Abstract
Background
In Western populations, a higher level of fruit consumption has been associated with a lower risk of cardiovascular disease, but little is known about such associations in China, where the consumption level is low and rates of stroke are high.
Methods
Between 2004 and 2008, we recruited 512,891 adults, 30 to 79 years of age, from 10 diverse localities in China. During 3.2 million person-years of follow-up, 5173 deaths from cardiovascular disease, 2551 incident major coronary events (fatal or nonfatal), 14,579 ischemic strokes, and 3523 intracerebral hemorrhages were recorded among the 451,665 participants who did not have a history of cardiovascular disease or antihypertensive treatments at baseline. Cox regression yielded adjusted hazard ratios relating fresh fruit consumption to disease rates.
Results
Overall, 18.0% of participants reported consuming fresh fruit daily. As compared with participants who never or rarely consumed fresh fruit (the “nonconsumption” category), those who ate fresh fruit daily had lower systolic blood pressure (by 4.0 mm Hg) and blood glucose levels (by 0.5 mmol per liter [9.0 mg per deciliter]) (P<0.001 for trend for both comparisons). The adjusted hazard ratios for daily consumption versus nonconsumption were 0.60 (95% confidence interval [CI], 0.54 to 0.67) for cardiovascular death, and 0.66 (95% CI, 0.58 to 0.75), 0.75 (95% CI, 0.72 to 0.79), and 0.64 (95% CI, 0.56 to 0.74), respectively, for incident major coronary events, ischemic stroke, and hemorrhagic stroke. There was a strong loglinear dose–response relationship between the incidence of each outcome and the amount of fresh fruit consumed. These associations were similar across the 10 study regions and in subgroups of participants defined by baseline characteristics.
Conclusions
Among Chinese adults, a higher level of fruit consumption was associated with lower blood pressure and blood glucose levels and, largely independent of these and other dietary and nondietary factors, with significantly lower risks of major cardiovascular diseases. (Funded by the Wellcome Trust and others.)
Cardiovascular disease is a leading cause of premature death and disability worldwide and is responsible for more than 17 million deaths annually, with approximately 80% of the disease burden in low- and middle-income countries, such as China.1 A low level of fruit consumption is a major risk factor for cardiovascular disease, accounting for an estimated 104 million disability-adjusted lifeyears worldwide in 2010,2 including approximately 30 million in China.3 However, these estimates were based mainly on findings from Western studies, with little reliable evidence from China and other developing countries, where diet, lifestyle factors, and disease patterns differ substantially from those in Western populations.3–5 Moreover, most previous studies tended to involve a combination of fresh and processed fruit (frozen, dried, or canned fruit or fruit juice), with limited data specifically on fresh fruit, which is usually consumed raw as a snack in China. Furthermore, the associations of fruit intake with stroke subtypes, especially hemorrhagic stroke, are less well established than the association with ischemic heart disease,3,6,7 underscoring the importance of performing studies in China, where rates of stroke (particularly hemorrhagic stroke) are high. We examined the association of fresh fruit consumption with risks of major cardiovascular events in China, where fresh fruit consumption is low, although fresh vegetable consumption is high.8
Methods
Study Design and Oversight
The China Kadoorie Biobank Study is a nationwide, prospective cohort study involving 10 diverse localities (regions) in China, which is jointly coordinated by the University of Oxford and the Chinese Academy of Medical Sciences. The study design and methods have been reported previously. 9,10 Approval of the study was obtained from ethics committees or institutional review boards at the University of Oxford, the Chinese Center for Disease Control and Prevention (China CDC), the Chinese Academy of Medical Sciences, and all participating regions. The funders had no role in study design, data collection and analysis, preparation of the manuscript, or the decision to submit it for publication.
Baseline Survey
We selected 10 regional study sites (5 urban and 5 rural) in order to cover a wide range of risk exposures and disease patterns, taking into account the accuracy and completeness of death and disease registries for each region and the local capability to gather the necessary study data. Between June 2004 and July 2008, all nondisabled, permanent residents of each region who were 35 to 74 years of age were invited to participate in the study. Of the total of approximately 1.8 million eligible adults in these regions, almost 1 in 3 (33% in rural areas and 27% in urban areas) responded. Overall, 512,891 persons were recruited, including a few who were just outside the targeted age range, and all provided written informed consent.
At the local study clinics, trained health workers administered a laptop-based questionnaire on sociodemographic characteristics, smoking and alcohol consumption, diet, physical activity, and medical history; measured height, weight, waist circumference, and blood pressure; and performed spot random blood glucose testing using the SureStep Plus System (Johnson & Johnson). Blood pressure was measured at least twice with the use of an automated digital blood-pressure monitor (model UA-779, A&D Medical) after at least 5 minutes of rest in a seated position; the mean of two satisfactory measurements was used for analyses.11,12
Dietary data covered 12 major food groups: rice, wheat products, other staple foods, meat, poultry, fish, eggs, dairy products, fresh vegetables, preserved vegetables, fresh fruit, and soybean products. Respondents were asked about the frequency of habitual consumption during the previous 12 months and chose among five categories of frequency (daily, 4 to 6 days per week, 1 to 3 days per week, monthly, or never or rarely [the reference category]). In a subsample of 926 participants, the survey questionnaire was repeated within a year after the baseline assessment (mean interval, 5.4 months) in order to assess the reproducibility of the responses.
Resurveys
After completion of the baseline survey, we randomly selected 5 to 6% of the original participants for two resurveys, using procedures similar to those at baseline. The first resurvey took place from July through October 2008, with 19,788 participants resurveyed, and the second was conducted from August 2013 through September 2014, with just over 25,000 participants resurveyed. In addition to questions about the frequency of consumption, the second resurvey questionnaire asked about the amount consumed for each food group, which was used as a proxy measure to estimate the average consumption at baseline for each of the five frequency categories (see the Supplementary Appendix, available with the full text of this article at NEJM.org).
