Abstract
Background
Since the National Expanded Program on Immunization was implemented in China, considerable progress has been made in reducing the incidence of measles. However, the incidence of measles increased again in 2004. Few post-marketing studies on measles vaccine effectiveness were reported in China. In this study, we aimed to describe the measles epidemic and to evaluate the effectiveness of the measles vaccine in Guangzhou, southern China.
Methods
Based on the surveillance data for measles, we investigated the epidemiology during different periods between 1951 and 2012. We analyzed the clinical characteristics of laboratory-confirmed cases of measles between 2009 and 2012 and conducted a case-control study using test-negative cases as controls. We determined the protective effect of measles vaccine.
Results
The highest annual incidence in Guangzhou was 2187.15/100 000 in 1964, and the lowest was 0.32/100 000 in 2011. The average incidence of measles from 1951 to 2012 was 306.27/100 000. There was a significant tendency of decline in recent years. From 2009 to 2012, there are 700 laboratory-confirmed cases reported with an average onset age of 2.5 (median) years. The non-vaccinated target population (age <8 months and ≥15 years) accounted for 56.7% of the cases. The transient (non-resident) population accounted for 51.3% of the cases. Fewer cases were observed in the population targeted for measles vaccine (aged 8 months to 14 years). The effectiveness of a single dose of the measles vaccine was 89.1% (95% confidence interval (CI), 44.5–97.9), and the effectiveness of ≥2 doses of the measles vaccine was 97.8% (95% CI, 88.3–99.6) in children aged 8 months to 14 years old.
Conclusions
There is a significant overall decline in the incidence of measles (including clinical and laboratory confirmed cases) in the measles vaccine targeted population in Guangzhou. Two doses of measles vaccine are more effective than one dose in preventing measles in China. In order to accelerate the elimination of measles, vaccination should also be given to the transient and the non-vaccine targeted population.
Keywords: measles epidemic, measles elimination, vaccine effectiveness, case-control studies, China
Introduction
Measles is a highly contagious infectious disease caused by the measles virus. The unvaccinated population is at a high risk of measles and its severe complications, such as pneumonia, diarrhea, and encephalitis. Before widespread vaccination, measles caused an estimated 2.6 million deaths worldwide each year. Although a safe and cost-effective vaccine is available, measles remains one of the leading causes of death among young children.1-4 More than 95% of measles deaths occur in low-income countries with weak health infrastructures. Despite the considerable global effort to eliminate measles, there were 158 000 measles deaths globally in 2011.5,6
Humans are the only animal host for the measles virus. Infected individuals can acquire long-lasting immunity. The measles vaccine has been used worldwide and has significantly reduced the incidence of measles. The local transmission of the measles virus has been successfully decreased in certain developed countries. Similar to smallpox, it is possible to completely eliminate measles from the world. The measles-rubella (MR) Initiative, a collaborative effort of World Health Organization (WHO), United Nations International Children's Emergency Fund (UNICEF), and the United Nations Foundation, has set global goals to (1) reduce global measles deaths by at least 95% compared with the level of 2000; (2) achieve regional measles and rubella/congenital rubella syndrome (CRS) elimination goals by the end of 2015; (3) eliminate measles and rubella in at least 5 WHO regions by the end of 2020.6
The HU-191 and CHANG-47 measles vaccine strains developed in China have been used since 1966. The HU-191 strain has been one of the most commonly used measles vaccines in the world, covering 80% of the population of China.7 A 15-y follow up study conducted in Zhuji, China showed that the duration of immunity produced by the HU-191 and CHANG-47 measles vaccines was not inferior to the vaccines of the Schwarz or L-16 strain.8
The genotype of measles is relatively stable in China; the H1a genotype has been the predominant subtype of measles since 2000 in mainland China.9,10 The measles vaccine has been used in China since 1967. In 1986, the national Expanded Program on Immunization (EPI), which used a 2-dose monovalent measles vaccine schedule, was implemented in China. In this vaccine schedule, the first dose of the vaccine was given to children at 8 mo of age (monovalent attenuated vaccine), and the second dose being given at 7 y of age (monovalent vaccine or MR or measles-mumps-rubella/MMR vaccine).11 Subsequently in 2006, the second dose of measles vaccine has been administered at 18–24 mo of age. The measles vaccination is mandatory by the Chinese government for children aged from 8 mo to 14 y of age. All measles vaccinations are provided at no cost. The measles vaccination is usually performed by community health practitioners, and includes routine vaccination, follow-up Supplement Immunity Activities (SIAs), catch-up SIAs and school-based vaccination. The objective of SIAs is to increase population immunity by reaching those children who were not reached through the routine immunization program and immunizing those children that were reached through routine services but did not seroconvert. The coverage of the measles vaccination is routinely reported as high (>90%) and is typically monitored by random-cluster sampling, as recommended by the WHO.
