, participants were asked about the frequency of adding either medications or supplements that were not recommended by a health care provider, and they provided 74 responses. Most of these reflected changes to diet and nutrition (eg, adding or adjusting intake of fiber and drinking juice) and taking over-the-counter laxatives, supplements, or stool softeners.
Of the 245 valid responses, only 2.9% reported regularly performing other activities for bowel management that were recommended by a health care provider. These included abdominal massage and using suppositories, laxatives, and dietary supplements.
The same percentage of individuals (2.9%) endorsed regularly performing other bowel management activities that were not recommended by a health care provider; they reported 20 different behaviors. These concerned changing diet and adding nutritional supplements, using enemas, and manipulating their bodies (eg, pressure on the abdomen; pulling on buttocks to assist with evacuation; and straining, pushing, and rocking). Other behaviors that were reported included smoking cigarettes, drinking herbal laxative tea, using marijuana to generate a deep cough, and walking.
Associated characteristics and outcomes
Seventeen behaviors listed on the B3MQ had sufficient variability in responses (operationalized as having less than 80% of responses at either end of the response continuum) to examine further. For each of these, responses were re-categorized into either 2 (never/rarely/sometimes and often/always) or 3 (never/rarely, sometimes, and often/always) categories to reduce response choices and allow for additional analyses. After assumptions were checked, differential statistics were calculated to determine whether relationships existed between self-reported frequency in performing behaviors and both demographic/injury characteristics and health-related outcomes. When appropriate, post hoc analyses were performed to provide more information about group differences. Table 5 provides a summary of significant findings.
Table 5.
Significant findings between self-reported frequency in performing behaviors and demographic/injury characteristics and health-related outcomes
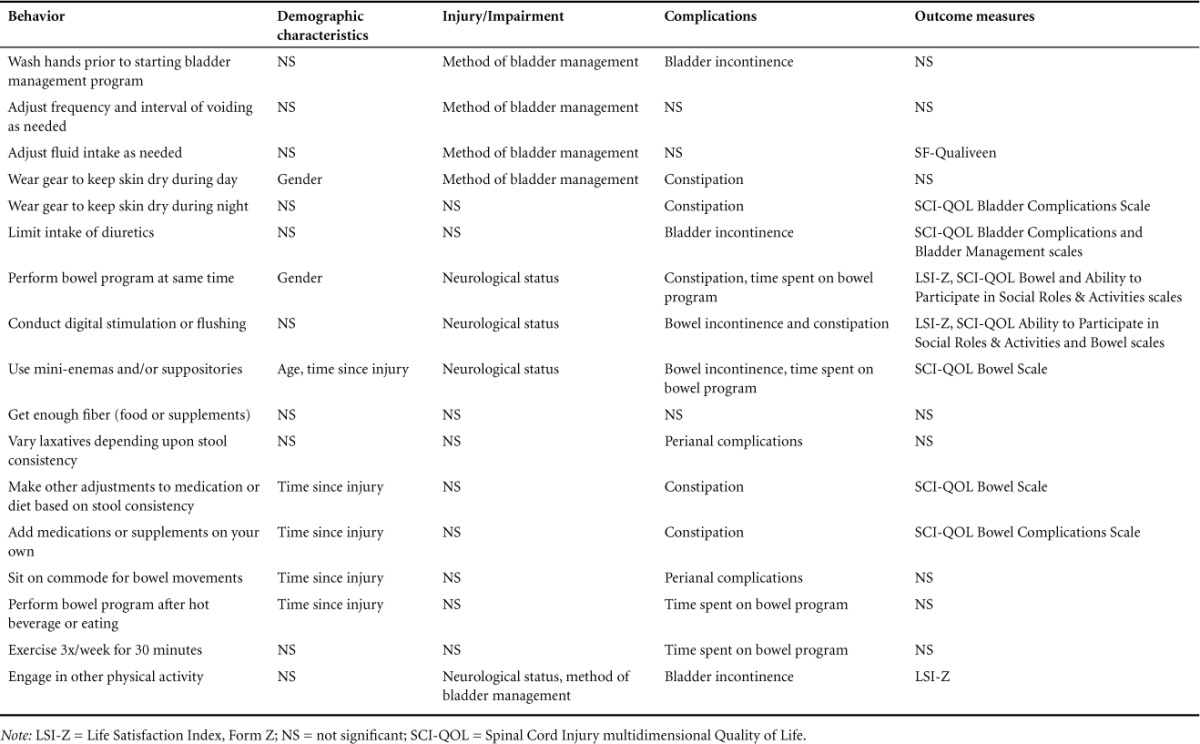
Wash hands prior to starting your bladder management program (2 categories). A significant difference was observed with method of bladder management (χ2 = 15.678; p < .001). Those who empty their bladders without devices were least likely to wash their hands, whereas those using an indwelling, suprapubic, or condom catheter were the most likely. Performance of hand washing was also associated with bladder incontinence (χ2 = 6.384; p = .041); those washing their hands often or always had fewer incidents. No relationship was found with UTIs (occurrence or frequency) or measures of QOL.