Follow-up and Outcome Measures
The vital status of each participant was determined periodically through the Disease Surveillance Points (DSP) system of the China CDC.13 The DSP vital-status data sets were checked annually against local residential records and health insurance records and were confirmed with street committees or village administrators. In addition, information about major diseases and episodes of hospitalization was collected through linkages with disease registries (for cancer, cardiovascular disease, and diabetes) and national health insurance claims databases. The Chinese National Health Insurance scheme provides electronic linkage to all hospitalization data.
Fatal and nonfatal events were documented according to the International Classification of Diseases, 10th Revision (ICD-10), by coders who were unaware of the baseline characteristics of the study participants.10 The four main outcome measures that were examined were cardiovascular death (ICD-10 codes I00 to I25, I27 to I88, and I95 to I99) and the incidence of major coronary events (fatal ischemic heart disease [codes I20 to I25] plus nonfatal myocardial infarction [code I21]), hemorrhagic stroke (code I61), and ischemic stroke (code I63). Other ischemic heart disease (i.e., ischemic heart disease not meeting the criteria for a major coronary event) and other cerebrovascular diseases (ICD-10 codes I60, I62, and I64 to I69) were analyzed separately. For analyses of incident disease, only the first cardiovascular event was counted.
Statistical Analysis
For the current study, we excluded persons who had a history of cardiovascular disease (23,132 persons) or antihypertensive treatment (48,174 persons) at baseline. Baseline characteristics of the remaining 451,665 participants were described as means and standard deviations or percentages in each category of fruit consumption, with adjustment for age, sex, and region as appropriate, by means of either multiple linear regression (for continuous outcomes) or logistic regression (for binary outcomes). The marginal mean values and 95% confidence intervals for body-mass index (BMI), waist circumference, blood pressure, and blood glucose according to frequency of fruit consumption were estimated separately for men and women with the use of multiple linear regression models adjusted for baseline covariates.
Cox regression was used to calculate hazard ratios and 95% confidence intervals for relative risks in relation to fruit consumption, with adjustment for baseline covariates and with stratification according to age at risk (in 5-year intervals), sex, and region. For analyses involving more than two exposure categories, the floatingabsolute- risk method was used, which provides the variance of the logarithm of the hazard ratio (i.e., to compute a confidence interval for the hazard ratio) for each category (including the reference category) to facilitate comparisons among the different exposure categories.14 Conventional (unfloated) analyses were also performed so that the results of the two methods could be compared. We calculated the hazard ratio for cardiovascular death with nondaily fruit consumption as compared with daily consumption in order to estimate the population-attributable fraction, using the formula Pe(HR − 1) ÷ [Pe(HR − 1) + 1],15 where Pe is the prevalence of nondaily consumption of fresh fruit in the Chinese population, and HR is the hazard ratio. Additional information about the statistical analyses is provided in the Supplementary Appendix.
Results
Patterns of Fresh Fruit Consumption
Among the 451,665 participants included in the study, the mean age was 50.5 years (range, 30 to 79); 58.8% of the participants were women, and 42.5% were from urban areas (Table 1). Overall, 18.0% of participants reported consumption of fresh fruit on a daily basis, 9.4% reported consumption 4 to 6 days per week, and 6.3% reported no or rare consumption (also referred to as nonconsumption). The proportion of participants with regular fruit consumption (i.e., 4 to 6 days per week or more) was inversely associated with age among rural participants and urban women (Fig. S1 and S2 in the Supplementary Appendix). Among urban men, however, the association was U-shaped, with men who were 50 to 55 years of age (preretirement age in China) reporting the lowest consumption. There was no south-tonorth gradient in fruit consumption, with two urban areas (Qingdao and Harbin) having the highest consumption and two rural areas (Henan and Hunan) having the lowest consumption (Fig. S3 in the Supplementary Appendix). The Spearman correlation coefficient of 0.55 between responses a few months apart indicated moderate reliability of the measure of fruit-consumption frequency (Table S2 in the Supplementary Appendix).
Table 1. Baseline Characteristics of the Study Participants According to the Frequency of Fresh Fruit Consumption.*.