In Guangzhou immunization records of children less than 7 y of age are registered in the Children’s EPI Administrative Computerized System since 1997. However, there were a number of transient (non-resident) children coming from other cities to Guangzhou, and the majority of these children are not registered in the EPI system. As a result, vaccination information data collected in the field investigation usually include vaccination from records, vaccination recalled from guardians’ memory, and missing vaccination history with uncertain sources.
Guangzhou is an economic, educational, and cultural hub in southern China. Guangzhou city has a sub-tropical climate, a permanent population of 7.94 million residents, a transient population of 4.67 millions and 60 000 births each year. The morbidity of measles shows a seasonal variation as in temperate climates, measles outbreaks typically occur in the late winter and early spring every year, whereas in the tropics, measles outbreaks have variable associations with rainy seasons, suggesting that climatic factors partly underlie the seasonality of measles virus infections.
Since the National Expanded Program on Immunization was implemented in China, considerable progress has been made in reducing the incidence of measles. However, the incidence of measles began to increase again in 2004. To achieve the goal of measles elimination in 2012, the accelerated measles elimination campaign including enhanced routine vaccination and contiguous vaccination was launched in Guangzhou since 2006. Also, few post-marketing studies on measles vaccine effectiveness were reported in China. In this study, we report the incidence of measles between 1951 and 2012 and described the epidemiological characteristics of the laboratory-confirmed cases between 2009 and 2012 to evaluate the effectiveness of measles vaccine. We found that there is a significant overall decline in the incidence of measles in the measles vaccine targeted population in Guangzhou.
Results
Measles incidence
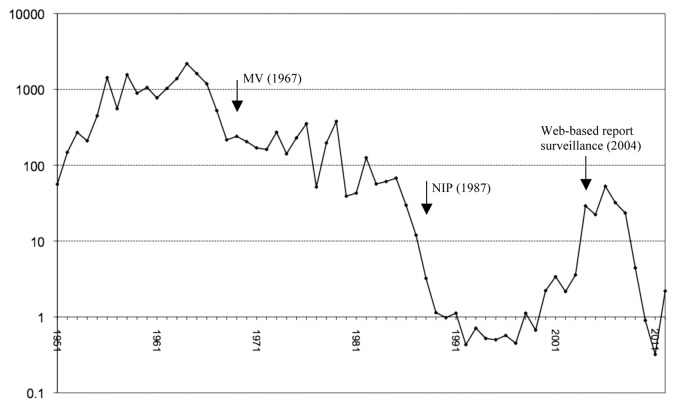
Figure 1 shows a significant overall declining trend in the incidence of measles in Guangzhou (including clinical and laboratory confirmed cases) between 1951 and 2012 with an average incidence of 306.27/100 000 people. The highest annual incidence was 2187.15/100 000 in 1964, and the lowest one was 0.32/100,000 in 2011. The epidemic trend of measles can be divided into the following 4 stages: (1) a natural infectious stage between 1951 and 1966 (average incidence of 931.81/100 000), (2) a promotion of the vaccination stage between 1967 and 1985 (average incidence plunged to 186.81/100 000), (3) a planned regular vaccination stage between 1986 and 2005 (average incidence then dropped to 6.7/100 000), in which children routinely received the vaccination as the national EPI program recommended, and (4) an accelerated measles elimination stage between 2006 and 2012 (average incidence increased to 16.78/100 000). The seasonal distribution of measles is presented in Figure 2, with a peak incidence between January and April each year.
