Abstract
Background
Liver resections have classically been distinguished as “minor” or “major” based on the number of segments removed. However, it is clear that the number of segments alone does not convey the complexity of a resection. To date, no study has been conducted that formally assesses the complexity of various anatomic liver resections.
Study Design
A four-question survey was administered to 135 expert liver surgeons in 14 countries. The first three questions related to the country in which the surgeon was practicing and the surgeon's experience. In the fourth question, the experts were asked to rate the difficulty of various open, anatomic liver resections on a scale of 1-10.
Results
66 of 135 (48.9%) surgeons responded to the survey. Twelve procedures were rated. The lowest mean score of 1.37—indicating least difficulty—was given to peripheral wedge resection. Left trisectionectomy with caudate resection was deemed most difficult with a score of 8.28. The mean scores for the two procedures perceived as least difficult—peripheral wedge resection and left lateral sectionectomy—were lower than the mean scores of all the rest of the procedures at a highly statistically significant level (p < 0.0001). The four procedures with the highest scores shared the common attribute that they involved the right intersectional plane.
Conclusions
These data represent the first quantitative assessment of the perceived difficulty of a variety of liver resections. The complexity scores generated allow for separation of liver resections into three categories of complexity (Low Complexity, Medium Complexity, and High Complexity) on a quantitative basis.
Introduction
Since the first description of anatomic right hepatectomy in 1952 (1), hepatic resection has advanced significantly in both safety and complexity. As a result, resection has become the treatment of choice for many patients with benign and malignant liver lesions. Multiple factors account for the advance of liver surgery. One important factor is better appreciation of the anatomy of the liver as delineated initially by Couinaud (2) and Goldsmith and Woodbourne (3) among others. Bismuth's landmark analysis in the 1980s summarized the anatomical details underlying these operations and the steps to carrying them out (4, 5). With this understanding, segment-oriented approaches to liver resection have become standard with documented benefit (6-8).
As illustrated by Couinaud's initial segmental description, each of the eight segments has individual biliary drainage, vascular inflow, and vascular outflow. Each can therefore be resected independently without compromising other segments. This allows for a variety of anatomic liver resections, some of which are more complex and challenging than others. Classically, liver resections have been grouped as “minor” and “major” based on the number of Couinaud segments resected (9, 10). In this classification, a minor resection is one in which two or fewer segments are resected, and a major resection is one in which three or more segments are removed. The classical grouping into minor and major has been in use for more than 50 years. However, as liver resections have increased in variety and complexity, it has become apparent that a classification based simply on the number of segments is inadequate. For instance, left lateral sectionectomy (Segments 2 and 3) and right anterior sectionectomy (Segments 5 and 8) are both two-segment resections but are clearly not in the same category of complexity. One basis for an updated classification would be the perceptions of expert surgeons on the complexity of various resections.
To date, no study has been conducted that formally assesses the complexity of various anatomic liver resections. In this study, a questionnaire regarding the difficulty of a variety of open, anatomic liver resections was administered to experienced hepatic surgeons across the world. The results yielded a complexity score for each procedure that allowed ranking of liver resections by perceived difficulty and facilitated the generation of a new three-tier classification for these resections.
Methods
Design
A four-question survey was administered by email to 135 expert liver surgeons in 14 countries from March 2014 through April 2014. The surgical experts were identified primarily by their contributions to the literature. All surveys were anonymous. The survey was created using a widely available internet tool (http://www.surveymonkey.com). See the supplemental material for the survey questions.
The first three questions related to the country in which the surgeon was practicing and the surgeon's experience. In the fourth question, the experts were asked to rate the difficulty of various liver resections on a scale of 1-10. Level 1 was labeled as “easier,” and level 10 was labeled as “more difficult.” The survey specified that all resections were to be considered open rather than laparoscopic procedures, and all resections besides a peripheral wedge resection were considered anatomic in nature.