| Characteristic | Consumption of Fresh Fruit |
|||||
|---|---|---|---|---|---|---|
| Never or Rarely (N = 28,479) | Monthly (N = 156,098) | 1–3 Days/Wk (N = 143,183) | 4–6 Days/Wk (N = 42,519) | Daily (N = 81,386) | All Participants (N = 451,665) | |
| Age (yr) | 53.6±10.4 | 51.7±10.9 | 49.8±10.4 | 48.8±10.4 | 48.9±11.6 | 50.5±10.4 |
| Female sex (%) | 47.1 | 55.5 | 56.5 | 62.1 | 71.7 | 58.8 |
| Urban residence (%) | 29.9 | 21.7 | 41.5 | 52.7 | 83.2 | 42.5 |
| Educational level (%) | ||||||
| No formal education | 28.7 | 22.6 | 17.5 | 13.9 | 9.1 | 18.1 |
| Primary school | 34.1 | 34.8 | 32.8 | 29.6 | 25.6 | 32.0 |
| Middle or high school | 35.3 | 38.1 | 46.0 | 50.5 | 52.5 | 44.2 |
| College or university | 1.9 | 4.5 | 3.7 | 6.0 | 12.8 | 5.7 |
| Household income (%)† | ||||||
| <10,000 yuan/yr | 45.3 | 36.7 | 27.7 | 18.5 | 15.4 | 28.8 |
| 10,000—19,999 yuan/yr | 26.4 | 28.8 | 31.3 | 30.6 | 25.5 | 29.0 |
| 20,000—34,999 yuan/yr | 17.6 | 24.1 | 24.4 | 25.9 | 27.3 | 24.5 |
| ≥35,000 yuan/yr | 10.7 | 10.4 | 16.6 | 25.0 | 31.8 | 17.7 |
| Regular smoking (%) | ||||||
| Never | 55.4 | 63.0 | 68.8 | 73.4 | 74.5 | 67.4 |
| Previous | 4.2 | 4.6 | 5.4 | 5.9 | 6.4 | 5.3 |
| Current | 40.4 | 32.4 | 25.8 | 20.7 | 19.1 | 27.3 |
| Regular alcohol intake (%) | ||||||
| Never | 76.5 | 81.7 | 83.9 | 85.9 | 85.5 | 83.2 |
| Previous | 1.7 | 1.3 | 1.4 | 1.5 | 1.6 | 1.4 |
| Current | 21.8 | 17.0 | 14.7 | 12.6 | 12.9 | 15.4 |
| Physical activity (MET-hr/day)‡ | 21.8±12.3 | 22.4±12.9 | 22.0±12.2 | 21.4±12.2 | 21.0±13.7 | 21.9±13.9 |
| Regular consumption of foods (%)§ | ||||||
| Fresh vegetables | 92.7 | 90.9 | 95.9 | 97.7 | 98.5 | 94.6 |
| Preserved vegetables | 27.3 | 21.6 | 21.6 | 24.0 | 23.3 | 22.5 |
| Meat | 38.8 | 39.1 | 47.3 | 58.5 | 59.6 | 47.2 |
| Dairy products | 6.8 | 5.5 | 8.6 | 15.5 | 24.7 | 11.0 |
Plus–minus values are means ±SD. Data were adjusted for age, sex, and region when appropriate.
At the exchange rate as of March 2016, 1 yuan is approximately equal to 0.15 U.S. dollars.
MET denotes metabolic equivalent.
Data shown are for daily consumption of fresh vegetables and for consumption on most days (at least 4 days per week) for other foods.
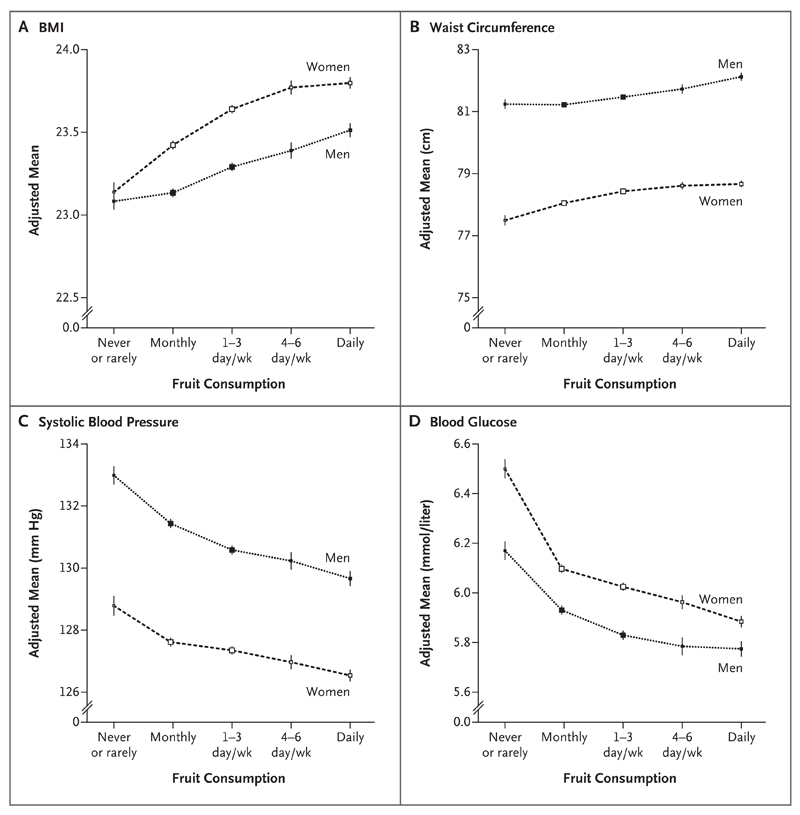
Participants who consumed fresh fruit more frequently (as compared with those who consumed it less frequently) were more likely to be women and to live in urban areas, were younger, had a higher level of education and higher household income, and were less likely to smoke or drink alcohol regularly and more likely to consume dairy products and meat, but they had similar levels of consumption of preserved and fresh vegetables (Table 1). Our participants had an overall mean BMI (the weight in kilograms divided by the square of the height in meters) of 23.5 and overall mean systolic blood pressure of 128.8 mm Hg. As compared with participants who never or rarely consumed fresh fruit, the BMI of daily consumers was 0.5 points higher, the waist circumference 0.9 cm larger, the blood pressure 4.0 mm Hg systolic lower and 1.4 mm Hg diastolic lower, and the blood glucose level 0.5 mmol per liter (9.0 mg per deciliter) lower (Fig. 1). These associations were largely unchanged after additional adjustment for potential confounders or mediators, except for systolic blood pressure, for which the association was attenuated by about one fifth (to 3.3 mm Hg in men and to 2.2 mm Hg in women).
Figure 1. Adjusted Mean Body-Mass Index (BMI), Waist Circumference, Blood Pressure, and Blood Glucose According to the Frequency of Fresh Fruit Consumption.