Figure 1. Semi-logarithmic graph of reported measles incidence rate (per 100 000) in Guangzhou city during 1951–2012). NIP, National Immunization Program.

Figure 2. Monthly distributions of measles cases in Guangzhou city from 1965 to 2012.
Seven hundred laboratory-confirmed cases were reported between 2009 and 2012 with an average onset age of 2.5 (median) years. Among these cases, the patients from 0 to 7 mo, aged 8 mo to 14 y and aged over 15 y accounted for 17.1% (120 cases), 43.3% (303 cases), and 39.6% (277 cases) of the reported cases, respectively. The transient and resident population accounted for 51.3% (359 cases) and 48.7% (341 cases) of the cases, respectively.
Vaccine effectiveness
We analyzed data from 578 patients (82.6% of 700 cases) who were greater than 8 mo of age during 2009 to 2012 in Guangzhou (Table 1). We used individuals who were seronegative for measles as controls. The basic demographic characteristics were similar between the case group and control group. The study subjects with immunization recalled from guardians’ memory, written immunization, and an uncertain source of immunization history accounted for 26.3% (152 cases), 27.3% (158 cases), and 46.4% (268 cases) of the cases, respectively. The subjects in the case group who received measles vaccine accounted for 20.3% of the cases (11.8% received single doses of the measles vaccine, and 8.5% received at least 2 doses of measles vaccine). The subjects in the control group who received the measles vaccine accounted for 64.6% (22.9% received single doses, and 41.7% received 2 or more doses).
Table 1. Demographic characteristics of study subjects.
| Case (n = 482) | Control (n = 96) | χ2 | P | |
|---|---|---|---|---|
| Age | 60.172 | <0.001 | ||
| 0 to 7 mo | 115 (23.9) | 0 | ||
| 8 mo to 14 y | 257 (53.3) | 40 (41.7) | ||
| 15 y | 110 (22.8) | 56 (58.3) | ||
| Gender | 1.631 | 0.202 | ||
| Male | 285 (59.1) | 50 (52.1) | ||
| Household register location | 14.200 | <0.001 | ||
| Local | 235 (48.8) | 67 (69.8) | ||
| Vaccine dose | ||||
| 1 dose* | 57 (11.8) | 22 (22.9) | 25.828 | <0.001 |
| ≥2 doses* | 41 (8.5) | 40 (41.7) | 91.403 | <0.001 |
| 0 dose | 384 (79.7) | 34 (35.4) | ||
1 or ≥2 doses vs. 0 dose.
Eighty-nine subjects had an immunization record reporting the specific dates, including 77.5% (69 cases) who received their first dose of the vaccine before 1 y of age, 5.6% (5 cases) who received it before 2 y of age, and 9.0% (8 cases) who received it between 3 and 14 y of age. Among these 89 subjects, 22.5% (20 cases) received the second dose of the vaccine before 2 y of age, and 5.6% (5 cases) received the second dose between 3 and 14 y of age. The remaining subjects either received the measles vaccine after 15 y of age, or the specific dates of immunization were not available. Among the breakthrough cases, the time period between the vaccination and onset of illness was 1.05 ± 1.83 y in the group of 8-mo-old to 14-y-old and 13.23 ± 8.34 y in those older than 15 y of age.