The expert surgeons were randomly divided into two groups prior to sending out the survey. The groups received surveys that differed slightly in order to evaluate the perceived increase in difficulty when formal caudate resection is added to a procedure. The survey administered to group 1 included the operations “left hepatectomy with caudate resection” and “left trisectionectomy without caudate resection,” while the survey administered to group 2 included the operations ”left hepatectomy without caudate resection” and “left trisectionectomy with caudate resection.” The other eight resections presented in the questionnaire were common to both groups.
Data Analysis
For each procedure, the score of perceived difficulty was summarized using mean and standard error. As stated, all recipients were asked to assess the difficulty of eight procedures, but the other two procedures differed between the two groups. Results for the eight procedures that were common to the two groups were compared using Mann-Whitney rank-sum test. When analyzing the results it was found that Group 1 responders consistently rated the eight in common procedures as less difficult than Group 2 responders. To make the scores among all 12 procedures comparable, a regression analysis was performed using generalized estimating equation (GEE) to adjust surgeons’ characteristics including country (US vs. non-US) and the number of resections performed (annually and career). GEE also allowed us to account for the correlation among scores from the same surgeon and provided an efficient way to handle repeated measurement data without requiring multivariate normal distribution (11). The differences among individual procedures were further compared and the resultant p-values were corrected for multiple comparisons using False discovery rate (FDR) adjustment (12). All tests were two-sided and an adjusted p-value of 0.05 or less was taken to indicate statistical significance. The statistical analysis was performed using SAS 9.2 (SAS Institutes, Cary, NC).
Results
Participants and their experience
66 of 135 (48.9%) surgeons responded to the survey—33 surgeons from Group 1 and 33 surgeons from Group 2. 34 of 66 (54.5%) responders practice within the United States, and 39 practice in North America (59.0%). 12 (18%) surgeons practice in Europe, and 12 practice in Asia. 44 of 66 (66.7%) respondents worked in a country in which English is a national language. 51/81 (63.0%) experts from countries in which English is a national language responded to the survey as compared to 13/54 (24.1%) experts from countries in which it is not. This difference was highly significant by Chi squared test (P < 0.0002). The countries in which 2 of the responding surgeons practice were uncertain. Characteristics of the responding surgeons are summarized in Table 1.
Table 1.
Characteristics of Responding Surgeons
| Characteristic | No. of respondents |
|---|---|
| Country/continent | |
| USA | 34 |
| Canada | 5 |
| Europe | 12 |
| Asia | 12 |
| South America | 1 |
| Group 1 | |
| No. of resections performed in career | |
| 0-250 | 5 |
| 250-500 | 6 |
| 500-1000 | 13 |
| >1000 | 9 |
| No. of resections performed per year | |
| 0-25 | 4 |
| 25-50 | 9 |
| 50-75 | 4 |
| 75-100 | 7 |
| >100 | 9 |
| Group 2 | |
| No. of resections performed in career | |
| 0-250 | 9 |
| 250-500 | 10 |
| 500-1000 | 5 |
| >1000 | 9 |
| No. of resections performed per year | |
| 0-25 | 7 |
| 25-50 | 10 |
| 50-75 | 4 |
| 75-100 | 4 |
| >100 | 8 |
Respondents encompassed all levels of experience. 30/66 surgeons (45.5%) have performed fewer than 500 resections in their career, while 36/66 (54.5%) have performed more. Notably, responders from Group 1 tended to be more experienced than those from Group 2— while 22/33 (66.7%) surgeons from Group 1 had performed greater than 500 liver resections in their career, only 14/33 (42.4%) from Group 2 had done so. This trend approached but did not meet statistical significance (P = 0.140). However, the current annual surgical volume was similar between the two groups (P = 0.781). Group 1 responders consistently rated the same operation as less difficult than Group 2 responders (data not shown). For instance, the unadjusted mean difficulty for a right hepatectomy among Group 1 responders was 4.58 (on a scale of 1-10), while that for Group 2 responders was 5.18. This was true for every operation that the two groups both rated except the peripheral wedge resection (mean 1.30 for both groups).