Mean values for BMI (Panel A) and waist circumference (Panel B) were adjusted for age (10 categories), area of China (10 regions), educational level (4 categories), annual household income (4 categories), smoking status (4 categories, with the category of “Never” subdivided into “Never” and “Occasional”), alcohol intake (4 categories, with the category of “Never” subdivided into “Never” and “Occasional”), physical activity (continuous variable), survey season (4 categories), and consumption of meat (3 categories), dairy products (3 categories), and preserved vegetables (5 categories). Mean values for systolic blood pressure (Panel C) and random blood glucose measurements (Panel D) were adjusted for the listed variables plus BMI and waist circumference. Blood glucose values were missing for 7503 study participants. To convert the values for glucose to milligrams per deciliter, divide by 0.05551. Vertical lines indicate 95% confidence intervals. P<0.001 for trend, for all comparisons.
Association of Fruit Consumption with Cardiovascular Outcomes
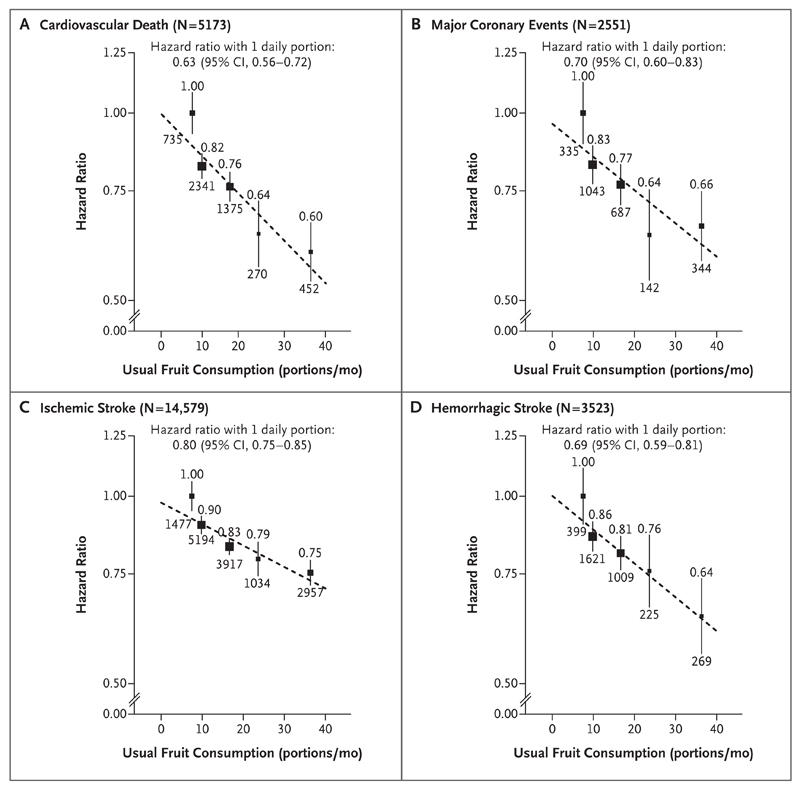
During 3.2 million person-years of follow-up, there were 5173 cardiovascular deaths, 2551 major coronary events (plus 16,563 other ischemic heart disease events), 14,579 ischemic strokes, and 3523 hemorrhagic strokes (plus 11,054 other cerebrovascular disease events) recorded. The risks of these major cardiovascular events were strongly and inversely associated with the level of fruit consumption (P<0.001 for trend, for all comparisons) (Fig. 2 and Table 2). As compared with nonconsumption, the adjusted hazard ratios for daily consumption were 0.60 (95% confidence interval [CI], 0.54 to 0.67) for cardiovascular death, 0.66 (95% CI, 0.58 to 0.75) for major coronary events, 0.75 (95% CI, 0.72 to 0.79) for ischemic stroke, and 0.64 (95% CI, 0.56 to 0.74) for hemorrhagic stroke. After correction for regression dilution bias, the associations were approximately log-linear; the hazard ratios for one daily portion of fruit were 0.63 (95% CI, 0.56 to 0.72), 0.70 (95% CI, 0.60 to 0.83), 0.80 (95% CI, 0.75 to 0.85), and 0.69 (95% CI, 0.59 to 0.81), respectively. The level of fruit consumption was also significantly and inversely associated with risks of other ischemic heart disease and other cerebrovascular diseases, although the associations were less strong (Table 2, and Fig. S4 in the Supplementary Appendix).
Figure 2. Adjusted Hazard Ratios for Major Cardiovascular Events According to the Level of Fresh Fruit Consumption.
Analyses were adjusted for educational level, income, alcohol intake, smoking status, physical activity, survey season, and consumption of dairy products, meat, and preserved vegetables and were stratified according to age at risk, sex, and region. The black boxes represent hazard ratios, with the size inversely proportional to the variance of the logarithm of the hazard ratio, and the vertical lines represent 95% confidence intervals. The numbers above the vertical lines are point estimates for hazard ratios, and the numbers below the lines are numbers of events.
Table 2. Incidence Rates and Adjusted Hazard Ratios for Major Cardiovascular Events According to Fresh Fruit Consumption.*.