Adjust frequency and interval of voiding or catheterizations as needed (3 categories). There were no significant differences in frequency of this behavior as a function of gender, age, or time since injury. A significant relationship was observed with method of bladder management (χ2 = 7.73; p < .05); most of those not using devices reported doing this never or rarely while most who used intermittent catheterization reported doing this often or always. Frequency was not associated with health-related outcomes or QOL scores.
Adjust fluid intake as needed, drinking at least 6 cups of fluid a day (2 categories). Adjusting fluid intake was associated with method of bladder management (χ2 = 8.60; p = .014), with almost 90% of those using indwelling, suprapubic, or condom catheters reporting that they often or always made adjustments compared to about two-thirds of the other subjects. A relationship with SF-Qualiveen scores (t = 2.11; p = .036) was also observed; individuals who reported inconsistently adjusting their fluid intake had higher scores, indicating higher interference of urinary problems. No relationships with other measures of QOL or health-related complications were observed.
Wear appropriate gear/use appliances or supplies to keep skin dry during the day (2 categories). Frequency of performance was associated with gender (χ2 = 6.31; p = .012), method of bladder management (χ2 = 10.88; p = .004), and occurrence of significant constipation (χ2 = 8.31; p = .004). Females and those with significant constipation were more likely to keep their skin dry during the day, as were those using indwelling, suprapubic, or condom catheters. No other significant associations were observed.
Wear appropriate gear/use appliances or supplies to keep skin dry at night (2 categories). Differences in performance were found for scores on the SCI-QOL Bladder Complications Scale (t = −2.29; p = .024); those experiencing more impactful bladder complications were more likely to often or always conduct this activity, as were those with significant constipation. No other differences were observed.
Limit intake of diuretics such as caffeinated and diet drinks and alcohol (3 categories). Differences in performance were found for bladder incontinence (Kruskal-Wallis χ2 = 10.83; p = .004), with post hoc analyses suggesting significant differences between participants who responded never/rarely and sometimes (p = .005). Consistency in performance was also associated with differences on the SCI-QOL Bladder Complications (F = 6.62; p = .002) and Bladder Management (F = 5.85; p = .003) scales. Post hoc tests using Bonferroni correction found that Bladder Complications T-scores differed significantly between those reporting never/rarely and sometimes (p = .003) as well as between those reporting never/rarely and often/always (p = .007). No other differences were observed.
Perform bowel program approximately the same time every day or every other day (2 categories). Differences in methods of bowel and bladder management were not assessed. Performing this activity was associated with gender (χ2 = 9.88; p = .003), with males performing this activity more consistently than females. Differences were also found for neurological status (F = 15.60; p = .001), with individuals with complete tetraplegia being most likely to often or always show consistency and those with incomplete paraplegia being most likely to never/rarely/sometimes be consistent.
Consistency of performing bowel program was related to constipation (χ2 = 5.81; p = .020) and average time spent on bowel program (χ2 = 9.03; p = .029). Individuals were more likely to be consistent who did not experience significant constipation and who spent more time on their bowel programs, with those averaging more than 90 minutes being the most likely to report being consistent often or always. Consistency was also significantly associated with scores on 3 QOL measures: the LSI-Z (t = −2.58; p = .011), with respondents who were less consistent having lower scores; the SCI-QOL Bowel Distress Scale (t = 2.18; p = .030), with respondents who were less consistent having scores indicative of greater bowel problems; and the SCI-QOL Ability to Participate in Social Roles & Activities (t = −2.12; p = .035), with individuals who were less consistent reporting lower levels of health-related QOL in this area.