After adjusting for age, validation of immunization records and household register location, the effectiveness of the single-dose measles vaccine was 89.1%, and the effectiveness of the two-dose measles vaccine was 97.8% in individuals between 8 mo and 14 y of age (Table 2). No protective effect was observed for people older than 15 y (–52.8%, 95% confidence interval [CI], –354.9 to 48.7).
Table 2. Measles vaccine effectiveness by dose (8 mo to 14 y old)*.
| OR (95%CI) | VE (%, 95%CI) | |||
|---|---|---|---|---|
| Crude | Adjusted | Crude | Adjusted | |
| 1 vs. 0 Dose | 0.081 (0.020, 0.317) | 0.109 (0.021, 0.555) | 91.9 (68.3, 98.0) | 89.1 (44.5, 97.9) |
| 2 vs. 0 Dose | 0.017 (0.005, 0.060) | 0.022 (0.004, 0.117) | 98.3 (94.0, 99.5) | 97.8 (88.3, 99.6) |
| ≥1 Dose vs. 0 Dose | 0.031 (0.009, 0.104) | 0.053 (0.012, 0.238) | 96.9 (89.6, 99.1) | 94.8 (76.2, 98.8) |
Adjusted by age, validation of immunization records, and household register location.
Discussion
We evaluated the epidemiology of measles between 1951 and 2012 in Guangzhou in southern China and analyzed the effectiveness of the measles vaccine based on laboratory-confirmed cases between 2009 and 2012. This study demonstrated that children who received measles vaccine at the vaccination-targeted age between 8 mo to 14 y had a lower incidence of measles. While higher incidence of measles was observed in those non-vaccination target population at age less than 8 mo or over 15 y old, as well as in the transient population. In addition, a two-dose measles vaccine provided at least 95% protection for the population aged from 8 mo to 14 y. Thus measles vaccine should also be given to the nonvaccination target population in order to accelerate the elimination of measles.
The analysis presented in this study indicated that the occurrence of measles in infants younger than 8 mo accounted for nearly one-fourth of all cases. Antibodies to the measles virus in infants are passively acquired from the mother. Because the current generation of mothers was born in the period when the city had a regular vaccination plan for every child, the maternal antibodies acquired from vaccination might have decreased as the women aged. Similar to other countries, infants in China are susceptible to measles infection due to insufficient antibodies prior to receiving the first dose of the vaccine within the first year of life.12,13 Our analysis indicated that the cases of measles in individuals older than 15 y accounted for approximately 23% of all cases between 2009 and 2012, similar to other developed countries where measles has been well-controlled.14-16 By increasing the vaccination rate in the target population for measles vaccination (8 mo and 14 y of age), a decrease in the incidence of measles was observed in individuals older than 15 y of age over time. The shift in the age distribution of measles is one of the events that occur prior to the stage of disease elimination.17,18
Our results indicated that the transient population is a major target of the measles virus, as they accounted for about one-half of the total cases. China has undergone a remarkable period of rapid socio-economic development and urbanization. Guangzhou is a city with a large transient population, which accounting for nearly 40% of 12.6 million people; and because Guangzhou’s rapid economic growth and relatively low cost of living, it has attracted a considerable portion of its population from other regions. With the exception of a small portion of the population with a high socio-economic status, including managers and technical personnel, the vast majority of the transient population works in manual labor, and many of these people emigrated from other places. In addition, the winter weather in Guangzhou is mild and thus it is suitable for the transient population. Typically, individuals of the transient population generally have a lower living standard, a lack of awareness regarding the needs of vaccination for their children and a tendency to ignore the mandatory vaccinations that are legally required for children in their resident regions. The transient population has become a major challenge in terms of eliminating measles in China.19 The measles vaccination rate varies among the population at different socio-economic levels.20 Children who are difficult to identify using a standard protocol should be the real target population for the vaccination program.