| Event | Consumption of Fresh Fruit |
||||
|---|---|---|---|---|---|
| Never or Rarely | Monthly | 1–3 Days/Wk | 4–6 Days/Wk | Daily | |
| Death from cardiovascular causes | |||||
| No. of events | 735 | 2341 | 1375 | 270 | 452 |
| Incidence rate (no./1000 person-yr) | 3.68 | 2.10 | 1.34 | 0.88 | 0.78 |
| Hazard ratio | 1.00 | 0.82 | 0.76 | 0.64 | 0.60 |
| 95% CI, with floating absolute risk | 0.93–1.08 | 0.78–0.86 | 0.72–0.80 | 0.57–0.72 | 0.54–0.67 |
| 95% CI, without floating absolute risk | — | 0.75–0.90 | 0.69–0.84 | 0.55–0.74 | 0.52–0.69 |
| Major coronary events | |||||
| No. of events | 335 | 1043 | 687 | 142 | 344 |
| Incidence rate (no./1000 person–yr) | 1.68 | 0.94 | 0.67 | 0.46 | 0.59 |
| Hazard ratio | 1.00 | 0.83 | 0.77 | 0.64 | 0.66 |
| 95% CI, with floating absolute risk | 0.89–1.12 | 0.77–0.89 | 0.71–0.83 | 0.54–0.75 | 0.58–0.75 |
| 95% CI, without floating absolute risk | — | 0.73–0.94 | 0.67–0.88 | 0.52–0.78 | 0.55–0.78 |
| Ischemic stroke | |||||
| No. of events | 1477 | 5194 | 3917 | 1034 | 2957 |
| Incidence rate (no./1000 person–yr) | 7.58 | 4.75 | 3.88 | 3.42 | 5.17 |
| Hazard ratio | 1.00 | 0.90 | 0.83 | 0.79 | 0.75 |
| 95% CI, with floating absolute risk | 0.95–1.06 | 0.87–0.93 | 0.81–0.86 | 0.74–0.84 | 0.72–0.79 |
| 95% CI, without floating absolute risk | — | 0.85–0.95 | 0.79–0.88 | 0.73–0.86 | 0.70–0.81 |
| Hemorrhagic stroke | |||||
| No. of events | 399 | 1621 | 1009 | 225 | 269 |
| Incidence rate (no./1000 person-yr) | 2.05 | 1.48 | 1.00 | 0.74 | 0.47 |
| Hazard ratio | 1.00 | 0.86 | 0.81 | 0.76 | 0.64 |
| 95% CI, with floating absolute risk | 0.90–1.11 | 0.82–0.91 | 0.76–0.86 | 0.66–0.87 | 0.56–0.74 |
| 95% CI, without floating absolute risk | — | 0.77–0.97 | 0.72–0.92 | 0.64–0.90 | 0.54–0.76 |
| Other ischemic heart disease | |||||
| No. of events | 1190 | 5694 | 4573 | 1421 | 3685 |
| Incidence rate (no./1000 person-yr) | 6.07 | 5.21 | 4.53 | 4.71 | 6.47 |
| Hazard ratio | 1.00 | 0.96 | 0.90 | 0.92 | 0.88 |
| 95% CI, with floating absolute risk | 0.94–1.06 | 0.93–0.99 | 0.88–0.93 | 0.88–0.97 | 0.85–0.92 |
| 95% CI, without floating absolute risk | — | 0.90–1.02 | 0.85–0.97 | 0.85–1.00 | 0.82–0.95 |
| Other cerebrovascular disease | |||||
| No. of events | 717 | 4013 | 3309 | 894 | 2121 |
| Incidence rate (no./1000 person-yr) | 3.70 | 3.70 | 3.30 | 2.97 | 3.73 |
| Hazard ratio | 1.00 | 1.02 | 0.96 | 0.82 | 0.88 |
| 95% CI, with floating absolute risk | 0.93–1.08 | 0.98–1.06 | 0.93–0.99 | 0.86–0.98 | 0.84–0.93 |
| 95% CI, without floating absolute risk | — | 0.94–1.11 | 0.88–1.05 | 0.83–1.02 | 0.80–0.97 |
Hazard ratios were adjusted for educational level, income, alcohol consumption, smoking status, physical activity, survey season, and consumption of dairy products, meat, and preserved vegetables and were stratified according to age at risk, sex, and region. The floating-absolute-risk method provides the variance of the logarithm of the hazard ratio for each category (including the reference category) to facilitate comparisons among the different exposure categories.14
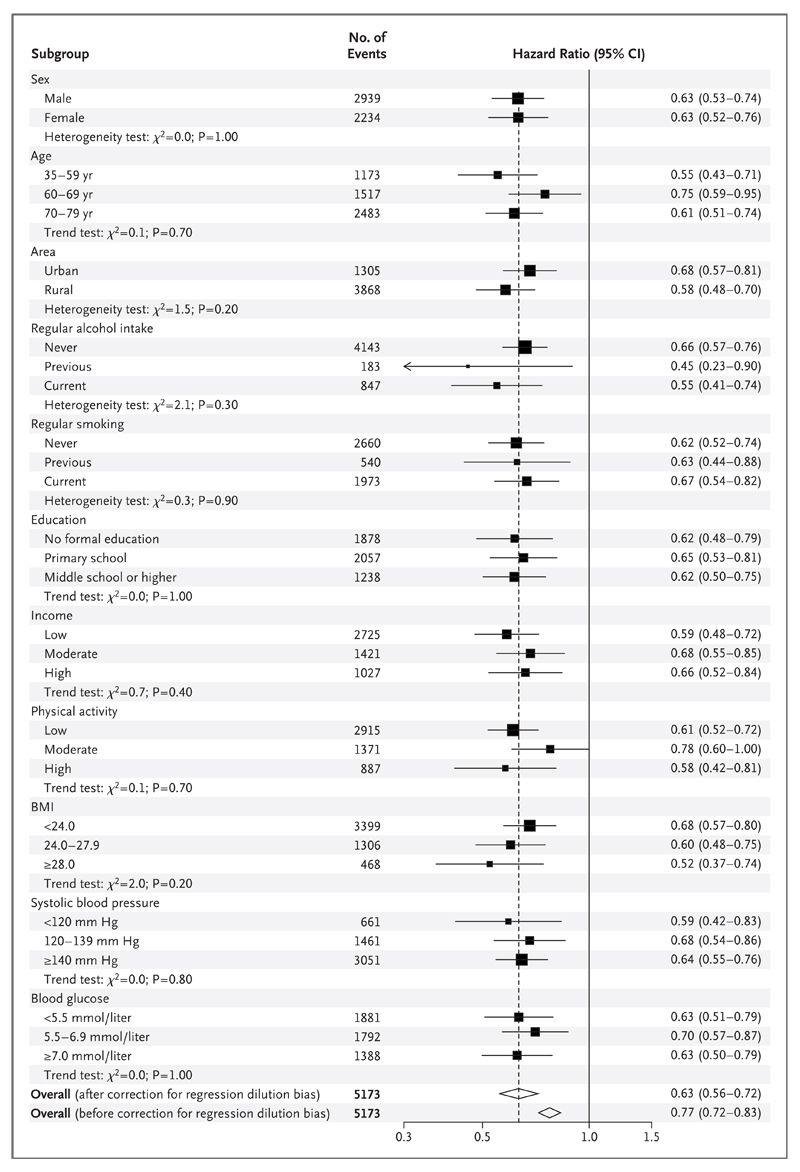
With the exception of ischemic stroke and other cerebrovascular diseases, the associations between the level of fruit consumption and the risk of major cardiovascular events did not appear to be modified by baseline characteristics such as sex, age, region, or season of enrollment (Fig. 3, and Fig. S5 through S8 in the Supplementary Appendix). For ischemic stroke, the association appeared to be somewhat greater among men, participants from urban areas, those who drank alcohol regularly, those with higher educational levels, and those with higher blood glucose levels (Fig. S5 in the Supplementary Appendix). None of the associations or interactions were materially attenuated by additional adjustment for BMI, waist circumference, systolic blood pressure, and blood glucose level (Fig. S9 in the Supplementary Appendix).