Conduct digital stimulation or flushing (2 categories). Regular performance of digital stimulation or flushing was found to differ significantly as a function of neurological status (χ2 = 42.07; p < .001), with individuals with complete injuries (both paraplegia and tetraplegia) being more likely to perform these behaviors often or always than those with incomplete injuries. Regularly performing digital stimulation or flushing was also associated with bowel incontinence (χ2 = 4.09; p = .043) and constipation (χ2 = 6.45; p = .014); those performing digital stimulation or flushing regularly were less likely to report either complication. Regular performance was also associated with better life satisfaction, as indicated by higher LSI-Z scores (t = −2.54; p = .012) and the SCI-QOL Ability to Participate in Social Roles & Activities Scale (t = −2.02; p = .045), and lower scores on the SCI-QOL Bowel Scale (t = 2.12; p = .036).
Use of mini-enemas and/or suppositories (2 categories). Significant differences in use were found for both age and time since injury, with younger individuals (t = 2.81; p = .006) and those with shorter durations of SCI (t = 2.39; p = .018) being more likely to report regular use. Use patterns also differed by neurological status (χ2 = 27.16; p < .001); individuals with complete tetraplegia were most likely to often or always use mini-enemas or suppositories.
In terms of complications, differences in use were associated with bowel incontinence (χ2 = 3.71; p = .054) and average time spent on the bowel program (χ2 = 37.35; p < .001). Those who had bowel incontinence once a month or less were more likely to regularly use mini-enemas or suppositories, as were those who spent at least 60 minutes on their bowel programs. Regular use of mini-enemas and suppositories was also associated with better health-related QOL as reflected by scores on the SCI-QOL Bowel Scale (t = 2.021; p = .045).
Eat enough high fiber foods or take fiber supplement (2 categories). No differences were found in frequency of performance of this behavior as a function of any of the factors assessed.
Take more or less laxatives depending on stool consistency (2 categories). Differences in performance of this behavior were found for the incidence of any perianal complications (χ2 = 4.90; p = .027), with individuals who vary the frequency of laxatives often or always being less likely to report their occurrence.
Make other adjustments to medication or diet based on stool consistency (3 categories). Differences were observed as a function of time since injury (F = 4.45; p = .013), with those who sometimes made adjustments having the longest durations of SCI. Differences in the frequency of making adjustments was also associated with constipation (c2 = 6.83; p = .033) and SCI-QOL Bowel scores (F = 9.70; p < .001). The highest rate of constipation occurred among those who never/rarely made adjustments, whereas post hoc analyses of SCI-QOL Bowel t-tests scores showed that those who responded never/rarely had significantly lower scores than either those who responded sometimes (p = .002) or often/always (p = .001).
Add (bowel-related) medications or supplements. Responses to this question were dichotomized differently (never/rarely and sometimes/often/always) than the other questions. Responses differed as a function of time since injury (t=−2.91;p=.004),with those with longer durations of SCI adding medications or supplements more regularly. Differences in performance of this behavior were also found for the occurrence of constipation (χ2 = 6.80; p = .009) and scores on the SCI-QOL Bowel Complications Scale (t = −4.39; p < .001); those who were more likely to regularly add medications and supplements had more problems with bowel complications. No other differences were observed.
Sit on commode or toilet during bowel movements (2 categories). Time since injury was associated with regularly sitting on a commode or toilet, with those who did so often or always having longer durations of injury (t = 3.383; p = .001). Differences in performance of this behavior were associated with perianal complications (χ2 = 7.018; p = .008); respondents who consistently sit on a commode or toilet were more likely to report experiencing these complications.
Perform bowel program 30 minutes to 1 hour after drinking a hot beverage or eating (3 categories). Responses were associated with time since injury (F = 3.693; p = .027); those who said they sometimes did this activity had longer durations of SCI than those saying they did so more or less often. Responses were also related to average time spent on bowel program (Kruskal-Wallis χ2 = 9.30; p = .010); post hoc analyses revealed that individuals who sometimes did this had significantly longer durations than those who did so often or always (p = .032).
Exercise 3 times per week for 30 minutes (3 categories). Difference in performance of this activity were associated with time spent on one's bowel program (χ2 = 15.069, p = .020), with a majority of those spending less than 30 minutes exercising often or always while a majority of those spending more than an hour exercised never or rarely.
Engage in other physical activity for at least 30 minutes weekly (3 categories). Differences in engagement in this activity were associated with neurological category (χ2 = 20.005; p = .003), with a majority of those with complete paraplegia endorsing participation in this activity often or always and a majority of those with complete tetraplegia doing so never or rarely. Differences were also observed as a function of type of bladder management (χ2 = 10.098; p = .028), with 50% of those emptying without devices doing this often or always and 51% of those using indwelling, suprapubic, or condom catheters never or rarely doing so. Frequency of engagement in other physical activities was also associated with frequency of bladder incontinence (χ2 = 10.841; p = .028); those never or rarely participating in this activity were more likely to experience incontinence less than monthly. Engaging in this activity was also associated with LSI-Z scores (t = 4.566, p = .011), with those who do this activity never or rarely having the lowest levels of life satisfaction.