Scores and Ranks of the 12 Procedures
Table 2 and Figure 1 summarize the adjusted scores for each resection included in the survey. In all, 12 procedures were rated. 8 procedures were rated by all respondents, while 4 were rated by either group 1 or group 2 (33 respondents). We found when analyzing the results that Group 1 responders consistently rated the eight in-common procedures as less difficult than Group 2 responders. To make the scores among all 12 procedures comparable, a regression analysis was performed to adjust for surgeons’ characteristics including experience as outlined in the Methods section.
Table 2.
Complexity Scores for Liver Resections.
| Procedure | n | Mean score (SE) | Confidence interval |
|---|---|---|---|
| Peripheral wedge resection (< 3 cm) | 66 | 1.365 (0.177) | 1.018-1.712 |
| Left lateral sectionectomy | 66 | 2.011 (0.165) | 1.687-2.335 |
| Left hepatectomy without caudate resection | 33 | 4.240 (0.250) | 3.751-4.729 |
| Right hepatectomy | 66 | 4.919 (0.171) | 4.584-5.254 |
| Right posterior sectionectomy | 66 | 5.488 (0.231) | 5.037-5.940 |
| Left hepatectomy with caudate resection | 33 | 5.525 (0.254) | 5.028-6.023 |
| Isolated caudate resection | 66 | 5.904 (0.240) | 5.433-6.374 |
| Right trisectionectomy | 66 | 6.242 (0.201) | 5.849-6.635 |
| Right anterior sectionectomy | 65 | 6.680 (0.222) | 6.245-7.114 |
| Anatomic middle hepatectomy | 65 | 7.217 (0.216) | 6.794-7.640 |
| Left trisectionectomy without caudate resection | 32 | 7.581 (0.315) | 6.964-8.197 |
| Left trisectionectomy with caudate resection | 32 | 8.283 (0.224) | 7.843-8.723 |
SE, standard error.
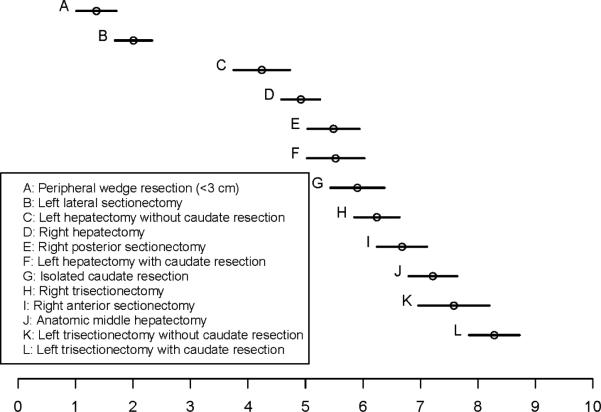
Figure 1.
The mean complexity score and 95% confidence interval for each resection included in the survey.
The lowest mean score of 1.37—indicating least difficulty—was given to peripheral wedge resection. The highest mean score of 8.28 was given to left trisectionectomy with caudate resection. The mean scores for the two procedures perceived as least difficult—peripheral wedge resection and left lateral sectionectomy—were lower than the mean scores of all the rest of the procedures at a highly statistically significant level (P < 0.0001 for each of these procedures versus all of the other procedures). Thus, peripheral wedge resection and left lateral sectionectomy make up a group that is easily distinguished from the other ten procedures.