Figure 3. Adjusted Hazard Ratios for Cardiovascular Death with One Daily Portion of Fresh Fruit, According to Baseline Characteristics.
Analyses were adjusted for educational level, income, alcohol intake, smoking status, physical activity, survey season, and consumption of dairy products, meat, and preserved vegetables and were stratified according to age at risk, sex, and region, as appropriate. The black boxes represent hazard ratios, with the size inversely proportional to the variance of the logarithm of the hazard ratio, and the horizontal lines represent 95% confidence intervals. The open diamonds represent the overall hazard ratios and 95% confidence intervals. Chi-square tests (χ2) were performed to examine either trend (with 1 df) or heterogeneity (with n –1 df, where n represents the number of categories). To convert the values for glucose to milligrams per deciliter, divide by 0.05551.
In our study, approximately 95% of participants reported daily consumption of fresh vegetables. Additional adjustment for consumption of fresh vegetables and other dietary variables did not alter the risk estimates for fresh fruit consumption (Table S3 in the Supplementary Appendix). Likewise, the exclusion of the first 2 years of follow-up in order to further reduce the effect of reverse causality did not materially change the observed associations (data not shown).
Population-Attributable Fraction of Low Fruit Consumption
The hazard ratio for cardiovascular death with nondaily versus daily fruit consumption was 1.30 (95% CI, 1.17 to 1.46). In our second resurvey, about 65% of the participants reported nondaily fruit consumption (Table S4 in the Supplementary Appendix), which was in line with the proportion in the most recent China Health and Nutrition Survey, conducted in 2011.16 We performed an exploratory analysis to estimate the effect of fruit consumption on cardiovascular death under the assumption that there is a causal association. On the basis of this assumption, our data suggest that 16% (95% CI, 10 to 23) of deaths from cardiovascular causes could be attributed to low fruit consumption. Applying this proportion to national data on cardiovascular mortality17 suggests that about 560,000 (95% CI, 350,000 to 800,000) deaths from cardiovascular causes each year, including about 200,000 before 70 years of age, could be prevented if daily consumption of fresh fruit were universal in China. However, it is difficult to establish causality reliably in observational studies of dietary factors that have such moderate relative risks and potential for confounding.
Discussion
In our study involving more than 450,000 men and women in China without prior cardiovascular disease or antihypertensive treatment, higher fresh fruit consumption was associated with significantly lower levels of blood pressure and blood glucose. Largely independent of blood pressure, blood glucose levels, and other dietary and nondietary factors, higher fruit consumption was also associated with significantly lower risks of cardiovascular disease, including cardiovascular death, major coronary events, hemorrhagic stroke, and ischemic stroke. These associations were consistent across 10 regions and in various subgroups of participants defined by various baseline characteristics. If these associations are largely causal, the potential health gain from increased consumption of fresh fruit in China would be substantial.
Several large prospective studies of mostly Western populations have assessed the association of fruit consumption with cardiovascular disease.18–25 Most of them showed an inverse association, but the magnitude of the benefit varied considerably, and the association was typically weaker than that observed in the current study. For example, in a recent meta-analysis of six studies involving nearly 680,000 participants and 10,000 cardiovascular deaths, each additional serving (80 g) of fruit per day was associated with a 5% (95% CI, 0 to 9) lower risk of cardiovascular death, which is not good evidence of a real protective effect.19 Only one previous prospective study in China has shown an association between fresh fruit consumption and cardiovascular risk. In that study, involving approximately 130,000 adults from Shanghai and approximately 1600 cardiovascular deaths during follow-up, the risk of cardiovascular death among people in the highest quintile of fruit consumption was about 30% lower than among those in the lowest quintile,26 but no overall association with the incidence of major coronary events was observed, perhaps in part because of the small number of such events (365).27 Information on the association between fruit consumption and stroke subtypes is limited, 18 especially for hemorrhagic stroke, which is relatively uncommon in Western populations. In our study, which involved more than 3500 hemorrhagic strokes, we found that higher consumption of fresh fruit was associated with a significantly lower risk of hemorrhagic stroke, largely independent of blood pressure.