The measles vaccine is one of the first vaccinations required by the Chinese government. We used individuals who were seronegative for measles as controls to improve the efficacy of the study. If we randomly selected our controls from a general population in the immunization registry system, it is likely that the included controls have been immunized with at least 2 doses of a measles vaccine; therefore, the estimation of the vaccine effectiveness might be inaccurate. The study design is different from our previous study regarding the second class of vaccines, which are not provided free of charge.21-23 All suspected cases of measles were confirmed by a serological test, which provided us with the opportunity to calculate the effectiveness of the measles vaccine. Controls without measles were excluded from the same test as cases. Case and test-negative controls may be comparable to exposure to measles. Therefore, using test-negative controls may reduce the unclear or unmeasurable confounders in the study.
Our results indicated that the marketed measles vaccine indicated in the individuals between 8 mo and 14 y of age, the effectiveness of 1 or 2 or more doses of the vaccine was 89.1% and 97.8%, respectively. These results suggested that the measles vaccine has a high level of efficacy, consistent with serological studies. As most measles vaccinations were administered before the age of 2 y, the protective effects of the vaccine are reduced in the adult population. A serological study has reported that the protective effects of the vaccine can be sustained for approximately 20 y when the measles virus is in circulation in the environment.24
We used the test-negative cases as controls to evaluate the effectiveness of the vaccine, an approach that is less susceptible to bias due to misclassification of infection and to confounding by health care-seeking behavior, which is relative to traditional case-control or cohort studies. The caveat associated with the test-negative design is the additional, difficult-to-test assumptions that the incidence of non-measles virus infections is similar between the vaccinated and unvaccinated groups within any stratum of care-seeking behavior, and that the vaccine effectiveness does not vary across care-seeking strata.25 The methodology in our study appears to be valid for vaccine effectiveness, especially as the overall incidence of measles was low during the study period suggesting that the odds ratio (OR) could provide a good estimation of relative risk (RR).
This study has several limitations. The measles cases reported between 1951 and 2004 are mainly based on the record of clinical diagnosis; thus, the disease description might not be specific and accurate. We did not access the measles vaccination history in 33% percent of the study subjects, which may lead to a bias on the efficacy of the vaccine in our study.13 The measles cases from the surveillance system were reported by physicians in this city. Finally, there is a possibility that physicians did not report some measles cases. These factors may result from a biased selection of cases and an incompleteness of the surveillance system in Guangzhou, which may affect the validity of the vaccine effectiveness in our study.
In addition, the sample size of the control group is relatively small in that most of the suspected measles cases were confirmed by the laboratory, which might reduce the study accuracy. Only 40 suspected cases from ages 8 mo to 14 y were enrolled as controls in our analysis, which is significantly less than the sample size of case group (257). This would also lead to bias. The measles vaccination is mandated in China, as a result, it was not possible to do this study using the immunization population registry to find unvaccinated persons as controls. So we take negative cases enrolled in the field investigation as controls in the study, who may not usually receive the measles vaccine as required.
Although considerable progress has been made in reducing the incidence of measles, the process of eliminating measles still faces many challenges in China. Our study showed that the measles vaccination is still the effective way for the elimination of measles from the population. We believe that the schedule of a two-dose immunization is appropriate and suitable in China. To strengthen regular immunization and improve the sensitivity and specificity of the measles surveillance system, a government-led, cooperative effort from multiple departments should be continuously implemented with an emphasis to reinforce vaccination among the transient population and reduce the measles incidence in the non-immunized target population.
Methods
Measles epidemic from 1951 to 2012
Measles is one of the statutory notifiable infectious diseases, as outlined by law in China. Doctors and other medical professionals from any medical institution in Guangzhou are required to report measles cases within a specified time period. The diagnosis should include clinical diagnosis and laboratory diagnosis. From 1951 to 2003, information regarding statutory notifiable infectious diseases was reported by medical institutes to the Guangzhou Center for Disease Control and Prevention (CDC) on a monthly basis. The direct network reporting system has been applied since 2004.