The relationship of the ten more difficult procedures to each other is best understood from Figure 1 which shows the mean scores and 95% confidence limits. Left hepatectomy without caudate resection had the lowest score in this group of ten procedures (4.24). This score was not significantly different from the next highest score of 4.92 given to right hepatectomy (P = 0.013). In fact, none of the scores in this upper group of 10 resections was significantly different from the procedure immediately above or below it. However, all of the procedures statistically differed from other procedures two or more ranks away. For instance, though the score for left hepatectomy without caudate was not significantly different from right hepatectomy, its mean score significantly differed from the other eight procedures ranked above right hepatectomy. At the other end of the spectrum, left trisectionectomy with caudate significantly differed from every resection except left trisectionectomy without caudate—the procedure ranked immediately below it (P = 0.086).
The addition of caudate resection consistently resulted in a higher score. The difference was significant when left hepatectomy was compared to left hepatectomy with caudate resection (P = 0.001). The score was also higher when left trisectionectomy was compared to left trisectionectomy with caudate resection, but this difference was not significant (P = 0.086). Isolated caudate resection was ranked as the sixth most difficult procedure with a mean score of 5.90. This was significantly different from the mean scores of all four procedures with the lowest ranks. These included right and left hepatectomy, in which four and three segments are removed as compared to the one segment removed in isolated caudate resection. In fact, the relationship between the number of segments resected and the perceived difficulty of the procedure was rather weak. Perhaps the best example is left lateral sectionectomy versus right anterior sectionectomy. While both are two-segment resections, the former was ranked as the second easiest procedure while the latter was deemed the fourth most difficult. In fact, right anterior sectionectomy was considered more difficult than four procedures in which three or more segments are removed.
Discussion
Forming a new classification
These data represent the first quantitative assessment of the perceived difficulty of a variety of liver resections. The results provide the mean score and confidence limits for twelve liver operations. Indeed they may be thought of as a difficulty/complexity score for these liver resections. While a Complexity Score for Liver Resections is obviously useful and may form the basis for quantitative methods in this area, a simple classification that groups the procedures is also desirable. The two procedures with the lowest scores form a statistically distinct group. This provides a cutpoint between these procedures and the ten with higher scores. A statistically distinct division cannot be made for the ten procedures with the highest scores because there is no significant difference between one member of this group and another ranked just above or below it. However, statistically significant differences do exist for the lower and higher members of that group. As a result, a cutpoint for this group must be selected on a different basis. The four procedures with the highest scores share the common attribute that they are resections through the right intersectional plane. They are also more complex than right posterior sectionectomy, the only other procedure included that traverses that plane. The two variants of left trisectionectomy are much larger resections than right posterior sectionectomy, and both right anterior sectionectomy and middle hepatectomy require an additional resection plane. Thus, although somewhat arbitrary, a cutpoint for classification that separates the ten more difficult procedures into six intermediate and four highly-complex resections is reasonable. This provides a three-level classification.
Selecting the names for the three groups is of importance. The classical division into minor and major is disadvantageous in that “minor” in the English language has the connotation of inconsequential, slight, or trivial. The terms small, medium, and large might be considered, but they relate to size which is clearly not the chief determinant of the scores obtained. The terms Low Complexity, Medium Complexity and High Complexity seem to come closest to what one would want to convey in this classification. Low Complexity will contain the two lowest ranks, Medium Complexity will refer to the six next highest ranks, and High Complexity to the highest four ranks (Table 3).
Table 3.
A New Classification for the Complexity of Liver Resections
| Group | Resection (mean difficulty [1-10]) |
|---|---|
| Low complexity | Peripheral wedge resection (1.37) Left lateral sectionectomy (2.01) |
| Medium complexity | Left hepatectomy without caudate (4.24) Right hepatectomy (4.92) Right posterior sectionectomy (5.49) Left hepatectomy with caudate (5.53) Isolated caudate resection (5.90) Right trisectionectomy (6.24) |
| High complexity | Right anterior sectionectomy (6.68) Middle hepatectomy (7.22) Left trisectionectomy without caudate resection (7.58) Left trisectionectomy with caudate resection (8.28) |
Not all liver resections have been scored in this survey. Each expert was asked to weigh 10 procedures. It was felt that this was the maximum number of procedures that experts should be asked to process at one time and that the addition of extra variables in the survey would reduce the response rate. However, there are other factors that influence the complexity of liver resections such as the need for concomitant bile duct resection and hepatico-jejunostomy or the need for vascular resections and reconstructions. There are also other procedures that were not assessed such as monosegmentectomies and bisegmentectomies other than those included. Corresponding laparoscopic procedures also need to be evaluated. These variables can be tested in further surveys that include appropriate examples. This study can act as a standard by which adjustments may be made.