The association between the level of fruit consumption and cardiovascular risk in our study (a 40% lower risk of cardiovascular death and a 34% lower risk of major coronary events among participants who consumed fresh fruit daily as compared with those who never or rarely consumed fresh fruit) was much stronger than the associations observed in previous studies. Several factors may account for this difference. First, unlike many previous studies, our study focused on fresh fruit, which is universally consumed raw in China, perhaps maximizing its potential benefits.23,28 Moreover, the average level of fruit consumption in the Chinese population is very low,8 and there is evidence that the association of fruit consumption with disease risks may be particularly strong at the low end of the range of intake (i.e., fewer than two servings per day).19 In addition, our analyses excluded not only persons with a history of cardiovascular disease but also those receiving antihypertensive treatment, thereby reducing confounding by medication use. Our analysis also takes into account regression dilution bias,29,30 whereas previously, few large, prospective studies have dealt with this important issue.20
Our study has several limitations. First, we did not collect information on processed fruit because its consumption is extremely low in China. Second, we were unable to properly examine the association of fresh vegetables with cardiovascular risk because daily consumption is almost universal in our study population. Third, fruit consumption at baseline was assessed with the use of a simple qualitative food-frequency questionnaire, and information on mean consumption amounts was estimated indirectly on the basis of data from resurveys (under the assumption that there were no large changes between the baseline survey and the second resurvey). Fourth, we did not collect information about types of fruit consumed, which is likely to vary greatly according to season and region (although the most commonly consumed fruits in China are apples, citrus fruit, and pears). Fifth, our study was not exactly nationally representative, and the questionnaire used has not been validated against another dietary measure. Finally, and perhaps most important, fruit consumption in our study was closely correlated with socioeconomic status, which in turn has been closely associated with health status and the risk of cardiovascular disease.31 Although we adjusted carefully for several variables related to socioeconomic status (i.e., region, educational level, and income) and analyses stratified according to these variables showed consistent findings, residual confounding by socioeconomic status is still possible.
Our study does not permit reliable inference of causality, but the observed inverse association between fruit consumption and cardiovascular risk could be causal,32,33 given that fruit is a rich source of potassium, dietary fiber, folate, antioxidants, and various bioactive phytochemicals, each of which has potential cardioprotective effects,34 and contains little sodium and fat and few calories. The association may be mediated through conventional cardiovascular risk factors such as hypertension, diabetes, and overweight.35 However, in our relatively lean study population (mean BMI, 23.5), fruit intake was associated with higher, instead of lower, adiposity, perhaps through improved nutrition, since a stronger positive association was observed among those with a lower BMI, and adjustment for blood pressure and blood glucose levels attenuated the association only slightly, suggesting the involvement of other mechanisms.36
In conclusion, our evaluation of the relationship between fresh fruit consumption and cardiovascular disease in China showed that the level of fruit consumption was inversely associated with blood pressure and blood glucose levels. Largely independent of blood pressure, blood glucose levels, and other dietary and nondietary factors, higher fruit consumption was associated with a significantly lower risk of major cardiovascular events.
Supplementary Material
Acknowledgments
Supported by grants from the Wellcome Trust, the Kadoorie Charitable Foundation, and the Chinese National Natural Science Foundation (81390541), with core funding provided by the British Heart Foundation, the Medical Research Council, and Cancer Research UK to the Clinical Trial Service Unit and Epidemiological Studies Unit, University of Oxford.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
We thank the study participants and project staff, the Chinese Center for Disease Control and Prevention (China CDC) and its regional offices for access to death and disease registries, Prof. Yuna He from the National Institute for Nutrition and Food Safety, China CDC, for sharing unpublished information about current levels of fruit intake in China, and the Chinese National Health Insurance Scheme for providing data.
References
- 1.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 2.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang G, Wang Y, Zeng Y, et al. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381:1987–2015. doi: 10.1016/S0140-6736(13)61097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370:1929–38. doi: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 5.Oude Griep LM, Verschuren WM, Kromhout D, Ocké MC, Geleijnse JM. Raw and processed fruit and vegetable consumption and 10-year stroke incidence in a population-based cohort study in the Netherlands. Eur J Clin Nutr. 2011;65:791–9. doi: 10.1038/ejcn.2011.36. [DOI] [PubMed] [Google Scholar]
- 6.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu Z, Yao C, Zhao D, et al. Sino- MONICA project: a collaborative study on trends and determinants in cardiovascular diseases in China. I. morbidity and mortality monitoring. Circulation. 2001;103:462–8. doi: 10.1161/01.cir.103.3.462. [DOI] [PubMed] [Google Scholar]
- 8.Micha R, Khatibzadeh S, Shi P, Andrews KG, Engell RE, Mozaffarian D. Global, regional and national consumption of major food groups in 1990 and 2010: a systematic analysis including 266 country-specific nutrition surveys worldwide. BMJ Open. 2015;5(9):e008705. doi: 10.1136/bmjopen-2015-008705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen Z, Lee L, Chen J, et al. Cohort profile: the Kadoorie Study of Chronic Disease in China (KSCDC) Int J Epidemiol. 2005;34:1243–9. doi: 10.1093/ije/dyi174. [DOI] [PubMed] [Google Scholar]