We calculated the annual number of measles cases divided by annual population reported by the Guangzhou Bureau of Statistics. The incidence of measles between 1951 and 2012 is presented as a semi-logarithmic graph. The measles case surveillance system was based on all hospitals or health communities located in 12 districts of Guangzhou City. The out-patients or in-patients who had body temperature ≥38 °C accompanied by dermal eruptions were identified as suspected cases of measles. We analyzed individual cases of serologically confirmed measles (IgM positive) between 2009 and 2012 and presented the incidence of measles for different age groups (0–7 mo-old, 8-mo to 14-y-old and over 15-y-old).
Vaccine effectiveness case-control study
A case-control study was conducted based on all suspected measles cases with laboratory diagnosis during 2009 to 2012 in Guangzhou. Within 4 to 28 d after eruption of rash, the time that IgM antibody begin to occur in the serum of measles patients, serum samples were collected from these suspected cases for further serological surveillance in 2 hospitals (Guangzhou infectious Disease Hospital and Guangzhou Women and Children’s Medical Center) and in the CDCs of the 12 districts of Guangzhou city. All detection reagents were obtained from the Guangzhou City CDC and quality controls were performed annually. Cases were confirmed serologically by enzyme-linked immunosorbent assay for measles-specific IgM antibodies. The controls were individuals who were serologically negative for measles. Measles vaccination information was obtained (recalled from guardians’ memory or written immunization record) in the field investigation. We determined the incidence of measles in different populations receiving the measles vaccine, and we calculated the effectiveness of the measles vaccine in each group. The measles vaccination (measles or MMR vaccine) status was categorized into one dose, two doses, or unvaccinated. Measles vaccination information collected usually included: (1) vaccination from electronic records, (2) vaccination recalled from guardians’ memory, and (3) missing vaccination history with uncertain sources. We gave priority to electronic vaccination registry. If the guardians failed to recall the measles vaccine information or the immunization record was unavailable, the measles vaccine vaccination information was defined as missing. Only vaccinations received at least 3 wk before the onset of disease were considered valid.
We defined the measles vaccine effectiveness as the proportional reduction in the risk of illness associated with vaccination among vaccine recipients. This value was estimated using a formula developed by Greenwood and Yule (1- RR).26 The vaccine effectiveness was calculated as one minus the OR × 100%, substituting the OR for the RR in the above formula, where the odds of confirmed measles among the vaccinated subjects was compared with the odds of measles among the unvaccinated subjects. We used binary, unconditional logistic regression to calculate the ORs and 95% confidence intervals (CIs). The model was adjusted by age, validation of immunization records, and household register location, which were selected by univariate analysis. The data analysis was conducted using SPSS statistical software (Version 13.0, SPSS, Inc.). We used χ2 and t tests to compare the characteristics of each group. For all analyses, P values less than 0.05 were regarded as significant. The ethics committee of Guangzhou City CDC reviewed and approved this protocol.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
Funding
This work was supported by grants from the Guangdong Provincial Department of Science and Technology (2012B091100045), Science and information Technology of Guangzhou (2012J5100005).
Acknowledgments
We appreciate the participation of all enrollees in this study. We wish to give special thanks to the coordinators and nurses in the public unit of surveillance hospitals in Guangzhou. We also thank the Project For Key Medicine Discipline Construction Of Guangzhou Municipality (2013-2015-07) for their contribution in the study.