Limitations of the study
Although the responders to the two surveys were chosen at random, there are slight differences in the two groups with respect to current activity, career experience, and country of practice. As aforementioned, responders from Group 1 were less experienced than those from Group 2. This required an unexpected need for adjustment of scores. However, the adjustment was relatively minor and based on reasonable methods.
An arbitrary cutpoint had to be used to create the upper division of the classification. It is possible that statistically significant separations between each of the 10 most complex procedures would have been found if the survey had a larger number of respondents. In that event, though, other criteria for cutpoints would still be needed or a multi-level classification would result. In this study, the upper cutpoint was not based on a statistical separation but was instead based on the perceived complexity of procedures that pass through the right intersectional plane. Another approach might have been to divide the 12 procedure solely based upon score (e.g. 1.00-3.99, 4.00-6.99 and 7.00 -10.00). This did not seem less arbitrary.
The response rate in this study approached 50% but was less than optimal. A clear majority of the respondents came from countries in which English is a national language. In these countries, the response rate was 63%. By contrast, a low response rate of 24% was obtained from countries such as China and Japan in which English was not a national language. This was likely in part due to the selection of experts from the English language literature. The results suggest that the response rate was principally limited by language difficulties, and that translating this survey into multiple languages from the outset may have been productive. This is unlikely in our opinion to impact the findings of the study. Though the language limitation affected the number of respondents, surgeons’ perceptions of the difficulty of liver resection are not likely correlated with native language. Thus although a limitation it is unlikely to be a serious limitation.
A final limitation of the study is that it is purely technical and thus does not relate to the morbidity and mortality of liver resection. Multiple studies have shown that morbidity and mortality in liver resection are associated with multiple preoperative and intraoperative variables including but not limited to age, extent of resection, preoperative comorbidities, blood loss/transfusion, background liver disease (cirrhosis and cholestasis), and concomitant procedures (13-18). Thus, the technical complexity of a procedure is not necessarily aligned with its morbidity and patient outcomes, but that issue might be studied in subsequent studies Studies such as this one that formally assess the difficulty of various liver resections are necessary in order to make these associations. Though this study is subjective in nature, it provides a relatively simple, generalizable classification derived quantitatively that can be referenced easily in studies associating outcome with technical complexity.