Discussion
The B3MQ was developed to examine the types and frequencies of various health behaviors used in managing neurogenic bowel and bladder. Participant responses provide insight into the consistency with which individuals post SCI for at least 5 years perform these behaviors. In particular, these responses allow us to address the objectives of this study with regard to (a) the behaviors that individuals with SCI perform to manage their bowels and bladder; (b) the existence of response patterns related to either demographic or injury-related characteristics; (c) associations between specific behaviors and secondary conditions and QOL; and (d) identification of a subset of behaviors that may be valuable to encourage to promote health and QOL, at least within cohorts of the SCI population. Results do not allow for addressing issues of causality.
Study results indicate that people with SCI of long duration are fairly consistent; almost all conduct certain specific behaviors for management of neurogenic bladder or hardly ever do so. Many of these are method-specific behaviors (highlighted in Table 2) while some are universal recommendations (highlighted in Tables 3 and 4).
Some sets of responses highlighted inconsistencies in attribution. In particular, there was significant overlap between the “other behaviors that were performed” that were recommended or not recommended by a health care provider. This suggests that individuals with SCI of long duration often do not know where they learned to do some of their management behaviors. This is likely to be less common among people with recent injuries.
When inferential statistics were performed to assess associations between the behaviors on the B3MQ and demographic and injury-related characteristics, complications, and outcomes, only a limited number of significant associations were found. In general, demographic characteristics were not associated with performance of bowel- and bladder-related behaviors. Females were more likely to wear/bring gear to keep their skin dry during the day and males were more likely to perform bowel program at a consistent time, but no other gender differences were noted.
Age was only significant as associated with the use of mini-enemas and/or suppositories; younger individuals were more likely to report regular use. This finding is also echoed by the association between enema/suppository use and time since injury; participants with shorter durations of SCI also were more likely to report regular use. Longer time since injury was associated with more willingness to make adjustments to diet and use of supplements and medications, whether with or without physician approval, as well as to regularly sit on a commode or toilet during bowel movements.
Neurological level and method of bladder management were significantly related to a number of behaviors. It is likely that level of injury and type of bladder management influenced the performance of these behaviors rather than vice versa. As might be expected, individuals using intermittent catheterization were more likely to wash their hands prior to starting bladder management program, to regularly sit on the toilet for the bowel program, and to adjust the frequency and interval of voiding as needed. They were less likely to either adjust fluid intake as needed or to wear gear to keep skin dry during day than were those using indwelling, suprapubic, or condom catheters. Unlike for those using indwelling or suprapubic catheters, for people doing intermittent catheterization, increasing fluid intake increases the time required for the bladder programs.
With regard to neurological level, significant differences were found related to regularly engaging in other types of physical activity, performing bowel program at a consistent time, conducting digital stimulation or flushing, and using enemas or suppositories. With regard to physical activity, a majority of those with complete paraplegia engaged in other physical activity for at least 30 minutes often or always and a majority of those with complete tetraplegia did so never or rarely. Individuals with complete tetraplegia were most likely to often or always be consistent in performing their bowel program at the same time every day or every other day, while those with incomplete paraplegia were the least likely to be consistent. Those with complete injuries (both paraplegia and tetraplegia) were more likely to conduct digital stimulation or flushing often or always. Finally, individuals with complete tetraplegia were more likely to regularly use mini-enemas or suppositories.
This study found that individuals with fewer incidents of bladder incontinence reported washing their hands more consistently, being more likely to limit their intake of diuretics, and being more likely to engage in other physical activities for at least 30 minutes 3 times a week. Those with significant constipation were more likely to wear gear both during the day and night to keep their skin clean and dry; were less likely to regularly perform digital stimulation or flushing; were less likely to consistently perform bowel program at same time; and were more likely to add medications or make other adjustments to medication or diet based on stool consistency. Those with perianal complications were less likely to vary laxatives depending upon stool consistency and were more likely to sit on a commode for bowel movements. Finally, bowel incontinence was associated with less consistent use of digital stimulation or flushing and more use of mini-enemas or suppositories.