References
- 1.Atkinson WL. . Epidemiology and prevention of measles. Dermatol Clin 1995; 13:553 - 9; PMID: 7554503 [PubMed] [Google Scholar]
- 2.Campbell H, Andrews N, Brown KE, Miller E. . Review of the effect of measles vaccination on the epidemiology of SSPE. Int J Epidemiol 2007; 36:1334 - 48; http://dx.doi.org/ 10.1093/ije/dym207; PMID: 18037676 [DOI] [PubMed] [Google Scholar]
- 3.Duke T, Mgone CS. . Measles: not just another viral exanthem. Lancet 2003; 361:763 - 73; http://dx.doi.org/ 10.1016/S0140-6736(03)12661-X; PMID: 12620751 [DOI] [PubMed] [Google Scholar]
- 4.Perry RT, Halsey NA. . The clinical significance of measles: a review. J Infect Dis 2004; 189:Suppl 1 S4 - 16; http://dx.doi.org/ 10.1086/377712; PMID: 15106083 [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC). . Measles--United States, 1999. MMWR Morb Mortal Wkly Rep 2000; 49:557 - 60; PMID: 10921493 [PubMed] [Google Scholar]
- 6.World Health Organization. Measles. 2013. Available from: http://www.who.int/mediacentre/factsheets/fs286/en/
- 7.Wu T. . The history and present situation of measles in China. Chin J Epidemiol 2000; 21:63 - 6 [Google Scholar]
- 8.Dai B, Chen ZH, Liu QC, Wu T, Guo CY, Wang XZ, Fang HH, Xiang YZ. . Duration of immunity following immunization with live measles vaccine: 15 years of observation in Zhejiang Province, China. Bull World Health Organ 1991; 69:415 - 23; PMID: 1934235 [PMC free article] [PubMed] [Google Scholar]
- 9.Ma C, Liu H, An Z, Zhang P, Wen N, Xia W, Li L. . Analysis on Epidemiological Characteristics and Measures of Measles Control in China During 2006-2007. Zhongguo Yi Miao He Mian Yi 2008; 14:208 - 13 [Google Scholar]
- 10.Zhang Y, Ji YX, Zhu Z. . [Circulating pattern analysis for endemic measles viruses in mainland of China]. Zhongguo Yi Miao He Mian Yi 2009; 15:97 - 103; PMID: 20077650 [PubMed] [Google Scholar]
- 11.Yu X, Wang S, Guan J, Mahemuti, Purhati, Gou A, Liu Q, Jin X, Ghildyal R. . Analysis of the cause of increased measles incidence in Xinjiang, China in 2004. Pediatr Infect Dis J 2007; 26:513 - 8; http://dx.doi.org/ 10.1097/INF.0b013e31805ce299; PMID: 17529869 [DOI] [PubMed] [Google Scholar]
- 12.Leuridan E, Sabbe M, Van Damme P. . Measles outbreak in Europe: susceptibility of infants too young to be immunized. Vaccine 2012; 30:5905 - 13; http://dx.doi.org/ 10.1016/j.vaccine.2012.07.035; PMID: 22841972 [DOI] [PubMed] [Google Scholar]
- 13.Fu C, Xu J, Liu W, Zhang W, Wang M, Nie J, Rüdiger K. . Low measles seropositivity rate among children and young adults: a sero-epidemiological study in southern China in 2008. Vaccine 2010; 28:8219 - 23; http://dx.doi.org/ 10.1016/j.vaccine.2010.07.071; PMID: 20688039 [DOI] [PubMed] [Google Scholar]
- 14.Ma C, An Z, Hao L, Cairns KL, Zhang Y, Ma J, Cao L, Wen N, Xu W, Liang X, et al. . Progress toward measles elimination in the People’s Republic of China, 2000-2009. J Infect Dis 2011; 204:Suppl 1 S447 - 54; http://dx.doi.org/ 10.1093/infdis/jir103; PMID: 21666198 [DOI] [PubMed] [Google Scholar]