Conclusions
This study for the first time quantitatively separates liver resections into three categories of complexity. Peripheral wedge resection and left lateral sectionectomy represent the only liver resections of low complexity, while resections involving the right intersectional plane are viewed as the most complex. Contrary to prior inferences, the number of segments does not alone reflect the complexity of a resection
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information:
Brief Title: Perceived Complexity of Liver Resections
References
- 1.Lortat-Jacob JL, Robert HG. [Well defined technic for right hepatectomy]. La Presse medicale. 1952 Apr 16;60(26):549–51. PubMed PMID: 14948909. Hepatectomie droite reglee. [PubMed] [Google Scholar]
- 2.Couinaud C. Etudes Anatomiques et Chirugicales. Masson & Cie; Paris: 1957. Le foie. 1957. [Google Scholar]
- 3.Goldsmith NA, Woodburne RT. The surgical anatomy pertaining to liver resection. Surg Gynecol Obstet. 1957;105:310–318. PubMed PMID: 13467662. [PubMed] [Google Scholar]
- 4.Bismuth H, Houssin D, Castaing D. Major and minor segmentectomies “reglees” in liver surgery. World J Surg. 1982;6:10–24. doi: 10.1007/BF01656369. PubMed PMID: 7090385. [DOI] [PubMed] [Google Scholar]
- 5.Bismuth H. Surgical anatomy and anatomical surgery of the liver. World J Surg. 1982;6:3–9. doi: 10.1007/BF01656368. PubMed PMID: 7090393. [DOI] [PubMed] [Google Scholar]
- 6.DeMatteo RP, Palese C, Jarnagin WR, et al. Anatomic segmental hepatic resection is superior to wedge resection as an oncologic operation for colorectal liver metastases. J Gastrointest Surg. 2000;4:178–184. doi: 10.1016/s1091-255x(00)80054-2. PubMed PMID: 10675241. [DOI] [PubMed] [Google Scholar]
- 7.Liau KH, Blumgart LH, DeMatteo RP. Segment-oriented approach to liver resection. The Surg Clin North Am. 2004;84:543–561. doi: 10.1016/j.suc.2003.12.003. PubMed PMID: 15062661. [DOI] [PubMed] [Google Scholar]
- 8.Billingsley KG, Jarnagin WR, Fong Y, Blumgart LH. Segment-oriented hepatic resection in the management of malignant neoplasms of the liver. J Am Coll Surg. 1998;187:471–481. doi: 10.1016/s1072-7515(98)00231-2. PubMed PMID: 9809562. [DOI] [PubMed] [Google Scholar]
- 9.Bismuth H, Chiche L. Surgery of hepatic tumors. Progr Liver Dis. 1993;11:269–285. PubMed PMID: 8272515. [PubMed] [Google Scholar]
- 10.Couinaud C. [Contribution of anatomical research to liver surgery]. France Medecine. 1956;19:5–12. PubMed PMID: 13344728. Contribution de la recherche anatomique a la chirurgie du foie. [PubMed] [Google Scholar]
- 11.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. PubMed PMID: 3719049. [PubMed] [Google Scholar]
- 12.Benjamini YaH Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Statist Soc Series B. 1995;57:289–300. [Google Scholar]
- 13.Jarnagin WR, Gonen M, Fong Y, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 2002;236:397–406. doi: 10.1097/01.SLA.0000029003.66466.B3. discussion -7. PubMed PMID: 12368667. Pubmed Central PMCID: 1422593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Belghiti J, Hiramatsu K, Benoist S, et al. Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg. 2000;191:38–46. doi: 10.1016/s1072-7515(00)00261-1. PubMed PMID: 10898182. [DOI] [PubMed] [Google Scholar]
- 15.Dokmak S, Fteriche FS, Borscheid R, et al. 2012 Liver resections in the 21st century: we are far from zero mortality. HPB. 2013 Mar 6; doi: 10.1111/hpb.12069. PubMed PMID: 23461811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Erdogan D, Busch OR, Gouma DJ, van Gulik TM. Morbidity and mortality after liver resection for benign and malignant hepatobiliary lesions. Liver Int. 2009;29:175–180. doi: 10.1111/j.1478-3231.2008.01806.x. PubMed PMID: 18564213. [DOI] [PubMed] [Google Scholar]
- 17.Poon RT, Fan ST, Lo CM, et al. Improving perioperative outcome expands the role of hepatectomy in management of benign and malignant hepatobiliary diseases: analysis of 1222 consecutive patients from a prospective database. Ann Surg. 2004;240:698–708. doi: 10.1097/01.sla.0000141195.66155.0c. discussion 710. PubMed PMID: 15383797. Pubmed Central PMCID: 1356471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cescon M, Vetrone G, Grazi GL, et al. Trends in perioperative outcome after hepatic resection: analysis of 1500 consecutive unselected cases over 20 years. Ann Surg. 2009;249:995–1002. doi: 10.1097/SLA.0b013e3181a63c74. PubMed PMID: 19474679. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.