Time spent on bowel programs was associated with several behaviors. Those who spent more time on their bowel program were more likely to often or always wash their hands prior to starting their bladder management, to consistently perform their bowel program at the same time each day, and to consistently use enemas or suppositories, and they were less likely to consistently perform bowel program after hot beverages or eating or to exercise 3 times weekly.
Several behaviors performed to manage neurogenic bowel and bladder were associated with QOL. Individuals with higher levels of general QOL (as reflected by LSI-Z scores) were more likely to engage in other levels of physical activity, to regularly perform digital stimulation or flushing, and to more consistently perform their bowel programs at the same time each day. Consistent timing of the bowel program and regular performance of digital stimulation were also related to greater ability to participate in social roles and activities.
With regard to health-related QOL and bladder functioning, individuals with better scores on the SF-Qualiveen were more likely to consistently adjust fluid intake as needed. Better scores on the SCI-QOL bladder scales were associated with regularly limiting intake of diuretics; in contrast, lower bladder-related QOL was associated with consistently wearing gear to keep skin dry during the night. Lower levels of bowel-related QOL were associated with less consistency in the timing of one's bowel program and less regularity in conducting digital stimulation/flushing and in using mini-enemas and suppositories and with increased consistency in making other adjustments to medication or diet based on stool consistency.
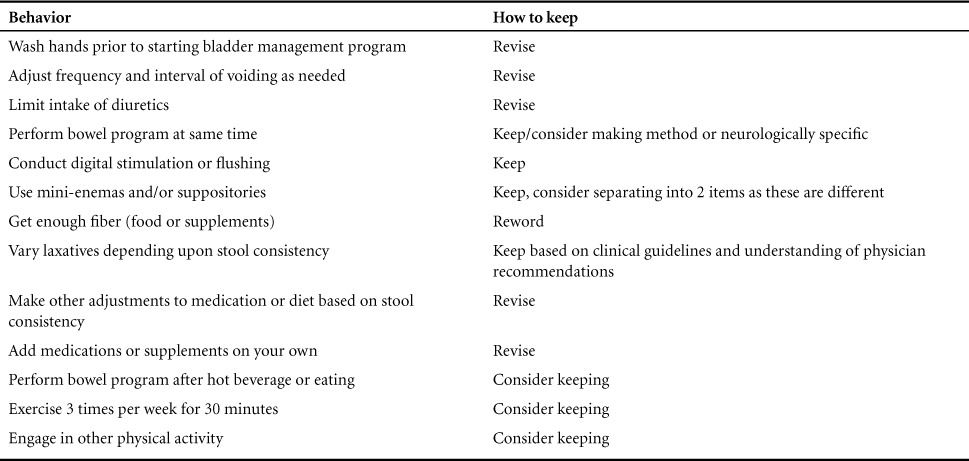
A set of 13 questions that deserve further exploration are listed in Table 6. Some of these seem appropriate as they are written, while others appear to need to be reworded. Also, a few items that are currently asked in the context of either bowel or bladder management appear to be useful across both.
Table 6.
Items to keep and continue to assess in future versions of the B3MQ (either as written or in a revised manner)
Limitations
This study has several limitations that must be acknowledged. The way questions were presented to participants – that is, over the phone by an interviewer and with a particular phrasing – may have increased the tendency of participants to answer in a way that was socially desirable such that responses reflected perceived expectations. Also, the B3MQ was administered immediately following the BBTI, which included detailed questions about methods of bowel and bladder management, medication, laxative and suppository use, and complications. This overlap likely led to an underreporting on the B3MQ, as participants may have felt they had already answered these questions. Also, the number of analyses that were conducted was quite large, increasing the likelihood that some “significant” findings were chance associations.
This was a cross-sectional study, which makes it impossible to draw conclusions about causality. Additionally, due to the relatively small sample, multivariate analyses could not be conducted to control for external factors. Finally, generalizability of the results of this study may be limited by where the sample was drawn from; because participants were primarily recruited through sites associated with an SCI Model System, their standard of care might not be typical but rather reflect better access and consistency of recommendations. Also, the long average time since injury may limit the ability to draw conclusions about “people with SCI.” People with long-term SCI have developed habits, and their understanding of whether their practices were recommended by a clinician or obtained from another source (eg, web postings or friends) is less likely to be accurate than are the recollections of people with recent injuries.