- 15.Rota MC, Massari M, Gabutti G, Guido M, De Donno A, Ciofi degli Atti ML. . Measles serological survey in the Italian population: interpretation of results using mixture model. Vaccine 2008; 26:4403 - 9; http://dx.doi.org/ 10.1016/j.vaccine.2008.05.094; PMID: 18585420 [DOI] [PubMed] [Google Scholar]
- 16.Velicko I, Müller LL, Pebody R, Gergonne B, Aidyralieva C, Kostiuchenko N, Spika JS. . Nationwide measles epidemic in Ukraine: the effect of low vaccine effectiveness. Vaccine 2008; 26:6980 - 5; http://dx.doi.org/ 10.1016/j.vaccine.2008.09.012; PMID: 18805455 [DOI] [PubMed] [Google Scholar]
- 17.Bernard H, Fischer R, Wild F. . Ongoing measles outbreak in southern Bavaria, Germany. Euro Surveill 2008; 13:8002; PMID: 18445381 [PubMed] [Google Scholar]
- 18.Wichmann O, Siedler A, Sagebiel D, Hellenbrand W, Santibanez S, Mankertz A, Vogt G, Treeck Uv, Krause G. . Further efforts needed to achieve measles elimination in Germany: results of an outbreak investigation. Bull World Health Organ 2009; 87:108 - 15; http://dx.doi.org/ 10.2471/BLT.07.050187; PMID: 19274362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fu C, Wang M, Liang J, He T, Wang D, Xu J. . Effectiveness of Lanzhou lamb rotavirus vaccine against rotavirus gastroenteritis requiring hospitalization: a matched case-control study. Vaccine 2007; 25:8756 - 61; http://dx.doi.org/ 10.1016/j.vaccine.2007.10.036; PMID: 18023510 [DOI] [PubMed] [Google Scholar]
- 20.Nagaoka K, Fujiwara T, Ito J. . Do income inequality and social capital associate with measles-containing vaccine coverage rate?. Vaccine 2012; 30:7481 - 8; http://dx.doi.org/ 10.1016/j.vaccine.2012.10.055; PMID: 23107596 [DOI] [PubMed] [Google Scholar]
- 21.Fu C, He Q, Xu J, Xie H, Ding P, Hu W, Dong Z, Liu X, Wang M. . Effectiveness of the Lanzhou lamb rotavirus vaccine against gastroenteritis among children. Vaccine 2012; 31:154 - 8; http://dx.doi.org/ 10.1016/j.vaccine.2012.10.078; PMID: 23127516 [DOI] [PubMed] [Google Scholar]
- 22.Fu C, Liang J, Wang M. . Matched case-control study of effectiveness of live, attenuated S79 mumps virus vaccine against clinical mumps. Clin Vaccine Immunol 2008; 15:1425 - 8; http://dx.doi.org/ 10.1128/CVI.00122-08; PMID: 18667635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fu C, Wang M, Liang J, Xu J, Wang C, Bialek S. . The effectiveness of varicella vaccine in China. Pediatr Infect Dis J 2010; 29:690 - 3; http://dx.doi.org/ 10.1097/INF.0b013e3181d7380e; PMID: 20216242 [DOI] [PubMed] [Google Scholar]
- 24.Kontio M, Jokinen S, Paunio M, Peltola H, Davidkin I. . Waning antibody levels and avidity: implications for MMR vaccine-induced protection. J Infect Dis 2012; 206:1542 - 8; http://dx.doi.org/ 10.1093/infdis/jis568; PMID: 22966129 [DOI] [PubMed] [Google Scholar]
- 25.Jackson ML, Nelson JC. . The test-negative design for estimating influenza vaccine effectiveness. Vaccine 2013; 31:2165 - 8; http://dx.doi.org/ 10.1016/j.vaccine.2013.02.053; PMID: 23499601 [DOI] [PubMed] [Google Scholar]
- 26.Greenwood M, Yule GU. . The Statistics of Anti-typhoid and Anti-cholera Inoculations, and the Interpretation of such Statistics in general. Proc R Soc Med 1915; 8:Sect Epidemiol State Med 113 - 94; PMID: 19978918 [DOI] [PMC free article] [PubMed] [Google Scholar]