- 10.Chen Z, Chen J, Collins R, et al. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol. 2011;40:1652–66. doi: 10.1093/ije/dyr120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lewington S, Li L, Sherliker P, et al. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie Biobank. J Hypertens. 2012;30:1383–91. doi: 10.1097/HJH.0b013e32835465b5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Su D, Du H, Zhang X, et al. Season and outdoor temperature in relation to detection and control of hypertension in a large rural Chinese population. Int J Epidemiol. 2014;43:1835–1845. doi: 10.1093/ije/dyu158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang GH, Stroup DF, Thacker SB. National public health surveillance in China: implications for public health in China and the United States. Biomed Environ Sci. 1997;10:1–13. [PubMed] [Google Scholar]
- 14.Plummer M. Improved estimates of floating absolute risk. Stat Med. 2004;23:93–104. doi: 10.1002/sim.1485. [DOI] [PubMed] [Google Scholar]
- 15.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88:15–9. doi: 10.2105/ajph.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xiao Y, Su C, Ouyang Y, Zhang B. Trends of vegetables and fruits consumption among Chinese adults aged 18 to 44 years old from 1991 to 2011. Zhonghua Liu Xing Bing Xue Za Zhi. 2015;36:232–6. [PubMed] [Google Scholar]
- 17.Hu S, Gao R, Liu L, et al. National Center for Cardiovascular Diseases report on cardiovascular diseases in China in 2014. Beijing: Encyclopaedia of China Publishing House. 2015 ( http://www.nccd.org.cn/en/Down/19204/) [Google Scholar]
- 18.Hu D, Huang J, Wang Y, Zhang D, Qu Y. Fruits and vegetables consumption and risk of stroke: a meta-analysis of prospective cohort studies. Stroke. 2014;45:1613–9. doi: 10.1161/STROKEAHA.114.004836. [DOI] [PubMed] [Google Scholar]
- 19.Wang X, Ouyang Y, Liu J, et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ. 2014;349:g4490. doi: 10.1136/bmj.g4490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhupathiraju SN, Wedick NM, Pan A, et al. Quantity and variety in fruit and vegetable intake and risk of coronary heart disease. Am J Clin Nutr. 2013;98:1514–23. doi: 10.3945/ajcn.113.066381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Crowe FL, Roddam AW, Key TJ, et al. Fruit and vegetable intake and mortality from ischaemic heart disease: results from the European Prospective Investigation into Cancer and Nutrition (EPIC)- Heart study. Eur Heart J. 2011;32:1235–43. doi: 10.1093/eurheartj/ehq465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr. 2006;136:2588–93. doi: 10.1093/jn/136.10.2588. [DOI] [PubMed] [Google Scholar]
- 23.Oyebode O, Gordon-Dseagu V, Walker A, Mindell JS. Fruit and vegetable consumption and all-cause, cancer and CVD mortality: analysis of Health Survey for England data. J Epidemiol Community Health. 2014;68:856–62. doi: 10.1136/jech-2013-203500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.He FJ, Nowson CA, Lucas M, Mac-Gregor GA. Increased consumption of fruit and vegetables is related to a reduced risk of coronary heart disease: meta-analysis of cohort studies. J Hum Hypertens. 2007;21:717–28. doi: 10.1038/sj.jhh.1002212. [DOI] [PubMed] [Google Scholar]
- 25.Larsson SC, Virtamo J, Wolk A. Total and specific fruit and vegetable consumption and risk of stroke: a prospective study. Atherosclerosis. 2013;227:147–52. doi: 10.1016/j.atherosclerosis.2012.12.022. [DOI] [PubMed] [Google Scholar]
- 26.Zhang X, Shu XO, Xiang YB, et al. Cruciferous vegetable consumption is associated with a reduced risk of total and cardiovascular disease mortality. Am J Clin Nutr. 2011;94:240–6. doi: 10.3945/ajcn.110.009340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yu D, Zhang X, Gao YT, et al. Fruit and vegetable intake and risk of CHD: results from prospective cohort studies of Chinese adults in Shanghai. Br J Nutr. 2014;111:353–62. doi: 10.1017/S0007114513002328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington, DC: American Institute for Cancer Research; 2007. World Cancer Research Fund. [Google Scholar]
- 29.Clarke R, Shipley M, Lewington S, et al. Underestimation of risk associations due to regression dilution in longterm follow-up of prospective studies. Am J Epidemiol. 1999;150:341–53. doi: 10.1093/oxfordjournals.aje.a010013. [DOI] [PubMed] [Google Scholar]
- 30.Lewington S, Thomsen T, Davidsen M, Sherliker P, Clarke R. Regression dilution bias in blood total and high-density lipoprotein cholesterol and blood pressure in the Glostrup and Framingham prospective studies. J Cardiovasc Risk. 2003;10:143–8. doi: 10.1097/01.hjr.0000060834.46105.3c. [DOI] [PubMed] [Google Scholar]
- 31.Rosengren A, Subramanian SV, Islam S, et al. Education and risk for acute myocardial infarction in 52 high, middle and low-income countries: INTERHEART casecontrol study. Heart. 2009;95:2014–22. doi: 10.1136/hrt.2009.182436. [DOI] [PubMed] [Google Scholar]
- 32.Rautiainen S, Levitan EB, Mittleman MA, Wolk A. Fruit and vegetable intake and rate of heart failure: a populationbased prospective cohort of women. Eur J Heart Fail. 2015;17:20–6. doi: 10.1002/ejhf.191. [DOI] [PubMed] [Google Scholar]
- 33.Hartley L, Igbinedion E, Holmes J, et al. Increased consumption of fruit and vegetables for the primary prevention of cardiovascular diseases. Cochrane Database Syst Rev. 2013;6:CD009874. doi: 10.1002/14651858.CD009874.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu RH. Health benefits of fruit and vegetables are from additive and synergistic combinations of phytochemicals. Am J Clin Nutr. 2003;78(Suppl):517S–20S. doi: 10.1093/ajcn/78.3.517S. [DOI] [PubMed] [Google Scholar]
- 35.Bazzano LA, Serdula MK, Liu S. Dietary intake of fruits and vegetables and risk of cardiovascular disease. Curr Atheroscler Rep. 2003;5:492–9. doi: 10.1007/s11883-003-0040-z. [DOI] [PubMed] [Google Scholar]
- 36.Tuohy KM, Conterno L, Gasperotti M, Viola R. Up-regulating the human intestinal microbiome using whole plant foods, polyphenols, and/or fiber. J Agric Food Chem. 2012;60:8776–82. doi: 10.1021/jf2053959. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.