Conclusions
Findings from this study provide insight into the range and frequency of behaviors that individuals with chronic SCI perform for management of neurogenic bowel and bladder. In general, there was little relationship between patterns of responses and either demographic or injury-related characteristics. Individuals reported more consistent patterns of performance for method-specific management approaches, such as colostomy and indwelling catheters, and more variability in behaviors conducted to manage their bowel programs that are considered pertinent for everyone.
Although the B3MQ appears to need additional refinement before it is useful as a clinical tool, results of this study illuminate the need for health care providers to talk with their SCI patients about their understanding of prescribed treatments for the management of neurogenic bowel and bladder. Providers can also clarify other recommendations that they may have or that their patients may have learned of from other sources, such as herbal supplements and over-the-counter medications and their potential drug interactions. Providers should explain and teach the skills needed so that patients can follow recommendations to vary the medications, laxatives, and supplements for bowel management based on stool consistency.
Acknowledgments
The authors declare that they have no conflicts of interest to report. All procedures performed with human participants were in accordance with the ethical standards of the Institutional Research Committee and with the 1964 Helsinki Declaration and its later amendments. Informed consent was obtained from all individual participants in the study. Funding for this research was provided to the University of Michigan SCI Model Systems through grants 90SI5000-0103 from NIDRR/NIDLIR. Joanna Jennie assisted in the preparation of this manuscript.
REFERENCES
- 1.Benevento BT, Sipski ML. Neurogenic bladder, neurogenic bowel, and sexual dysfunction in people with spinal cord injury. Phys Ther. 2002;82(6):601–612. [PubMed] [Google Scholar]
- 2.Consortium for Spinal Cord Medicine. Clinical practice guidelines: Neurogenic bowel management in adults with spinal cord injury. J Spinal Cord Med. 1998;21(3):248–293. doi: 10.1080/10790268.1998.11719536. Available at: http://www.pva.org/atf/cf/%7BCA2A0FFB-6859-4BC1-BC96-6B57F57F0391%7D/cpg_neurogenic%20bowel.pdf. Accessed on December 1, 2015. [DOI] [PubMed] [Google Scholar]
- 3.Consortium for Spinal Cord Medicine. Bladder management for adults with spinal cord injury: A clinical practice guideline for health-care providers. J Spinal Cord Med. 2006;29:527–573. Available at: http://www.pva.org/atf/cf/%7BCA2A0FFB-6859-4BC1-BC96-6B57F57F0391%7D/CPGBladderManageme_1AC7B4.pdf. Accessed on December 1, 2015. [PMC free article] [PubMed] [Google Scholar]
- 4.Stiens SA, Bergman SB, Goetz LL. Neurogenic bowel dysfunction after spinal cord injury: Clinical evaluation and rehabilitative management. Arch Phys Med Rehabil. 1997;78:S86–S102. doi: 10.1016/s0003-9993(97)90416-0. [DOI] [PubMed] [Google Scholar]
- 5.Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment: Three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26(5):331–342. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 6.Kirshblum SC, Burns SP, Biering-Sørensen F et al. International Standards for Neurological Classification of Spinal Cord Injury 2011 revision. J Spinal Cord Med. 2011;34(6):535–546. doi: 10.1179/204577211X13207446293695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burns SP, Hammond MC, editors. Yes, You Can! A Guide to Self-Care for Persons with Spinal Cord Injury. 4th ed. Washington, DC: Paralyzed Veterans of America; 2009. http://www.sh-sci.org/index.php?option=com_docman&task=cat_view&gid=43&Itemid=31. Accessed December 1, 2015. [Google Scholar]
- 8.Forchheimer M, Tate DG, Chiodo A et al. The International Spinal Cord Injury Data Sets for Bowel and Bladder: Development of interview forms. Top Spinal Cord Inj Rehabil. 2013;19(suppl 1):S35. [Google Scholar]
- 9.Bonniaud V, Bryant D, Parratte B, Guyatt G. Development and validation of the short form of a urinary quality of life questionnaire: SF-Qualiveen. J Urol. 2008;180(6):2592–2598. doi: 10.1016/j.juro.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 10.Tulsky DS, Kisala PA, Victorson D et al. Overview of the Spinal Cord Injury – Quality of Life (SCI-QOL) measurement system. J Spinal Cord Med. 2015;38(3):257–269. doi: 10.1179/2045772315Y.0000000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wood V, Wylie ML, Sheafor B. An analysis of a short self-report measure of life satisfaction: Correlation with rater judgments. J Gerontol. 1969;24:465–469. doi: 10.1093/geronj/24.4.465. [DOI] [PubMed] [Google Scholar]


